Psycho-Social Factors in Patients with Cardiovascular Disease Attending a Family-Centred Prevention and Rehabilitation Programme: EUROACTION Model in Spain
Abstract
1. Introduction
2. Materials and Methods
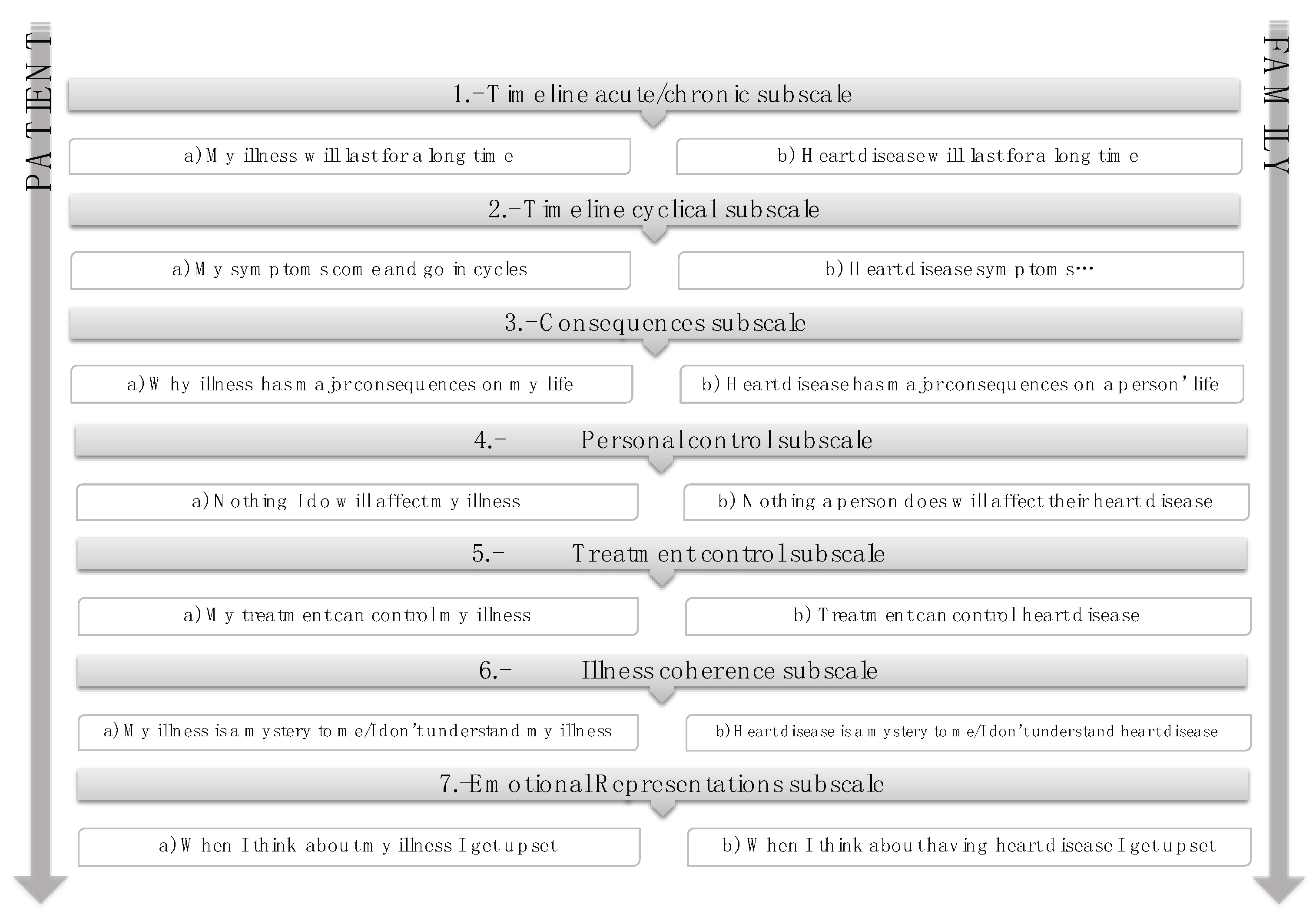
- Self-Administered Questionnaires
2.1. Measurement of Biochemical Markers
2.2. Sociodemographic and Clinical Variables
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Study Population
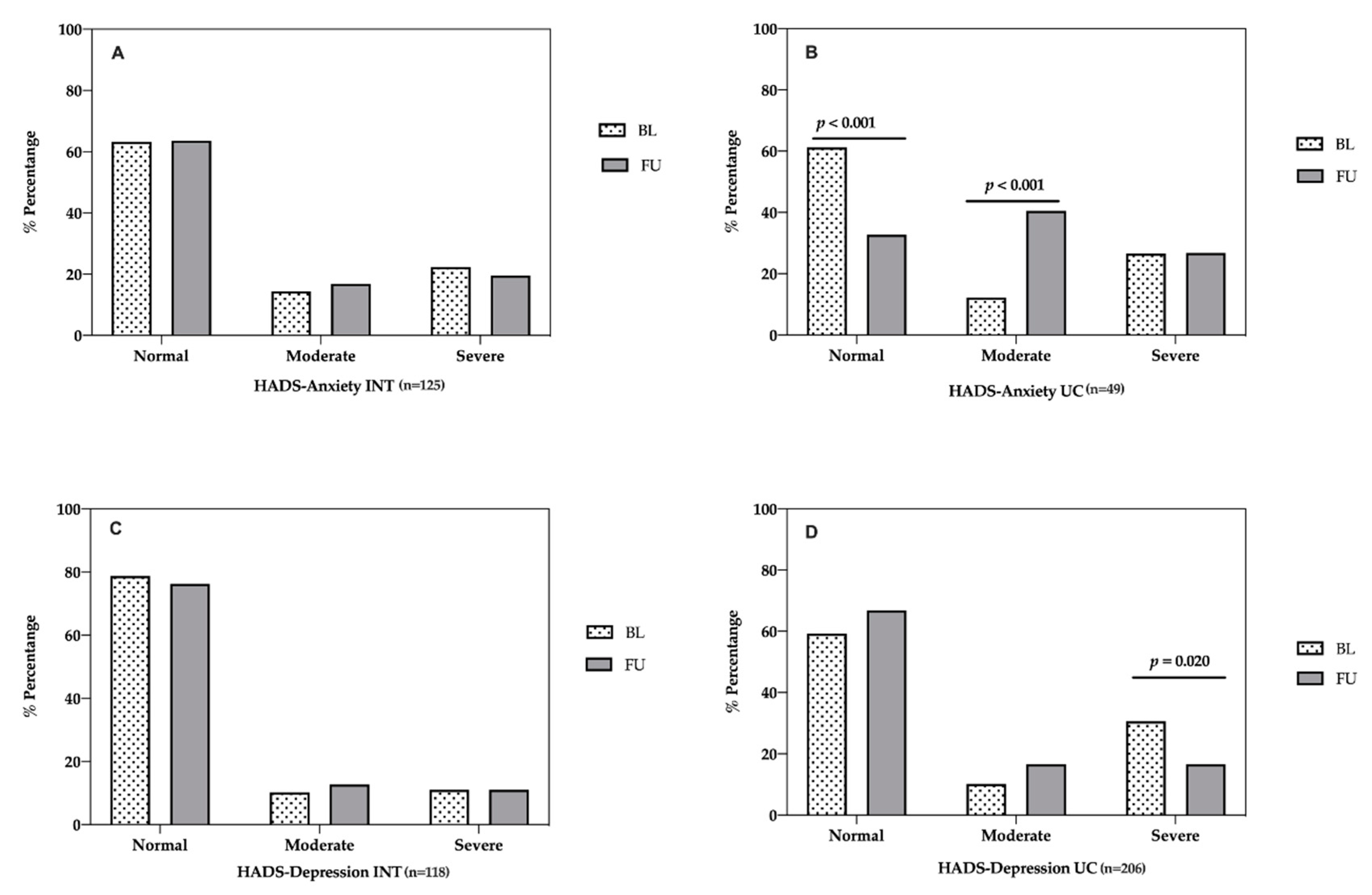
3.2. Evaluation of Psycho-Social Factors in the Study Sample
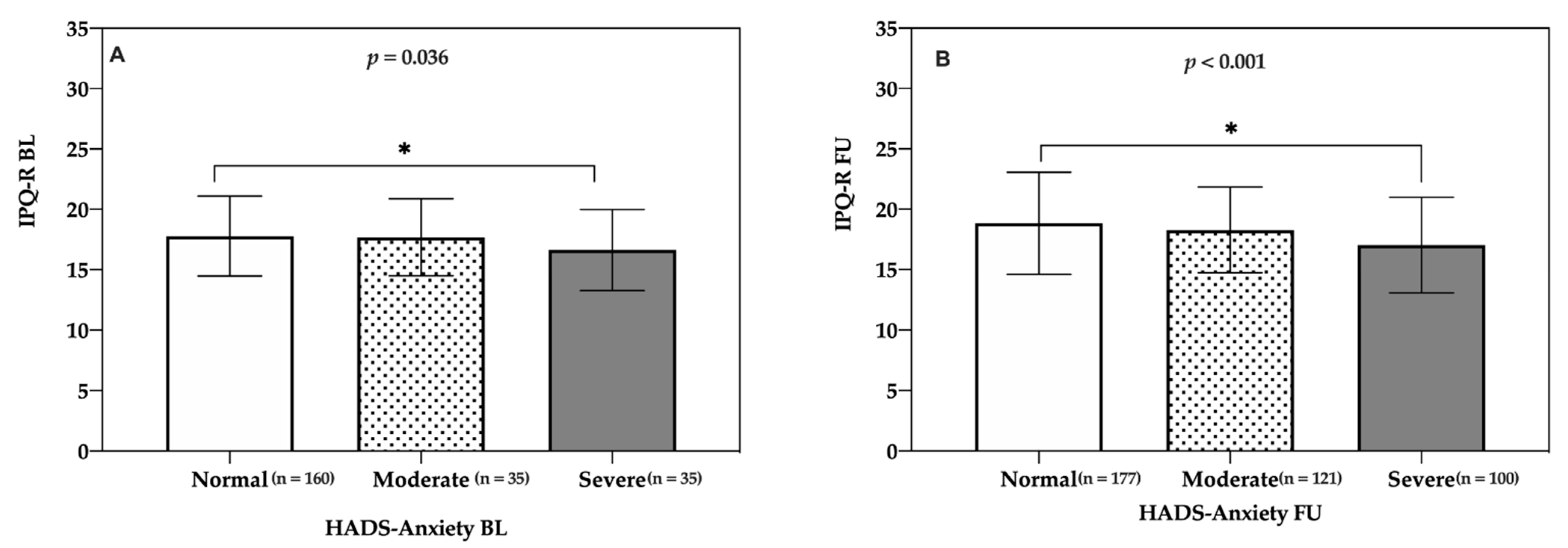
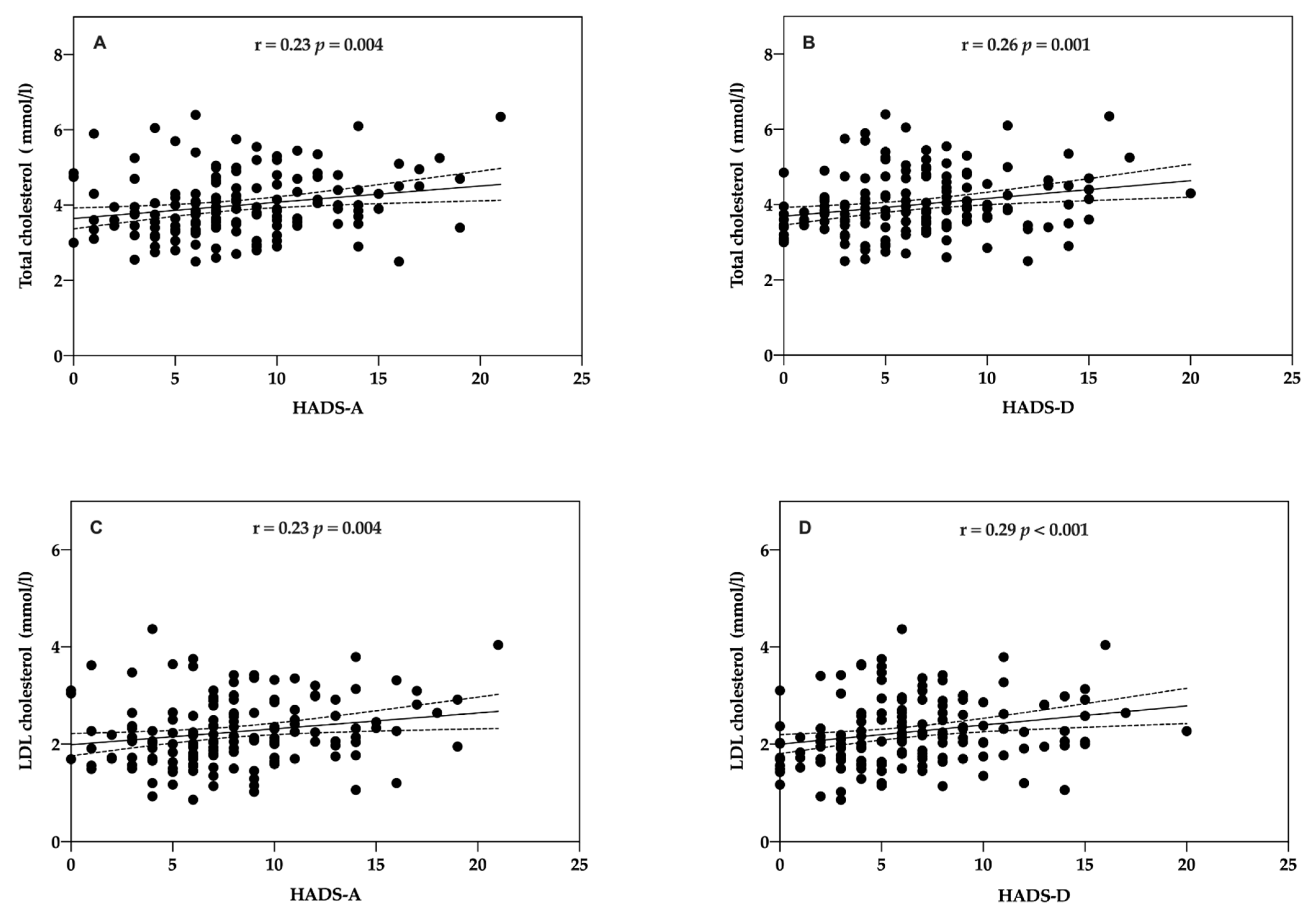
3.3. Association between Health Beliefs, Psycho-Social Factors, and Cardiovascular Risk Factors
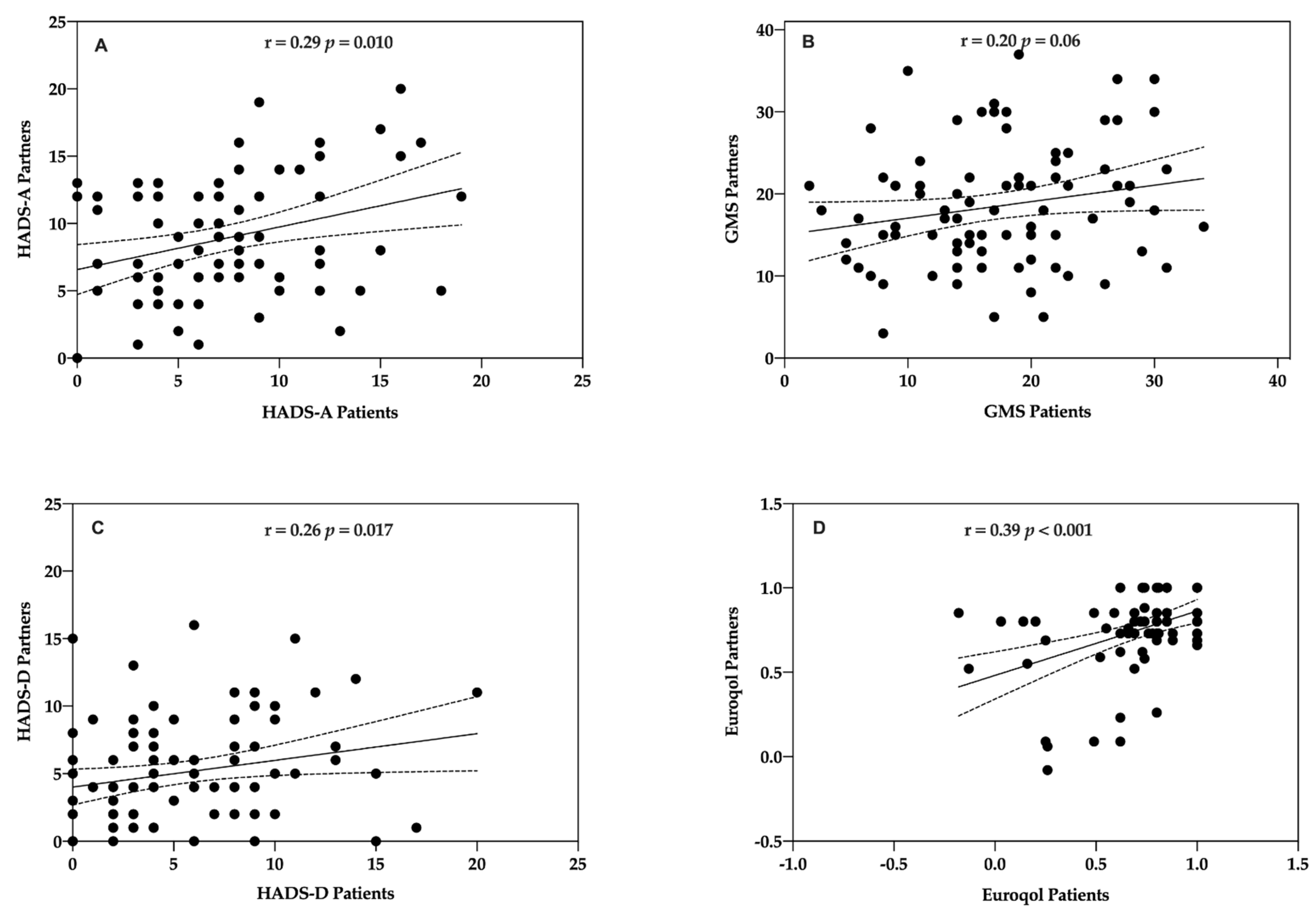
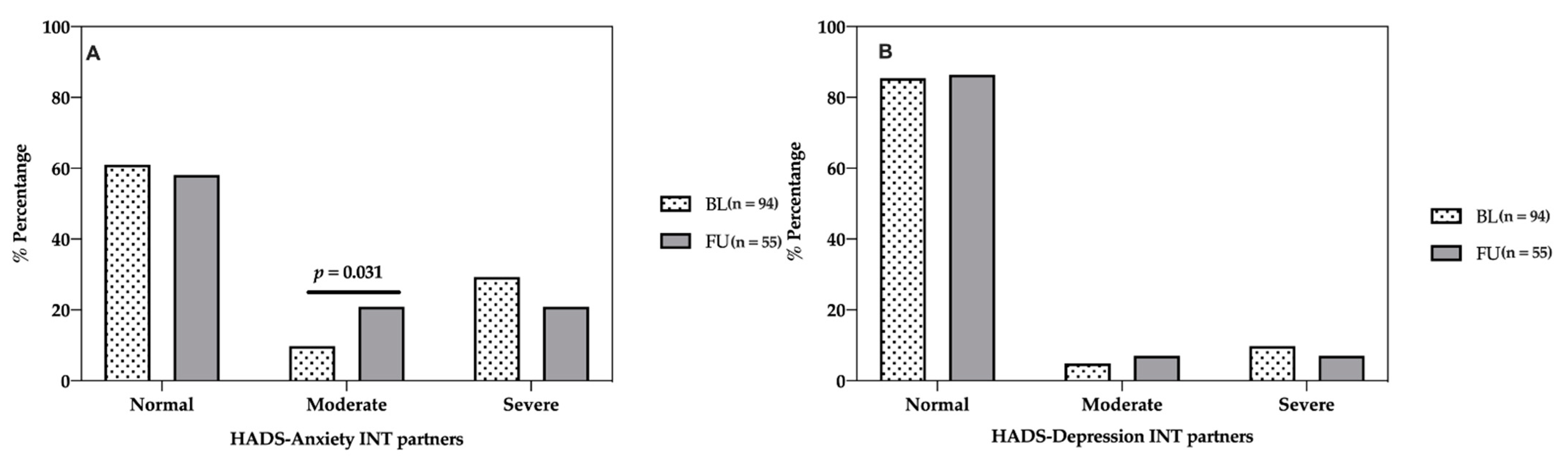
3.4. Association of Psycho-Social Factors between Partners and Patients with Coronary Disease
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Soriano, J.B.; Rojas-Rueda, D.; Alonso, J.; Antó, J.M.; Cardona, P.-J.; Fernández, E.; Garcia-Basteiro, A.L.; Benavides, F.G.; Glenn, S.D.; Krish, V.; et al. La Carga de Enfermedad En España: Resultados Del Estudio de La Carga Global de Las Enfermedades 2016. Med. Clin. 2018, 151, 171–190. [Google Scholar] [CrossRef]
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Davidson, K.W.; Alcántara, C.; Miller, G.E. Selected Psychological Comorbidities in Coronary Heart Disease: Challenges and Grand Opportunities. Am. Psychol. 2018, 73, 1019–1030. [Google Scholar] [CrossRef]
- Berg, S.K.; Rasmussen, T.B.; Thrysoee, L.; Thorup, C.B.; Borregaard, B.; Christensen, A.V.; Mols, R.E.; Juel, K.; Ekholm, O. Mental Health Is a Risk Factor for Poor Outcomes in Cardiac Patients: Findings from the National DenHeart Survey. J. Psychosom. Res. 2018, 112, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Moser, D.K.; McKinley, S.; Riegel, B.; Doering, L.V.; Meischke, H.; Pelter, M.; Davidson, P.; Baker, H.; Dracup, K. Relationship of Persistent Symptoms of Anxiety to Morbidity and Mortality Outcomes in Patients with Coronary Heart Disease. Psychosom. Med. 2011, 73, 803–809. [Google Scholar] [CrossRef] [PubMed]
- Richards, S.H.; Anderson, L.; Jenkinson, C.E.; Whalley, B.; Rees, K.; Davies, P.; Bennett, P.; Liu, Z.; West, R.; Thompson, D.R.; et al. Psychological Interventions for Coronary Heart Disease: Cochrane Systematic Review and Meta-Analysis. Eur. J. Prev. Cardiol. 2018, 25, 247–259. [Google Scholar] [CrossRef]
