Abstract
The chance to critically and microscopically inspect the quality of bonded restorations once they are delivered to the patient after several pre-cementation steps is rare or nonexistent. Replicas of in-service restorations can provide a wealth of information on the integrity of the restorations and moreover make it possible to bring this information to the laboratory for further detailed analysis. This study aimed to characterize the epoxy replicas of 27 cemented monolithic yttria-stabilized zirconia crowns of the maxillary and mandibular arch to assess surface roughness, topography, and symmetry. The topography of the facial, lingual, and occlusal/incisal surfaces of each crown was observed under the optical microscope and further characterized using the scanning electron microscope. Surface roughness measurements were performed using the atomic force microscope. The optical microscope was used to measure the golden proportion and visible width of the anterior maxillary crowns. Surface damage consistent with unpolished adjustment was identified mostly in the occlusal surface of the posterior teeth. Other irregularities, such as scratch marks, small pits, and coarse pits were also found. The surface roughness had great variability. Not all of the anterior maxillary and mandibular teeth followed the golden proportion concept. This study design allows in vitro characterization of in-service restorations. It provides a framework for using replicas for early identification of patterns or features that can trigger fracture and for analysis of morphology and symmetry.
1. Introduction
A wide variety of ceramic materials are available for the fabrication of indirect restorations, such as veneers, crowns, multi-unit fixed dental prostheses, inlays, and onlays. Polycrystalline ceramics began to be used in the 1990s, initially with alumina crystals and later with zirconia crystals [1,2]. In general, the main characteristics that differentiated these polycrystalline ceramics from the others are the absence of a glass matrix, the high mechanical properties, and the great opacity [2]. More recently, yttria-stabilized zirconia (YSZ) ceramics that contain a higher yttria content and a higher cubic/tetragonal ratio have been introduced into dentistry, allowing greater translucency and their use in a monolithic form [3]. This latest YSZ generation brings the opportunity to provide the patient with esthetic improvement, as well as outstanding mechanical properties. Moreover, gradient monolithic YSZ restorations enable a more simplified procedure for manufacturing the restorations than in previous generations by prescinding a veneer material and possibly being less costly. To date, monolithic YSZ restorations, also known as full- contour restorations, have shown a success and survival rate of 98–100% after a 1-year follow-up [4,5] and 98% after 5 years [6]. However, we are still learning more and more about the behavior of monolithic YSZ structures while they are in service and about the potential causes of failure.
In general, the failure mechanism of dental ceramics has been defined as complex [7]. It is more common to find studies characterizing the surface and morphology of the ceramic restorations after catastrophic failure occurs. The chances to critically observe the restorations with regard to the mechanical, biological, and esthetic requirements, once delivered and placed in the patient’s mouth, are rare or nonexistent. The unfeasibility of putting the cemented restorations and the patient under the microscope for further analysis can be overcome by the replication of the restorations using the replica technique [8,9,10]. Epoxy resin replicas obtained from polyvinylsiloxane impressions have proven to reproduce up to the nanometric features of the replicated object: the tooth structure, the restorative material, or even the complete arch [9,10]. Therefore, information such as the topography, superficial integrity, and surface roughness can be collected from replicas. Another important aspect of examining the replicas of post-cementation restorations is the characterization of the restorations’ symmetry or asymmetry analysis. The analysis of the golden proportion, also referred to as Phi, is suggested as a mathematical approach to developing the ideal size and shape relationships for maxillary teeth, hence the association with esthetics, a pleasant smile and harmony [11,12]. This proportion was first introduced and described geometrically by Euclid in the 4th century BC as the division of a line (AB) into 2 parts (AC and CB) in such a way that AB:AC = AC:CB. The golden proportion is a constant ratio between the larger and the smaller teeth. This ratio is approximately 1.618:1. According to this ratio, the smaller anterior tooth is nearly 62% of the adjacent larger tooth. The concept of the golden proportion is not restricted only to dentistry, but has also been widely applied in other fields, such as art, engineering (e.g., building construction), and modern architecture (e.g., in windows, furniture, and cars). Indeed, it is found in nature in shells, flowers, trees, hurricanes, and the alignment of the planets, just to name a few [13].
