Inactivation of Enveloped Bovine Viral Diarrhea Virus and Non-Enveloped Porcine Parvovirus Using Low-Pressure Non-Thermal Plasma
Abstract
:1. Introduction
2. Materials and Methods
2.1. Viruses and Cell Lines
2.2. Spiking Procedure
2.3. Plasma Process
2.4. Treatment Conditions
2.5. Recovery Procedure
2.6. Titration Assay
2.7. Statistical Analysis
3. Results
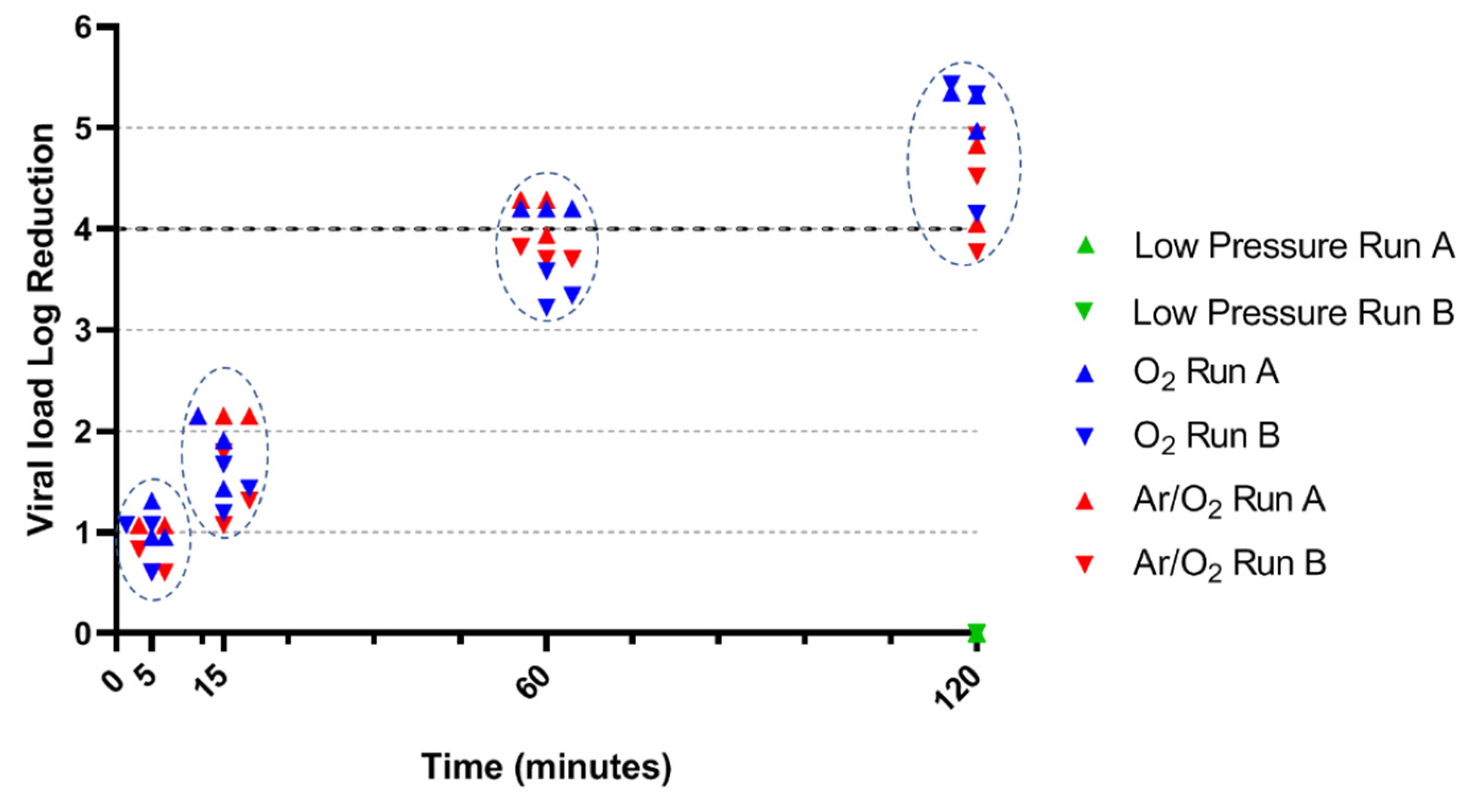
3.1. PPV Inactivation by O2 and Ar/O2 NTP
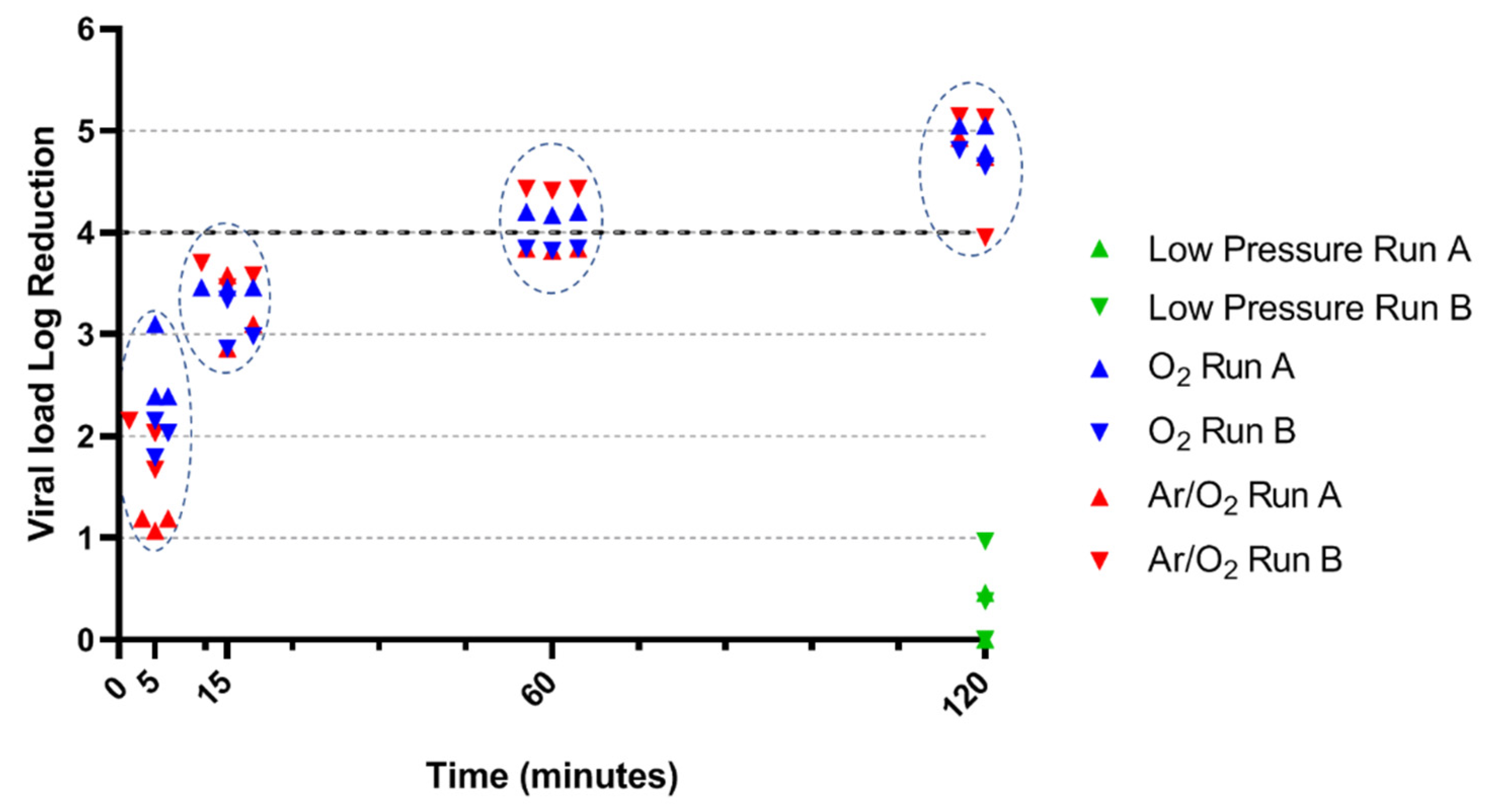
3.2. BVDV Inactivation by O2 and Ar/O2 NTP
4. Discussion
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Pittet, D.; Allegranzi, B.; Sax, H.; Dharan, S.; Pessoa-Silva, C.L.; Donaldson, L.; Boyce, J.M. Evidence-Based Model for Hand Transmission during Patient Care and the Role of Improved Practices. Lancet Infect. Dis. 2006, 6, 641–652. [Google Scholar] [CrossRef]
- Ansari, S.A.; Springthorpe, V.S.; Sattar, S.A. Survival and Vehicular Spread of Human Rotaviruses: Possible Relation to Seasonality of Outbreaks. Rev. Infect. Dis. 1991, 13, 448–461. [Google Scholar] [CrossRef] [PubMed]
- Gwaltney, J.M.; Moskalski, P.B.; Hendley, J.O. Hand-to-Hand Transmission of Rhinovirus Colds. Ann. Intern. Med. 1978, 88, 463–467. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Leong, F.Y.; Xu, G.; Kang, C.W.; Lim, K.H.; Tan, B.H.; Loo, C.M. Airborne Dispersion of Droplets during Coughing: A Physical Model of Viral Transmission. Sci. Rep. 2021, 11, 4617. [Google Scholar] [CrossRef] [PubMed]
