A Perspective on Rehabilitation Through Open-Source Low-Cost 3D-Printed Distal to the Wrist Joint Transitional Prosthetics: Towards Autonomous Hybrid Devices
Abstract
1. Introduction
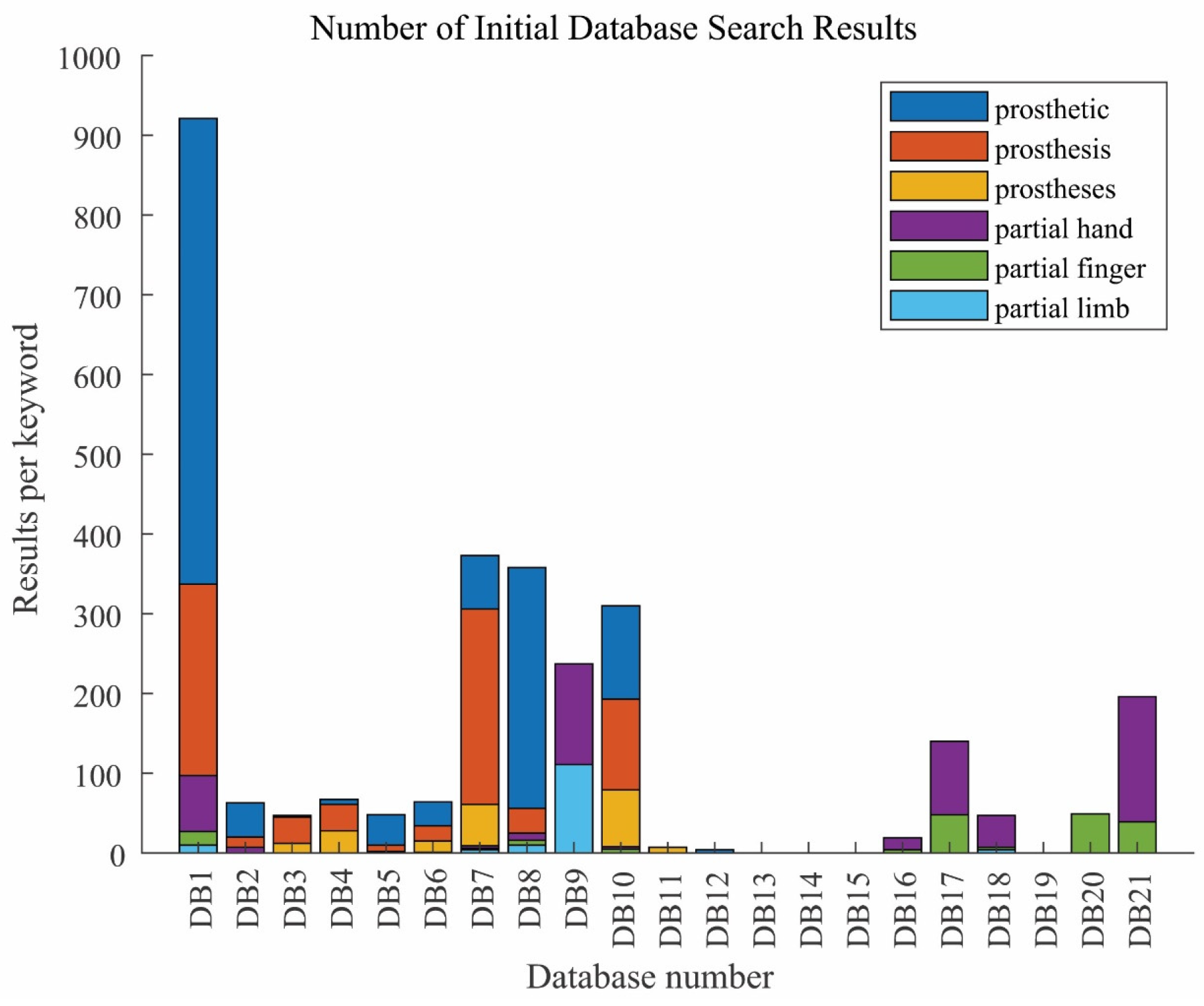
2. Methodology
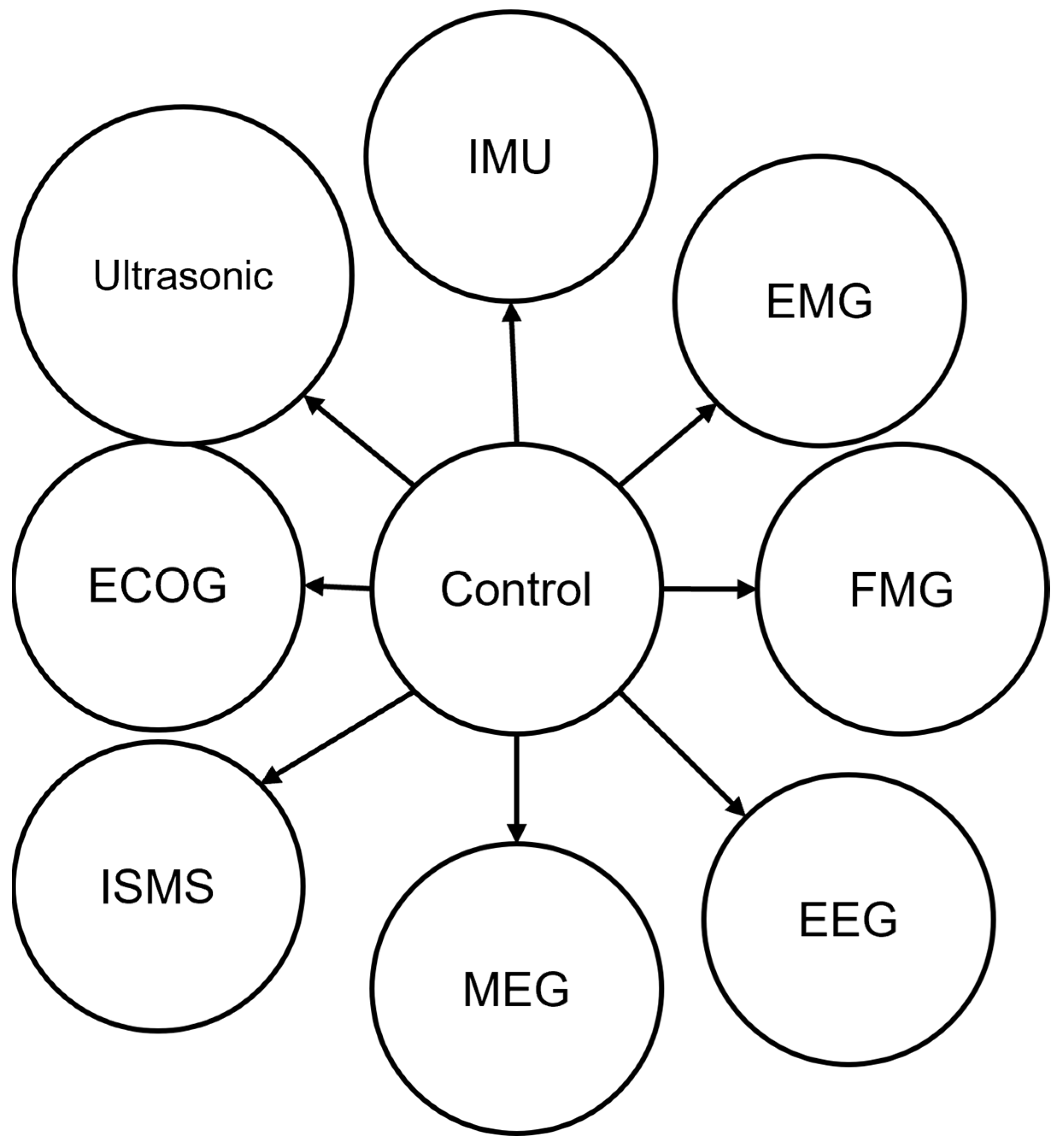
3. Control and Signal Processing Algorithms
3.1. IMU
3.2. EMG
3.3. EEG
3.4. FMG
3.5. MEG
3.6. ISMS
3.7. ECOG
3.8. Ultrasonic
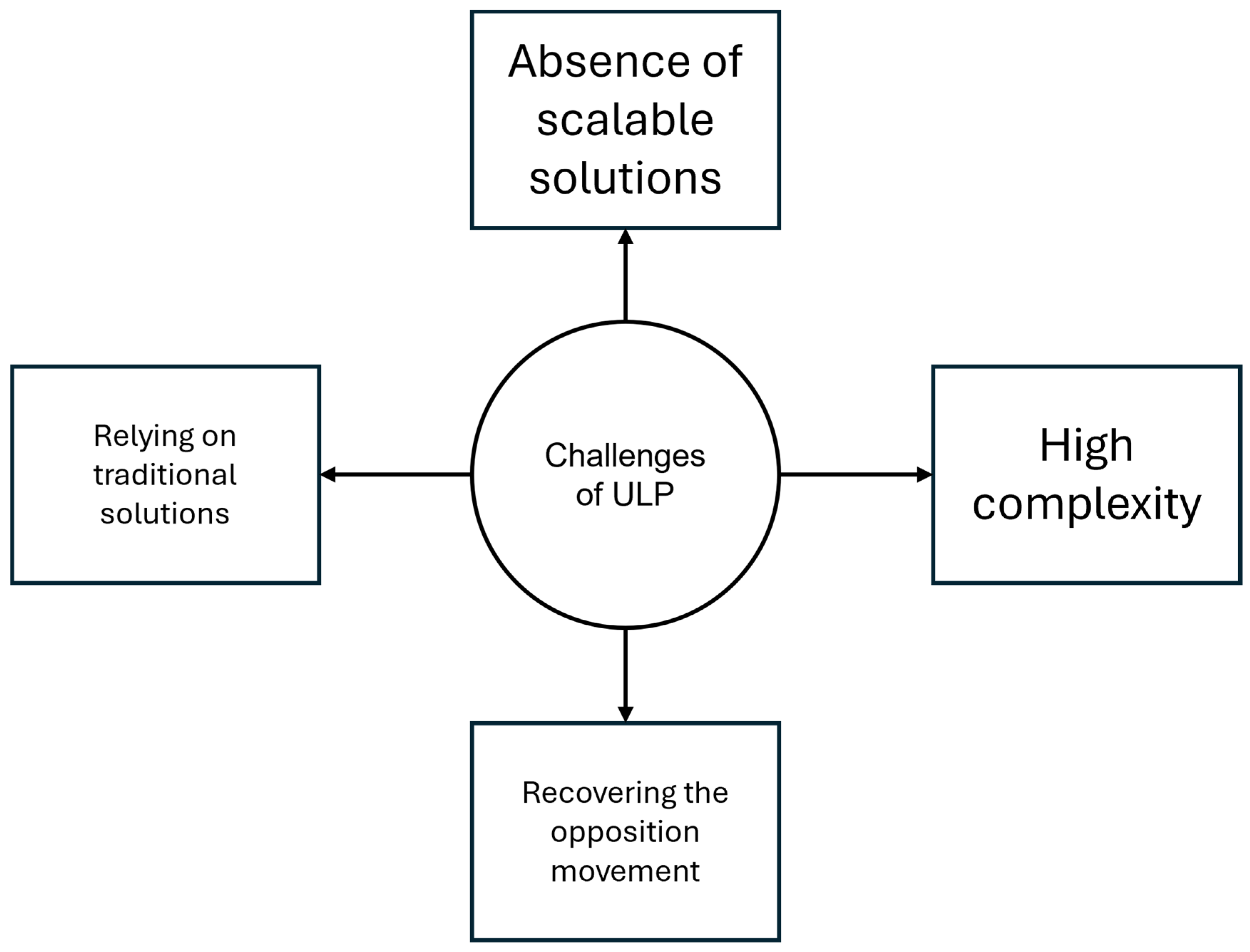
4. Functional Challenges of 3D-Printed Prosthetics
5. Rehabilitation of Partial Hand Reduction
6. Surgical Intervention for Optimal Prosthetic Embodiment
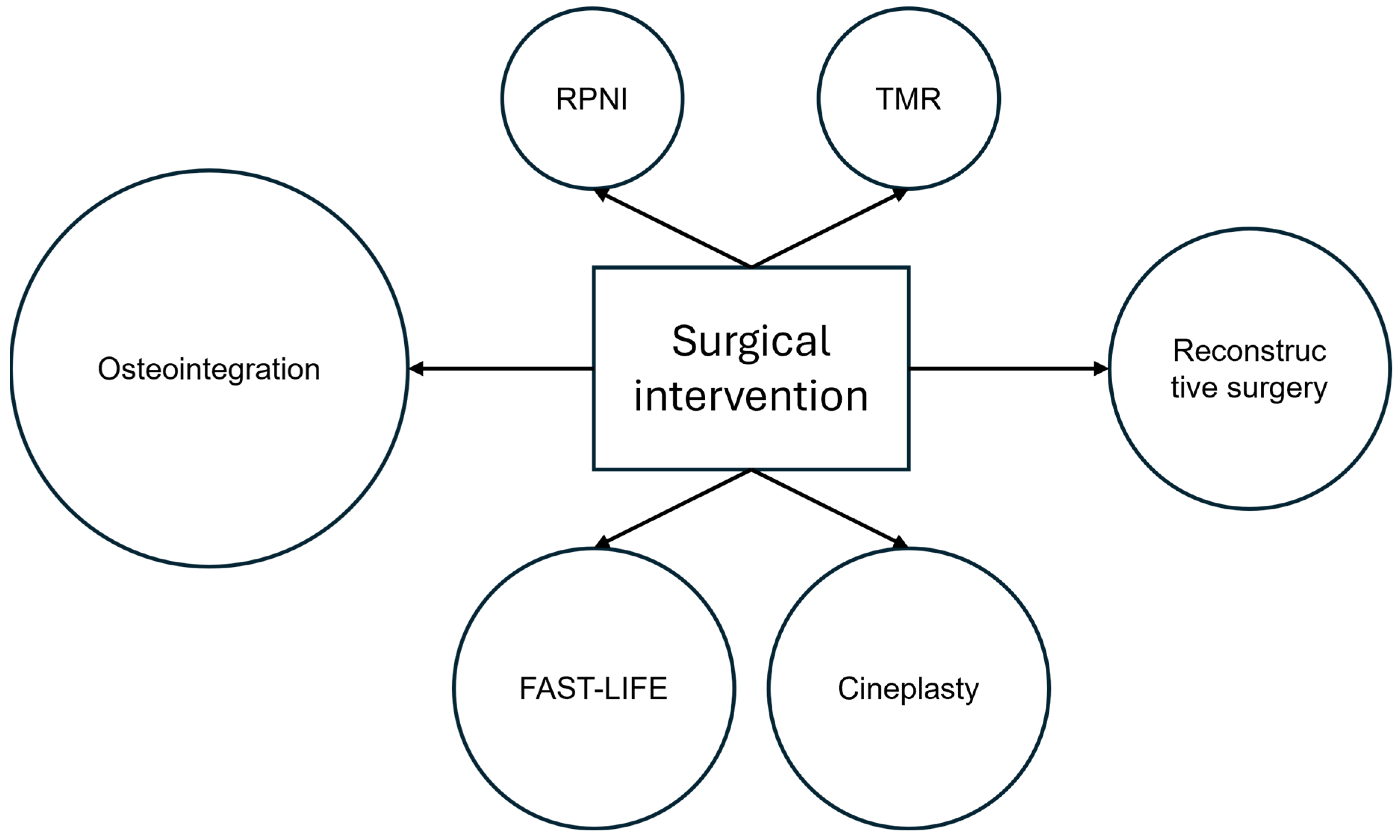
7. Proprioceptive Feedback Enhancements
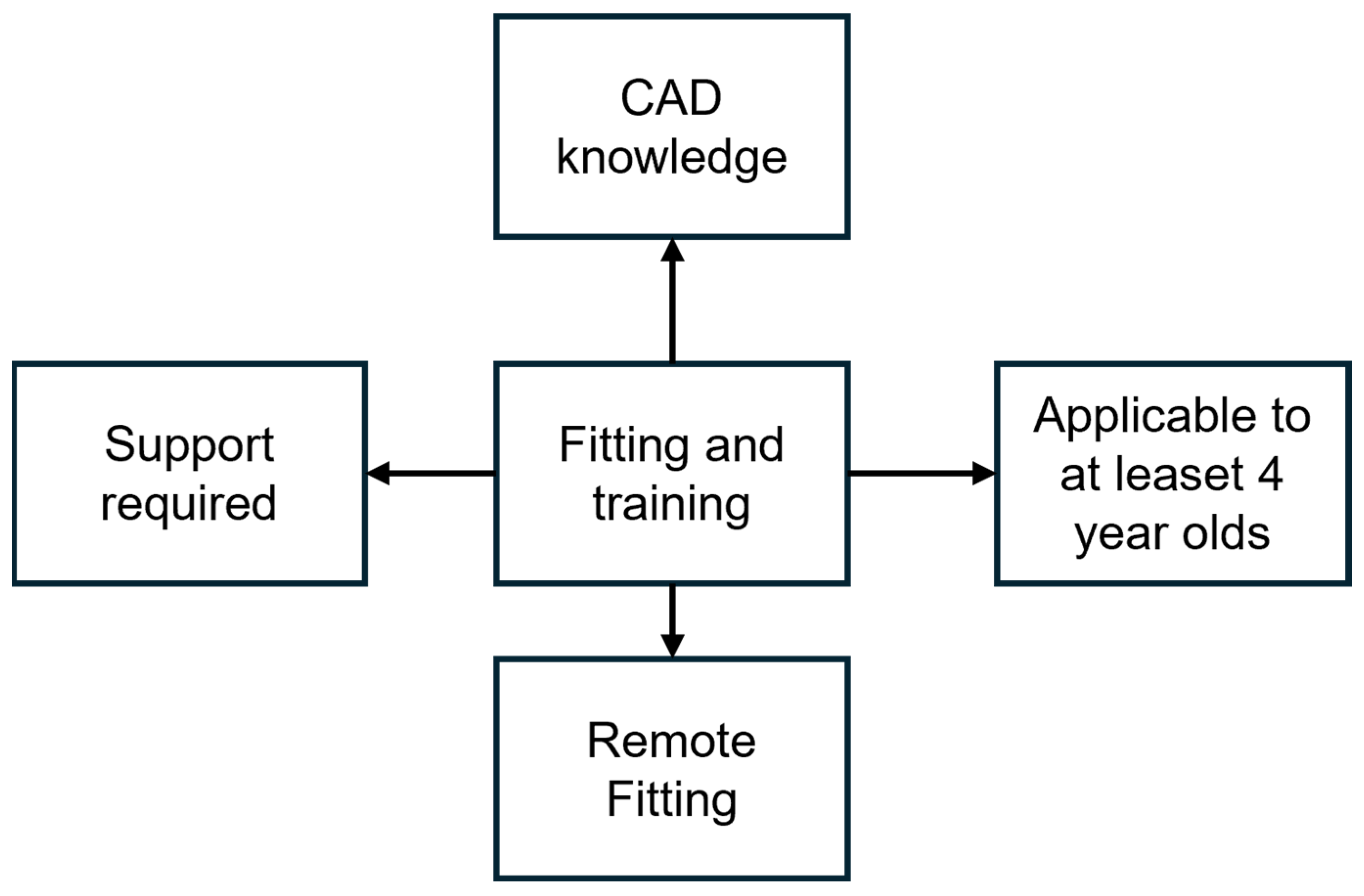
8. Initial Fitting and Training
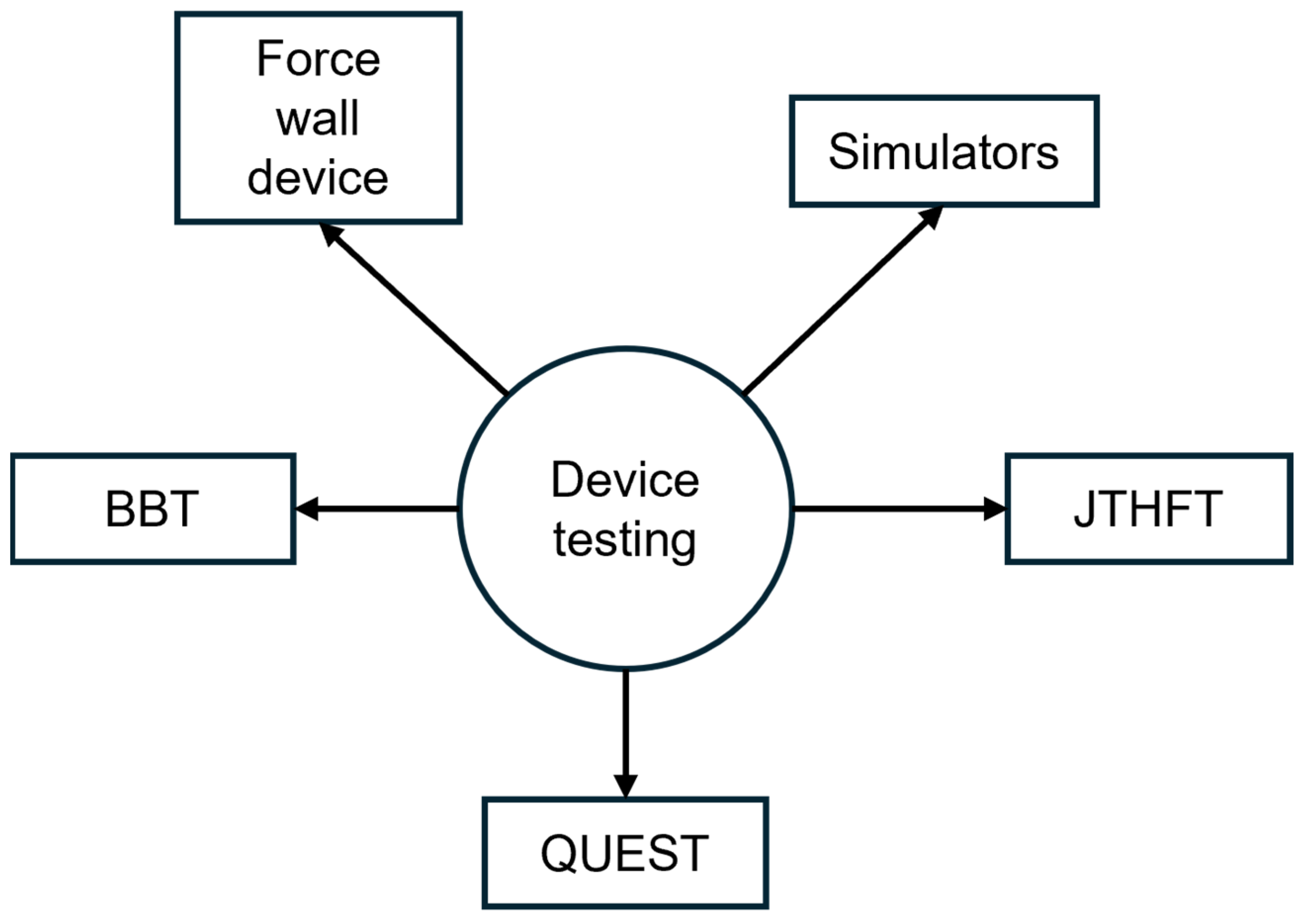
9. Device Testing
10. Implementation of FFF 3D Printing Technology
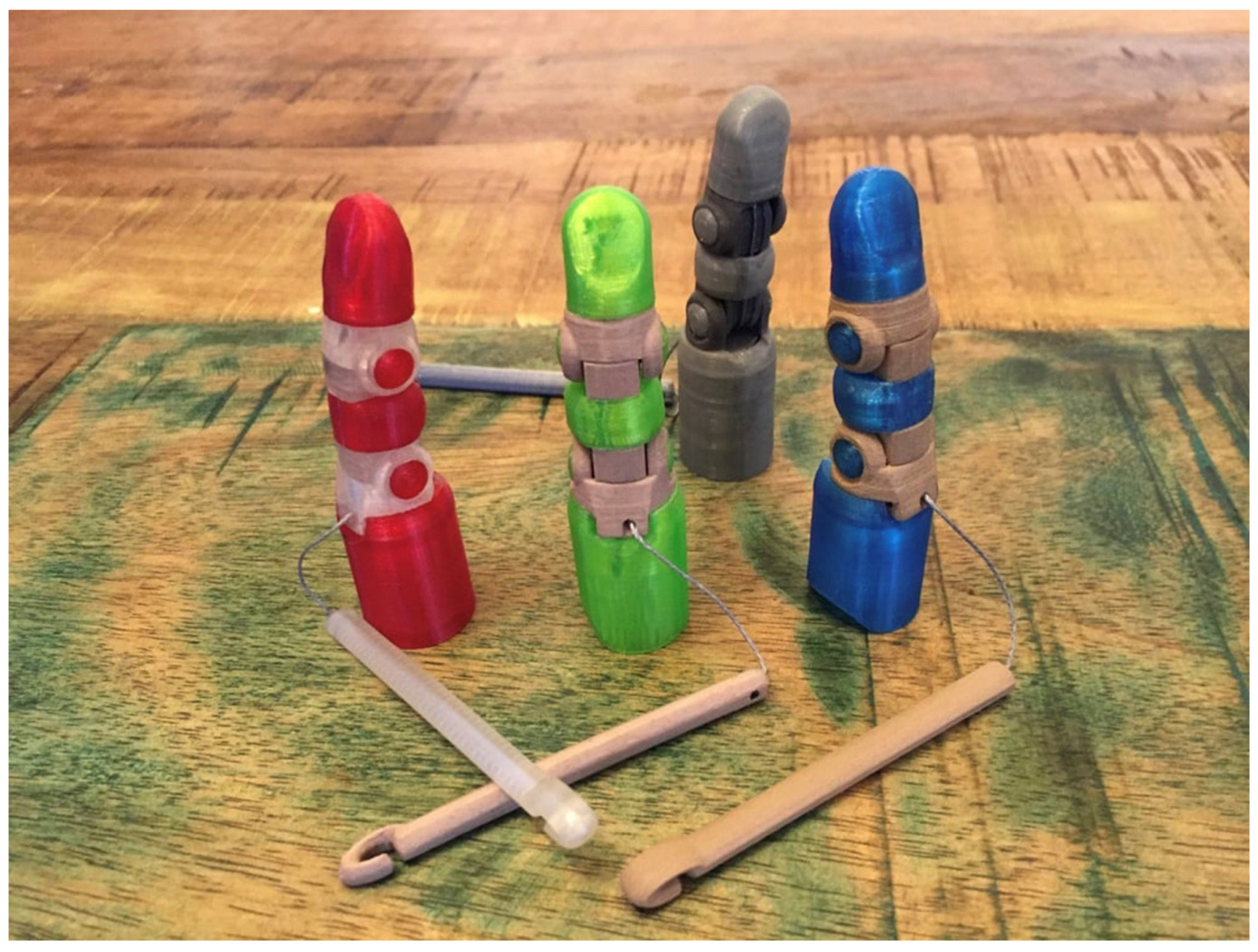
11. Device Additive Manufacturing
12. Paediatric Prosthetics
13. Future Development
14. Results
15. Discussion
15.1. Finger Prosthetics
15.2. Partial Hand Prosthetic with All Fingers Amputated
15.3. Partial Hand Prosthetic with Weak Wrist
15.4. Paediatric Partial Hand Prosthetic
- -
- Developing other means of performance comparisons between prosthetics that may lead to a unified testing procedure for medical devices. Although some criteria have been proposed by this work and others, there is still a need for further development.
- -
- Multidisciplinary teams in clinical studies may unite to give a prescription prosthetic based on both open source and commercial solutions while thinking about both engineering and medical effects on the patient’s wellbeing, including both surgeons and prosthetists, as well as biomedical engineers in the discussion may lead to better outcomes.
- -
- A procedure to filter or certify platforms to provide medical equipment should be considered. This may provide patients with files and instructions but under the guidance and supervision of a specialist.
- -
- Technology development in the field of additive manufacturing may open new capabilities for healing of patients with trauma and helping them adapt to their new situation. The 4D printing process is promising to revolutionize the field of manufacturing once again. The medical applications are still under development but have promising results.
- -
- Proprioceptive feedback techniques development may lead to a better handling of prosthetic devices in the future. Better control will also mean more people will be able to use a prosthetic. Nowadays, there are problems with device abandonment due to poor control strategies that cause frustration.
16. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Graham, E.M.; Hendrycks, R.; Baschuk, C.M.; Atkins, D.J.; Keizer, L.; Duncan, C.C.; Mendenhall, S.D. Restoring Form and Function to the Partial Hand Amputee: Prosthetic Options from the Fingertip to the Palm. Hand Clin. 2021, 37, 167–187. [Google Scholar] [CrossRef] [PubMed]
- Manero, A.; Smith, P.; Sparkman, J.; Dombrowski, M.; Courbin, D.; Kester, A.; Womack, I.; Chi, A. Implementation of 3D Printing Technology in the Field of Prosthetics: Past, Present, and Future. Int. J. Environ. Res. Public Health 2019, 16, 1641. [Google Scholar] [CrossRef] [PubMed]
- Kate, J.T.; Smit, G.; Breedveld, P. 3D-printed upper limb prostheses: A review. Disabil. Rehabil. Assist. Technol. 2017, 12, 300–314. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, K.S.; Lightdale-Miric, N. Advances in 3D-Printed Pediatric Prostheses for Upper Extremity Differences. J. Bone Jt. Surg. Am. 2016, 98, 1320–1326. [Google Scholar] [CrossRef]
- Rudd, G.; Daly, L.; Jovanovic, V.; Cuckov, F. A Low-Cost Soft Robotic Hand Exoskeleton for Use in Therapy of Limited Hand–Motor Function. Appl. Sci. 2019, 9, 3751. [Google Scholar] [CrossRef]
- Demofonti, A.; Carpino, G.; Zollo, L.; Johnson, M.J. Affordable Robotics for Upper Limb Stroke Rehabilitation in Developing Countries: A Systematic Review. IEEE Trans. Med. Robot. Bionics 2021, 3, 11–20. [Google Scholar] [CrossRef]
- Francoisse, C.A.; Sescleifer, A.M.; King, W.T.; Lin, A.Y. Three-dimensional printing in medicine: A systematic review of pediatric applications. Pediatr. Res. 2021, 89, 415–425. [Google Scholar] [CrossRef]
- Vujaklija, I.; Farina, D. 3D printed upper limb prosthetics. Expert Rev. Med. Devices 2018, 15, 505–512. [Google Scholar] [CrossRef]
- Maroti, P.; Varga, P.; Abraham, H.; Falk, G.; Zsebe, T.; Meiszterics, Z.; Mano, S.; Csernatony, Z.; Rendeki, S.; Nyitrai, M. Printing orientation defines anisotropic mechanical properties in additive manufacturing of upper limb prosthetics. Mater. Res. Express 2018, 6, 035403. [Google Scholar] [CrossRef]
- Baethge, C.; Goldbeck-Wood, S.; Mertens, S. SANRA—A scale for the quality assessment of narrative review articles. Res. Integr. Peer Rev. 2019, 4, 5. [Google Scholar] [CrossRef]
- Rayna, T.; Striukova, L.; Darlington, J. Co-creation and user innovation: The role of online 3D printing platforms. J. Eng. Technol. Manag. 2015, 37, 90–102. [Google Scholar] [CrossRef]
- Wendo, K.; Barbier, O.; Bollen, X.; Schubert, T.; Lejeune, T.; Raucent, B.; Olszewski, R. Open-Source 3D Printing in the Prosthetic Field—The Case of Upper Limb Prostheses: A Review. Machines 2022, 10, 413. [Google Scholar] [CrossRef]
- Fonseca, L.; Bo, A.; Guiraud, D.; Navarro, B.; Gelis, A.; Azevedo-Coste, C. Investigating Upper Limb Movement Classification on Users with Tetraplegia as a Possible Neuroprosthesis Interface. In Proceedings of the 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Honolulu, HI, USA, 18–21 July 2018; pp. 5053–5056. [Google Scholar] [CrossRef]
- Ahmed, M.H.; Chai, J.; Shimoda, S.; Hayashibe, M. Synergy-Space Recurrent Neural Network for Transferable Forearm Motion Prediction from Residual Limb Motion. Sensors 2023, 23, 4188. [Google Scholar] [CrossRef] [PubMed]
- Rizzoglio, F.; Giordano, M.; Mussa-Ivaldi, F.A.; Casadio, M. A Non-Linear Body Machine Interface for Controlling Assistive Robotic Arms. IEEE Trans. Biomed. Eng. 2023, 70, 2149–2159. [Google Scholar] [CrossRef]
- Adewuyi, A.A.; Hargrove, L.J.; Kuiken, T.A. Evaluating EMG Feature and Classifier Selection for Application to Partial-Hand Prosthesis Control. Front. Neurorobotics 2016, 10, 15. Available online: https://www.frontiersin.org/articles/10.3389/fnbot.2016.00015 (accessed on 24 April 2023). [CrossRef]
- Zuleta, J.N.; Ferro, M.; Murillo, C.; Franco-Luna, R.A. Identification of EMG activity with machine learning in patients with amputation of upper limbs for the development of mechanical prostheses. IOP Conf. Ser. Mater. Sci. Eng. 2019, 519, 012010. [Google Scholar] [CrossRef]