This study aimed to characterize replicas of in-service dental crowns made of monolithic translucent zirconia in terms of their surface roughness, surface topography, and symmetry. It is hypothesized that the in-service restorations will show similar surface features, and the anterior teeth will follow the golden proportion.
2. Materials and Methods
The characterization of translucent zirconia restorations was performed by using epoxy replicas obtained by casting low-viscosity, low-shrinkage epoxy (EpoxySet, Allied High Tech Products Inc., Compton, CA, USA) onto the disinfected polyvinylsiloxane impressions (Elite HD + light and heavy body, Zhermack, Badia Polesine (RO), Italy) of a full-mouth rehabilitation of the upper and lower jaw. The impressions were taken by the dentist 2 days after cementation of the restorations as a control of his work. The information about the zirconia restorations is de-identified (without the patient’s name, address, birthdate, age, social security number, zip code, or any other identifier associated with the patient’s personal and health information). Twenty-seven monolithic zirconia crowns were present and examined. Those 27 restorations constituted the sample size of our study. As seen in the epoxy resin model, tooth #1, 15–17, and 32 were not present. The free surfaces—facial (F), incisal (I), or occlusal (O), and lingual (L) surfaces of each restoration—were characterized qualitatively and quantitatively. Mesial and distal surfaces were not possible to analyze because of the adjacent teeth in the model. Our study did not include the lingual surface of the last posterior teeth in the arch in the inspection to standardize the surface analysis.
2.1. Topography Analysis
All 27 epoxy replicas of the restorations were carefully observed under the optical microscope (VHX-1000, Keyence, Itasca, IL, USA). Surface damage and irregularities (texture differences) were registered. Both were further characterized in a scanning electron microscope (SEM, SUPRA 40, Carl Zeiss, Thornwood, NY, USA). Prior to SEM examination, the epoxy replicas were sprayed with the scanning preparation CEREC® Optispray (Sirona Dental, Bensheim, Germany) for the acquisition of the digital images using the Planmeca Emerald™ intraoral scanner (Planmeca Emerald, Helsinki, Finland). The scans were recorded and exported from the Romexis software in STL format. The total area of surface damage found in each surface was analyzed using free and open-source software (3D Slicer 4.11.20210226, http://www.slicer.org/ (accessed on 20 July 2021)) for image analysis. Following this analysis, the epoxy-poured replicas were cleaned with enzymatic detergent (Patterson Multipurpose Enzyme Tablets, Patterson Dental, Saint Paul, MN, USA) followed by deionized water, both in an ultrasonic bath (Model 150T, Aqua Sonic, VWR scientific products, Radnor, PA, USA) to remove surface contamination. The epoxy replicas were air dried with an oil-free stream, sputter-coated with 4 nm gold (EM ACE-600, Leica Microsystems, Buffalo Grove, IL, USA) and observed under the SEM using a secondary electron detector. Twenty gold-coated, epoxy-poured replicas of the restorations were re-examined.
2.2. Surface Roughness Analysis
Another set of epoxy resin replicas was obtained from the impressions. The epoxy was poured on the previously identified smooth and rough areas of the facial and lingual surfaces of each tooth and observed under the optical microscope. The epoxy replicas were then carefully placed on polymeric clay (Sculpey III, Polyform Products Company, Elk Grove Village, IL, USA), ensuring that the area of interest was facing upward and macroscopically leveled. A 15 µm by 15 µm region on the replicas was scanned using an atomic force microscope (AFM, Bioscope Catalyst, Bruker Corporation, Santa Barbara, CA, USA) with a ScanAsyst Air probe (Bruker Corporation, Santa Barbara, CA, USA) in the PeakForce Tapping mode at a scanning rate of 0.977 Hz with 512 by 512 samples/line. The scans were leveled digitally using the Nanoscope analysis software (Bruker Corporation, Santa Barbara, CA, USA) to remove any tilt. Surface roughness measured by the AFM-topography images was measured with the Gwyddion 2.39 software [14].
