Effect of Reciprocating Gait Orthosis with Hip Actuation on Upper Extremity Loading during Ambulation in Patient with Spinal Cord Injury: A Single Case Study
Abstract
1. Introduction
2. Methods
2.1. Participant
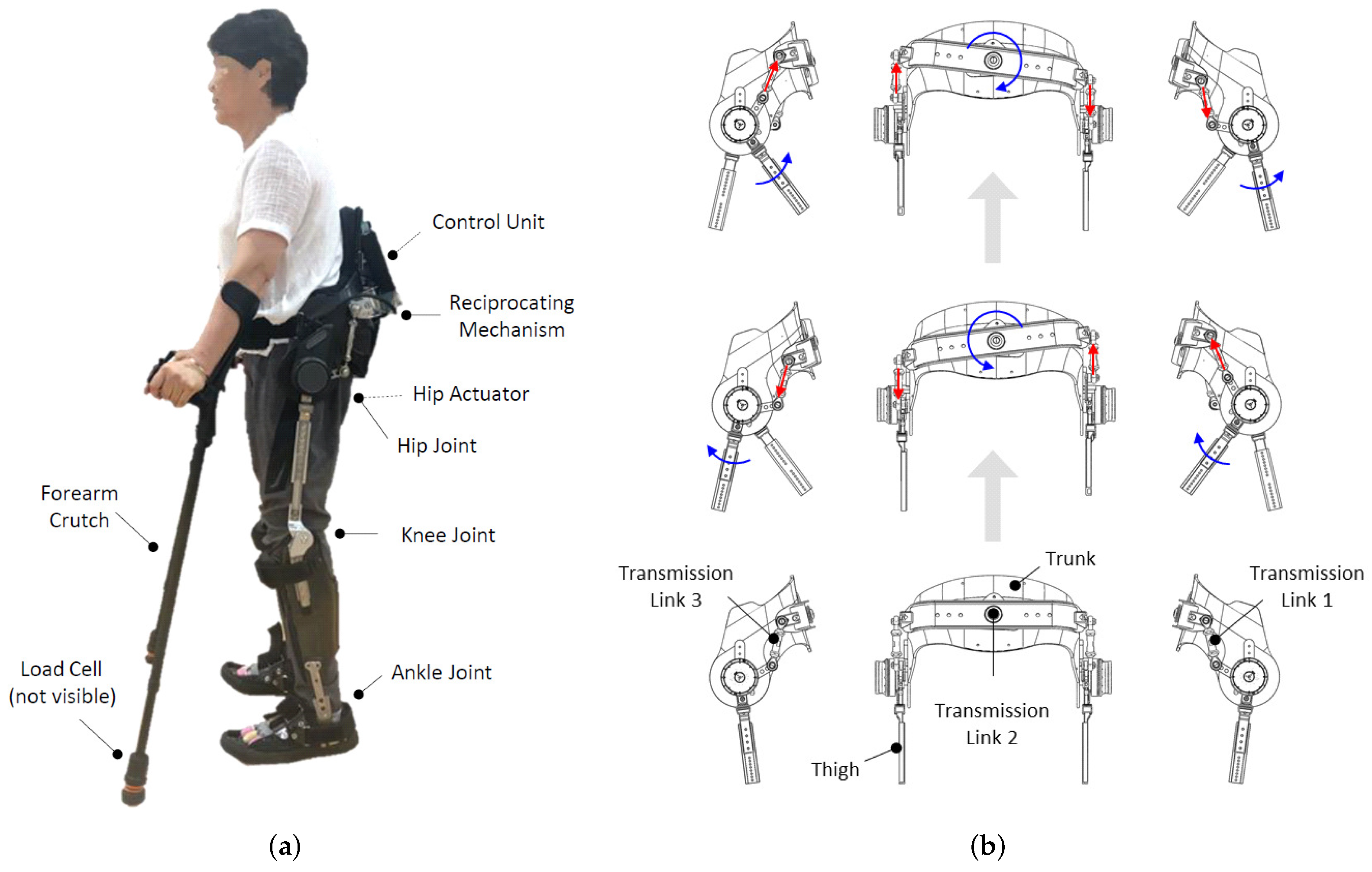
2.2. Reciprocating Gait Orthosis
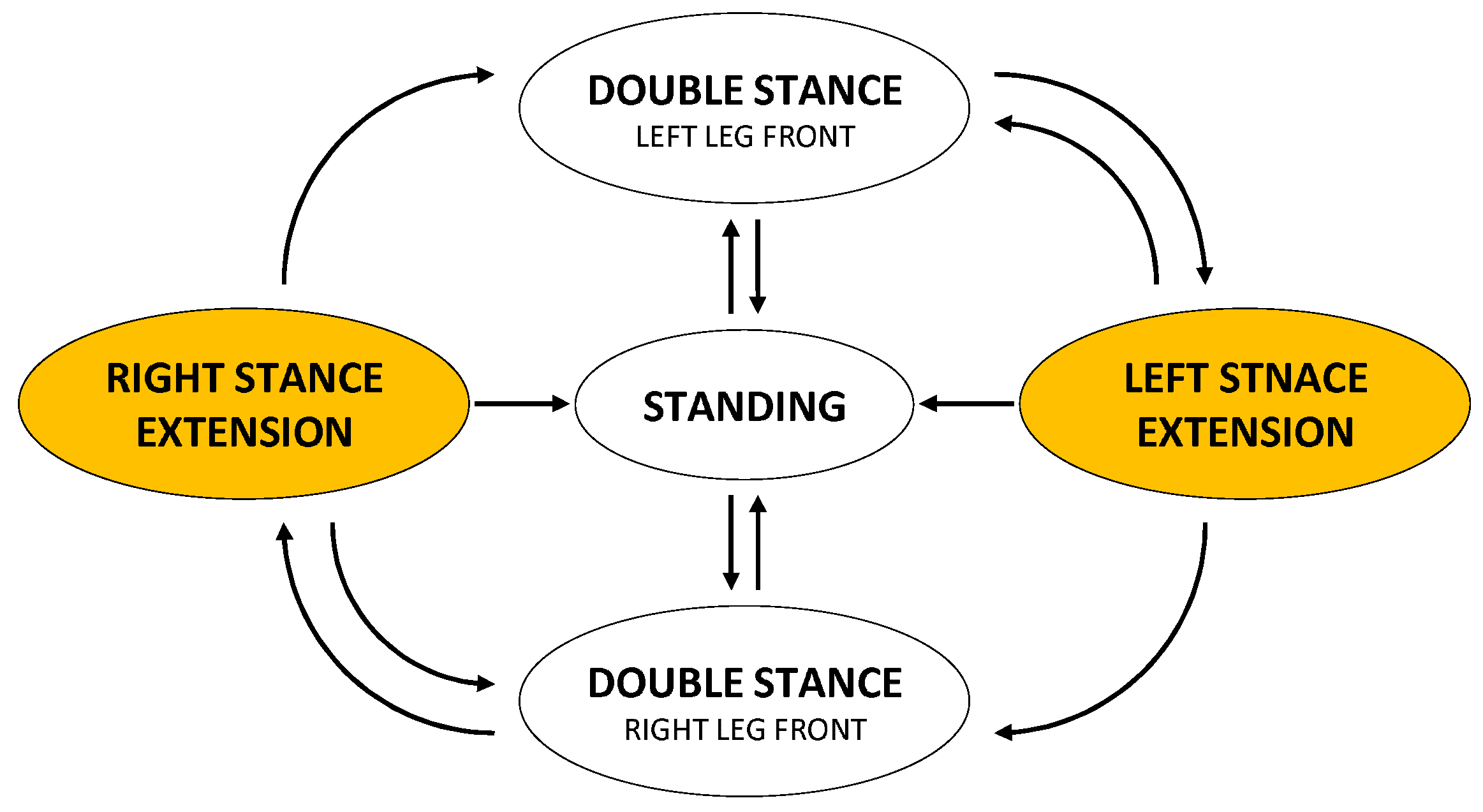
2.3. Sensing and Control
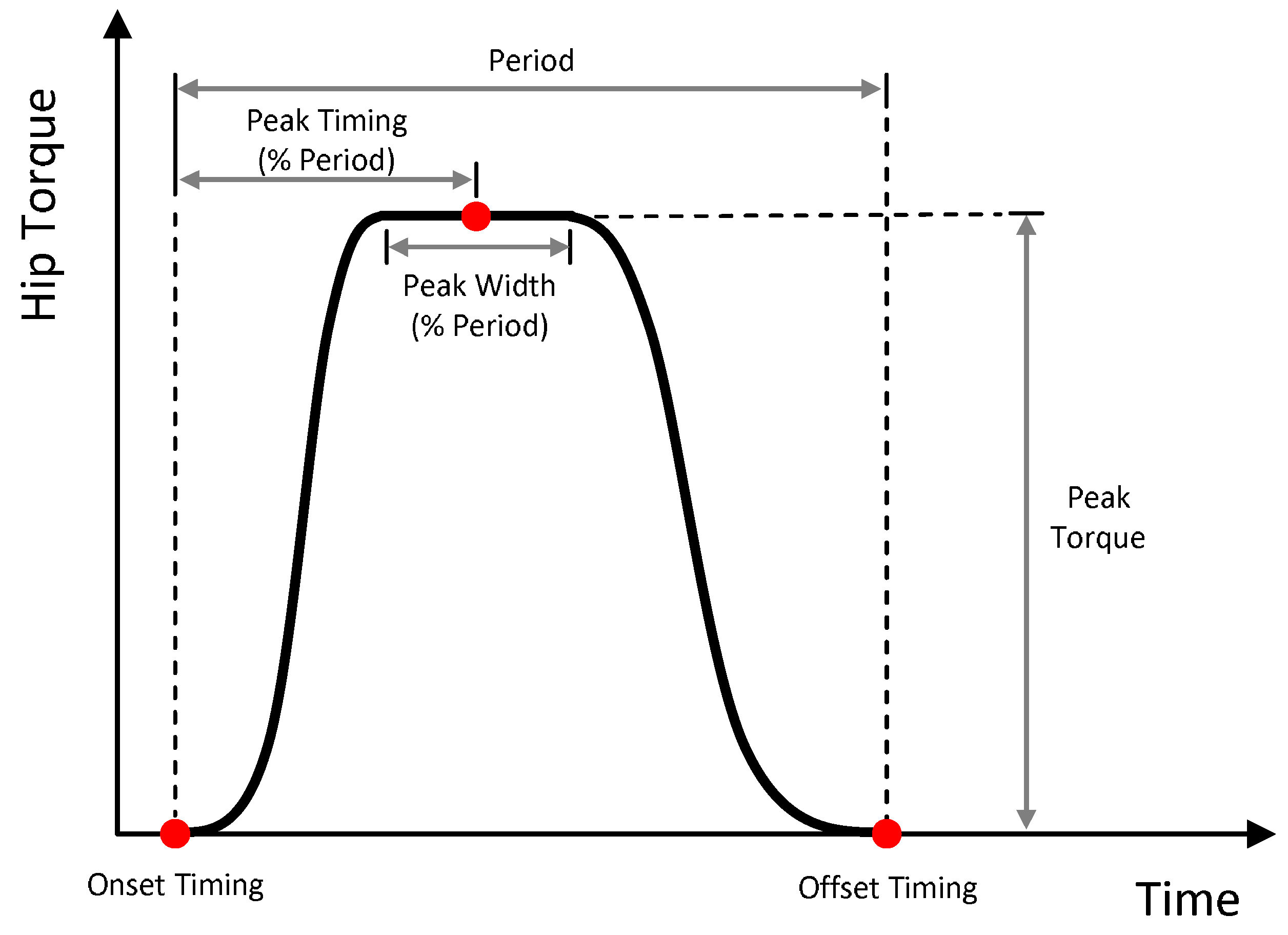
2.4. Hip Actuation
2.5. Experimental Protocol
2.6. Data Collection
2.7. Data Analysis
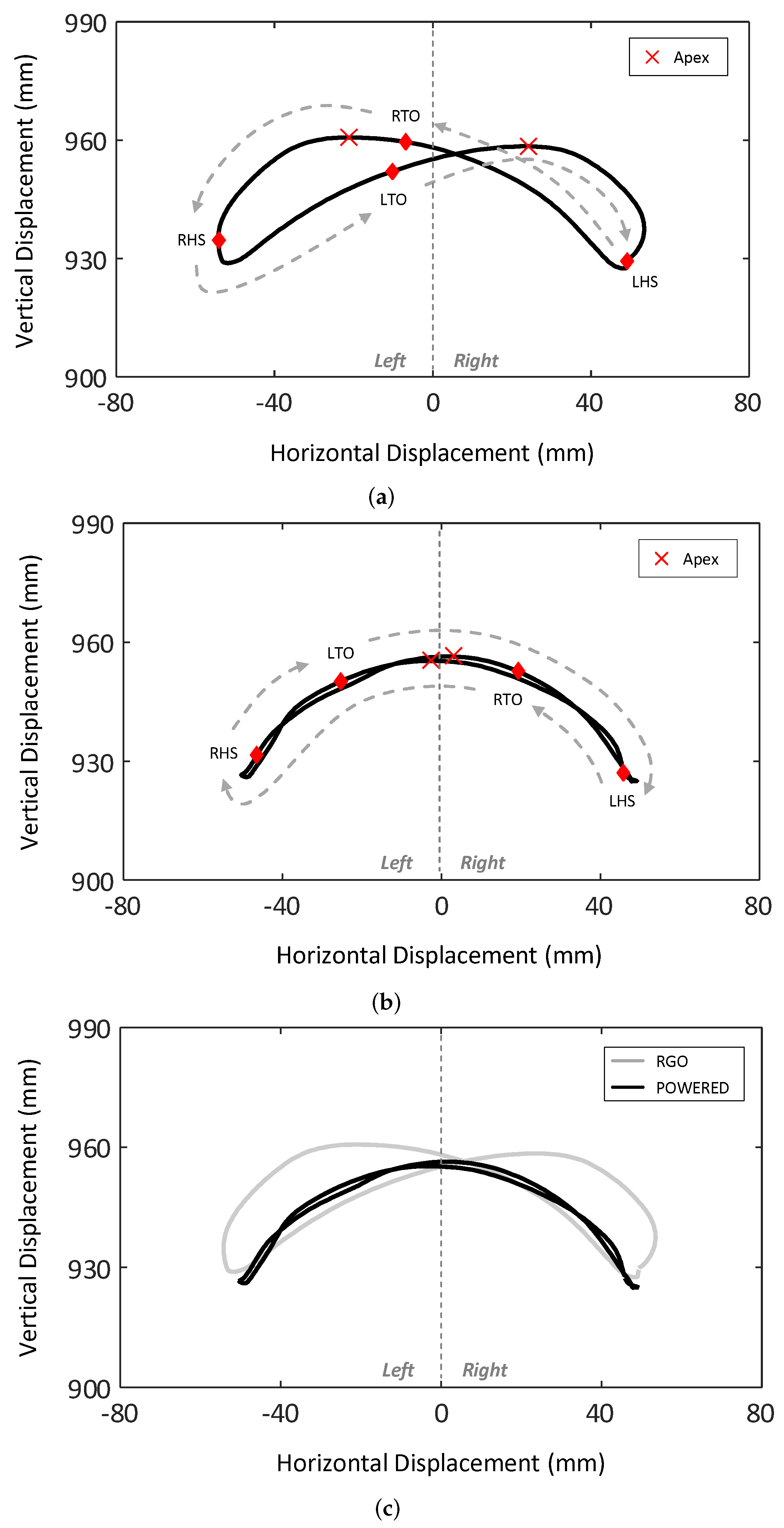
2.7.1. Center of Mass Trajectory
2.7.2. Spatio-Temporal Gait Parameters
2.7.3. Upper Extremity Loading
2.7.4. Statistics
3. Results
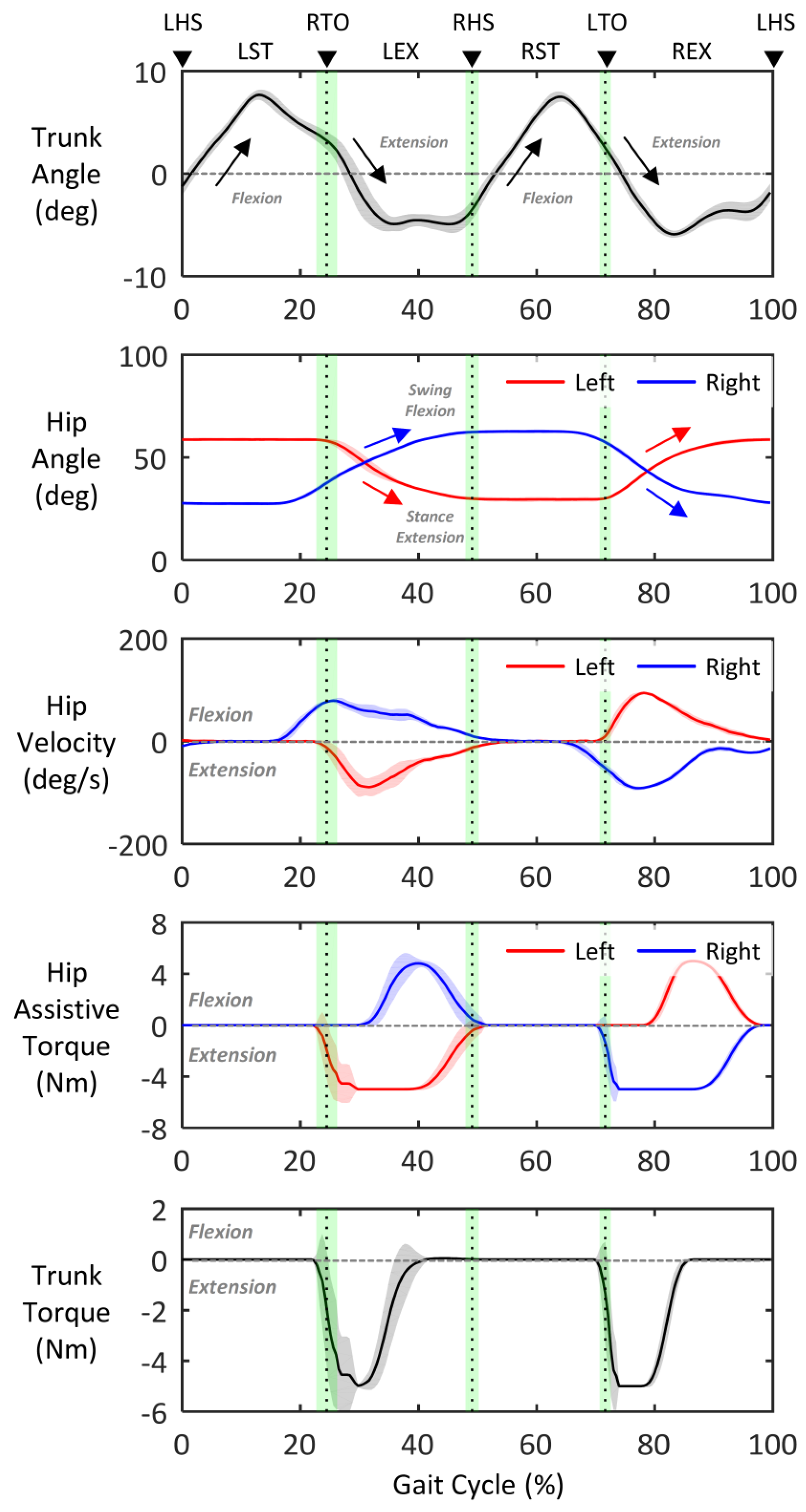
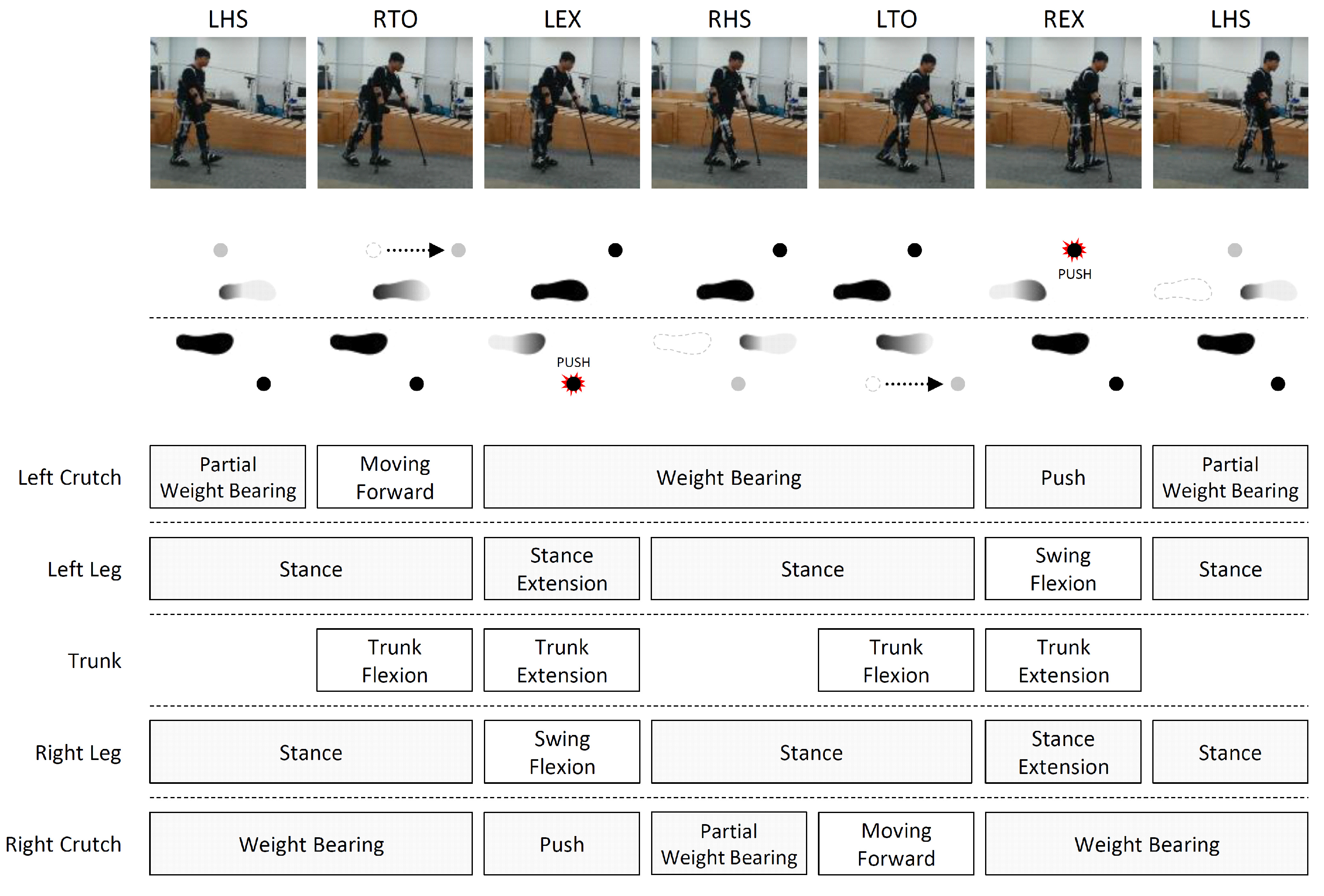
3.1. Gait Pattern
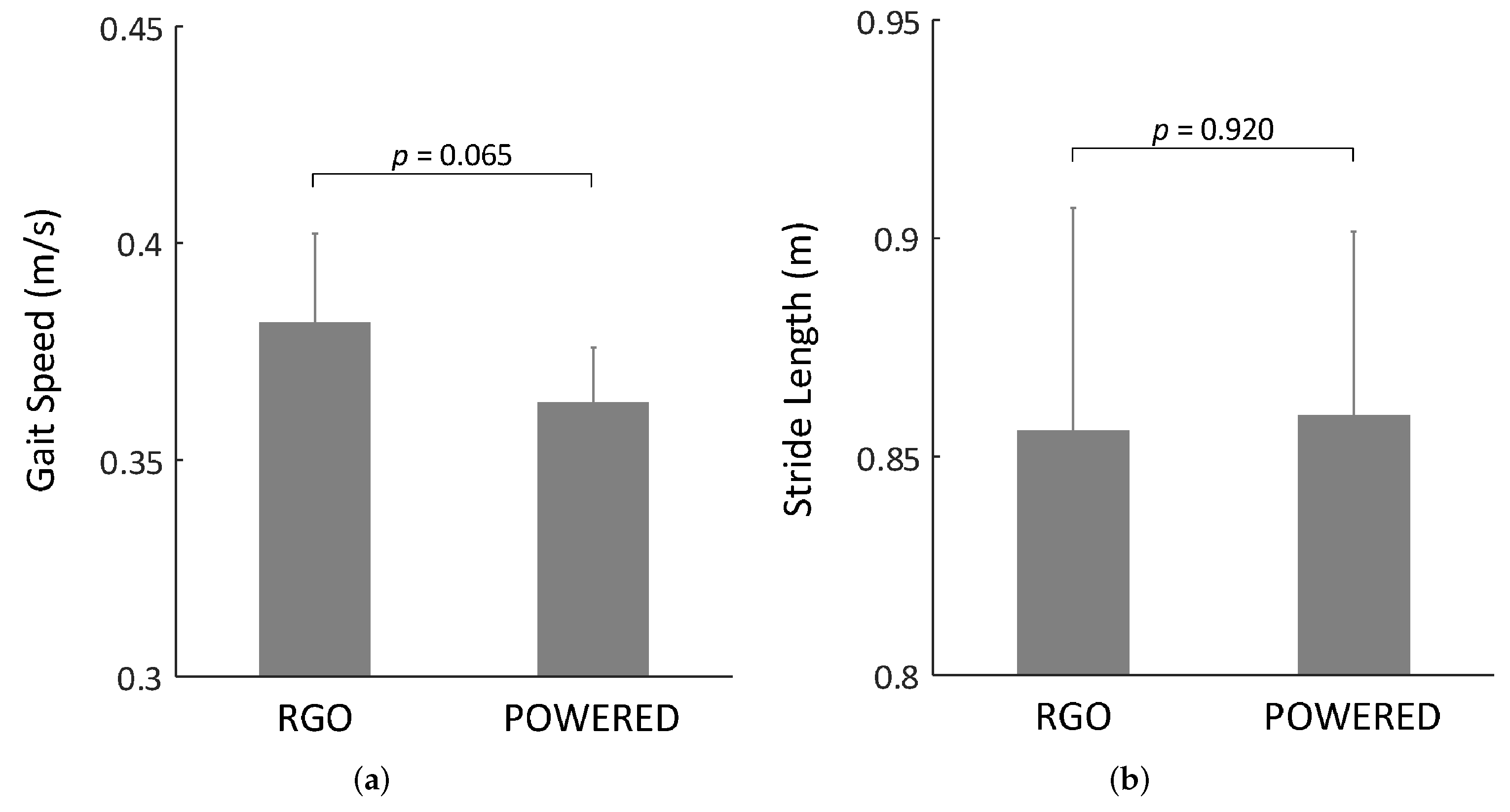
3.2. Spatio-Temporal Gait Parameters
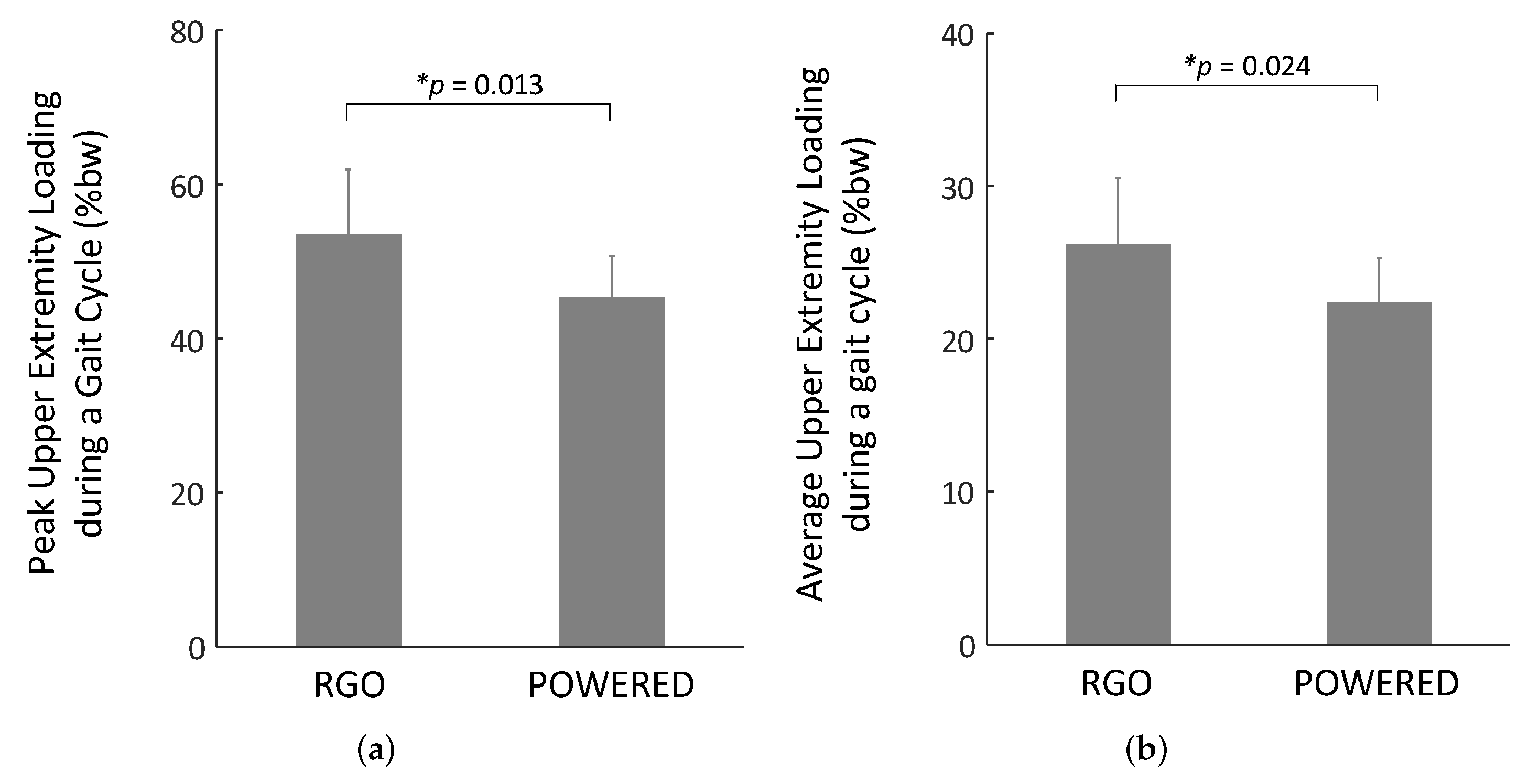
3.3. Upper Extremity Loading
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ditunno, P.; Patrick, M.; Stineman, M.; Ditunno, J. Who wants to walk? Preferences for recovery after SCI: A longitudinal and cross-sectional study. Spinal Cord 2008, 46, 500–506. [Google Scholar] [CrossRef] [PubMed]
- Sezer, N.; Akkuş, S.; Uğurlu, F.G. Chronic complications of spinal cord injury. World J. Orthop. 2015, 6, 24. [Google Scholar] [CrossRef] [PubMed]
