Abstract
In the face of an increasingly high-demand environment for outpatients, achieving a balance between allocation of limited medical resources and patient satisfaction has considerable social and economic benefits. Therefore, appointment scheduling (AS) system operation is used in clinics and hospitals, and its operation optimization research is of great significance. This study reviews the research progress on appointment scheduling system optimization. Firstly, we classify and conclude the existing appointment scheduling system structures and decision-making frameworks. Subsequently, we summarize the system reliability optimization framework from three aspects: appointment scheduling system optimization objectives, decision variables and constraints. Following that, we methodically review the most applied system optimization algorithms in different appointment scheduling systems. Lastly, a literature bibliometric analysis is provided. During our review of the literature, we observe that (1) optimization methods in ASs predominantly involve the application of genetic algorithms and simulation optimization algorithms; (2) neural networks and deep learning methods are core technologies in health management optimization; (3) a bibliometric analysis reveals a heightened interest in the optimization technology of ASs within China compared to other nations; and (4) further advancements are essential in the comprehensive optimization of the system, exploration of practical usage scenarios, and the application of advanced simulation and modeling techniques in this research.
Keywords:
appointment scheduling; optimization algorithm; healthcare; system structure; queuing theory; literature bibliometric MSC:
90B22
1. Introduction
Healthcare extends beyond medical care and encompasses the delivery of services aimed at promoting, preserving, monitoring, or restoring health for individuals or communities through the expertise of healthcare professionals or services [1]. The development of the healthcare system is more important over the past few decades, and it is facing increased costs, increasing number of users, a more conscious population about healthcare issues, and increased demand for quality healthcare services [2]. Most countries are experiencing ageing and population growth, which led to an oversupply of doctors, unequal distribution of resources and inefficiency. This shows that the experience of the healthcare system affects the economy and prosperity of cities around the world [3,4,5].
The scheduling of outpatient departments has become more important in healthcare systems aiming at the efficient utilization of available hospital resources to provide satisfactory services to patients. Patient access to healthcare services and extended wait durations have been identified as major problems in ambulatory care systems [6,7]. It affects the productivity, pressure, and effectiveness of medical staff, as well as the cost and availability, quality, and efficiency of care. Various factors can impact the performance of outpatient delivery systems, including the clinic’s environment and conditions, the adopted appointment policies, the timeliness of patients, and the unpredictability of demand [8]. Appointment scheduling (AS) is an indispensable part of the efficient operation of an outpatient clinic, which improves the utilization of healthcare resources such as personnel and equipment. The core problem of AS is to reduce patient waiting and doctor downtime by creating an appointment system that assigns an available time slot to the patient [9]. Appointment scheduling constitutes a challenge in allocating resources amid uncertainty within the field of IE/OR. A decision-making process is needed to reduce operational costs and improve health management services [10,11,12,13].
With the advancement of modernization of medical technology and the continuous growth of patient consultation in recent years, AS will have a wider application in the future. Therefore, theoretical value and significance are associated with the research on optimizing AS operations. By conducting optimization calculations, an AS system is formulated to improve the efficiency of medical operation [14,15,16]. There are many related studies on AS system optimization.
As a result, various reviews concerning appointment scheduling systems have surfaced in recent years. For instance, Cayirli et al. [17] studies problem formulation and modeling considerations used in the previous literature about appointment scheduling in outpatient services. Amir et al. [18] reviewed studies focusing on decision-support tools for the design and planning of OASs. It offered a structured approach to organizing the latest literature based on various criteria, including a framework for classifying decisions across strategic, tactical, and operational levels. Elizabeth et al. [19] documented patient self-scheduling, along with its advantages and intervention characteristics. Moreover, Marynissen et al. [20] introduced multi-appointment scheduling problems in hospitals and used them to classify the scientific work on MASPHs published before the end of 2017. Ali et al. [21] published a review for the complexity of the appointment scheduling problem. Concomitantly, they presented a critical review of the simulation appointment scheduling system (SASS) research topic, and highlighted critical challenges and outlined potential research topics [22].
A well-designed appointment scheduling system requires many rule constraints; in fact, missing or delaying appointments can reduce the efficiency of outpatient clinic operations and increase healthcare costs. Research on the behavior of patients who missed appointments is also an important direction. Gupta et al. [3] offered a comprehensive synthesis of previous research related to the AS environments and decisions within primary care clinics, specialty clinics, and hospitals. Leila et al. [23] provided a systematic literature review (SLR) on appointment scheduling no-shows; their study analyzes the characteristics of existing research, synthesizes results on factors impacting missed appointment rates, and compares these findings with previous studies. Wilson et al. [24] explored absences within the National Health Service in terms of causes (inefficiencies in appointment systems, traditional reminder failures and inconvenient scheduling), the effects of missed appointments and explores potential strategies.
However, a comprehensive review summarizing methods and techniques for optimizing AS systems is still lacking. Therefore, to help designers and researchers in addressing challenges and giving recommendations for the practical implementation of AS system operations, this paper examines the previous studies on AS system optimization across three dimensions: (1) system structure classification; (2) optimization framework; and (3) optimization algorithms. Additionally, this paper includes a literature bibliometric analysis of prior research on AS system optimization. This paper contributes a comprehensive review dedicated to AS system optimization, unlike previous partial reviews. First, it is a review focusing on AS system optimization, whereas previous reviews have only partially addressed this issue. Second, optimization methods are discussed in terms of system structure, optimization framework and optimization algorithms. Finally, this paper includes the bibliometric analysis of the literature, serving as an additional reference to illustrate the development of our matter.
For the literature bibliometric analysis, we adopt a bibliometric methodology. This methodology is a quantitative approach to analyzing the scientific literature, providing insights into the characteristics, trends, and impact of research within a particular content or across various disciplines. This approach obtains a literature overview, identifies thematic gaps by systematically collecting and analyzing bibliographic data, including citation patterns, author trends, publication outputs and other relevant bibliographic elements to understand the current state of the research and identify new research ideas [25].
This paper provided a SLR of AS system optimization. A systematic literature review is a structured methodology widely used in academic research, healthcare, social sciences, etc., to provide a comprehensive overview of existing knowledge, to help identify gaps in research, and at the same time to guide future research directions. It is recognized as a valuable tool for evidence-based decision-making.
The remainder of this study is organized as follows. Section 2 provides an overview of the structure of AS system. Section 3 studies the optimization of AS systems in optimization objectives, decision variables and constraints. Section 4 explores various primary algorithms utilized. Section 5 includes the literature bibliometric analysis on the optimization of AS system. Section 6 discusses the status and trends in the development of AS systems in different countries. Section 7 gives a summary of the article.
2. System Structure of AS
2.1. AS Characteristics
The scheduling of appointments within outpatient departments stands as an extensively investigated subject, playing a pivotal role in facilitating the efficient utilization of clinical services. It is a topic that demands in-depth research, given its significance in ensuring timely access to high-quality care for patients. In outpatient services, a central issue for scheduling staff is how to allocate available time slots for patients, thereby reducing patient delays and physician availability or additional time [26,27]. The role of appointment scheduling systems in optimizing quality healthcare has been recognized as a challenging problem [28]. Appointment scheduling systems are a well-positioned and practical research area. Unlike the traditional way of registering for appointments, it avoids crowd gathering as well as the unknown nature of patient scheduling, and greatly improves the services’ efficiency, which is an emerging field of research within healthcare [29,30,31]. The attributes of ASs are primarily evident in two aspects:
- Uncertainty AS performance;
Patient unpunctuality is common in many healthcare organizations, and even failure to show up for appointments exists. Patients arriving earlier or later can complicate the AS system design. Late or no-show patients can lead to doctor availability affecting the waiting time of subsequent patients thus reducing efficiency [32,33]. At the same time, the AS system considers that doctors are not always on time, and the nature of their work leads to the possibility that they may not always arrive on time when they are on the operating table or in emergency resuscitation ward consultations [34,35]. The AS system considers the changing circumstances of both parties and thus conducts outpatient scheduling.
- 2.
- ASs can be extended to represent other industries.
AS system design and analysis are very complex. AS systems need to consider nurses and other medical tests or other staff operating diagnostic machines and assisting patients, so the appointment scheduling plan is mainly considered as a resource focused on physician professors [36,37]. It is also comprehensive to consider that nurses and other staff members are assigned to diagnostic resources before patients can be scheduled for further consultation. The AS problem is a resource allocation problem, and the establishment of AS systems can be extended to multiple other resource-limited industries. Outside of healthcare, transportation, hospitality, restaurant reservations, etc., have been referenced and improved in terms of operations, profit models, and customer wait times [38,39,40].
2.2. System Structure of AS
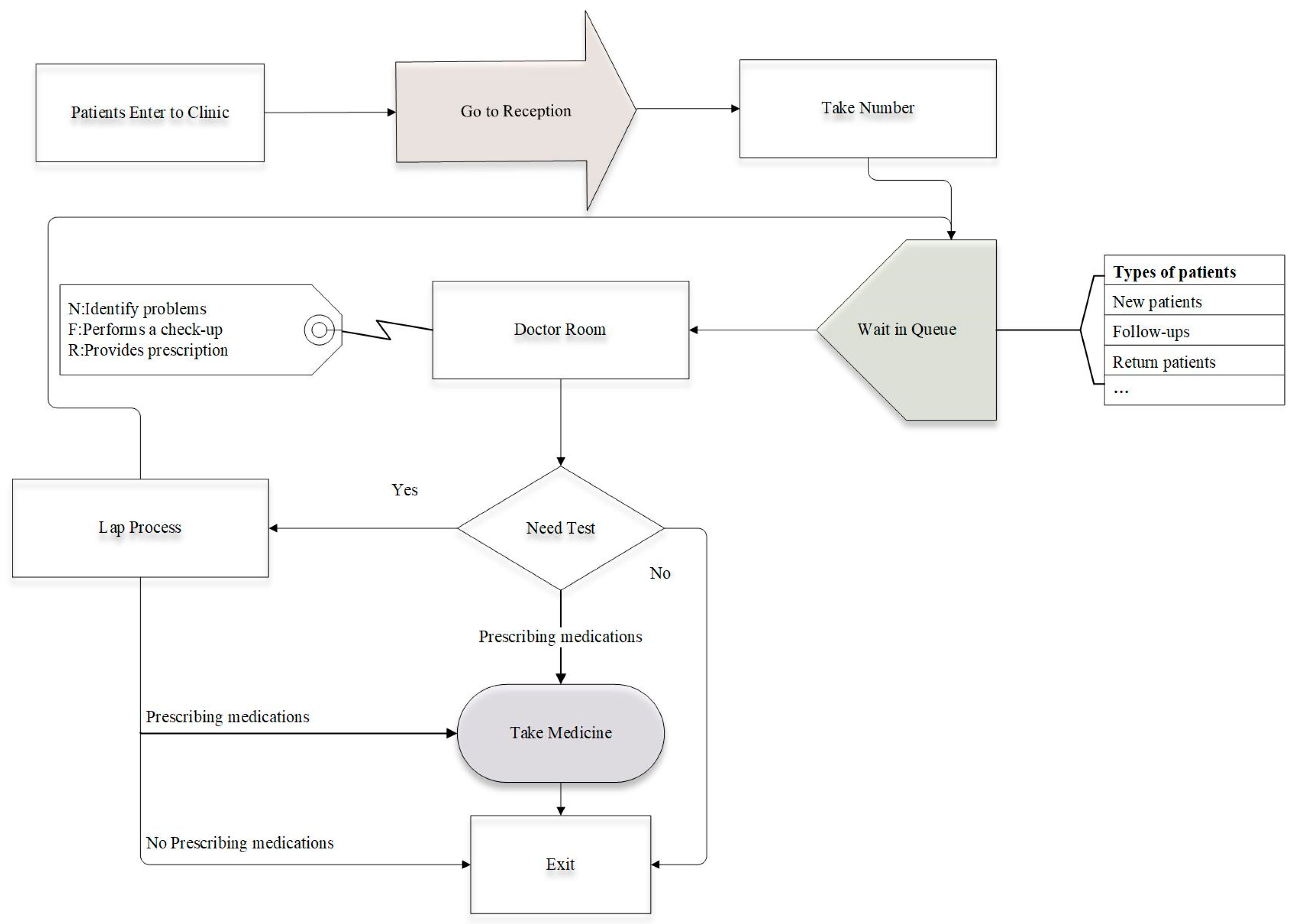
The prerequisite for building an AS system is to be familiar with the patient consultation process, as we all know, anyone who wants to consult needs to arrive at the hospital outpatient clinic as early as possible, and then go to the registration desk to obtain a number (even if you use the online advance booking needs to be in accordance with the booking time to report to the queue and wait). After receiving your number, you will wait in the designated viewing area and meet with the doctor when you are called. After the consultation, the patient may need to undergo further tests and return to the queue to consult with the doctor again after receiving the results [41]. Figure 1 illustrates the structure of the process for the patient’s outpatient consultation in a clinical setting. The AS system design is viewed as a range of decision-making hierarchies, including appointment rules, classification of patients, and adjustments for reducing the disruptive effect of no-shows, walk-ins, and emergency patients [42].
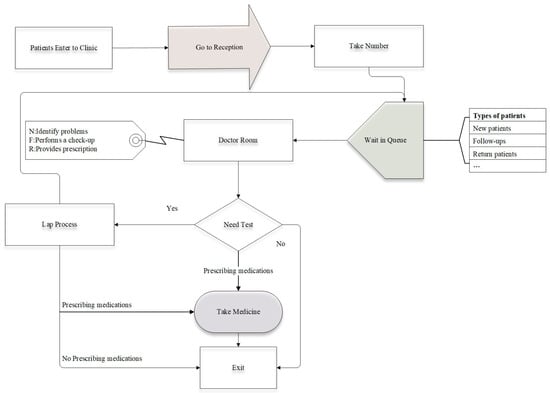
Figure 1.
The flow structure of the patient in the hospitals.
2.2.1. Appointment Rules
AS system operation optimization typically improves healthcare system performance by designing AS rules. These regulations describe the duration of each appointment interval and the number of patients (block size) to be accommodated during that interval. By utilizing various permutations of fixed and variable appointment interval lengths, several innovative rules have been developed to make the operation of the system more responsive to actual consultation needs [17]. The appointment rules of the AS system are expressed in terms of block-size (: the number of patients assigned per block ), begin-block (:patients assigned the same appointments at the session’s outset), and appointment interval (: the interval between two consecutive appointments). The block size and the scheduling interval can be fixed or variable, so the reservation rules composed by the combination of any of its three variables () [43].
- Fixed-interval rules.
The fixed-interval rule refers to equal intervals throughout the consultation. The intervals between the first patient and the subsequent patient and between every two subsequent patients are fixed, i.e., ai is constant. There are some differences in the other two variables under the fixed-interval rule. Simply, the IBFI (individual-block/fixed-interval rule) assigns individual appointments to every patient with equal intervals throughout the consultation, meaning that [44]. Considering the patient’s late arrival or no-show, it is possible to increase the number of appointments at the beginning of the meeting for the same time patient refers to n1 > 1. Avoiding the phenomenon of doctor’s idleness improves the efficiency of healthcare workers. Bailey et al. [45,46] proposed an individual-block system assigning two patients at the session’s start and scheduling the rest at intervals matching the mean consultation time. This highlights the need for thorough research into outpatient appointment scheduling ().
The multiple-block/fixed-interval rule can be interpreted as assigning m patients to the appointment slot with a constant appointment interval. The multiple-block rule performs better when the consultation time is shorter, and the rise in patient numbers in the same appointment time slot allows for more flexibility in the physician’s and patient’s time. Soriano et al. [47] studied a system in which patients are scheduled in pairs, with intervals set at twice the mean consultation time. In fact, block-size can also be variable; the rules allow variations in block sizes throughout the clinic session.
- 2.
- Variable-interval rules.
