Telemedicine and Remote Monitoring as an Adjunct to Medical Management of Bronchiectasis
Abstract
:1. Introduction
2. Home Monitoring of Treatment
3. Home Monitoring for Early Detection of Exacerbation
4. Lung Function Monitoring with Home Spirometry and Peak Expiratory Flow Rate (PEFR)
5. Home Monitoring of Physical Activity
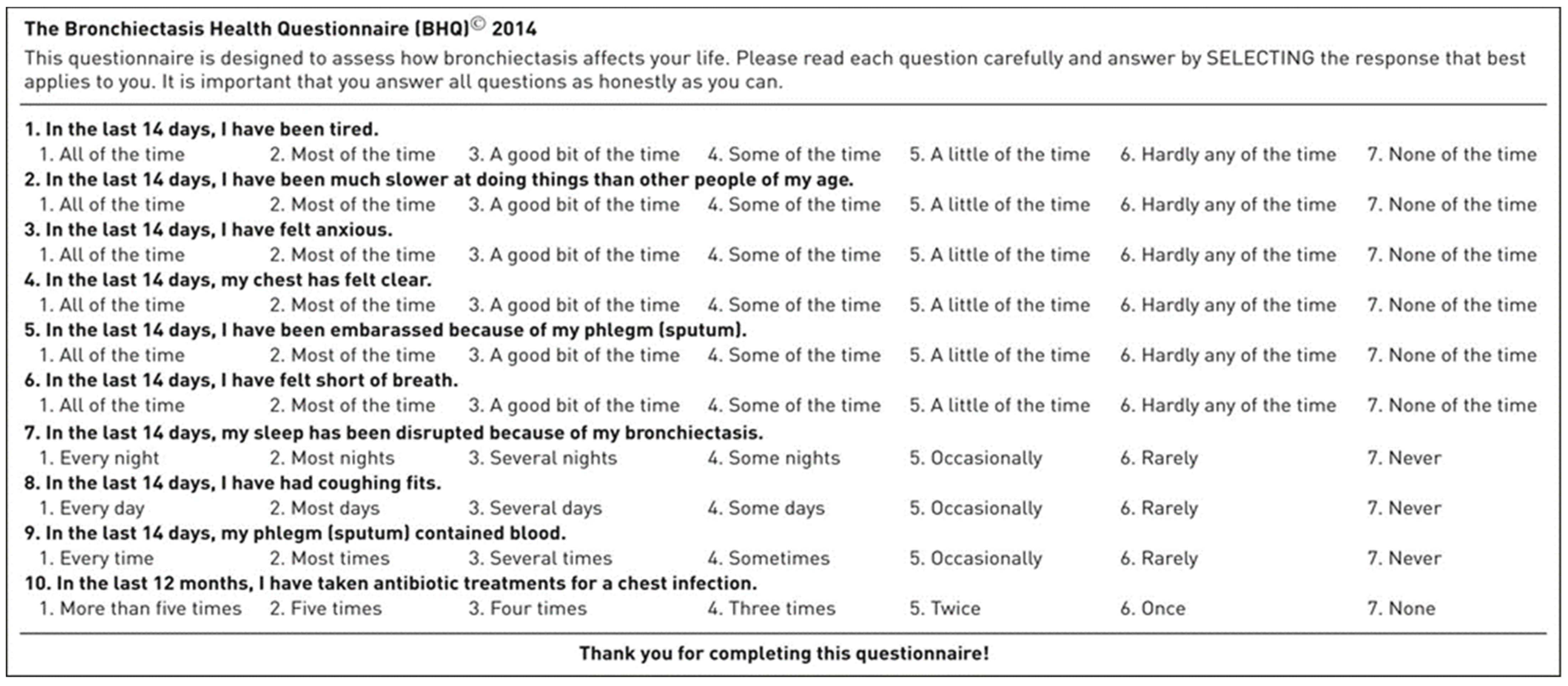
6. Home Monitoring for Quality of Life (QoL)
7. Tele-Rehabilitation
8. Experience in Telemedicine in Patients with Bronchiectasis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cole, P.J. Inflammation: A two-edged sword--the model of bronchiectasis. Eur. J. Respir. Dis. Suppl. 1986, 147, 6–15. [Google Scholar]
- King, P.T. The pathophysiology of bronchiectasis. Int. J. Chron. Obstruct. Pulmon. Dis. 2009, 4, 411–419. [Google Scholar] [CrossRef] [PubMed]
- Amati, F.; Simonetta, E.; Gramegna, A.; Tarsia, P.; Contarini, M.; Blasi, F.; Aliberti, S. The biology of pulmonary exacerbations in bronchiectasis. Eur. Respir. Rev. 2019, 28, 190055. [Google Scholar] [CrossRef] [Green Version]
- Chalmers, J.D.; Goeminne, P.; Aliberti, S.; McDonnell, M.J.; Lonni, S.; Davidson, J.; Poppelwell, L.; Salih, W.; Pesci, A.; Dupont, L.J.; et al. The bronchiectasis severity index. An international derivation and validation study. Am. J. Respir. Crit. Care Med. 2014, 189, 576–585. [Google Scholar] [CrossRef]
- Chalmers, J.D.; Smith, M.P.; McHugh, B.J.; Doherty, C.; Govan, J.R.; Hill, A.T. Short- and long-term antibiotic treatment reduces airway and systemic inflammation in non-cystic fibrosis bronchiectasis. Am. J. Respir. Crit. Care Med. 2012, 186, 657–665. [Google Scholar] [CrossRef] [PubMed]
- Sheehan, R.E.; Wells, A.U.; Copley, S.J.; Desai, S.R.; Howling, S.J.; Cole, P.J.; Wilson, R.; Hansell, D.M. A comparison of serial computed tomography and functional change in bronchiectasis. Eur. Respir. J. 2002, 20, 581–587. [Google Scholar] [CrossRef] [Green Version]
- Aliberti, S.; Lonni, S.; Dore, S.; McDonnell, M.J.; Goeminne, P.C.; Dimakou, K.; Fardon, T.C.; Rutherford, R.; Pesci, A.; Restrepo, M.I.; et al. Clinical phenotypes in adult patients with bronchiectasis. Eur. Respir. J. 2016, 47, 1113–1122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kapur, N.; Masters, I.B.; Chang, A.B. Longitudinal growth and lung function in pediatric non-cystic fibrosis bronchiectasis: What influences lung function stability? Chest 2010, 138, 158–164. [Google Scholar] [CrossRef] [PubMed]
