Abstract
Due to serious challenges in the healthcare sector, high expectations are placed on the use of assistive robotics. However, only a few systems are currently commercially available. Key challenges in the automation of care activities concern the identification and robust mediation of medical and nursing standards as well as the distribution of agency between caregivers, robots, and patients. With regard to successful mediation of this relational framework, this research aims to identify (1) prerequisites for the implementation and use of robots, (2) potential areas of application as well as ethical considerations, and, finally, (3) requirements for the design of human–robot interactions (HRI) within inpatient elderly care settings. Using a qualitative research approach with semi-structured interviews, a total of 19 health professionals were interviewed in two constitutive studies. The results illustrate that robotic assistance is expected to provide potential relief in various application areas. At the same time, there was a great need for measures that support professionals in their responsibility for the care process and consider the professional values of care in the interpersonal relationship. To ensure high acceptance and use of robotics in care, its capabilities, role models, and agency must be increasingly aligned to professional standards and values.
1. Introduction
Evidence from the COVID-19 pandemic clearly demonstrated the central importance of the care sector in the provision of healthcare. At the same time, problems within this sector became apparent, too; some of which have existed for decades. Most of these problems can be traced back to the pressing shortage of labor. Although there has been an increase in employment in recent years, the global shortage of health professionals now stands at 5.9 million [1]. Moreover, due to the aging of the profession, an additional 4.7 million (17%) nurses are expected to retire over the next 10 years. In total, the global shortage of health professionals is, therefore, expected to reach 10.6 million by 2030 [2].
Equally important as the demographic effects in connection with the predicted shortage of skilled workers are the working conditions, which have a significant influence on the recruitment of young professionals as well as turnover in this occupational field. These working conditions include an accumulation of different working strains caused by the understaffing in care facilities, the increasing delegation of medical tasks, the increased guidance and supervision of service and assistance staff, as well as a considerable bureaucratic documentation burden [3]. As a result of the associated high psychological and physical burden, caregivers are exposed to an increased health risk for the occurrence of musculoskeletal disorders, cardiovascular diseases, sleep disorders, and other psychological disorders (e.g., burnout) [4,5]. In addition, atypical working hours have a significant impact on working life [5]. According to a representative survey for the DGB-Index Gute Arbeit [6], 78% of the health professionals surveyed assume that they will be unable to maintain their occupation until retirement.
Despite various attempts to improve working conditions in the care sector as part of political reforms and recruitment campaigns, the use of technical assistance systems is becoming increasingly important. There are great expectations for the use of robotic assistance systems in care, which are intended to relieve staff of physically and mentally demanding routine tasks and to support and promote the independence of patients.
1.1. Robotics in Healthcare and Caregivers’ Perspective
Research and development on robotic assistance in healthcare dates back to the 1980s [7]. As a result of the various efforts, a large number of different systems have been developed today for a wide variety of applications. Robotic systems are currently used primarily in the context of hospitals. Higher occupancy rates as well as architectural requirements to create the necessary operating environments form the essential basis for efficient and economical use [8,9,10]. Areas of application include surgery, logistics, therapy, and telemedicine [10,11].
With regard to the care sector, it must be noted that the use of robotics is primarily investigated within the context of research and development projects. In sum, most of these systems, however, are still at the prototype and development stage, while only a few are already commercially available [12,13]. Potential areas of application with regard to the target group of healthcare professionals concern patient mobilization and hygiene (e.g., RIBA, Elevon, Roboticbed, RobotBathtub); feeding assistance (e.g., My Spoon, obi, bestic); cleaning and disinfection (e.g., UVD Robot); material and medication management (e.g., SeRoDi, Moxi, Lio); remote monitoring and emergency detection (e.g., Double, Beam); liquid delivery, reminder, and monitoring (e.g., Care-O-bot); or cognitive, emotional, and physical therapy services as well as socialization and entertainment (e.g., Zora, Pepper, Paro).
Studies on the potential effects of robot use on the work environment and job satisfaction have already identified both positive and negative effects [14]. Positive effects of robot use are specifically identified in reducing physical demands of heavy lifting activities [15], providing cognitive and social support to people with dementia, or reducing workload by monitoring vital signs, alerting in case of emergency, reminding patients of medications and appointments, navigating and escorting individuals, and counseling patients and family members to promote self-management skills [16]. In contrast, negative effects exist primarily when the use of the robot results in additional work for the healthcare professionals. Such a burden exists when the setup of the robot requires a substantial amount of time and effort, when the use of the robot must be monitored, or when the human–robot interaction (HRI) with the care recipients must be mediated [17,18]. In addition, effects related to professional values as specific standards for action in care and nursing are also addressed. These relate, for example, to ethical dimensions such as integrity (patient safety), dignity, autonomy, caring, and distributive justice [14,19,20,21]. In this respect, there are indications that reservations about the use of robots exist, in particular, for activities that require direct (physical) contact with the care recipient, necessitate a high duty of care for patient safety, or serve to satisfy elementary emotional needs [16,22]. Further effects of the use of robots also relate to the reconfiguration of the interpersonal relationship between caregiver and care recipient [15,22] as well as the associated effects on work identity [14,23] or employment opportunities [16,24].
The perceived usefulness as well as the acceptance of robots thus depend on multiple factors. In addition, age, education, gender, cultural background, the institutional setting (e.g., nursing home or residence), the occupational group (nursing assistant, nurse, or management), and the perspective of colleagues play prominent roles [24,25]. Moreover, technical and functional factors such as appearance, size, adaptability, safety, accessibility, usability, and practical utility also play important roles. Finally, several studies suggest that knowledge about and experience with robots has a significant impact on evaluation and acceptance [26,27].
In sum, we can state that the application of robotics in care is not merely a technical mediation of care work but can fundamentally change the relationship of healthcare professionals to the care recipient, to their work environment, and to their work identity. In this context, several approaches have already been developed to conceptualize this reconfiguration of care work through the use of robotics both from a normative perspective of professional values and ethical considerations as well as from the relationship of robot performance to the requirements of care intervention goals [12,14,28]. In this respect, these approaches provide an opportunity to consider the type and role of robotic activities, the required robotic capabilities, and the impact of robotic use towards the goals and normative standards of the care activity early in the development process. Although these approaches constitute an important prerequisite for a generic development of robots in the field of health, it remains an open question how the distribution of actions and responsibilities should be organized within the care intervention and which requirements arise from this for the design of the HRI in the relationship between caregiver, robot, and the care recipient.
The present study addresses these research gaps and, therefore, aims at identifying not only generic implementation requirements and potential tasks for robot use, but also at addressing the concrete interaction requirements between humans and robots in the relationship of caregiver, robot, and care receiver.
1.2. Objectives
This article summarizes the results of a requirements analysis with healthcare professionals. In two consecutive studies, the basic requirements for the use of robots in the inpatient care context were examined. The studies aimed at (1) the identification of prerequisites for robotic implementation and the use in inpatient care settings as well as (2) potential application areas for robotics in general and ethical considerations (study I). Moreover, we aimed to identify (3) basic requirements for HRI and to concretize those in exemplified interaction sequences (study I and study II). These aims and the according approach are summarized in Figure 1. In the following, the methodological design as well as the central results for the two studies are presented and discussed.
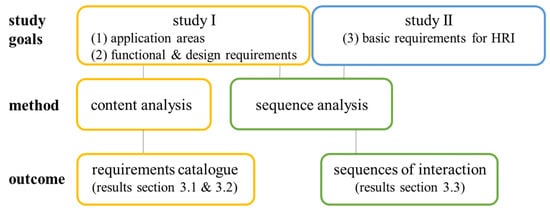
Figure 1.
General procedure, aims, methods, and outcome of analyses of the two consecutive studies.
2. Materials and Methods
Both studies were designed as online studies in order to minimize face-to-face contact in view of the COVID-19 pandemic and to be able to respond flexibly to the time resources of the participants. Both studies used a qualitative approach by means of semi-structured interviews (interview guidelines are provided as Supplementary Materials).
2.1. Recruitment
For a detailed investigation of the presented objectives, we selected a study sample that included healthcare professionals with and without robotics experience. The recruitment of healthcare professional without robot experience was based on existing contacts with long-term care facilities of the Geriatrics Research Group of Charité Universitätsmedizin Berlin and the Institute of Psychology of Humboldt–Universität zu Berlin. In addition, to identify study participants with robot experience, an internet search was conducted as a first step. On the one hand, the focus was on the websites of nursing home providers who reported the use of a robot in their facility. On the other hand, online articles from municipal newspapers that reported on the use of robotics in a nursing home were used. In a second step, we contacted the identified facilities, presented the research project to the facility management, and asked to forward the study information to the healthcare professionals responsible for the use of the robot in the facility. Study participants were recruited from a total of eight nursing homes. Table 1 provides an overview of the distribution of recruited study participants according to the characteristic of prior experience with robots.

Table 1.
Number of participants without and with robotic experience.
2.2. Participants
For the first study, the inclusion criteria of participants were as follows: (1) healthy adults aged 18 years or older, (2) employment as a health professional (including registered nurses, nursing assistants, physiotherapist and occupational therapists, social workers, and managers), and (3) half of the participants should have previous experience with robotics. A total of 16 participants were included in the study (12 care workers, 2 social workers, 1 therapist, and 1 manager). Due to their respective health care professions, all participants had experience in long-term care for elderly and dependent people with a wide range of health conditions requiring inpatient care. The mean age of the participants was 46.4 years (SD = 14.7 years; min = 21 years; max = 70 years). Most participants were women (n = 12). The average work experience, including time in education, was 19.8 years (SD = 14.4 years; min = 1 year; max = 42 years). An equal distribution of participants with and without robotics experience could be realized (n = 8 each). Seven persons with robotics experience indicated experience with the socially interactive robot Pepper from SoftBanks. One person reported experience with the telepresence robot James from the company RobShare. All participants with robotics experience in their own facility reported that the robotic systems were primarily used by social workers and therapists. Main fields of application were memory training, physical activation, entertainment, or telepresence communication between residents and their relatives.