2.3. Symmetry Analysis
The height, width, and height-to-width ratio of the facial surfaces of the maxillary and mandibular anterior crowns were measured using the 3D Slicer and compared with the golden proportion. The height of the maxillary and mandibular anterior teeth were measured from the incisal edge up to the most apical point at the gingival margin (the longest visible apicocoronal distance parallel to the long axis of the tooth), while the width was measured at three levels: at the gingival third (the distance between the mesial and distal gingival embrasures), at the middle third (the distance between the mesial and distal points of contact), and at the incisal third (the distance between the mesial and distal incisal facial embrasures). The visible width of the maxillary anterior teeth was noted for the height-to-width ratio calculation. In addition to that, the facial form of the anterior teeth (square, ovoid, or tapered) and the visible width of the upper posterior teeth were registered. The measurement of the facial surfaces’ anatomical contour was performed using the Open Curve Markup tool in 3D Slicer. The visible width of the facial surface of every posterior restoration was measured and compared to the mesio-distal distance in the frontal view.
The qualitative data on topography were not submitted to statistical analysis since the observations cannot be tested to see if they are statistically significant. Surface roughness data were analyzed using one-way ANOVA (α = 0.050). The symmetry data of the anterior restorations were compared by the percent difference between the obtained value and the gold standard to determine their closeness.
3. Results
3.1. Topography Analysis
The optical microscope revealed that 20 (74.1%) out of the 27 examined teeth presented surface damage, while 13 (48.1%) presented irregularities different from the surface damage. The SEM evaluation highlighted that the damage was predominant on the occlusal surface of the posterior teeth. Surface irregularities were found the most in the lingual face of the posterior teeth. Detailed results are depicted in Table 1.

Table 1.
Surface topography (surface irregularities and damage) of the epoxy resin replicas of zirconia monolithic restorations.
Figure 1 shows representative images of the different surface damage findings observed under both microscope analyses. The damage observed was mostly compatible with traces of machining or manual adjustment with diamond or polishing burs by either the dental technician or the dentist. In some cases, the flattening of the cusp tips on the posterior teeth was observed. The damaged area was measured in each detected surface as shown in Table 2. Damage was found in a variety of extensions. In some cases, it compromised as little as ~1% of the surface (tooth #2, occlusal surface, and #31, facial surface), and in other cases it affected a large area of the surface (e.g., 90% of the occlusal surface of tooth #18).
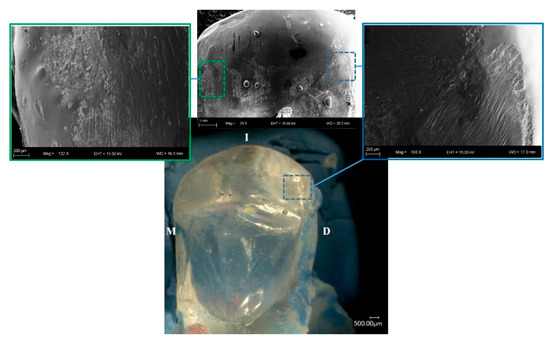
Figure 1.
Lingual view of the epoxy replica of zirconia restoration placed in tooth #6 (bottom). SEM map (top) shows in detail the damage present on the surface to be mostly compatible with adjustment-introduced damage.

Table 2.
Surface damage area per surface per tooth.
The optical microscope revealed irregular surface topography, such as light parallel scratch marks (Figure 2a), small pits (Figure 2b), coarse pits, and irregularities (Figure 2c).
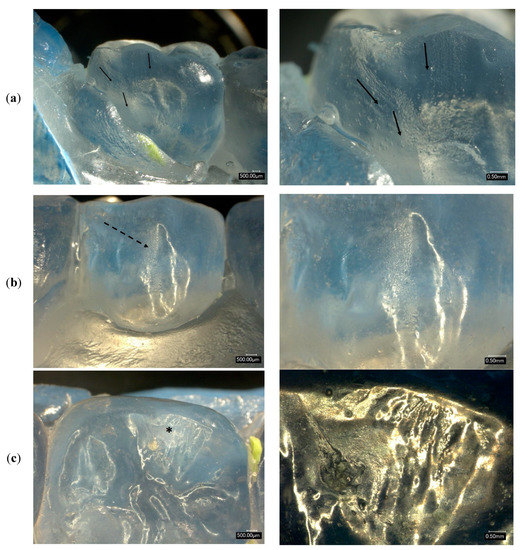
Figure 2.