- Rutledge, T.; Redwine, L.S.; Linke, S.E.; Mills, P.J. A Meta-Analysis of Mental Health Treatments and Cardiac Rehabilitation for Improving Clinical Outcomes and Depression among Patients with Coronary Heart Disease. Psychosom. Med. 2013, 75, 335–349. [Google Scholar] [CrossRef]
- Lavie, C.J.; Milani, R.V. Prevalence of Anxiety in Coronary Patients with Improvement Following Cardiac Rehabilitation and Exercise Training. Am. J. Cardiol. 2004, 93, 336–339. [Google Scholar] [CrossRef]
- Lee, S.M.; Schneider, S.M.; Feiveson, A.H.; Macias, B.R.; Smith, S.M.; Watenpaugh, D.E.; Hargens, A.R. WISE-2005: Countermeasures to Prevent Muscle Deconditioning during Bed Rest in Women. J. Appl. Physiol. 2014, 116, 654–667. [Google Scholar] [CrossRef]
- Madueño, A.J.; Mellado, M.L.; Pardos, M.; Muñoz, M.; Martín, C.; Gomez-Salgado, S. Perceived self-efficacy in patients after cardiac rehabilitation program in Primary Care: A new model of care. Rev Esp Salud Publica 2019, 93, e1–e11. [Google Scholar]
- Jokar, F.; Yousefi, H.; Yousefy, A.; Sadeghi, M. Begin Again and Continue With Life: A Qualitative Study on the Experiences of Cardiac Rehabilitation Patients. J. Nurs. Res. 2017, 25, 344–352. [Google Scholar] [CrossRef] [PubMed]
- Herman, R.; Liebergall, M.; Rott, D. Correlation between Participation in a Cardiac Rehabilitation Program and Quality of Life of Patients with Coronary Artery Disease. Rehabil. Nurs. Off. J. Assoc. Rehabil. Nurses 2014, 39, 192–197. [Google Scholar] [CrossRef] [PubMed]
- Dickens, C.; McGowan, L.; Percival, C.; Tomenson, B.; Cotter, L.; Heagerty, A.; Creed, F. Negative Illness Perceptions Are Associated with New-Onset Depression Following Myocardial Infarction. Gen. Hosp. Psychiatry 2008, 30, 414–420. [Google Scholar] [CrossRef] [PubMed]
- Yohannes, A.M.; Willgoss, T.G.; Baldwin, R.C.; Connolly, M.J. Depression and Anxiety in Chronic Heart Failure and Chronic Obstructive Pulmonary Disease: Prevalence, Relevance, Clinical Implications and Management Principles. Int. J. Geriatr. Psychiatry 2010, 25, 1209–1221. [Google Scholar] [CrossRef] [PubMed]
- Thomson, P.; Angus, N.J.; Andreis, F.; Rushworth, G.F.; Mohan, A.R.; Chung, M.L.; Leslie, S.J. Longitudinal Evaluation of the Effects of Illness Perceptions and Beliefs about Cardiac Rehabilitation on Quality of Life of Patients with Coronary Artery Disease and Their Caregivers. Health Qual. Life Outcomes 2020, 18, 1–14. [Google Scholar] [CrossRef]
- Scotto, C.J.; Waechter, D.J.; Rosneck, J. Adherence to Prescribed Exercise and Diet Regimens Two Months Post-Cardiac Rehabilitation. Can. J. Cardiovasc. Nurs. 2011, 21, 11–17. [Google Scholar] [PubMed]