- Menon, R.; Di Caterina, G.; Lakany, H.; Petropoulakis, L.; Conway, B.A.; Soraghan, J.J. Study on Interaction Between Temporal and Spatial Information in Classification of EMG Signals for Myoelectric Prostheses. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 1832–1842. [Google Scholar] [CrossRef]
- Earley, E.J.; Adewuyi, A.A.; Hargrove, L.J. Optimizing pattern recognition-based control for partial-hand prosthesis application. In Proceedings of the 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA, 26–30 August 2014; pp. 3574–3577. [Google Scholar] [CrossRef]
- Earley, E.J.; Hargrove, L.J.; Kuiken, T.A. Dual Window Pattern Recognition Classifier for Improved Partial-Hand Prosthesis Control. Front. Neurosci. 2016, 10, 58. Available online: https://www.frontiersin.org/articles/10.3389/fnins.2016.00058 (accessed on 30 June 2023). [CrossRef]
- Al-Timemy, A.H.; Bugmann, G.; Escudero, J. Adaptive Windowing Framework for Surface Electromyogram-Based Pattern Recognition System for Transradial Amputees. Sensors 2018, 18, 2402. [Google Scholar] [CrossRef]
- Adewuyi, A.A.; Hargrove, L.J.; Kuiken, T.A. Resolving the effect of wrist position on myoelectric pattern recognition control. J. NeuroEngineering Rehabil. 2017, 14, 39. [Google Scholar] [CrossRef]
- Beaulieu, R.J.; Masters, M.R.; Betthauser, J.B.; Smith, R.J.; Kaliki, R.; Thakor, N.V.; Soares, A.B. Multi-Position Training Improves Robustness of Pattern Recognition and Reduces Limb-Position Effect in Prosthetic Control. JPO J. Prosthet. Orthot. 2017, 29, 54. [Google Scholar] [CrossRef] [PubMed]
- Earley, E.J.; Hargrove, L.J. The effect of wrist position and hand-grasp pattern on virtual prosthesis task performance. In Proceedings of the 2016 6th IEEE International Conference on Biomedical Robotics and Biomechatronics (BioRob), Singapore, 26–29 June 2016; pp. 542–547. [Google Scholar] [CrossRef]
- Yu, B.; Zhang, X.; Wu, L.; Chen, X.; Chen, X. A Novel Postprocessing Method for Robust Myoelectric Pattern-Recognition Control Through Movement Pattern Transition Detection. IEEE Trans. Hum.-Mach. Syst. 2020, 50, 32–41. [Google Scholar] [CrossRef]
- Teh, Y.; Hargrove, L.J. Understanding Limb Position and External Load Effects on Real-Time Pattern Recognition Control in Amputees. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 1605–1613. [Google Scholar] [CrossRef] [PubMed]
- Furui, A.; Igaue, T.; Tsuji, T. EMG pattern recognition via Bayesian inference with scale mixture-based stochastic generative models. Expert Syst. Appl. 2021, 185, 115644. [Google Scholar] [CrossRef]
- Sarabia, P.; Araujo, A.; Sarabia, L.A.; Ortiz, M.d.l.C. Electromyography Gesture Model Classifier for Fault-Tolerant-Embedded Devices by Means of Partial Least Square Class Modelling Error Correcting Output Codes (PLS-ECOC). Algorithms 2023, 16, 149. [Google Scholar] [CrossRef]
- He, J.; Joshi, M.V.; Chang, J.; Jiang, N. Efficient correction of armband rotation for myoelectric-based gesture control interface. J. Neural Eng. 2020, 17, 036025. [Google Scholar] [CrossRef]
- Valencia, O.; Ortiz, M.C.; Sánchez, M.S.; Sarabia, L.A. A modified entropy-based performance criterion for class-modelling with multiple classes. Chemom. Intell. Lab. Syst. 2021, 217, 104423. [Google Scholar] [CrossRef]
- Ciocarlie, M.T.; Clanton, S.T.; Spalding, M.C.; Allen, P.K. Biomimetic grasp planning for cortical control of a robotic hand. In Proceedings of the 2008 IEEE/RSJ International Conference on Intelligent Robots and Systems, Nice, France, 22–26 September 2008; pp. 2271–2276. [Google Scholar] [CrossRef]
- Hu, X.; Song, A.; Wang, J.; Zeng, H.; Wei, W. Finger Movement Recognition via High-Density Electromyography of Intrinsic and Extrinsic Hand Muscles. Sci. Data 2022, 9, 373. [Google Scholar] [CrossRef]
- RWoodward, B.; Hargrove, L.J. Adapting myoelectric control in real-time using a virtual environment. J. NeuroEng. Rehabil. 2019, 16, 11. [Google Scholar] [CrossRef]
- Adewuyi, A.A.; Hargrove, L.J.; Kuiken, T.A. An Analysis of Intrinsic and Extrinsic Hand Muscle EMG for Improved Pattern Recognition Control. IEEE Trans. Neural Syst. Rehabil. Eng. 2016, 24, 485–494. [Google Scholar] [CrossRef]
- Dyson, M.; Barnes, J.; Nazarpour, K. Myoelectric control with abstract decoders. J. Neural Eng. 2018, 15, 056003. [Google Scholar] [CrossRef] [PubMed]
- Dyson, M.; Dupan, S.; Jones, H.; Learning, K.N. Generalization, and Scalability of Abstract Myoelectric Control. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 1539–1547. [Google Scholar] [CrossRef] [PubMed]
- Krasoulis, A.; Nazarpour, K. Discrete Action Control for Prosthetic Digits. IEEE Trans. Neural Syst. Rehabil. Eng. 2022, 30, 610–620. [Google Scholar] [CrossRef] [PubMed]
- Rouse, A.G. A four-dimensional virtual hand brain–machine interface using active dimension selection. J. Neural Eng. 2016, 13, 036021. [Google Scholar] [CrossRef]
- Clancy, E.A.; Martinez-Luna, C.; Wartenberg, M.; Dai, C.; Farrell, T.R. Two degrees of freedom quasi-static EMG-force at the wrist using a minimum number of electrodes. J. Electromyogr. Kinesiol. 2017, 34, 24–36. [Google Scholar] [CrossRef]
- Chen, Y.; Dai, C.; Chen, W. Cross-Comparison of EMG-to-Force Methods for Multi-DoF Finger Force Prediction Using One-DoF Training. IEEE Access 2020, 8, 13958–13968. [Google Scholar] [CrossRef]
- Toro-Ossaba, A.; Jaramillo-Tigreros, J.; Tejada, J.C.; Peña, A.; López-González, A.; Castanho, R.A. LSTM Recurrent Neural Network for Hand Gesture Recognition Using EMG Signals. Appl. Sci. 2022, 12, 9700. [Google Scholar] [CrossRef]
- Toro-Ossaba, A.; Tejada, J.C.; Rúa, S.; Núñez, J.D.; Peña, A. Myoelectric Model Reference Adaptive Control with Adaptive Kalman Filter for a soft elbow exoskeleton. Control Eng. Pract. 2024, 142, 105774. [Google Scholar] [CrossRef]
- Echtioui, A.; Mlaouah, A.; Zouch, W.; Ghorbel, M.; Mhiri, C.; Hamam, H. A Novel Convolutional Neural Network Classification Approach of Motor-Imagery EEG Recording Based on Deep Learning. Appl. Sci. 2021, 11, 9948. [Google Scholar] [CrossRef]
- Ali, O.; Saif-ur-Rehman, M.; Dyck, S.; Glasmachers, T.; Iossifidis, I.; Klaes, C. Enhancing the decoding accuracy of EEG signals by the introduction of anchored-STFT and adversarial data augmentation method. Sci. Rep. 2022, 12, 4245. [Google Scholar] [CrossRef]
- Chu, Y.; Zhao, X.; Zou, Y.; Xu, W.; Song, G.; Han, J.; Zhao, Y. Decoding multiclass motor imagery EEG from the same upper limb by combining Riemannian geometry features and partial least squares regression. J. Neural Eng. 2020, 17, 046029. [Google Scholar] [CrossRef] [PubMed]
- Ma, Z.; Wang, K.; Xu, M.; Yi, W.; Xu, F.; Ming, D. Transformed common spatial pattern for motor imagery-based brain-computer interfaces. Front. Neurosci. 2023, 17, 1116721. Available online: https://www.frontiersin.org/articles/10.3389/fnins.2023.1116721 (accessed on 9 August 2023). [CrossRef] [PubMed]