For the second study, we recruited three participants for an in-depth interview. This interview aimed at further refining the sequence analyses of HRI that were deduced from study I. Participants were recruited based on two conditions: (1) healthy adults aged 18 years or older, (2) employment as a health professional (see inclusion criteria of the first study). We originally aimed for a larger sample size (n = 5; oriented on usability studies to identify gaps in existing systems or, in our case, sequence analyses.). However, recruitment was limited due to the COVID-19 pandemic. Original and actual sample size are very small, which is, however, considered sufficient as they are used for exploratory in-depth analyses. All participants were female with a mean age of 35.3 years (SD = 6.4 years; min = 28 years; max = 39 years). One participant was working as a care worker; the other two were employed as managers in care facilities with backgrounds as professional caregivers. One of the three participants had already gained robotic experience through her workplace (Pepper robot).
2.3. Procedure
The data collection and evaluation procedure were carried out consecutively. A temporal outline of the study procedure is presented in Figure 2. First, study I was conducted. Based on the results of study I, study II was conducted. The results from study I and II were used in combination for the creation and refinement of specific sequence models for HRI. The entire data collection ran from July 2020 to May 2021.
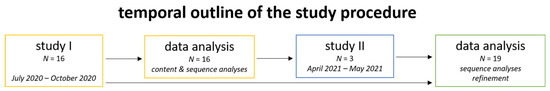
Figure 2.
Temporal outline of the study procedure.
For study I, participants were first contacted by telephone and informed about the purpose and procedure of the study. After formal consent, participants received a link with access to an online questionnaire (visit 1). Completing the questionnaire took about 15–20 min. Subsequently, appointments were made for the qualitative interviews (visit 2), which were conducted as online interviews due to contact restrictions related to the COVID-19 pandemic. The video conferencing service DFNconf of the German Research Network was used to realize the online interviews. The interviews were recorded, and the audio file was saved.
In visit 1, participants were asked about socio-demographic data (age, gender) as well as their professional title and duration of employment by means of an online questionnaire. In addition, participants were asked about their burden of care using three questions about emotional, cognitive, and physical stress.
In visit 2, participants were first informed about the interview purpose, and informed consent was obtained for them to be recorded. In order to develop a common understanding of robotics and to eliminate any bias towards robots appearing in the media, interviewees were given a brief overview of the use of robotics in various societal applications as well as in healthcare. This was followed by a guideline-based interview about possible tasks and areas of application for robotics in the care context as well as the associated development and design requirements. Since both caregivers and social care workers with and without robotics experience took part in the study, slightly modified interview guidelines were issued for both groups. The interviews lasted approx. 60 min (SD = 12 min; min = 46 min; max = 101 min). For taking part in the online questionnaire and the interview, participants received 20€ for compensation. In addition to the recording, the main contents were documented in an interview protocol. The recordings were later used to verify and complement the protocols.
For study II, participants were informed about the purpose and procedure of the interview via e-mail. If necessary, any questions that arose were also answered by telephone. After formal consent, participants received a link for the online interview. This time, Zoom was used as conference service tool, and no recordings of the interviews were made. First, a general introduction into the to-be-applied method of sequence analysis and objectives of this approach was given. Next, ten potential tasks for robotic support in healthcare were presented (based on study I, see Figure 7). Out of the ten, the three most important tasks should be selected for robot deployment. The selected ones were discussed in-depth. During the interviews, one interviewer and one transcript writer attended. Both had the opportunity to ask follow-up questions. To support the interviews visually, Miro—an online collaboration platform—was used. The interviews lasted approx. 60 min (SD = 8 min; min = 55 min; max = 70 min). Participants were compensated with 15€.
2.4. Addressed Topics of the Semi-Structured Interviews
Four main topics were addressed in study I. As mentioned above, slightly modified interview guidelines were designed for the two groups of healthcare professionals with and without robotics experience.
The first set of questions aimed to gain an overview of the daily structure of routine activities from the respective professional perspective in the inpatient setting. Since this section also served to open the interview, simple questions were asked, which primarily had a “warm-up” function [29]. This was intended to allow interviewees to engage with the topic and create a natural conversational situation.
In the second set of questions, the focus was on those routine tasks in which the interviewees would appreciate assistance. A distinction was made between activities that must be performed by a qualified healthcare professional, activities that do not necessarily require a qualified healthcare professional, and all other everyday activities. First, the questions were to be answered generally in terms of the desire for assistance. In a second step, questions were explicitly asked with regard to the possibility of robotic assistance. In this context, requirements for the design of a robot and its functionalities as well as HRI were discussed.
The third set of questions focused on exploring essential requirements for the external and functional design of a robot with respect to the target group of people in need of care.
For the group of participants with a robotic background, a further set of questions was discussed, which dealt with the respective areas of application of the robot, the experiences in handling it, as well as the resulting requirements for further development.
At the end of the interview, interviewees were asked if they had missed any important aspects of the topic that had not been considered in the preparation. This question was again intended to stimulate the generation of information and increase the openness of the interview [29].
To further specify the results of study I, a second study was conducted to identify the most relevant tasks for robotic use (top 3) and to further detail the specific interactions between robot and healthcare professionals as well as caretakers when performing those tasks (sequence analyses). For this purpose, the identified task pool from study I was presented to the interviewees who were asked to select the three most important ones. Second, concrete interaction sequences for the selected tasks and requirements for the robot use were elaborated in more detail (again based on previous results of study I). A particular focus was on concrete interaction channels which the robot should use to engage with the users.
For better comparability of the interviewees’ answers, most questions in both studies were asked in identical or similar form to further ensure comparability between all interviews [29].
2.5. Data Analysis
All study data (including voice recordings) were pseudonymized and treated confidentially. The interviews of study I were evaluated in the form of summary protocols. To ensure an accurate representation of the interviewees’ responses, the protocols were reviewed and supplemented with audio material according to the principle of researcher triangulation. The interviews of study II were documented accordingly. Additionally, results of the second study were captured graphically by using the online collaboration platform Miro. Content was developed together with the participants, and changes were directly documented in Miro by the interviewer and the transcript writer. In line with the data minimization principle of the General Data Protection Regulation (GDPR), audio recordings were not considered necessary for the analyses, as, e.g., no content analysis according to Mayring was planned. The collection of personal information was, therefore, limited to the Miro documentation. In this case, however, audio recordings were not considered necessary as study II was more of an interactive workshop than a traditional qualitative interview. All interviews were conducted in German. For the report of the results, they were translated into English.
2.5.1. Content Analysis
For data analysis, we conducted a summary content analysis according to Mayring [30]. In view of the targeted research objective, the analysis included the paraphrasing of content-relevant text passages in the interviewees’ statements. Based on this, the targeted level of abstraction was determined, and the paraphrases were generalized under this level. Subsequently, a first reduction of paraphrases with the same sense was carried out by means of selection. In a further reduction step, paraphrases were bundled and integrated at the targeted abstraction level. For the purpose of ensuring data quality, these analysis steps were carried out by a total of four trained researchers (the research team is introduced further in the author contribution section). The formation of categories in the context of paraphrasing, generalization, and reduction involved three iterations with multiple material reviews. The analysis steps of paraphrasing and generalization were performed using the qualitative data analysis software Atlas.ti 9. The analysis steps of generalization and reduction were based on MS Excel 2016. A total of 39 codes were assigned, and 2304 citations were classified as relevant. To determine the degree of agreement between coders, the inter-rater reliability (IRR) was computed using Krippendorff’s Cu-Alpha (cuα). The coefficient can take values between 0 (low IRR) and 1 (high IRR). The four researchers achieved a cuα of 0.726. The results of the summary content analysis were grouped into basic requirements for implementation and use, system design and automation activities, and potential application areas.
2.5.2. Sequence Analysis
Based on study I and II (n = 19), sequence models were created to specify interaction requirements for the tasks that were considered for robot use by healthcare professionals (e.g., results of the sequence analyses in Figures 8–10). For the creation of sequence models, four aspects had to be determined [31]: (1) The intent of the sequence had to be formulated. This serves as a basis to constantly check during the further creation of the sequence, whether it still serves the actual purpose or whether individual points are not related to the stated intent. (2) The users involved in the sequence had to be identified. Based on our data, this meant determining whether the robot performs the action only with healthcare professionals, only with care recipients, with both, or in combination with a third party (e.g., relatives or visitors). In Figures 8–10, the users are listed on top of the sequences with dark green boxes. (3) The single steps of the users’ activities had to be identified and listed in chronological order (see the light blue boxes in Figures 8–10). A detailed description of action aims at identifying what needs to be done to achieve the predefined goal and at which points interactions between the individual users and the robot take place. To highlight interactions more clearly, we used arrows between the involved users in the sequence analyses (see the connections with red lines between some boxes in Figures 8–10). Furthermore, we used loops to illustrate which steps are repeated several times in the same order. In Figures 8 and 9, these loops are realized with orange boxes and arrows. (4) Finally, triggers were required to clarify who or what starts an action (e.g., pressing a button or a specific time) and the criteria that determine the successful task fulfilment based on the intent definition. In Figures 8–10, the triggers are presented with green boxes and an indication of whether it is a start or end trigger.
The collected data from study I was used to create the sequence models according to the four aspects mentioned above. The defined sequence analyses were then presented to the participants of study II. The participants were asked to select the three most important application sequences from all the application sequences presented. These were discussed with the participants in a further step and gradually expanded. Hence, the presented sequence models are based on a total of 19 interviewed participants.
3. Results
The results of the content and the sequence analyses can be divided into three thematic areas. In the first part, basic requirements for the implementation and use as well as the design of HRI are presented. In a second part, we present potential areas of application with particular tasks for robotic assistance as well as requirements for the level of robot autonomy. Finally, the third part comprises our results on the design of human–robot collaboration in three exemplary sequence analyses.
3.1. Prerequisites for Robotic Implementation and Use
This part summarizes the statements that focus on the requirements for the introduction and use of a robotic system in an inpatient care setting (see Figure 3). A first area of requirements consists in the importance of specifying the robot’s application profile in advance with the facility. In this context, the results showed that an early discussion of the individual expectations of use, the actual possibilities of use, and the possibility of making one’s own experiences with the potential robotic system are essential prerequisites for the acceptance and use of robotic systems in care: “[…] I would appreciate, for example, that a robot will come to our facility and we can just take a look at it for a day and then say, it works or it doesn’t work.” (Int-L/nurse).
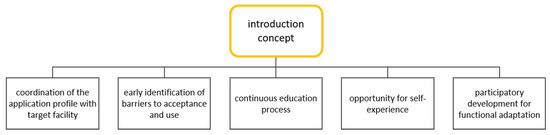
Figure 3.
Requirements for the successful introduction of a robot in an inpatient care facility.