- National Clinical Guideline Centre UK. MI—Secondary Prevention. Secondary Prevention in Primary and Secondary Care for Patients Following a Myocardial Infarction; Royal College of Physicians: London, UK, 2013. [Google Scholar]
- Thomson, P.; Rushworth, G.F.; Andreis, F.; Angus, N.J.; Mohan, A.R.; Leslie, S.J. Longitudinal Study of the Relationship between Patients’ Medication Adherence and Quality of Life Outcomes and Illness Perceptions and Beliefs about Cardiac Rehabilitation. BMC Cardiovasc. Disord. 2020, 20, 71. [Google Scholar] [CrossRef]
- Gistelinck, F.; Loeys, T. The Actor–Partner Interdependence Model for Longitudinal Dyadic Data: An Implementation in the SEM Framework. Struct. Equ. Model. A Multidiscip. J. 2019, 26, 329–347. [Google Scholar] [CrossRef]
- Gallagher, J.; Parenti, G.; Doyle, F. Psychological Aspects of Cardiac Care and Rehabilitation: Time to Wake Up to Sleep? Curr. Cardiol. Rep. 2015, 17. [Google Scholar] [CrossRef]
- Petrie, K.J.; Weinman, J. Why Illness Perceptions Matter. Clin. Med. J. R. Coll. Physicians London 2006, 6, 536–539. [Google Scholar] [CrossRef]
- Hagger, M.S.; Orbell, S. A Meta-Analytic Review of the Common-Sense Model of Illness Representations. Psychol. Heal. 2003, 18, 141–184. [Google Scholar] [CrossRef]
- Lotfi-Tokaldany, M.; Shahmansouri, N.; Karimi, A.; Sadeghian, S.; Saadat, S.; Abbasi, S.H.; Jalali, A. Association between Illness Perception and Health-Related Quality of Life in Patients with Preexisting Premature Coronary Artery Disease. J. Psychosom. Res. 2019, 120, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Wood, D.A. EUROACTION: A European Society of Cardiology Demonstration Project in Preventive Cardiology.: A Cluster Randomised Controlled Trial of a Multi-Disciplinary Preventive Cardiology Programme for Coronary Patients, Asymptomatic High Risk Individuals and Their. Eur. Hear. J. Suppl. 2004, 6, j3–j15. [Google Scholar] [CrossRef]
- Wood, D.; De Backer, G.; Faergeman, O.; Graham, I.; Mancia, G.; Pyorala, K. Prevention of Coronary Heart Disease in Clinical Practice: Recommendations of the Second Joint Task Force of European and Other Societies on Coronary Prevention. Atherosclerosis 1998, 140, 199–270. [Google Scholar] [CrossRef]
- Brooks, R.; De Charro, F. EuroQol: The Current State of Play. Health Policy 1996, 37, 53–72. [Google Scholar] [CrossRef]
- Schweikert, B.; Hahmann, H.; Leidl, R. Validation of the EuroQol Questionnaire in Cardiac Rehabilitation. Heart 2006, 92, 62–67. [Google Scholar] [CrossRef]