- Fuentes-Gonzalez, J.; Infante-Alarcón, A.; Asanza, V.; Loayza, F.R. A 3D-Printed EEG based Prosthetic Arm. In Proceedings of the 2020 IEEE International Conference on E-health Networking, Application & Services (HEALTHCOM), Shenzhen, China, 1–2 March 2021; pp. 1–5. [Google Scholar] [CrossRef]
- Chegani, R.S.; Menon, C. Regressing grasping using force myography: An exploratory study. Biomed. Eng. OnLine 2018, 17, 159. [Google Scholar] [CrossRef]
- Belyea, A.; Englehart, K.; Scheme, E. FMG Versus EMG: A Comparison of Usability for Real-Time Pattern Recognition Based Control. IEEE Trans. Biomed. Eng. 2019, 66, 3098–3104. [Google Scholar] [CrossRef] [PubMed]
- Yanagisawa, T.; Fukuma, R.; Seymour, B.; Tanaka, M.; Yamashita, O.; Hosomi, K.; Kishima, H.; Kamitani, Y.; Saitoh, Y. Neurofeedback Training without Explicit Phantom Hand Movements and Hand-Like Visual Feedback to Modulate Pain: A Randomized Crossover Feasibility Trial. J. Pain 2022, 23, 2080–2091. [Google Scholar] [CrossRef]
- Fukuma, R.; Yanagisawa, T.; Yorifuji, S.; Kato, R.; Yokoi, H.; Hirata, M.; Saitoh, Y.; Kishima, H.; Kamitani, Y.; Yoshimine, T. Closed-Loop Control of a Neuroprosthetic Hand by Magnetoencephalographic Signals. PLoS ONE 2015, 10, e0131547. [Google Scholar] [CrossRef]
- Zimmermann, J.B.; Seki, K.; Jackson, A. Reanimating the arm and hand with intraspinal microstimulation. J. Neural Eng. 2011, 8, 054001. [Google Scholar] [CrossRef]
- Guiho, T.; Baker, S.N.; Jackson, A. Epidural and transcutaneous spinal cord stimulation facilitates descending inputs to upper-limb motoneurons in monkeys. J. Neural Eng. 2021, 18, 046011. [Google Scholar] [CrossRef]
- Freudenburg, Z.V.; Branco, M.P.; Leinders, S.; van der Vijgh, B.H.; Pels, E.G.M.; Denison, T.; Berg, L.H.v.D.; Miller, K.J.; Aarnoutse, E.J.; Ramsey, N.F.; et al. Sensorimotor ECoG Signal Features for BCI Control: A Comparison Between People with Locked-In Syndrome and Able-Bodied Controls. Front. Neurosci. 2019, 13, 1058. Available online: https://www.frontiersin.org/articles/10.3389/fnins.2019.01058 (accessed on 7 September 2023). [CrossRef]
- Yin, Z.; Chen, H.; Yang, X.; Liu, Y.; Zhang, N.; Meng, J.; Liu, H. A Wearable Ultrasound Interface for Prosthetic Hand Control. IEEE J. Biomed. Health Inform. 2022, 26, 5384–5393. [Google Scholar] [CrossRef]
- Whelan, L.; Flinn, S.; Wagner, N. Individualizing goals for users of externally powered partial hand prostheses. J. Rehabil. Res. Dev. 2014, 51, 885–894. [Google Scholar] [CrossRef] [PubMed]
- Koudelkova, Z.; Mizera, A.; Karhankova, M.; Mach, V.; Stoklasek, P.; Krupciak, M.; Minarcik, J.; Jasek, R. Verification of Finger Positioning Accuracy of an Affordable Transradial Prosthesis. Designs 2023, 7, 14. [Google Scholar] [CrossRef]
- Segil, J.L.; Pulver, B.; Huddle, S.; Weir, R.F.F.; Sliker, L. The Point Digit II: Mechanical Design and Testing of a Ratcheting Prosthetic Finger. Mil. Med. 2021, 186, 674–680. [Google Scholar] [CrossRef] [PubMed]
- Murali, B.; Huddle, S.; Weir, R.F.F. Design and evaluation of a distally actuated powered finger prosthesis with self-contained transmission for individuals with partial hand loss. Adv. Mech. Eng. 2019, 11, 1687814019834114. [Google Scholar] [CrossRef]
- Jeong, G.-C.; Kim, Y.; Choi, W.; Gu, G.; Lee, H.-J.; Hong, M.B.; Kim, K. On the Design of a Novel Underactuated Robotic Finger Prosthesis for Partial Hand Amputation. In Proceedings of the 2019 IEEE 16th International Conference on Rehabilitation Robotics (ICORR), Toronto, ON, Canada, 24–28 June 2019; pp. 861–867. [Google Scholar] [CrossRef]
- Young, K.J.; Pierce, J.E.; Zuniga, J.M. Assessment of body-powered 3D printed partial finger prostheses: A case study. 3D Print. Med. 2019, 5, 7. [Google Scholar] [CrossRef]
- Copeland, C.; Reyes, C.C.; Peck, J.L.; Srivastava, R.; Zuniga, J.M. Functional performance and patient satisfaction comparison between a 3D printed and a standard transradial prosthesis: A case report. Biomed. Eng. OnLine 2022, 21, 7. [Google Scholar] [CrossRef]
- Alturkistani, R.; A, K.; Devasahayam, S.; Thomas, R.; Colombini, E.L.; Cifuentes, C.A.; Homer-Vanniasinkam, S.; Wurdemann, H.A.; Moazen, M. Affordable passive 3D-printed prosthesis for persons with partial hand amputation. Prosthet. Orthot. Int. 2020, 44, 92. [Google Scholar] [CrossRef]
- Anderson, B.; Schanandore, J.V. Using a 3D-Printed Prosthetic to Improve Participation in a Young Gymnast. Pediatr. Phys. Ther. 2021, 33, E1. [Google Scholar] [CrossRef]
- Lake, C. Experience with Electric Prostheses for the Partial Hand Presentation: An Eight-Year Retrospective. JPO J. Prosthet. Orthot. 2009, 21, 125. [Google Scholar] [CrossRef]
- Uellendahl, J.E.; Mandacina, S.; Ramdial, S. Custom Silicone Sockets for Myoelectric Prostheses. JPO J. Prosthet. Orthot. 2006, 18, 35. [Google Scholar] [CrossRef]
- Reissman, T.; Halsne, E.; Lipschutz, R.; Miller, L.; Kuiken, T. A novel gel liner system with embedded electrodes for use with upper limb myoelectric prostheses. PLoS ONE 2018, 13, e0198934. [Google Scholar] [CrossRef] [PubMed]
- Imbinto, I.; Peccia, C.; Controzzi, M.; Cutti, A.G.; Davalli, A.; Sacchetti, R.; Cipriani, C. Treatment of the Partial Hand Amputation: An Engineering Perspective. IEEE Rev. Biomed. Eng. 2016, 9, 32–48. [Google Scholar] [CrossRef] [PubMed]
- Desteli, E.E.; İmren, Y.; Erdoğan, M.; Sarısoy, G.; Coşgun, S. Comparison of upper limb amputees and lower limb amputees: A psychosocial perspective. Eur. J. Trauma Emerg. Surg. 2014, 40, 735–739. [Google Scholar] [CrossRef] [PubMed]
- Al-Turaiki, H.S.; Al-Falahi, L.A.A. Amputee population in the Kingdom of Saudi Arabia. Prosthet. Orthot. Int. 1993, 17, 147. [Google Scholar] [CrossRef]
- Khalil, M.T.; Raza, A. Rehabilitation of Partial Hand Amputations in Pakistan. Pak. Armed Forces Med. J. 2022, 72, 713–716. [Google Scholar] [CrossRef]
- Leow, M.E.L.; Kour, A.K.; Ng, W.K.M.; Pho, R.W.H. Creating a model for fabricating a partial hand glove prosthesis using the realigned casts of the contralateral digits. Prosthet. Orthot. Int. 1999, 23, 72. [Google Scholar] [CrossRef]
- Gemiudeas, G.; Dahlan, A.; Gemiudeas, G.; Dahlan, A. A simplified silicone finger prosthesis: A clinical report. World J. Adv. Res. Rev. 2022, 14, 353–358. [Google Scholar] [CrossRef]
- Kuret, Z.; Burger, H.; Vidmar, G.; Maver, T. Adjustment to finger amputation and silicone finger prosthesis use. Disabil. Rehabil. 2019, 41, 1307–1312. [Google Scholar] [CrossRef]
- Bhaskaran, S.; Zachariah, G.P. Enhancing retention and esthetics of fabricated silicone finger prosthesis using stump reduction technique and customized acrylic nail: A unique approach. Natl. J. Maxillofac. Surg. 2022, 13, S140. [Google Scholar] [CrossRef]
- Kini, A.Y.; Byakod, P.P.; Angadi, G.S.; Pai, U.; Bhandari, A.J. Comprehensive prosthetic rehabilitation of a patient with partial finger amputations using silicone biomaterial: A technical note. Prosthet. Orthot. Int. 2010, 34, 488–494. [Google Scholar] [CrossRef]