Three examples of the irregularities present in the resin epoxy replicas of the zirconia restorations. (a) Light scratches on the lingual surface of tooth #31. Black arrows run parallel to the scratches. (b) Dotted arrow points at the small pits on the facial surface of tooth #29. (c) Asterisk shows the irregularity on the occlusal surface relative to the facial cusps. Right images are at higher magnification to show details of the regions of interest indicated by the arrows and asterisk. For Figure (c), the gold-coated epoxy resin sample was observed under the optical microscope.
3.2. Surface Roughness
There was quite a bit of variability in surface roughness values (Ra) among the smooth and irregular surfaces that were analyzed. For instance, Figure 3 shows the difference in surface roughness between an identified smooth area versus another one with irregularities within the same surface. Some surfaces that were classified as smooth under the optical microscope had a surface roughness value in the range of 23.9–46.9 nm, while other smooth surfaces were in the range of 0.1–0.2 nm.
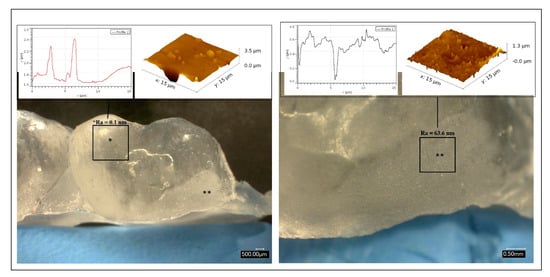
Figure 3.
Buccal surface of an upper posterior tooth (#2) and surface roughness 3D map and profile.
3.3. Symmetry
The width-to-height ratio between the two maxillary central incisors (4:3) and between the lateral incisors (4:3) was similar, although their dimensions varied. There were minor differences between the canines. For the maxillary teeth, the highest mean mesio-distal dimensions were found in the canines (#6, and #11), while the lowest were in the lateral incisors. The mandibular anterior teeth followed a similar trend to the maxillary teeth with regard to the medio-distal dimensions, where the canines had the highest dimensions. However, the lower central incisors were the ones with the lowest mesio-distal width. Moreover, the width-to-height ratio of the four anterior incisors (#23 to #26) was similar, while the canines had ratios very close to each other. All the maxillary anterior teeth were tapered-shaped, while the mandibular anterior teeth were square tapered- shaped. Table 3 summarizes the symmetry results.

Table 3.
Height, width, and width-to-height ratio measurements of the epoxy replicas of the anterior zirconia restorations.
The width of the facial contour and the visible width of the maxillary posterior teeth (2–6, 11–14) showed that for the most posterior we look at there is less visible facial contour of the upper right posterior teeth than the upper left posterior ones, or no visible facial contour (Table 4).

Table 4.
Visible width of the maxillary posterior teeth.
The anterior maxillary zirconia restorations measured by their epoxy replicas did not follow the golden proportion (Figure 4A). A digital simulation of the same teeth following the golden proportion showed that the teeth would look long and narrow (Figure 4B).
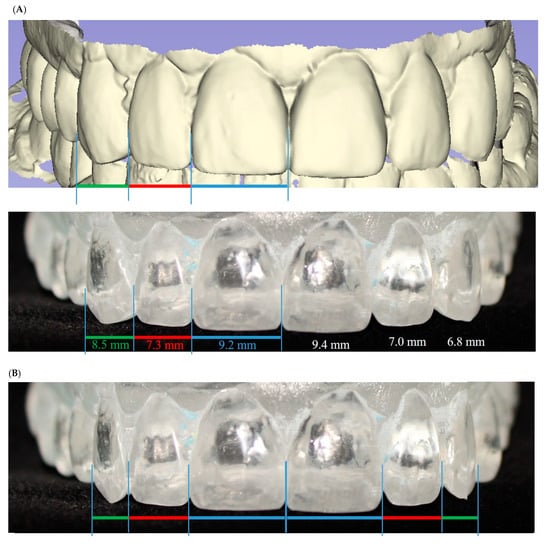
Figure 4.