- Cowling, B.J.; Ip, D.K.M.; Fang, V.J.; Suntarattiwong, P.; Olsen, S.J.; Levy, J.; Uyeki, T.M.; Leung, G.M.; Malik Peiris, J.S.; Chotpitayasunondh, T.; et al. Aerosol Transmission Is an Important Mode of Influenza A Virus Spread. Nat. Commun. 2013, 4, 1935. [Google Scholar] [CrossRef]
- Sattar, S.A.; Karim, Y.G.; Springthorpe, V.S.; Johnson-Lussenburg, C.M. Survival of Human Rhinovirus Type 14 Dried onto Nonporous Inanimate Surfaces: Effect of Relative Humidity and Suspending Medium. Can. J. Microbiol. 1987, 33, 802–806. [Google Scholar] [CrossRef]
- Xiao, S.; Tang, J.W.; Li, Y. Airborne or Fomite Transmission for Norovirus? A Case Study Revisited. Int. J. Environ. Res. Public Health 2017, 14, 1571. [Google Scholar] [CrossRef] [Green Version]
- Otter, J.A.; Donskey, C.; Yezli, S.; Douthwaite, S.; Goldenberg, S.D.; Weber, D.J. Transmission of SARS and MERS Coronaviruses and Influenza Virus in Healthcare Settings: The Possible Role of Dry Surface Contamination. J. Hosp. Infect. 2016, 92, 235–250. [Google Scholar] [CrossRef] [Green Version]
- Lopman, B.; Gastañaduy, P.; Park, G.W.; Hall, A.J.; Parashar, U.D.; Vinjé, J. Environmental Transmission of Norovirus Gastroenteritis. Curr. Opin. Virol. 2012, 2, 96–102. [Google Scholar] [CrossRef]