- Ringshausen, F.C.; de Roux, A.; Pletz, M.W.; Hamalainen, N.; Welte, T.; Rademacher, J. Bronchiectasis-associated hospitalizations in Germany, 2005-2011: A population-based study of disease burden and trends. PLoS ONE 2013, 8, e71109. [Google Scholar] [CrossRef] [Green Version]
- Weycker, D.E.J.; Oster, G.; Tino, G. Prevalence and economic burden of bronchiectasis. Clin. Pulm. Med. 2005, 12, 205–209. [Google Scholar] [CrossRef]
- Polverino, E.; Goeminne, P.C.; McDonnell, M.J.; Aliberti, S.; Marshall, S.E.; Loebinger, M.R.; Murris, M.; Cantón, R.; Torres, A.; Dimakou, K.; et al. European Respiratory Society guidelines for the management of adult bronchiectasis. Eur. Respir. J. 2017, 50, 1700629. [Google Scholar] [CrossRef]
- Germino, R.; Liao, L. Resource utilization associated with non-cystic fibrosis bronchiectasis patients who are being treated for exacerbations. Value Health 2016, 19, A1116. [Google Scholar] [CrossRef] [Green Version]
- Joish, V.N.; Spilsbury-Cantalupo, M.; Kamalakar, R.; Operschall, E.; Luong, B. Direct medical costs associated with exacerbations related to non-cystic fibrosis bronchiectasis. Value Health 2013, 16, A188. [Google Scholar] [CrossRef] [Green Version]
- De la Rosa, D.; Martinez-Garcia, M.A.; Olveira, C.; Giron, R.; Maiz, L.; Prados, C. Annual direct medical costs of bronchiectasis treatment: Impact of severity, exacerbations, chronic bronchial colonization and chronic obstructive pulmonary disease coexistence. Chron. Respir. Dis. 2016, 13, 361–371. [Google Scholar] [CrossRef]
- De San Miguel, K.; Smith, J.; Lewin, G. Telehealth remote monitoring for community-dwelling older adults with chronic obstructive pulmonary disease. Telemed. J. E Health 2013, 19, 652–657. [Google Scholar] [CrossRef] [PubMed]
- Haesum, L.K.; Soerensen, N.; Dinesen, B.; Nielsen, C.; Grann, O.; Hejlesen, O.; Toft, E.; Ehlers, L. Cost-utility analysis of a telerehabilitation program: A case study of COPD patients. Telemed. J. E Health 2012, 18, 688–692. [Google Scholar] [CrossRef]
- Vitacca, M.; Bianchi, L.; Guerra, A.; Fracchia, C.; Spanevello, A.; Balbi, B.; Scalvini, S. Tele-assistance in chronic respiratory failure patients: A randomised clinical trial. Eur. Respir. J. 2009, 33, 411–418. [Google Scholar] [CrossRef] [Green Version]