Visible width and width-to-height ratio measurements of the epoxy replicas of the anterior zirconia restorations from the facial view. (A) Original view of right and left central incisors, lateral incisors, and canines in 3D (top) and epoxy resin (bottom) model. The teeth did not follow the golden proportion. (B) Same image as (A), but digitally modified to fit the golden proportion. Lateral incisor now in the proportion of 1:1.618 with central incisor and 1:0.618 with canine; the size of the central incisor was maintained.
The null hypothesis was rejected as the epoxy replicas of the in-service restorations showed different surface features, including irregularities and damage, and the anterior teeth did not follow the golden proportion.
4. Discussion
The inspection of the ceramic restorations after being delivered to the patient is not a common practice in dentistry. This step is crucial and raises concerns because unnoticed surface changes can occur in the bonded restoration after undergoing processing, adjustment, and finishing by the lab technician or the dentist. Rekow et al. reported that the performance of dental ceramics depends on aspects that inevitably damage the material such as the physical properties of the material, the fabrication methods, the clinical procedures and the oral environment [15]. Failure in ceramic restorations can originate at different locations, such as the top surface, intaglio surfaces, margins, and subsurface [15,16]. Therefore, this study aimed to characterize macro- and microscopically the surface of in-service monolithic crowns, as well as the morphology of the anterior maxillary restorations by using epoxy resin replicas.
The replica technique has been widely used to study the fracture surfaces of specimens in the laboratory or components that failed in service [8,9]. Numerous studies have proven that it can also be useful for other purposes, such as registering the morphological characteristics of cavities, wear, restored teeth, and even plaque formation on human tooth surfaces [10,17,18,19,20,21]. An epoxy resin replica is prepared out of a polyvinylsiloxane impression [8,9] from the object or surface of interest. Epoxy replicas have been shown to retain information from features that are present in the original piece [10]. Our study successfully used epoxy resin replicas in the quest for more information about the quantitative and qualitative macro- and microscopic morphological aspects of ceramic restorations made of the latest generation of a high-strength ceramic material such as YSZ ceramics.
The examination of the epoxy replicas revealed the presence of irregularities and surface damage in many surfaces except on the proximal surfaces of each restoration. The fact that the replicas of the restoration were obtained from the impressions of the already bonded and in-service restorations prevented us from having access to the mesial and distal surfaces and, hence, from inspecting them at those levels. Ten out of the thirteen teeth where surface irregularities were identified presented different flaws predominately in the lingual surfaces. The light parallel scratches suggested adjustment in the restoration surface but with insufficient polishing to achieve a smooth surface. The small pits are consistent with insufficient or incomplete finishing before the restoration delivery to the patient. The coarse pits and irregularities, observed in some elements, seem to be evidence of thick finishing, without the succession of steps from coarse to fine abrasive grits. All of the irregularities suggest a lack of smoothness. Indirect restorations such as the ones examined are supposed to leave the laboratory with a smooth, highly polished surface with the possibility of alteration in the case that the dentist makes adjustments while trying, or after cementing, the restorations. Most of the irregularities were found in the lingual surfaces, which are the less likely areas to be adjusted by the dentist and suggest that the restorations might have been received with the flaws identified here, perhaps in the attempt to contour the restoration. The surface roughness of the “smooth area” of the examined replicas was much lower than the roughness of surfaces submitted to the four-step polishing procedures [22].
The shape, sharpness, size, and depth of the surface flaws can reduce the strength of the ceramic, leading to chipping or bulk fracture of the restoration [23]. The damage tolerance of dental ceramics can differ depending on the grinding direction. Loss in strength has been corroborated more after transversal grinding than longitudinal grinding [24]. Another negative aspect of high surface roughness is that, if present mostly in occlusal contact areas, it can abrade the opposing dentition or restoration [25,26,27]. Polished monolithic YSZ crowns have been reported to generate more wear of opposed enamel than natural teeth [25,26], and this phenomenon is exacerbated when unpolished zirconia is opposing natural dentition. The attrition of monolithic zirconia crowns on natural teeth is lower for premolars (42.10 ± 4.30 μm) than molars (127.00 ± 5.03 μm) [27]. We agree with Øilo’s statement that careful handling of the ceramic is critical and that more emphasis should be given to producing smooth surfaces to avoid unfavorable stress concentrations that can act as fracture origins [23]. High surface roughness can also contribute to plaque accumulation and biofilm growth [28,29]. Thus, it is worrisome when high surface roughness is detected. In this study, high surface roughness values characterized with sharp peaks and valleys were found near the cervical margin of posterior teeth (Figure 3), lingually and facially, which happen to be areas more prone to plaque accumulation. In that sense, it would have been interesting to compare the scan of the restorations before and after cementation to identify the damages made by the dentist during cementation and finishing. However, we did not have access to any records of the patients, including digital records such as scanned images, because they contained patient data and thus allow his/her identification.