- Herdman, M.; Badia, X.; Berra, S. El EuroQol-5D: Una Alternativa Sencilla Para La Medición de La Calidad de Vida Relacionada Con La Salud En Atención Primaria. Atención Primaria 2001, 28, 425–429. [Google Scholar] [CrossRef]
- Badia, X.; Roset, M.; Montserrat, S.; Herdman, M.; Segura, A. The Spanish version of EuroQol: A description and its applications. European Quality of Life scale. Med. Clin. 1999, 112, 79–85. [Google Scholar]
- Moss-Morris, R.; Weinman, J.; Petrie, K.; Horne, R.; Cameron, L.; Buick, D. The Revised Illness Perception Questionnaire (IPQ-R). Psychol. Health 2002, 17, 1–16. [Google Scholar] [CrossRef]
- Pacheco-Huergo, V.; Viladrich, C.; Pujol-Ribera, E.; Cabezas-Peña, C.; Núñez, M.; Roura-Olmeda, P.; Amado-Guirado, E.; Núñez, E.; Del Val, J.L. Percepción En Enfermedades Crónicas: Validación Lingüística Del Illness Perception Questionnaire Revised y Del Brief Illness Perception Questionnaire Para La Población Española. Aten. Primaria 2012, 44, 280–287. [Google Scholar] [CrossRef]
- Herrmann, C. International Experiences with the Hospital Anxiety and Depression Scale—A Review of Validation Data and Clinical Results. J. Psychosom. Res. 1997, 42, 17–41. [Google Scholar] [CrossRef]
- Herrero, M.J.; Blanch, J.; Peri, J.M.; De Pablo, J.; Pintor, L.; Bulbena, A. A Validation Study of the Hospital Anxiety and Depression Scale (HADS) in a Spanish Population. Gen. Hosp. Psychiatry 2003, 25, 277–283. [Google Scholar] [CrossRef]
- Denollet, J. Emotional Distress and Fatigue in Coronary Heart Disease: The Global Mood Scale (GMS). Psychol. Med. 1993, 23, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Denollet, J.; De Vries, J. Positive and Negative Affect within the Realm of Depression, Stress and Fatigue: The Two-Factor Distress Model of the Global Mood Scale (GMS). J. Affect. Disord. 2006, 91, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- EuroQol Group. EuroQol—A New Facility for the Measurement of Health-Related Quality of Life. Health Policy 1990, 16, 199–208. [Google Scholar] [CrossRef]
- Weinman, J.; Petrie, K.J.; Moss-Morris, R.; Horne, R. The Illness Perception Questionnaire: A New Method for Assessing the Cognitive Representation of Illness. Psychol. Heal. 1996, 11, 431–445. [Google Scholar] [CrossRef]
- Leventhal, H.; Diefenbach, M.; Leventhal, E.A. Illness Cognition: Using Common Sense to Understand Treatment Adherence and Affect Cognition Interactions. Cognit. Ther. Res. 1992, 16, 143–163. [Google Scholar] [CrossRef]