- Colvenkar, S.; Kota, S.P.; Chalapathi, M.; Bandari, G.; Sriteja, D. Acrylic Finger Prosthesis: A Case Report. Cureus 2022, 14, e30974. [Google Scholar] [CrossRef] [PubMed]
- Rajeev Kumar Reddy, K.; Bandela, V.; Bharathi, M.; Giridhar Reddy, S.V. Acrylic Finger Prosthesis: A Case Report. J. Clin. Diagn. Res. JCDR 2014, 8, ZD07–ZD08. [Google Scholar] [CrossRef]
- Carroll, Á.M.; Fyfe, N. A Comparison of the Effect of the Aesthetics of Digital Cosmetic Prostheses on Body Image and Well-Being. JPO J. Prosthet. Orthot. 2004, 16, 66. [Google Scholar] [CrossRef]
- Shim, J.K.; Oliveira, M.A.; Hsu, J.; Huang, J.; Park, J.; Clark, J.E. Hand digit control in children: Age-related changes in hand digit force interactions during maximum flexion and extension force production tasks. Exp. Brain Res. 2007, 176, 374–386. [Google Scholar] [CrossRef]
- Lee, M.-Y.; Lee, S.H.; Leigh, J.-H.M.; Nam, H.S.; Hwang, E.Y.O.; Lee, J.Y.O.; Han, S.O.; Lee, G.M. Functional improvement by body-powered 3D-printed prosthesis in patients with finger amputation: Two case reports. Medicine 2022, 101, e29182. [Google Scholar] [CrossRef]
- Phillips, S.L.; Harris, M.S.; Koss, L.; Latlief, G. Experiences and Outcomes with Powered Partial Hand Prostheses: A Case Series of Subjects With Multiple Limb Amputations. JPO J. Prosthet. Orthot. 2012, 24, 93. [Google Scholar] [CrossRef]
- Whelan, L.R.; Farley, J. Functional Outcomes with Externally Powered Partial Hand Prostheses. JPO J. Prosthet. Orthot. 2018, 30, 69. [Google Scholar] [CrossRef]
- Borrell, J.A.; Copeland, C.; Lukaszek, J.L.; Fraser, K.; Zuniga, J.M. Use-Dependent Prosthesis Training Strengthens Contralateral Hemodynamic Brain Responses in a Young Adult with Upper Limb Reduction Deficiency: A Case Report. Front. Neurosci. 2021, 15, 693138. Available online: https://www.frontiersin.org/articles/10.3389/fnins.2021.693138 (accessed on 27 March 2023). [CrossRef]
- Lukaszek, J.L.; Borrell, J.A.; Cortes, C.; Zuniga, J.M. Home intervention for children and adolescents with unilateral trans-radial and partial carpal reduction deficiencies. Sci. Rep. 2022, 12, 7447. [Google Scholar] [CrossRef]
- Latour, D. Advances in Upper Extremity Prosthetic Technology: Rehabilitation and the Interprofessional Team. Curr. Phys. Med. Rehabil. Rep. 2022, 10, 71–76. [Google Scholar] [CrossRef]
- Timm, L.; Etuket, M.; Sivarasu, S. Design and Development of an Open-Source Adl-Compliant Prosthetic Arm for Trans-Radial Amputees. presented at the 2022 Design of Medical Devices Conference. Am. Soc. Mech. Eng. Digit. Collect. 2022, 84815, V001T09A004. [Google Scholar] [CrossRef]
- Mano, H.; Fujiwara, S.; Haga, N. Effect of prostheses on children with congenital upper limb deficiencies. Pediatr. Int. 2020, 62, 1039–1043. [Google Scholar] [CrossRef] [PubMed]
- Peterson, J.K.; Prigge, P. Early Upper-Limb Prosthetic Fitting and Brain Development: Considerations for Success. JPO J. Prosthet. Orthot. 2020, 32, 229. [Google Scholar] [CrossRef]
- Zuniga, J.M.; Peck, J.L.; Srivastava, R.; Pierce, J.E.; Dudley, D.R.; Than, N.A.; Stergiou, N. Functional changes through the usage of 3D-printed transitional prostheses in children. Disabil. Rehabil. Assist. Technol. 2019, 14, 68–74. [Google Scholar] [CrossRef]
- Cancio, J.M.; Orr, A.; Eskridge, S.; Shannon, K.; Mazzone, B.; Farrokhi, S. Occupational Therapy Practice Patterns for Military Service Members with Upper Limb Amputation. Mil. Med. 2020, 185, 444–450. [Google Scholar] [CrossRef]
- Yanagisawa, T.; Fukuma, R.; Seymour, B.; Hosomi, K.; Kishima, H.; Shimizu, T.; Yokoi, H.; Hirata, M.; Yoshimine, T.; Kamitani, Y.; et al. Induced sensorimotor brain plasticity controls pain in phantom limb patients. Nat. Commun. 2016, 7, 13209. [Google Scholar] [CrossRef]
- Wu, F.; Asada, H. Supernumerary Robotic Fingers: An Alternative Upper-Limb Prosthesis. presented at the ASME 2014 Dynamic Systems and Control Conference. Am. Soc. Mech. Eng. Digit. Collect. 2014, 46193, V002T16A009. [Google Scholar] [CrossRef]
- Guggenheim, J.; Hoffman, R.; Song, H.; Asada, H.H. Leveraging the Human Operator in the Design and Control of Supernumerary Robotic Limbs. IEEE Robot. Autom. Lett. 2020, 5, 2177–2184. [Google Scholar] [CrossRef]
- Schicktanz, S.; Amelung, T.; Rieger, J.W. Qualitative assessment of patients’ attitudes and expectations toward BCIs and implications for future technology development. Front. Syst. Neurosci. 2015, 9, 64. Available online: https://www.frontiersin.org/articles/10.3389/fnsys.2015.00064 (accessed on 25 April 2023). [CrossRef]
- Sullivan, L.S.; Klein, E.; Brown, T.; Sample, M.; Pham, M.; Tubig, P.; Folland, R.; Truitt, A.; Goering, S. Keeping Disability in Mind: A Case Study in Implantable Brain–Computer Interface Research. Sci. Eng. Ethics 2018, 24, 479–504. [Google Scholar] [CrossRef]
- Kögel, J.; Jox, R.; Friedrich, O. What is it like to use a BCI?—Insights from an interview study with brain-computer interface users. BMC Med. Ethics 2020, 21, 2. [Google Scholar] [CrossRef] [PubMed]
- Ring, H.; Rosenthal, N. Controlled study of neuroprosthetic functional electrical stimulation in sub-acute post-stroke rehabilitation. J. Rehabil. Med. 2005, 37, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Hara, Y.; Ogawa, S.; Tsujiuchi, K.; Muraoka, Y. A home-based rehabilitation program for the hemiplegic upper extremity by power-assisted functional electrical stimulation. Disabil. Rehabil. 2008, 30, 296–304. [Google Scholar] [CrossRef] [PubMed]
- Godfrey, S.B.; Piazza, C.; Felici, F.; Grioli, G.; Bicchi, A.; Catalano, M.G. Usability Assessment of Body Controlled Electric Hand Prostheses: A Pilot Study. Front. Neurorobotics 2021, 15, 683253. Available online: https://www.frontiersin.org/articles/10.3389/fnbot.2021.683253 (accessed on 22 November 2022). [CrossRef]
- Graham, J.; Wang, M.; Frizzell, K.; Watkins, C.; Beredjiklian, P.; Rivlin, M. Conventional vs 3-Dimensional Printed Cast Wear Comfort. HAND 2020, 15, 388–392. [Google Scholar] [CrossRef]
- Graham, E.M.; Arbon, J.; Baschuk, C.M.; Duncan, A.; Mendenhall, S.D. Making the Best of a Bad Situation: Case Report of a Nonreplantable Four-finger Amputation with Flap Coverage and Partial Hand Prosthesis Utilization. Plast. Reconstr. Surg.—Glob. Open 2022, 10, e4253. [Google Scholar] [CrossRef]
- Chug, M.; Williams, N.; Benn, D.; Brindley, S. Outcome of uncemented trapeziometacarpal prosthesis for treatment of thumb carpometacarpal joint arthritis. Indian J. Orthop. 2014, 48, 394–398. [Google Scholar] [CrossRef]
- Mahmood, I.; Burton, R.; Choudhry, M.N.; Coapes, C. Early to Mid-Term Results in Trapezio-metacarpal Joint Replacement using the ARPE Implant. Open Orthop. J. 2020, 14, 683253. [Google Scholar] [CrossRef]