The other set of data collected in this study was used to assess the symmetry of the anterior teeth which can affect the esthetic aspect of the smile. The mathematical theorem known as the “golden proportion” was proposed to be used in dentistry to obtain the adequate mesiodistal and cervicoincisal dimensions of the anterior teeth. However, different ratios have been described in the literature as the ideal ones. Some studies stated that the central incisor is in golden proportion when the coronal width-to-height ratio is 62%, and others said that the 75–80% ratio is considered to be most esthetically pleasing [30]. Similarly, Sterret reported that the width-to-height ratio that represents the most stable reference is 81% [31]. More recently, another study reported that the proportion of 85% central incisor, and 80% lateral incisor and canine were considered as more esthetic for both professionals and laypersons [32,33]. Our results showed that tooth #9 was the only one that satisfied precisely Sterret’s recommended ratio (81%). However, the adjacent incisor tooth had a slightly lower ratio (78%). The lateral incisors showed a similar width-to-height ratio (66%), which means that narrow incisors would not be perceived as too esthetic as suggested by Alvarez-Alvarez [33]. The relationship between the width and the length of the clinical crown of teeth can be a useful reference to establish the starting point when managing a case where the original reference of dimensionality of the anterior teeth has been lost. Beyond that, it should be possible to achieve functional stability along with esthetic harmony. However, other parameters can also influence the perception of symmetry and proportion, such as facial contour and the transition of line angles.
Further research studies are needed to critically assess post-cementation, indirect restorations as well as direct restorations. For instance, fiberglass post restored teeth combined with a resin composite core showed a different failure mode than the ceramic restorations, being more susceptible to failure at the post/cement and cement/dentin interfaces rather than superficially [34]. In addition, as further research it would be interesting to continue a periodic follow-up on the performance of the damaged new generation of zirconia restorations over time.
5. Conclusions
Epoxy replicas of the post-cementation final restorations can help identify early patterns or features that can trigger fracture. They were helpful for measurements of surface roughness, symmetry, and topography analysis. Surface flaws were present in more than 50% of the restoration replicas. The considerably variable surface roughness suggests that finishing protocols are not consistently used.
Author Contributions
Conceptualization of study, S.M.S.M.; planning of methodology: S.M.S.M.; metric analysis, M.B.V., A.P. and S.M.S.M.; resources: F.M. and A.P., writing, S.M.S.M. and reviewing and editing the paper, S.M.S.M., M.B.V., F.M., A.P. and S.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data is contained within the article.
Acknowledgments
The authors acknowledge support from the Intramural Research Support Program, and the Biomedical Materials Science Shared Equipment Facility at the School of Dentistry, University of Mississippi Medical Center (UMMC). M.B.V. acknowledges the Summer Undergraduate Research Experience Program at UMMC.
Conflicts of Interest
The authors declare that they have no conflict of interest in preparing this article.
