Proposal for Hemiplegic Thumb Rehabilitation Device Based on Repetitive Facilitation Exercise
Abstract
1. Introduction
2. Analysis of Manual RFE for Thumbs
2.1. Principle of RFE
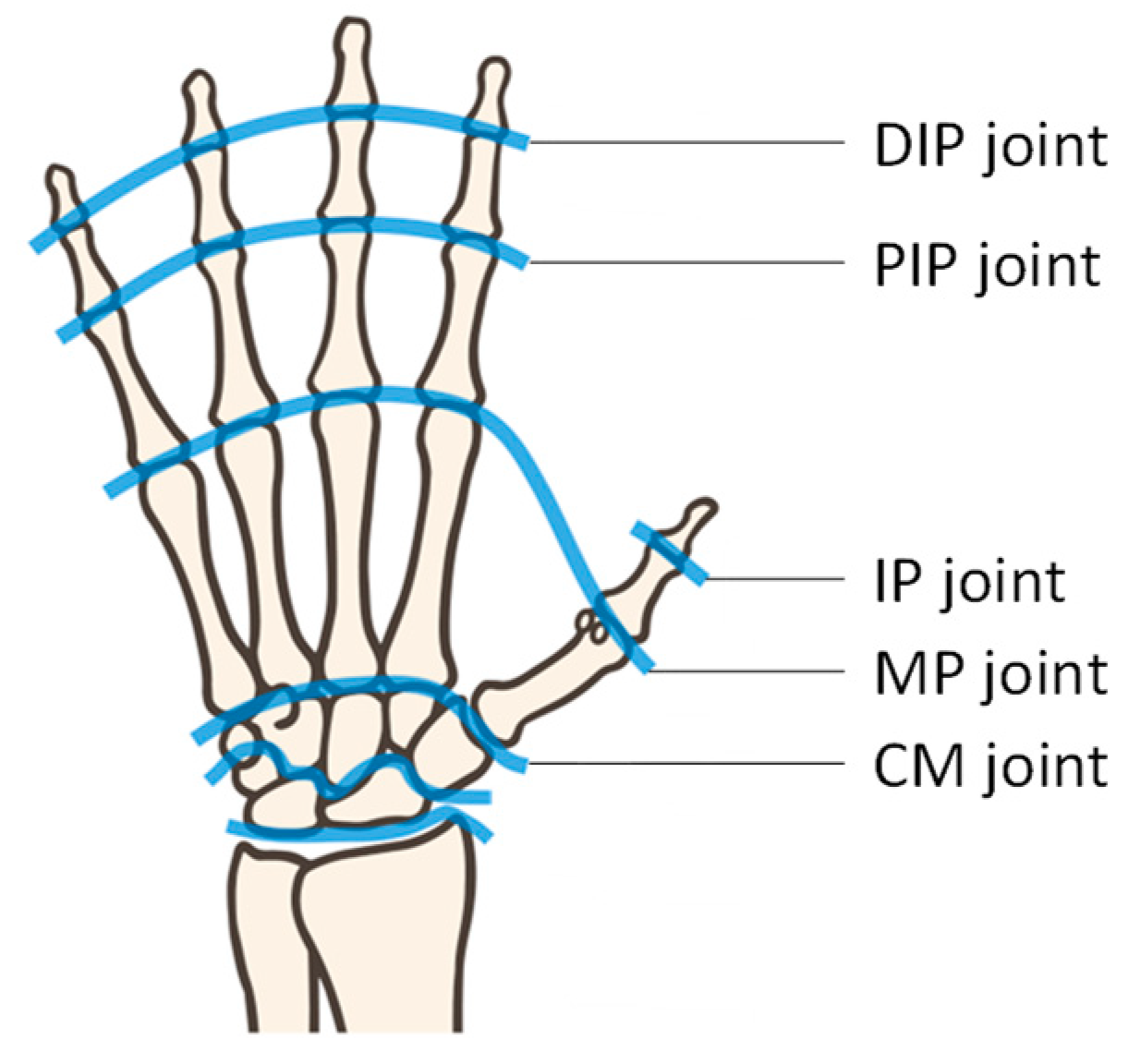
2.2. Movement of Thumb
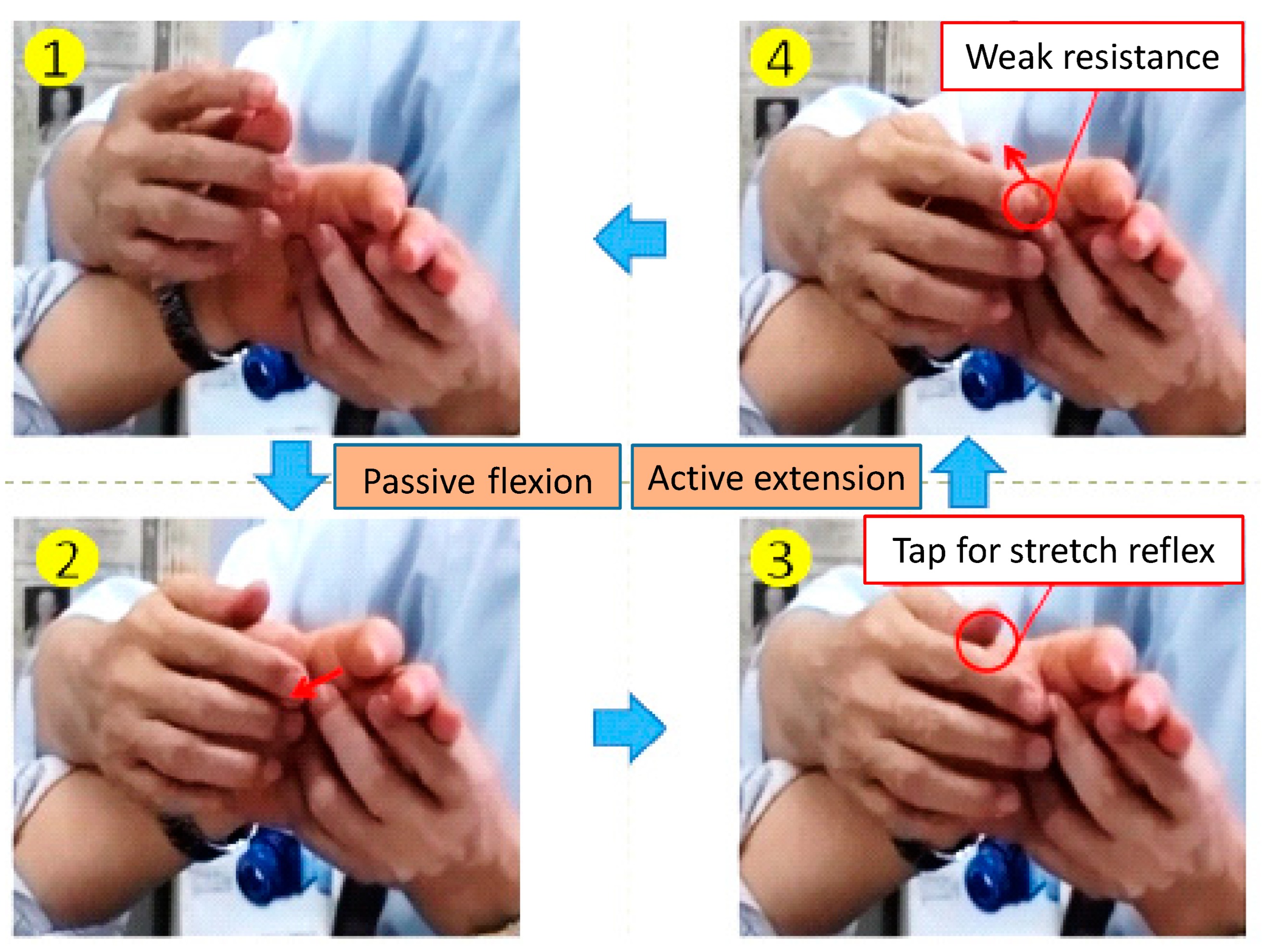
2.3. Manual RFE for Thumb Flexion/Extension
- The therapist passively flexes the hemiplegic thumb;
- The therapist finishes the passive flexion at the maximal flexion position to induce the stretch reflex of the extensor muscle. Thus, the extensor muscles become under muscle tone;
- The therapist gives a signal and taps the MP joint to induce a stretch reflex, facilitating active extension;
- The therapist continues to give slight resistance force against the active extension of the thumb to maintain the tension of the extensor muscle;
- The therapist repeats the above procedure 100 times.
