Running Experimental Research of a Cable-Driven Astronaut on-Orbit Physical Exercise Equipment
Abstract
:1. Introduction
2. Cable-Driven On-Orbit Astronaut Physical Exercise Equipment (CAPE)
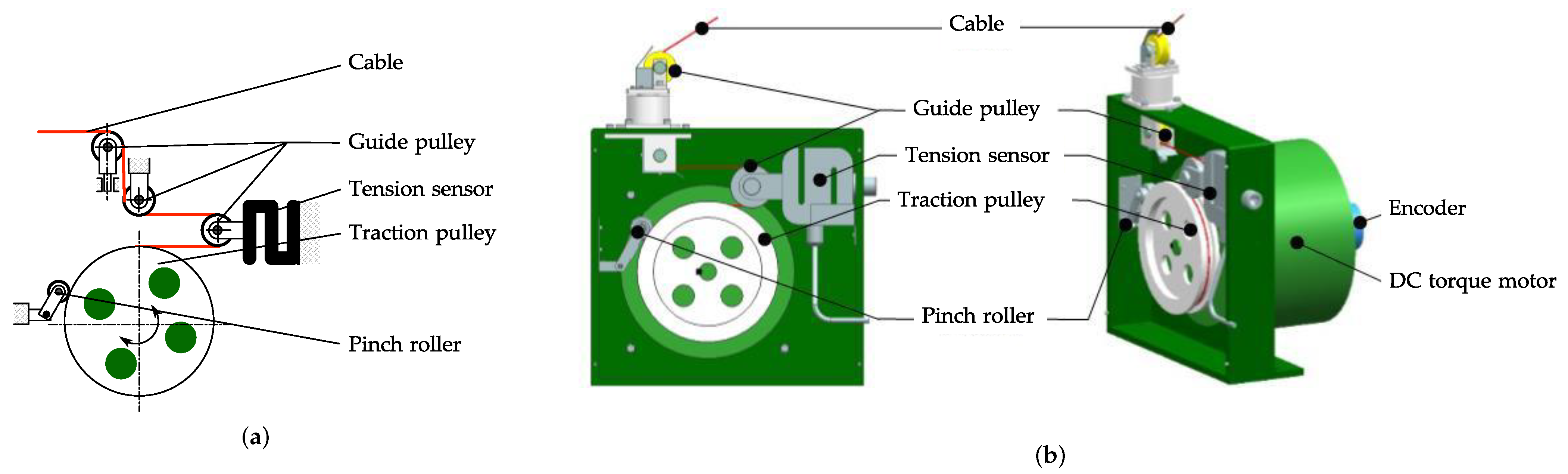
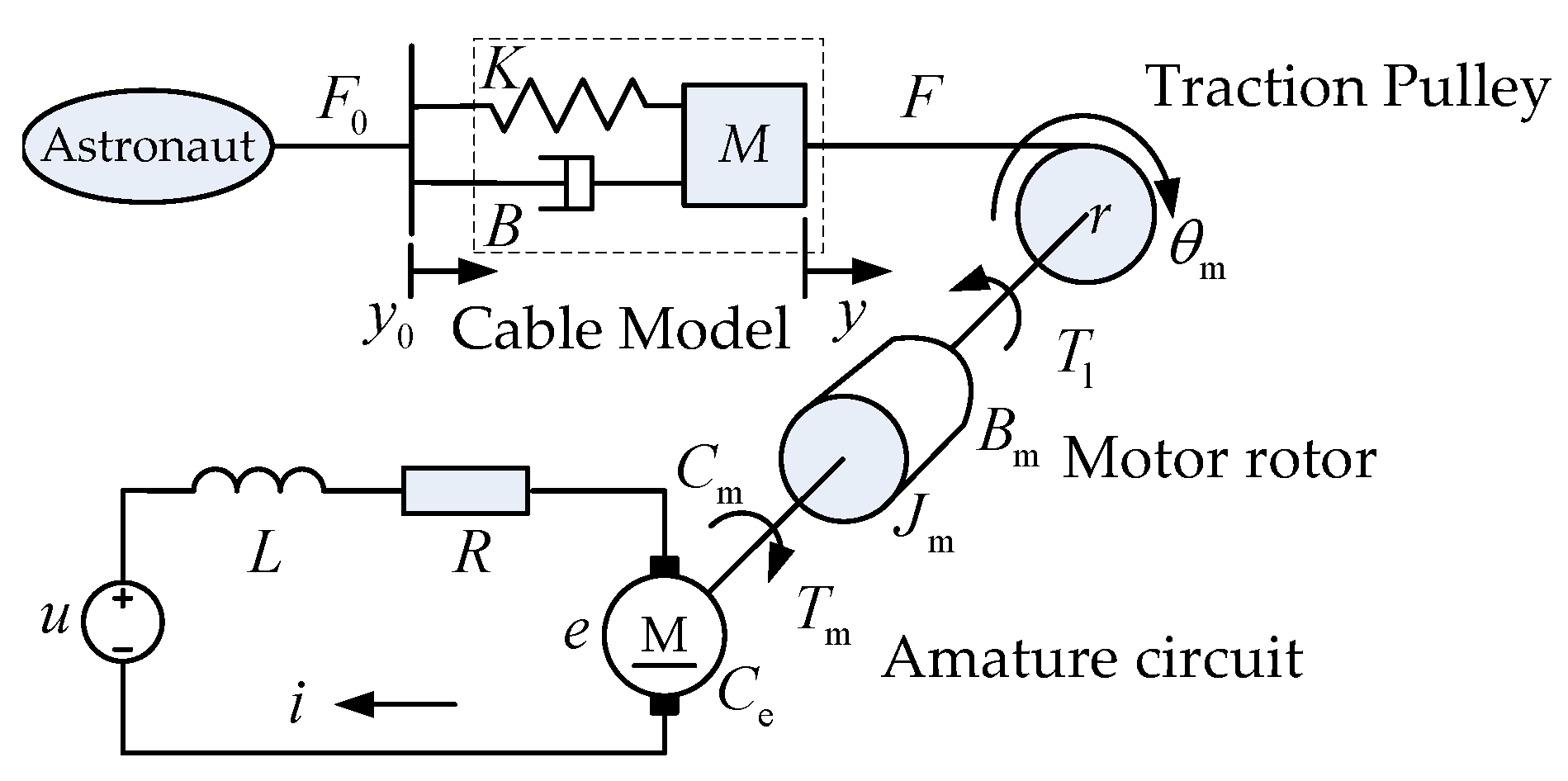
2.1. Cable Module