In line with this, an early identification of potential barriers to acceptance and use in the target groups as well as their continuous education regarding the role and tasks of the robot can be named as a second area of requirements. In this context, four key requirements for reducing such barriers were identified: (1) The individual prerequisites for using a robot should be determined at an early stage (both in the group of care recipients and healthcare professionals): “So you should really check in advance what level of affinity there is for robotic systems or technology. […] For whom is it a pleasure and for whom is it an imposition?” (Int-J/nurse). (2) Related to this, information and education of the target groups should be designed as a continuous process in order to be able to reduce usage and acceptance barriers due to insufficient technology and robotics experience in the long term. In this context, one respondent stated, “I also have to say that there are still staff members in our care facility who don’t want to work with it. Or there are also caregivers who ridicule the idea. And then, of course, it’s always your turn and you have to explain the advantages of the [robot label] to the employees […]” (Int-N/therapist). (3) In view of the target group of care recipients, a familiarization phase should be provided in which the robot accompanies a healthcare professional in the daily routine similar to a trainee or new employee: “If the robot, like a trainee or like someone who is to be trained, would accompany you in the course or daily routine, the familiarization would succeed relatively well. But putting the robot into the running routine, I think, would be difficult.” (Int-C/nursing assistant). (4) Finally, the group of interviewees with robotics experience in particular emphasized that the staff should be involved in the development and design of the functions and contents. This is of particular importance because current systems are often only rudimentarily adapted to specific user requirements, and these can vary across facilities. In this context, the results show that a long-term participatory development approach comprises great advantages for the further development as well as the successful use of the systems: “In the beginning we got [robot label] raw, now we have a book of requests of what we imagine how to make it even better, in terms of software improvements. So now it’s more according to our wishes or the wishes of the guests.” (Int-Q/nurse).
3.2. Areas of Application and Ethical Considerations
3.2.1. Potential Areas of Application and Collaboration Requirements
We identified 9 potential areas of application with an overall of 25 associated subtasks (see Figure 4), which will be explained in more detail in the following.
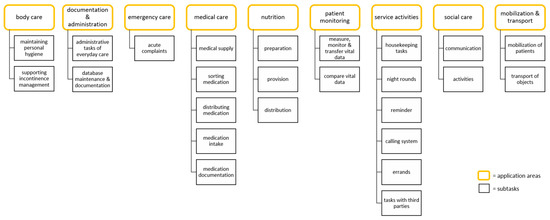
Figure 4.
Identified application areas with their associated subtasks.
The application area of body care summarizes tasks in which the robot can support basic care activities in the inpatient setting. On the one hand, the interviewees named tasks for maintaining personal hygiene (e.g., washing/showering immobile patients with robot support as some sort of lift). On the other hand, tasks in supporting incontinence management were mentioned, such as changing incontinence material, emptying catheters, or helping to balance excretory function. The interviewees rated robotic assistance in washing/showering intimate body areas and in dressing and undressing patients as a concern: “For the patient, (...) it is a no-go if [the robot] (...) [has to] wash a patient against his will, for example, because that is simply a very intimate (...) and (...) vulnerable area that must not be replaced by robotics.” (Int-J/nurse).
The area of documentation and administration summarizes activities for the robot, which relate to the administrative tasks in everyday care. One respondent stated, “Such a robot that answers the phone would of course also be something nice. (...) It would simply give people the feeling that it is now there and that it is recording all their complaints and aches and pains and that someone will definitely get back to them.” (Int-D/nurse). They also mentioned (nursing) activities such as sorting and filling files and helping with bookkeeping. There was also a desire for the robot to assist with updating the patient database and documenting care planning (e.g., helpful for when a new patient is transferred to the service or is admitted for the first time). The interviewees emphasized that the robot should receive an introduction before taking over these activities.
The application area emergency care summarizes tasks in which the interviewees would like support in emergencies or in the event of acute complaints by the care recipients. This applies, for example, for tasks in which the robot immediately forwards the alarm signal to the healthcare professionals in the event of an emergency. In order to fulfill these tasks, the robot should be able to assess the degree of danger/emergency, on the one hand, and to define an appropriate response in advance, on the other. For this reason, the interviewees exclude robotic assistance for tasks in which dangerous situations/emergencies are not detectable, such as aspiration/collapse.
Another application area of activity is medical care. Mostly, tasks in connection with the medication itself were described. The desired assistance by the robot in this task includes both the reminder and control of the medication intake, the sorting and distribution of medications as well as the documentation of medications: “For example distributing tablets, bringing tablets to the client, and reminding the client that the tablet must now be taken with a sip of water (...). In that area it would also be a great relief. In time management, it’s madness.” (Int-K/nurse). In addition, interviewees expressed that the robot could assist in changing medical supplies (e.g., wound materials, compression stockings). By contrast, the injection of insulin was rejected.
The application area of nutrition summarizes tasks in which healthcare professionals may need support in the preparation, provision, and distribution of food and liquids (e.g., meal/drink reminder, accompaniment during food intake, motivation to eat). One interviewee stated, “So especially when the housekeeper prepares food, breakfast, etc. and the robot can bring the food adequately to the places where the clients are, (...).” (Int-K/nurse). Moreover, tasks were named in which a healthcare professional may require additional help, as there are care recipients who need special support. These include assistance, reminding and control with food intake as well as the provision of tube feedings. Reservations existed in particular with regard to the assistance of motivation to eat in the case of people with cognitive impairments and palliative care recipients.
Another area is patient monitoring. It summarizes tasks for the robot, which relate to the process of recording, monitoring, and transferring vital data of care recipients. Examples are assistance in measuring blood pressure, blood oxygen, blood glucose, and body temperature as well as recording sleep duration and sleep quality. This can simultaneously relieve the burden on caregivers during rounds: “Sometimes the rounds are so long that they tie up a specialist (...) and it would be nice if robotics could support this so that the nurse is not tied up for so long.” (Int-J/nurse). Additionally, the interviewees expressed the wish to check other important parameters such as pressure sores, drinking behavior, and well-being of the care recipients. When recording and processing personal vital signs, interviewees always felt it was relevant to consider data protection. In addition, it was conceivable to the interviewees that the robot would compare the measured vital data with reference values and alert the caregivers if the tolerance ranges were exceeded. Forwarding this data to a hospital information system was also conceivable.
Service activities are activities that describe the support of a robot with tasks that are not relevant to nursing but are time-consuming. The interviewees mainly mentioned housekeeping tasks, such as tidying up (patient) rooms, putting the dishwasher in and taking it out, washing and sorting (bed) linen, cleaning and disinfecting surfaces or switching the light/TV on and off. The interviewees could also imagine tasks of night rounds (e.g., providing day clothes for people in need of care). Furthermore, the interviewees mentioned reminder functions such as remembering birthdays or wearing the protective mask. In addition, it was conceivable for the interviewees that the robot could take over tasks that arise from the individual request by the residents ringing the bell (tasks in the residents’ room, e.g., light on/off, TV on/off, picking up something from the floor): “For nervous reasons, I think it would be good if, for example, the patients [sometimes just] rang the bell because they couldn’t reach the remote control (...) that [the robot] checks beforehand what the problem is, why the patient is ringing or you could also send it so that it could say: “Just a moment, we’ll be right there”. That would make things a lot easier. Yes, if it can take pictures of what the patient in room X needs, (...) if you have information in advance and can work calmly on the patient who has an emergency.” (Int-H/nursing assistant). Ringing the bell is further detailed in Figure 9 as “calling system”. Moreover, helping with trips/errands outside the home (e.g., to the doctor, to external care providers, or as a shopping companion) could also be imagined as a task for the robot. In addition, service activities with external persons were also mentioned, for example, greeting and then escorting visitors at the entrance gate. Furthermore, support in contacting relatives via a video conferencing system was mentioned.
The application area of social care describes tasks of robot support for care-relevant activities. In this field of activity, the interviewees not only wanted robot support in activating residents but also in promoting communication among residents. With regard to activation, they mentioned, for example, the use in different care concepts (group occupation, individual occupation, care of dementia patients). With regard to communication, the interviewees expressed tasks that are related to the content design of the care concepts and contribute to the promotion of interaction (e.g., occupation through music or games, physical or cognitive activation). In general, the interviewees wished for the possibility of implementing individual care times for the residents and varied content.
The last application area, mobilization and transport, involves requirements for the robot, which includes tasks for mobilization of patients and transport of objects (e.g., care materials, wound care). Interviewees expressed a desire for robotic assistance in getting up, repositioning, or walking (mobilization) the patient: “Maybe when dressing, when walking, when the residents just need someone to hold on to.” (Int-T/nurse). According to the interviewees, attaching straps, pulleys, and arms to the robot would provide additional assistance with mobilization. However, when performing these tasks, a caregiver should always supervise the robot’s assistance. Furthermore, interviewees mentioned help with material transport, e.g., clothing or hygiene materials for wound care, bandages, etc. (transfer): “I now imagine (...) I transported everything into the room together with the robot, which carried everything. Then, that you sort the things, because I think the first robots won’t be able to see what’s what when you have the (...) in front of you so that they always hand you everything, so that you don’t always have to search for everything. That would be quite cool.” (Int-S/nurse).
3.2.2. Ethical Considerations towards the Automation of Care Activities
Although the use of robots in long-term care was highly advocated and considered a potential relief, there were also some reservations about the automation of care interventions, i.e., the translation of work processes into robot actions that can be performed independently by the respective system without human intervention. On the one hand, several interviewees could imagine a higher level of autonomy for a robot, particularly in pick-up and drop-off services; placing medications; reminding patients of appointments, events, or even eating and drinking; and performing entertainment. On the other hand, there were concerns regarding care interventions characterized by direct physical and emotional interaction with the care recipients. These concerns related to the technical capabilities of a robot to adequately manage the complexity of the care activities as well as the individual needs of the care recipients (see Figure 5). An essential prerequisite in this regard is the adequate detection of the health and emotional state of the care recipient as well as the interventions derived from this. It was difficult for the interviewees to imagine how the various human perceptional skills—which are an essential prerequisite for adequate patient monitoring—could be technically implemented and how a system could be trained to respond for the varied needs and care demands of each patient. In addition to complexity and variability, ensuring patient safety within care interventions was another requirement. Concerns here related in particular to the early detection of hazardous situations and the initiation of necessary measures: “The problems I see are when there is a risk of falling. That a robot might not recognize early enough how it should react to avoid a fall.” (Int-T/nurse).