Rules with constant intervals are in fact unlikely to perform well in all environments, so more research has focused on optimizing AS systems using variable interval rules. This rule is to schedule patients individually when the interval is variable. Considerations are made for walk-ins, no-shows, and urgent cases whenever they occur during the planning of an AS [48]. Therefore, there is a need to adjust AS by making advanced predictions to reduce their damaging effects. The literature suggests two solutions. The first is to book other patients into a single slot in the presence of no-shows and maintain some vacant slots for walk-ins [49]. The other method is to adjust the appointment interval so that it is proportional to the probability [50]. Universal rules are proposed, for example, the” offset” rules, the” dome” rules and the “plateau-dome” rules.
- The “offset” rule.
The “offset” rule refers to a set of rules which modifies the appointment times based on the allocated appointment slots. A framework of different reservation rules for different operational environments is established, which emphasizes that there is no “universally good” rule, and that the appropriate rule needs to be selected by determining the value of some environmental factors. Rohleder et al. [51] applied the offset as shown in Equation (1), where the early time slots are below the average service duration and the late time slots are even longer, which in various situations leads to a very late end of the session.
where Ti is the planned time for client i appointment, as is the standard time for s, and is variability in service time. The parameters , are the early breakpoints, delay breakpoints and the multipliers. controls the earliness rate imposed on the first patients and the rate of lateness imposed on the remaining patients.
- The “dome” appointment rule.
The most prominent finding in the study of variable interval rules is the “dome” rule, including absences and appointments, and patient categorization. The universal appointment rule demonstrate effective performance, independent of the clinical environment [52]. Optimal scheduling exhibits a dome pattern, whereby appointment intervals begin to grow later in the session and then decrease. Dome mode reduces wait times compared to other scheduling rules [53]. Considering no-shows and walk-ins, the patient count scheduled to achieve the target T patients served at a session is calculated as follows [54].
In this formula, is that a patient fails to attend and is the probability of coming without an appointment.
The appointment times are determined through a two-step process employing the subsequent formula:
In this formula, is the patient ’s scheduled time, with the mean duration of service μ, and variability in service time . The k controls the appointment intervals for different appointment rules by setting different values. π is a parameter utilized to establish a pattern resembling a “dome” in the appointment intervals.
In Equation (4), is the coefficient of variation; and CR is the ratio of the cost of the doctor’s time to that of the patients’ time.
Considering the combined impact of no-shows and walk-ins on the consultation durations, the updated formulas for the mean and variance are shown:
- The “plateau-dome” appointment rule.
Doctors could find advantages in implementing a “plateau-dome” rule with fixed individual blocks evenly distributed in the middle of the appointment session [55], explicitly modelling the impact that the doctor’s interruptions may have on optimal appointment times, and thereby affecting waiting times for patients. A traditional pattern for the high number of interrupts and flat dome mode for a low number of interrupts performs better [56]. This was achieved by conducting an additional run with the supplementary constraint:
In this formula, is the appointment time, and and are the appointment slots corresponding to the beginning and end of the plateau portion, respectively.
2.2.2. Patient Classification
Several investigations have explored the implementation of patient classification (PC) based on the assumption that populations can be categorized into distinct groups. For example, in practice, a prevalent method of classifying patients is according to whether they are new or old who have been examined for a different length of time. This allows patients to be sorted at the time of the appointment, and diversity in consultation duration is combined by patient categorization to adjust the length of the appointment interval according to the characteristics of each group. Most studies are only concerned with the scheduling of patients attending elective appointments [57]. Meersman et al. proposed the scheduling horizon involves the time slots for elective and urgent patient categories [58], considering the slot allocation of non-elective patients.
Cayirli et al. [59] proposed to consider generic extended “dome” rules for patient classification to schedule and order appointments by distinguishing patients based on the average and variability in service time. The alternative appointment system was tested by simulation using the generic dome rules. Equation (8) represents the appointment times ():
In Equations (8) and (9), class A and B are two patient groups, where class A is characterized by distinct mean and standard deviation in service times and probabilities. The parameter π contributes to forming a dome pattern within the appointment interval, where , .
Salzarulo et al. [60] introduced a methodology for heterogeneous scheduling (HS) wherein appointment times are established by forecasting examination durations using the individual characteristics of the patient rather than traditional patient classifications. Several models were calculated to evaluate how patient characteristics influence appointment schedules. And three levels (HS1, HS2, HS3) of information usage were considered when making appointment schedules.
2.3. AS System Decision Framework
In AS system design and planning, a range of decisions and planning determine the main structure of the optimization research system. They can be categorized into three types which are strategic, tactical and operational [18]. Strategic decisions are the keys in shaping the modeling process and determining the practical applicability of the proposed solutions. Such decisions are usually considered as inputs to the AS system. Tactical decisions aim at determining the system structure. While operational decisions rely on the first two to develop optimization models and rules. In Table 1, their features and related studies are summarized.

Table 1.
The features and related studies of AS system decision framework.
2.3.1. Strategic Decisions
Strategic decisions are considered as inputs and are long-term decisions that determine the main structure of the AS system. Robinson et al. [61] proposed three main types of access strategies for scheduled patients: traditional, open access, and hybrid. Traditional policies mean all capacity is allocated to pre-scheduled patients, which results in higher no-show rates and longer wait times. Qu et al. [62] proposed a policy that allocates all capacity to one-day appointments to prevent the worse impact of high absenteeism rates under traditional policies and meet same-day demand, which bring low resource utilization. Resource allocation is an important step in designing AS systems. The main resources considered in many studies include clinical staff, medical equipment, rooms and beds/chairs [63]. The number of servers and resource levels are key factors affecting clinic profits. High resource levels can be costly and wasteful, while low levels can increase latency services, thereby reducing care quality and clinic revenue [64].
Walk-in patients refer to patients who go to the clinic without an appointment during the consultation period. Accepting appointments is a means of mitigating the negative impact of no-shows while increasing modeling complexity due to the dynamic random arrival of non-appointment patients [65]. Appointment scheduling methods are categorized into online and offline [66]. In the offline method, arranged once all requests have been received, whereas in the online method, patients are promptly scheduled after requests arrive. Pérez et al. [67] proposed to categorize the patient and resource scheduling problem into three aspects: offline, online and stochastic online. Stochastic online scheduling is an extension of the concept of online scheduling. With the development of the Internet, online systems are gradually becoming the subject of research.
2.3.2. Tactical Decisions
The primary purpose of approaching the decision problem at the tactical level is to characterize the system to optimize resource utilization and the integrity of the consultation service. For example, in allocating capacity among various groups, the decision should consider factors such as the needs of each patient group, prioritization, probability of absence, revenue per patient group, and patient and physician preferences [68], which affect the absence rate and hence the system efficiency. A decrease in the scheduling window results in a reduction of indirect wait time, consequently leading to decrease the absence rate. This enables a more effective use of the clinic’s capacity. Excessive constraints on scheduling windows may result in a reduced patient count, leading to a decline in clinic revenue [69]. Issues such as appointment intervals (slots), block size, panel size, etc., are essentially capacity allocation issues as well, affecting tactical-level decisions [70,71,72].
2.3.3. Operational Decisions
Operational decisions are associated with plans at the individual-patient level. Rule-based approaches (RBA) and optimization-based approaches (OBA) are used to determine these decisions [68]. RBA refers to a set of instructions having associated rules and parameters, but it does not guarantee the realization of optimal performance compared to OBA. Whereas OBA specifies the level of operational decisions, its goal is to attain globally optimal answers for operational decisions [73].
Early research on appointment scheduling usually focused on RBA [17]. In scenarios with homogeneous patients, the primary scheduling rule combines two factors: the appointment interval and block size. Appointment time handling is aimed at the issue of scheduling a specific time for a patient to begin treatment to optimize performance criteria. Most models proposed for the appointment time decision problem use simplifying assumptions (e.g., offline scheduling, on-time patients, single-phase service) [74]. That time is usually combined with the appointment date problem, which refers to determining the appointment date for each patient [75] to satisfy restrictions on patient prioritization and the waiting time objective. Most of the problems such as appointment date and patient selection from list of waiting are usually solved using OBA [14].
3. Optimization Framework
There are several optimization objectives: societal benefit, economic performance, and capacity utilization. A summary of their contributions and relevant studies can be found in the following Table 2.

Table 2.
Contribution of different optimization objectives and related studies.
3.1. Optimization Objective
3.1.1. Societal Benefit
Many studies in the literature on AS have been devoted to minimizing pathway completion time or maximizing patient satisfaction, which leads to better societal benefits and is the primary goal that hospital management needs to follow. The key performance indicators for minimizing the time to complete all tasks include the average waiting time of patients (WAIT), the average idle time of physicians (IDLE) and the average overtime of physicians (OVER). Anderson et al. [76] investigated an Overlapping Appointment Scheduling (OLAS) model to minimize waiting time and physician idle time in medical clinics, considering randomized service times. Han et al. [77] used the sum of patient wait and physician idle costs as the system cost and introduced an analytical model and demonstrated the optimality of a fixed-interval policy. Guido et al. [78] derived a local search algorithm with an objective weighted average of the patient’s expected waiting time, the doctor’s idle time, and the lateness time, and proves that the algorithm converges to optimal scheduling, with the following objective function:
In Equation (10), are the mean waiting time, idle time, and lateness, respectively. α is the weight of function. represents the total number of patients. is the number of patients scheduled at the start of interval .
Dharmadhikari et al. [79] used performance metrics of average rewards per patient to assess the effectiveness of the proposed block scheduling strategy with prioritization. Cordier et al. [80] developed algorithmic tools to construct one-day schedules and optimize these schedules to optimize the length of patient stay. Nazanin et al. [81] conducted case studies for different healthcare settings and selected the most effective scheduling model that fits the case in terms of the balance between three types of metrics related to patient appointment scheduling systems: patient satisfaction, scheduler utilization, and scheduling system cost. Accessibility was a factor of patient satisfaction, measured by the average waiting time before connecting to the dispatch program and the average duration of call. Ma et al. [82] examined the scheduling of outpatient appointments in a multi-server model as a two-stage stochastic optimization problem. The initial step focus is on optimizing doctor planning based on capacity and patient requests, and the second step optimizes patient planning with considering uncertain service times, which first aim to maximize patient service time per unit cost:
where Cf is total amount of allowances for all doctors on assignment based on time worked. R is the hours of service each patient, is total number of patient weeks, and P is the total working hours per week. is the fixed working hours and α indicates the unit allowance.
3.1.2. Economic Performance
The appointment scheduling system is a potentially useful tool for reducing health management costs and maximizing medical benefits. Improving system reliability and cost savings are the main ideas of optimization [101,102,103,104]. Profit maximization is becoming a major research objective due to the need for cost efficiency and facing budget cuts. Some hospitals maximize profits by rising the number of patients scheduled and maximizing contribution margins. El-Sharo et al. [83] modeled an overbooking scheduling model for multi-provider practices to optimize patient overbooking and maximize expected profits. Parizi et al. [84] studied a class of scheduling problems where his system is rewarded for service provision; and costs incurred for rejected requests, delays, and overtime. Chakraborty [85,86] proposed a sessional sequential scheduling algorithm without time slots proving that the expected profit of scheduling is single-peaked, providing the stopping criterion for the scheduling algorithms, with the following total expected profit:
where set indicates partial schedule after n call-ins, and is the time of the ith “scheduled” customer. The expected cost is given by due to customer waiting and overtime. is the expected revenue, where r is the revenue per unit time, and the random variable denotes the number of scheduled clients arriving for service after n clients are scheduled.
Muthuraman et al. [87] built a stochastic overbooking model and developed an outpatient AS strategy that considers patient arrival and removal probabilities from slots to maximize operational profitability. Geng et al. [88] used the Markov decision process model to consider outpatients with different waiting time goals and different rewards to maximize the expected benefit. Patrick et al. [89] developed a Markov Decision Process (MDP) model that explores tradeoffs between patient-related measures and physician-related measures. Maximizing system profit as the objective function (revenue minus overtime for visiting patients, idle time, indirect waiting time, and referral schedule), the MDP strategy is shown through simulation to be even better than open access in maximizing profit and providing more consistent throughput. Wang et al. [90] developed a model for scheduling appointments and managing capacity concurrently, taking into account no-show patients and walk-in patients. The objective is to maximize the overall profit and the objective function is a multimodal function, with the following total expected profit:
In Equation (19), r is the revenue of per patient, and is calculated as the total number of patients in the schedule. is the probability of the patient arriving on time each time interval, while is the probability of walk-in patient. In this equation, walk-in patient income is considered to maximize the economic benefits.
3.1.3. Resource Utilization
With limited healthcare resources, clinics are under tremendous pressure to the increasing demand. Therefore, rational capacity allocation is one of the main goals of AS. Previous papers on outpatient capacity assignment can be divided into two broad categories. One category is where the overall capacity is a constant, the hospital must assign limited medical capacity to various types of patients. For instance, Nguyen et al. [91] presented a mixed-integer planning model with the aim of minimizing the maximum demand capacity to plan the demand of outpatient physicians to achieve the service goal of patient appointment lead time. The other category, where the capacity is a variable that needs to be solved in conjunction with the allocation scheduling problem, is categorized into static and dynamic cases. The former means that the decision is made before the session, e.g., Zeng et al. [92] investigated the appointment booking problem for heterogeneous patients. The features of optimal scheduling with heterogeneous patients are determined, and a method of local search algorithm is proposed to for finding the locally optimized scheduling. The latter means that appointments are made sequentially, and when a patient calls in, capacity allocation is conducted online, and the hospital needs to decide how much capacity is available for each time slot. Yan et al. [93] studied a sequential AS method that considers choice for patients and equity of services to balance clinic effectiveness and patient satisfaction. Tsai et al. [94] offered a overbooking model to consider the patients’ call-in order, who proposes two methods, convolutional estimation with upper and lower bounds and joint cumulative estimation, to make the workload of each appointment slot more balanced.
Jiang et al. [95,96] investigated a capacity addition strategy to mitigate the supply demand mismatch and proposed a two-tier enumeration search algorithm based on how to allocate normal capacities between regular and same-day patients. A demand-driven approach to allocating additional capacity at outpatient clinics is also discussed, and the capacity assignment optimization problem under CAP is investigated to optimize the whole process by jointly setting the optimal values for both additional and conventional capacity. Sevinc et al. [97] used a two-stage approach to optimize the chemotherapy regimen and proposed an adaptive negative feedback scheduling algorithm for managing system loads. Two heuristics were evaluated to optimize the utilization of infusion chairs by assigning patients to specific infusion seats.
3.1.4. Other Objectives
In general, the literature on optimization studies of AS systems covers many aspects, as well as the optimization of objectives through other aspects to obtain better social and economic effects.
Savelsbergh et al. [98] investigated methods based on optimization and cohorts to SA for patients in a chronic disease management program. The objective was to minimize the overall probability of a patient entering an uncontrolled health state. The approach considers transitions in disease control since the last appointment time and the probability of the patient not attending the appointment. Ozen et al. [72] used the probability of demand exceeding capacity as a measure of access capacity. Formulating the problem of minimizing the maximum overflow of a multi-medicine practitioner clinic as a non-linear integration programming problem describes how the frequency of overflow varies from physician to physician and demonstrates how these supply and demand imbalances can be minimized in the long run using real-world data from primary care practices. Zhu et al. [99] provides a method for efficient outpatient scheduling that maximizes the matching between patient preferences and scheduling by collecting patient choices from available time slots through special processing to find an allocation scheme for all patients that maximizes the preferences of all patients. Erdelyi et al. [100] exploited a stochastic approximation method to find a favorable class of protection. The levels calculated through the stochastic approximation method which consistently outperforms those computed using the deterministic approximation method.