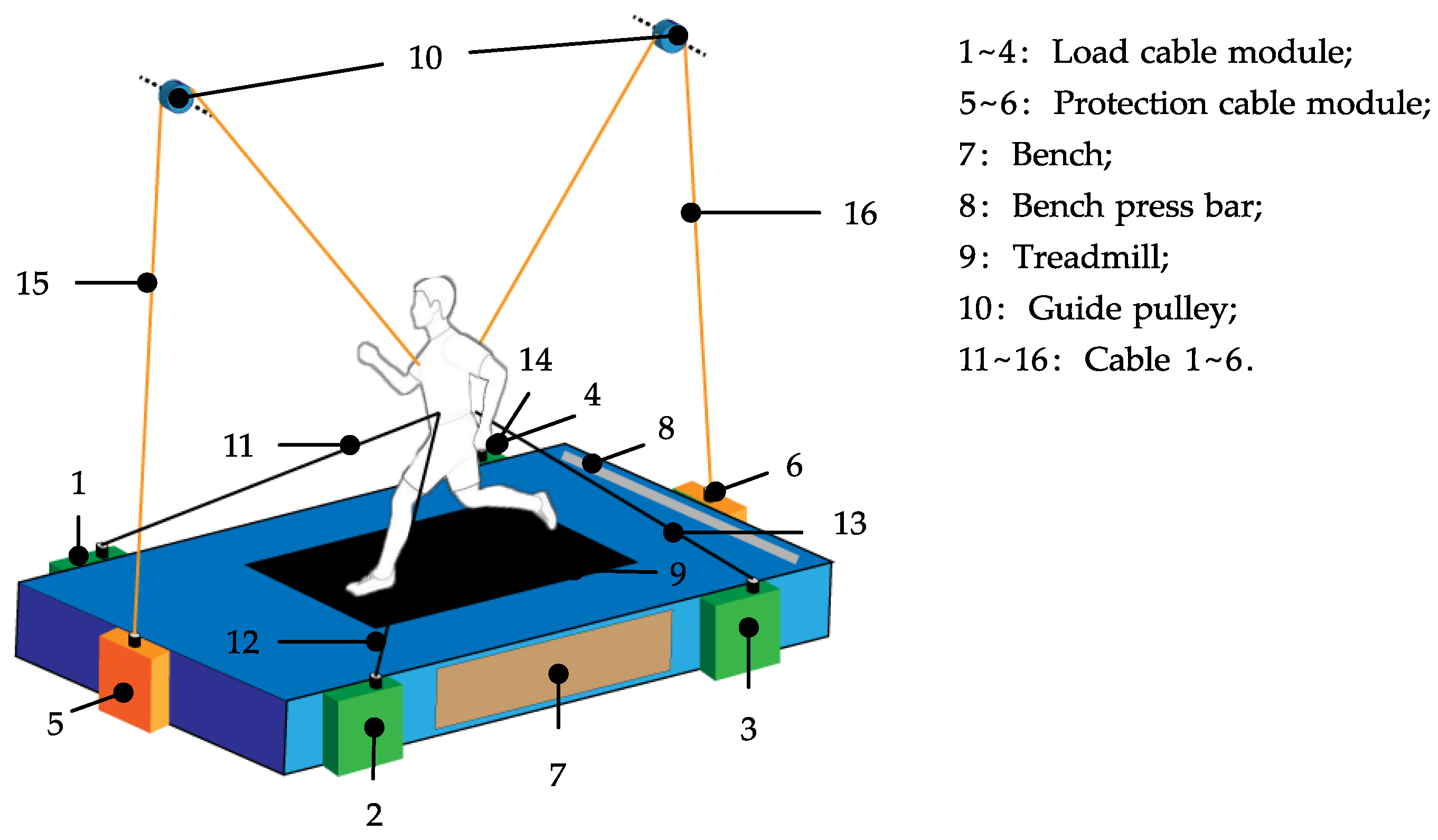
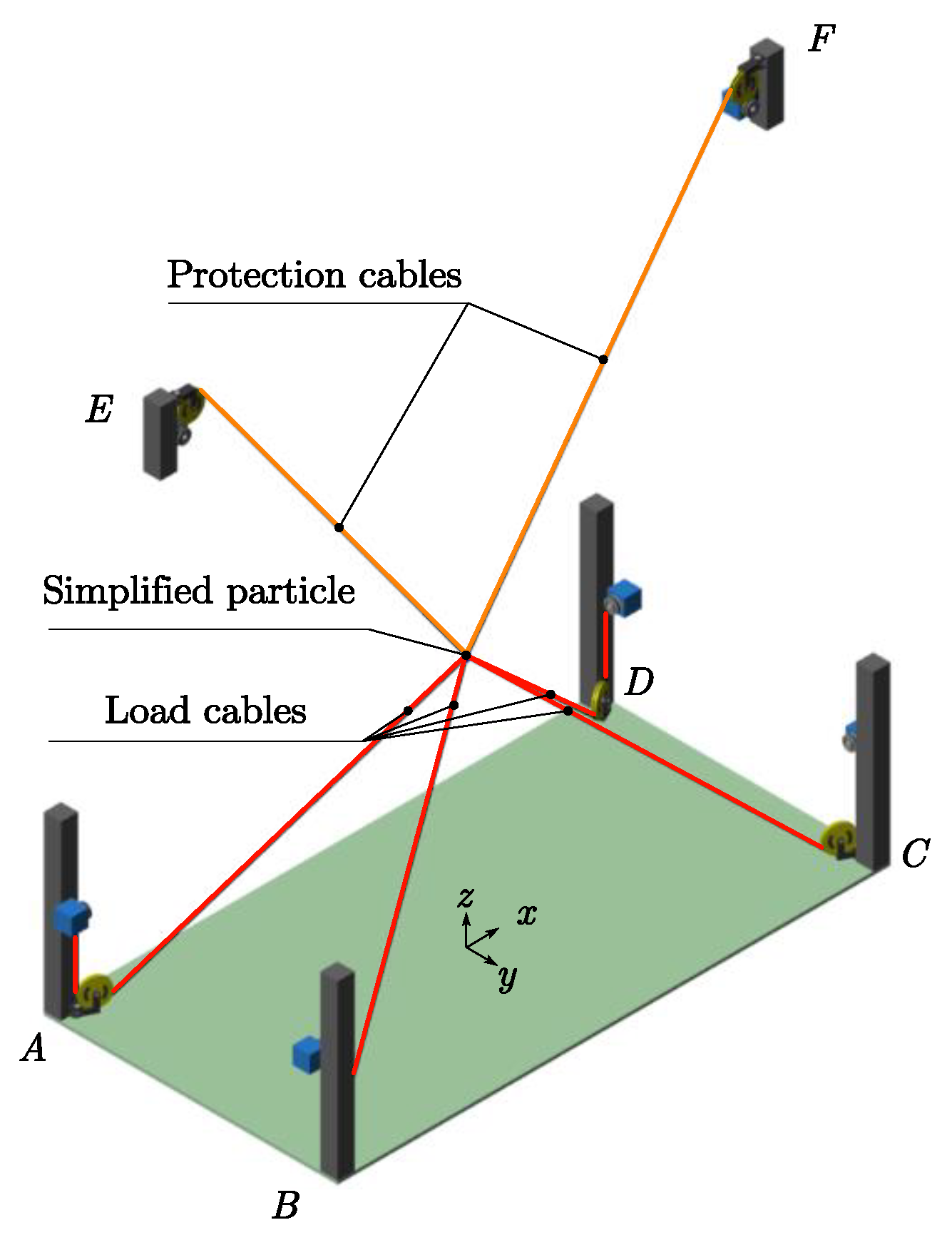
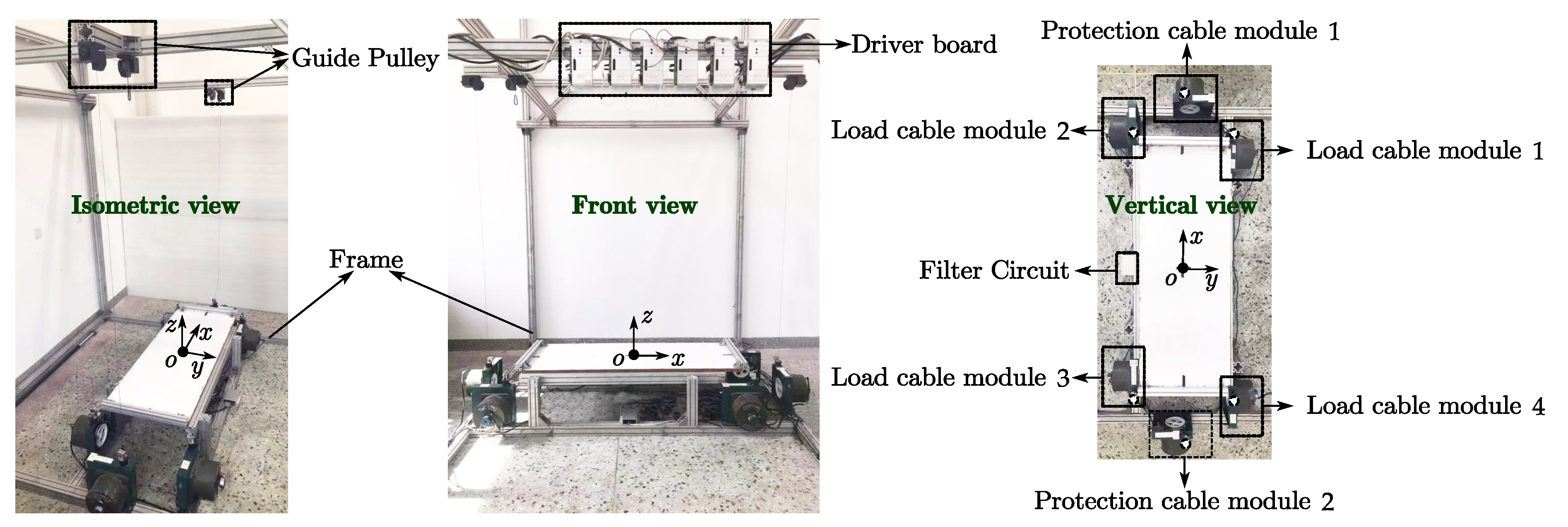
2.2. Configuration of CAPE
- (1)
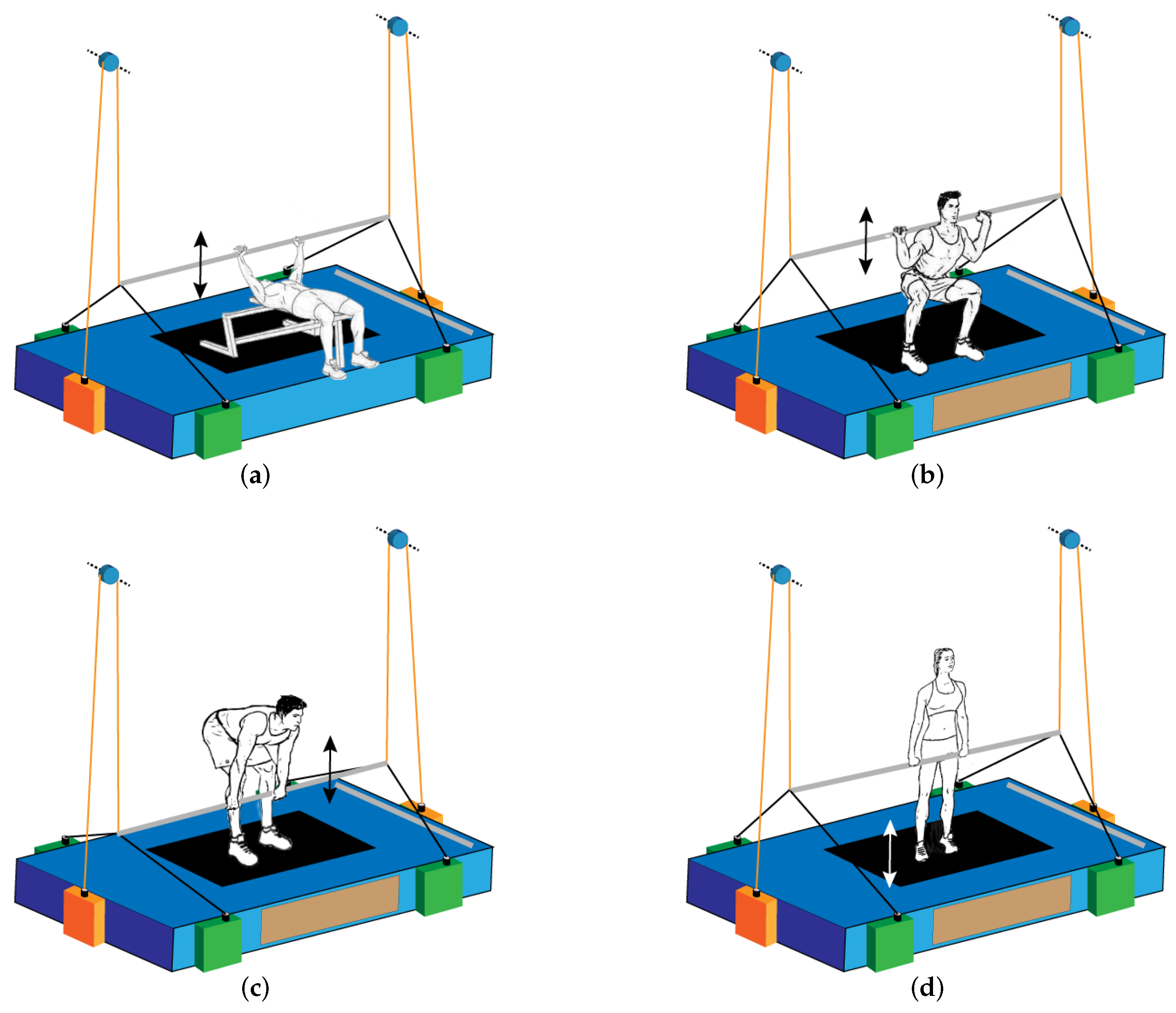
- CAPE provides astronauts with a variety of exercise modes, realizing high efficiency without increasing the cost of the equipment. As shown in Figure 2 and Figure 3, with the assistance of CAPE, astronauts are able to carry out bench press, deep squat, deadlift, heel raise, and running exercise. In which running is aerobic exercise, while others are weight-exercises.