- Morter, S.; Bennet, G.; Fish, J.; Richards, J.; Allen, D.J.; Nawaz, S.; Iturriza-Gómara, M.; Brolly, S.; Gray, J. Norovirus in the Hospital Setting: Virus Introduction and Spread within the Hospital Environment. J. Hosp. Infect. 2011, 77, 106–112. [Google Scholar] [CrossRef]
- Weber, D.J.; Rutala, W.A.; Miller, M.B.; Huslage, K.; Sickbert-Bennett, E. Role of Hospital Surfaces in the Transmission of Emerging Health Care-Associated Pathogens: Norovirus, Clostridium Difficile, and Acinetobacter Species. Am. J. Infect. Control 2010, 38, S25–S33. [Google Scholar] [CrossRef]
- Prevost, B.; Goulet, M.; Lucas, F.S.; Joyeux, M.; Moulin, L.; Wurtzer, S. Viral Persistence in Surface and Drinking Water: Suitability of PCR Pre-Treatment with Intercalating Dyes. Water Res. 2016, 91, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Kramer, A.; Schwebke, I.; Kampf, G. How Long Do Nosocomial Pathogens Persist on Inanimate Surfaces? A Systematic Review. BMC Infect. Dis. 2006, 6, 130. [Google Scholar] [CrossRef] [Green Version]
- Wallace, C.A. New Developments in Disinfection and Sterilization. Am. J. Infect. Control 2016, 44, e23–e27. [Google Scholar] [CrossRef] [PubMed]
- US EPA, O. Health Effects Notebook for Hazardous Air Pollutants. Available online: https://www.epa.gov/haps/health-effects-notebook-hazardous-air-pollutants (accessed on 20 September 2021).
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans Chemical Agents and Related Occupations. IARC Monogr. Eval. Carcinog. Risks Hum. 2012, 100, 379–400.