- Nambu, S.; Ikebuchi, M.; Taniguchi, M.; Park, C.S.; Kitagawa, T.; Nakajima, S.; Koike, T. Advantages of externally powered prosthesis with feedback system using pseudo-cineplasty. J. Rehabil. Res. Dev. 2014, 51, 1095–1102. [Google Scholar] [CrossRef]
- Cheng, J.; Yang, Z.; Overstreet, C.K.; Keefer, E. Fascicle-Specific Targeting of Longitudinal Intrafascicular Electrodes for Motor and Sensory Restoration in Upper-Limb Amputees. Hand Clin. 2021, 37, 401–414. [Google Scholar] [CrossRef]
- Jönsson, S.; Caine-Winterberger, K.; Brånemark, R. Osseointegration amputation prostheses on the upper limbs: Methods, prosthetics and rehabilitation. Prosthet. Orthot. Int. 2011, 35, 190. [Google Scholar] [CrossRef] [PubMed]
- Tsikandylakis, G.; Berlin, Ö.; Brånemark, R. Implant Survival, Adverse Events, and Bone Remodeling of Osseointegrated Percutaneous Implants for Transhumeral Amputees. Clin. Orthop. Relat. Res. 2014, 472, 2947. [Google Scholar] [CrossRef] [PubMed]
- Hooper, R.C.; Cederna, P.S.; Brown, D.L.; Haase, S.C.; Waljee, J.F.; Egeland, B.M.; Kelley, B.P.; Kung, T.A. Regenerative Peripheral Nerve Interfaces for the Management of Symptomatic Hand and Digital Neuromas. Plast. Reconstr. Surg.—Glob. Open 2020, 8, e2792. [Google Scholar] [CrossRef] [PubMed]
- Burke, K.; Kung, T.; Hooper, R.; Kemp, S.; Cederna, P. Regenerative peripheral nerve interfaces (RPNIs): Current status and future direction. Plast. Aesthetic Res. 2022, 9, 48. [Google Scholar] [CrossRef]
- Bergmeister, K.D.; Salminger, S.; Aszmann, O.C. Targeted Muscle Reinnervation for Prosthetic Control. Hand Clin. 2021, 37, 415–424. [Google Scholar] [CrossRef]
- Borrell, J.A.; Manattu, A.K.; Copeland, C.; Fraser, K.; D’ovidio, A.; Granatowicz, Z.; Lesiak, A.C.; Figy, S.C.; Zuniga, J.M. Phantom limb therapy improves cortical efficiency of the sensorimotor network in a targeted muscle reinnervation amputee: A case report. Front. Neurosci. 2023, 17, 1130050. Available online: https://www.frontiersin.org/articles/10.3389/fnins.2023.1130050 (accessed on 17 July 2023). [CrossRef]
- Hruby, L.A.; Sturma, A.; Mayer, J.A.; Pittermann, A.; Salminger, S.; Aszmann, O.C. Algorithm for bionic hand reconstruction in patients with global brachial plexopathies. J. Neurosurg. 2017, 127, 1163–1171. [Google Scholar] [CrossRef]
- Sturma, A.; Hruby, L.A.; Boesendorfer, A.; Pittermann, A.; Salminger, S.; Gstoettner, C.; Politikou, O.; Vujaklija, I.; Farina, D.; Aszmann, O.C. Prosthetic Embodiment and Body Image Changes in Patients Undergoing Bionic Reconstruction Following Brachial Plexus Injury. Front. Neurorobotics 2021, 15, 645261. Available online: https://www.frontiersin.org/articles/10.3389/fnbot.2021.645261 (accessed on 20 July 2023). [CrossRef]
- Hughes, K.; Hamdan, A.; Schermerhorn, M.; Giordano, A.; Scovell, S.; Pomposelli, F. Bypass for chronic ischemia of the upper extremity: Results in 20 patients. J. Vasc. Surg. 2007, 46, 303–307. [Google Scholar] [CrossRef]
- Frontario, S.C.; Hammond, B.J.; Sagarwala, A.; Bernik, T.R. Surgical management for refractory Raynaud’s phenomena, a rare presentation of upper extremity limb ischemia. Ann. Vasc. Surg.—Brief Rep. Innov. 2022, 2, 100078. [Google Scholar] [CrossRef]
- Pessia, P.; Cordella, F.; Schena, E.; Davalli, A.; Sacchetti, R.; Zollo, L. Evaluation of Pressure Capacitive Sensors for Application in Grasping and Manipulation Analysis. Sensors 2017, 17, 2846. [Google Scholar] [CrossRef] [PubMed]
- Mishra, R.B.; Khan, S.M.; Shaikh, S.F.; Hussain, A.M.; Hussain, M.M. Low-cost foil/paper based touch mode pressure sensing element as artificial skin module for prosthetic hand. In Proceedings of the 2020 3rd IEEE International Conference on Soft Robotics (RoboSoft), New Haven, CT, USA, 15 May–15 July 2020; pp. 194–200. [Google Scholar] [CrossRef]
- Mishra, R.B.; Al-Modaf, F.; Babatain, W.; Hussain, A.M.; El-Atab, N. Structural Engineering Approach for Designing Foil-Based Flexible Capacitive Pressure Sensors. IEEE Sens. J. 2022, 22, 11543–11551. [Google Scholar] [CrossRef]
- Wolterink, G.; Kosmas, D.; Schouten, M.; van Beijnum, B.-J.F.; Veltink, P.H.; Krijnen, G. Evaluation of a 3D Printed Soft Sensor for Measuring Fingertip Interaction Forces. IEEE Sens. J. 2022, 22, 11499–11508. [Google Scholar] [CrossRef]
- Romeo, R.A.; Lauretti, C.; Gentile, C.; Guglielmelli, E.; Zollo, L. Method for Automatic Slippage Detection with Tactile Sensors Embedded in Prosthetic Hands. IEEE Trans. Med. Robot. Bionics 2021, 3, 485–497. [Google Scholar] [CrossRef]
- Barone, D.; D’Alonzo, M.; Controzzi, M.; Clemente, F.; Cipriani, C. A cosmetic prosthetic digit with bioinspired embedded touch feedback. In Proceedings of the 2017 International Conference on Rehabilitation Robotics (ICORR), London, UK, 17–20 July 2017; pp. 1136–1141. [Google Scholar] [CrossRef]
- Xu, X.; Deng, H.; Zhang, Y.; Chen, J. Continuous Grasping Force Estimation with Surface EMG Based on Huxley-Type Musculoskeletal Model. IEEE Trans. Neural Syst. Rehabil. Eng. 2023, 31, 346–355. [Google Scholar] [CrossRef]
- Ccorimanya, L.; Watanabe, R.; Hassan, M.; Hada, Y.; Suzuki, K. Design of a myoelectric 3D-printed prosthesis for a child with upper limb congenital amputation. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 5394–5398. [Google Scholar] [CrossRef]
- Imbinto, I.; Montagnani, F.; Bacchereti, M.; Cipriani, C.; Davalli, A.; Sacchetti, R.; Gruppioni, E.; Castellano, S.; Controzzi, M. The S-Finger: A Synergetic Externally Powered Digit with Tactile Sensing and Feedback. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 1264–1271. [Google Scholar] [CrossRef]
- Pistohl, T.; Joshi, D.; Ganesh, G.; Jackson, A.; Nazarpour, K. Artificial Proprioceptive Feedback for Myoelectric Control. IEEE Trans. Neural Syst. Rehabil. Eng. 2015, 23, 498–507. [Google Scholar] [CrossRef]
- Engels, L.F.; Shehata, A.W.; Scheme, E.J.; Sensinger, J.W.; Cipriani, C. When Less Is More—Discrete Tactile Feedback Dominates Continuous Audio Biofeedback in the Integrated Percept While Controlling a Myoelectric Prosthetic Hand. Front. Neurosci. 2019, 13, 578. Available online: https://www.frontiersin.org/articles/10.3389/fnins.2019.00578 (accessed on 22 July 2023). [CrossRef]
- Abd, M.A.; Ingicco, J.; Hutchinson, D.T.; Tognoli, E.; Engeberg, E.D. Multichannel haptic feedback unlocks prosthetic hand dexterity. Sci. Rep. 2022, 12, 2323. [Google Scholar] [CrossRef]
- Gu, G.; Zhang, N.; Xu, H.; Lin, S.; Yu, Y.; Chai, G.; Ge, L.; Yang, H.; Shao, Q.; Sheng, X.; et al. A soft neuroprosthetic hand providing simultaneous myoelectric control and tactile feedback. Nat. Biomed. Eng. 2021, 7, 589–598. [Google Scholar] [CrossRef]
- Berman, B. 3-D printing: The new industrial revolution. Bus. Horiz. 2012, 55, 155–162. [Google Scholar] [CrossRef]