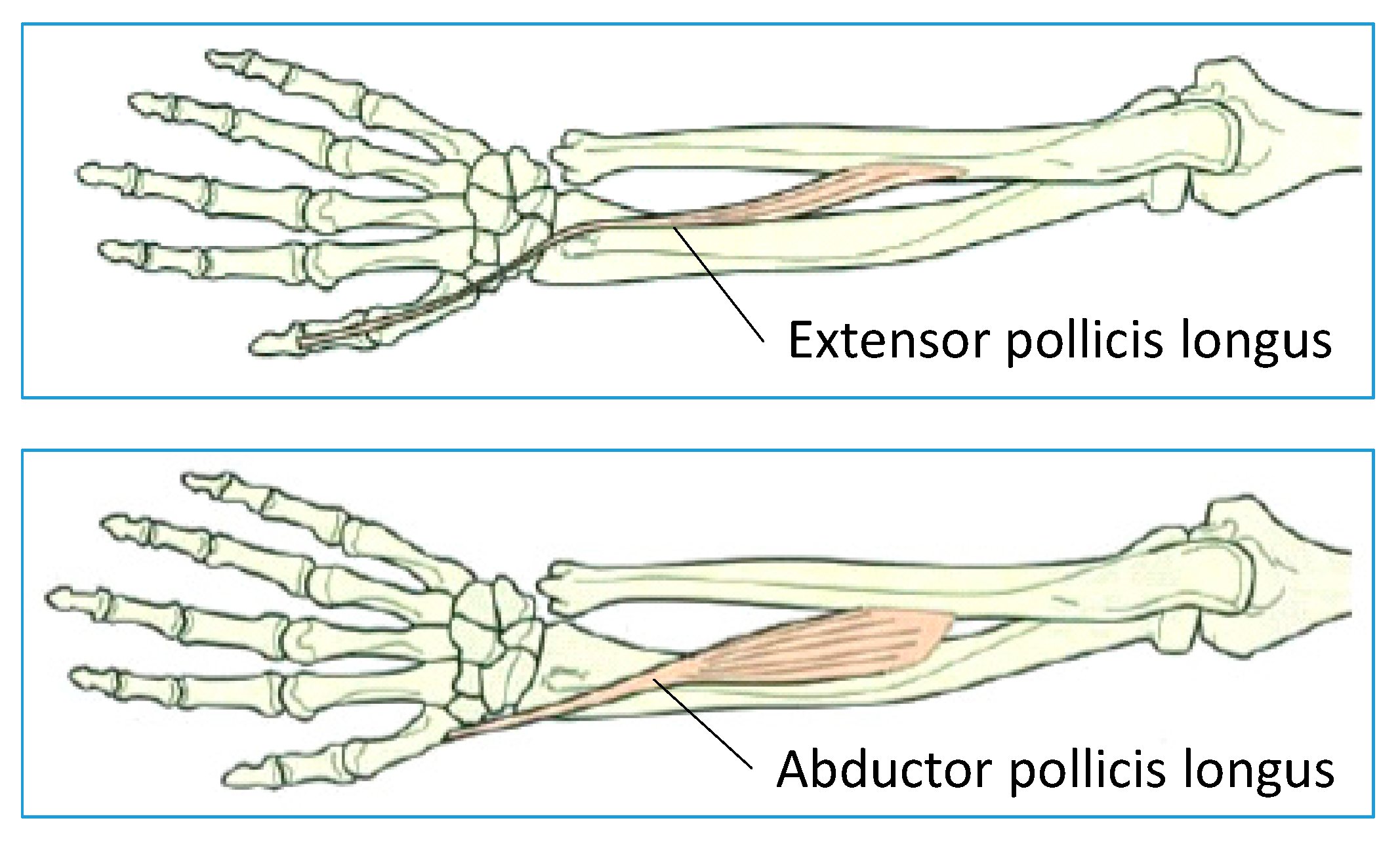
2.4. Manual RFE for Thumb Palmar Adduction/Abduction
- The therapist passively performs palmar adduction on the hemiplegic thumb;
- The therapist finishes the passive palmar adduction at the maximal adduction position to induce the stretch reflex of the palmar abduction muscle; thus, the abductor muscles become under muscle tone;
- The therapist signals and taps the thenar to induce a stretch reflex, enabling active palmar abduction by the patient;
- The therapist continues to give a slight resistance force against the active palmar abduction of the thumb to maintain the tension of the abductor muscle.
- The therapist repeats the above procedure 100 times.
3. Proposed Rehabilitation Device for Hemiplegic Thumb
3.1. Device Specifications
- The device needs to induce stretch reflexes of a target muscle;
- The device needs to track the active motion facilitated by the stretch reflex; in addition, the tracking motion must force slight resistance;
- The device needs a high-sensitivity force sensing mechanism to measure the force of active motion;