- Karimi, M.T. What are the next steps in designing an orthosis for paraplegic subjects? Int. J. Prev. Med. 2012, 3, 145. [Google Scholar] [PubMed]
- Douglas, R.; Larson, P.F.; McCall, R.E. The LSU reciprocation-gait orthosis. Orthopedics 1983, 6, 834–839. [Google Scholar] [CrossRef]
- Jefferson, R.; Whittle, M. Performance of three walking orthoses for the paralysed: A case study using gait analysis. Prosthetics Orthot. Int. 1990, 14, 103–110. [Google Scholar] [CrossRef]
- Whittle, M.; Cochrane, G.; Chase, A.; Copping, A.; Jefferson, R.; Staples, D.; Fenn, P.; Thomas, D. A comparative trial of two walking systems for paralysed people. Spinal Cord 1991, 29, 97–102. [Google Scholar] [CrossRef][Green Version]
- Franceschini, M.; Baratta, S.; Zampolini, M.; Loria, D.; Lotta, S. Reciprocating gait orthoses: A multicenter study of their use by spinal cord injured patients. Arch. Phys. Med. Rehabil. 1997, 78, 582–586. [Google Scholar] [CrossRef]
- Tashman, S.; Zajac, F.E.; Perkash, I. Modeling and Simulation of Paraplegic Ambulation in a Reciprocating Gait Orthosis. J. Biomech. Eng. 1995, 117, 300–308. [Google Scholar] [CrossRef]