- (2)
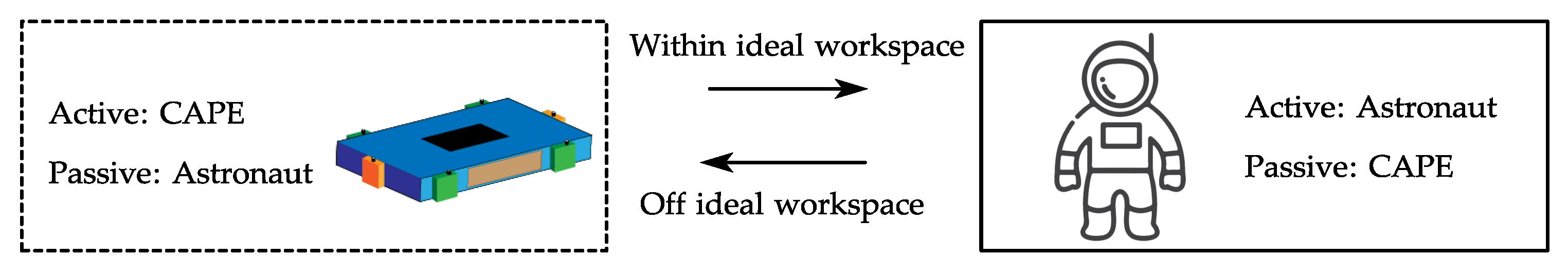
- The CAPE can be easily set up by the help of the carabiners at the each end of the cables. Compared with the rigid connections with the human body of most of the existing exercise devices in space, the type of cable-driven will significantly reduce the injury risk. Furthermore, to ensure the safety of the astronaut, CAPE provides a safety protection strategy. As presented in Figure 2, the four green cable modules realize the load force during exercises, and two orange cable modules are responsible for the safety monitoring and the protection of astronauts. Normally, the two orange cable modules follow the movement of astronauts passively, while in some cases to avoid accidents or instability, these two modules collaborate with the other four green cable modules to complete safety protection actions, which is described in Section 3.
- (3)
- Modular design is adopted to develop the cable module, and the cable modules could be hidden in the floor of the space station. Several advantages are brought by this kind of modular design and arrangement: economical in cost; easy to replace, maintain, and repair; in addition, when the CAPE is inactive, the cable can be coiled on the traction pulley to occupy less space and improve the utilization rate of space, which is significant for the narrow space capsule, and provides an orderly living environment for astronauts.
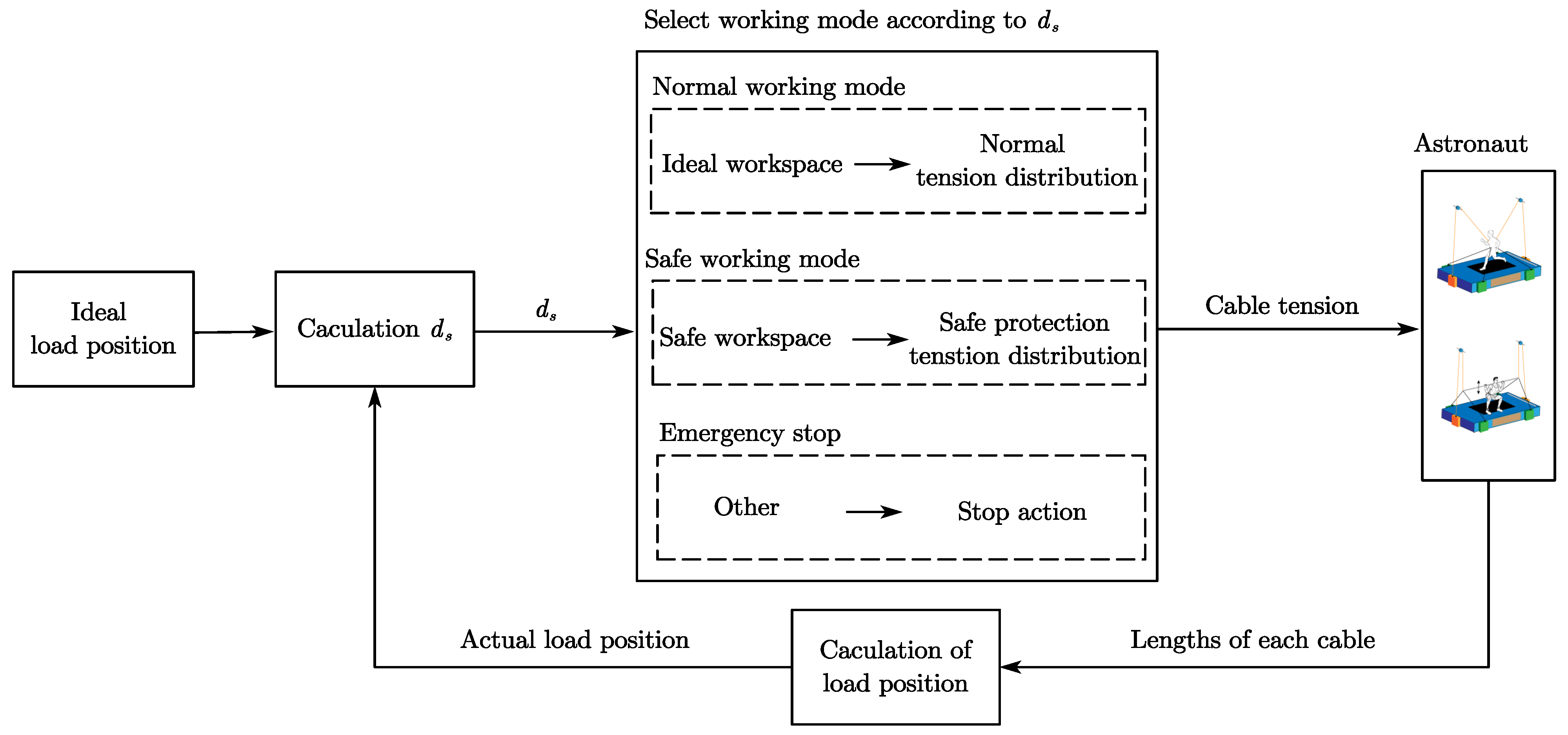
3. Two-Level Controller and Safety Protection Strategy of CAPE
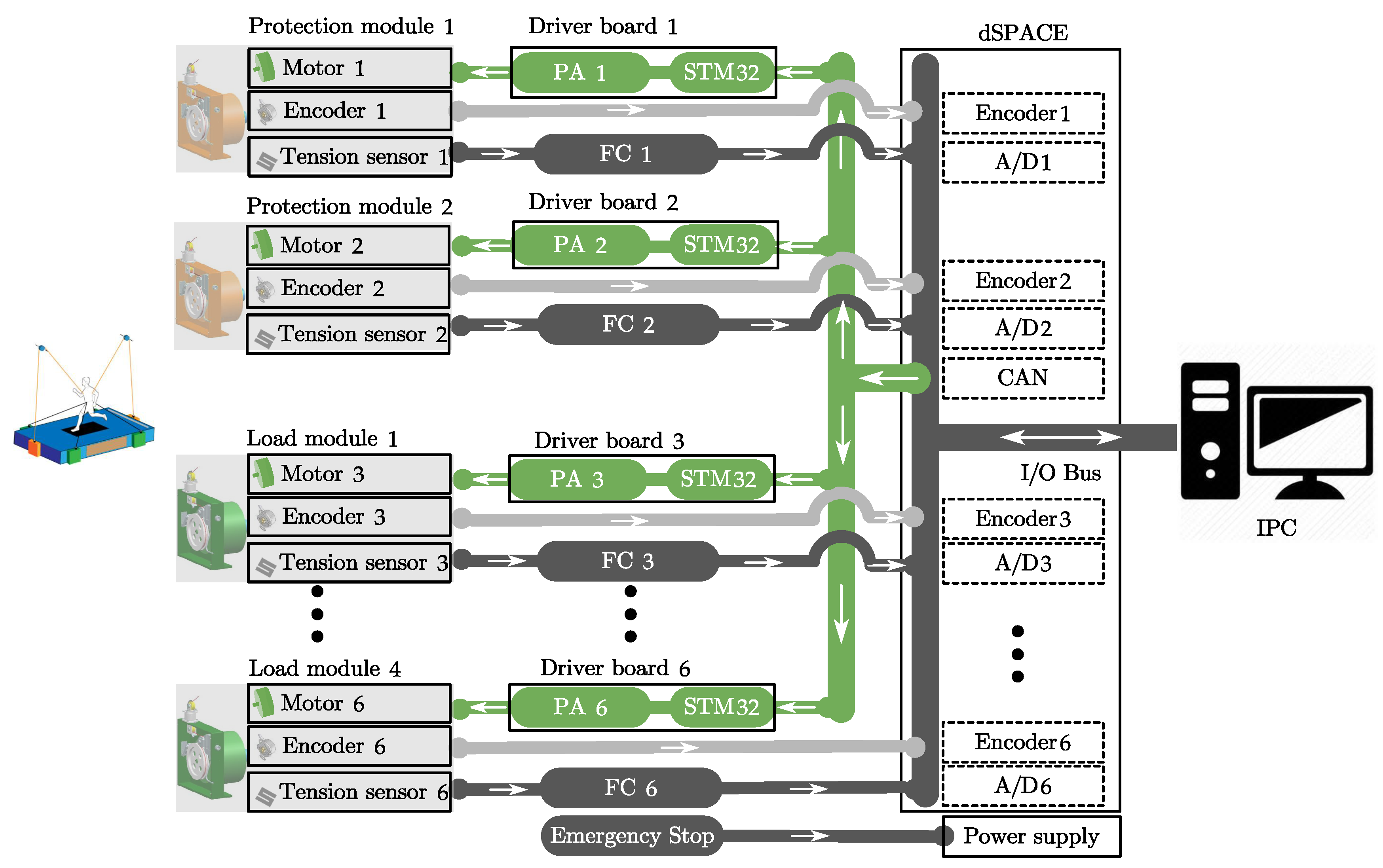
3.1. Two-Level Controller
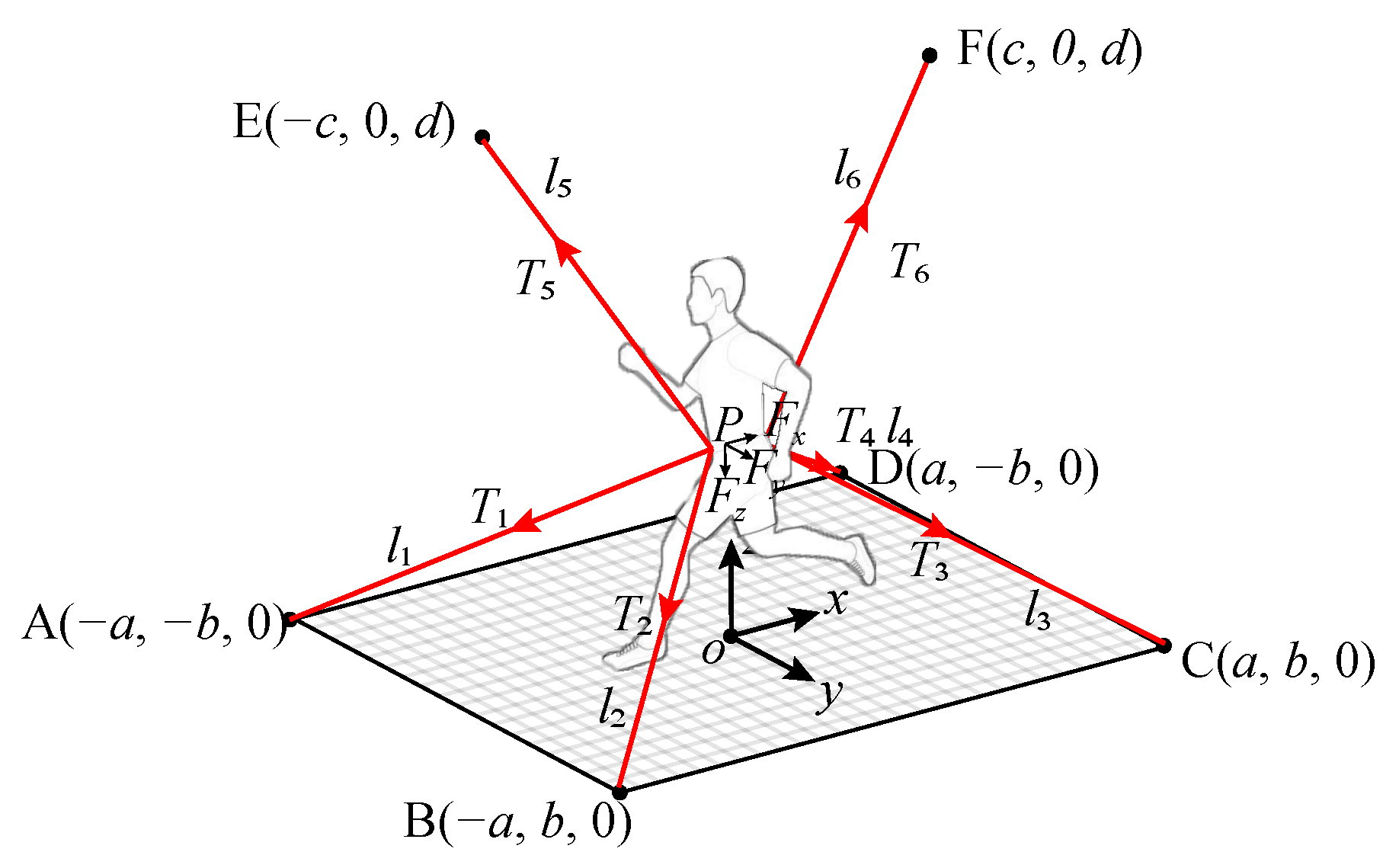
3.1.1. Cable Tension Distribution Algorithm for Running Exercise
- (1)
- If , the objective function obtains the minimum value when ; then, there are three cases:
- (2)
- If , the objective function can be written as ; then, there are three cases:
3.1.2. Tension Controller of Cable Module
3.2. Safety Protection Strategy
4. Simulation and Experiment of Running Exercise with CAPE
4.1. Simulation of Running Exercise
4.2. Running Experiment
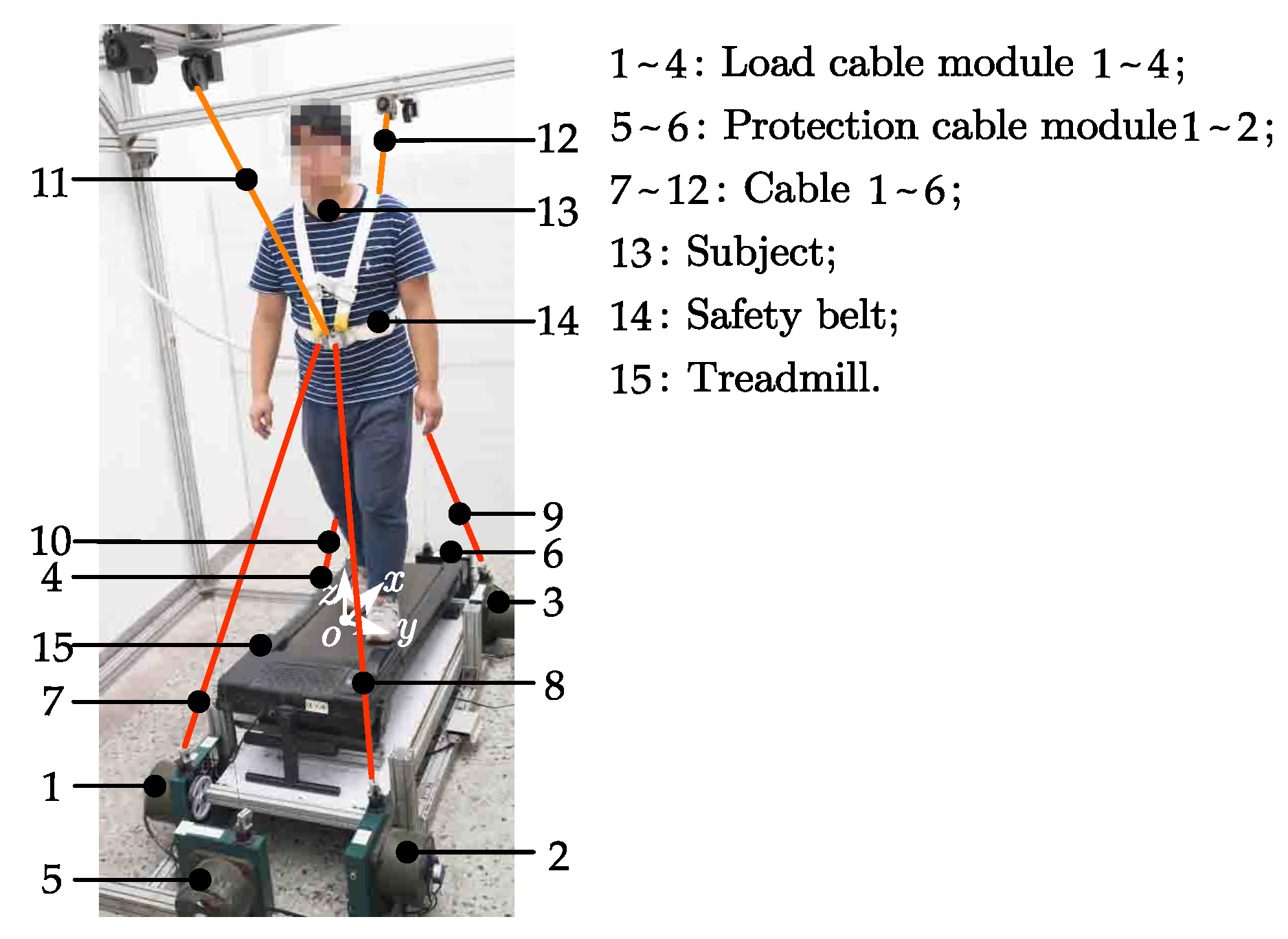
4.2.1. Implementation of the CAPE
4.2.2. Experiment Platform
4.2.3. Data Processing
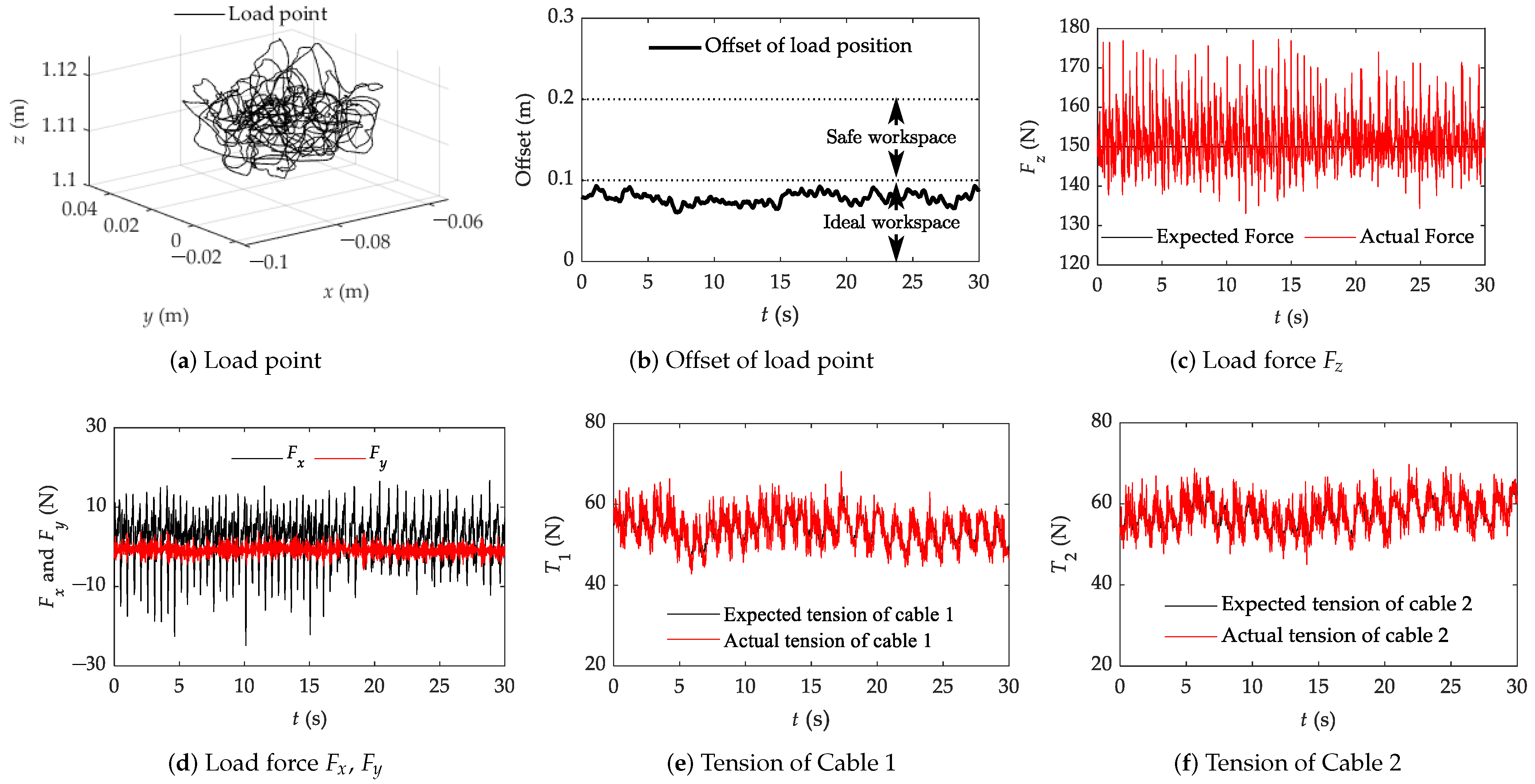