- Patients can watch the target thumb;
- The device needs to support training for both the left and right hands with a single device;
- Patients need to be able to easily wear the device while ensuring safety;
- The device needs to be a single-link mechanism owing to low costs.
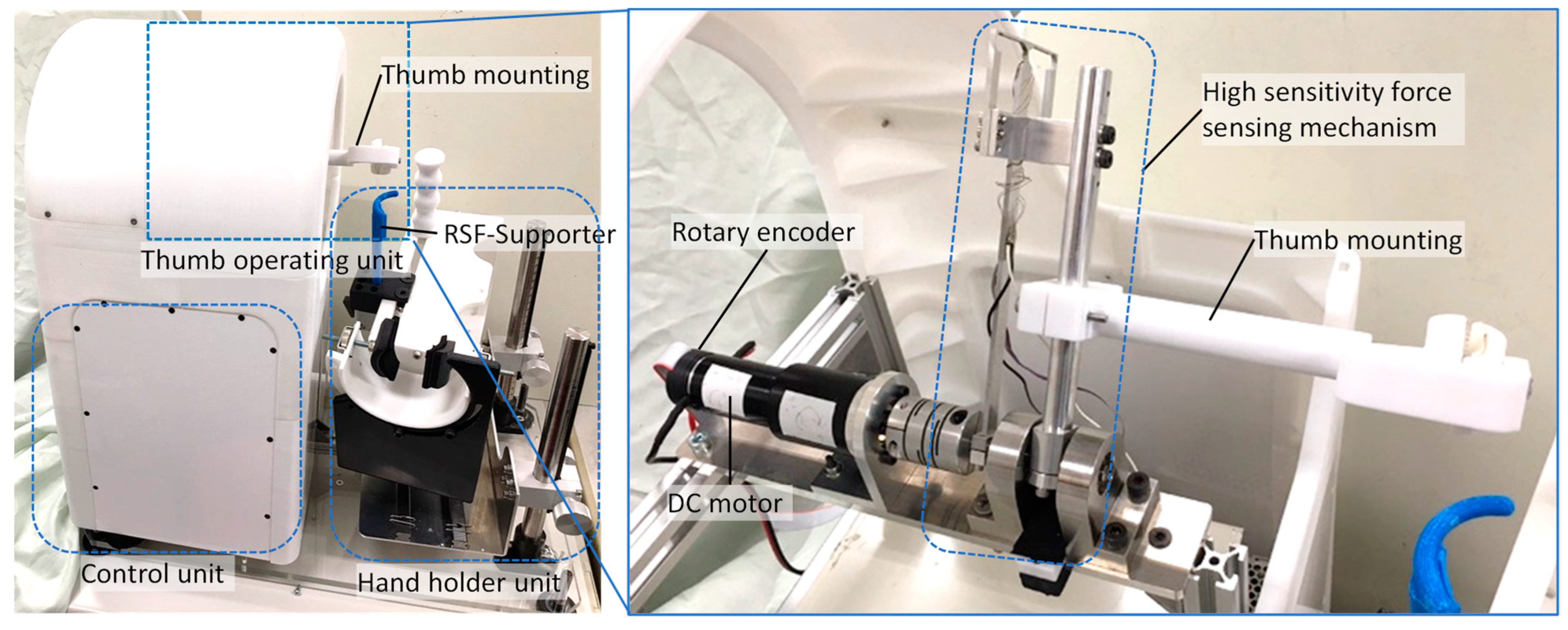
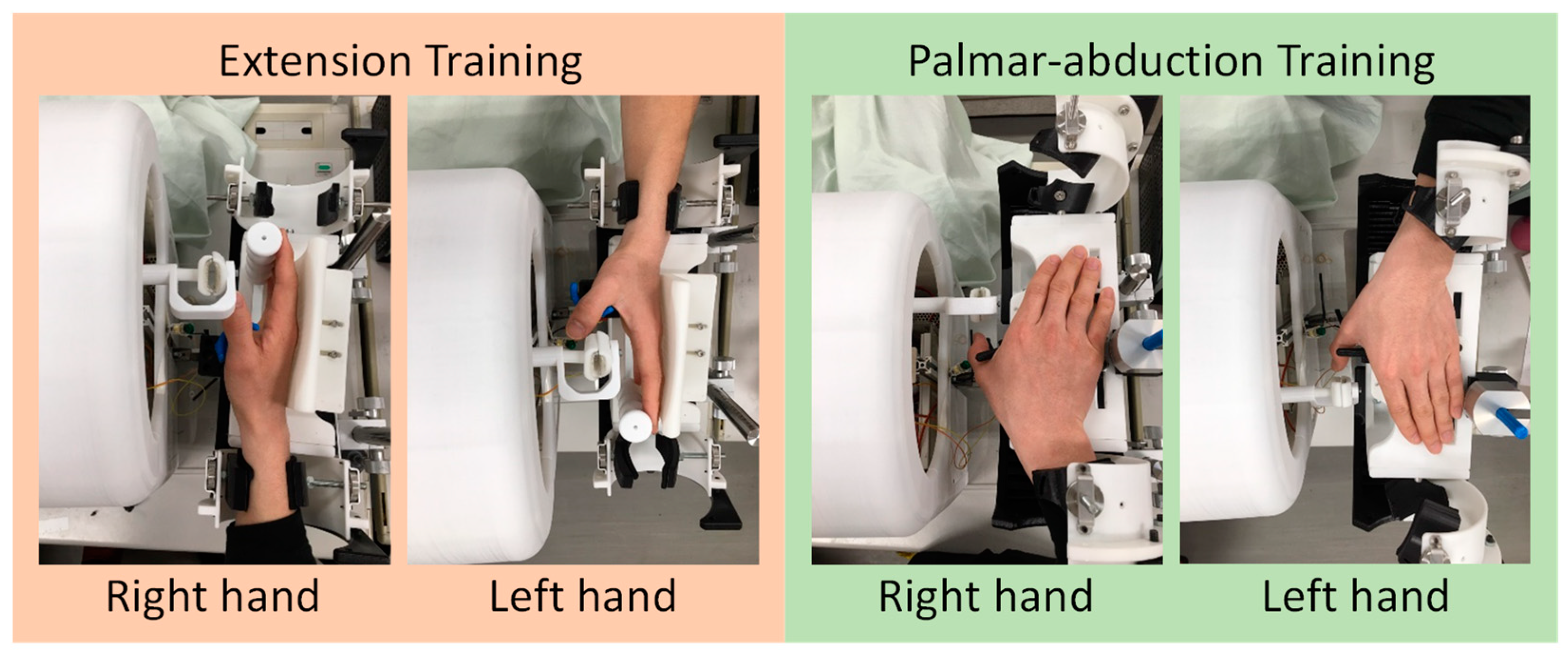
3.2. Proposed Device
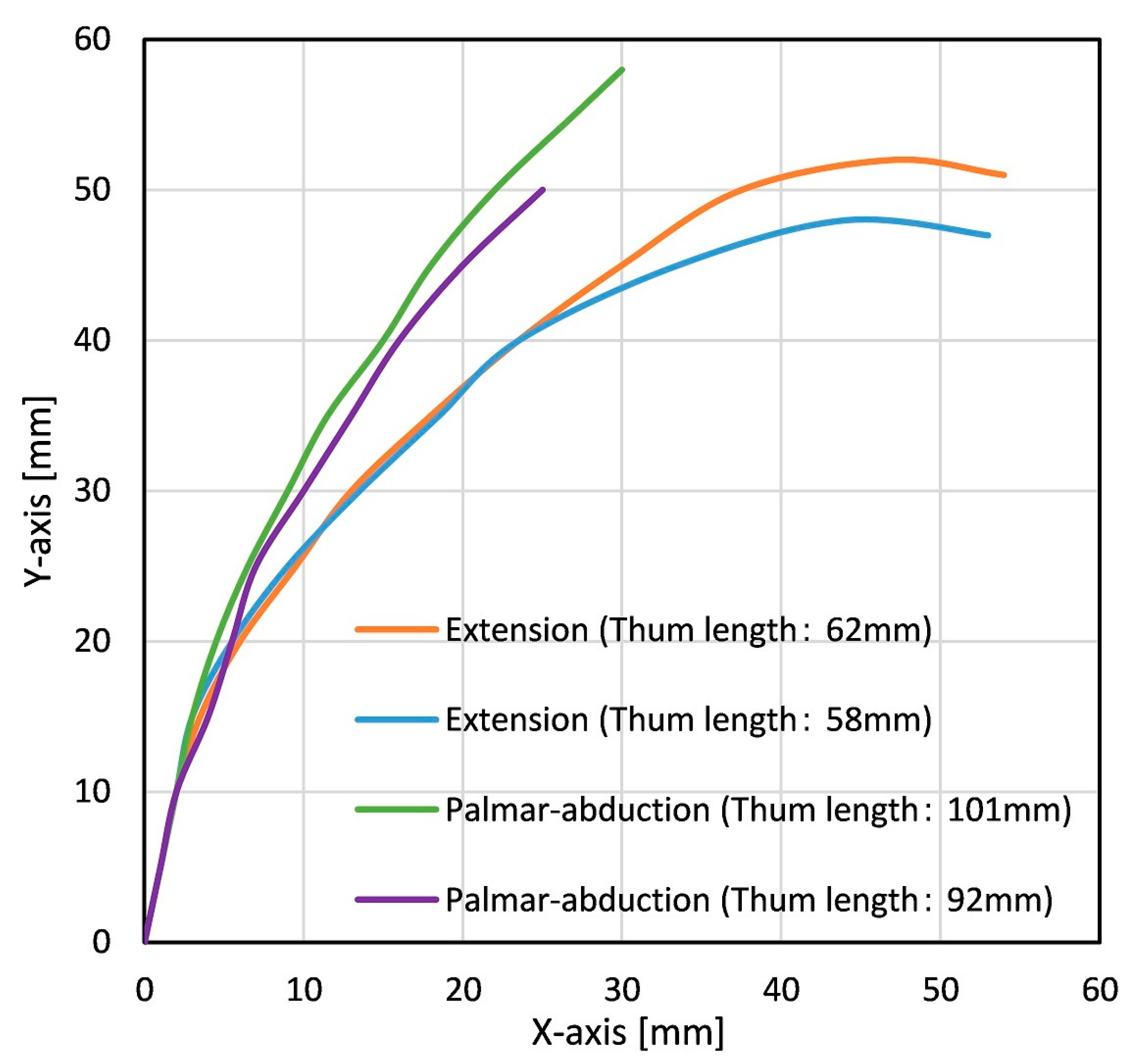
3.3. Trajectory of Thumb
3.4. Driving Mechanism of Thumb Training
- The user places the palm vertically/horizontally on the table and aligns the rotary axis of the MP/CM joint with the rotary axis of the driving mechanism;
- The device bends the training thumb to its pre-measured maximum flexion/palmar adduction angle with the circular movement;
- After the training thumb finger reaches the maximum flexion/palmar adduction angle, the device performs extension/palmar abduction with the circular movement;
- The device performs extension/palmar abduction until the training thumb returns to its initial posture with the circular movement.