- Wood, D.A.; Kotseva, K.; Connolly, S.; Jennings, C.; Mead, A.; Jones, J.; Holden, A.; De Bacquer, D.; Collier, T.; De Backer, G.; et al. Nurse-Coordinated Multidisciplinary, Family-Based Cardiovascular Disease Prevention Programme (EUROACTION) for Patients with Coronary Heart Disease and Asymptomatic Individuals at High Risk of Cardiovascular Disease: A Paired, Cluster-Randomised Controlle. Lancet 2008, 371, 1999–2012. [Google Scholar] [CrossRef]
- Dolan, P.; Roberts, J. Brief Report An Alternative Model Using Differences in Valuations. Med. Care 2002, 40, 442–446. [Google Scholar] [CrossRef]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.-T.; Corra, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on Cardiovascular Disease Prevention in Clinical Practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (Constituted by Representati. Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [CrossRef] [PubMed]
- Celano, C.M.; Daunis, D.J.; Lokko, H.N.; Campbell, K.A.; Huffman, J.C. Anxiety Disorders and Cardiovascular Disease. Curr. Psychiatry Rep. 2016, 18, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Leventhal, H.; Phillips, L.A.; Burns, E. The Common-Sense Model of Self-Regulation (CSM): A Dynamic Framework for Understanding Illness Self-Management. J. Behav. Med. 2016, 39, 935–946. [Google Scholar] [CrossRef] [PubMed]
- Leventhal, H. Next Steps for Examining the Common-Sense of Health Behaviour. Health Psychol. Rev. 2019, 13, 487–489. [Google Scholar] [CrossRef] [PubMed]
- Orbell, S.; Alison Phillips, L. Automatic Processes and Self-Regulation of Illness. Health Psychol. Rev. 2019, 13, 378–405. [Google Scholar] [CrossRef] [PubMed]
- Shelley, E.T.; Helgeson, V.S.; Reed, G.M.; Skokan, L.A. Self-Generated Feelings of Control and Adjustment to Physical Illness. J. Soc. Issues 1991, 47, 91–109. [Google Scholar]
- Pai, H.C.; Li, C.C.; Tsai, S.M.; Pai, Y.C. Association between Illness Representation and Psychological Distress in Stroke Patients: A Systematic Review and Meta-Analysis. Int. J. Nurs. Stud. 2019, 94, 42–50. [Google Scholar] [CrossRef]
- Nur, K.R.M. Illness Perception and Cardiovascular Health Behaviour among Persons with Ischemic Heart Disease in Indonesia. Int. J. Nurs. Sci. 2018, 5, 174–180. [Google Scholar] [CrossRef]
- Bordoni, B.; Marelli, F.; Morabito, B.; Sacconi, B. Depression and Anxiety in Patients with Chronic Heart Failure. Future Cardiol. 2018, 14, 115–119. [Google Scholar] [CrossRef]
