Vascular Wall Reactions to Coronary Stents—Clinical Implications for Stent Failure
Abstract
1. Introduction
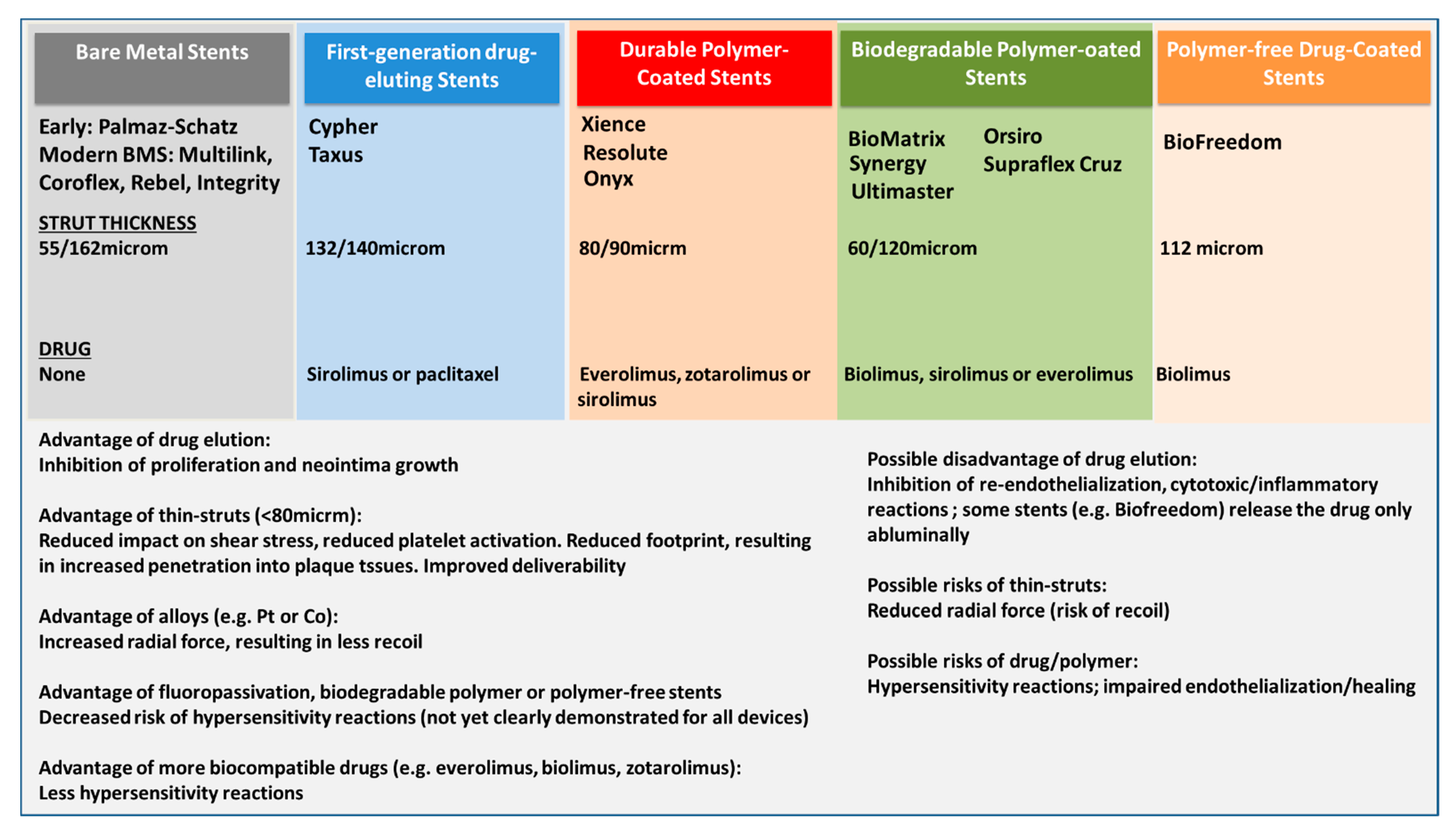
2. Stent Complications and Stent Pathology among Different Device Generations
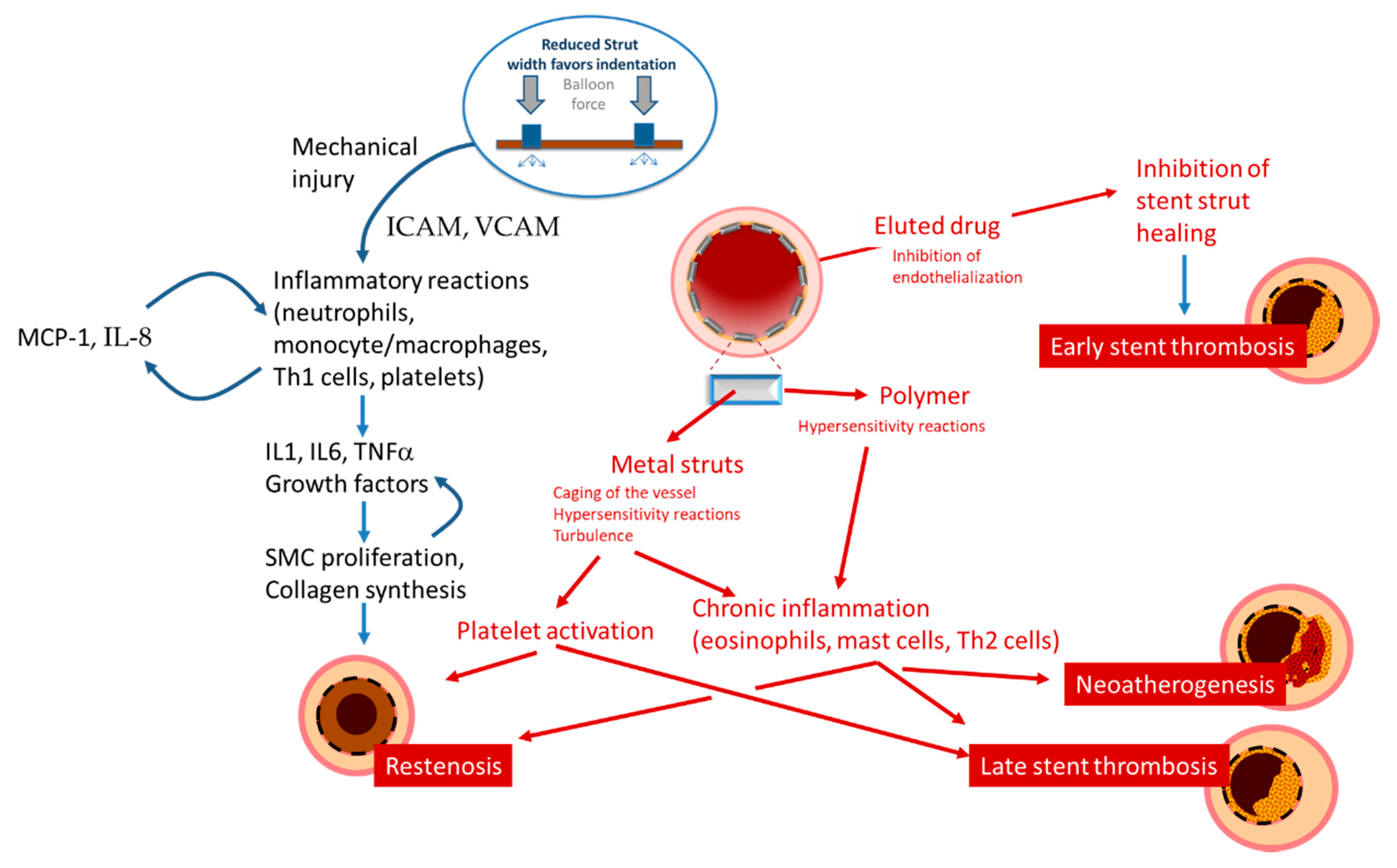
3. The Mechanisms of Restenosis
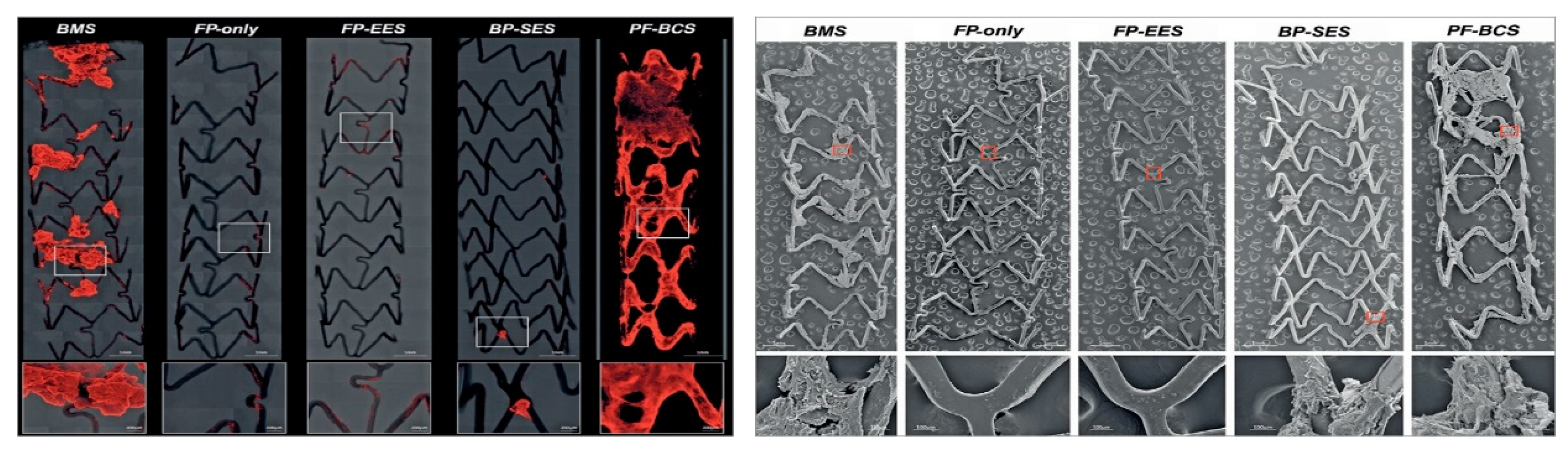
4. The Mechanisms of Stent Thrombosis
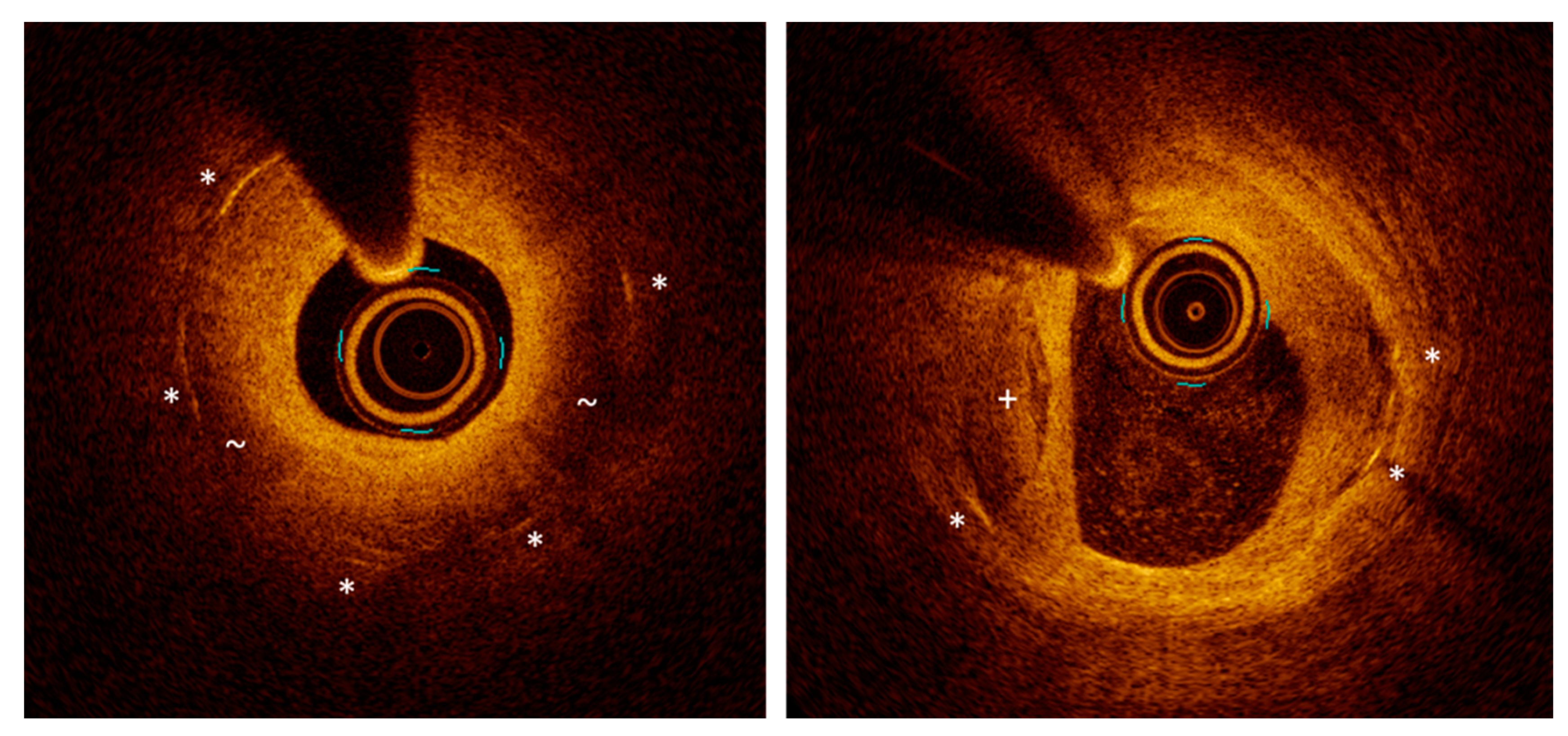
5. Neoatherogenesis: A Long-Term Complication
6. Conclusions
Funding
Conflicts of Interest
References
- Timmis, A.; Townsend, N.; Gale, C.; Grobbee, R.; Maniadakis, N.; Flather, M.; Wilkins, E.; Wright, L.; Vos, R.; Bax, J.; et al. European Society of Cardiology: Cardiovascular Disease Statistics 2017. Eur. Heart J. 2018, 39, 508–579. [Google Scholar] [CrossRef] [PubMed]
- Moses, J.W.; Leon, M.B.; Popma, J.J.; Fitzgerald, P.J.; Holmes, D.R.; O‘Shaughnessy, C.; Caputo, R.P.; Kereiakes, D.J.; Williams, D.O.; Teirstein, P.S.; et al. Sirolimus-eluting stents versus standard stents in patients with stenosis in a native coronary artery. N. Engl. J. Med. 2003, 349, 1315–1323. [Google Scholar] [CrossRef] [PubMed]
- Waksman, R.; Kirtane, A.J.; Torguson, R.; Cohen, D.J.; Ryan, T.; Raber, L.; Applegate, R.; Waxman, S.; Gordon, P.; Kaneshige, K.; et al. Correlates and outcomes of late and very late drug-eluting stent thrombosis: Results from DESERT (International Drug-Eluting Stent Event Registry of Thrombosis). JACC Cardiovasc. Interv. 2014, 7, 1093–1102. [Google Scholar] [CrossRef] [PubMed]
- Claessen, B.E.; Henriques, J.P.; Jaffer, F.A.; Mehran, R.; Piek, J.J.; Dangas, G.D. Stent thrombosis: A clinical perspective. JACC Cardiovasc. Interv. 2014, 7, 1081–1092. [Google Scholar] [CrossRef] [PubMed]
- Torrado, J.; Buckley, L.; Duran, A.; Trujillo, P.; Toldo, S.; Valle Raleigh, J.; Abbate, A.; Biondi-Zoccai, G.; Guzman, L.A. Restenosis, Stent Thrombosis, and Bleeding Complications: Navigating Between Scylla and Charybdis. J. Am. Coll. Cardiol. 2018, 71, 1676–1695. [Google Scholar] [CrossRef] [PubMed]
- Iakovou, I.; Schmidt, T.; Bonizzoni, E.; Ge, L.; Sangiorgi, G.M.; Stankovic, G.; Airoldi, F.; Chieffo, A.; Montorfano, M.; Carlino, M.; et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA 2005, 293, 2126–2130. [Google Scholar] [CrossRef] [PubMed]
- Claessen, B.E.; Dangas, G.D. The quest for the optimal treatment for in-stent restenosis. Catheter. Cardiovasc. Interv. 2018, 92, 300–301. [Google Scholar] [CrossRef]
- Magalhaes, M.A.; Minha, S.; Chen, F.; Torguson, R.; Omar, A.F.; Loh, J.P.; Escarcega, R.O.; Lipinski, M.J.; Baker, N.C.; Kitabata, H.; et al. Clinical presentation and outcomes of coronary in-stent restenosis across 3-stent generations. Circ. Cardiovasc. Interv. 2014, 7, 768–776. [Google Scholar] [CrossRef]
- Gori, T.; Polimeni, A.; Indolfi, C.; Raber, L.; Adriaenssens, T.; Munzel, T. Predictors of stent thrombosis and their implications for clinical practice. Nat. Rev. Cardiol. 2019, 16, 243–256. [Google Scholar] [CrossRef]