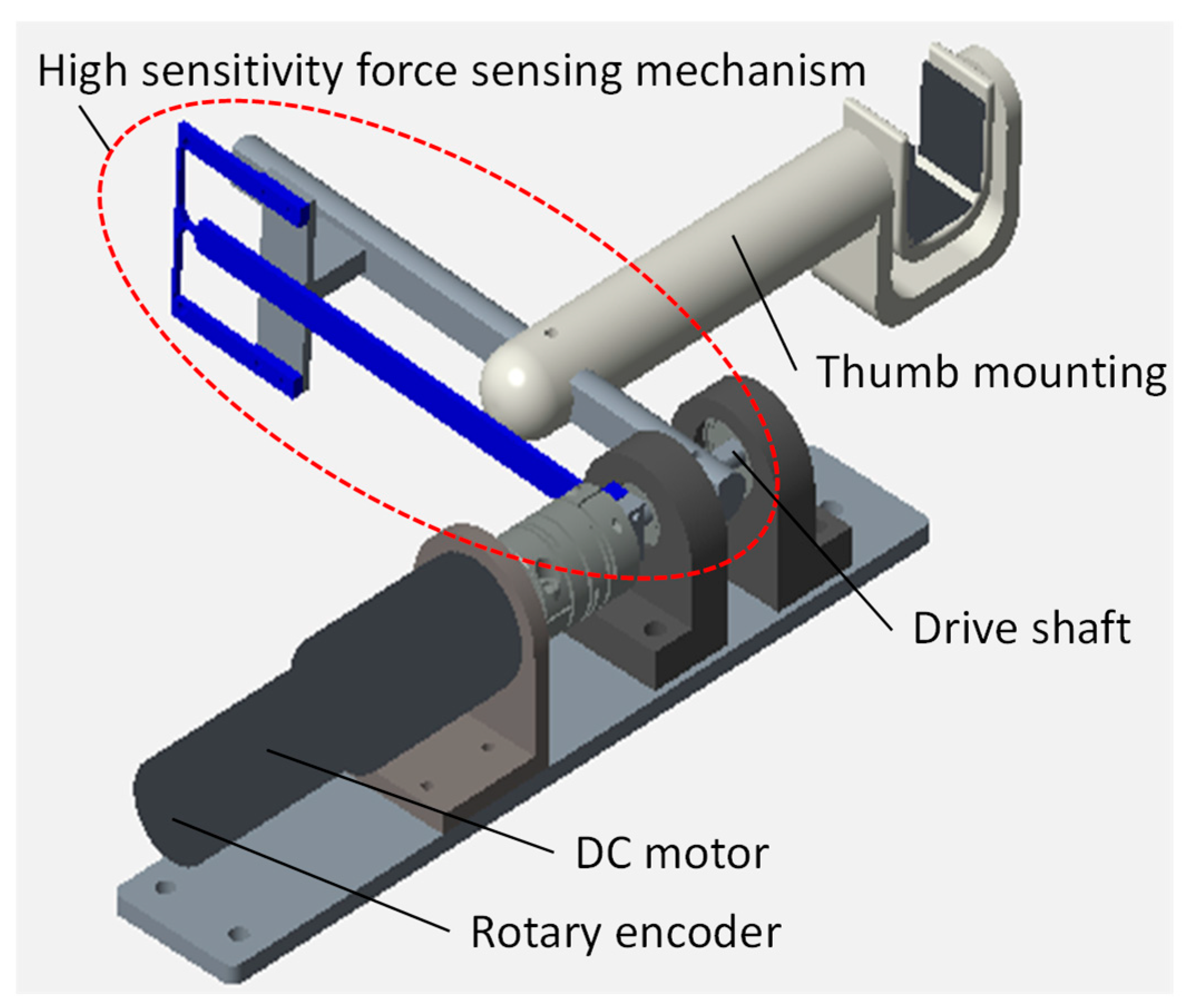
3.5. Thumb Operating Unit
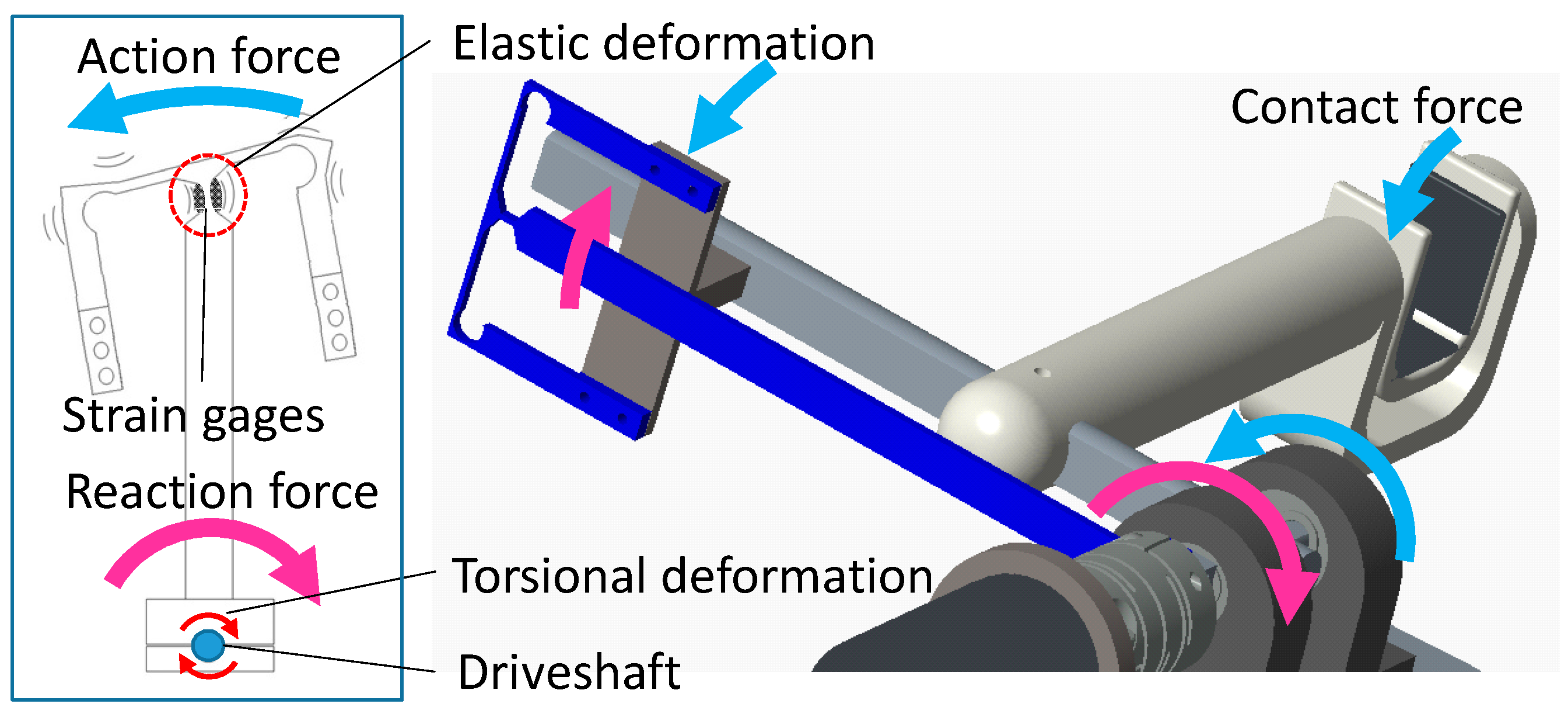
3.6. The High-Sensitivity Force-Sensing Mechanism
4. Control Method
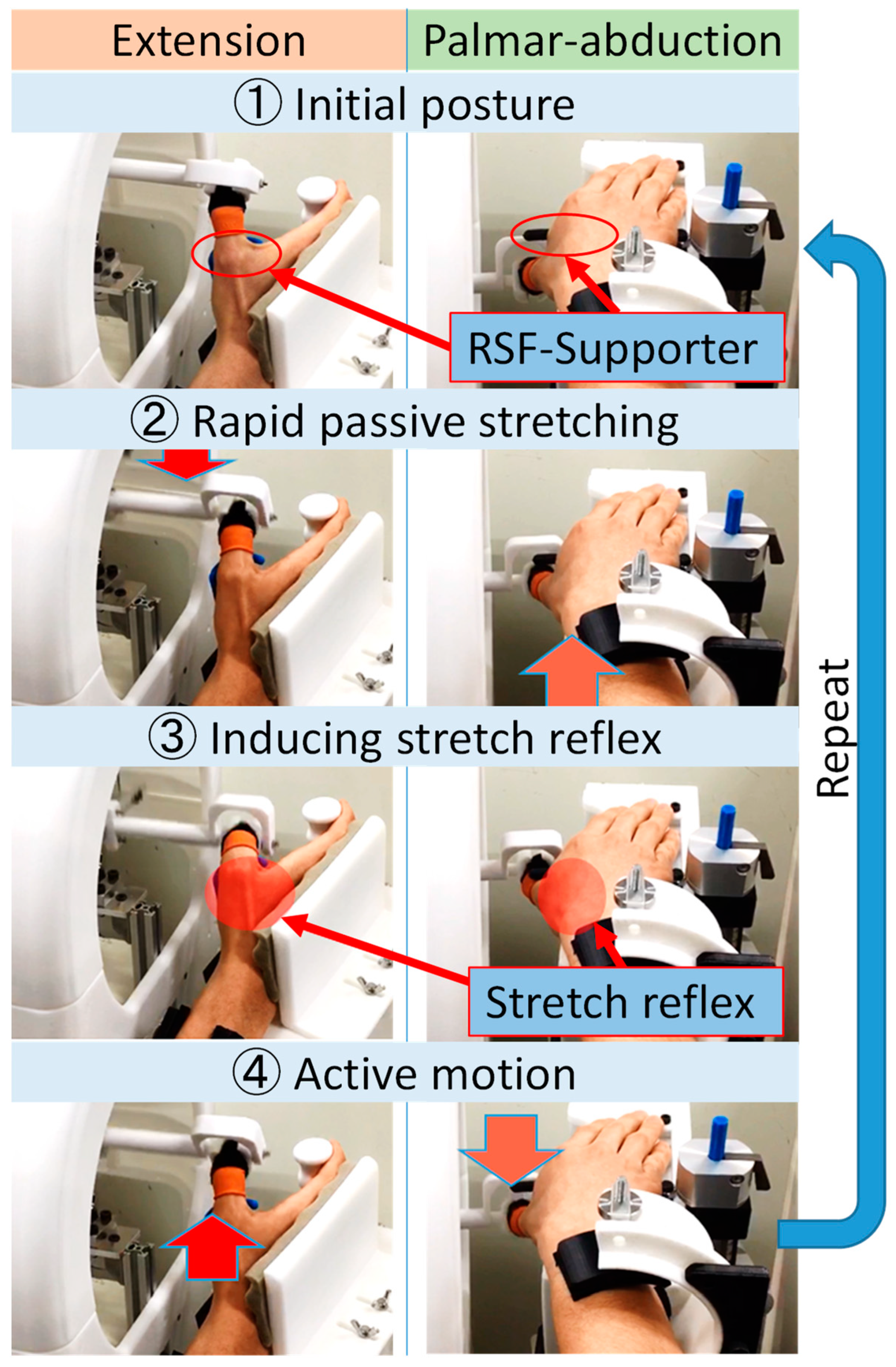
4.1. Training Method for Thumb Extension/Palmar Abduction Using Proposed Device
- The driving part of the fingertip of the device controls the flexion/palmar adduction of the thumb passively;
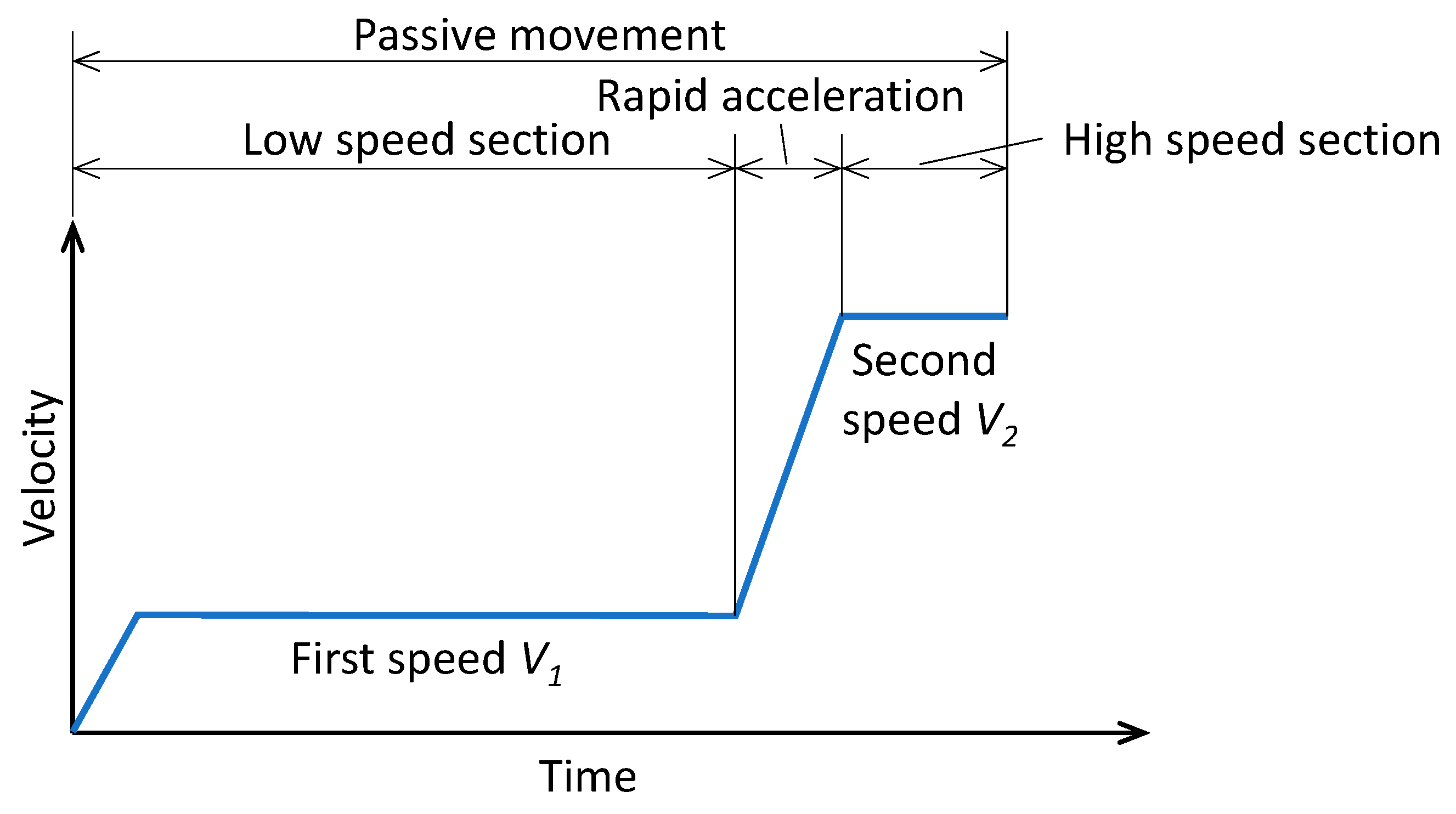
- The device accelerates flexion/palmar adduction before reaching the maximal position, increasing motion velocity from the first to the second speed (Figure 11);