- Zuniga, J.M.; Pierce, J.E.; Copeland, C.; Cortes-Reyes, C.; Salazar, D.; Wang, Y.; Arun, K.M.; Huppert, T. Brain lateralization in children with upper-limb reduction deficiency. J. NeuroEng. Rehabil. 2021, 18, 24. [Google Scholar] [CrossRef] [PubMed]
- Zuniga, J.M.; Young, K.J.; Peck, J.L.; Srivastava, R.; Pierce, J.E.; Dudley, D.R.; Salazar, D.A.; Bergmann, J. Remote fitting procedures for upper limb 3d printed prostheses. Expert Rev. Med. Devices 2019, 16, 257–266. [Google Scholar] [CrossRef] [PubMed]
- Zuniga, J.M.; Dimitrios, K.; Peck, J.L.; Srivastava, R.; Pierce, J.E.; Dudley, D.R.; Salazar, D.A.; Young, K.J.; Knarr, B.A. Coactivation index of children with congenital upper limb reduction deficiencies before and after using a wrist-driven 3D printed partial hand prosthesis. J. NeuroEng. Rehabil. 2018, 15, 48. [Google Scholar] [CrossRef]
- Giaconi, C.; Nahuelhual, P.; Dote, J.; Cubillos, R.; Fuentes, G.; Zúñiga, J. Experiences of the use of 3D printed hand ortoprosthesis (Cyborg Beast) in adolescents with congenital hand amputation and their main caregivers: A study of cases. Rev. Chil. Pediatría 2019, 90, 539–544. [Google Scholar] [CrossRef]
- McDonald, C.L.; Bennett, C.L.; Rosner, D.K.; Steele, K.M. Perceptions of ability among adults with upper limb absence: Impacts of learning, identity, and community. Disabil. Rehabil. 2020, 42, 3306–3315. [Google Scholar] [CrossRef]
- Demers, L.; Weiss-Lambrou, R.; Ska, B. Development of the Quebec User Evaluation of Satisfaction with assistive Technology (QUEST). Assist. Technol. Off. J. RESNA 1996, 8, 3–13. [Google Scholar] [CrossRef]
- Desrosiers, J.; Bravo, G.; Hébert, R.; Dutil, E.; Mercier, L. Validation of the Box and Block Test as a measure of dexterity of elderly people: Reliability, validity, and norms studies. Arch. Phys. Med. Rehabil. 1994, 75, 751–755. [Google Scholar] [CrossRef]
- Fabbri, B.; Berardi, A.; Tofani, M.; Panuccio, F.; Ruotolo, I.; Sellitto, G.; Galeoto, G. A systematic review of the psychometric properties of the Jebsen–Taylor Hand Function Test (JTHFT). Hand Surg. Rehabil. 2021, 40, 560–567. [Google Scholar] [CrossRef]
- Kang, J.; Gonzalez, M.A.; Gillespie, R.B.; Gates, D.H. A Haptic Object to Quantify the Effect of Feedback Modality on Prosthetic Grasping. IEEE Robot. Autom. Lett. 2019, 4, 1101–1108. [Google Scholar] [CrossRef]
- Sinke, M.; Chadwell, A.; Smit, G. State of the art of prosthesis simulators for the upper limb: A narrative review. Ann. Phys. Rehabil. Med. 2022, 65, 101635. [Google Scholar] [CrossRef] [PubMed]
- Pan, T.-T.; Fan, P.-L.; Chiang, H.K.; Chang, R.-S.; Jiang, J.-A. Mechatronic experiments course design: A myoelectric controlled partial-hand prosthesis project. IEEE Trans. Educ. 2004, 47, 348–355. [Google Scholar] [CrossRef]
- Snajdarova, M.; Barabas, J.; Radil, R.; Hock, O. Proof of Concept EMG-Controlled Prosthetic Hand System—An Overview. In Proceedings of the 19th International Conference Computational Problems of Electrical Engineering, Banska Stiavnica, Slovakia, 9–12 September 2018; pp. 1–4. [Google Scholar] [CrossRef]
- Ribeiro, D.; Cimino, S.R.; Mayo, A.L.; Ratto, M.; Hitzig, S.L. 3D printing and amputation: A scoping review. Disabil. Rehabil. Assist. Technol. 2021, 16, 221–240. [Google Scholar] [CrossRef] [PubMed]
- Cappetti, N.; Naddeo, A.; Salerno, G. Influence of Control Parameters on Consumer FDM 3D Printing. Transdiscipl. Eng. Methods Soc. Innov. Ind. 2018, 40, 165–177. [Google Scholar] [CrossRef]
- Koprnický, J.; Najman, P.; Šafka, J. 3D printed bionic prosthetic hands. In Proceedings of the 2017 IEEE International Workshop of Electronics, Control, Measurement, Signals and Their Application to Mechatronics (ECMSM), Donostia, Spain, 24–26 May 2017; pp. 1–6. [Google Scholar] [CrossRef]
- Antreas, K.; Piromalis, D. Employing a Low-Cost Desktop 3D Printer: Challenges, and How to Overcome Them by Tuning Key Process Parameters. Int. J. Mech. Appl. 2021, 10, 11–19. [Google Scholar] [CrossRef]
- Brack, R.; Amalu, E.H. A review of technology, materials and R&D challenges of upper limb prosthesis for improved user suitability. J. Orthop. 2021, 23, 88–96. [Google Scholar] [CrossRef]
- Cianchetti, M.; Laschi, C.; Menciassi, A.; Dario, P. Biomedical applications of soft robotics. Nat. Rev. Mater. 2018, 3, 143–153. [Google Scholar] [CrossRef]
- Zuniga, J.M. 3D Printed Antibacterial Prostheses. Appl. Sci. 2018, 8, 1651. [Google Scholar] [CrossRef]
- Kantaros, A. 3D Printing in Regenerative Medicine: Technologies and Resources Utilized. Int. J. Mol. Sci. 2022, 23, 14621. [Google Scholar] [CrossRef]
- Fox, B.; Subic, A. An Industry 4.0 Approach to the 3D Printing of Composite Materials. Engineering 2019, 5, 621–623. [Google Scholar] [CrossRef]
- Kondiah, P.J.; Kondiah, P.P.D.; Choonara, Y.E.; Marimuthu, T.; Pillay, V. A 3D Bioprinted Pseudo-Bone Drug Delivery Scaffold for Bone Tissue Engineering. Pharmaceutics 2020, 12, 166. [Google Scholar] [CrossRef] [PubMed]
- Binedell, T.; Meng, E.; Subburaj, K. Design and development of a novel 3D-printed non-metallic self-locking prosthetic arm for a forequarter amputation. Prosthet. Orthot. Int. 2021, 45, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Prakash, A.; Kumari, B.; Sharma, S. A low-cost, wearable sEMG sensor for upper limb prosthetic application. J. Med. Eng. Technol. 2019, 43, 235–247. [Google Scholar] [CrossRef]
- Prakash, A.; Sharma, S. A low-cost transradial prosthesis controlled by the intention of muscular contraction. Phys. Eng. Sci. Med. 2021, 44, 229–241. [Google Scholar] [CrossRef]
- Mio, R.; Villegas, B.; Ccorimanya, L.; Flores, K.M.; Salazar, G.; Elías, D. Development and assessment of a powered 3D-printed prosthetic hand for transmetacarpal amputees. In Proceedings of the 2017 3rd International Conference on Control, Automation and Robotics (ICCAR), Nagoya, Japan, 24–26 April 2017; pp. 85–90. [Google Scholar] [CrossRef]
- Jiang, L.; Zeng, B.; Fan, S.; Sun, K.; Zhang, T.; Liu, H. A modular multisensory prosthetic hand. In Proceedings of the 2014 IEEE International Conference on Information and Automation (ICIA), Hailar, China, 28–30 July 2014; pp. 648–653. [Google Scholar] [CrossRef]
- Slade, P.; Akhtar, A.; Nguyen, M.; Bretl, T. Tact: Design and performance of an open-source, affordable, myoelectric prosthetic hand. In Proceedings of the 2015 IEEE International Conference on Robotics and Automation (ICRA), Seattle, WA, USA, 26–30 May 2015; pp. 6451–6456. [Google Scholar] [CrossRef]
- Gao, G.; Shahmohammadi, M.; Gerez, L.; Kontoudis, G.; Liarokapis, M. On Differential Mechanisms for Underactuated, Lightweight, Adaptive Prosthetic Hands. Front. Neurorobotics 2021, 15, 702031. [Google Scholar] [CrossRef]
- Cuellar, J.S.; Plettenburg, D.; Zadpoor, A.A.; Breedveld, P.; Smit, G. Design of a 3D-printed hand prosthesis featuring articulated bio-inspired fingers. Proc. Inst. Mech. Eng. [H] 2021, 235, 336–345. [Google Scholar] [CrossRef]