- Haim Zada, M.; Kumar, A.; Elmalak, O.; Mechrez, G.; Domb, A.J. Effect of Ethylene Oxide and Gamma (γ-) Sterilization on the Properties of a PLCL Polymer Material in Balloon Implants. ACS Omega 2019, 4, 21319–21326. [Google Scholar] [CrossRef] [Green Version]
- Navarro, R.; Burillo, G.; Adem, E.; Marcos-Fernández, A. Effect of Ionizing Radiation on the Chemical Structure and the Physical Properties of Polycaprolactones of Different Molecular Weight. Polymers 2018, 10, 397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Filipić, A.; Gutierrez-Aguirre, I.; Primc, G.; Mozetič, M.; Dobnik, D. Cold Plasma, a New Hope in the Field of Virus Inactivation. Trends Biotechnol. 2020, 38, 1278–1291. [Google Scholar] [CrossRef]
- Fiebrandt, M.; Lackmann, J.-W.; Stapelmann, K. From Patent to Product? 50 Years of Low-Pressure Plasma Sterilization. Plasma Process. Polym. 2018, 15, 1800139. [Google Scholar] [CrossRef] [Green Version]
- Sakudo, A.; Yagyu, Y.; Onodera, T. Disinfection and Sterilization Using Plasma Technology: Fundamentals and Future Perspectives for Biological Applications. Int. J. Mol. Sci. 2019, 20, 5216. [Google Scholar] [CrossRef] [Green Version]
- Bourke, P.; Ziuzina, D.; Han, L.; Cullen, P.J.; Gilmore, B.F. Microbiological Interactions with Cold Plasma. J. Appl. Microbiol. 2017, 123, 308–324. [Google Scholar] [CrossRef] [Green Version]
- Soušková, H.; Scholtz, V.; Julák, J.; Kommová, L.; Savická, D.; Pazlarová, J. The Survival of Micromycetes and Yeasts under the Low-Temperature Plasma Generated in Electrical Discharge. Folia Microbiol. 2011, 56, 77–79. [Google Scholar] [CrossRef]
- Ben Belgacem, Z.; Carré, G.; Boudifa, M.; Charpentier, E.; Cawe, B.; Gellé, M.P. Effectiveness of Non-Thermal O2–N2 Plasma on P. Aeruginosa Multilayer Biofilms Cultured on Hydroxyapatite. IRBM 2016, 37, 68–74. [Google Scholar] [CrossRef]
- Ben Belgacem, Z.; Carré, G.; Charpentier, E.; Le-Bras, F.; Maho, T.; Robert, E.; Pouvesle, J.-M.; Polidor, F.; Gangloff, S.C.; Boudifa, M.; et al. Innovative Non-Thermal Plasma Disinfection Process inside Sealed Bags: Assessment of Bactericidal and Sporicidal Effectiveness in Regard to Current Sterilization Norms. PLoS ONE 2017, 12, e0180183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carré, G.; Charpentier, E.; Audonnet, S.; Terryn, C.; Boudifa, M.; Doliwa, C.; Belgacem, Z.B.; Gangloff, S.C.; Gelle, M.-P. Contribution of Fluorescence Techniques in Determining the Efficiency of the Non-Thermal Plasma Treatment. Front. Microbiol. 2018, 9, 2171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Halfmann, H.; Denis, B.; Bibinov, N.; Wunderlich, J.; Awakowicz, P. Identification of the Most Efficient VUV/UV Radiation for Plasma Based Inactivation of Bacillus Atrophaeus Spores. J. Phys. Appl. Phys. 2007, 40, 5907. [Google Scholar] [CrossRef]
- Raballand, V.; Benedikt, J.; Wunderlich, J.; Keudell, A. von Inactivation OfBacillus Atrophaeusand OfAspergillus Nigerusing Beams of Argon Ions, of Oxygen Molecules and of Oxygen Atoms. J. Phys. Appl. Phys. 2008, 41, 115207. [Google Scholar] [CrossRef]
- Bräuniger, S.; Peters, J.; Borchers, U.; Kao, M. Further Studies on Thermal Resistance of Bovine Parvovirus against Moist and Dry Heat. Int. J. Hyg. Environ. Health 2000, 203, 71–75. [Google Scholar] [CrossRef]