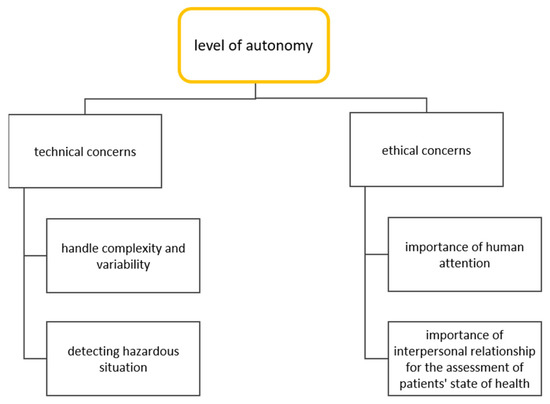
Figure 5.
Overview of the technical and ethical concerns related to the automation of care activities as well as the level of robot autonomy.
Besides technical issues, ethical concerns were also identified in relation to the automation of care activities (see Figure 5). In this regard, interpersonal care activities with physical contact are of particular importance, since the care recipients experience human attention, touch, and physical closeness, which represent essential emotional needs. Overall, the use of robots should not lead to a reduction in direct interpersonal contact between healthcare professionals and care recipients in order to be able to both perceive and satisfy emotional needs: “Because the residents need this emotional support and always need little encouraging words. That is very important, or to express feelings. To express emotional needs. That must not be lost through the use of robots.” (Int-T/nurse).
Finally, concerns were expressed about a predominantly technical mediation of patients’ state of health and the associated effects on healthcare professionals’ competence development and duty of care. Thus, healthcare professionals achieve a holistic impression of the patients’ state of health within the work of interpersonal relationships. At the same time, this relationship provides the framework for continuous development of the necessary skills for professional perception and evaluation of health status and care needs. A reduction of direct interpersonal contact as well as the operationalization and quantification of user characteristics was considered a possible limitation for the development and maintenance of those skills: “I think there’s a danger of focusing too much on these technologies and losing the interpersonal aspect. Because this interpersonal aspect also has to do with the fact that I, as a human being, observe my counterpart and also perceive certain things. If I drop that exorbitantly because I only talk to electronic devices, then I’m no longer in a position to evaluate the situation, because I unlearn that.” (Int-D/nurse).
3.3. Requirements for Human-Robot Interaction and Collaboration in Selected Scenarios
3.3.1. General Requirements for the Design of HRI
In this section, we present our findings on the design requirements for HRI from the perspective of health professionals (see Figure 6). A first set of requirements refers to the external design and appearance of a robot. In the context of promoting acceptance and use, a robot should have a friendly and not frightening appearance. A human-like, infantile design was also evaluated positively, as this can contribute to the promotion of acceptance in the target group of residents (especially according to the view of the interviewees with robotics experience): “I do think that the inhibition level decreases when it’s a little bit human.” (Int-Q/nurse). Another design requirement concerns the surface. For the purpose of direct physical contact between robots and humans (e.g., for mobilization), the surface should be skin-friendly, provide a certain degree of flexibility and be suitable to be warmed up to body temperature. It was emphasized that, especially in the context of mobilization of physically impaired care recipients, technical assistance systems can cause a negative self-perception. An essential requirement would, therefore, be to reduce the machine-like character of the robot through the design in order to promote a positive perception of the physical contact between the robot and the care recipient: “Maybe it should also not be rigid, that it really feels like being lifted by an arm. That it is not something rigid, where the patient has the feeling that it is a machine that is doing it.” (Int-J/nurse).
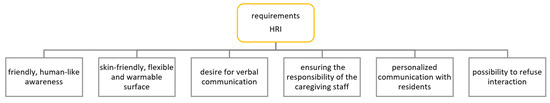
Figure 6.
Overview of the identified HRI requirements.
Various requirements can be summarized in the dimension of interactive capabilities for an assistive robot for inpatient care. Great agreement was found in the desire for verbal communication between humans and robots. Important requirements were reliable speech and intention recognition, human voice timbre, and the possibility of longer dialogues between robot and user: “It’s always a dialogue of two responses. […] And that’s where we would like it to go on. That the dialogues could be longer, that you get four or five sentences as answers.” (Int-M/social worker). In addition, the robot should exhibit a polite etiquette in communicating with all user groups involved. Attributes of this etiquette were described as “friendly and humorous” and “expressing its support character”.
Further requirements in connection with the design of the HRI can be divided according to the target groups of the healthcare professionals and the care recipients. A crucial issue of the group of healthcare professionals was that the responsibility for care activities should remain with them and that this should be considered in the design of the HRI. For example, the opportunities to delegate tasks should be limited in advance, and warnings should be issued by the robotic system if the duty of care for activities is violated by the delegation of a task: “That the robot has some kind of warning function: “That’s not possible””. In addition, during instruction, it should be made very clear that the robot is just a support system and not a substitute for human and responsible action.” (Int-J/nurse). In addition, measures should be taken that should allow caregivers to have insight into autonomous activities of a robot at any time.
Requirements for the design of the HRI towards the group of patients consisted, in particular, in a friendly, polite, and personalized interaction. A robot should be able to identify the patients and address them by name. Furthermore, the robot should be able to provide support and information appropriate to the patient’s daily routine and individual needs. In this regard, one of the interviewees stated that he had the same expectations of a robot as of an employee: “I would almost say the same expectations as for an employee. They have to be empathetic, they shouldn’t be rude in their interactions, and they have to respond to the clients’ feelings and needs.” (Int-K/nurse). Finally, another requirement was the general opportunity to terminate the interaction with the robot at any time.
3.3.2. Requirements for Human Robot Collaboration in Selected Scenarios
The most frequently mentioned tasks for robotic support in study I (see Figure 7) were used as a task pool for participants in study II in the form of sequence analyses. Out of these ten tasks, the following three were selected as most important by interviewees of study II: Reminder, calling system, and mobilization of patients. These were further detailed and analyzed to highlight specific interaction requirements when collaborating with caregivers and patients.
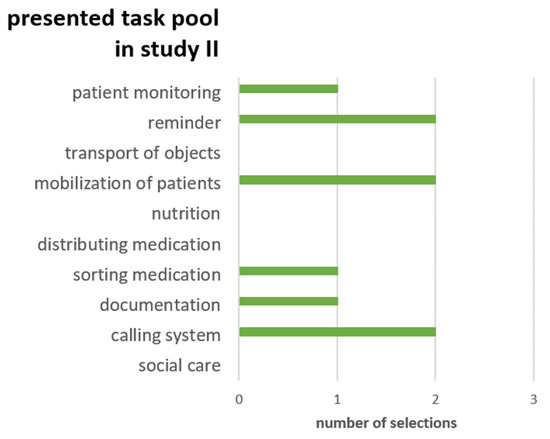
Figure 7.
Task pool presented in study II including number of selections.
Robots should remind people about upcoming events or tasks. This reminder function (see Figure 8) should include care recipient-related (e.g., drinking reminders, reminders for doctor visits, or when to take the medicines) and healthcare professional-related events (e.g., pharmacies orders, appointments, or special medication dispensing). A repeated reminder was perceived as positive because often information gets lost in the stressful daily routine. A function to acknowledge the reminder when the according task is done was therefore felt to be useful. This function was only desired for the healthcare professional-related reminders and is, therefore, only located on the left column in Figure 8. With regard to requirements for the concrete input and output of such reminders, i.e., how should the appointments be entered into the robot and how should the reminders be displayed or expressed to the respective interaction partner, interviewees stated that a reminder is only helpful if it does not cost additional time or resources. For that reason, it was desired that the robot should retrieve the appointments and reminders directly from the existing electronic data processing system (EDP system). The robot should, therefore, not operate separately from existing systems but be integrated into the existing infrastructure. Reminders that arise at short notice or are not retrievable from the existing system (e.g., visit of a patient’s daughter in the afternoon) should either be selectable via presets or implemented via voice input. One important aspect was that the creation of additional reminders can only be done by healthcare professionals. For this reason, an additional interaction between the healthcare professional and the robot is added in Figure 8 before the sequence begins with the start trigger. With regard to the output, the content of the reminder was of major importance. In general, a visual representation was desired. This could be done on the robot or projected from the robot onto the wall. Additional end devices to which the reminders are sent were also conceivable. In the case of relevant reminders, an additional acoustic signal or a voice output should be integrated to reflect the higher relevance. However, data protection must be maintained in the case of sensitive information. In the patient’s room or in the presence of other persons who are not authorized to receive the information, the acoustic output should be disengaged. Face recognition is seen as a prerequisite for such personalized reminder outputs, which was deemed acceptable by the interviewees for this purpose.
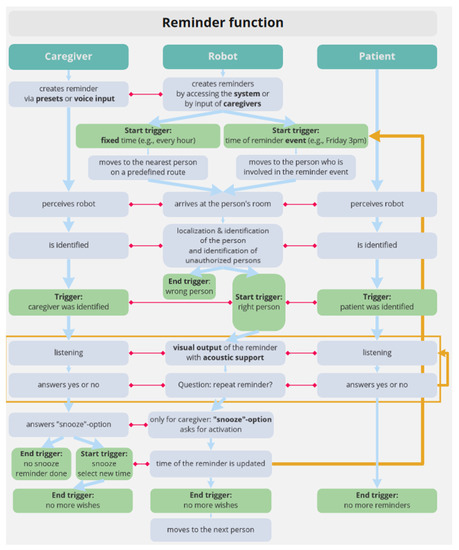
Figure 8.
Sequence model of the reminder function.
The calling system is an elementary component in retirement and nursing homes. Residents can ring a bell to call a healthcare professional when they have a wish or an emergency. The detailed sequence for the calling system is illustrated in Figure 9. One important aspect by the integration of the robot is the coupling of the robot with the existing calling system as differentiating between different buttons would be too difficult for many care recipients. When receiving a call, healthcare professionals can send the robot to check what the call is about. In this case, the healthcare professional is interposed between trigger (patient) and executor (robot). The chronological order of the interaction sequences in Figure 9 highlights the role of the healthcare professional. Optionally, the robot could make rounds at predefined times to take requests or check on patients. In this way, attention would also be paid to people who forget to use the calling system (e.g., because of dementia) or people who are physically limited. During the concrete interaction between robot and patients, all interviewees agreed that a combination of spoken and visual support is desired. A visual support of verbal communication is intended to lead to a better understanding and both hearing and visually impaired patients should easily interact with the robot. To pass information to the caregivers, a video call was perceived as a feasible option. However, feedback to the healthcare professionals was also desired when the task was carried out independently by the robot. For this, a text message, for example, would be sufficient. Regardless of the (non-) successful execution, it is important that the healthcare professional remains informed about the current status.