- Pare, G.; Sicotte, C.; St-Jules, D.; Gauthier, R. Cost-minimization analysis of a telehomecare program for patients with chronic obstructive pulmonary disease. Telemed. J. E Health 2006, 12, 114–121. [Google Scholar] [CrossRef] [PubMed]
- Tagliente, I.; Trieste, L.; Solvoll, T.; Murgia, F.; Bella, S. Telemonitoring in cystic fibrosis: A 4-year assessment and simulation for the next 6 years. Interact. J. Med. Res. 2016, 5, e11. [Google Scholar] [CrossRef]
- Agha, Z.; Schapira, R.M.; Maker, A.H. Cost effectiveness of telemedicine for the delivery of outpatient pulmonary care to a rural population. Telemed. J. E Health 2002, 8, 281–291. [Google Scholar] [CrossRef] [Green Version]
- Shah, N.M.; Kaltsakas, G. Telemedicine in the management of patients with chronic respiratory failure. Breathe 2021, 17, 210008. [Google Scholar] [CrossRef]
- Calthorpe, R.J.; Smith, S.; Gathercole, K.; Smyth, A.R. Using digital technology for home monitoring, adherence and self-management in cystic fibrosis: A state-of-the-art review. Thorax 2020, 75, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Himes, B.E.; Weitzman, E.R. Innovations in health information technologies for chronic pulmonary diseases. Respir. Res. 2016, 17, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blakey, J.D.; Bender, B.G.; Dima, A.L.; Weinman, J.; Safioti, G.; Costello, R.W. Digital technologies and adherence in respiratory diseases: The road ahead. Eur. Respir. J. 2018, 52, 1801147. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Kim, E.G.; Cao, G.; Liu, S.; Xu, Y. Physiological acoustic sensing based on accelerometers: A survey for mobile healthcare. Ann. Biomed. Eng. 2014, 42, 2264–2277. [Google Scholar] [CrossRef]
- Nesmith, A.H.T.; Edwards, L.; Solomon, G.M. Comparison between lung function parameters measured using home spirometry and routine office spirometry in stable cystic fibrosis patients. Am. J. Respir. Crit. Care Med. 2021, 203, A2021. [Google Scholar]
- Martinez-Garcia, M.A.; de Gracia, J.; Vendrell Relat, M.; Giron, R.M.; Maiz Carro, L.; de la Rosa Carrillo, D.; Olveira, C. Multidimensional approach to non-cystic fibrosis bronchiectasis: The FACED score. Eur. Respir. J. 2014, 43, 1357–1367. [Google Scholar] [CrossRef] [PubMed]
- A Prospective Randomised Pilot Study of Videoconferencing in Adults with Cystic Fibrosis Receiving Intravenous Antibiotics for Acute Pulmonary Exacerbations (VIRTUALCF). Available online: https://www.clinicaltrials.gov/ct2/show/NCT03069651 (accessed on 10 June 2021).