- Penninx, B.W.J.H. Depression and Cardiovascular Disease: Epidemiological Evidence on Their Linking Mechanisms. Neurosci. Biobehav. Rev. 2017, 74, 277–286. [Google Scholar] [CrossRef]
- Felger, J.C. Imaging the Role of Inflammation in Mood and Anxiety-Related Disorders. Curr. Neuropharmacol. 2017, 15, 533–558. [Google Scholar] [CrossRef] [PubMed]
- Chauvet-Gelinier, J.C.; Bonin, B. Stress, Anxiety and Depression in Heart Disease Patients: A Major Challenge for Cardiac Rehabilitation. Ann. Phys. Rehabil. Med. 2017, 60, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Paterniti, S.; Zureik, M.; Ducimetière, P.; Touboul, P.; Fève, J.; Alpérovitch, A. Sustained anxiety and 4-year progression of carotid atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2001, 360, 136–141. [Google Scholar]
- Tully, P.J.; Harrison, N.J.; Cheung, P.; Cosh, S. Anxiety and Cardiovascular Disease Risk: A Review. Curr. Cardiol. Rep. 2016, 18. [Google Scholar] [CrossRef]
- Kollia, N.; Panagiotakos, D.; Georgousopoulou, E.; Chrysohoou, C.; Yannakoulia, M.; Stefanadis, C.; Chatterji, S.; Haro, J.M.; Papageorgiou, C.; Pitsavos, C. Exploring the Path between Depression, Anxiety and 10-Year Cardiovascular Disease Incidence, among Apparently Healthy Greek Middle-Aged Adults: The ATTICA Study. Maturitas 2017, 106, 73–79. [Google Scholar] [CrossRef]
- Bonnet, F.; Irving, K.; Terra, J.L.; Nony, P.; Berthezène, F.; Moulin, P. Anxiety and Depression Are Associated with Unhealthy Lifestyle in Patients at Risk of Cardiovascular Disease. Atherosclerosis 2005, 178, 339–344. [Google Scholar] [CrossRef]
- Conversano, C.; Rotondo, A.; Lensi, E.; Della Vista, O.; Arpone, F.; Reda, M.A. Optimism and Its Impact on Mental and Physical Well-Being. Clin. Pract. Epidemiol. Ment. Health 2010, 6, 25–29. [Google Scholar] [CrossRef]
- Steptoe, A.; Wright, C.; Kunz-Ebrecht, S.R.; Iliffe, S. Dispositional Optimism and Health Behaviour in Community-Dwelling Older People: Associations with Healthy Ageing. Br. J. Health Psychol. 2006, 11, 71–84. [Google Scholar] [CrossRef]
- Van Halewijn, G.; Deckers, J.; Tay, H.Y.; van Domburg, R.; Kotseva, K.; Wood, D. Lessons from Contemporary Trials of Cardiovascular Prevention and Rehabilitation: A Systematic Review and Meta-Analysis. Int. J. Cardiol. 2017, 232, 294–303. [Google Scholar] [CrossRef]
- Yates, B.C.; Vazquez Hernandez, M.L.; Rowland, S.A.; Bainter, D.E.; Schulz, P.; Hanson, C.K. A Qualitative Study of Experiences of Participants in Cardiac Rehabilitation. J. Cardiopulm. Rehabil. Prev. 2018, 38, E6–E9. [Google Scholar] [CrossRef]