- That acceleration facilitates the stretch reflex of the extensor muscle by supporting the MP joint/thumb root with RSF-Supporter at the same time as rapid passive flexion/adduction;
- Stretch reflex increases the excitement of the target nerve tract and facilitates voluntary active extension/palmar abduction. The device follows the active motion by measuring the intention of the active motion via the torque sensor. Moreover, the device performs extension/palmar abduction while giving slight resistance to that active motion before returning the initial posture so that the device provides kinesthesia and keeps the stretch reflex.
4.2. Proposal of Resistance-Accompanying Cooperation Control
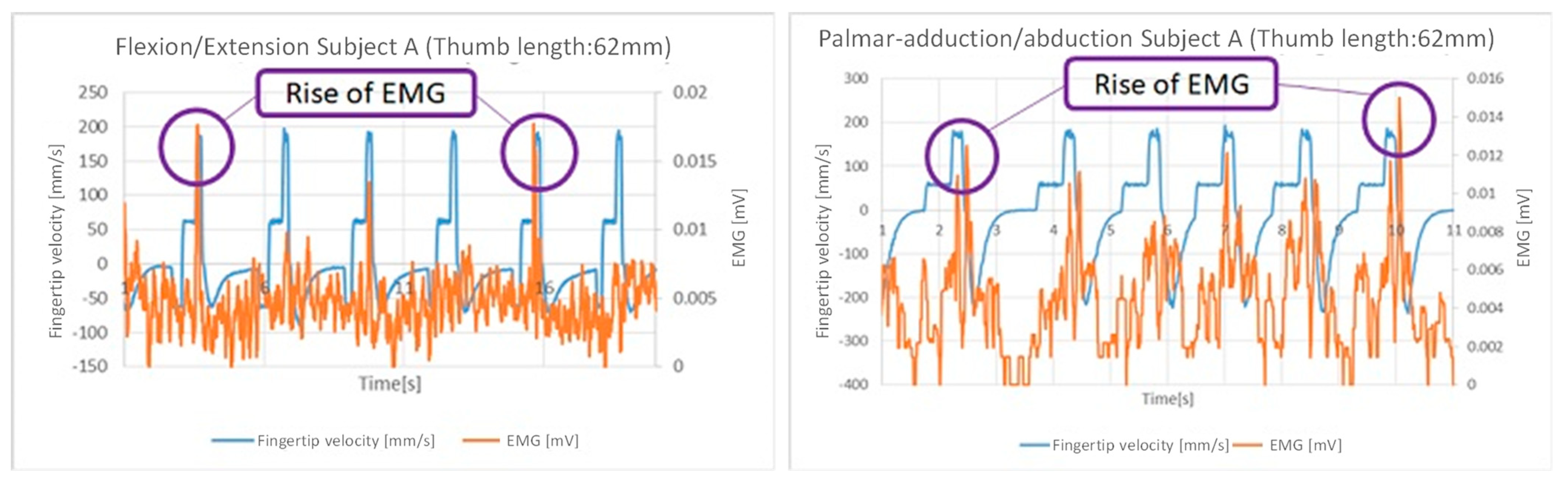
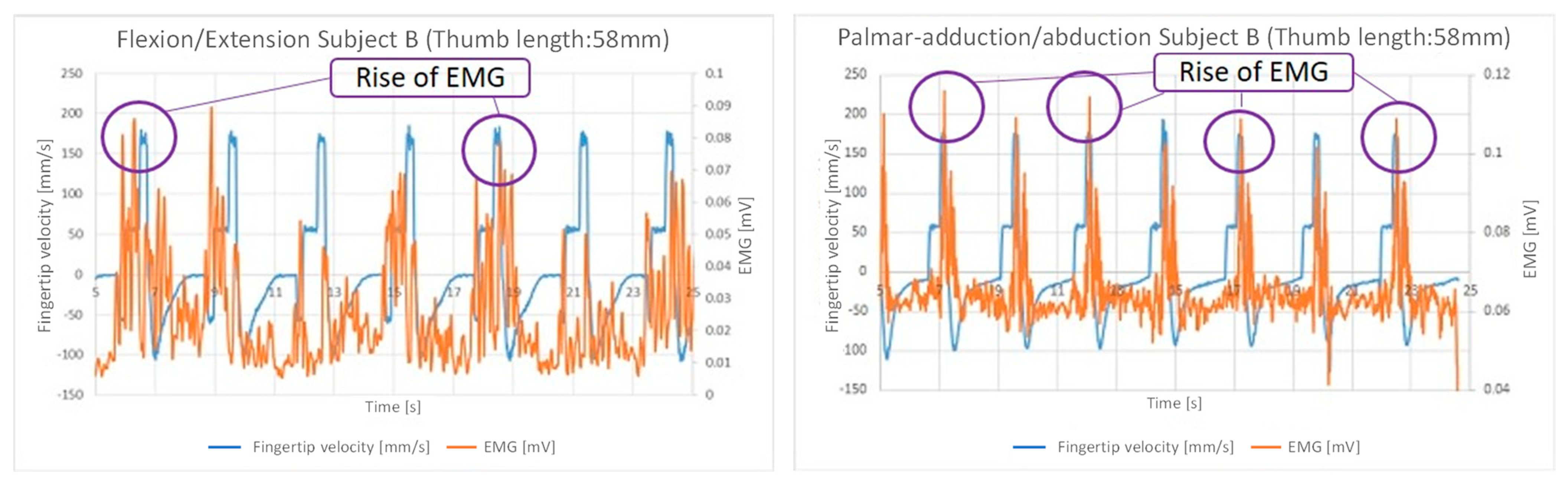
4.3. Tuning Control for the Stretch Reflex Time Lag
5. Verification of the Proposed Device
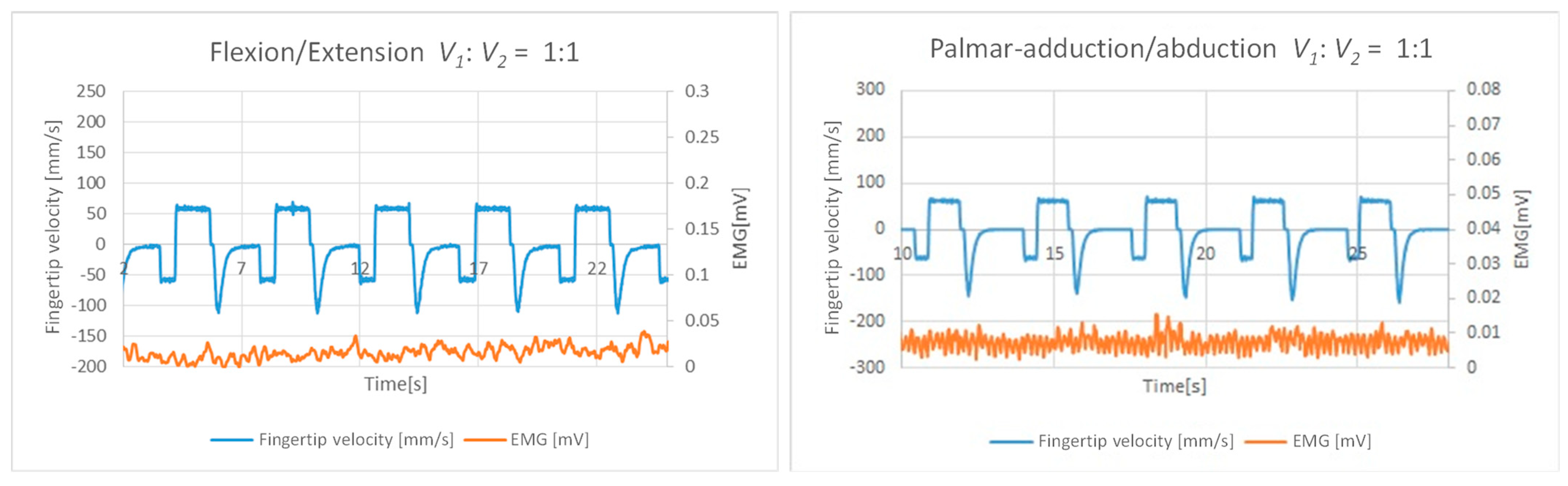
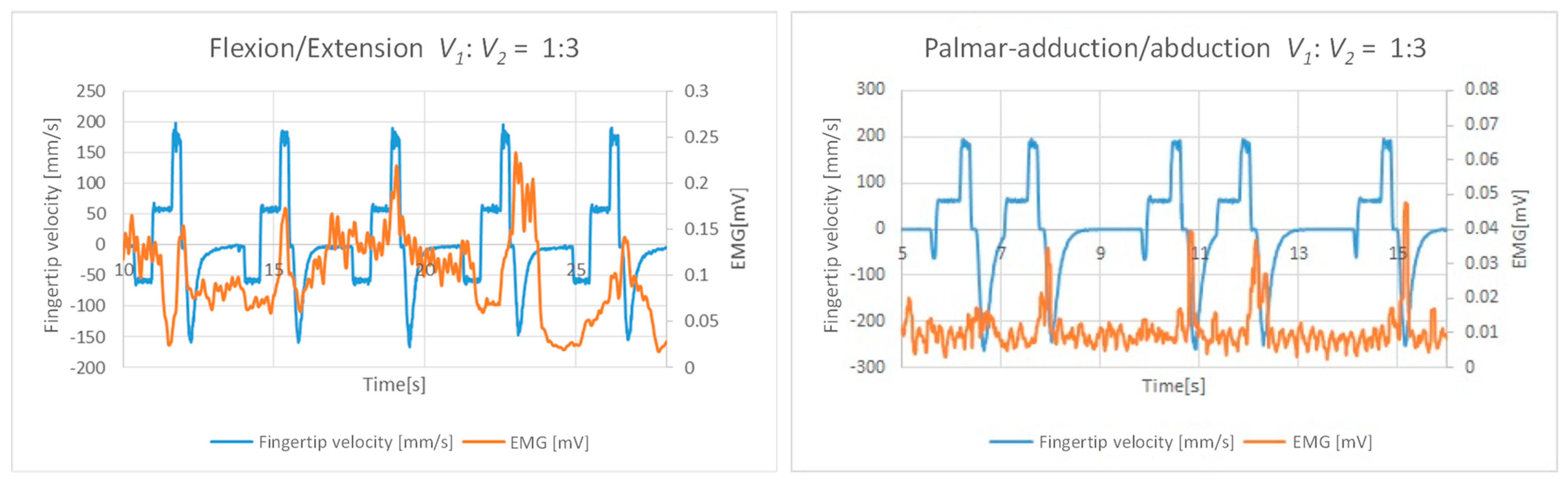
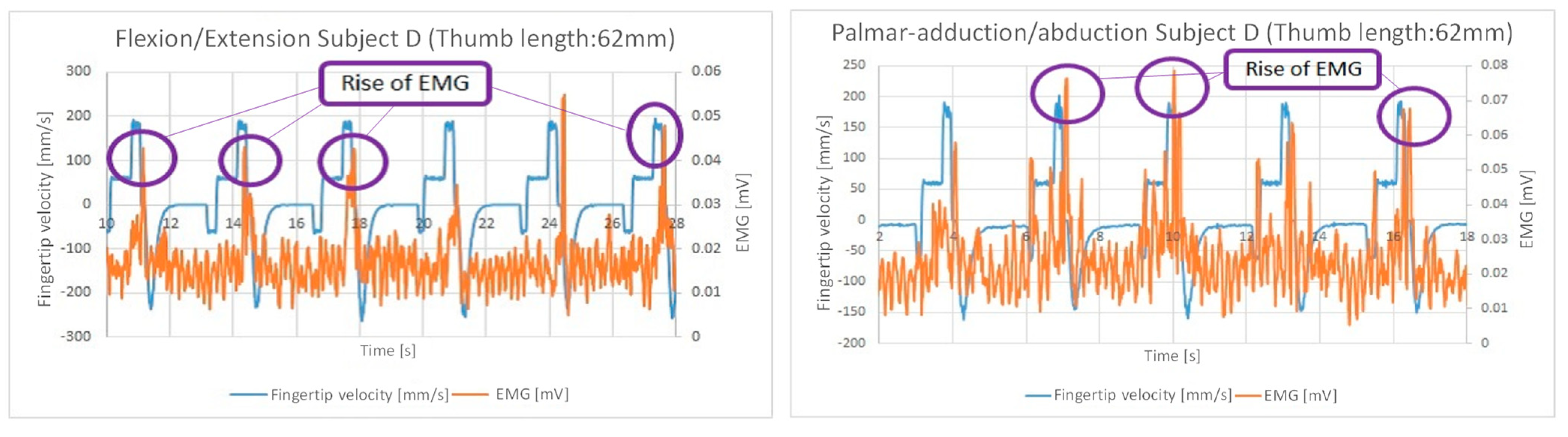
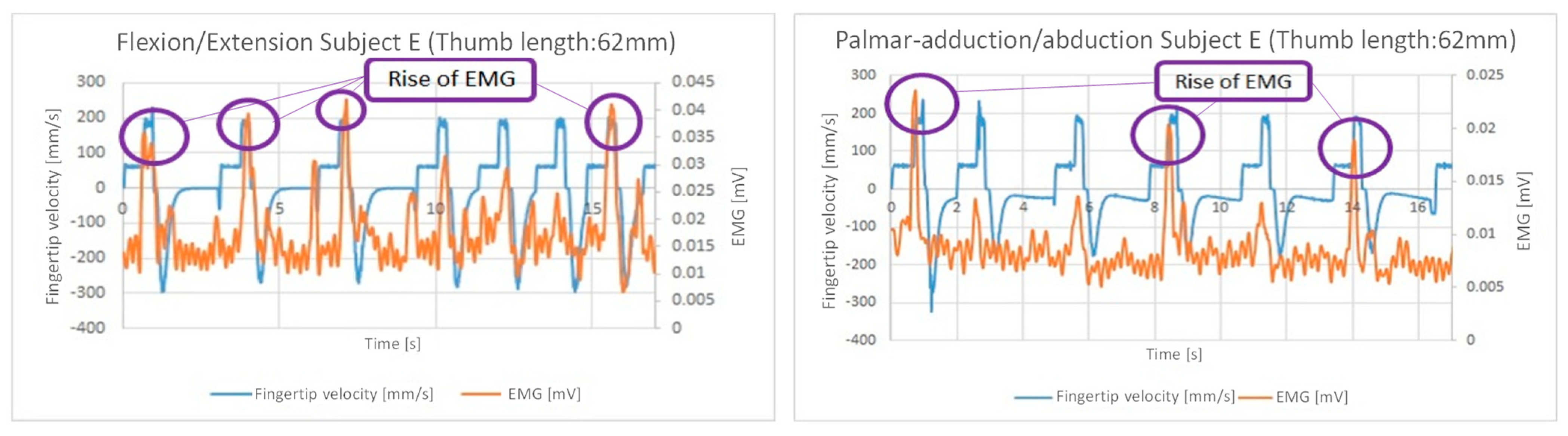