- Charles, T.; Quinn, D.; Weatherall, M.; Aldington, S.; Beasley, R.; Holt, S. An audiovisual reminder function improves adherence with inhaled corticosteroid therapy in asthma. J. Allergy Clin. Immunol. 2007, 119, 811–816. [Google Scholar] [CrossRef]
- Haworth, C.S.; Foweraker, J.E.; Wilkinson, P.; Kenyon, R.F.; Bilton, D. Inhaled colistin in patients with bronchiectasis and chronic Pseudomonas aeruginosa infection. Am. J. Respir. Crit. Care Med. 2014, 189, 975–982. [Google Scholar] [CrossRef] [Green Version]
- McNamara, P.S.; McCormack, P.; McDonald, A.J.; Heaf, L.; Southern, K.W. Open adherence monitoring using routine data download from an adaptive aerosol delivery nebuliser in children with cystic fibrosis. J. Cyst. Fibros. 2009, 8, 258–263. [Google Scholar] [CrossRef] [Green Version]
- Thornton, C.L.O.; Chan, E. The use of telehealth system in improving adherence to nebulised treatment in children with cystic fibrosis: Benefits and pitfalls. Eur. Respir. J. 2014, 44, P1965. [Google Scholar]
- Elborn, J.S.; Bell, S.C. Pulmonary exacerbations in cystic fibrosis and bronchiectasis. Thorax 2007, 62, 288–290. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seitz, A.E.; Olivier, K.N.; Steiner, C.A.; Montes de Oca, R.; Holland, S.M.; Prevots, D.R. Trends and burden of bronchiectasis-associated hospitalizations in the United States, 1993–2006. Chest 2010, 138, 944–949. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Finklea, J.D.; Khan, G.; Thomas, S.; Song, J.; Myers, D.; Arroliga, A.C. Predictors of mortality in hospitalized patients with acute exacerbation of bronchiectasis. Respir. Med. 2010, 104, 816–821. [Google Scholar] [CrossRef] [Green Version]
- Roberts, M.E.; Lowndes, L.; Milne, D.G.; Wong, C.A. Socioeconomic deprivation, readmissions, mortality and acute exacerbations of bronchiectasis. Intern. Med. J. 2012, 42, e129–e136. [Google Scholar] [CrossRef] [PubMed]
- Dupont, M.; Gacouin, A.; Lena, H.; Lavoue, S.; Brinchault, G.; Delaval, P.; Thomas, R. Survival of patients with bronchiectasis after the first ICU stay for respiratory failure. Chest 2004, 125, 1815–1820. [Google Scholar] [CrossRef] [Green Version]
- Alzeer, A.H.; Masood, M.; Basha, S.J.; Shaik, S.A. Survival of bronchiectatic patients with respiratory failure in ICU. BMC Pulm. Med. 2007, 7, 17. [Google Scholar] [CrossRef] [Green Version]
- Wood, J.; Jenkins, S.; Putrino, D.; Mulrennan, S.; Morey, S.; Cecins, N.; Bear, N.; Hill, K. A smartphone application for reporting symptoms in adults with cystic fibrosis improves the detection of exacerbations: Results of a randomised controlled trial. J. Cyst. Fibros. 2020, 19, 271–276. [Google Scholar] [CrossRef]
- Guan, W.J.; Gao, Y.H.; Xu, G.; Lin, Z.Y.; Tang, Y.; Li, H.M.; Lin, Z.M.; Zheng, J.P.; Chen, R.C.; Zhong, N.S. Characterization of lung function impairment in adults with bronchiectasis. PLoS ONE 2014, 9, e113373. [Google Scholar] [CrossRef]
- Breuer, O.; Caudri, D.; Stick, S.; Turkovic, L. Predicting disease progression in cystic fibrosis. Expert Rev. Respir. Med. 2018, 12, 905–917. [Google Scholar] [CrossRef]