- Kawamoto, R.; Hatakeyama, K.; Imamura, T.; Ishikawa, T.; Date, H.; Shibata, Y.; Takenaga, M.; Asada, Y.; Eto, T. Relation of C-reactive protein to restenosis after coronary stent implantation and to restenosis after coronary atherectomy. Am. J. Cardiol. 2004, 94, 104–107. [Google Scholar] [CrossRef]
- Yilmaz, S.; Sen, F.; Unal, S.; Yayla, C.; Ozeke, O.; Aras, D.; Topaloglu, S.; Aydogdu, S. Usefulness of the platelet-to-lymphocyte ratio in predicting bare-metal stent restenosis. Scand. Cardiovasc. J. 2015, 49, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Liu, Y.; Jiang, H.; Ding, X.; Zhu, R.; Li, B.; Zhao, Y. Plasma levels of interleukin 18, interleukin 10, and matrix metalloproteinase-9 and -137G/C polymorphism of interleukin 18 are associated with incidence of in-stent restenosis after percutaneous coronary intervention. Inflammation 2013, 36, 1129–1135. [Google Scholar] [CrossRef] [PubMed]
- Ullrich, H.; Munzel, T.; Gori, T. Coronary Stent Thrombosis- Predictors and Prevention. Dtsch. Arztebl. Int. 2020, 117, 320–326. [Google Scholar] [CrossRef] [PubMed]
- Tada, T.; Byrne, R.A.; Simunovic, I.; King, L.A.; Cassese, S.; Joner, M.; Fusaro, M.; Schneider, S.; Schulz, S.; Ibrahim, T.; et al. Risk of stent thrombosis among bare-metal stents, first-generation drug-eluting stents, and second-generation drug-eluting stents: Results from a registry of 18,334 patients. JACC Cardiovasc. Interv. 2013, 6, 1267–1274. [Google Scholar] [CrossRef] [PubMed]
- Palmerini, T.; Biondi-Zoccai, G.; Della Riva, D.; Mariani, A.; Genereux, P.; Branzi, A.; Stone, G.W. Stent thrombosis with drug-eluting stents: Is the paradigm shifting? J. Am. Coll. Cardiol. 2013, 62, 1915–1921. [Google Scholar] [CrossRef]
- Sakamoto, A.; Jinnouchi, H.; Torii, S.; Virmani, R.; Finn, A.V. Understanding the Impact of Stent and Scaffold Material and Strut Design on Coronary Artery Thrombosis from the Basic and Clinical Points of View. Bioengineering 2018, 5, 71. [Google Scholar] [CrossRef]
- Vorpahl, M.; Yazdani, S.K.; Nakano, M.; Ladich, E.; Kolodgie, F.D.; Finn, A.V.; Virmani, R. Pathobiology of stent thrombosis after drug-eluting stent implantation. Curr. Pharm. Des. 2010, 16, 4064–4071. [Google Scholar] [CrossRef]
- Finn, A.V.; Nakazawa, G.; Joner, M.; Kolodgie, F.D.; Mont, E.K.; Gold, H.K.; Virmani, R. Vascular responses to drug eluting stents: Importance of delayed healing. Arterioscler. Thromb. Vasc. Biol. 2007, 27, 1500–1510. [Google Scholar] [CrossRef]
- Nakazawa, G.; Finn, A.V.; Vorpahl, M.; Ladich, E.R.; Kolodgie, F.D.; Virmani, R. Coronary responses and differential mechanisms of late stent thrombosis attributed to first-generation sirolimus- and paclitaxel-eluting stents. J. Am. Coll. Cardiol. 2011, 57, 390–398. [Google Scholar] [CrossRef]
- Borovac, J.A.; D‘Amario, D.; Vergallo, R.; Porto, I.; Bisignani, A.; Galli, M.; Annibali, G.; Montone, R.A.; Leone, A.M.; Niccoli, G.; et al. Neoatherosclerosis after drug-eluting stent implantation: A novel clinical and therapeutic challenge. Eur. Heart J. Cardiovasc. Pharmacother. 2019, 5, 105–116. [Google Scholar] [CrossRef]