3.2. Decision Variable
About the optimizing appointment scheduling’s study, the decision variables for optimization show the strategy and actions taken to enhance the objectives [105]. Appointment time is one of the common decision variables in the AS problem. Tito et al. [106] considered whether patient absence was affected by appointment time using arrival time as the decision variable and investigates a stochastic optimization problem with a random distribution of service times and patient decision-dependent no-show behavior. Solutions are given for different patterns of absenteeism behavior, and it is shown that disrupting the hypothesis of a fixed probability of attendance greatly alters the scheduling scheme. Liu et al. [107] used a programmatic single-server queuing model to pattern appointments scheduled for providers, examine demand and capacity control decisions and consider two distinct problems, which considered service capacity as a fixed and decision variable, respectively. Maximizing the net reward function is used as the objective and the optimal strategy is given.
Zhang et al. [108] described the server’s response to congestion as influenced by client waiting time, the model employs the scheduled arrival time of a sequence of clients as the decision variable. And provided replacements for the simulation optimization model and the SIP model. SIP models have been shown to enable servers to react to congestion under certain conditions. This resolved the challenge of scheduling appointments while considering the server’s response to congestion in the service system.
Luo et al.’s work [109] is applicable for identifying optimal appointment strategies under varying assumptions regarding rewards, costs, and decision variables. The aim was to balance between patient waiting time and server utilization. It was also investigated whether a strategy performs very poorly when it ignores interferences when the decision variable is the appointment’s number.
3.3. Constraints
Various optimization decisions about appointment scheduling systems will have different constraints. Optimization studies of ASs are often inseparable from the optimization of operational costs as well as time from the perspective of economic or social benefits [110]. Considering the minimum cost of AS operation and the minimum waiting time or the minimum physician overtime time, the constraints consist of appointment sequence, resource capacity, time constraints, etc.
3.3.1. Queue Balance Constraints
Consider the need to have maintained a normal flow of patients through the system. It is essential to maintain a balance between the number of patients in the line at each stage and the sum of the initial number of patients, the additional patients entering the stage, and the reduction from patients who have exited thus far [111]. The queue balance constraints can be expressed as follows:
where is the number of patients, is the starting count of patients of type , and is the cumulative count of patients of type at stage .
3.3.2. Capacity Constraints
Capacity allocation, including equipment resources, medical staff, and patient numbers, requires constraints. The equations are as follows:
- Surgeon availability constraint:
Considering the availability and scheduling of surgeons, it is required that a sufficient number of surgeons needs to be available to operate at each time period, where is surgeons of type s who are currently available at time t; the values of stage index j of 1, 2 and 3 refer to the pre-, mid- and post-run stages, respectively, where is the service duration during the operation.
- Operating room availability constraint:
3.3.3. The Completion Time Constraint
Same-day appointment patients cannot have a wasted visit, so it is necessary to stipulate that services are available to all patients before the end of treatment. The number of patients that must be served is determined as follows:
The constraint indicated by completion time determines the time block for the discharge of the last patient.
In Equation (24), indicates whether the patient is discharged where it is 1 if discharged and 0 otherwise. is an arbitrarily large number and is the last time block, which means completion time.
4. Optimization Algorithms
Numerous studies have been undertaken to determine the optimal allocation of AS systems to reduce operational and time costs, improve patient satisfaction and system reliability dependability. Various algorithms are applied to the optimization of AS systems, with genetic algorithms (GAs) being the most utilized. For instance, Braune et al. [112] proposed a combination of GAs and Monte Carlo simulation to heuristically solve a stochastic optimization model developed for planning the appointment times of healthcare units under uncertain activity durations, allowing to minimize the waiting time of patients while maximizing the use of resources. Fan et al. [113] considered patient preferences for highly qualified general practitioners and specialist doctors. By analyzing real data from hospital outpatient clinics, a behavioral pattern was derived in which the patient’s tolerance limit adapted to the expected waiting time. A simulation optimization framework for maximizing clinic benefits and minimizing patient dissatisfaction is proposed. Utilizing multi-objective optimization and a genetic algorithm, a simulation budget allocation approach is integrated to derive an approximate Pareto scheme for joint capacity planning and patient scheduling across multiple servers. Alizadeh et al. [114] presented an optimization problem for non-urgent outpatient appointments, where only one machine (equipment) and a finite number of healthcare professionals are required to satisfy the medical needs of many waiting patients.
In addition, the key to the appointment dilemma is the challenge of solving the multi-objective optimization problem; therefore, many decisions need to be made using a multi-objective evolutionary algorithm. Mohammad et al. [115] improved the quality of operational efficiency and healthcare quality by writing a MOPSO algorithm and introducing a MO-PASS architecture. Ali et al. [116] investigated a multi-criteria approach in appointment scheduling by WOA. optimization for hospital management quality and patient satisfaction. Qiu et al. [117] studied the AS challenge for a single diagnostic device, namely, a magnetic resonance imaging (MRI) device. The issue is expressed as a two-stage stochastic modelling of programming. An enhanced evolutionary algorithm for multiple objectives is subsequently introduced within the framework of multi-objective evolutionary algorithm based on decomposition (MOEA/D) to simulate uncertainty by constructing several different scenarios, and the validity of the presented model is evaluated by comparing it with the typical NSGA-II and MOEA/D algorithms using real healthcare data. Meersman et al. [58] utilized a multi-objective archived simulated annealing heuristic algorithm to design a Pareto-cyclic appointment schedule according to the wait times with various capacity allocations for emergency patients.
There are some other methods to solve this problem. Garaix et al. [118] proposed a heuristic to calculate the order in which patients receive treatment at outpatient chemotherapy centers called the GRASP algorithm. It optimizes the facility’s closing time and overtime working time. It can reach near-optimal solutions quickly and the performance of the patient-listing strategy is comparable to more complex scheduling strategies. Corsini et al. [119] developed a hybrid harmonic search element heuristic algorithm to simulate a multi-stage chemotherapy ward to explore the problem of scheduling same-day chemotherapy outpatients to optimize patient waiting time. Ali et al. [120] studied an integer planning model with a contraindicated search approach along with the addition of a simulation model solved in the ASs. This was conducted to assess diverse patient flow control in emergency centers, aiming to minimize patient waiting time and enhance patient satisfaction during hospital experiences. Rajakumari et al. [121] used Convolutional Neural Networks (CNNs) for clinician schedule analysis to develop a web-based appointment system to improve the efficiency and quality of deliveries to minimize waiting times. Ali et al. [122] proposed a simulation-optimization methodology for sequentially scheduled appointments to provide ideal schedules from both patient and medical practice perspectives. The goal is to minimize the weighted expected cost associated with direct and indirect waiting time, idle time, and overtime.
Typically, there exist specific methods for addressing optimization problems. Table 3 provides a summary of their characteristics and related studies. The subsequent section presents the utilization of these algorithms in optimizing appointment scheduling operations.

Table 3.
The features of the most used algorithms and related research.
4.1. Genetic Algorithm
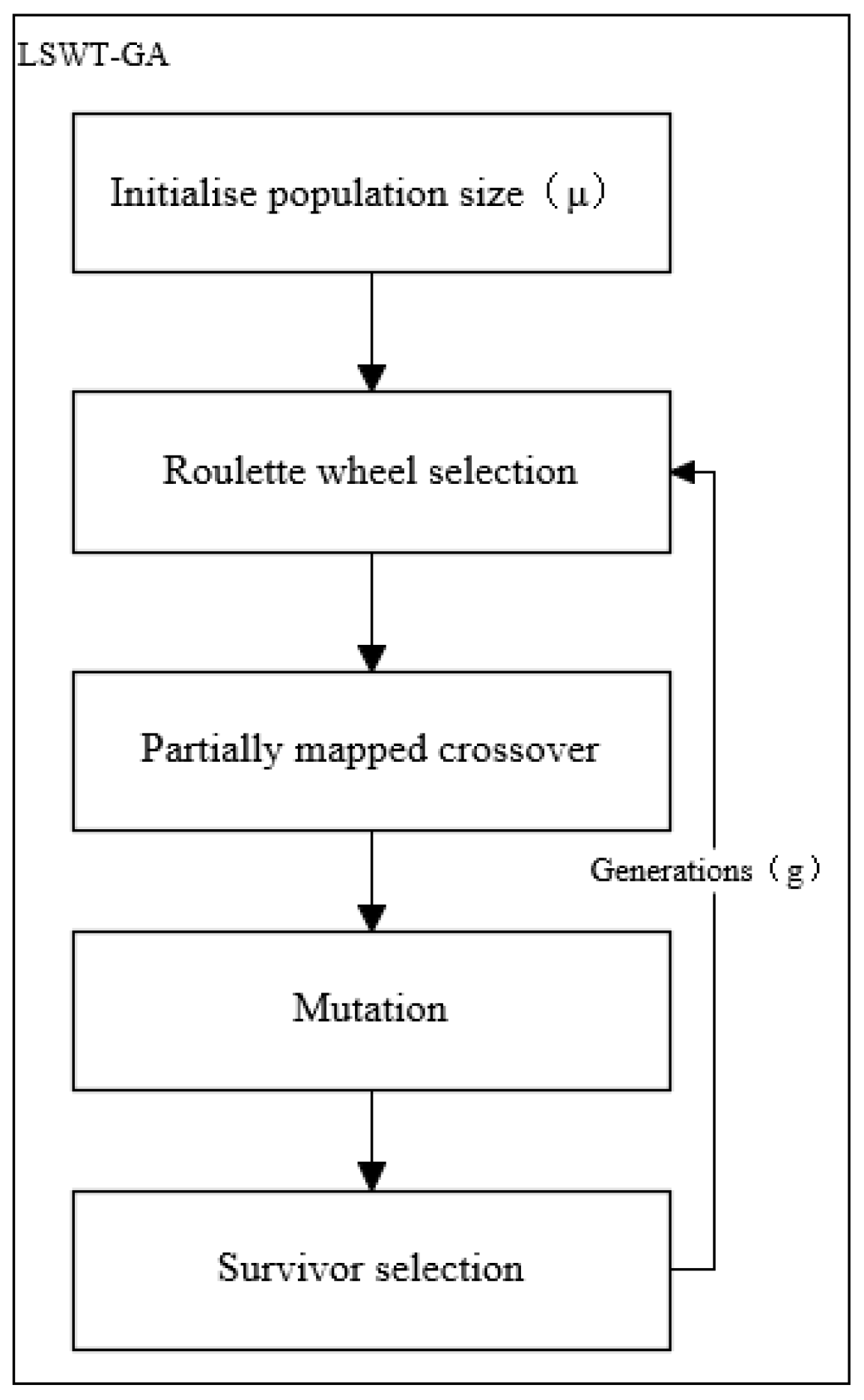
Genetic algorithms (GAs) offer an efficient approach to optimizing complex systems. Previous research indicates that many scholars have employed GAs to address optimization problems in the scheduling fields. For example, Squires et al. [124] proposed a new genetic algorithm designed for scheduling repetitive transcranial magnetic stimulation (rTMS) appointments. The mentioned algorithm (LSWT-GA) combines a novel survivor selection strategy with heuristic population initialization. The objective of the algorithm is to enhance the operational efficiency of medical centers by optimizing the scheduling of repetitive transcranial magnetic stimulation (rTMS) appointments.
4.1.1. Objective Function and Constraint
The primary goal of the initial aim in the experiment is to minimize the job processing time expressed as and aim to minimize weighted flowtime secondly. The problem can be under the category of minimizing make span in a parallel machine scenario, where job processing times are deterministic, and preemption is not allowed.
where
In this formula, is a group of patients waiting for a treatment, denotes the flowtime of patient ; is the time to finish the treatment for and is the release time of the job.
4.1.2. Optimization Process
This study presents the new genetic algorithm used. Drawing inspiration from evolution, the genetic algorithm relies on natural selection to choose the most suitable chromosomes, as determined by a fitness function, for the reproduction phase of the genetic algorithm. Figure 2 illustrates the flowchart of the optimization algorithm employed in this paper.
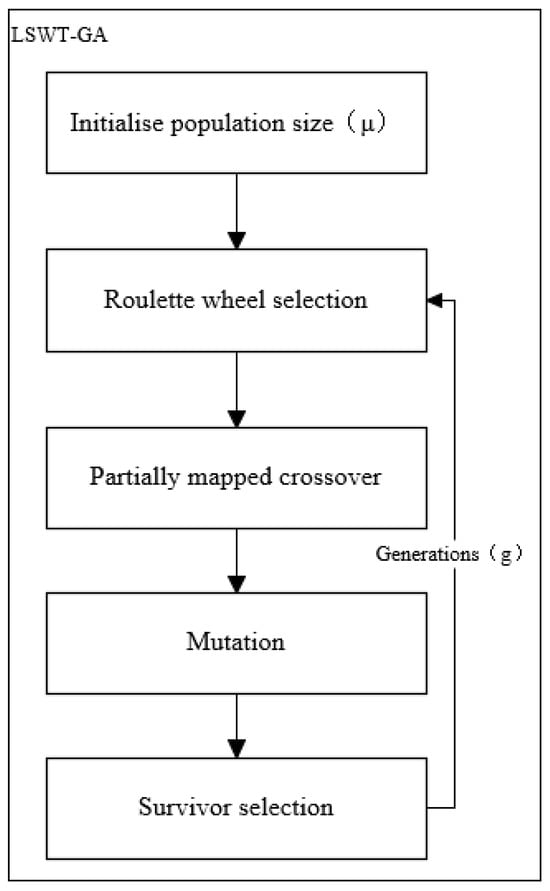
Figure 2.
Flowchart of genetic algorithm modules.
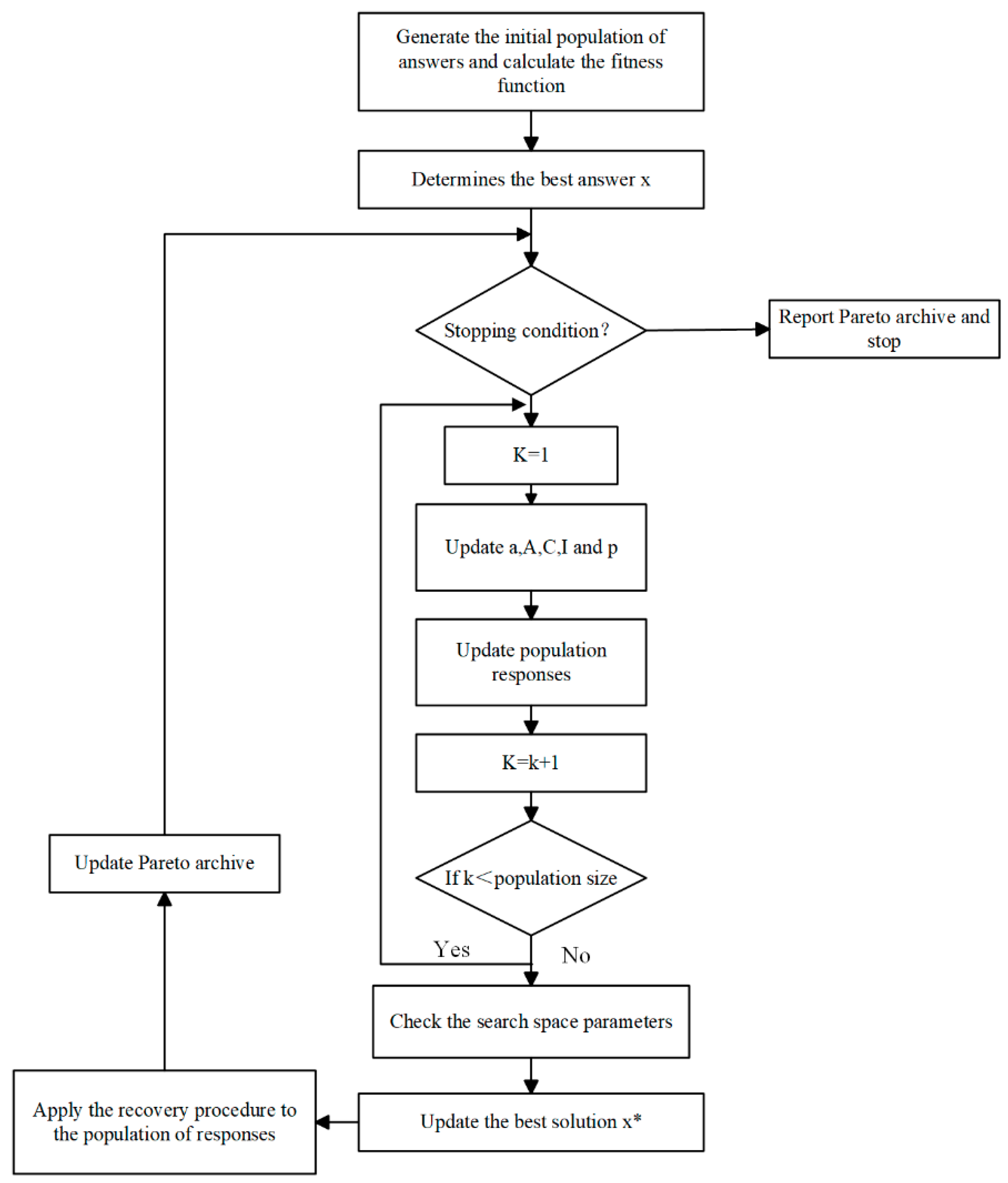
4.2. Whale Optimization Algorithm
The WOA algorithm is a meta-heuristic algorithm designed with both subtlety and character, which is derived from simulating the hunting behavior of humpback whale groups in nature and realizes the purpose of optimizing search through the process of searching, pursuing, and attacking prey by the whale group. The WOA literature has been widely used in solving various of optimization problems, and Ali et al. [116] explores the multi-criteria in AS were analyzed using both algorithms, WOA and NSGA techniques. They are computed using various assumptions to meet the requirements and aspects associated with WOA and NSGA.