- Baardman, G.; IJzerman, M.J.; Hermen, H.; Veltink, P.H.; Boom, H.; Zilvold, G. The influence of the reciprocal hip joint link in the Advanced Reciprocating Gait Orthosis on standing performance in paraplegia. Prosthetics Orthot. Int. 1997, 21, 210–221. [Google Scholar] [CrossRef][Green Version]
- Dall, P.; Müller, B.; Stallard, I.; Edwards, J.; Granat, M.H. The functional use of the reciprocal hip mechanism during gait for paraplegic patients walking in the Louisiana State University reciprocating gait orthosis. Prosthetics Orthot. Int. 1999, 23, 152–162. [Google Scholar] [CrossRef][Green Version]
- Johnson, W.B.; Fatone, S.; Gard, S.A. Walking mechanics of persons who use reciprocating gait orthoses. J. Rehabil. Res. Dev. 2009, 46, 436–446. [Google Scholar]
- Merritt, J.; Miller, N.; Hanson, T. Preliminary Studies of Energy Expenditures in Paraplegics Using Swing-Thru and Reciprocating Gait Patterns. Arch. Phys. Med. Rehabil. 1983, 64, 510. [Google Scholar]
- Sykes, L.; Edwards, J.; Powell, E.S.; Ross, E.R.S. The reciprocating gait orthosis: Long-term usage patterns. Arch. Phys. Med. Rehabil. 1995, 76, 779–783. [Google Scholar] [CrossRef]
- Scivoletto, G.; Petrelli, A.; Di Lucente, L.; Giannantoni, A.; Fuoco, U.; D’Ambrosio, F.; Filippini, V. One year follow up of spinal cord injury patients using a reciprocating gait orthosis: Preliminary report. Spinal Cord 2000, 38, 555–558. [Google Scholar] [CrossRef][Green Version]