- Garcia-Garcia, H.M.; McFadden, E.P.; Farb, A.; Mehran, R.; Stone, G.W.; Spertus, J.; Onuma, Y.; Morel, M.A.; van Es, G.A.; Zuckerman, B.; et al. Standardized End Point Definitions for Coronary Intervention Trials: The Academic Research Consortium-2 Consensus Document. Circulation 2018, 137, 2635–2650. [Google Scholar] [CrossRef] [PubMed]
- Kruger-Genge, A.; Hiebl, B.; Franke, R.P.; Lendlein, A.; Jung, F. Effects of Tacrolimus or Sirolimus on the adhesion of vascular wall cells: Controlled in-vitro comparison study. Clin. Hemorheol. Microcirc. 2017, 67, 309–318. [Google Scholar] [CrossRef] [PubMed]
- Mori, H.; Otsuka, F.; Gupta, A.; Jinnouchi, H.; Torii, S.; Harari, E.; Virmani, R.; Finn, A.V. Revisiting the role of durable polymers in cardiovascular devices. Expert Rev. Cardiovasc. Ther. 2017, 15, 835–846. [Google Scholar] [CrossRef] [PubMed]
- Szott, L.M.; Irvin, C.A.; Trollsas, M.; Hossainy, S.; Ratner, B.D. Blood compatibility assessment of polymers used in drug eluting stent coatings. Biointerphases 2016, 11, 029806. [Google Scholar] [CrossRef] [PubMed]
- Torii, S.; Cheng, Q.; Mori, H.; Lipinski, M.J.; Acampado, E.; Perkins, L.E.L.; Hossainy, S.F.; Pacetti, S.D.; Kolodgie, F.D.; Virmani, R.; et al. Acute thrombogenicity of fluoropolymer-coated versus biodegradable and polymer-free stents. EuroIntervention 2019, 14, 1685–1693. [Google Scholar] [CrossRef] [PubMed]
- Bangalore, S.; Toklu, B.; Patel, N.; Feit, F.; Stone, G.W. Newer-Generation Ultrathin Strut Drug-Eluting Stents Versus Older Second-Generation Thicker Strut Drug-Eluting Stents for Coronary Artery Disease. Circulation 2018, 138, 2216–2226. [Google Scholar] [CrossRef]
- Iantorno, M.; Lipinski, M.J.; Garcia-Garcia, H.M.; Forrestal, B.J.; Rogers, T.; Gajanana, D.; Buchanan, K.D.; Torguson, R.; Weintraub, W.S.; Waksman, R. Meta-Analysis of the Impact of Strut Thickness on Outcomes in Patients With Drug-Eluting Stents in a Coronary Artery. Am. J. Cardiol. 2018, 122, 1652–1660. [Google Scholar] [CrossRef]
- Taniguchi, Y.; Otake, H.; Shinke, T.; Nakagawa, M.; Hariki, H.; Inoue, T.; Osue, T.; Hiranuma, N.; Nishio, R.; Kinutani, H.; et al. Two-year vessel healing after everolimus-eluting stent implantation: Serial assessment by optical coherence tomography. J. Cardiol. 2015, 65, 298–304. [Google Scholar] [CrossRef][Green Version]
- Kawakami, R.; Hao, H.; Imanaka, T.; Shibuya, M.; Ueda, Y.; Tsujimoto, M.; Ishibashi-Ueda, H.; Hirota, S. Initial pathological responses of second-generation everolimus-eluting stents implantation in Japanese coronary arteries: Comparison with first-generation sirolimus-eluting stents. J. Cardiol. 2018, 71, 452–457. [Google Scholar] [CrossRef]
- Picard, F.; Pighi, M.; de Hemptinne, Q.; Airaksinen, J.; Vinco, G.; de Pommereau, A.; Biancari, F.; Varenne, O. Comparison of the biodegradable polymer everolimus-eluting stent with contemporary drug-eluting stents: A systematic review and meta-analysis. Int. J. Cardiol. 2019, 278, 51–56. [Google Scholar] [CrossRef]