- Mosleh, S.M.; Almalik, M.M.A. Illness Perception and Adherence to Healthy Behaviour in Jordanian Coronary Heart Disease Patients. Eur. J. Cardiovasc. Nurs. 2014, 15, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Moore, S.M.; Prior, K.N.; Bond, M.J. The Contributions of Psychological Disposition and Risk Factor Status to Health Following Treatment for Coronary Artery Disease. Eur. J. Cardiovasc. Nurs. 2007, 6, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Minneboo, M.; Lachman, S.; Snaterse, M.; Jørstad, H.T.; ter Riet, G.; Boekholdt, S.M.; Scholte op Reimer, W.J.M.; Peters, R.J.G.; Riezebos, R.K.; van Liebergen, R.A.M.; et al. Community-Based Lifestyle Intervention in Patients With Coronary Artery Disease: The RESPONSE-2 Trial. J. Am. Coll. Cardiol. 2017, 70, 318–327. [Google Scholar] [CrossRef] [PubMed]

| Category | Variation | Intervention | Usual Care | p | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Civil status | Married | 136 | 82.4 | 38 | 77.6 | <0.001 |
| Widower | 15 | 9.1 | 8 | 16.3 | ||
| Divorced | 5 | 3.0 | 1 | 2 | ||
| Other | 9 | 5.5 | 2 | 4.1 | ||
| Cohabitation status | Single | 16 | 9.7 | 8 | 16.3 | 0.592 |
| With partner/family | 149 | 90.3 | 41 | 83.7 | ||
| Educational level | Without studies | 7 | 4.2 | 2 | 4.1 | 0.002 |
| Primary | 84 | 50.9 | 20 | 40.8 | ||
| Secondary | 29 | 17.6 | 22 | 44.9 | ||
| University | 14 | 8.5 | 1 | 2 | ||
| Professional situation before CV event | Full-time worker | 76 | 46.1 | 8 | 16.3 | <0.001 |
| Part-time worker | 2 | 1.2 | 1 | 2 | ||
| Self-employed | 10 | 6.1 | 2 | 4.1 | ||
| Unemployed | 6 | 3.6 | 1 | 2 | ||
| Retired | 58 | 35.2 | 25 | 51 | ||
| Other | 13 | 7.8 | 12 | 24.5 | ||
| CV diagnosis | AMI | 122 | 75.8 | 23 | 48.9 | <0.001 |
| Unstable angina | 31 | 19.3 | 23 | 48.9 | ||
| Stable angina | 8 | 5 | 1 | 2.1 | ||
| Psycho-Social Characteristics | Baseline | Follow-Up | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| INT (n = 125) | UC (n = 49) | p | INT (n = 118) | UC (n = 206) | p | |||||
| Median/ Mean Value | IQR/ ±SD | Median/ Mean Value | IQR/ ±SD | Median/ Mean Value | IQR/ ±SD | Median/ Mean Value | IQR/ ±SD | |||
| HADS-Anxiety | 7.0 | 6.0 | 8.0 | 5.0 | 0.024 | 6.0 | 5.0 | 9.0 | 4.0 | <0.001 |
| HADS-Depression | 5.0 | 6.0 | 8.0 | 5.0 | <0.001 | 5.0 | 6.25 | 7.0 | 4.0 | <0.001 |
| GMS | 17.21 | 7.77 | 19.0 | 9.50 | 0.836 | 18.17 | 6.72 | 21.5 | 7.5 | <0.001 |
| EQ-5D | 0.79 | 0.29 | 0.72 | 0.16 | 0.044 | 0.84 | 0.31 | 0.76 | 0.19 | 0.048 |