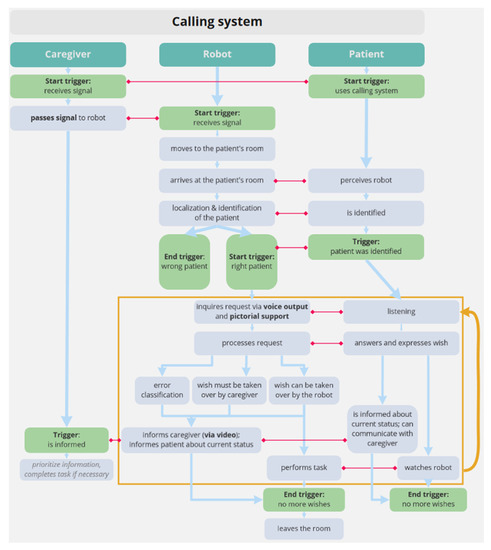
Figure 9.
Sequence model of the calling system.
For mobilization of patients, two specific tasks were considered and discussed. One task for the robot was to transfer a patient from the bed to the wheelchair. The other was to transfer the patient from one place to another. Only the first example is illustrated in Figure 10. For both scenarios, we were at first interested in how these tasks are launched/started. Interviewees indicated that this depends on the presence or absence of a healthcare professional. If the robot and a caregiver are in the same room, a voice command is preferred; otherwise, calling the robot via tablet or a similar device is favored. However, commanding the robot can only be done by the healthcare professional. Since in mobilizing patients the robot is physically very close to the patients (e.g., robot sits the patient up or a patient leaning on the robot while walking), trust in the robot must first be established. In addition to an initial introduction in cooperation with the caregivers, verbal communication during the tasks is considered to promote trust. When transferring patients from bed to wheelchair, the caregivers stated a need to be present at all times to ensure patient safety (see Figure 10). In terms of accompanying patients, emergency situations, such as patient falls, were often addressed, as the caregivers would not be directly involved in these situations. In such situations, the robot should make a direct call to the caregivers and request help. Text messages in emergency situations are clearly rejected as they need a higher visibility.
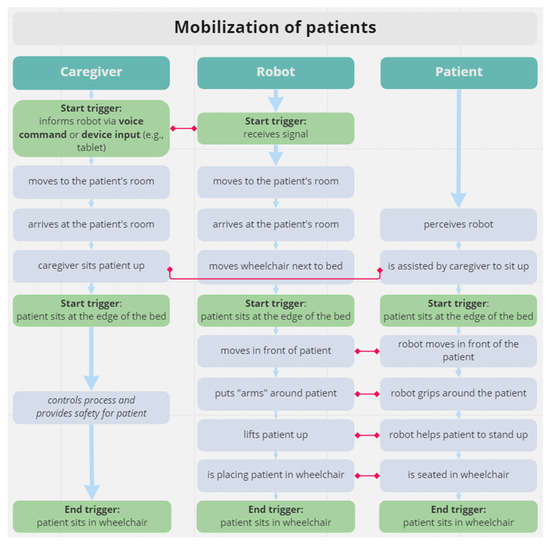
Figure 10.
Sequence model of mobilization of patients. Figure 10 summarizes the results of the survey of healthcare professionals on their individual perceptions of the process of mobilization of a patient with robotic assistance. The illustration indicates that the process of mobilization by a robot involves specific abilities on the part of the patient in order to support the transfer. In this context, the authors emphasize that the characteristics of the robot as well as the mobilization procedure must be checked for patients with significant limitations in their motor abilities.
4. Discussion
The results of the present studies clearly demonstrate that care robots are perceived as a potential relief and support for various tasks in everyday care provision. At the same time, however, it also becomes evident that a number of efforts still need to be made, which we discuss in the following.
4.1. Co-Creation Process as Necessary Prerequisite
The results of our study illustrate that healthcare professionals do not see themselves merely as potential users of robotic assistance systems but want to play an active role in developing them. In this respect, early involvement already in the definition of the application profile is highlighted as an essential prerequisite for a successful development and introduction of robots. This finding is consistent with previous research in the field of co-design approaches highlighting the need to involve potential user groups already in the problem definition stage to determine requirements for the robot’s role and agency as well as the associated technical and functional capabilities in the context of healthcare intervention [12]. Furthermore, another key finding is that the integration of a robot into everyday care should be planned as a long-term process, in the context of which resistance in the addressed user groups must be countered by appropriate education and participation formats. In line with previous studies, our results emphasize the importance of hands-on experience in promoting the acceptance and use of robots. For example, Melkas et al. [32] highlight, in their study on the impact of the introduction of the Zora care robot on the user groups of the elderly and caregivers, that the opportunity for self-experience with the robot as well as the positive reactions of care recipients promoted positive attitudes and motivation to learn the system. Empowering caregivers to successfully use robots also relates to their central role as intermediaries between care recipients and their families, on the one hand, and healthcare providers and services, on the other. Given the growing importance of assistive technologies such as robots in care work, it can be assumed that activities such as advising, setting up, and teaching assistive technologies will become a central part of caregivers’ daily work. Against this background, Sharts-Hopko [33] points to the need to adapt the current curricula for nursing education more closely to technical concepts.
4.2. Key Factors for Potential Areas of Application and the Level of Automation
A second challenge consists in the identification of potential areas of application as well as the organization of the human–robot collaboration related to them. In principle, participants in the current study were able to imagine a wide range of possible areas of application in everyday care. We identified 9 potential application areas with a total of 25 subordinate tasks. These were in line with previous studies, implying that there are no substantial blind spots in the current state of research [21,22,24,34,35,36]. The nine application areas comprised body care, documentation and administration, emergency care, medical care, nutrition, patient monitoring, service activities, social care, and mobilization and transportation. Moreover, our results showed that a higher degree of automation was preferred especially for activities in logistics, administration, and navigation, which are perceived as physically and mentally demanding in everyday work. At the same time, however, we found that there was a restriction to the automation in tasks that require a high level of professional supervision for patient safety and that are characterized by interpersonal physical and emotional relationship. This finding is consistent with previous studies in which professional caregivers rejected the use of autonomous robots in the context of personal care, toileting, dressing, feeding, meeting emotional needs, as well as care in emergency situations or palliative care [16,21,22,24,34,36]. Against this background, three important factors must be considered when determining the potential areas of application for assistive robotics as well as the associated level of automation of care interventions.
First, the high demands on the technical capabilities of autonomous robots to reliably detect, interpret, and respond to care-relevant events. This includes mechanisms for capturing and transmitting health-related data to the systems necessary for the needs-oriented care of a patient. It also includes measures for personalized use of assistive robotics to promote user experience and acceptance. For example, Fiorini et al. [37] identified several technical and functional requirements regarding a robot’s movement, manipulation, perception, decision autonomy, and interaction capabilities. Thus, robots should have the necessary technical capabilities to perceive and plan their behavior in unstructured and dynamic environments so that they can act safely and reliably. Another requirement is a personalized and needs-based approach to robot behavior, which should be based on a user’s individual, health, and cultural characteristics. Such a personalized and needs-based approach requires the integration of different types and sources of data, including sensors on the robot, physiological sensors on the user, a priori and personalized knowledge as a result of a learning system, and clinical data from the end user. Finally, such a personalized and needs-based approach picks up the user in his or her everyday state of mind and enables a robust and pleasant interaction based on intelligent actuators and a multimodal user interface.
A second critical factor covers healthcare professionals’ concerns about the technical substitution of interpersonal relations, which is an essential prerequisite for the promotion and evaluation of individual care goals and the satisfaction of basic emotional needs. This aspect was particularly emphasized by the results of the presented sequence analyses. According to the preferred application scenarios, the focus of human–robot collaboration was primarily on informational support but not on emotional or intimate physical care. Especially, the emotional support of the patient is very important for the caregiver and should, therefore, not be replaced by the robot. Concerns about automating interpersonal relational work are also highlighted by Parviainen et al. [22] with regard to touch-based care. Based on a survey with 3800 professional caregivers, they concluded that the use of autonomous robots is rejected by the majority for touch-based care activities and, in contrast, is preferred primarily for tasks without physical contact. As requirements for the technical conception and design of human–robot collaboration, special attention should, therefore, be paid to the promotion and support of interpersonal relational work. In this context, Parviainen et al. [22], for example, propose a triadic approach of human–robot–human interaction that considers the reciprocity of care activities in technical mediation. Furthermore, capabilities for different levels of remote control or teleoperation should be considered with respect to the specific intervention [12].
Finally, a third factor exists with regard to the respondents’ work identity. The focus here is on the responsibility for the care process as well as the qualification required for this. In this context, the results of both of our studies illustrate that the caregiver is attributed a central role in the initiation and supervision of tasks that were considered suitable for robotic assistance. This allocation of responsibilities values the caregiver as a supervisory instance, who is still responsible and decides on task fulfillment. In addition, this role distribution ensures a transparent process and, therefore, supports caregivers’ situation awareness regarding the entire care process. Keeping caregivers in the loop is, therefore, a key aspect when integrating robots into the daily care routine. These findings are in line with the results of Olatunji et al. [38], who also recommend a permanent involvement of caregivers independent of the robot’s level of automation. Taking these three factors together, it can be concluded that the challenge of potential applications for robotics is that central professional values of care are not yet sufficiently considered in the conceptualization and design of assistive robotics as well as the related models of human–robot collaboration [12,14].
4.3. Key Factors for HRI and Design Guidelines from the Current Study
In application domains that include multiple target groups, different requirements for the implementation of HRI arise for the various user groups. In this respect, there are different requirements for the provision and exchange of information as well as for specific robot qualities. Pigini et al. [36] solved this challenge by providing specific user interfaces for each user group involved—the elderly, their relatives, and caregivers. Derived from the sequence analyses, it is shown that most application areas primarily involve a triadic relationship between a robot, a caregiver, and the patient. Therefore, in contrast to Pigini et al. [36], our target group-oriented design for a successful HRI focuses mainly on caregivers and the elderly. A more detailed examination of the specific interaction scenarios through sequence models revealed, furthermore, three key factors that are required in particular for a successful execution of interactions with the robot.