- Anadol, R.; Gori, T. The mechanisms of late scaffold thrombosis. Clin. Hemorheol. Microcirc. 2017, 67, 343–346. [Google Scholar] [CrossRef] [PubMed]
- Kereiakes, D.J.; Onuma, Y.; Serruys, P.W.; Stone, G.W. Bioresorbable Vascular Scaffolds for Coronary Revascularization. Circulation 2016, 134, 168–182. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.S.; John, J.M.; Chew, D.P.; Lee, D.S.; Ellis, S.G.; Bhatt, D.L. Bare metal stent restenosis is not a benign clinical entity. Am. Heart J. 2006, 151, 1260–1264. [Google Scholar] [CrossRef] [PubMed]
- Schnorbus, B.; Daiber, A.; Jurk, K.; Warnke, S.; Koenig, J.; Lackner, K.J.; Munzel, T.; Gori, T. Effects of clopidogrel vs. prasugrel vs. ticagrelor on endothelial function, inflammatory parameters, and platelet function in patients with acute coronary syndrome undergoing coronary artery stenting: A randomized, blinded, parallel study. Eur. Heart J. 2020, 41, 3144–3152. [Google Scholar] [CrossRef]
- Gori, T. Endothelial Function: A Short Guide for the Interventional Cardiologist. Int. J. Mol. Sci. 2018, 19, 3838. [Google Scholar] [CrossRef]
- Donners, M.M.; Daemen, M.J.; Cleutjens, K.B.; Heeneman, S. Inflammation and restenosis: Implications for therapy. Ann. Med. 2003, 35, 523–531. [Google Scholar] [CrossRef]
- Christen, T.; Verin, V.; Bochaton-Piallat, M.; Popowski, Y.; Ramaekers, F.; Debruyne, P.; Camenzind, E.; van Eys, G.; Gabbiani, G. Mechanisms of neointima formation and remodeling in the porcine coronary artery. Circulation 2001, 103, 882–888. [Google Scholar] [CrossRef]
- Puricel, S.; Kallinikou, Z.; Espinola, J.; Arroyo, D.; Goy, J.J.; Stauffer, J.C.; Baeriswyl, G.; Smits, P.C.; Cook, S.; Togni, M. Comparison of endothelium-dependent and -independent vasomotor response after abluminal biodegradable polymer biolimus-eluting stent and persistent polymer everolimus-eluting stent implantation (COMPARE-IT). Int. J. Cardiol. 2016, 202, 525–531. [Google Scholar] [CrossRef]
- Togni, M.; Raber, L.; Cocchia, R.; Wenaweser, P.; Cook, S.; Windecker, S.; Meier, B.; Hess, O.M. Local vascular dysfunction after coronary paclitaxel-eluting stent implantation. Int. J. Cardiol. 2007, 120, 212–220. [Google Scholar] [CrossRef]
- Inoue, T.; Croce, K.; Morooka, T.; Sakuma, M.; Node, K.; Simon, D.I. Vascular inflammation and repair: Implications for re-endothelialization, restenosis, and stent thrombosis. JACC Cardiovasc. Interv. 2011, 4, 1057–1066. [Google Scholar] [CrossRef]
- Moldoveanu, E.; Mut-Vitcu, B.; Tanaseanu, G.R.; Marta, D.S.; Manea, G.; Kosaka, T.; Vidulescu, C.; Tanaseanu, C. Low basal levels of circulating adiponectin in patients undergoing coronary stenting predict in-stent restenosis, independently of basal levels of inflammatory markers: Lipoprotein associated phospholipase A2, and myeloperoxidase. Clin. Biochem. 2008, 41, 1429–1433. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Li, M.; Lu, H.; Qiao, W.; Xi, D.; Luo, T.; Xiong, H.; Guo, Z. Effects of probucol on restenosis after percutaneous coronary intervention: A systematic review and meta-analysis. PLoS ONE 2015, 10, e0124021. [Google Scholar] [CrossRef] [PubMed]