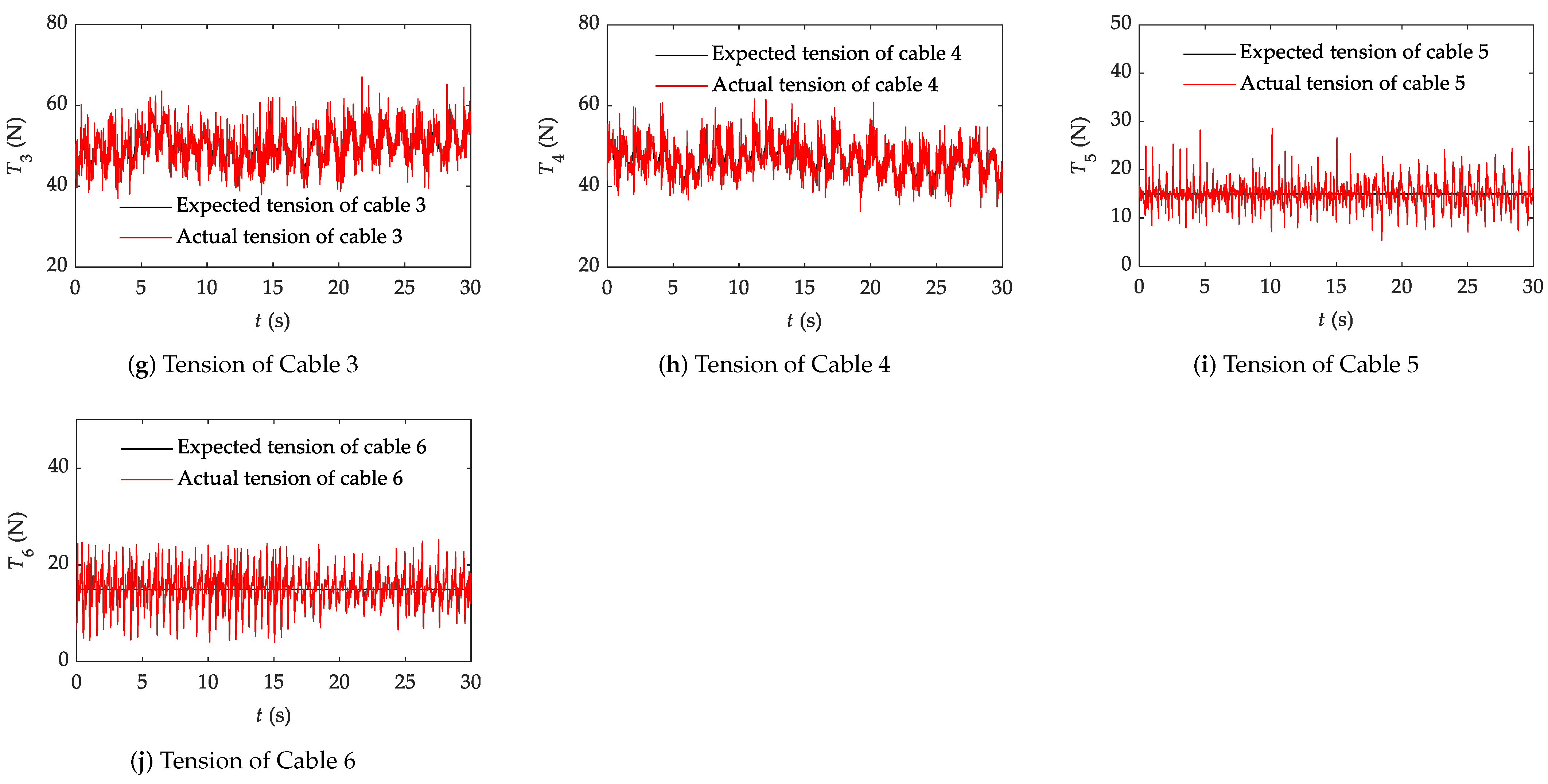
4.2.4. Results
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Komorowski, M.; Fleming, S.; Mawkin, M.; Hinkelbein, J. Anaesthesia in austere environments: Literature review and considerations for future space exploration missions. NPJ Microgravity 2018, 4, 5. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Du, Z.; Cheng, C.; Shen, P. Building a compound and collaborative governance framework to improve international space sustainability. Glob. Public Policy Gov. 2021, 1, 202–224. [Google Scholar] [CrossRef]
- Das, M.C. Space Exploration: It’s Impact on Society—A Critical Review. Int. J. Adv. Technol. Eng. Res. 2018, 1, 92–97. [Google Scholar]
- Maffiuletti, N.A.; Green, D.A.; Vaz, M.A.; Dirks, M.L. Neuromuscular electrical stimulation as a potential countermeasure for skeletal muscle atrophy and weakness during human spaceflight. Front. Physiol. 2019, 10, 1030. [Google Scholar] [CrossRef] [Green Version]
- Löbrich, M.; Jeggo, P.A. Hazards of human spaceflight. Science 2019, 364, 127–128. [Google Scholar] [CrossRef]
- Kandarpa, K.; Schneider, V.; Ganapathy, K. Human health during space travel: An overview. Neurol. India 2019, 67, 176. [Google Scholar]
- Hodkinson, P.; Anderton, R.; Posselt, B.; Fong, K. An overview of space medicine. BJA Br. J. Anaesth. 2017, 119, i143–i153. [Google Scholar] [CrossRef] [Green Version]
- Seidler, R.D.; Koppelmans, V.; Bloomberg, J.; Mulavara, A.P. 10 Sensory and Sensorimotor Changes with Spaceflight. In Intracranial Pressure in Addition, Its Effect on Vision in Space and on Earth: Vision Impairment in Space; World Scientific: Singapore, 2017; p. 225. [Google Scholar]
- Gunga, H.C.; Ahlefeld, V.W.v.; Appell Coriolano, H.J.; Werner, A.; Hoffmann, U. Red blood cells in space. In Cardiovascular System, Red Blood Cells, and Oxygen Transport in Microgravity; Springer: Berlin, Germany, 2016; pp. 35–55. [Google Scholar]
- De Santo, N.G.; Cirillo, M.; Kirsch, K.A.; Correale, G.; Drummer, C.; Frassl, W.; Perna, A.F.; Di Stazio, E.; Bellini, L.; Gunga, H.C. Anemia and erythropoietin in space flights. Semin. Nephrol. 2005, 25, 379–387. [Google Scholar] [CrossRef]