The first central factor was the integration of the robot into existing information and data systems so that no additional burden is created for caregivers by the need for manual data transfer. In addition to the identified systems, such as the EDP system or the calling system, Christoforou [39] pointed out that key integration examples include hospitals’ enterprise resource planning (ERP) and electronic health records (EHR). In view of the high workload in care facilities and the already known barriers to acceptance and use due to complex technical integration, special attention should be paid to simple implementation and integration solutions.
A second key factor for the successful and easy completion of interaction tasks with the robot was the communication mode. In line with previous studies and the current state of the art, a voice communication mode is required from the robot [40,41]. Previous studies have already examined different factors of voice communication (e.g., voice gender and voice style effects, [42]; or voice accent effect, [43]). Our results provide further insights into the division of in- and output requirements for the communication mode. With regard to the communication input, voice control was considered to be the easiest input format for both caregivers and patients to operate the robot. For this purpose, central requirements consist of reliable speech and intention recognition. With regard to communication output, our results show a preference for a multimodal user interface combining acoustic (speech output is preferred, but sound is also conceivable) with visual elements. A detailed examination of communication channels can already be found in existing taxonomies for HRI classifications [44], which underline the need for a more specific consideration. Especially for the group of care recipients, the design of HRI has to consider age- and disease-related changes in physical (e.g., tactile) and communicative (vision, speech and hearing) abilities. Therefore, further adjustments must still be made with speech-based communication modes (e.g., louder for hearing impaired). In line with that, Pineau et al. [45] reported that a key challenge in the development of their robotic system was to meet the demands on the technology with respect to the varying gait patterns, vocalizations, and hearing abilities of the target elderly population. Beyond that, further requirements with regard to the interactive capabilities of a robot were found. Robotic systems should have both polite and supportive etiquette and personalized and demand-oriented interaction in their communicative behavior [46,47]. Additionally, our results show that for a long-term engagement of the user, a higher flexibility and versatility in communicative capabilities is required.
The last key factor refers to the appearance of a robot. The appearance is used as a central stimulus to guide social attribution processes as well as the associated behavioral expectations of users regarding the interactive capabilities of a robot [48]. The overall goal is to make the interaction more familiar and robust and, thus, to promote effectiveness and safety in HRI [49]. In our study, an anthropomorphic design was found to promote acceptance—especially for the target group of care recipients. The tendency for anthropomorphic design features is consistent with previous findings [50,51]. In particular, within the field of social robotics, the use of anthropomorphic features has been established as a guiding principle [52]. By implying anthropomorphic features onto the robot, social interaction schemes can seamlessly be applied and become more familiar [53]. Similar to the preferred mode of communication, the results regarding the appearance of the robot further replicate a previous study in which we investigated the preferred robot design in a healthcare context [41]. This study revealed a preference for an anthropomorphic appearance of the robot, too. Nevertheless, the degree of anthropomorphic design should be evaluated at an early stage to avoid false expectations on the robots’ capabilities as well as negative effects on the users’ acceptance [44,54,55]. In relation to the appearance, it was additionally found that the material characteristics of the surface design also require special attention in interventions with physical contact. Regarding the size of the robots, no concrete deductions could be derived based on our results. The size was primarily task-specific (e.g., larger robots for patient transport). The negligible influence of the size is again in line with previous results and, therefore, seems to represent a valid insight [41].
Overall, these requirements imply an in-depth analysis when designing a robot and interactional qualities for HRI in the healthcare domain. To deduce concrete design guidelines based on results of this study, we structure and apply findings to the taxonomy for HRI proposed by Onnasch and Roesler [44]. The taxonomy provides a comprehensible framework and considers three hierarchical aspects of HRI: (1) the interactional context; (2) the robotic qualities including task specifications, targeted level of autonomy, and robot morphology; as well as (3) the team classification referring to the team composition (e.g., is it a dyadic or triadic interaction?), the respective roles in the interaction (e.g., the human as supervisor of the robot or as collaborator), communication channels, as well as temporal and physical proximity requirements between human and robot [44] (see Figure 11).
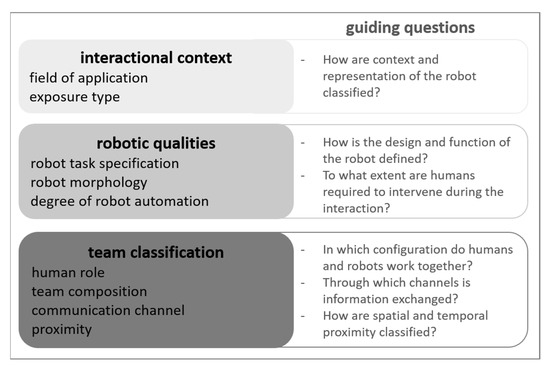
Figure 11.
Taxonomy and guiding questions for HRI according Onnasch and Roesler [44].
The interactional context is determined by our application domain in the healthcare sector. The identified healthcare tasks for potential robot assistance are imbedded in therapeutic, service, and entertainment settings. This implies that such robots need to have social (e.g., motivational) as well as functional properties (e.g., a gripper to manipulate or pick up objects). The requirements for robotic qualities can further be derived from the characteristics of the task a robot should perform. In particular, we identified three tasks that were considered as most appropriate for a robot. These were a reminder function, the integration of a robot into the calling system, and the mobilization of care recipients. With regard to the HRI taxonomy classification, these tasks represent aspects of information exchange (reminder and calling system) and manipulation (mobilization). In terms of requirements, this task combination reflects the categorization of application domain that includes social as well as functional tasks and again underlines the challenge for healthcare robots to combine an easy, approachable appearance and interface for social interaction while at the same time having acceptable payloads to manipulate or transport objects or even humans. An alternative to solve the at-first-sight-incompatible requirements could be the decision for specialized or modular robots. Moreover, the robotic qualities derived from the interviews underline the need for high robot autonomy concerning information acquisition, information analysis, decision-making, as well as action implementation. Although caregivers emphasize that in most tasks a robot is thought as an assistance tool (e.g., in mobilizing care recipients) which supports caregivers in task fulfillment, the subtasks that would be resumed by the robot still require a high autonomy level as they include complex sensing, computational, and executive functions. For example, when lifting a care recipient from bed to wheelchair, a robot would have to sense the care recipient’s position and weight, the position of the wheelchair, the height difference between bed and wheelchair, and the probability of unforeseen movements of the care recipient to adapt its movements and accomplish the task. A high level of autonomy is also required for tasks such as a reminder or calling system as these include the autonomous navigation through the facility and the identification of caregivers and care recipients.
With regard to the team classification, our results of the sequence analyses suggest a mostly triadic interaction between a caregiver, a robot, and a patient in which caregivers primarily act as supervisors (e.g., when calling the robot) or operators of the robot (e.g., in teleoperation mode) and patients as collaborators (e.g., in mobilization tasks) or supervisors. These role allocations clearly imply a hierarchical relation between humans and robots with the robot always on the lower level. This positively addresses caregivers’ concerns about a technical substitution and further values and promotes a positive work identity as well as care recipients’ self-determination. With regard to the communication channels, caregivers preferred a natural verbal communication supported by text input or visual output. This implies a certain degree of complexity of communicational scripts. Natural dialogues would imply a reciprocity and adaptivity in communication protocols [56] which is often challenging and beyond technical feasibility in terms of unstructured environments and different target groups with specific requirements. A hands-on solution to this problem might be provided by the robot’s morphology. Caregivers tended to prefer an anthropomorphic and infantile appearance of a robot. First of all, this matches the hierarchical role of humans when interacting with the technical system, and second, this might also lower expectations with regard to communicational skills. However, an infantile anthropomorphic robot appearance might be difficult to realize in a robot with a high payload which requires a certain height, too. Moreover, an infantile appearance might induce non-intended consequences such as a reluctance to hand over certain tasks to the robot (e.g., dull, dirty, or dangerous tasks [57]). Another possibility, probably even more appropriate, could be a zoomorphic robot design which triggers interaction scripts more related to pets. In consequence, communication could be more unidirectional without violating caregivers’ and care recipients’ expectations. Additionally, infantile anthropomorphic as well as zoomorphic robot designs evoke the so-called psychological caregiver effect [58,59] which describes the perception of being responsible for the robot and increases empathy and acceptance [60]. With regard to proximity, study insights clearly point to a close physical proximity with haptic contact (touching) which underlines the need of a disinfectable and, at the same time, pleasing surface (e.g., smooth, having human body temperature).
These guidelines with respect to the design of healthcare robots and interactional requirements represent a comprehensive first step which is based on insights of the current study and, also, in line with previous research and theories of HRI [53]. To further validate findings and answer the question of transferability from theory to application, future research needs to implement such guidelines into actual robot designs to create embodied testable prototypes.
4.4. Limitations
The generalizability of the study results is subject to several limitations, which will be discussed in the following. One such limitation relates to the sample size and characteristics. Although we considered explicitly including caregivers with and without robotics experience as part of the deliberate case selection process, the results should be considered indicative for future studies because of the small group sizes. For the construction of the sequence analysis in study II, data from all 19 participants were included. Although three participants can be considered sufficient for an in-depth analysis of single, relatively concrete aspects, larger samples should be targeted with respect to the addressed user groups as well as for the development of specific models of human–robot collaboration. Furthermore, our sample consisted mainly of female participants. Only four men could be acquired for the study. However, this reflects approximately the gender distribution in the healthcare sector globally, where women represent approximately 90% of the nursing workforce [1]. Finally, with regard to the sample, it must also be noted that the healthcare professionals in our study work in the field of inpatient care for the elderly. In this respect, our results reflect a specific perspective on the care process of older people and may differ from experiences in the care of other target groups (such as in the field of pediatric care). A further limitation concerns the type of robotic systems with which the interviewees had previous experience. In the majority of cases, these are related to the socially interactive robot Pepper, which was used for the purpose of activating, orienting, and entertaining care recipients. In this respect, it cannot be excluded that the mental model of a robot in care is strongly co-constructed by these previous experiences. Finally, a last limitation concerns the selected research method using the guideline-based video interview. Although this methodological approach allowed us a high degree of flexibility with regard to the job involvements of the interviewees and was also necessary because of the existing health protection constraints due to the COVID-19 pandemic, there are general limitations of guided interviews. It might be difficult for the interviewees to put their experiences and knowledge into words. Overall, it must be stated that our findings are, however, consistent with previous research and, moreover, provide important suggestions for successful implementation in care settings.