- Kufner, S.; Sorges, J.; Mehilli, J.; Cassese, S.; Repp, J.; Wiebe, J.; Lohaus, R.; Lahmann, A.; Rheude, T.; Ibrahim, T.; et al. Randomized Trial of Polymer-Free Sirolimus- and Probucol-Eluting Stents Versus Durable Polymer Zotarolimus-Eluting Stents: 5-Year Results of the ISAR-TEST-5 Trial. JACC Cardiovasc. Interv. 2016, 9, 784–792. [Google Scholar] [CrossRef] [PubMed]
- Guerra, E.; Byrne, R.A.; Kastrati, A. Pharmacological inhibition of coronary restenosis: Systemic and local approaches. Expert Opin. Pharmacother. 2014, 15, 2155–2171. [Google Scholar] [CrossRef]
- Ullrich, H.; Gori, T. The pleiotropic effects of antiplatelet therapies. Clin. Hemorheol. Microcirc. 2019, 73, 29–34. [Google Scholar] [CrossRef]
- Cook, S.; Ladich, E.; Nakazawa, G.; Eshtehardi, P.; Neidhart, M.; Vogel, R.; Togni, M.; Wenaweser, P.; Billinger, M.; Seiler, C.; et al. Correlation of intravascular ultrasound findings with histopathological analysis of thrombus aspirates in patients with very late drug-eluting stent thrombosis. Circulation 2009, 120, 391–399. [Google Scholar] [CrossRef]
- Nebeker, J.R.; Virmani, R.; Bennett, C.L.; Hoffman, J.M.; Samore, M.H.; Alvarez, J.; Davidson, C.J.; McKoy, J.M.; Raisch, D.W.; Whisenant, B.K.; et al. Hypersensitivity cases associated with drug-eluting coronary stents: A review of available cases from the Research on Adverse Drug Events and Reports (RADAR) project. J. Am. Coll. Cardiol. 2006, 47, 175–181. [Google Scholar] [CrossRef]
- Virmani, R.; Guagliumi, G.; Farb, A.; Musumeci, G.; Grieco, N.; Motta, T.; Mihalcsik, L.; Tespili, M.; Valsecchi, O.; Kolodgie, F.D. Localized hypersensitivity and late coronary thrombosis secondary to a sirolimus-eluting stent: Should we be cautious? Circulation 2004, 109, 701–705. [Google Scholar] [CrossRef]
- Chaabane, C.; Otsuka, F.; Virmani, R.; Bochaton-Piallat, M.L. Biological responses in stented arteries. Cardiovasc. Res. 2013, 99, 353–363. [Google Scholar] [CrossRef]
- Koster, R.; Vieluf, D.; Kiehn, M.; Sommerauer, M.; Kahler, J.; Baldus, S.; Meinertz, T.; Hamm, C.W. Nickel and molybdenum contact allergies in patients with coronary in-stent restenosis. Lancet 2000, 356, 1895–1897. [Google Scholar] [CrossRef]
- Hiebl, B.; Nennig, E.; Schiestel, S.; Kovacs, A.; Jung, F.; Fischer, H. Biocompatibility of a novel zinc stent with a closed-cell-design. Clin. Hemorheol. Microcirc. 2015, 61, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Jinnouchi, H.; Kutyna, M.; Torii, S.; Cheng, Q.; Sakamoto, A.; Guo, L.; Cornelissen, A.; Perkins, L.E.L.; Hossainy, S.F.; Pacetti, S.D.; et al. Comparison of Acute Thrombogenicity and Albumin Adsorption in Three Different Durable Polymer Coronary Drug-Eluting Stents. EuroIntervention 2020. [Google Scholar] [CrossRef]