| EQ-VAS | 70.0 | 30.0 | 60.0 | 25.0 | 0.219 | 70.0 | 23.50 | 60.0 | 10.0 | 0.001 |
| IPQ-R | 17.38 | 3.46 | 17.75 | 2.57 | 0.430 | 18.35 | 3.77 | 18.0 | 5.00 | 0.726 |
| Baseline | Follow-Up | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| INT (n = 142) | UC (n = 49) | p | INT (n = 119) | UC (n = 206) | p | |||||
| Does the Patient Believe that the Following Behaviours are Harmful to His/Her Health | Median | IQR | Median | IQR | Median | IQR | Median | IQR | ||
| Smoking | 4.0 | 2.0 | 2.0 | 1.0 | <0.001 | 4.0 | 1.00 | 3.0 | 2.0 | <0.001 |
| Being overweight (10 kgs or more) | 3.0 | 1.0 | 2.0 | 1.0 | <0.001 | 3.0 | 1.00 | 3.0 | 1.0 | <0.001 |
| High-fat diet | 3.0 | 1.0 | 2.0 | 1.0 | <0.001 | 3.0 | 1.0 | 3.0 | 1.0 | <0.001 |
| Drinking heavily | 3.0 | 1.0 | 3.0 | 1.0 | 0.001 | 4.0 | 1.0 | 3.0 | 2.0 | <0.001 |
| Not exercising regularly (at least 3 to 4 times a week) | 2.0 | 2.0 | 2.0 | 1.75 | 0.220 | 3.0 | 1.0 | 3.0 | 1.0 | 0.289 |
| Feeling under regular stress (at least twice a week) | 3.0 | 2.0 | 2.0 | 2.0 | 0.010 | 3.0 | 1.0 | 3.0 | 1.0 | <0.001 |
| Not taking prescribed medication | 4.0 | 2.0 | 2.0 | 1.0 | <0.001 | 4.0 | 2.0 | 3.0 | 2.0 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buigues, C.; Queralt, A.; De Velasco, J.A.; Salvador-Sanz, A.; Jennings, C.; Wood, D.; Trapero, I. Psycho-Social Factors in Patients with Cardiovascular Disease Attending a Family-Centred Prevention and Rehabilitation Programme: EUROACTION Model in Spain. Life 2021, 11, 89. https://doi.org/10.3390/life11020089
Buigues C, Queralt A, De Velasco JA, Salvador-Sanz A, Jennings C, Wood D, Trapero I. Psycho-Social Factors in Patients with Cardiovascular Disease Attending a Family-Centred Prevention and Rehabilitation Programme: EUROACTION Model in Spain. Life. 2021; 11(2):89. https://doi.org/10.3390/life11020089
Chicago/Turabian StyleBuigues, Cristina, Ana Queralt, Jose Antonio De Velasco, Antonio Salvador-Sanz, Catriona Jennings, David Wood, and Isabel Trapero. 2021. "Psycho-Social Factors in Patients with Cardiovascular Disease Attending a Family-Centred Prevention and Rehabilitation Programme: EUROACTION Model in Spain" Life 11, no. 2: 89. https://doi.org/10.3390/life11020089
APA StyleBuigues, C., Queralt, A., De Velasco, J. A., Salvador-Sanz, A., Jennings, C., Wood, D., & Trapero, I. (2021). Psycho-Social Factors in Patients with Cardiovascular Disease Attending a Family-Centred Prevention and Rehabilitation Programme: EUROACTION Model in Spain. Life, 11(2), 89. https://doi.org/10.3390/life11020089