4.2.1. Optimization Model
Scheduling and counseling patients for scheduling to the hospital is the issue discussed. Each hospital section has a varying number of operators to handle distinct operations. Moreover, each capable of providing specific services. In this system, there are n patients, categorized as either emergency or general patients. There are several surgeries for each patient that must be performed in different departments. In addition to this, it may diagnose a patient as an emergency at the time of planning. Emergency patients are usually visited earlier than general patients and are given precedence (fairness). After doing something such as seeing a doctor, the diagnosis depending on the patient’s condition, in which case the patient is referred to an inpatient unit with limited beds.
4.2.2. Objective Function
The objective function is to minimize the average total weighted patient time and to reduce dissatisfaction because of increased waiting time for patients.
4.2.3. Constraint
Examination or processing of each patient’s procedure is exclusive in one location on one ward, as shown in the formula below. And for the restriction in a sequencing assured to prevent patients from being assigned to a segment of the surgery when another area is empty, as shown in the Formulas (33) and (34).
where x is the Appointment System Decision Variables and is equivalent to 1 if the action is performed in section at position . It is also important to consider the indexes used for appointments, appointment durations, association variables, etc.
4.2.4. Model Solving
This study solves the model by introducing a local search operator to optimize the solution, using the stochastic WOA nature of the meta-heuristic algorithm. The WOA begins with stochastic solutions. Depending on each search factor, the search agent arbitrarily changes according to the optimal solution. The position of the task agent can be updated through two methods. If |A| > 1, a random search agent is chosen; otherwise, the optimal solution is selected. The whale can transition between two types of motions, either spiral or rotational, depending on the p-value. Eventually, the algorithm concludes when it attains a predefined satisfaction criterion, where x* represents the best solution, as shown in Figure 3.
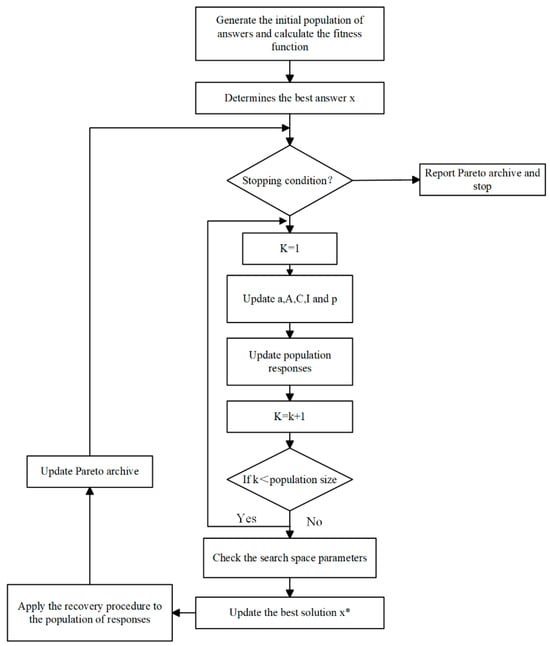
Figure 3.
Proposed flowchart for the whale optimization algorithm.
WOA mining and discovery is divided into two phases. In the operational phase, a bubble net attack strategy is demonstrated the procedures of searching for agents based on the current optimum. There are two approaches to this attack, including pride and spiral swims. Based on a randomly selected search agent, each whale independently changes its position during the discovery process.
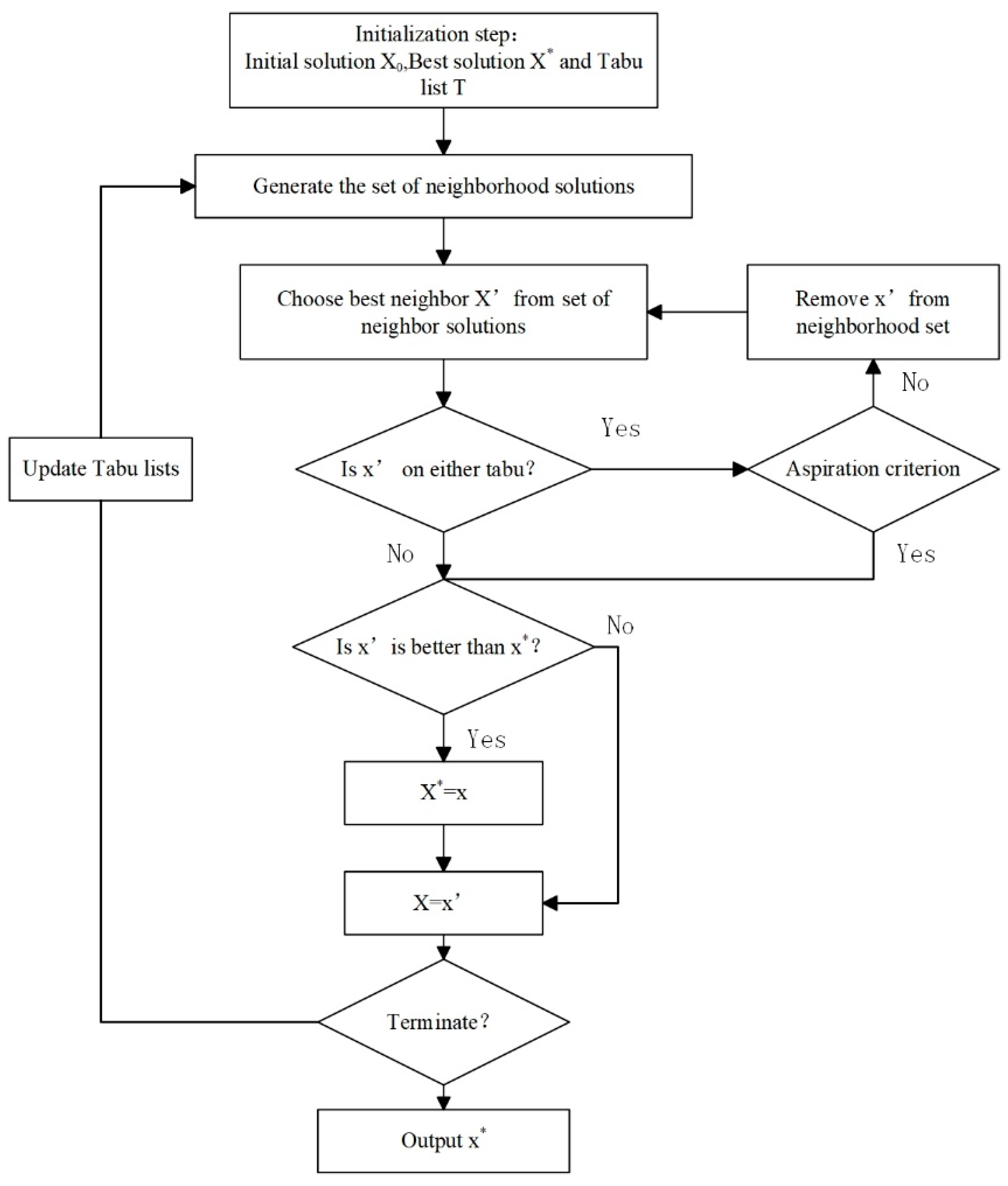
4.3. Tabu Search Algorithm
Tabu search selects a candidate solution from the neighborhood using a set of techniques. This chosen solution is then subjected to the measurement phase within the simulation. The scheduling process implements the candidate’s solution and computes its output through numerous replicates [120].
4.3.1. The Integer Programming Model in a Definitive Model
The optimization objective is reducing waiting periods and the cost of completion times to a minimum. Every patient went through three phases of initial admission and surgery and recovery phases of surgery.
where denotes the queue limit, is the resource capacity content, and denotes the patient visit or procedure completion time. Meanwhile, patient queue balance as well as resource capacity versus the number of patients to be served are constraints of the appointment system.
4.3.2. Algorithm Optimal Progress
The random solution called at the beginning of the algorithm is . And the best-found neighbor solution, , is named as a pivot. Tabu tenure comes into play to navigate away from local optima throughout the search process. An iterative update of the list is implemented to enable the algorithm to adapt to the status of the search. This methodology ensures the comprehensive exploration of the entire solution space while simultaneously addressing the objectives of intensification and diversification. Additionally, in specific instances, the aspiration criterion is applied to supersede the Tabu list. Figure 4 illustrates the proposed TS algorithm, where X* represents the best solution.
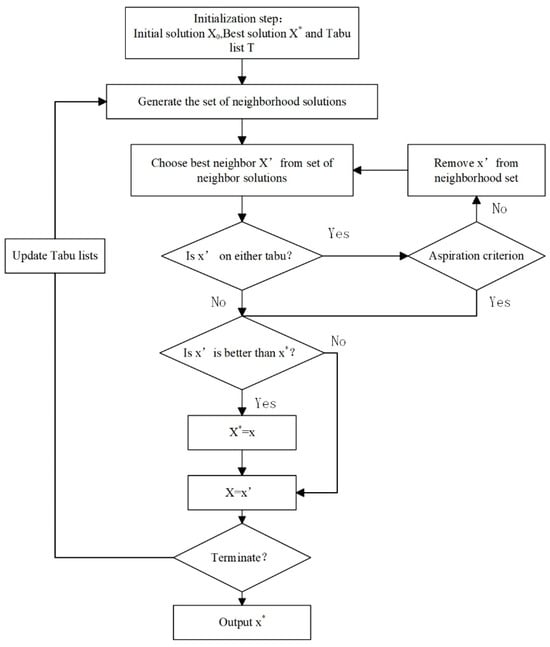
Figure 4.
The flowchart of the Tabu search algorithm.
The term of Tabu was determined from some preliminary experiments. The taboo retention period specified the upper limit for the number of iterations. The maximum computation time is set as the criterion for terminating the algorithm when no improvement is observed within the specified number of iterations. The second method uses integer programming with stochastic models, which are executed separately and then compared.
4.4. Other Heuristic Algorithm
4.4.1. Problem Description
A heuristic optimization algorithm is an intuitively or empirically constructed algorithm that provides a viable solution for the combinatorial optimization problem at an acceptable cost, considering computational time and space constraints. This means that the heuristic algorithm solves the problem empirically or according to some rules, and the solution to the problem is not necessarily optimal but is likely to be approximate (or near optimal). Akbarzadeh et al. [124] proposed a three-phase heuristic algorithm for constructing high-quality feasible solutions using column generation, which is further improved by local branching. The surgical case replanning and scheduling problem with resource rescheduling is investigated in the presence of a chunk release time when the OR planners aim to achieve equilibrium between the capacity and demand for operating rooms. The following equation involves four components that reflect the benefits, resulting in weighted sums of various metrics.
where the initial component compels the model to allocate surgical cases to an appropriate day. Following this, the second component seeks to minimize waiting time. Subsequently, the next component aims to minimize the overall nurse rescheduling cost. Finally, the last component focuses on minimizing the deviation of the surgeon’s schedule from the Master Surgery Schedule (MSS). The weights assigned to these different objective functions are relative and collectively sum to 1, i.e., α + β + γ + δ = 1.
4.4.2. Constraint
There needs to be a requirement for nurses to perform only one procedure at a time, and to assign procedures to nurses only if they have been assigned a shift. In fact, a surgeon is restricted to one operating room at any given time, and each surgery is limited to being conducted only once.
In Equation (37), denotes the case where nurse n received the task for schedule at time t on day , indicates whether the scheduling is accepted or not, indicates whether nurse n worked on shift on day ; denotes whether surgeon s is assigned to the r-room b area on day d of program ; denotes if surgical case i is included in schedule , day ; and is the decision variable implies that the surgery is performed within the time frame under consideration.
In addition, some other constraints should be considered, such as the order of nurse scheduling and the number of physician surgical blocks.
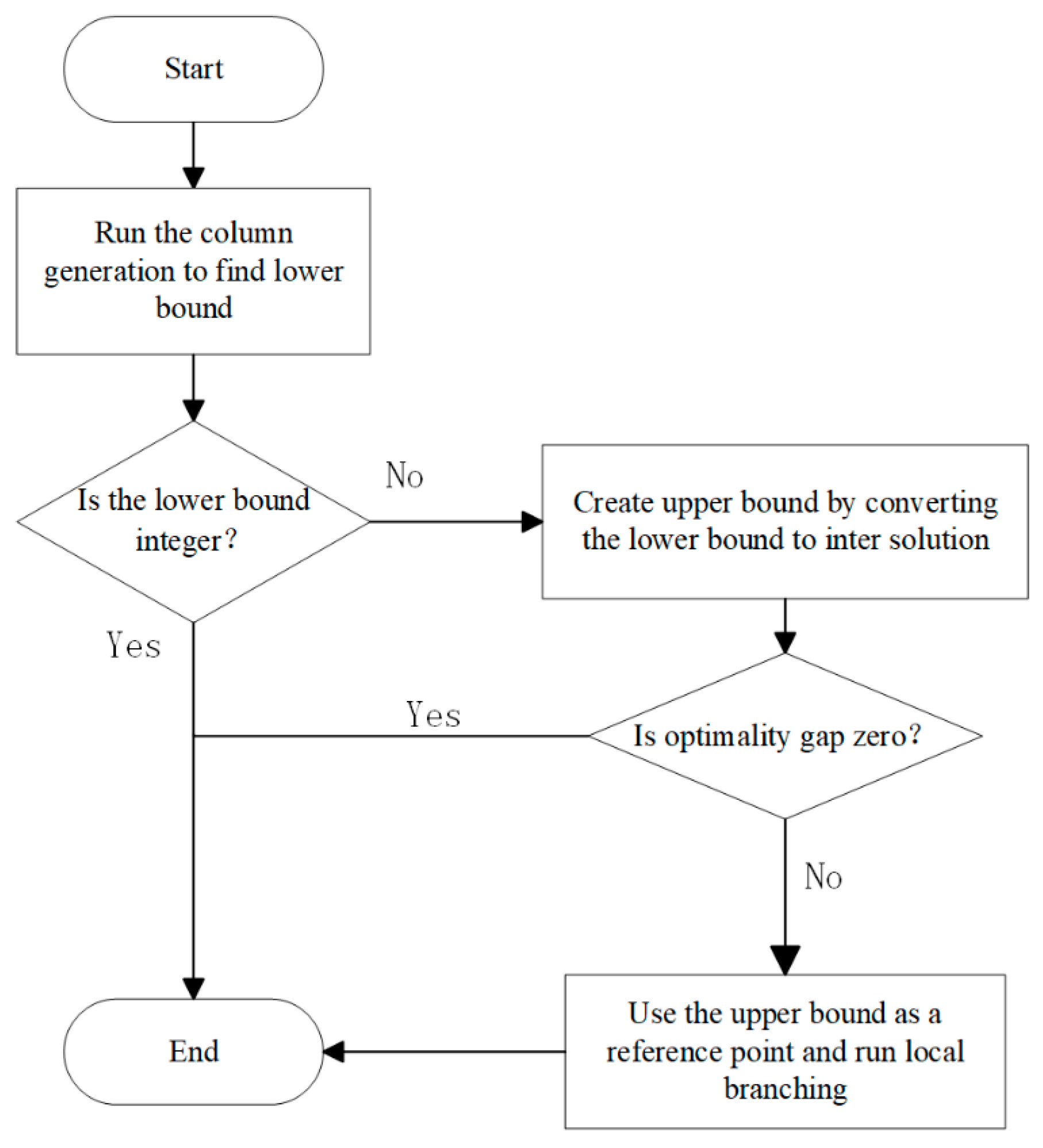
4.4.3. Solution Methodology
The solution procedure named Column Generation and Local Branching Heuristic (CLH) is proposed to address the integrated problem. Figure 5 provides an overview for the solution procedure, consisting of three distinct steps. Firstly, the CLH algorithm employs a computationally feasible column generation procedure to address the impracticality of generating all possible OR schedules directly. If the solution is an integer, it is optimal; otherwise, transforming fractional solutions into feasible integer solutions offers an upper bound on the optimal solution. If the upper bound matches the lower, the optimal solution is identified. If not, the optimal upper bound is used as input for an improvement step, using local branches to narrow the optimality gap.