- Mészáros, I.; Olasz, F.; Cságola, A.; Tijssen, P.; Zádori, Z. Biology of Porcine Parvovirus (Ungulate Parvovirus 1). Viruses 2017, 9, 393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Callens, N.; Brügger, B.; Bonnafous, P.; Drobecq, H.; Gerl, M.J.; Krey, T.; Roman-Sosa, G.; Rümenapf, T.; Lambert, O.; Dubuisson, J.; et al. Morphology and Molecular Composition of Purified Bovine Viral Diarrhea Virus Envelope. PLoS Pathog. 2016, 12, e1005476. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klämpfl, T.G.; Isbary, G.; Shimizu, T.; Li, Y.-F.; Zimmermann, J.L.; Stolz, W.; Schlegel, J.; Morfill, G.E.; Schmidt, H.-U. Cold Atmospheric Air Plasma Sterilization against Spores and Other Microorganisms of Clinical Interest. Appl. Environ. Microbiol. 2012, 78, 5077–5082. [Google Scholar] [CrossRef] [Green Version]
- Shintani, H. Inactivation of Bacterial Spore, Endotoxin, Lipid A, Normal Prion and Abnormal Prion by Exposures to Several Sorts of Gases Plasma. Biocontrol Sci. 2016, 21, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Aboubakr, H.A.; Mor, S.K.; Higgins, L.; Armien, A.; Youssef, M.M.; Bruggeman, P.J.; Goyal, S.M. Cold Argon-Oxygen Plasma Species Oxidize and Disintegrate Capsid Protein of Feline Calicivirus. PLoS ONE 2018, 13, e0194618. [Google Scholar] [CrossRef]
- Yamashiro, R.; Misawa, T.; Sakudo, A. Key Role of Singlet Oxygen and Peroxynitrite in Viral RNA Damage during Virucidal Effect of Plasma Torch on Feline Calicivirus. Sci. Rep. 2018, 8, 17947. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Xu, R.; Gou, L.; Liu, Z.; Zhao, Y.; Liu, D.; Zhang, L.; Chen, H.; Kong, M.G. Mechanism of Virus Inactivation by Cold Atmospheric-Pressure Plasma and Plasma-Activated Water. Appl. Environ. Microbiol. 2018, 84, e00726-18. [Google Scholar] [CrossRef] [Green Version]
- Lackmann, J.-W.; Schneider, S.; Edengeiser, E.; Jarzina, F.; Brinckmann, S.; Steinborn, E.; Havenith, M.; Benedikt, J.; Bandow, J.E. Photons and Particles Emitted from Cold Atmospheric-Pressure Plasma Inactivate Bacteria and Biomolecules Independently and Synergistically. J. R. Soc. Interface 2013, 10, 20130591. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Case | Subcase | Titer (T) |
|---|---|---|
| Infectious particles detected ≥12.5% positive wells/total tested wells | N/A | T = TSK |
| Few infectious particles detected <12.5% positive wells/total tested wells | TMaxL > LOD | T = TMaxL |
| LOD > TMaxL | T = LOD | |
| No infectious particles detected 0% positive well/total tested wells | N/A | T < LOD |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Le Bras, F.; Carré, G.; Aguemon, Y.; Colin, M.; Gellé, M.-P. Inactivation of Enveloped Bovine Viral Diarrhea Virus and Non-Enveloped Porcine Parvovirus Using Low-Pressure Non-Thermal Plasma. Life 2021, 11, 1292. https://doi.org/10.3390/life11121292
Le Bras F, Carré G, Aguemon Y, Colin M, Gellé M-P. Inactivation of Enveloped Bovine Viral Diarrhea Virus and Non-Enveloped Porcine Parvovirus Using Low-Pressure Non-Thermal Plasma. Life. 2021; 11(12):1292. https://doi.org/10.3390/life11121292
Chicago/Turabian StyleLe Bras, Florian, Gaëlle Carré, Yasmina Aguemon, Marius Colin, and Marie-Paule Gellé. 2021. "Inactivation of Enveloped Bovine Viral Diarrhea Virus and Non-Enveloped Porcine Parvovirus Using Low-Pressure Non-Thermal Plasma" Life 11, no. 12: 1292. https://doi.org/10.3390/life11121292
APA StyleLe Bras, F., Carré, G., Aguemon, Y., Colin, M., & Gellé, M.-P. (2021). Inactivation of Enveloped Bovine Viral Diarrhea Virus and Non-Enveloped Porcine Parvovirus Using Low-Pressure Non-Thermal Plasma. Life, 11(12), 1292. https://doi.org/10.3390/life11121292