References
- Salazar Marocho, S.M.; Studart, A.R.; Bottino, M.A.; Bona, A.D. Mechanical strength and subcritical crack growth under wet cyclic loading of glass-infiltrated dental ceramics. Dent. Mater. 2010, 26, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.R.; Benetti, P. Ceramic materials in dentistry: Historical evolution and current practice. Aust. Dent. J. 2011, 56, 84–96. [Google Scholar] [CrossRef] [PubMed]
- Fathy, S.M.; Al-Zordk, W.; EGrawish, M.; VSwain, M. Flexural strength and translucency characterization of aesthetic monolithic zirconia and relevance to clinical indications: A systematic review. Dent. Mater. 2021, 37, 711–730. [Google Scholar] [CrossRef]
- Pathan, M.S.; Kheur, M.G.; Patankar, A.H.; Kheur, S.M. Assessment of antagonist enamel wear and clinical performance of full-contour monolithic zirconia crowns: One-year results of a prospective study. J. Prosthodont. 2019, 28, e411–e416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Konstantinidis, I.; Trikka, D.; Gasparatos, S.; Mitsias, M.E. Clinical outcomes of monolithic zirconia crowns with CAD/CAM technology. A 1-Year Follow-Up Prospective Clinical Study of 65 Patients. Int. J. Environ. Res. Public Health 2018, 15, 2523. [Google Scholar] [CrossRef] [Green Version]
- Solá-Ruiz, M.F.; Baixauli-López, M.; Roig-Vanaclocha, A.; Amengual-Lorenzo, J.; Agustín-Panadero, R. Prospective study of monolithic zirconia crowns: Clinical behavior and survival rate at a 5-year follow-up. J. Prosthodont. Res. 2020. online ahead of print. [Google Scholar] [CrossRef]
- Denry, I. How and when does fabrication damage adversely affect the clinical performance of ceramic restorations? Dent. Mater. 2013, 29, 85–96. [Google Scholar] [CrossRef]
- Quinn, G.D. NIST Recommended Practice Guide: Fractography of Ceramics and Glasses; NIST: Gaithersburg, MD, USA, 2006.
- Scherrer, S.S.; Quinn, J.B.; Quinn, G.D.; Wiskott, H.W. Fractographic ceramic failure analysis using the replica technique. Dent. Mater. 2007, 23, 1397–1404. [Google Scholar] [CrossRef] [Green Version]
- Mihlbachler, M.C.; Foy, M.; Beatty, B.L. Surface replication, fidelity and data loss in traditional dental microwear and dental microwear texture analysis. Sci. Rep. 2019, 9, 159. [Google Scholar] [CrossRef] [Green Version]
- Swileh, M.A.; Abuaffan, A.H.; Alhajj, M.N. Evaluation of the golden proportion and golden standard of maxillary anterior teeth in relation to smile attractiveness. Braz. Dent. Sci. 2019, 22, 178–189. [Google Scholar] [CrossRef] [Green Version]
- Al-Marzok, M.I.; Majeed, K.R.; Ibrahim, I.K. Evaluation of maxillary anterior teeth and their relation to the golden proportion in Malaysian population. BMC Oral Health 2013, 13, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chavan, A.D.; Suryawanshi, C.V. Correlation of fibonacci sequence and golden ratio with its applications in engineering and science. Int. J. Eng. Manag. Res. 2020, 10, 31–36. [Google Scholar] [CrossRef]
- Nečas, D.; Klapetek, P. Gwyddion: An open-source software for SPM data analysis. Cent. Eur. J. Phys. 2012, 10, 181–188. [Google Scholar] [CrossRef]
- Rekow, E.D.; Silva, N.R.; Coelho, P.G.; Zhang, Y.; Guess, P.; Thompson, V.P. Performance of dental ceramics: Challenges for improvements. J. Dent. Res. 2011, 90, 937–952. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rashid, H. The effect of surface roughness on ceramics used in dentistry: A review of literature. Eur. J. Dent. 2014, 8, 571–579. [Google Scholar] [CrossRef]
- Lie, T.; Gusberti, F. Replica study of plaque formation on human tooth surfaces. Acta Odontol. Scand. 1979, 37, 65–72. [Google Scholar] [CrossRef]
- Ekfeldt, A.; Flöystrand, F.; Oilo, G. Replica techniques for in vivo studies of tooth surfaces and prosthetic materials. Scand. J. Dent. Res. 1985, 93, 560–565. [Google Scholar] [CrossRef]