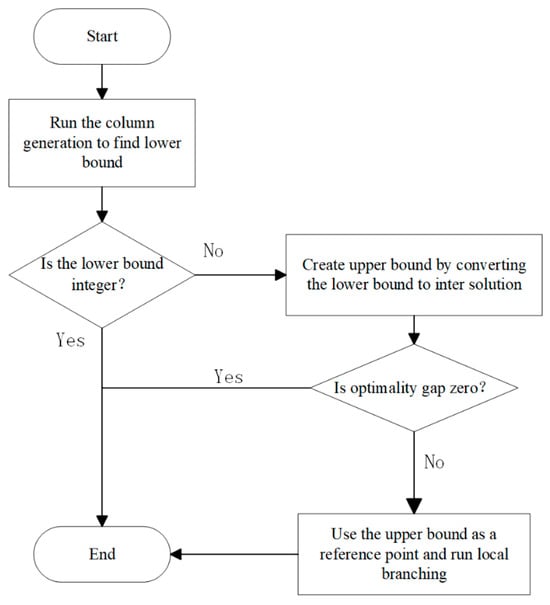
Figure 5.
Summary of the Column Generation and Local Branching Heuristic.
5. Bibliometric Analysis of Literature
Research on AS systems has attracted significant attention. A literature bibliometric analysis is therefore needed to systematically collect and analyze bibliographic data to gain a more detailed understanding of the research field and the future direction of research ideas. This article provides a summary of the literature on AS optimism published in SCI-indexed journals from 1 January 2016 to 25 August 2023, utilizing Cite Space. The search terms employed were “appointment scheduling” and “system optimism.” The paper’s representative institution and country were determined based on the first author’s affiliation and location.
5.1. Methods and Data
5.1.1. Methods
To conduct the analysis, we utilized Cite Space, a Java program established in 2006 [125]. This powerful tool specializes in document analysis and bibliometric visualization, providing valuable insights into scientific literature databases. Its notable features encompass co-citation analysis for discerning paper relationships, burst detection to highlight emerging trends and influential works, visualization tools. In contrast to tools like VOS viewer, Cite Space uniquely provides spatiotemporal visualization, illustrating the evolution of literature citations over time. It identifies core nodes, tracks keyword trends, and constructs citation coupling networks for intrinsic connections in the research field. With a user-friendly interface, Cite Space stands out for its accessibility and analytical depth.
5.1.2. Data
Bibliographic information on AS was collected using the Web of Science (WOS) over a span of seven years (2016–2023). A total of 1144 records are present in WOS, excluding reviews. WOS is a global academic literature search tool covering a wide range of disciplines in the natural sciences, social sciences, humanities, engineering, and technology, and includes many well-known journals and academic publications. It provides the ability to search by keywords in multiple dimensions and can be used to gain insights into the linkages between the literature by visual citation analysis tools, which can help promote an in-depth understanding of the literature and scientific research. This paper investigates a review of methods for optimizing the operation of appointment scheduling systems in the healthcare field, so the key subject terms for the literature search were “appointment scheduling” as well as “system optimism”. Since 2010, the digital transformation of AS systems and the spread of healthcare information technology have driven the development of the optimization of the operation of AS systems. And, in 2016, digital tools such as smart queuing systems, online pre-screening and other digital tools began to be invested in healthcare system optimization research. Numerous healthcare institutions began to realize the importance of digital transformation, and researchers began to explore how to use big data and analytical tools to optimize AS system operations, including improving resource utilization as well as predicting patient demand. During this period, research on the operation optimization of AS systems may start to receive more attention and gradually develop and improve in the following years. Therefore, literature reviews from 2016 onwards were selected for bibliometric analysis.
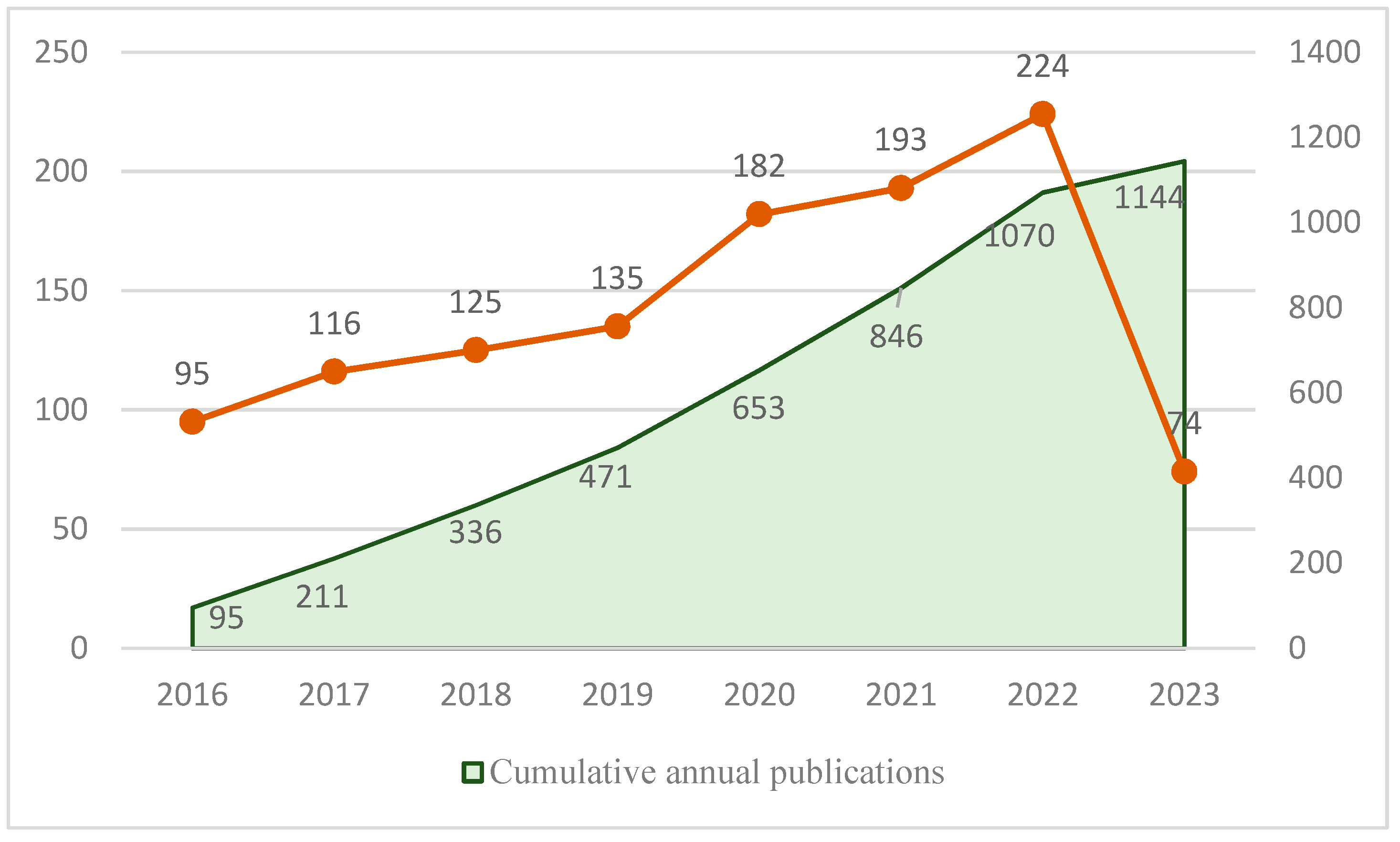
5.2. Operational Results
Cite Space is employed to analyze data from various countries, institutions, journals, and scholars, facilitating a comparative assessment of their contributions. Utilizing Cite Space, we summarized the articles and the cumulative count of articles related to the optimization of AS systems, as illustrated in Figure 6.
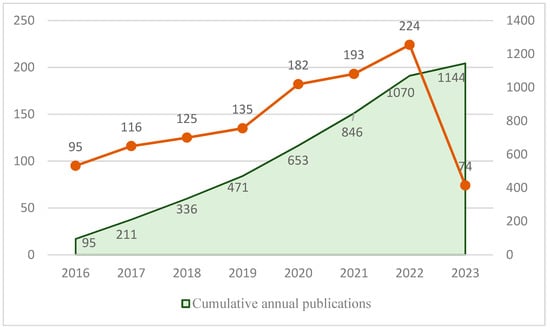
Figure 6.
Yearly distribution of papers and cumulative publications over the period 2016–2023.
Since 2016, there have been 1144 publications related to the optimization of AS systems. The annual publication count rose from 95 articles in 2016 to 224 articles in 2022, indicating a substantial increase each year. The cumulative number of yearly publications demonstrates a noteworthy upward trend, reflecting a growing scholarly interest in healthcare optimization studies.
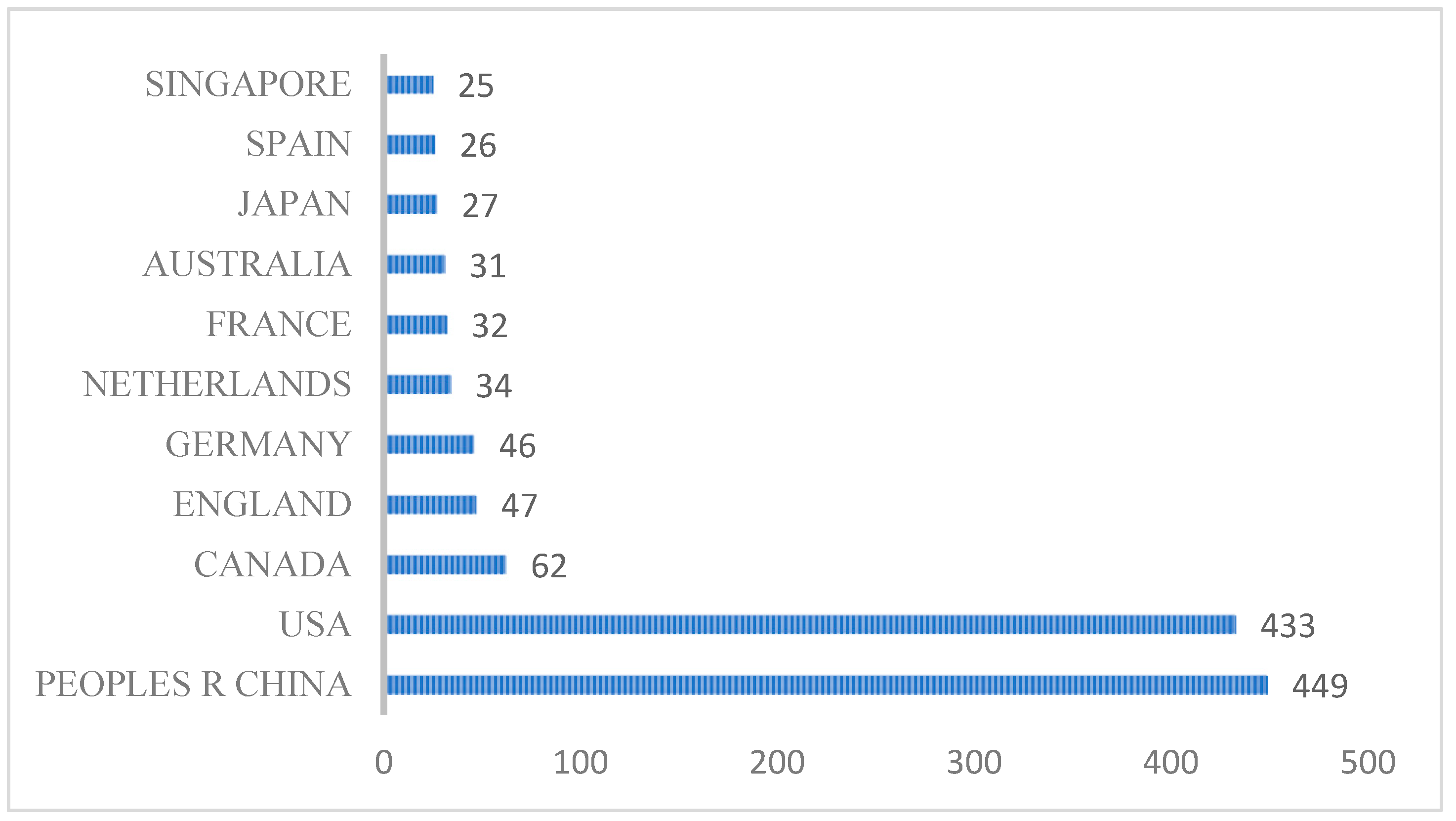
5.2.1. Country and Publisher
As shown in Figure 7, the leading nations in publications concerning the optimization technology of ASs include: China with 449 publications, the United States with 433 publications, Canada with 62 publications, England with 47 publications, and Germany with 46 publications. Notably, China exhibits the highest volume of papers, indicating its prominent focus on AS optimization technology.
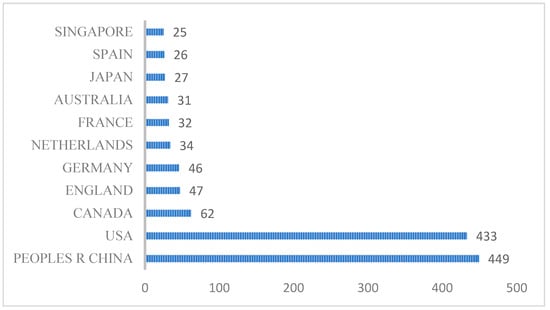
Figure 7.
Annual bar chart depicting the top ten countries based on the number of publications.
The institutions leading in the publication of papers related to optimization of AS systems in Figure 8 are Shanghai University (66 papers), Shanghai Jiao Tong University (59 papers), University of Shanghai for Science Technology (56 papers), Fudan University (42 papers), US FDA (34 papers), Shanghai Maritime University (29 papers), East China University of Science Technology (27 papers), Shanghai University of Engineering Science (23 papers), Tongji University (22 papers), and the Chinese Academy of Sciences (17 papers). Among these institutions, there are nine in China, and one in the US. This indicates China’s interest in the research of ASs optimization technology, making extensive efforts to the development of intelligent healthcare management compared to other nations.

Figure 8.
Dendrogram of the top ten institutions ranked by the number of publications.
5.2.2. Author
In this paper, Cite Space is employed to conduct a statistical analysis of authors contributing to published research on optimization technology for ASs. The results highlight several authors who have made a significant impact in this field, as depicted in Figure 9.