- Ellis, D.A.; Thornley, P.E.; Wightman, A.J.; Walker, M.; Chalmers, J.; Crofton, J.W. Present outlook in bronchiectasis: Clinical and social study and review of factors influencing prognosis. Thorax 1981, 36, 659–664. [Google Scholar] [CrossRef] [Green Version]
- Brill, S.E.; Patel, A.R.; Singh, R.; Mackay, A.J.; Brown, J.S.; Hurst, J.R. Lung function, symptoms and inflammation during exacerbations of non-cystic fibrosis bronchiectasis: A prospective observational cohort study. Respir. Res. 2015, 16, 16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barry, J.S.J.; Akuhota, P.; Conrad, D.J. Reliability of home spirometry compared to traditional clinic spirometry in an adult cystic fibrosis population. Am. J. Respir. Crit. Care Med. 2021, 203, A2021. [Google Scholar]
- Larson, E.C.G.M.; Boriello, G.; Heltshe, S.; Rosenfeld, M.; Patel, S.N. SpiroSmart: Using a microphone to measure lung function on a mobile phone. In Proceedings of the 2012 ACM Conference on Ubiquitous Computing, Pittsburgh, PA, USA, 5–8 September 2012; pp. 280–289. [Google Scholar]
- A Randomized Control Trial of ZEPHYRx Gamified Incentive Spirometry Compared to Traditional Spirometry. Available online: https://clinicaltrials.gov/ct2/show/study/NCT04429009 (accessed on 10 May 2021).
- Murgia, F.; Bianciardi, F.; Solvoll, T.; Tagliente, I.; Bella, F.; Carestia, A.; Bella, S. Telemedicine home program in patients with cystic fibrosis: Results after 10 years. Clin. Ter. 2015, 166, e384–e388. [Google Scholar]
- Lechtzin, N.; Mayer-Hamblett, N.; West, N.E.; Allgood, S.; Wilhelm, E.; Khan, U.; Aitken, M.L.; Ramsey, B.W.; Boyle, M.P.; Mogayzel, P.J., Jr.; et al. Home monitoring of patients with cystic fibrosis to identify and treat acute pulmonary exacerbations. eICE study results. Am. J. Respir. Crit. Care Med. 2017, 196, 1144–1151. [Google Scholar] [CrossRef]
- Burtin, C.; Hebestreit, H. Rehabilitation in patients with chronic respiratory disease other than chronic obstructive pulmonary disease: Exercise and physical activity interventions in cystic fibrosis and non-cystic fibrosis bronchiectasis. Respiration 2015, 89, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Olveira, G.; Olveira, C.; Gaspar, I.; Porras, N.; Martin-Nunez, G.; Rubio, E.; Colomo, N.; Rojo-Martinez, G.; Soriguer, F. Fat-free mass depletion and inflammation in patients with bronchiectasis. J. Acad. Nutr. Diet. 2012, 112, 1999–2006. [Google Scholar] [CrossRef] [PubMed]
- O′Neill, B.; McDonough, S.M.; Wilson, J.J.; Bradbury, I.; Hayes, K.; Kirk, A.; Kent, L.; Cosgrove, D.; Bradley, J.M.; Tully, M.A. Comparing accelerometer, pedometer and a questionnaire for measuring physical activity in bronchiectasis: A validity and feasibility study? Respir. Res. 2017, 18, 16. [Google Scholar] [CrossRef] [Green Version]
- Mendoza, L.; Horta, P.; Espinoza, J.; Aguilera, M.; Balmaceda, N.; Castro, A.; Ruiz, M.; Diaz, O.; Hopkinson, N.S. Pedometers to enhance physical activity in COPD: A randomised controlled trial. Eur. Respir. J. 2015, 45, 347–354. [Google Scholar] [CrossRef] [Green Version]