- Mohammadi, A.; Lavranos, J.; Zhou, H.; Mutlu, R.; Alici, G.; Tan, Y.; Choong, P.; Oetomo, D. A practical 3D-printed soft robotic prosthetic hand with multi-articulating capabilities. PLoS ONE 2020, 15, e0232766. [Google Scholar] [CrossRef]
- Mohammadi, A.; Lavranos, J.; Tan, Y.; Choong, P.; Oetomo, D. Preliminary Clinical Evaluation of the X-Limb Hand: A 3D Printed Soft Robotic Hand Prosthesis. In Converging Clinical and Engineering Research on Neurorehabilitation IV; Torricelli, D., Akay, M., Pons, J.L., Eds.; Biosystems & Biorobotics; Springer International Publishing: Cham, Switzerland, 2022; pp. 869–873. [Google Scholar] [CrossRef]
- Piazza, C.; Santina, C.D.; Catalano, M.; Grioli, G.; Garabini, M.; Bicchi, A. SoftHand Pro-D: Matching dynamic content of natural user commands with hand embodiment for enhanced prosthesis control. In Proceedings of the 2016 IEEE International Conference on Robotics and Automation (ICRA), Stockholm, Sweden, 16–21 May 2016; pp. 3516–3523. [Google Scholar] [CrossRef]
- Capsi-Morales, P.; Catalano, M.G.; Grioli, G.; Schiavon, L.; Fiaschi, E.; Bicchi, A. Adaptable Poly-Articulated Bionic Hands EnhanceBoth Performance and User’s Perception in Bilateral Amputation: A Case Study. IEEE Trans. Neural Syst. Rehabil. Eng. Publ. IEEE Eng. Med. Biol. Soc. 2022, 30, 2437–2445. [Google Scholar] [CrossRef]
- Zuniga, J.; Katsavelis, D.; Peck, J.; Stollberg, J.; Petrykowski, M.; Carson, A.; Fernandez, C. Cyborg beast: A low-cost 3d-printed prosthetic hand for children with upper-limb differences. BMC Res. Notes 2015, 8, 10. [Google Scholar] [CrossRef]
- Zuniga, J.M.; Peck, J.; Srivastava, R.; Katsavelis, D.; Carson, A. An Open Source 3D-Printed Transitional Hand Prosthesis for Children. JPO J. Prosthet. Orthot. 2016, 28, 103–108. [Google Scholar] [CrossRef]
- da Silva, L.A.; Medola, F.O.; Rodrigues, O.V.; Rodrigues, A.C.T.; Sandnes, F.E. Interdisciplinary-Based Development of User-Friendly Customized 3D Printed Upper Limb Prosthesis. In Advances in Usability, User Experience and Assistive Technology; Ahram, T.Z., Falcão, C., Eds.; Advances in Intelligent Systems and Computing; Springer International Publishing: Cham, Switzerland, 2019; pp. 899–908. [Google Scholar] [CrossRef]
- Hou, Z.; Liu, Q.; Zhao, H.; Xie, J.; Cao, J.; Liao, W.-H.; Bowen, C.R. Biomechanical modeling and experiments of energy harvesting backpacks. Mech. Syst. Signal Process. 2023, 200, 110612. [Google Scholar] [CrossRef]
- Ramezani, M.; Mohd, Z. Ripin 4D Printing in Biomedical Engineering: Advancements, Challenges, and Future Directions. J. Funct. Biomater. 2023, 14, 347. [Google Scholar] [CrossRef] [PubMed]
- Fajardo, J.; Cardona, D.; Maldonado, G.; Ferman, V.; Rohmer, E. A Robust Control Strategy for Sensorless Under-Tendon-Driven Prosthetic Hands. In Proceedings of the 2021 20th International Conference on Advanced Robotics (ICAR), Ljubljana, Slovenia, 6–10 December 2021; pp. 581–587. [Google Scholar] [CrossRef]
- Iqbal, M.; Imtiaz, J.; Mahmood, A. Bond graph modeling with linear quadratic integral control synthesis of a robotic digit in a human impaired hand for anthropomorphic coordination. Trans. Inst. Meas. Control 2023, 45, 400–413. [Google Scholar] [CrossRef]
- Iqbal, M.; Imtiaz, J.; Mughal, A.M. Mixed mu-synthesis tracking control and disturbance rejection in a robotic digit of an impaired human hand for anthropomorphic coordination. Biol. Cybern. 2023, 117, 221–247. [Google Scholar] [CrossRef] [PubMed]






| Study of | Method | Postures | Accuracy |
|---|---|---|---|
| Fonseca et al., 2018 [13] | 1 IMU | 3 | - supervised learning 89% - unsupervised 76% - adaptive 88% |
| Rizzoglio et al., 2023 [15] | 2 IMU | 4 | - unsupervised |
| Adewuyi et al., 2016 [16] | offline | 7 | - |
| Zuleta et al., 2016 [17] | 1 IMU + 8 EMG | 5 | 90% |
| Earley et al., 2014 [19] | 12 EMG | 7 | - |
| Al-Timemy et al., 2018 [21] | 7 pairs of EMG | - | 87% |
| Adewuyi et al., 2017 [22] | 9 EMG | 4 | - |
| Beaulieu et al., 2017 [23] | EMG + position | - | 90% |
| Sarabia et al., 2023 [28] | - | - | Accuracy 87.5% Precision 91.87% F1 score 86.34% |
| Toro et al., 2022 [41] | 4 EMG | 5 | 87 ± 7% |
| No. | Database | Web Address | Access Date |
|---|---|---|---|
| DB1 | thingiverse | https://www.thingiverse.com/ | 30 June 2023 |
| DB 2 | myminifactory | https://www.myminifactory.com/ | 30 June 2023 |
| DB 3 | pinshape | https://pinshape.com/ | 30 June 2023 |
| DB 4 | printables | https://www.printables.com/ | 30 June 2023 |
| DB 5 | NIH 3D print exchange | https://3d.nih.gov/ | 30 June 2023 |
| DB 6 | youmagine | https://www.youmagine.com/ | 30 June 2023 |
| DB 7 | grabcad | https://grabcad.com/ | 30 June 2023 |
| DB 8 | instructables | https://www.instructables.com/ | 30 July 2023 |
| DB 9 | Sketchfab | https://sketchfab.com/ | 30 July 2023 |
| DB 10 | Cults | https://cults3d.com/ | 30 July 2023 |
| DB 11 | CGtrader | https://www.cgtrader.com/ | 30 July 2023 |
| DB 12 | TurboSquid | https://www.turbosquid.com/ | 30 July 2023 |
| DB 13 | 3D export | https://3dexport.com/ | 30 July 2023 |
| DB 14 | Free3D | https://free3d.com/ | 30 July 2023 |
| DB 15 | Redpah | https://www.redpah.com/ | 30 July 2023 |
| DB 16 | Zortrax | https://zortrax.com/ | 30 July 2023 |
| DB 17 | Creality cloud | https://www.crealitycloud.com/ | 20 September 2023 |
| DB 18 | Thangs | https://thangs.com/ | 20 September 2023 |
| DB 19 | sketchup 3D warehouse | https://3dwarehouse.sketchup.com/ | 20 September 2023 |
| DB 20 | Creazilla | https://creazilla.com/ | 20 September 2023 |
| DB 21 | Threeding | https://www.threeding.com/ | 20 September 2023 |
| No | Prosthetic Device Name | Link |
|---|---|---|
| 01 | Knick’s Prosthetic Finger v3.5.5 | https://www.thingiverse.com/thing:1340624, accessed on 30 July 2023 |
| 02 | Flexy Hand 2 | https://www.thingiverse.com/thing:380665, accessed on 30 July 2023 |
| 03 | Raptor Reloaded by e-NABLE | https://www.thingiverse.com/thing:596966, accessed on 30 July 2023 |
| 04 | AH- Partial Finger Prosthetic | https://www.thingiverse.com/thing:471755, accessed on 30 July 2023 |
| 05 | PROSTHETIC THUMB H.A. | https://www.thingiverse.com/thing:2565563, accessed on 30 July 2023 |
| 06 | e-NABLE Phoenix Hand v2 | https://www.thingiverse.com/thing:1453190, accessed on 30 July 2023 |
| 07 | Cathy’s Lucky Fin V3 | https://www.thingiverse.com/thing:4902137, accessed on 30 July 2023 |
| 08 | Flexibone Prosthetic Hand 2019 | https://www.thingiverse.com/thing:3962905, accessed on 30 July 2023 |
| 09 | Cyborg Beast | https://www.thingiverse.com/thing:261462, accessed on 30 July 2023 |
| 10 | Roth Hand (Progressive and Independent Finger Movement) | https://www.thingiverse.com/thing:220942, accessed on 30 July 2023 |