- Requejo, P.S.; Wahl, D.P.; Bontrager, E.L.; Newsam, C.J.; Gronley, J.K.; Mulroy, S.J.; Perry, J. Upper extremity kinetics during Lofstrand crutch-assisted gait. Med. Eng. Phys. 2005, 27, 19–29. [Google Scholar] [CrossRef]
- Rasouli, F.; Reed, K.B. Walking assistance using crutches: A state of the art review. J. Biomech. 2020, 98, 109489. [Google Scholar] [CrossRef] [PubMed]
- Melis, E.; Torres-Moreno, R.; Barbeau, H.; Lemaire, E. Analysis of assisted-gait characteristics in persons with incomplete spinal cord injury. Spinal Cord 1999, 37, 430–439. [Google Scholar] [CrossRef]
- Solomonow, M.; Baratta, R.; Hirokawa, S.; Rightor, N.; Walker, W.; Beaudette, P.; Shoji, H. The RGO generation II: Muscle stimulation powered orthosis as a practical walking system for thoracic paraplegics. Orthopedics 1989, 12, 1309–1315. [Google Scholar] [CrossRef] [PubMed]
- Ferrarin, M.; Pedotti, A.; Boccardi, S.; Palmieri, R. Biomechanical assessment of paraplegic locomotion with hip guidance orthosis (HGO). Clin. Rehabil. 1993, 7, 303–308. [Google Scholar] [CrossRef]
- Slavens, B.A.; Sturm, P.F.; Bajournaite, R.; Harris, G.F. Upper extremity dynamics during Lofstrand crutch-assisted gait in children with myelomeningocele. Gait Posture 2009, 30, 511–517. [Google Scholar] [CrossRef][Green Version]