5. Conclusions
This work aims to contribute to a stronger consideration of the perspective of professional caregivers as one of the central user groups of robotics in care. Based on a qualitative research approach with semi-structured interviews, three main research topics were addressed in two consecutive studies: (1) prerequisites for implementation and use, (2) potential application areas for robotics in general as well as ethical considerations, and, finally, (3) basic requirements for HRI. Our results illustrate that robot assistance is expected to provide potential relief in a wide range of application areas. At the same time, however, there are reservations about the automation of care activities that require high levels of professional supervision for patient safety and that are characterized by an interpersonal, physical, and emotional relationship. In addition to the high technical requirements for reliable identification, interpretation, and reaction to care-relevant events, basic professional values as specific standards for action as well as the work identity of the caregivers play a crucial role. Two central implications can be derived from this for the use of robots. First, the technical capabilities and the question of agency of robotic solutions must be increasingly oriented to the specific problems and goals of the care process. Second, human–robot collaboration must promote the caregiver’s responsibility and situational awareness for the care recipient throughout the entire care process. Another challenge consists in the design of the HRI. Basically, it has to be considered that different user groups with heterogeneous needs and roles are involved in care-related intervention. While speech control was found to be the most intuitive form of operation across all user groups, there are significant differences, for example, with regard to the type of user feedback and the level of access to functions. Further requirements also concern the interactive capabilities and the appearance of the robot, both of which play a decisive role for the expectation management of the user groups with respect to the role and capabilities of the robot but also for their self-perception.
In summary, it can be stated that for a successful introduction and long-term use of assistive robotics in care, a generic development approach is imperative. This should not only apply to an episodic involvement of the user group of caregivers in various phases of the development process, but also to a consistent involvement as early as the problem definition stage. To enable caregivers in making informed decisions about specific needs and requirements for the use of robots, more comprehensive orientation programs must be created. These should raise awareness of the practical relevance of robotic solutions, offer practical experience, and provide the opportunity to develop the necessary competencies.
Supplementary Materials
The following supporting information can be downloaded at: www.mdpi.com/xxx/S1, Document S1: Semi-structured interview script–study I; Document S2: Semi-structured interview script–study II.
Author Contributions
Conceptualization, R.K., K.K., R.D. and L.O.; Data curation, R.K., K.K., R.D. and L.O.; Formal analysis, R.K., K.K. and R.D.; Funding acquisition, R.D. and L.O.; Investigation, R.K., K.K. and R.D.; Methodology, R.K., K.K., R.D. and L.O.; Project administration, R.K., K.K. and R.D.; Resources, R.K., K.K. and R.D.; Supervision, L.O.; Validation, R.K., K.K., R.D. and L.O.; Visualization, R.K., K.K. and R.D.; Writing—original draft, R.K., K.K. and R.D.; Writing—review & editing, R.K., K.K., R.D. and L.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the German Federal Ministry of Education and Research (BMBF) within the project RoMi “Roboterunterstützung bei Routineaufgaben zur Stärkung des Miteinanders in Pflegeheimen” under grant number 16SV8436. The APC was funded by the Open Access Publication Fund of Charité–Universitätsmedizin Berlin and the German Research Foundation (DFG).
Institutional Review Board Statement
The studies involving human participants were reviewed and approved by the ethics committee at the Institute of Psychology at the Humboldt-Universität zu Berlin (number: 2020-40 and 2021-11). Furthermore, the studies were preregistered at the German Clinical Trials Register (DRKS number: 00022318).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets presented in this article are not readily available because complete anonymization of the data is not possible due to the combinability of different content within the qualitative interviews. Requests to access the datasets should be directed to the corresponding author.
Acknowledgments
The authors would like to thank all the caregivers who participated in the survey and were willing to share some of their limited time with us. Furthermore, we would like to thank Franz Mönke for his support in coding the results of the first study and Edith Aull for assisting with the interviews of the second study.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- World Health Organisation. State of the World’s Nursing 2020: Investing in Education, Jobs and Leadership; World Health Organization: Geneva, Switzerland, 2020.
- Buchan, J.; Catton, H.; Shaffer, F.A. Ageing Well? Policies to Support Older Nurses at Work. International Centre on Nurse Migration; International Centre on Nurse Migration: Philadelphia, PA, USA, 2020. [Google Scholar]
- Jacobs, K.; Kuhlmey, A.; Greß, S.; Klauber, J.; Schwinger, A. Pflege-Report 2019: Mehr Personal in der Langzeitpflege- aber woher? Springer: Berlin, Heidelberg, 2020; ISBN 978-3-662-58934-2. [Google Scholar]
- Hasselhorn, H.-M.; Müller, B.H.; Tackenberg, P.; Kümmerling, A.; Simone, M. Berufsausstieg bei Pflegepersonal: Arbeitsbedingungen und Beabsichtigter Berufsausstieg bei Pflegepersonal in Deutschland und Europa; Schriftenreihe der Bundesanstalt für Arbeitsschutz und Arbeitsmedizin Ü, Übersetzung; Wirtschaftsverl. NW, Verl. für Neue Wiss GmbH: Bremerhaven, Germany, 2005; ISBN 978-3-86509-247-2. [Google Scholar]
- Statistik der Bundesagentur für Arbeit. Berichte: Blickpunkt Arbeitsmarkt—Arbeitsmarktsituation im Pflegebereich; Blickpunkt Arbeitsmarkt: Nürnberg, Germany, 2021; p. 22. [Google Scholar]
- Institut DGB-Index Gute Arbeit. Arbeitsbedingungen in der Alten- und Krankenpflege—So beurteilen die Beschäftigten die Lage; Institut DGB-Index Gute Arbeit: Berlin, Germany, 2018; p. 24. [Google Scholar]
- Engelberger, J.F. Robotics in Service; Springer: Dordrecht, The Netherlands, 1989; ISBN 978-94-010-6985-4. [Google Scholar]
- Frazier, R.M.; Carter-Templeton, H.; Wyatt, T.H.; Wu, L. Current Trends in Robotics in Nursing Patents—A Glimpse Into Emerging Innovations. CIN Comput. Inform. Nurs. 2019, 37, 290–297. [Google Scholar] [CrossRef]
- Graf, B. Assistenzroboter für die Pflege. Z. Für Gerontol. Geriatr. 2020, 53, 608–614. [Google Scholar] [CrossRef]
- Kehl, C. Robotik und Assistive Neurotechnologien in der Pflege—Gesellschaftliche Herausforderungen; 177. TAB-Arbeitsbericht. Büro für Technikfolgen-Abschätzung beim Deutschen Bundestag (TAB): Berlin, Germany, 2018; p. 240. [Google Scholar]
- Robotik in Betreuung und Gesundheitsversorgung; Becker, H., Ed.; TA-SWISS; vdf Hochschulverl: Zürich, Switzerland, 2013; ISBN 978-3-7281-3520-9. [Google Scholar]
- Bardaro, G.; Antonini, A.; Motta, E. Robots for Elderly Care in the Home: A Landscape Analysis and Co-Design Toolkit. Int. J. Soc. Robot. 2021, 14, 657–681. [Google Scholar] [CrossRef]
- Bedaf, S.; Gelderblom, G.J.; de Witte, L. Overview and Categorization of Robots Supporting Independent Living of Elderly People: What Activities Do They Support and How Far Have They Developed. Assist. Technol. 2015, 27, 88–100. [Google Scholar] [CrossRef]
- Persson, M.; Redmalm, D.; Iversen, C. Caregivers’ Use of Robots and Their Effect on Work Environment—A Scoping Review. J. Technol. Hum. Serv. 2022, 40, 251–277. [Google Scholar] [CrossRef]
- Wright, J. Tactile Care, Mechanical Hugs: Japanese Caregivers and Robotic Lifting Devices. Asian Anthropol. 2018, 17, 24–39. [Google Scholar] [CrossRef]
- Papadopoulos, I.; Koulouglioti, C.; Ali, S. Views of Nurses and Other Health and Social Care Workers on the Use of Assistive Humanoid and Animal-like Robots in Health and Social Care: A Scoping Review. Contemp. Nurse 2018, 54, 425–442. [Google Scholar] [CrossRef]
- Beedholm, K.; Frederiksen, K.; Lomborg, K. What Was (Also) at Stake When a Robot Bathtub Was Implemented in a Danish Elder Center: A Constructivist Secondary Qualitative Analysis. Qual. Health Res. 2016, 26, 1424–1433. [Google Scholar] [CrossRef]
- Mossfeldt Nickelsen, N.C. Imagining and Tinkering with Assistive Robotics in Care for the Disabled. Paladyn J. Behav. Robot. 2019, 10, 128–139. [Google Scholar] [CrossRef]
- Johansson-Pajala, R.-M.; Thommes, K.; Hoppe, J.A.; Tuisku, O.; Hennala, L.; Pekkarinen, S.; Melkas, H.; Gustafsson, C. Care Robot Orientation: What, Who and How? Potential Users’ Percept. Int. J. Soc. Robot. 2020, 12, 1103–1117. [Google Scholar] [CrossRef]