- Myers, J.; Eke, C.; Werner, C.; Nelson, E.; Mulugeta, L.; Feola, A.; Raykin, J.; Samuels, B.; Ethier, C. Microgravity-Induced Physiological Fluid Redistribution: Computational Analysis to Assess Influence of Physiological Parameters. In Proceedings of the 2016 NASA Human Research Program Investigators’ Workshop (HRP IWS 2016), Galveston, TX, USA, 8–10 February 2016. number GRC-E-DAA-TN29818. [Google Scholar]
- Shen, M.; Frishman, W.H. Effects of spaceflight on cardiovascular physiology and health. Cardiol. Rev. 2019, 27, 122–126. [Google Scholar] [CrossRef]
- Demontis, G.C.; Germani, M.M.; Caiani, E.G.; Barravecchia, I.; Passino, C.; Angeloni, D. Human pathophysiological adaptations to the space environment. Front. Physiol. 2017, 8, 547. [Google Scholar] [CrossRef]
- LeBlanc, A.; Lin, C.; Shackelford, L.; Sinitsyn, V.; Evans, H.; Belichenko, O.; Schenkman, B.; Kozlovskaya, I.; Oganov, V.; Bakulin, A.; et al. Muscle volume, MRI relaxation times (T2), and body composition after spaceflight. J. Appl. Physiol. 2000, 89, 2158–2164. [Google Scholar] [CrossRef]
- Crucian, B.E.; Choukèr, A.; Simpson, R.J.; Mehta, S.; Marshall, G.; Smith, S.M.; Zwart, S.R.; Heer, M.; Ponomarev, S.; Whitmire, A.; et al. Immune system dysregulation during spaceflight: Potential countermeasures for deep space exploration missions. Front. Immunol. 2018, 9, 1437. [Google Scholar] [CrossRef] [PubMed]
- Van Ombergen, A.; Demertzi, A.; Tomilovskaya, E.; Jeurissen, B.; Sijbers, J.; Kozlovskaya, I.B.; Parizel, P.M.; Van de Heyning, P.H.; Sunaert, S.; Laureys, S.; et al. The effect of spaceflight and microgravity on the human brain. J. Neurol. 2017, 264, 18–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hurst, C.; Scott, J.P.; Weston, K.L.; Weston, M. High-intensity interval training: A potential exercise countermeasure during human spaceflight. Front. Physiol. 2019, 10, 581. [Google Scholar] [CrossRef] [PubMed]
- Taddeo, T.A.; Gilmore, S.; Armstrong, C.W. Spaceflight medical systems. In Principles of Clinical Medicine for Space Flight; Springer: Berlin, Germany, 2019; pp. 201–231. [Google Scholar]