- Pintado, M.R.; Conry, J.P.; Douglas, W.H. Fissure sealant wear at 30 months: New evaluation criteria. J. Dent. 1991, 19, 33–38. [Google Scholar] [CrossRef]
- Youngson, C.C.; Grey, N.J. An in vitro comparative analysis: Scanning electron microscopy of dentin/restoration interfaces. Dent. Mater. 1992, 8, 252–258. [Google Scholar] [CrossRef]
- Jodha, K.S.; Salazar Marocho, S.M.; Scherrer, S.S.; Griggs, J.A. Fractal analysis at varying locations of clinically failed zirconia dental implants. Dent. Mater. 2020, 36, 1052–1058. [Google Scholar] [CrossRef]
- Juma’ah, A.A.; Brunton, P.A.; Li, K.C.; Waddell, J.N. Simulated clinical adjustment and intra-oral polishing of two translucent, monolithic zirconia dental ceramics: An in vitro investigation of surface roughness. J. Dent. 2020, 101, 103447. [Google Scholar] [CrossRef]
- Øilo, M.; Quinn, G.D. Fracture origins in twenty-two dental alumina crowns. J. Mech. Behav. Biomed. 2016, 53, 93–103. [Google Scholar] [CrossRef]
- Coldea, A.; Fischer, J.; Swain, M.V.; Thiel, N. Damage tolerance of indirect restorative materials (including PICN) after simulated bur adjustments. Dent. Mater. 2015, 31, 684–694. [Google Scholar] [CrossRef]
- Stober, T.; Bermejo, J.L.; Schwindling, F.S.; Schmitter, M. Clinical assessment of enamel wear caused by monolithic zirconia crowns. J. Oral Rehabil. 2016, 43, 621–629. [Google Scholar] [CrossRef]
- Esquivel-Upshaw, J.F.; Kim, M.J.; Hsu, S.M.; Abdulhameed, N.; Jenkins, R.; Neal, D.; Ren, F.; Clark, A.E. Randomized clinical study of wear of enamel antagonists against polished monolithic zirconia crowns. J. Dent. 2018, 68, 19–27. [Google Scholar] [CrossRef] [Green Version]
- Mundhe, K.; Jain, V.; Pruthi, G.; Shah, N. Clinical study to evaluate the wear of natural enamel antagonist to zirconia and metal ceramic crowns. J. Prosthet. Dent. 2015, 114, 358–363. [Google Scholar] [CrossRef] [PubMed]
- Anami, L.C.; Pereira, C.A.; Guerra, E.; Assunção e Souza, R.O.; Jorge, A.O.; Bottino, M.A. Morphology and bacterial colonisation of tooth/ceramic restoration interface after different cement excess removal techniques. J. Dent. 2012, 40, 742–749. [Google Scholar] [CrossRef] [PubMed]
- Pereira, S.; Anami, L.C.; Pereira, C.A.; Souza, R.; Kantorski, K.Z.; Bottino, M.A.; Jorge, A.; Valandro, L.F. Bacterial Colonization in the Marginal Region of Ceramic Restorations: Effects of Different Cement Removal Methods and Polishing. Oper. Dent. 2016, 41, 642–654. [Google Scholar] [CrossRef] [PubMed]
- Levin, E.I. Dental esthetics and the golden proportion. J. Prosthet. Dent. 1978, 40, 244–252. [Google Scholar] [CrossRef]
- Sterrett, J.D.; Oliver, T.; Robinson, F.; Fortson, W.; Knaak, B.; Russell, C.M. Width/length ratios of normal clinical crowns of the maxillary anterior dentition in man. J. Clin. Periodontol. 1999, 26, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Orozco-Varo, A.; Arroyo-Cruz, G.; Martínez-de-Fuentes, R.; Jiménez-Castellanos, E. Biometric analysis of the clinical crown and the width/length ratio in the maxillary anterior region. J. Prosthet. Dent. 2015, 113, 565–570.e2. [Google Scholar] [CrossRef] [PubMed]
- Álvarez-Álvarez, L.; Orozco-Varo, A.; Arroyo-Cruz, G.; Jiménez-Castellanos, E. Width/length ratio in maxillary anterior teeth. Comparative study of esthetic preferences among professionals and laypersons. J. Prosthodont. 2019, 28, 416–420. [Google Scholar] [CrossRef]
- Chieruzzi, M.; Rallini, M.; Pagano, S.; Eramo, S.; D’Errico, P.; Torre, L.; Kenny, J.K. Mechanical effect of static loading on endodontically treated teeth restored with fiber-reinforced posts. J. Biomed. Mater. Res. B Appl. Biomater. 2014, 102, 384–394. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).