| 11 | Robohand | https://www.thingiverse.com/thing:305160, accessed on 30 July 2023 |
| 12 | Ody Hand 2.1 | https://www.thingiverse.com/thing:262930, accessed on 30 July 2023 |
| 13 | Flexy-Finger Prosthesis | https://www.thingiverse.com/thing:693429, accessed on 30 July 2023 |
| 14 | The Osprey Hand by Alderhand and e-Nable | https://www.thingiverse.com/thing:910465, accessed on 30 July 2023 |
| 15 | Talon Hand 3.0 | https://www.thingiverse.com/thing:229620, accessed on 30 July 2023 |
| 16 | Kinetic Finger | https://www.thingiverse.com/thing:1737001, accessed on 30 July 2023 |
| 17 | BioMech Finger Prosthesis (Index Left Hand) | https://www.thingiverse.com/thing:6202389, accessed on 30 July 2023 |
| 18 | Second Degree Hand | https://www.thingiverse.com/thing:300499, accessed on 30 July 2023 |
| 19 | Flex Lok Finger | https://www.thingiverse.com/thing:5499514, accessed on 30 July 2023 |
| 20 | Dynamic finger prosthesis | https://www.thingiverse.com/thing:498335, accessed on 30 July 2023 |
| 21 | Hollies hand V5 | https://www.thingiverse.com/thing:794079, accessed on 30 July 2023 |
| 22 | e-Nable Raptor Hand Lock | https://www.thingiverse.com/thing:1750858, accessed on 30 July 2023 |
| 23 | Aline’s Index | https://www.thingiverse.com/thing:4757371, accessed on 30 July 2023 |
| 24 | Flexy Index | https://www.thingiverse.com/thing:4845022, accessed on 30 July 2023 |
| 25 | Rainbow Phoenix | https://www.thingiverse.com/thing:4632992, accessed on 30 July 2023 |
| 26 | Falcon Hand V2 | https://www.thingiverse.com/thing:603039, accessed on 30 July 2023 |
| 27 | BIOT hand prosthesis | https://www.thingiverse.com/thing:1388216, accessed on 30 July 2023 |
| 28 | Solo Finger Pen | https://www.thingiverse.com/thing:2122752, accessed on 30 July 2023 |
| 29 | Kinetic Hand | https://www.thingiverse.com/thing:4618922, accessed on 30 July 2023 |
| 30 | “Spock” Basketball Prosthetic Hand | https://pinshape.com/items/24569-3d-printed-spock-basketball-prosthetic-hand, accessed on 30 July 2023 |
| 31 | V.2 Flex Fingers, Swivel Thumb Prosthetic Hand | https://pinshape.com/items/16478-3d-printed-v2-flex-fingers-swivel-thumb-prosthetic-hand, accessed on 30 July 2023 |
| 32 | BioMech Finger Prosthesis (Index Right Hand) | https://www.printables.com/model/572873-biomech-finger-prosthesis-index-right-hand, accessed on 30 July 2023 |
| 33 | Ody Hand | https://3d.nih.gov/entries/3DPX-001010, accessed on 30 July 2023 |
| 34 | Raptor Hand | https://3d.nih.gov/entries/3DPX-000996, accessed on 30 July 2023 |
| 35 | K1 Hand | https://3d.nih.gov/entries/3DPX-020271, accessed on 30 July 2023 |
| 36 | Ody Hand | https://3d.nih.gov/entries/3DPX-020274, accessed on 30 July 2023 |
| 37 | Talon Hand | https://3d.nih.gov/entries/3DPX-020273, accessed on 30 July 2023 |
| 38 | Kinetic Hand | https://3d.nih.gov/entries/3DPX-020261, accessed on 30 July 2023 |
| 39 | Osprey Hand | https://3d.nih.gov/entries/3DPX-020262, accessed on 30 July 2023 |
| 40 | e-NABLE Phoenix Hand v3 | https://3d.nih.gov/entries/3DPX-020260, accessed on 30 July 2023 |
| 41 | Cyborg Beast | https://3d.nih.gov/entries/3DPX-020267, accessed on 30 July 2023 |
| 42 | e-Nable—YuLia Custom hand | https://www.youmagine.com/designs/e-nable-yulia-custom-hand, accessed on 30 July 2023 |
| 43 | MULTIHAND 3.0 | https://www.youmagine.com/designs/multihand-3-0, accessed on 30 July 2023 |
| 44 | MCP Driver (Naked Prosthetics) | https://grabcad.com/library/mcp-driver-naked-prosthetics-1, accessed on 30 July 2023 |
| 45 | Hero Hand UPDATE—Bionic prosthetic hand | https://grabcad.com/library/hero-hand-update-bionic-prosthetic-hand-1, accessed on 30 July 2023 |
| 46 | T-hook: Prosthetic Design for 3D Printing | https://www.instructables.com/T-hook-prosthetic-design-for-3D-printing/, accessed on 30 July 2023 |
| 47 | Empower: The Aquatic 3-D Printed Prosthetic | https://www.instructables.com/EMPOWER-the-Aquatic-Prosthetic/, accessed on 30 July 2023 |
| 48 | The Paraglider | https://hub.e-nable.org/s/e-nable-devices/wiki/The+Paraglider, accessed on 30 July 2023 |
| 49 | Flex Finger | https://hub.e-nable.org/s/e-nable-devices/wiki/Flex+Finger, accessed on 30 July 2023 |
| Category | Criteria | Description |
|---|---|---|
| Presentation | Name | A proper name, not just a generic one like prosthetic hand |
| Graphics | Provides detailed graphics | |
| Description | Detail description | |
| Availability | Licensing | Proof of open-source licensing |
| Print files | User must be able to download the files | |
| Design files | Possibility to edit the design files | |
| Documentation | Manufacturing guides | Present at least in part the print settings |
| Assembly guides | Present at least in part the assembly process | |
| Tutorials | Present a guided text and image instruction or provide video tutorials | |
| Community forum | Have a community bulletin board or a means of communicating feedback and exchange messages with the interested groups. | |
| Technical | A sound design | Must adhere to engineering common sense in terms of assembly techniques |
| Version control history | Must have prior stable versions | |
| Practical application | Must be suitable to wear and provide realistic capability | |
| Research | Literature | Be present in research studies |
| Case studies | Must be present in case studies | |
| Research stage | Must have surpassed the stage of technical testing and moved on to human testing | |
| Validation through Online presence | Appear in results of reputable databases |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Răduică, F.-F.; Simion, I.; Enache, I.-C.; Valter, E.N.; Naddeo, A. A Perspective on Rehabilitation Through Open-Source Low-Cost 3D-Printed Distal to the Wrist Joint Transitional Prosthetics: Towards Autonomous Hybrid Devices. Machines 2024, 12, 889. https://doi.org/10.3390/machines12120889
Răduică F-F, Simion I, Enache I-C, Valter EN, Naddeo A. A Perspective on Rehabilitation Through Open-Source Low-Cost 3D-Printed Distal to the Wrist Joint Transitional Prosthetics: Towards Autonomous Hybrid Devices. Machines. 2024; 12(12):889. https://doi.org/10.3390/machines12120889
Chicago/Turabian StyleRăduică, Florin-Felix, Ionel Simion, Ioana-Cătălina Enache, Elena Narcisa Valter, and Alessandro Naddeo. 2024. "A Perspective on Rehabilitation Through Open-Source Low-Cost 3D-Printed Distal to the Wrist Joint Transitional Prosthetics: Towards Autonomous Hybrid Devices" Machines 12, no. 12: 889. https://doi.org/10.3390/machines12120889
APA StyleRăduică, F.-F., Simion, I., Enache, I.-C., Valter, E. N., & Naddeo, A. (2024). A Perspective on Rehabilitation Through Open-Source Low-Cost 3D-Printed Distal to the Wrist Joint Transitional Prosthetics: Towards Autonomous Hybrid Devices. Machines, 12(12), 889. https://doi.org/10.3390/machines12120889