- Lal, S. Premature degenerative shoulder changes in spinal cord injury patients. Spinal Cord 1998, 36, 186–189. [Google Scholar] [CrossRef] [PubMed]
- Pennycott, A.; Wyss, D.; Vallery, H.; Klamroth-Marganska, V.; Riener, R. Towards more effective robotic gait training for stroke rehabilitation: A review. J. Neuroeng. Rehabil. 2012, 9, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Molteni, F.; Gasperini, G.; Cannaviello, G.; Guanziroli, E. Exoskeleton and end-effector robots for upper and lower limbs rehabilitation: Narrative review. PM&R 2018, 10, S174–S188. [Google Scholar] [CrossRef]
- Miller, L.E.; Zimmermann, A.K.; Herbert, W.G. Clinical effectiveness and safety of powered exoskeleton-assisted walking in patients with spinal cord injury: Systematic review with meta-analysis. Med. Devices 2016, 9, 455. [Google Scholar] [CrossRef] [PubMed]
- Zeilig, G.; Weingarden, H.; Zwecker, M.; Dudkiewicz, I.; Bloch, A.; Esquenazi, A. Safety and tolerance of the ReWalk™ exoskeleton suit for ambulation by people with complete spinal cord injury: A pilot study. J. Spinal Cord Med. 2012, 35, 96–101. [Google Scholar] [CrossRef]
- Aach, M.; Cruciger, O.; Sczesny-Kaiser, M.; Höffken, O.; Meindl, R.C.; Tegenthoff, M.; Schwenkreis, P.; Sankai, Y.; Schildhauer, T.A. Voluntary driven exoskeleton as a new tool for rehabilitation in chronic spinal cord injury: A pilot study. Spine J. 2014, 14, 2847–2853. [Google Scholar] [CrossRef]