- Demeyer, H.; Louvaris, Z.; Frei, A.; Rabinovich, R.A.; de Jong, C.; Gimeno-Santos, E.; Loeckx, M.; Buttery, S.C.; Rubio, N.; Van der Molen, T.; et al. Physical activity is increased by a 12-week semiautomated telecoaching programme in patients with COPD: A multicentre randomised controlled trial. Thorax 2017, 72, 415–423. [Google Scholar] [CrossRef] [Green Version]
- Moy, M.L.; Collins, R.J.; Martinez, C.H.; Kadri, R.; Roman, P.; Holleman, R.G.; Kim, H.M.; Nguyen, H.Q.; Cohen, M.D.; Goodrich, D.E.; et al. An Internet-mediated pedometer-based program improves health-related quality-of-life domains and daily step counts in COPD: A randomized controlled trial. Chest 2015, 148, 128–137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Angelucci, A.; Aliverti, A. Telemonitoring systems for respiratory patients: Technological aspects. Pulmonology 2020, 26, 221–232. [Google Scholar] [CrossRef] [PubMed]
- Swigris, J.J.; Kuschner, W.G.; Jacobs, S.S.; Wilson, S.R.; Gould, M.K. Health-related quality of life in patients with idiopathic pulmonary fibrosis: A systematic review. Thorax 2005, 60, 588–594. [Google Scholar] [CrossRef] [Green Version]
- Spinou, A.; Fragkos, K.C.; Lee, K.K.; Elston, C.; Siegert, R.J.; Loebinger, M.R.; Wilson, R.; Garrod, R.; Birring, S.S. The validity of health-related quality of life questionnaires in bronchiectasis: A systematic review and meta-analysis. Thorax 2016, 71, 683–694. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Quittner, A.L.; O′Donnell, A.E.; Salathe, M.A.; Lewis, S.A.; Li, X.; Montgomery, A.B.; O′Riordan, T.G.; Barker, A.F. Quality of life questionnaire-bronchiectasis: Final psychometric analyses and determination of minimal important difference scores. Thorax 2015, 70, 12–20. [Google Scholar] [CrossRef] [Green Version]
- Spinou, A.; Siegert, R.J.; Guan, W.J.; Patel, A.S.; Gosker, H.R.; Lee, K.K.; Elston, C.; Loebinger, M.R.; Wilson, R.; Garrod, R.; et al. The development and validation of the Bronchiectasis Health Questionnaire. Eur. Respir. J. 2017, 49, 1601532. [Google Scholar] [CrossRef] [Green Version]
- Hill, A.T.; Welham, S.A.; Sullivan, A.L.; Loebinger, M.R. Updated BTS Adult Bronchiectasis Guideline 2018: A multidisciplinary approach to comprehensive care. Thorax 2019, 74, 1–3. [Google Scholar] [CrossRef]
- Lee, A.L.; Hill, C.J.; Cecins, N.; Jenkins, S.; McDonald, C.F.; Burge, A.T.; Rautela, L.; Stirling, R.G.; Thompson, P.J.; Holland, A.E. The short and long term effects of exercise training in non-cystic fibrosis bronchiectasis—A randomised controlled trial. Respir. Res. 2014, 15, 44. [Google Scholar] [CrossRef] [Green Version]
- Lee, A.L.; Hill, C.J.; McDonald, C.F.; Holland, A.E. Pulmonary rehabilitation in individuals with non-cystic fibrosis bronchiectasis: A systematic review. Arch. Phys. Med. Rehabil. 2017, 98, 774–782. [Google Scholar] [CrossRef]
- Chalmers, J.D.; Crichton, M.L.; Brady, G.; Finch, S.; Lonergan, M.; Fardon, T.C. Pulmonary rehabilitation after exacerbation of bronchiectasis: A pilot randomized controlled trial. BMC Pulm. Med. 2019, 19, 85. [Google Scholar] [CrossRef]