5.1. Verification of Relations of Fingertip Velocity and EMG
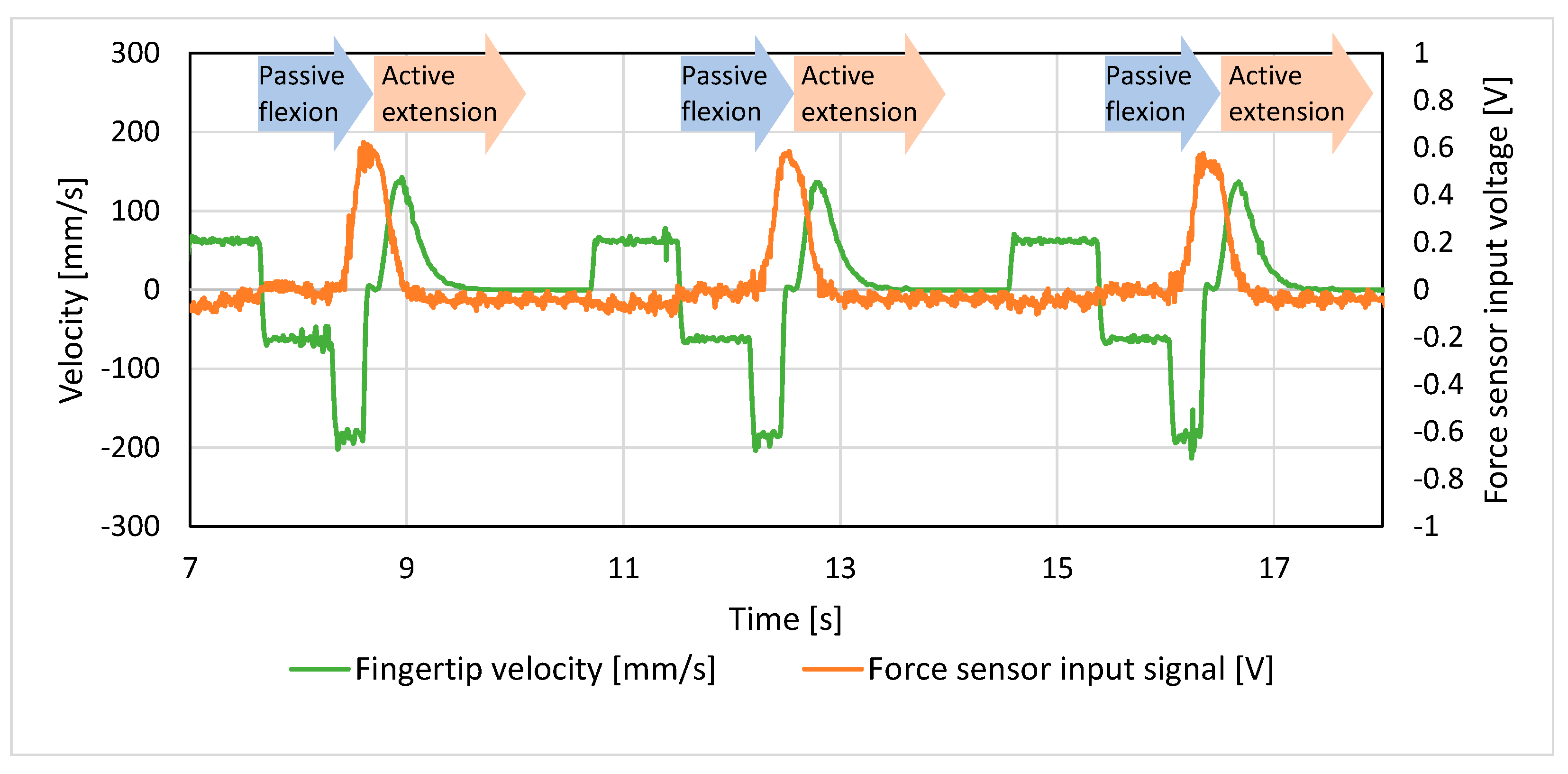
5.2. Verification of Stretch Reflex Induction Using the Proposed Device
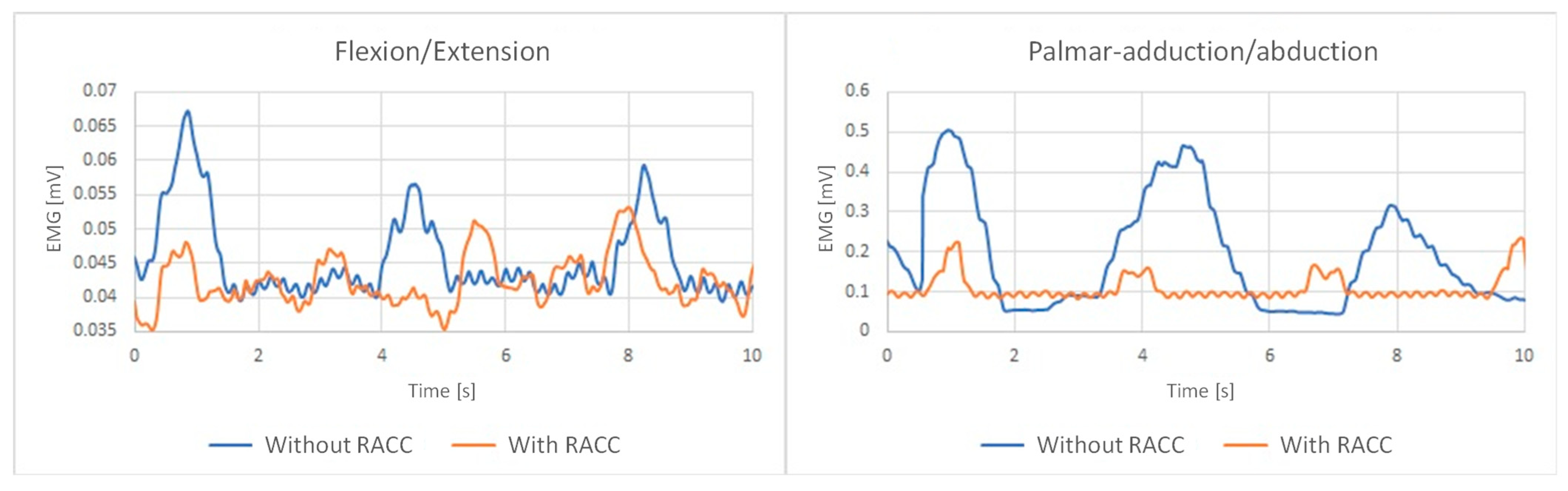
5.3. Verification of RACC Assistance
5.4. Verification Experiments of Thumb Extension/Palmar Abduction Training
6. Conclusions
7. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Stroke, Cerebrovascular Accident. 2024. Available online: https://www.emro.who.int/health-topics/stroke-cerebrovascular-accident/index.html (accessed on 18 June 2024).