- Farris, R.J.; Quintero, H.A.; Murray, S.A.; Ha, K.H.; Hartigan, C.; Goldfarb, M. A preliminary assessment of legged mobility provided by a lower limb exoskeleton for persons with paraplegia. IEEE Trans. Neural Syst. Rehabil. Eng. 2013, 22, 482–490. [Google Scholar] [CrossRef]
- Kwon, S.H.; Lee, B.S.; Lee, H.J.; Kim, E.J.; Lee, J.A.; Yang, S.P.; Kim, T.Y.; Pak, H.R.; Kim, H.K.; Kim, H.Y.; et al. Energy efficiency and patient satisfaction of gait with knee-ankle-foot orthosis and robot (ReWalk)-assisted gait in patients with spinal cord injury. Ann. Rehabil. Med. 2020, 44, 131–141. [Google Scholar] [CrossRef]
- Asselin, P.; Knezevic, S.; Kornfeld, S.; Cirnigliaro, C.; Agranova-Breyter, I.; Bauman, W.A. Heart rate and oxygen demand of powered exoskeleton-assisted walking in persons with paraplegia. J. Rehabil. Res. Dev. 2015, 52, 147. [Google Scholar] [CrossRef]
- Neptune, R.; Zajac, F.; Kautz, S. Muscle force redistributes segmental power for body progression during walking. Gait Posture 2004, 19, 194–205. [Google Scholar] [CrossRef]
- Liu, M.Q.; Anderson, F.C.; Pandy, M.G.; Delp, S.L. Muscles that support the body also modulate forward progression during walking. J. Biomech. 2006, 39, 2623–2630. [Google Scholar] [CrossRef] [PubMed]