- Laws, J.; Caplan, N.; Bruce, C.; McGrogan, C.; Lindsay, K.; Wild, B.; Debuse, D.; Wotring, V.; Winnard, A. Systematic review of the technical and physiological constraints of the Orion Multi-Purpose Crew Vehicle that affect the capability of astronauts to exercise effectively during spaceflight. Acta Astronaut. 2020, 170, 665–677. [Google Scholar] [CrossRef]
- Smith, S.M.; Heer, M.A.; Shackelford, L.C.; Sibonga, J.D.; Ploutz-Snyder, L.; Zwart, S.R. Benefits for bone from resistance exercise and nutrition in long-duration spaceflight: Evidence from biochemistry and densitometry. J. Bone Miner. Res. 2012, 27, 1896–1906. [Google Scholar] [CrossRef] [PubMed]
- Loehr, J.A.; Lee, S.; English, K.L.; Sibonga, J.; Smith, S.M.; Spiering, B.A.; Hagan, R.D. Musculoskeletal adaptations to training with the advanced resistive exercise device. Med. Sci. Sports Exerc. 2011, 43, 146–156. [Google Scholar] [CrossRef]
- Scott, J.P.; Weber, T.; Green, D.A. Introduction to the Frontiers research topic: Optimization of exercise countermeasures for human space flight–lessons from terrestrial physiology and operational considerations. Front. Physiol. 2019, 10, 173. [Google Scholar] [CrossRef] [Green Version]
- Shuai, L.; Yang, C.Q.; Yang, M.K. Analysis of the Designing Flaws of the Running Machine Facilitated on Tiangong-2. Mech. Manag. Dev. 2018, 33, 4. [Google Scholar]
- English, K.L.; Newby, N.J.; Hackney, K.J.; Witt, J.K.D.; Beck, C.E.; Rovekamp, R.N.; Rea, R.L.; Ploutz-Snyder, L.L.; English, K.L.; Newby, N.J. Comparison of Knee and Ankle Dynamometry between NASA’s X1 Exoskeleton and Biodex System 4: 1545 Board #285 May 29, 8. Med. Sci. Sports Exerc. 2014, 46, 419. [Google Scholar]
- Rea, R.; Beck, C.; Rovekamp, R.; Neuhaus, P.; Diftler, M. X1: A Robotic Exoskeleton for In-Space Countermeasures and Dynamometry. In Proceedings of the Aiaa Space Conference & Exposition, San Diego, CA, USA, 10–12 September 2013. [Google Scholar]
- Scott, J.P.; Weber, T.; Green, D.A. Optimization of Exercise Countermeasures for Human Space Flight—Lessons From Terrestrial Physiology and Operational Implementation. Front. Physiol. 2020, 10, 1567. [Google Scholar] [CrossRef] [PubMed]
- Laws, J.M. To the Moon, Mars and Beyond: Recommending Exercise Countermeasures against Musculoskeletal and Cardiovascular Deconditioning during Microgravity Exposure, for Future Spacecraft Applications. Ph.D. Thesis, Northumbria University, Newcastle upon Tyne, UK, 2021. [Google Scholar]