- Kapandji, I.A.; Owerko, C.; Anderson, A. The Physiology of the Joints—Volume 1: The Upper Limb, 5th ed.; Churchill Livingstone: London, UK, 1982; pp. 251–290. [Google Scholar]
- Rahman, M.A.; Al-Jumaily, A. Design and Development of a Hand Exoskeleton for Rehabilitation Following Stroke. Procedia Eng. 2012, 41, 1028–1034. [Google Scholar] [CrossRef]
- Xiong, J.; Muraki, S. An ergonomics study of thumb movements on smartphone touch screen. Ergonomics 2014, 57, 943–955. [Google Scholar] [CrossRef] [PubMed]
- Kawahira, K.; Shimodozono, M.; Etoh, S.; Kamada, K.; Noma, T.; Tanaka, N. Effects of Intensive Repetition of a New Facilitation Technique on Motor Functional Recovery of the Hemiplegic Upper Limb and Hand. Brain Inj. 2010, 24, 1202–1213. [Google Scholar] [CrossRef] [PubMed]
- Kawahira, K.; Shimodozono, M.; Ogata, A.; Tanaka, N. Addition of Intensive Repetition of Facilitation Exercise to Multidisciplinary Rehabilitation Promotes Motor Functional Recovery of the Hemiplegic Lower Limb. J. Rehabil. Med. 2004, 36, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Kawahira, K.; Noma, T.; Iiyama, J.; Etoh, S.; Ogata, A.; Shimodozono, M. Improvements in Limb Kinetic Apraxia by Repetition of a Newly Designed Facilitation Exercise in a Patient with Corticobasal Degeneration. Int. J. Rehabil. Res. 2009, 32, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Shimodozono, M.; Noma, T.; Nomoto, Y.; Hisamatsu, N.; Kamada, K.; Miyata, R.; Matsumoto, S.; Ogata, A.; Etoh, S.; Basford, J.R.; et al. Benefits of a Repetitive Facilitative Exercise Program for the Upper Paretic Extremity after Subacute Stroke: A Randomized Controlled Trial. Neurorehabilit. Neural Repair 2013, 27, 296–305. [Google Scholar] [CrossRef] [PubMed]
- Yue, Z.; Zhang, X.; Wang, J. Hand Rehabilitation Robotics on Poststroke Motor Recovery. Behav. Neurol. 2017, 2017, 3908135. [Google Scholar] [CrossRef]
- Murakami, Y.; Honaga, K.; Kono, H.; Haruyama, K.; Yamaguchi, T.; Tani, M.; Isayama, R.; Takakura, T.; Tanuma, A.; Hatori, K.; et al. New Artificial Intelligence-Integrated Electromyography-Driven Robot Hand for Upper Extremity Rehabilitation of Patients With Stroke: A Randomized, Controlled Trial. Neurorehabilit. Neural Repair 2023, 37, 298–306. [Google Scholar] [CrossRef] [PubMed]
- Schabowsky, C.N.; Godfrey, S.B.; Holley, R.J.; Lum, P.S. Development and pilot testing of HEXORR: Hand EXOskeleton Rehabilitation Robot. J. NeuroEng. Rehabil. 2010, 7, 36. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Iwashita, H.; Kawahira, K.; Hayashi, R. Development of Functional Recovery Training Device for Hemiplegic Fingers with Finger-expansion Facilitation Exercise by Stretch Reflex. Trans. Soc. Instrum. Control Eng. 2012, 48, 413–422. [Google Scholar] [CrossRef]
- Yu, Y.; Iwashita, H.; Kawahira, K.; Hayashi, R. Development of Rehabilitation Device for Hemiplegic Fingers by Finger-Expansion Facilitation Exercise with Stretch Reflex. In Proceedings of the 2013 IEEE International Conference on Robotics and Biomimetics, Shenzhen, China, 12–14 December 2013; pp. 1317–1323. [Google Scholar]
- Yu, Y.; Tanda, Y.; Kimoto, Y.; Taniguchi, K.; Kawahira, K.; Shimodozono, M. Research on Hemiplegic Thumb Rehabilitation Device Using Repetitive Stimulus by Rapid Accelerative Facilitation. In Proceedings of the 23th Robotics Symposia, Shizuoka, Japan, 14–15 March 2018; pp. 172–175. (In Japanese). [Google Scholar]
- Kawahira, K.; Shimodozono, M.; Noma, T. Exercise Therapy for Recovery from Hemiplegia: Theory and Practice of Repetitive Facilitative Exercise; Springer Nature: Singapore, 2022; pp. 3–46. [Google Scholar]
- Yu, Y.; Nakanishi, Y.; Kawahira, K.; Shimodozono, M.; Hayashi, R. Production of effective stretch reflex by a pronation and supination function recovery training device for hemiplegic forearms. In Proceedings of the 2015 IEEE International Conference on Robotics and Biomimetics (ROBIO2015), Zhuhai, China, 6–9 December 2015; pp. 150–157. [Google Scholar]
- Yu, Y.; Kodama, M.; Matsuwaki, H.; Matsumoto, S.; Taniguchi, K.; Yamanaka, H.; Fukuda, I.; Shimodozono, M.; Kawahira, K. Development of Functional Recovery Training Device for Hemiplegic Knee Flexion Based on Repetitive Facilitation Exercise. J. Robot. Soc. Jpn. 2017, 35, 239–248. (In Japanese) [Google Scholar] [CrossRef]
- Yu, Y.; Ishitsuka, T.; Tsujio, S. Torque Sensing of Finger Joint Using Strain-Deformation Expansion Mechanism. J. Robot. Soc. Jpn. 2002, 20, 526–538. [Google Scholar] [CrossRef]
- Yu, Y.; Kodama, M.; Matsuwaki, H.; Taniguchi, K.; Matsumoto, S.; Yamanaka, H.; Fukuda, I.; Shimodozono, M.; Kawahira, K. Research of Rehabilitation Device for Hemiplegic Knee Flexion Based on Repetitive Facilitation Exercise. Intell. Robot. Appl. 2016, 9835, 158–167. [Google Scholar]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taniguchi, K.; Tanda, Y.; Yu, Y. Proposal for Hemiplegic Thumb Rehabilitation Device Based on Repetitive Facilitation Exercise. Machines 2024, 12, 920. https://doi.org/10.3390/machines12120920
Taniguchi K, Tanda Y, Yu Y. Proposal for Hemiplegic Thumb Rehabilitation Device Based on Repetitive Facilitation Exercise. Machines. 2024; 12(12):920. https://doi.org/10.3390/machines12120920
Chicago/Turabian StyleTaniguchi, Koutaro, Yuta Tanda, and Yong Yu. 2024. "Proposal for Hemiplegic Thumb Rehabilitation Device Based on Repetitive Facilitation Exercise" Machines 12, no. 12: 920. https://doi.org/10.3390/machines12120920
APA StyleTaniguchi, K., Tanda, Y., & Yu, Y. (2024). Proposal for Hemiplegic Thumb Rehabilitation Device Based on Repetitive Facilitation Exercise. Machines, 12(12), 920. https://doi.org/10.3390/machines12120920