Figure 9.
Co-citation network of authors (timespan: 2016–2023; slice length = 1; g-index = 25; LRF = 3; LBY = 5; e = 1; n = 290; E = 481).
The number of co-occurring nodes is 290, the number of connections is 481, and the network density is 0.0115. Cayirli, T. has been cited 99 times, followed by Laganga, LR., with 96 citations; in addition, Klassen, KJ. and Robinson, LW.’s cited numbers are 88 times, and 62 times, respectively. Among them, Cayirli, T. is the most influential in the system optimization research of ASs, focusing on appointment arrangement operation and management optimization; Laganga, LR focus on the reservation over-capacity expansion problem and Klassen, KJ. focuses more on the research on simulation optimization methods. The work conducted by these authors reflects the predominant direction in the optimization research of ASs.
5.2.3. Thematic Trends
This study employs Cite Space to statistically assess topic trends spanning an 8-year period. The evaluation of topic trends involves analyzing keyword burstiness, as depicted in Table 4. The burstiness of keywords is measured using the “strength” based on a statistical formula to gauge changes in keyword frequency.

Table 4.
Thematic trend analysis over eight years.
As illustrated in Table 4, the lines depict the evolution of topic trends over the eight-year period. Specifically, covering the years 2016 to 2018, patient flow, discrete event simulation, overbooking model, time windows became hot keywords. This reflects the early trend of appointment scheduling research. The research is related to patient flow no-show and walk-in scenario simulation analysis. From 2019 to 2020, digital health, electronic health record and health information technology were the most popular keywords. Online registration and consultation have become more common, so research on health management informatization has become a trend. From 2020 to 2023, robust optimization, operations research and COVID-19 pandemic became popular keywords. Cost control requirements and resource allocation for outpatient appointments have become particularly important, and system optimization has become a key factor in health management consultation appointments. This result reflects the increasing importance of health management informatization and ASs system optimization research.
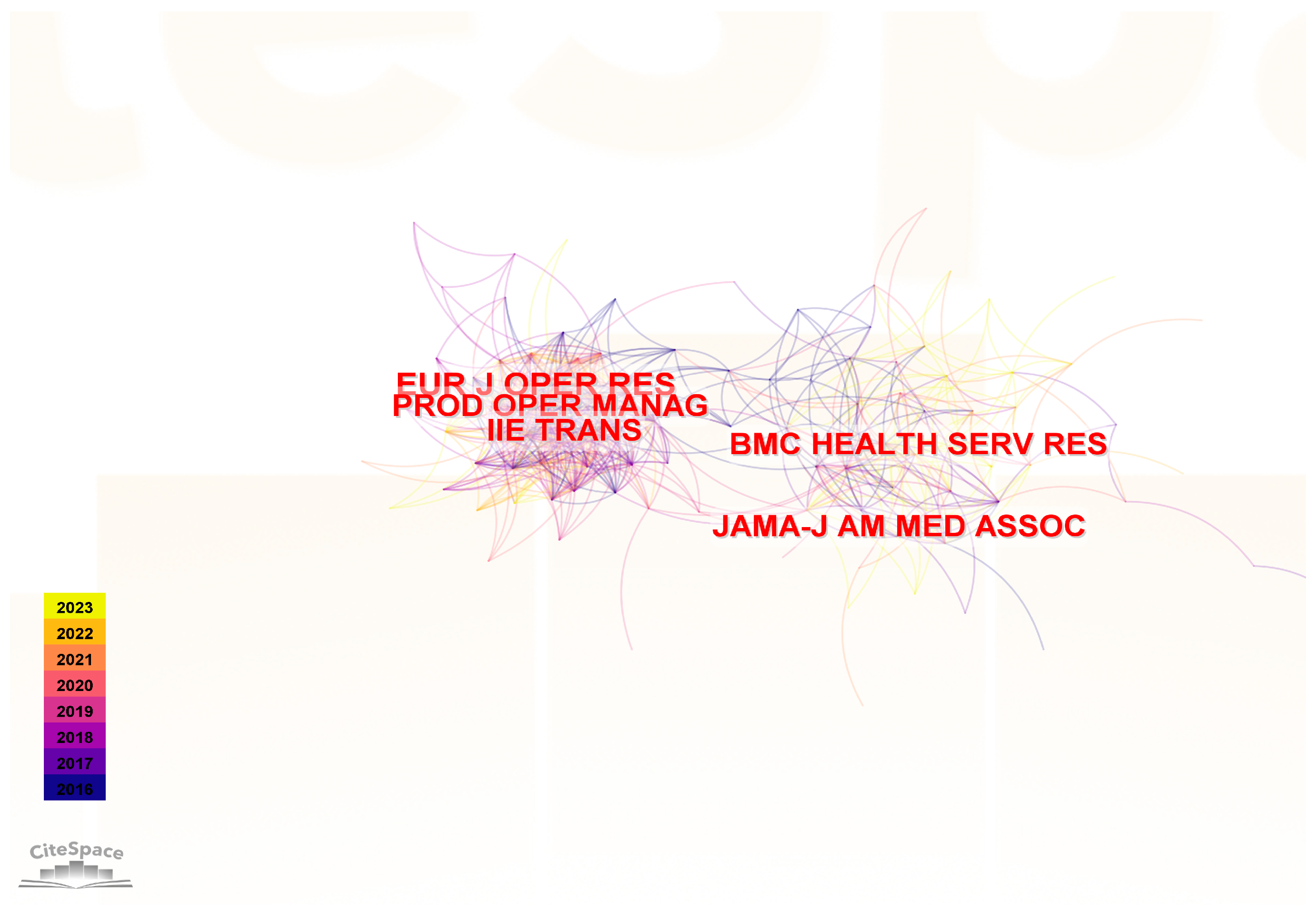
5.2.4. Cited Journals
In this paper, we use Cite Space to analyze the cited journal of published research on optimization technology for ASs as shown in Figure 10. The top 3 cited journals are European Journal of Operational Research (262 citations), Production and Operations Management (225 citations), BMC Health Services Research (214 citations). They belong to the fields of operations research, production and operations management, and health services research, respectively. These journals are important indicators in the research field and have a profound impact on the study of operational optimization of AS systems.
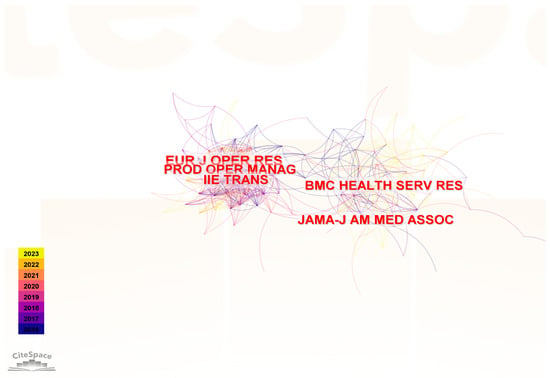
Figure 10.
Co-citation network of cited journals.
6. Discussion
Healthcare and appointment scheduling methods vary globally due to diverse cultural, economic, and infrastructural factors. Therefore, more comments about the specifics of the healthcare and the related methods for system appointment scheduling are necessary. For instance, some countries prioritize centralized electronic systems for appointments, ensuring efficiency and accessibility, while others might rely more on decentralized or traditional methods. Additionally, cultural attitudes towards healthcare, technology adoption, and government policies greatly influence these approaches. It is crucial to consider these nuances when analyzing and comparing healthcare systems worldwide.
6.1. Specifics of Healthcare
The healthcare specifics are explained in four areas which are online platforms, e-information, waiting lists and customization. Firstly, a range of processes and technologies are aimed at facilitating patient access to medical services involved in AS. Many healthcare providers use online appointment platforms that allow patients to make appointments through a website or mobile application. Secondly, it is also integrated with the electronic health record system to ensure that appointment arrangements are synchronized with patient records, reducing the risk of medical errors, saving costs through diagnostic examinations, reducing medication, and promoting the process of health management informatization [126]. Lastly, when patients cannot make an appointment at the ideal time, they can add the appointment entry to the waiting list through waiting list management. And when a patient is unable to make a desired appointment, the appointment entry can be placed on a waitlist through waitlist management, and patients on the waitlist receive automatic notifications once the time becomes available. In conclusion, the result of the current rapid development of AS is its customization and flexibility, with patients often using customizable templates for different types of appointments and services, and the overall system could handle emergencies outside of the regular scheduling process appointment services [127].
With the rise of telemedicine, AS systems include virtual consultation options that allow patients to schedule and attend appointments remotely, which also leads to the efficient utilization of healthcare resources, ensuring that future appointments are reasonable and matched with the right care or equipment. Indeed, the system cannot operate without security and compliance, and must adhere to healthcare privacy regulations, such as the Health Insurance Portability and Accountability Act (HIPAA), to ensure the security of patient information. And the use of online platforms should be secured with patient data, especially when transmitted online, which should be encrypted to prevent unauthorized access [128].
6.2. Differences of Related Methods
Differences in the structure of healthcare systems, uneven digitalization and technological development, resource allocation and cultural differences lead to variations in how appointments are booked in different countries. The United States, for example, emphasizes online platforms and electronic health records, relies on insurance processes, and offers convenience and telemedicine [129,130]. Japan achieves universal health coverage, with a greater focus on prevention and early intervention, but faces the challenges of aging. China is rapidly developing digital health technologies, including online platforms and the integration of Chinese medicine, but the operation and maintenance requirements are relatively high for system calculation examples [131]. The specifics of the healthcare and the related methods for system appointment scheduling in the different countries as shown in Table 5, and the unique characteristics of each country’s healthcare system have shaped different appointment booking practices and patient experiences. These specifics highlight the diverse approaches to healthcare delivery, financing, and coordination across different countries. Understanding these unique features is essential for developing effective healthcare policies and systems tailored to the needs of each population. It is important to note that the healthcare landscape is dynamic, and ongoing developments may lead to changes in these methods and differences over time.

Table 5.
Difference in AS system methods in global.
Healthcare has a high degree of specialization in developed countries, where AS systems are used to locate appropriate specialists and information is shared through electronic records. In contrast, some developing countries rely more on traditional queuing and on-site appointments due to lack of infrastructure, and healthcare IT is less efficient, especially in rural areas. In addition, some countries or regions may be wary of new technologies, perhaps due to cultural or religious differences and data security issues. Differences in healthcare systems worldwide reflect a combination of cultural influences, levels of technological development and resource allocation considerations.
6.3. Tendencies and Scientific Methods
Understanding the trends in healthcare systems allows for better optimization of systems to facilitate health management, with the trend across healthcare being towards streamlined appointment scheduling and optimized technology driven. Electronic medical records are replacing traditional paper-based medical records and shifting many clinical tasks that were once paper-based to electronic media. For instance, many countries such as the US, Germany, France, Finland, and New Zealand have demonstrated a tendency to integrate EHR systems by establishing EHR systems at the national level or simultaneously establishing national health information infrastructures [132]. Thus, patient data can be accessed in real time, facilitating efficient and centralized appointment management. However, the fact is that the process of integrating electronic health records is long and complex, healthcare systems with EHRs are expensive to develop as well as to maintain, and the digitization of technology-driven health management requires a greater focus on security [133], which are the trends and challenges for future research in healthcare AS systems.
Research on AS system optimization entails investigating and analyzing data collected from various healthcare systems, which employed methodologies such as comparative studies, statistical analyses, and surveys to assess the impact of different scheduling approaches on patient outcomes, resource allocation, and overall system efficiency. Furthermore, emerging technologies like machine learning and data analytics play a pivotal role in understanding and optimizing appointment scheduling processes. These scientific methods delve into patterns, patient preferences, and system performances, offering insights that contribute to the continual refinement of healthcare appointment systems on a global scale. E.g., data mining is calculated by analyzing and processing large amounts of medical data for modelling, identifying the connections and patterns between the information thus assisting doctors in decision-making [134]. Deep learning is applied to solve difficult problems in health management information technology through prediction and evaluation.
7. Conclusions
In this paper, we summarized the structural components of the system based on the existing literature review at first, and introduced the characteristics, system establishment process, and system decision-making framework. Then, we summarized the AS system optimization framework and reviewed the algorithms used for AS system optimization, among which we find that the GA algorithm is the most used optimization algorithm. Additionally, a bibliometric analysis and discussion were performed, which showed that ASs optimization has been growingly focused on developing countries exhibiting more interest in this field compared to developed nations.
Queuing theory, genetic algorithms, simulated annealing, particle swarm optimization, and other models have been mentioned, with a focus on addressing appointment scheduling and resource allocation issues in healthcare. Similarly, these models and techniques are widely applied to optimize resource utilization and enhance efficiency in supply chain management, transportation scheduling, production planning, customer service, and retail. Compared to scheduling problems in general fields, healthcare scheduling optimization involves specific models and techniques. This is primarily because the healthcare domain places a greater emphasis on patient healthcare needs and the specificity of healthcare resources. For instance, healthcare resource constraint models are designed to address the unique constraints associated with hospital resources. Disease epidemiology models, on the other hand, are employed to predict patient visit demands and hospital bed requirements. Additionally, there are models for patient prioritization, clinical pathway optimization, and healthcare service capacity planning, ensuring a comprehensive optimization of the entire healthcare service process. This is also a direction of researching optimization problems in healthcare appointment scheduling, focusing more on the study of optimization algorithms specifically tailored for the medical field. Therefore, we can say that, although AS system operation optimization has developed rapidly in recent years, more focused and practical research is still needed.