- Mori, M.; Sakata, K.; Yokawa, J.; Nakanishi, C.; Murai, K.; Okada, H.; Shimojima, M.; Yoshida, S.; Yoshioka, K.; Takuwa, Y.; et al. Everolimus-Eluting Biodegradable Abluminal Coating Stent versus Durable Conformal Coating Stent: Termination of the Inflammatory Response Associated with Neointimal Healing in a Porcine Coronary Model. J. Interv. Cardiol. 2020, 2020, 1956015. [Google Scholar] [CrossRef] [PubMed]
- Riegger, J.; Byrne, R.A.; Joner, M.; Chandraratne, S.; Gershlick, A.H.; Ten Berg, J.M.; Adriaenssens, T.; Guagliumi, G.; Godschalk, T.C.; Neumann, F.J.; et al. Histopathological evaluation of thrombus in patients presenting with stent thrombosis. A multicenter European study: A report of the prevention of late stent thrombosis by an interdisciplinary global European effort consortium. Eur. Heart J. 2016, 37, 1538–1549. [Google Scholar] [CrossRef]
- Taniwaki, M.; Radu, M.D.; Zaugg, S.; Amabile, N.; Garcia-Garcia, H.M.; Yamaji, K.; Jorgensen, E.; Kelbaek, H.; Pilgrim, T.; Caussin, C.; et al. Mechanisms of Very Late Drug-Eluting Stent Thrombosis Assessed by Optical Coherence Tomography. Circulation 2016, 133, 650–660. [Google Scholar] [CrossRef]
- Polimeni, A.; Sorrentino, S.; Spaccarotella, C.; Mongiardo, A.; Sabatino, J.; De Rosa, S.; Gori, T.; Indolfi, C. Stent Thrombosis After Percutaneous Coronary Intervention: From Bare-Metal to the Last Generation of Drug-Eluting Stents. Cardiol. Clin. 2020, 38, 639–647. [Google Scholar] [CrossRef]
- de Winter, R.J.; Katagiri, Y.; Asano, T.; Milewski, K.P.; Lurz, P.; Buszman, P.; Jessurun, G.A.J.; Koch, K.T.; Troquay, R.P.T.; Hamer, B.J.B.; et al. A sirolimus-eluting bioabsorbable polymer-coated stent (MiStent) versus an everolimus-eluting durable polymer stent (Xience) after percutaneous coronary intervention (DESSOLVE III): A randomised, single-blind, multicentre, non-inferiority, phase 3 trial. Lancet 2018, 391, 431–440. [Google Scholar] [CrossRef]
- Cassese, S.; Ndrepepa, G.; Byrne, R.A.; Kufner, S.; Lahmann, A.L.; Mankerious, N.; Xhepa, E.; Laugwitz, K.L.; Schunkert, H.; Fusaro, M.; et al. Outcomes of patients treated with ultrathin-strut biodegradable polymer sirolimus-eluting stents versus fluoropolymer-based everolimus-eluting stents: A meta-analysis of randomised trials. EuroIntervention 2018, 14, 224–231. [Google Scholar] [CrossRef]
- El-Hayek, G.; Bangalore, S.; Casso Dominguez, A.; Devireddy, C.; Jaber, W.; Kumar, G.; Mavromatis, K.; Tamis-Holland, J.; Samady, H. Meta-Analysis of Randomized Clinical Trials Comparing Biodegradable Polymer Drug-Eluting Stent to Second-Generation Durable Polymer Drug-Eluting Stents. JACC Cardiovasc. Interv. 2017, 10, 462–473. [Google Scholar] [CrossRef]
- Yamaji, K.; Zanchin, T.; Zanchin, C.; Stortecky, S.; Koskinas, K.C.; Hunziker, L.; Praz, F.; Blochlinger, S.; Moro, C.; Moschovitis, A.; et al. Unselected Use of Ultrathin Strut Biodegradable Polymer Sirolimus-Eluting Stent Versus Durable Polymer Everolimus-Eluting Stent for Coronary Revascularization. Circ. Cardiovasc. Interv. 2018, 11, e006741. [Google Scholar] [CrossRef]