- Hidayah, R.; Bishop, L.; Jin, X.; Chamarthy, S.; Stein, J.; Agrawal, S.K. Gait adaptation using a cable-driven active leg exoskeleton (C-ALEX) with post-stroke participants. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 1984–1993. [Google Scholar] [CrossRef] [PubMed]
- Haufe, F.L.; Duroyon, E.G.; Wolf, P.; Riener, R.; Xiloyannis, M. Outside testing of wearable robots for gait assistance shows a higher metabolic benefit than testing on treadmills. Sci. Rep. 2021, 11, 14833. [Google Scholar] [CrossRef] [PubMed]
- Georgarakis, A.M. Stability and Mobility: Textile Assistance for the Shoulder for Everyday Life. Ph.D. Thesis, ETH Zurich, Zurich, Switzerland, 2021. [Google Scholar]
- Kang, B.B.; Choi, H.; Lee, H.; Cho, K.J. Exo-glove poly II: A polymer-based soft wearable robot for the hand with a tendon-driven actuation system. Soft Robot. 2019, 6, 214–227. [Google Scholar] [CrossRef]
- Kim, J.; Lee, G.; Heimgartner, R.; Arumukhom Revi, D.; Karavas, N.; Nathanson, D.; Galiana, I.; Eckert-Erdheim, A.; Murphy, P.; Perry, D.; et al. Reducing the metabolic rate of walking and running with a versatile, portable exosuit. Science 2019, 365, 668–672. [Google Scholar] [CrossRef]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, L.; Zhang, L.; Wang, B.; Xue, F.; Zou, Y.; Song, D. Running Experimental Research of a Cable-Driven Astronaut on-Orbit Physical Exercise Equipment. Machines 2022, 10, 377. https://doi.org/10.3390/machines10050377
Li L, Zhang L, Wang B, Xue F, Zou Y, Song D. Running Experimental Research of a Cable-Driven Astronaut on-Orbit Physical Exercise Equipment. Machines. 2022; 10(5):377. https://doi.org/10.3390/machines10050377
Chicago/Turabian StyleLi, Lailu, Lixun Zhang, Bing Wang, Feng Xue, Yupeng Zou, and Da Song. 2022. "Running Experimental Research of a Cable-Driven Astronaut on-Orbit Physical Exercise Equipment" Machines 10, no. 5: 377. https://doi.org/10.3390/machines10050377
APA StyleLi, L., Zhang, L., Wang, B., Xue, F., Zou, Y., & Song, D. (2022). Running Experimental Research of a Cable-Driven Astronaut on-Orbit Physical Exercise Equipment. Machines, 10(5), 377. https://doi.org/10.3390/machines10050377