- Moyle, W.; Bramble, M.; Jones, C.; Murfield, J. Care Staff Perceptions of a Social Robot Called Paro and a Look-Alike Plush Toy: A Descriptive Qualitative Approach. Aging Ment. Health 2018, 22, 330–335. [Google Scholar] [CrossRef]
- Nilsen, E.R.; Dugstad, J.; Eide, H.; Gullslett, M.K.; Eide, T. Exploring Resistance to Implementation of Welfare Technology in Municipal Healthcare Services—A Longitudinal Case Study. BMC Health Serv. Res. 2016, 16, 657. [Google Scholar] [CrossRef]
- Parviainen, J.; Turja, T.; Van Aerschot, L. Robots and Human Touch in Care: Desirable and Non-Desirable Robot Assistance. In Social Robotics; Ge, S.S., Cabibihan, J.-J., Salichs, M.A., Broadbent, E., He, H., Wagner, A.R., Castro-González, Á., Eds.; Lecture Notes in Computer Science; Springer International Publishing: Cham, Switzerland, 2018; Volume 11357, pp. 533–540. ISBN 978-3-030-05203-4. [Google Scholar]
- Beane, M.; Orlikowski, W.J. What Difference Does a Robot Make? The Material Enactment of Distributed Coordination. Organ. Sci. 2015, 26, 1553–1573. [Google Scholar] [CrossRef]
- Chen, S.-C.; Jones, C.; Moyle, W. Health Professional and Workers Attitudes towards the Use of Social Robots for Older Adults in Long-Term Care. Int. J. Soc. Robot. 2020, 12, 1135–1147. [Google Scholar] [CrossRef]
- Rantanen, T.; Lehto, P.; Vuorinen, P.; Coco, K. Attitudes towards Care Robots among Finnish Home Care Personnel—A Comparison of Two Approaches. Scand. J. Caring Sci. 2018, 32, 772–782. [Google Scholar] [CrossRef]
- Flandorfer, P. Population Ageing and Socially Assistive Robots for Elderly Persons: The Importance of Sociodemographic Factors for User Acceptance. Int. J. Popul. Res. 2012, 2012, 829835. [Google Scholar] [CrossRef]
- Turja, T.; Van Aerschot, L.; Särkikoski, T.; Oksanen, A. Finnish Healthcare Professionals’ Attitudes towards Robots: Reflections on a Population Sample. Nurs. Open 2018, 5, 300–309. [Google Scholar] [CrossRef]
- van Wynsberghe, A. Designing Robots for Care: Care Centered Value-Sensitive Design. Sci. Eng. Ethics 2013, 19, 407–433. [Google Scholar] [CrossRef]
- Gläser, J.; Laudel, G. Experteninterviews und Qualitative Inhaltsanalyse als Instrumente Rekonstruierender Untersuchungen, 4th ed.; Lehrbuch; VS Verl. für Sozialwiss: Wiesbaden, Germany, 2010; ISBN 978-3-531-17238-5. [Google Scholar]
- Mayring, P. Qualitative Inhaltsanalyse: Grundlagen und Techniken, 12th ed.; Beltz Verlag: Basel, Switzerland, 2015; ISBN 978-3-407-25730-7. [Google Scholar]
- Beyer, H.; Holtzblatt, K. Contextual Design: Defining Customer-Centered Systems; Morgan Kaufmann: San Francisco, CA, USA, 1997; ISBN 978-1-55860-411-7. [Google Scholar]
- Melkas, H.; Hennala, L.; Pekkarinen, S.; Kyrki, V. Impacts of Robot Implementation on Care Personnel and Clients in Elderly-Care Institutions. Int. J. Med. Inf. 2020, 134, 104041. [Google Scholar] [CrossRef]
- Sharts-Hopko, N.C. The Coming Revolution in Personal Care Robotics: What Does It Mean for Nurses? Nurs. Adm. Q. 2014, 38, 5–12. [Google Scholar] [CrossRef]
- Coco, K.; Kangasniemi, M.; Rantanen, T. Care Personnel’s Attitudes and Fears toward Care Robots in Elderly Care: A Comparison of Data from the Care Personnel in Finland and Japan. J. Nurs. Scholarsh. 2018, 50, 634–644. [Google Scholar] [CrossRef] [PubMed]
- Kristoffersson, A.; Coradeschi, S.; Loutfi, A.; Severinson-Eklundh, K. An Exploratory Study of Health Professionals’ Attitudes about Robotic Telepresence Technology. J. Technol. Hum. Serv. 2011, 29, 263–283. [Google Scholar] [CrossRef]
- Pigini, L.; Facal, D.; Blasi, L.; Andrich, R. Service Robots in Elderly Care at Home: Users’ Needs and Perceptions as a Basis for Concept Development. Technol. Disabil. 2012, 24, 303–311. [Google Scholar] [CrossRef]
- Fiorini, L.; De Mul, M.; Fabbricotti, I.; Limosani, R.; Vitanza, A.; D’Onofrio, G.; Tsui, M.; Sancarlo, D.; Giuliani, F.; Greco, A.; et al. Assistive Robots to Improve the Independent Living of Older Persons: Results from a Needs Study. Disabil. Rehabil. Assist. Technol. 2021, 16, 92–102. [Google Scholar] [CrossRef] [PubMed]
- Olatunji, S.; Potenza, A.; Kiselev, A.; Oron-Gilad, T.; Loutfi, A.; Edan, Y. Levels of Automation for a Mobile Robot Teleoperated by a Caregiver. ACM Trans. Hum. -Robot. Interact. 2021, 11, 1–21. [Google Scholar] [CrossRef]
- Christoforou, E.G.; Avgousti, S.; Ramdani, N.; Novales, C.; Panayides, A.S. The Upcoming Role for Nursing and Assistive Robotics: Opportunities and Challenges Ahead. Front. Digit. Health 2020, 2, 585656. [Google Scholar] [CrossRef]
- Chatterji, N.; Allen, C.; Chernova, S. Effectiveness of Robot Communication Level on Likeability, Understandability and Comfortability. In Proceedings of the 2019 28th IEEE International Conference on Robot and Human Interactive Communication (RO-MAN), New Delhi, India, 14–18 October 2019; pp. 1–7. [Google Scholar]
- Klüber, K.; Onnasch, L. Appearance Is Not Everything—Preferred Feature Combinations for Care Robots. Comput. Hum. Behav. 2022, 128, 107128. [Google Scholar] [CrossRef]
- Eyssel, F.; Kuchenbrandt, D.; Bobinger, S.; de Ruiter, L.; Hegel, F. “If You Sound like Me, You Must Be More Human”: On the Interplay of Robot and User Features on Human-Robot Acceptance and Anthropomorphism. In Proceedings of the Seventh Annual ACM/IEEE International Conference on Human-Robot Interaction—HRI ’12, Boston, MA, USA, 5–8 March 2012; p. 125. [Google Scholar]
- Tamagawa, R.; Watson, C.I.; Kuo, I.H.; MacDonald, B.A.; Broadbent, E. The Effects of Synthesized Voice Accents on User Perceptions of Robots. Int. J. Soc. Robot. 2011, 3, 253–262. [Google Scholar] [CrossRef]
- Onnasch, L.; Roesler, E. A Taxonomy to Structure and Analyze Human–Robot Interaction. Int. J. Soc. Robot. 2021, 13, 833–849. [Google Scholar] [CrossRef]
- Pineau, J.; Montemerlo, M.; Pollack, M.; Roy, N.; Thrun, S. towards Robotic Assistants in Nursing Homes: Challenges and Results. Robot. Auton. Syst. 2003, 42, 271–281. [Google Scholar] [CrossRef]
- Leite, I.; Martinho, C.; Paiva, A. Social Robots for Long-Term Interaction: A Survey. Int. J. Soc. Robot. 2013, 5, 291–308. [Google Scholar] [CrossRef]
- Winkle, K.; Caleb-Solly, P.; Turton, A.; Bremner, P. Social Robots for Engagement in Rehabilitative Therapies: Design Implications from a Study with Therapists. In Proceedings of the 2018 ACM/IEEE International Conference on Human-Robot Interaction, Chicago, IL, USA, 26 February 2018; pp. 289–297. [Google Scholar]
- Epley, N.; Waytz, A.; Cacioppo, J.T. On Seeing Human: A Three-Factor Theory of Anthropomorphism. Psychol. Rev. 2007, 114, 864–886. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Zhu, B.; David, B. Kaber Anthropomorphism in Robots and Human Etiquette Expectations for Interaction. In Human–Computer Etiquette. Cultural Expectations and the Design Implications They Place on Computers and Technology; Hayes, C.C., Miller, C.A., Eds.; Taylor & Francis: London, UK, 2010; pp. 231–259. ISBN 978-0-429-24946-4. [Google Scholar]
- Rosenthal-von der Pütten, A.M.; Krämer, N.C. How Design Characteristics of Robots Determine Evaluation and Uncanny Valley Related Responses. Comput. Hum. Behav. 2014, 36, 422–439. [Google Scholar] [CrossRef]
- Kontogiorgos, D.; Pereira, A.; Andersson, O.; Koivisto, M.; Gonzalez Rabal, E.; Vartiainen, V.; Gustafson, J. The Effects of Anthropomorphism and Non-Verbal Social Behaviour in Virtual Assistants. In Proceedings of the 19th ACM International Conference on Intelligent Virtual Agents, Paris, France, 2–5 July 2019; pp. 133–140. [Google Scholar]
- Fong, T.; Nourbakhsh, I.; Dautenhahn, K. A Survey of Socially Interactive Robots. Robot. Auton. Syst. 2003, 42, 143–166. [Google Scholar] [CrossRef]
- Nass, C.; Moon, Y. Machines and Mindlessness: Social Responses to Computers. J. Soc. Issues 2000, 56, 81–103. [Google Scholar] [CrossRef]
- Duffy, B.R. Anthropomorphism and the Social Robot. Robot. Auton. Syst. 2003, 42, 177–190. [Google Scholar] [CrossRef]
- Mori, M.; MacDorman, K.; Kageki, N. The Uncanny Valley [From the Field]. IEEE Robot. Autom. Mag. 2012, 19, 98–100. [Google Scholar] [CrossRef]
- Rossi, S.; Ferland, F.; Tapus, A. User Profiling and Behavioral Adaptation for HRI: A Survey. Pattern Recognit. Lett. 2017, 99, 3–12. [Google Scholar] [CrossRef]
- Nof, S.Y. Automation: What It Means to Us around the World. In Springer Handbook of Automation; Nof, S.Y., Ed.; Springer: Berlin/Heidelberg, Germany, 2009; pp. 13–52. ISBN 978-3-540-78830-0. [Google Scholar]
- Calo, C.; Hunt-Bull, N.; Lewis, L.; Metzler, T. Ethical Implications of Using the Paro Robot, with a Focus on Dementia Patient Care. In Proceedings of the Human-Robot Interaction in Elder Care; Papers from the 2011 AAAI Workshop; AAAI: San Francisco, CA, USA, 2011; pp. 20–24. [Google Scholar]
- Darling, K. Extending Legal Protection to Social Robots: The Effects of Anthropomorphism, Empathy, and Violent Behavior towards Robotic Objects. SSRN Electron. J. 2012. [Google Scholar] [CrossRef]
- Friedman, B.; Kahn, P.H.; Hagman, J. Hardware Companions?: What Online AIBO Discussion Forums Reveal about the Human-Robotic Relationship. In Proceedings of the conference on Human factors in computing systems—CHI ’03, Ft. Lauderdale, FL, USA, 5–10 April 2003; p. 273. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).