- Zhu, P.; Zhou, X.; Zhang, C.; Li, H.; Zhang, Z.; Song, Z. Safety and efficacy of ultrathin strut biodegradable polymer sirolimus-eluting stent versus durable polymer drug-eluting stents: A meta-analysis of randomized trials. BMC Cardiovasc. Disord. 2018, 18, 170. [Google Scholar] [CrossRef] [PubMed]
- Jeger, R.V.; Brunner-La Rocca, H.P.; Bertel, O.; Kiowski, W.; Pfisterer, M.E.; Kaiser, C.A.; Investigators, B. Stent thrombosis after coronary stent implantation: A protective effect of high-dose statin therapy? Cardiology 2013, 126, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H.C.; Ahn, Y.; Hong, Y.J.; Kim, J.H.; Jeong, M.H.; Kim, Y.J.; Chae, S.C.; Cho, M.C.; Other Korea Acute Myocardial Infarction Registry, I. Statin therapy to reduce stent thrombosis in acute myocardial infarction patients with elevated high-sensitivity C-reactive protein. Int. J. Cardiol. 2013, 167, 1848–1853. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, D.; Yasumura, K.; Nakamura, H.; Matsuhiro, Y.; Yasumoto, K.; Tanaka, A.; Matsunaga-Lee, Y.; Yano, M.; Yamato, M.; Egami, Y.; et al. Different Neoatherosclerosis Patterns in Drug-Eluting-and Bare-Metal Stent Restenosis—Optical Coherence Tomography Study. Circ. J. 2019, 83, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Ando, H.; Amano, T.; Takashima, H.; Harada, K.; Kitagawa, K.; Suzuki, A.; Kunimura, A.; Shimbo, Y.; Harada, K.; Yoshida, T.; et al. Differences in tissue characterization of restenotic neointima between sirolimus-eluting stent and bare-metal stent: Integrated backscatter intravascular ultrasound analysis for in-stent restenosis. Eur. Heart J. Cardiovasc. Imaging 2013, 14, 996–1001. [Google Scholar] [CrossRef]
- Jinnouchi, H.; Kuramitsu, S.; Shinozaki, T.; Tomoi, Y.; Hiromasa, T.; Kobayashi, Y.; Domei, T.; Soga, Y.; Hyodo, M.; Shirai, S.; et al. Difference of Tissue Characteristics Between Early and Late Restenosis After Second-Generation Drug-Eluting Stents Implantation- An Optical Coherence Tomography Study. Circ. J. 2017, 81, 450–457. [Google Scholar] [CrossRef]
- Joner, M.; Nakazawa, G.; Finn, A.V.; Quee, S.C.; Coleman, L.; Acampado, E.; Wilson, P.S.; Skorija, K.; Cheng, Q.; Xu, X.; et al. Endothelial cell recovery between comparator polymer-based drug-eluting stents. J. Am. Coll. Cardiol. 2008, 52, 333–342. [Google Scholar] [CrossRef]
- Yahagi, K.; Kolodgie, F.D.; Otsuka, F.; Finn, A.V.; Davis, H.R.; Joner, M.; Virmani, R. Pathophysiology of native coronary, vein graft, and in-stent atherosclerosis. Nat. Rev. Cardiol. 2016, 13, 79–98. [Google Scholar] [CrossRef]
- Otsuka, F.; Byrne, R.A.; Yahagi, K.; Mori, H.; Ladich, E.; Fowler, D.R.; Kutys, R.; Xhepa, E.; Kastrati, A.; Virmani, R.; et al. Neoatherosclerosis: Overview of histopathologic findings and implications for intravascular imaging assessment. Eur. Heart J. 2015, 36, 2147–2159. [Google Scholar] [CrossRef]