- Patel, S.; Cole, A.D.; Nolan, C.M.; Barker, R.E.; Jones, S.E.; Kon, S.; Cairn, J.; Loebinger, M.; Wilson, R.; Man, W.D. Pulmonary rehabilitation in bronchiectasis: A propensity-matched study. Eur. Respir. J. 2019, 53, 1801264. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, B.; Casey, D.; Devane, D.; Murphy, K.; Murphy, E.; Lacasse, Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 2015, 2, CD003793. [Google Scholar] [CrossRef] [PubMed]
- Metersky, M.L.; ZuWallack, R.L. Pulmonary rehabilitation for bronchiectasis: If not now, when? Eur. Respir. J. 2019, 53, 1802474. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rochester, C.L.; Vogiatzis, I.; Holland, A.E.; Lareau, S.C.; Marciniuk, D.D.; Puhan, M.A.; Spruit, M.A.; Masefield, S.; Casaburi, R.; Clini, E.M.; et al. An official American Thoracic Society/European Respiratory Society Policy statement: Enhancing implementation, use, and delivery of pulmonary rehabilitation. Am. J. Respir. Crit. Care Med. 2015, 192, 1373–1386. [Google Scholar] [CrossRef] [Green Version]
- Sabit, R.; Griffiths, T.L.; Watkins, A.J.; Evans, W.; Bolton, C.E.; Shale, D.J.; Lewis, K.E. Predictors of poor attendance at an outpatient pulmonary rehabilitation programme. Respir. Med. 2008, 102, 819–824. [Google Scholar] [CrossRef] [Green Version]
- Cox, N.S.; Dal Corso, S.; Hansen, H.; McDonald, C.F.; Hill, C.J.; Zanaboni, P.; Alison, J.A.; O′Halloran, P.; Macdonald, H.; Holland, A.E. Telerehabilitation for chronic respiratory disease. Cochrane Database Syst. Rev. 2021, 1, CD013040. [Google Scholar] [CrossRef]
- José, A.; Holland, A.E.; Selman, J.P.; de Camargo, C.O.; Fonseca, D.S.; Athanazio, R.A.; Rached, S.Z.; Cukier, A.; Stelmach, R.; Dal Corso, S. Home-based pulmonary rehabilitation in people with bronchiectasis: A randomised controlled trial. ERJ Open Res. 2021, 7, 00021-2021. [Google Scholar] [CrossRef]
- Mehrotra, A.; Chernew, M.E.; Linetsky, D.; Hatch, H.; Cutler, D.A.; Schneider, E.C. The Impact of COVID-19 on Outpatient Visits in 2020: Visits Remained Stable, Despite a Late Surge in Cases. Available online: https://www.commonwealthfund.org/publications/2021/feb/impact-covid-19-outpatient-visits-2020-visits-stable-despite-late-surge (accessed on 12 October 2021).
- Nissen, L.; Lindhardt, T. A qualitative study of COPD-patients′ experience of a telemedicine intervention. Int. J. Med. Inform. 2017, 107, 11–17. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Congrete, S.; Metersky, M.L. Telemedicine and Remote Monitoring as an Adjunct to Medical Management of Bronchiectasis. Life 2021, 11, 1196. https://doi.org/10.3390/life11111196
Congrete S, Metersky ML. Telemedicine and Remote Monitoring as an Adjunct to Medical Management of Bronchiectasis. Life. 2021; 11(11):1196. https://doi.org/10.3390/life11111196
Chicago/Turabian StyleCongrete, Soontharee, and Mark L. Metersky. 2021. "Telemedicine and Remote Monitoring as an Adjunct to Medical Management of Bronchiectasis" Life 11, no. 11: 1196. https://doi.org/10.3390/life11111196
APA StyleCongrete, S., & Metersky, M. L. (2021). Telemedicine and Remote Monitoring as an Adjunct to Medical Management of Bronchiectasis. Life, 11(11), 1196. https://doi.org/10.3390/life11111196