Author Contributions
Conceptualization, T.N., B.L. and K.G.; methodology, T.N., B.L. and K.G.; software, T.N.; validation, T.N.; formal analysis, T.N., B.L. and Q.L.; investigation, K.G.; resources, L.G., S.F. and L.Y.; data curation, S.F., Q.L., B.G. and L.Y.; writing—original draft preparation, T.N.; writing—review and editing, T.N. and B.L.; visualization, T.N.; supervision, B.L. and K.G.; project administration, K.G.; funding acquisition, B.L. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded in part by Beijing Social Science Fund Project under Grant 22GLC055 and 21JCB041, the Beijing Municipal Commission of Education under Grant KM202111232007, and the China Postdoctoral Science Foundation under Grant 2021M693331.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Li, L. Development of China’s Health Care System in the Time of COVID-19: Challenges, Opportunities, and Call for Actions. Health Care Sci. 2022, 1, 33–40. [Google Scholar] [CrossRef]
- Batko, K.; Ślęzak, A. The Use of Big Data Analytics in Healthcare. J. Big Data 2022, 9, 3. [Google Scholar] [CrossRef] [PubMed]
- Gupta, D.; Denton, B. Appointment Scheduling in Health Care: Challenges and Opportunities. IIE Trans. 2008, 40, 800–819. [Google Scholar] [CrossRef]
- Gao, K.; Shi, X.; Wang, W. The Life-Course Impact of Smoking on Hypertension, Myocardial Infarction and Respiratory Diseases. Sci. Rep. 2017, 7, 4330. [Google Scholar] [CrossRef] [PubMed]
- Qu, L.; Gao, K.; Chen, X.; He, Q.; Ma, Y.; Peng, R. Optimal Quarantine Duration for Preventing Epidemic with Window Period. J. Infect. Non Infect. Dis. 2020, 5, 28. [Google Scholar]
- Alrefaei, M.H.; Diabat, A. Modelling and Optimization of Outpatient Appointment Scheduling. RAIRO-Oper. Res. 2015, 49, 435–450. [Google Scholar] [CrossRef]
- Hulshof, P.J.H.; Vanberkel, P.T.; Boucherie, R.J.; Hans, E.W.; Van Houdenhoven, M.; Van Ommeren, J.-K.C.W. Analytical Models to Determine Room Requirements in Outpatient Clinics. OR Spectr. 2012, 34, 391–405. [Google Scholar] [CrossRef]
- Huang, Y.-L.; Marcak, J. Grid Patient Appointment Template Design to Improve Scheduling Effectiveness. J. Healthc. Eng. 2015, 6, 239–258. [Google Scholar] [CrossRef]
- Liu, N.; Finkelstein, S.R.; Kruk, M.E.; Rosenthal, D. When Waiting to See a Doctor Is Less Irritating: Understanding Patient Preferences and Choice Behavior in Appointment Scheduling. Manag. Sci. 2018, 64, 1975–1996. [Google Scholar] [CrossRef]
- Wright, P.D.; Bretthauer, K.M.; Cote, M.J. Reexamining the Nurse Scheduling Problem: Staffing Ratios and Nursing Shortages. Decis. Sci. 2006, 37, 39–70. [Google Scholar] [CrossRef]
- Talluri, K.; Van Ryzin, G. Revenue Management Under a General Discrete Choice Model of Consumer Behavior. Manag. Sci. 2004, 50, 15–33. [Google Scholar] [CrossRef]
- Gao, K.; Wang, T.; Peng, K.; Wang, Z.; He, Q.; Peng, R. A Recursive Model of Residual Life Prediction for Human Beings with Health Information from Activities of Daily Living and Memory. Syst. Sci. Control Eng. 2021, 9, 529–541. [Google Scholar] [CrossRef]
- Gao, K.; Peng, R.; Qu, L.; Xing, L.; Wang, S.; Wu, D. Linear System Design with Application in Wireless Sensor Networks. J. Ind. Inf. Integr. 2022, 27, 100279. [Google Scholar] [CrossRef]
- Feldman, J.; Liu, N.; Topaloglu, H.; Ziya, S. Appointment Scheduling Under Patient Preference and No-Show Behavior. Oper. Res. 2014, 62, 794–811. [Google Scholar] [CrossRef]
- Gupta, D.; Wang, W.-Y. Patient appointments in ambulatory care. In Handbook of Healthcare System Scheduling; Hall, R., Ed.; International Series in Operations Research & Management Science; Springer US: Boston, MA, USA, 2012; Volume 168, pp. 65–104. ISBN 978-1-4614-1733-0. [Google Scholar]
- Vieira, B.; Hans, E.W.; Van Vliet-Vroegindeweij, C.; Van De Kamer, J.; Van Harten, W. Operations Research for Resource Planning and -Use in Radiotherapy: A Literature Review. BMC Med. Inf. Decis. Mak. 2016, 16, 149. [Google Scholar] [CrossRef] [PubMed]
- Cayirli, T.; Veral, E. Outpatient Scheduling in Health Care: A Review of Literature. Prod. Oper. Manag. 2009, 12, 519–549. [Google Scholar] [CrossRef]
- Ahmadi-Javid, A.; Jalali, Z.; Klassen, K.J. Outpatient Appointment Systems in Healthcare: A Review of Optimization Studies. Eur. J. Oper. Res. 2017, 258, 3–34. [Google Scholar] [CrossRef]
- Woodcock, E.W. Barriers to and Facilitators of Automated Patient Self-Scheduling for Health Care Organizations: Scoping Review. J. Med. Internet Res. 2022, 24, e28323. [Google Scholar] [CrossRef]
- Marynissen, J.; Demeulemeester, E. Literature Review on Multi-Appointment Scheduling Problems in Hospitals. Eur. J. Oper. Res. 2019, 272, 407–419. [Google Scholar] [CrossRef]
- Ala, A.; Chen, F. Appointment Scheduling Problem in Complexity Systems of the Healthcare Services: A Comprehensive Review. J. Healthc. Eng. 2022, 2022, 5819813. [Google Scholar] [CrossRef]
- Ala, A.; Simic, V.; Deveci, M.; Pamucar, D. Simulation-Based Analysis of Appointment Scheduling System in Healthcare Services: A Critical Review. Arch. Comput. Methods Eng. 2023, 30, 1961–1978. [Google Scholar] [CrossRef]
- Dantas, L.F.; Fleck, J.L.; Cyrino Oliveira, F.L.; Hamacher, S. No-Shows in Appointment Scheduling—A Systematic Literature Review. Health Policy 2018, 122, 412–421. [Google Scholar] [CrossRef] [PubMed]
- Wilson, R.; Winnard, Y. Causes, Impacts and Possible Mitigation of Non-Attendance of Appointments within the National Health Service: A Literature Review. J. Health Organ. Manag. 2022, 36, 892–911. [Google Scholar] [CrossRef] [PubMed]
- Donthu, N.; Kumar, S.; Mukherjee, D.; Pandey, N.; Lim, W.M. How to Conduct a Bibliometric Analysis: An Overview and Guidelines. J. Bus. Res. 2021, 133, 285–296. [Google Scholar] [CrossRef]
- Leeftink, A.G.; Vliegen, I.M.H.; Hans, E.W. Stochastic Integer Programming for Multi-Disciplinary Outpatient Clinic Planning. Health Care Manag. Sci. 2019, 22, 53–67. [Google Scholar] [CrossRef] [PubMed]
- Green, L.V.; Savin, S. Reducing Delays for Medical Appointments: A Queueing Approach. Oper. Res. 2008, 56, 1526–1538. [Google Scholar] [CrossRef]
- Bobbie, A.; Karwowski, W. Simulation-Based Evaluation of Patient Appointment Policies for a Primary Care Clinic with Unscheduled Visits: A Case Study. Int. J. Hum. Factors Model. Simul. 2019, 7, 152. [Google Scholar] [CrossRef]
- Lin, C.K.Y.; Ling, T.W.C.; Yeung, W.K. Resource Allocation and Outpatient Appointment Scheduling Using Simulation Optimization. J. Healthc. Eng. 2017, 2017, 9034737. [Google Scholar] [CrossRef]
- Robinson, L.W.; Chen, R.R. Scheduling Doctors’ Appointments: Optimal and Empirically-Based Heuristic Policies. IIE Trans. 2003, 35, 295–307. [Google Scholar] [CrossRef]
- Shonick, W. An Approach to Reducing the Adverse Effects of Broken Appointments in Primary Care Systems. Med. Care 1977, 15, 419–429. [Google Scholar] [CrossRef]
- Chen, P.-S.; Hong, I.-H.; Hou, Y.; Shao, Y.-C. Healthcare Scheduling Policies in a Sequence-Number Based Appointment System for Outpatients’ Arrivals: Early, on Time, or Late? Comput. Ind. Eng. 2019, 130, 298–308. [Google Scholar] [CrossRef]
- Tomkins, A.; Naylor, S.; Morgan, E. Short Message Service Cancellation Intervention to Reduce Integrated Sexual Health and HIV ‘Did Not Attend’ Appointment Rates. Int. J. STD AIDS 2019, 30, 201–203. [Google Scholar] [CrossRef] [PubMed]
- Williamson, A.E.; Ellis, D.A.; Wilson, P.; McQueenie, R.; McConnachie, A. Understanding Repeated Non-Attendance in Health Services: A Pilot Analysis of Administrative Data and Full Study Protocol for a National Retrospective Cohort. BMJ Open 2017, 7, e014120. [Google Scholar] [CrossRef] [PubMed]
- Dickey, W.; Morrow, J.I. Can Outpatient Non-Attendance Be Predicted from the Referral Letter? An Audit of Default at Neurology Clinics. J. R. Soc. Med. 1991, 84, 662–663. [Google Scholar] [CrossRef] [PubMed]
- Barz, C.; Rajaram, K. Elective Patient Admission and Scheduling under Multiple Resource Constraints. Prod. Oper. Manag. 2015, 24, 1907–1930. [Google Scholar] [CrossRef]
- Burke, E.K.; De Causmaecker, P.; Berghe, G.V.; Van Landeghem, H. The State of the Art of Nurse Rostering. J. Sched. 2004, 7, 441–499. [Google Scholar] [CrossRef]
- Jansson, B. Choosing a Good Appointment System—A Study of Queues of the Type (D, M, 1). Oper. Res. 1966, 14, 292–312. [Google Scholar] [CrossRef]
- Chiu, C.-K. Understanding Relationship Quality and Online Purchase Intention in E-Tourism: A Qualitative Application. Qual. Quant. 2009, 43, 669–675. [Google Scholar] [CrossRef]
- Mak, H.-Y.; Rong, Y.; Zhang, J. Sequencing Appointments for Service Systems Using Inventory Approximations. Manuf. Serv. Oper. Manag. 2014, 16, 251–262. [Google Scholar] [CrossRef]
- Denton, B.; Gupta, D. A Sequential Bounding Approach for Optimal Appointment Scheduling. IIE Trans. 2003, 35, 1003–1016. [Google Scholar] [CrossRef]
- Klassen, K.J.; Rohleder, T.R. Outpatient Appointment Scheduling with Urgent Clients in a Dynamic, Multi-period Environment. Int. J. Serv. Ind. Manag. 2004, 15, 167–186. [Google Scholar] [CrossRef]
- Cayirli, T.; Veral, E.; Rosen, H. Designing Appointment Scheduling Systems for Ambulatory Care Services. Health Care Manag. Sci. 2006, 9, 47–58. [Google Scholar] [CrossRef]
- Patrick, J.; Puterman, M.L.; Queyranne, M. Dynamic Multipriority Patient Scheduling for a Diagnostic Resource. Oper. Res. 2008, 56, 1507–1525. [Google Scholar] [CrossRef]
- Solmaz, H. Comparison of Patients’ Admissions to the Cardiology Outpatient Clinics Between the Appointment System and the Queue System. Arch. Turk. Soc. Cardiol. 2023, 51, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Afrane, S.; Appah, A. Queuing Theory and the Management of Waiting-Time in Hospitals: The Case of Anglo Gold Ashanti Hospital in Ghana. Int. J. Acad. Res. Bus. Soc. Sci. 2014, 4, 34–44. [Google Scholar] [CrossRef]
- Soriano, A.; Cayirli, T.; Yang, K.K.; Kong, Q.; Lee, C.-Y.; Teo, C.-P.; Zheng, Z.; Robinson, L.W.; Chen, R.R.; Denton, B.T.; et al. Comparison of Two Scheduling Systems. Oper. Res. 1966, 14, 388–397. [Google Scholar] [CrossRef]
- LaGanga, L.R.; Lawrence, S.R. Appointment Overbooking in Health Care Clinics to Improve Patient Service and Clinic Performance. Prod. Oper. Manag. 2012, 21, 874–888. [Google Scholar] [CrossRef]
- Shnits, B.; Bendavid, I.; Marmor, Y.N. An Appointment Scheduling Policy for Healthcare Systems with Parallel Servers and Pre-Determined Quality of Service. Omega 2020, 97, 102095. [Google Scholar] [CrossRef]
- Cayirli, T.; Yang, K.K. Altering the Environment to Improve Appointment System Performance. Serv. Sci. 2019, 11, 138–154. [Google Scholar] [CrossRef]
- Rohleder, T.; Klassen, K.J. Using Client-Variance Information to Improve Dynamic Appointment Scheduling Performance. Omega 2000, 28, 293–302. [Google Scholar] [CrossRef]
- Creemers, S.; Lambrecht, M.R.; Beliën, J.; Van Den Broeke, M. Evaluation of Appointment Scheduling Rules: A Multi-Performance Measurement Approach. Omega 2021, 100, 102231. [Google Scholar] [CrossRef]
- Bosch, P.M.V.; Dietz, D.C. Minimizing Expected Waiting in a Medical Appointment System. IIE Trans. 2000, 32, 841–848. [Google Scholar] [CrossRef]
- Cayirli, T.; Yang, K.K.; Quek, S.A. A Universal Appointment Rule in the Presence of No-Shows and Walk-Ins. Prod. Oper. Manag. 2012, 21, 682–697. [Google Scholar] [CrossRef]
- Klassen, K.J.; Yoogalingam, R. An Assessment of the Interruption Level of Doctors in Outpatient Appointment Scheduling. Oper. Manag. Res. 2008, 1, 95–102. [Google Scholar] [CrossRef]
- Klassen, K.J.; Yoogalingam, R. Improving Performance in Outpatient Appointment Services with a Simulation Optimization Approach. Prod. Oper. Manag. 2009, 18, 447–458. [Google Scholar] [CrossRef]
- Peng, Y.; Qu, X.; Shi, J. A Hybrid Simulation and Genetic Algorithm Approach to Determine the Optimal Scheduling Templates for Open Access Clinics Admitting Walk-in Patients. Comput. Ind. Eng. 2014, 72, 282–296. [Google Scholar] [CrossRef]
- Meersman, T.; Maenhout, B. Multi-Objective Optimisation for Constructing Cyclic Appointment Schedules for Elective and Urgent Patients. Ann. Oper. Res. 2022, 312, 909–948. [Google Scholar] [CrossRef]
- Cayirli, T.; Yang, K.K. A Universal Appointment Rule with Patient Classification for Service Times, No-Shows, and Walk-Ins. Serv. Sci. 2014, 6, 274–295. [Google Scholar] [CrossRef]
- Salzarulo, P.A.; Mahar, S.; Modi, S. Beyond Patient Classification: Using Individual Patient Characteristics in Appointment Scheduling. Prod. Oper. Manag. 2016, 25, 1056–1072. [Google Scholar] [CrossRef]
- Robinson, L.W.; Chen, R.R. A Comparison of Traditional and Open-Access Policies for Appointment Scheduling. Manuf. Serv. Oper. Manag. 2010, 12, 330–346. [Google Scholar] [CrossRef]
- Qu, X.; Rardin, R.L.; Williams, J.A.S. Single versus Hybrid Time Horizons for Open Access Scheduling. Comput. Ind. Eng. 2011, 60, 56–65. [Google Scholar] [CrossRef]
- Turkcan, A.; Zeng, B.; Lawley, M. Chemotherapy Operations Planning and Scheduling. IIE Trans. Healthc. Syst. Eng. 2012, 2, 31–49. [Google Scholar] [CrossRef]
- Gocgun, Y.; Bresnahan, B.W.; Ghate, A.; Gunn, M.L. A Markov Decision Process Approach to Multi-Category Patient Scheduling in a Diagnostic Facility. Artif. Intell. Med. 2011, 53, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Saghafian, S.; Austin, G.; Traub, S.J. Operations Research/Management Contributions to Emergency Department Patient Flow Optimization: Review and Research Prospects. IIE Trans. Healthc. Syst. Eng. 2015, 5, 101–123. [Google Scholar] [CrossRef]
- Sauré, A.; Puterman, M.L. The Appointment Scheduling Game. INFORMS Trans. Educ. 2014, 14, 73–85. [Google Scholar] [CrossRef]
- Pérez, E.; Ntaimo, L.; Wilhelm, W.E.; Bailey, C.; McCormack, P. Patient and Resource Scheduling of Multi-Step Medical Procedures in Nuclear Medicine. IIE Trans. Healthc. Syst. Eng. 2011, 1, 168–184. [Google Scholar] [CrossRef]