- Eng, J.J.; Winter, D. Estimations of the horizontal displacement of the total body centre of mass: Considerations during standing activities. Gait Posture 1993, 1, 141–144. [Google Scholar] [CrossRef]
- Gard, S.A.; Miff, S.C.; Kuo, A.D. Comparison of kinematic and kinetic methods for computing the vertical motion of the body center of mass during walking. Hum. Mov. Sci. 2004, 22, 597–610. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Pai, Y.C. Can sacral marker approximate center of mass during gait and slip-fall recovery among community-dwelling older adults? J. Biomech. 2014, 47, 3807–3812. [Google Scholar] [CrossRef]
- Thirunarayan, M.A.; Kerrigan, D.C.; Rabuffetti, M.; Della Croce, U.; Saini, M. Comparison of three methods for estimating vertical displacement of center of mass during level walking in patients. Gait Posture 1996, 4, 306–314. [Google Scholar] [CrossRef]


| State | Condition | Action |
|---|---|---|
| ST | and && | Friction compensation |
| LST | and && && | Friction compensation |
| LEX | == LST) && && | Friction compensation + Hip assistive force |
| RST | and && && | Friction compensation |
| REX | == RST) && && | Friction compensation + Hip assistive force |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.-W.; Bae, J.; Choi, H.-J.; Kwon, C.; Heo, Y.; Cho, H.; Kim, G. Effect of Reciprocating Gait Orthosis with Hip Actuation on Upper Extremity Loading during Ambulation in Patient with Spinal Cord Injury: A Single Case Study. Machines 2022, 10, 108. https://doi.org/10.3390/machines10020108
Lee J-W, Bae J, Choi H-J, Kwon C, Heo Y, Cho H, Kim G. Effect of Reciprocating Gait Orthosis with Hip Actuation on Upper Extremity Loading during Ambulation in Patient with Spinal Cord Injury: A Single Case Study. Machines. 2022; 10(2):108. https://doi.org/10.3390/machines10020108
Chicago/Turabian StyleLee, Jong-Won, Juhwan Bae, Hyuk-Jae Choi, Chilyong Kwon, Yoon Heo, Hyeonseok Cho, and Gyoosuk Kim. 2022. "Effect of Reciprocating Gait Orthosis with Hip Actuation on Upper Extremity Loading during Ambulation in Patient with Spinal Cord Injury: A Single Case Study" Machines 10, no. 2: 108. https://doi.org/10.3390/machines10020108
APA StyleLee, J.-W., Bae, J., Choi, H.-J., Kwon, C., Heo, Y., Cho, H., & Kim, G. (2022). Effect of Reciprocating Gait Orthosis with Hip Actuation on Upper Extremity Loading during Ambulation in Patient with Spinal Cord Injury: A Single Case Study. Machines, 10(2), 108. https://doi.org/10.3390/machines10020108