- Parry, T.J.; Brosius, R.; Thyagarajan, R.; Carter, D.; Argentieri, D.; Falotico, R.; Siekierka, J. Drug-eluting stents: Sirolimus and paclitaxel differentially affect cultured cells and injured arteries. Eur. J. Pharmacol. 2005, 524, 19–29. [Google Scholar] [CrossRef]
- Saxton, R.A.; Sabatini, D.M. mTOR Signaling in Growth, Metabolism, and Disease. Cell 2017, 169, 361–371. [Google Scholar] [CrossRef] [PubMed]
- Jinnouchi, H.; Guo, L.; Sakamoto, A.; Sato, Y.; Cornelissen, A.; Kawakami, R.; Mori, M.; Torii, S.; Kuntz, S.; Harari, E.; et al. Advances in mammalian target of rapamycin kinase inhibitors: Application to devices used in the treatment of coronary artery disease. Future Med. Chem. 2020, 12, 1181–1195. [Google Scholar] [CrossRef] [PubMed]
- Harari, E.; Guo, L.; Smith, S.L.; Paek, K.H.; Fernandez, R.; Sakamoto, A.; Mori, H.; Kutyna, M.D.; Habib, A.; Torii, S.; et al. Direct Targeting of the mTOR (Mammalian Target of Rapamycin) Kinase Improves Endothelial Permeability in Drug-Eluting Stents-Brief Report. Arterioscler. Thromb. Vasc. Biol. 2018, 38, 2217–2224. [Google Scholar] [CrossRef]
- Jang, J.Y.; Kim, J.S.; Shin, D.H.; Kim, B.K.; Ko, Y.G.; Choi, D.; Jang, Y.; Hong, M.K. Favorable effect of optimal lipid-lowering therapy on neointimal tissue characteristics after drug-eluting stent implantation: Qualitative optical coherence tomographic analysis. Atherosclerosis 2015, 242, 553–559. [Google Scholar] [CrossRef] [PubMed]
- Cui, Y.; Liu, Y.; Zhao, F.; Shi, D.; Chen, K. Neoatherosclerosis after Drug-Eluting Stent Implantation: Roles and Mechanisms. Oxid. Med. Cell. Longev. 2016, 2016, 5924234. [Google Scholar] [CrossRef]


| Mechanism(s) Involved | Mediators and Signaling | |
|---|---|---|
| Response to Damage | ||
| Proliferation | Migration of smooth muscle cells, production of membrane metalloproteinases | Cytokines (IL-1, IL-6, TNF-alpha) Growth factors (PDGF, IGF, FGF, VEGF) |
| Remodeling | Remodeling of the neointima, deposition of extracellular matrix, neoatherogenesis | Macrophages/Foam cells Cytokines (IFNgamma) Growth factors (PDGF, TGFbeta, IGF, VEGF) |
| Thrombus Formation | Adhesion and activation of platelets Recruitment and diapedesis of Inflammatory cells | Expression of vWF and TF Turbolent flow Nitric oxide, Thrombin Adhesion molecules Chemotactic factors (IL-8, MCP-1) Cytokines (IL-1, IL-6, TNF-alpha) Growth factors (PDGF, Thrombin) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gori, T. Vascular Wall Reactions to Coronary Stents—Clinical Implications for Stent Failure. Life 2021, 11, 63. https://doi.org/10.3390/life11010063
Gori T. Vascular Wall Reactions to Coronary Stents—Clinical Implications for Stent Failure. Life. 2021; 11(1):63. https://doi.org/10.3390/life11010063
Chicago/Turabian StyleGori, Tommaso. 2021. "Vascular Wall Reactions to Coronary Stents—Clinical Implications for Stent Failure" Life 11, no. 1: 63. https://doi.org/10.3390/life11010063
APA StyleGori, T. (2021). Vascular Wall Reactions to Coronary Stents—Clinical Implications for Stent Failure. Life, 11(1), 63. https://doi.org/10.3390/life11010063