- Wang, W.-Y.; Gupta, D. Adaptive Appointment Systems with Patient Preferences. Manuf. Serv. Oper. Manag. 2011, 13, 373–389. [Google Scholar] [CrossRef]
- Kong, Q.; Lee, C.-Y.; Teo, C.-P.; Zheng, Z. Scheduling Arrivals to a Stochastic Service Delivery System Using Copositive Cones. Oper. Res. 2013, 61, 711–726. [Google Scholar] [CrossRef]
- Erdogan, S.A.; Denton, B. Dynamic Appointment Scheduling of a Stochastic Server with Uncertain Demand. INFORMS J. Comput. 2013, 25, 116–132. [Google Scholar] [CrossRef]
- Turkcan, A.; Zeng, B.; Muthuraman, K.; Lawley, M. Sequential Clinical Scheduling with Service Criteria. Eur. J. Oper. Res. 2011, 214, 780–795. [Google Scholar] [CrossRef]
- Ozen, A.; Balasubramanian, H. The Impact of Case Mix on Timely Access to Appointments in a Primary Care Group Practice. Health Care Manag. Sci. 2013, 16, 101–118. [Google Scholar] [CrossRef] [PubMed]
- Balasubramanian, H.; Biehl, S.; Dai, L.; Muriel, A. Dynamic Allocation of Same-Day Requests in Multi-Physician Primary Care Practices in the Presence of Prescheduled Appointments. Health Care Manag. Sci. 2014, 17, 31–48. [Google Scholar] [CrossRef] [PubMed]
- Conforti, D.; Guerriero, F.; Guido, R. Optimization Models for Radiotherapy Patient Scheduling. 4OR 2008, 6, 263–278. [Google Scholar] [CrossRef]
- Truong, V.-A. Optimal Advance Scheduling. Manag. Sci. 2015, 61, 1584–1597. [Google Scholar] [CrossRef]
- Anderson, K.; Zheng, B.; Yoon, S.W.; Khasawneh, M.T. An Analysis of Overlapping Appointment Scheduling Model in an Outpatient Clinic. Oper. Res. Health Care 2015, 4, 5–14. [Google Scholar] [CrossRef]
- Zhu, H.; Chen, Y.; Leung, E.; Liu, X. Outpatient Appointment Scheduling with Unpunctual Patients. Int. J. Prod. Res. 2018, 56, 1982–2002. [Google Scholar] [CrossRef]
- Kaandorp, G.C.; Koole, G. Optimal Outpatient Appointment Scheduling. Health Care Manag. Sci. 2007, 10, 217–229. [Google Scholar] [CrossRef]
- Dharmadhikari, N.; Zhang, D.J. Simulation Optimization of Blocking Appointment Scheduling Policies for Multi-Clinic Appointments in Centralized Scheduling Systems. Ph.D. Thesis, North Dakota State University, Fargo, ND, USA, 2013. Volume 2. [Google Scholar]
- Cordier, J.-P.; Riane, F. Towards a Centralised Appointments System to Optimise the Length of Patient Stay. Decis. Support. Syst. 2013, 55, 629–639. [Google Scholar] [CrossRef]
- Aslani, N.; Zhang, J. Integration of Simulation and DEA to Determine the Most Efficient Patient Appointment Scheduling Model for a Specific Healthcare Setting. J. Ind. Eng. Manag. 2014, 7, 785–815. [Google Scholar] [CrossRef]
- Shuang, M.; Songlin, C.; Xiaotian, C. A Two-stage stochastic programming model for outpatient appointment scheduling. In Proceedings of the 2019 IEEE International Conference on Industrial Engineering and Engineering Management (IEEM), Macao, China, 15–18 December 2019; pp. 79–83. [Google Scholar]
- El-Sharo, M.; Zheng, B.; Yoon, S.W.; Khasawneh, M.T. An Overbooking Scheduling Model for Outpatient Appointments in a Multi-Provider Clinic. Oper. Res. Health Care 2015, 6, 1–10. [Google Scholar] [CrossRef]
- Salemi Parizi, M.; Ghate, A. Multi-Class, Multi-Resource Advance Scheduling with No-Shows, Cancellations and Overbooking. Comput. Oper. Res. 2016, 67, 90–101. [Google Scholar] [CrossRef]
- Chakraborty, S.; Muthuraman, K.; Lawley, M. Sequential Clinical Scheduling with Patient No-Shows and General Service Time Distributions. IIE Trans. 2010, 42, 354–366. [Google Scholar] [CrossRef]
- Chakraborty, S.; Muthuraman, K.; Lawley, M. Sequential Clinical Scheduling with Patient No-Show: The Impact of Pre-Defined Slot Structures. Socio-Econ. Plan. Sci. 2013, 47, 205–219. [Google Scholar] [CrossRef]
- Muthuraman, K.; Lawley, M. A Stochastic Overbooking Model for Outpatient Clinical Scheduling with No-Shows. IIE Trans. 2008, 40, 820–837. [Google Scholar] [CrossRef]
- Geng, N.; Xie, X. Optimal Dynamic Outpatient Scheduling for a Diagnostic Facility With Two Waiting Time Targets. IEEE Trans. Automat. Contr. 2016, 61, 3725–3739. [Google Scholar] [CrossRef]
- Patrick, J. A Markov Decision Model for Determining Optimal Outpatient Scheduling. Health Care Manag. Sci. 2012, 15, 91–102. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Yan, C.; Wang, L.; Lu, D.; Ma, L. Optimization methods for joint capacity and appointment scheduling problem with walk-in patients. In Proceedings of the 2016 35th Chinese Control Conference (CCC), Chengdu, China, 27–29 July 2016; pp. 9600–9604. [Google Scholar]
- Nguyen, T.B.T.; Sivakumar, A.I.; Graves, S.C. A Network Flow Approach for Tactical Resource Planning in Outpatient Clinics. Health Care Manag. Sci. 2015, 18, 124–136. [Google Scholar] [CrossRef] [PubMed]
- Zeng, B.; Turkcan, A.; Lin, J.; Lawley, M. Clinic Scheduling Models with Overbooking for Patients with Heterogeneous No-Show Probabilities. Ann. Oper. Res. 2010, 178, 121–144. [Google Scholar] [CrossRef]
- Yan, C.; Tang, J.; Jiang, B.; Fung, R.Y.K. Sequential Appointment Scheduling Considering Patient Choice and Service Fairness. Int. J. Prod. Res. 2015, 53, 7376–7395. [Google Scholar] [CrossRef]
- Tsai, P.-F.J.; Teng, G.-Y. A Stochastic Appointment Scheduling System on Multiple Resources with Dynamic Call-in Sequence and Patient No-Shows for an Outpatient Clinic. Eur. J. Oper. Res. 2014, 239, 427–436. [Google Scholar] [CrossRef]
- Jiang, B.; Tang, J.; Yan, C. Outpatient Capacity Allocation Considering Adding Capacity to Match High Patient Demand. J. Syst. Sci. Syst. Eng. 2017, 26, 487–516. [Google Scholar] [CrossRef]
- Jiang, B.; Yu, M. Optimal Outpatient Capacity Allocation under the Capacity-Addition Policy. Comput. Ind. Eng. 2022, 174, 108791. [Google Scholar] [CrossRef]
- Sevinc, S.; Sanli, U.A.; Goker, E. Algorithms for Scheduling of Chemotherapy Plans. Comput. Biol. Med. 2013, 43, 2103–2109. [Google Scholar] [CrossRef] [PubMed]
- Savelsbergh, M.; Smilowitz, K. Stratified Patient Appointment Scheduling for Mobile Community-Based Chronic Disease Management Programs. IIE Trans. Healthc. Syst. Eng. 2016, 6, 65–78. [Google Scholar] [CrossRef]
- Zhu, H.; Hou, M.; Wang, C.; Zhou, M. An Efficient Outpatient Scheduling Approach. IEEE Trans. Autom. Sci. Eng. 2012, 9, 701–709. [Google Scholar] [CrossRef]
- Erdelyi, A.; Topaloglu, H. Computing Protection Level Policies for Dynamic Capacity Allocation Problems by Using Stochastic Approximation Methods. IIE Trans. 2009, 41, 498–510. [Google Scholar] [CrossRef]
- Gao, K.; Peng, R.; Qu, L.; Wu, S. Jointly Optimizing Lot Sizing and Maintenance Policy for a Production System with Two Failure Modes. Reliab. Eng. Syst. Saf. 2020, 202, 106996. [Google Scholar] [CrossRef]
- Bai, G.; Chi, Y.; Gao, K.; Peng, R. Reliability Evaluation of Multi-State Systems with Common Bus Performance Sharing Considering Performance Excess. IEEE Access 2022, 10, 19174–19185. [Google Scholar] [CrossRef]
- Lei, B.; Ren, Y.; Luan, H.; Dong, R.; Wang, X.; Liao, J.; Fang, S.; Gao, K. A Review of Optimization for System Reliability of Microgrid. Mathematics 2023, 11, 822. [Google Scholar] [CrossRef]
- Gao, K.; Wang, T.; Han, C.; Xie, J.; Ma, Y.; Peng, R. A Review of Optimization of Microgrid Operation. Energies 2021, 14, 2842. [Google Scholar] [CrossRef]
- Ren, Y.; Jin, C.; Fang, S.; Yang, L.; Wu, Z.; Wang, Z.; Peng, R.; Gao, K. A Comprehensive Review of Key Technologies for Enhancing the Reliability of Lithium-Ion Power Batteries. Energies 2023, 16, 6144. [Google Scholar] [CrossRef]
- Homem-de-Mello, T.; Kong, Q.; Godoy-Barba, R. A Simulation Optimization Approach for the Appointment Scheduling Problem with Decision-Dependent Uncertainties. INFORMS J. Comput. 2022, 34, 2845–2865. [Google Scholar] [CrossRef]
- Liu, N.; Ziya, S. Panel Size and Overbooking Decisions for Appointment-Based Services under Patient No-Shows. Prod. Oper. Manag. 2014, 23, 2209–2223. [Google Scholar] [CrossRef]
- Zhang, Z.; Berg, B.P.; Denton, B.T.; Xie, X. Appointment Scheduling and the Effects of Customer Congestion on Service. IISE Trans. 2019, 51, 1075–1090. [Google Scholar] [CrossRef]
- Luo, J.; Kulkarni, V.G.; Ziya, S. Appointment Scheduling Under Patient No-Shows and Service Interruptions. Manuf. Serv. Oper. Manag. 2012, 14, 670–684. [Google Scholar] [CrossRef]
- Gao, K.; Yan, X.; Peng, R.; Xing, L. Economic Design of a Linear Consecutively Connected System Considering Cost and Signal Loss. IEEE Trans. Syst. Man. Cybern. Syst. 2021, 51, 5116–5128. [Google Scholar] [CrossRef]
- Saremi, A.; Jula, P.; ElMekkawy, T.; Wang, G.G. Appointment Scheduling of Outpatient Surgical Services in a Multistage Operating Room Department. Int. J. Prod. Econ. 2013, 141, 646–658. [Google Scholar] [CrossRef]
- Braune, R.; Gutjahr, W.J.; Vogl, P. Stochastic Radiotherapy Appointment Scheduling. Cent. Eur. J. Oper. Res. 2022, 30, 1239–1277. [Google Scholar] [CrossRef]
- Fan, X.; Tang, J.; Yan, C.; Guo, H.; Cao, Z. Outpatient Appointment Scheduling Problem Considering Patient Selection Behavior: Data Modeling and Simulation Optimization. J. Comb. Optim. 2021, 42, 677–699. [Google Scholar] [CrossRef]
- Alizadeh, R.; Rezaeian, J.; Abedi, M.; Chiong, R. A Modified Genetic Algorithm for Non-Emergency Outpatient Appointment Scheduling with Highly Demanded Medical Services Considering Patient Priorities. Comput. Ind. Eng. 2020, 139, 106106. [Google Scholar] [CrossRef]
- Dehghanimohammadabadi, M.; Rezaeiahari, M.; Seif, J. Multi-Objective Patient Appointment Scheduling Framework (MO-PASS): A Data-Table Input Simulation–Optimization Approach. Simulation 2023, 99, 363–383. [Google Scholar] [CrossRef]
- Ala, A.; Alsaadi, F.E.; Ahmadi, M.; Mirjalili, S. Optimization of an Appointment Scheduling Problem for Healthcare Systems Based on the Quality of Fairness Service Using Whale Optimization Algorithm and NSGA-II. Sci. Rep. 2021, 11, 19816. [Google Scholar] [CrossRef] [PubMed]
- Qiu, H.; Wang, D.; Wang, Y.; Yin, Y. MRI Appointment Scheduling with Uncertain Examination Time. J. Comb. Optim. 2019, 37, 62–82. [Google Scholar] [CrossRef]
- Garaix, T.; Rostami, S.; Xie, X. Daily Outpatient Chemotherapy Appointment Scheduling with Random Deferrals. Flex. Serv. Manuf. J. 2020, 32, 129–153. [Google Scholar] [CrossRef]
- Corsini, R.R.; Costa, A.; Fichera, S.; Parrinello, V. Hybrid Harmony Search for Stochastic Scheduling of Chemotherapy Outpatient Appointments. Algorithms 2022, 15, 424. [Google Scholar] [CrossRef]
- Ala, A.; Chen, F. An appointment scheduling optimization method in healthcare with simulation approach. In Proceedings of the 2020 IEEE 7th International Conference on Industrial Engineering and Applications (ICIEA), Bangkok, Thailand, 16–21 April 2020; pp. 833–837. [Google Scholar]
- Rajakumari, K.; Madhunisha, M. Intelligent and convolutional-neural-network based smart hospital and patient scheduling system. In Proceedings of the 2020 International Conference on Computer Communication and Informatics (ICCCI), Coimbatore, India, 22–24 January 2020; pp. 1–5. [Google Scholar]
- Dogru, A.K.; Melouk, S.H. Adaptive Appointment Scheduling for Patient-Centered Medical Homes. Omega 2019, 85, 166–181. [Google Scholar] [CrossRef]
- Squires, M.; Tao, X.; Elangovan, S.; Gururajan, R.; Zhou, X.; Acharya, U.R. A Novel Genetic Algorithm Based System for the Scheduling of Medical Treatments. Expert. Syst. Appl. 2022, 195, 116464. [Google Scholar] [CrossRef]
- Akbarzadeh, B.; Moslehi, G.; Reisi-Nafchi, M.; Maenhout, B. The Re-Planning and Scheduling of Surgical Cases in the Operating Room Department after Block Release Time with Resource Rescheduling. Eur. J. Oper. Res. 2019, 278, 596–614. [Google Scholar] [CrossRef]
- Chen, C. CiteSpace II: Detecting and Visualizing Emerging Trends and Transient Patterns in Scientific Literature. J. Am. Soc. Inf. Sci. 2006, 57, 359–377. [Google Scholar] [CrossRef]
- Fragidis, L.L.; Chatzoglou, P.D.; Aggelidis, V.P. Integrated Nationwide Electronic Health Records System: Semi-Distributed Architecture Approach. Technol. Health Care 2016, 24, 827–842. [Google Scholar] [CrossRef]
- Kallos, A.; Perez, A.; O’Neill, M.G.; Holt, N.L.; Bruce, A.; Childs, M.; Kane Poitras, S.; Kherani, T.; Ladha, T.; Majaesic, C.; et al. Recommendations from Parents, Administrative Staff and Clinicians to Improve Paediatric Ambulatory Appointment Scheduling. Child 2021, 47, 834–843. [Google Scholar] [CrossRef] [PubMed]
- Krzyzanowski, B.; Manson, S.M. Twenty Years of the Health Insurance Portability and Accountability Act Safe Harbor Provision: Unsolved Challenges and Ways Forward. JMIR Med. Inf. 2022, 10, e37756. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, C.-J.; King, J.; Hing, E.; Simon, A.E. The Role of Health Information Technology in Care Coordination in the United States. Med. Care 2015, 53, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Novillo-Ortiz, D.; Dumit, E.M.; D’Agostino, M.; Becerra-Posada, F.; Kelley, E.T.; Torrent-Sellens, J.; Jiménez-Zarco, A.; Saigí-Rubió, F. Digital Health in the Americas: Advances and Challenges in Connected Health. BMJ Innov. 2018, 4, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Lv, Z.; Qiao, L. Analysis of Healthcare Big Data. Future Gener. Comput. Syst. 2020, 109, 103–110. [Google Scholar] [CrossRef]
- Lee, J.; Park, Y.-T.; Park, Y.R.; Lee, J.-H. Review of National-Level Personal Health Records in Advanced Countries. Healthc. Inf. Res. 2021, 27, 102–109. [Google Scholar] [CrossRef]
- Ratwani, R.M. Electronic Health Records and Improved Patient Care: Opportunities for Applied Psychology. Curr. Dir. Psychol. Sci. 2017, 26, 359–365. [Google Scholar] [CrossRef]
- Yogesh, M.J.; Karthikeyan, J. Health Informatics: Engaging Modern Healthcare Units: A Brief Overview. Front. Public Health 2022, 10, 854688. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).