Abstract
Low back pain (LBP) is the most frequent cause of adult disability. One of the main reasons can be a herniated disc (lumbar disc herniation—LDH), potentially disturbing spinal movement patterns. Its influence on gait and lumbopelvic biomechanics still remains unclear. Little to no evidence was found on lumbopelvic kinematics and gait in young LDH adults. The purpose of this study was to analyze the lumbopelvic biomechanics in young adult individuals with lumbar disc herniation diagnosed by MRI. Forty-three participants (18–35 years) were divided into two groups: an LDH group (n = 19) and a control group (n = 24). All participants underwent dynamic lumbopelvic and gait measures by a G-Walk wearable device in a 6-m walking test (6MWT). The Oswestry Disability Index (ODI) questionnaire was used for subjective disability assessment. The LDH group showed higher speed (p = 0.02), lower symmetry of pelvis tilt (p = 0.01), and lower pelvis rotation (p = 0.04) compared to the healthy controls. Correlation calculations showed significance between pelvis obliquity and pelvis rotation (r = 0.53) but only in healthy controls. The lumbopelvic biomechanics shows differences in pelvis tilt and symmetry index of rotation parameters between LDH and healthy controls. In conclusion, LDH affects the gait kinematics, causing three-dimensional disorders and lack of synergy. This is probably due to pain avoidance behaviors and the compensation mechanisms of the adjacent body region.
1. Introduction
Low back pain (LBP) is the most frequent cause of adult disability, with 90% of cases considered nonspecific low back pain (nLBP) due to an unclear pathological background [1]. LBP has been present in over 70% of adults in their lives at least once [2]. Its prevalence is increasing in young adults, causing the risk of earlier degeneration and, as a result, more frequent surgical treatment in a mature society. However, nLBP is not a specific enough term; therefore, a determined pathological model should always be a point in the actual research [3]. The pathological background of LBP can be multifactorial. One of the main reasons can be the herniated disc (lumbar disc herniation—LDH). Its symptoms may vary from slight, local to severe referred pain affecting the lower extremities. While the intervertebral disc’s biomechanics have been widely investigated, their influent on patient outcomes regarding the progression of migrated prolapse remains unclear. Moreover, our previous studies confirmed that young adults’ outcomes may vary with different stages of the disease [4,5,6].
LBP affects everyday activities and musculoskeletal functioning. It has an effect on pelvis biomechanics resulting in gait and daily living activity disorders [7,8,9,10,11,12]. LBP leads to three-dimensional changes: trunk rotation, changes in pelvis-thorax coordination in the transverse plane, and disturbed gait cycle coordination in the frontal plane, especially during level walking [11,12]. As a result, gait asymmetry can be present within all the above measures. Winiarski et al. revealed that most asymmetries can be usually observable in the region of the body different from the most hypermobile region [13]. As the segmental hypermobility can be the primary background of LDH, its biomechanics might be changed, and dynamic assessment in those cases is needed. People with LBP have a temporarily reduced range of motion (ROM) and poorer proprioception with an overall movement downturn compared to people without LBP [10]. Moreover, differences in lumbar lordosis angle and pelvic tilt angle in standing are usually found to be correlated in LBP individuals [14]. Regarding clinical evaluation, a poor correlation is yet being found between radiology imaging and clinical outcome when considering disc pathology. Due to this, physical examination seems to be an essential part. This might also be useful in finding potential predictors when analyzing spinal canal width and disc pathomechanics for planning treatment [15]. However, it still remains unclear whether and how much the herniated disc could affect the gait phases and components, as well as activities of daily living.
While patient-reported outcome measures (PROMs) such as the Oswestry Disability Index (ODI) or the Roland–Morris Disability Index (RMDI) correlate well with self-reported symptoms, these are mostly not standardized for age or sex [16]; that is why one of the main physical examination components is observation of the lumbopelvic movement and body posture. Considering the lumbopelvic region function, timed up and go (TUG) and distance walk tests are commonly applied and were proposed in this study [17,18,19,20]. These tests mirror global function in a specific way with significantly less dependence on gender bias, body mass index (BMI), and age than PROMs [21]. As for the 6-m walk test (6MWT), none of the previous studies in the literature have investigated lumbopelvic biomechanics in young patients with LDH. Gait symmetry was defined as a consistent activity of the lower limbs being stabilized with the upper part of the body. Gait asymmetry reflects a natural functional difference between the limbs and appears to be related to the contribution of each limb to control tasks and propulsion [22]. The purpose of this study was to analyze the lumbopelvic biomechanics in young adult individuals with lumbar disc herniation based on MRI. We hypothesized that there might be an asymmetric lumbopelvic pattern correlated with the degenerated disc observed in gait and activities of daily living.
2. Materials and Methods
2.1. Participant Selection
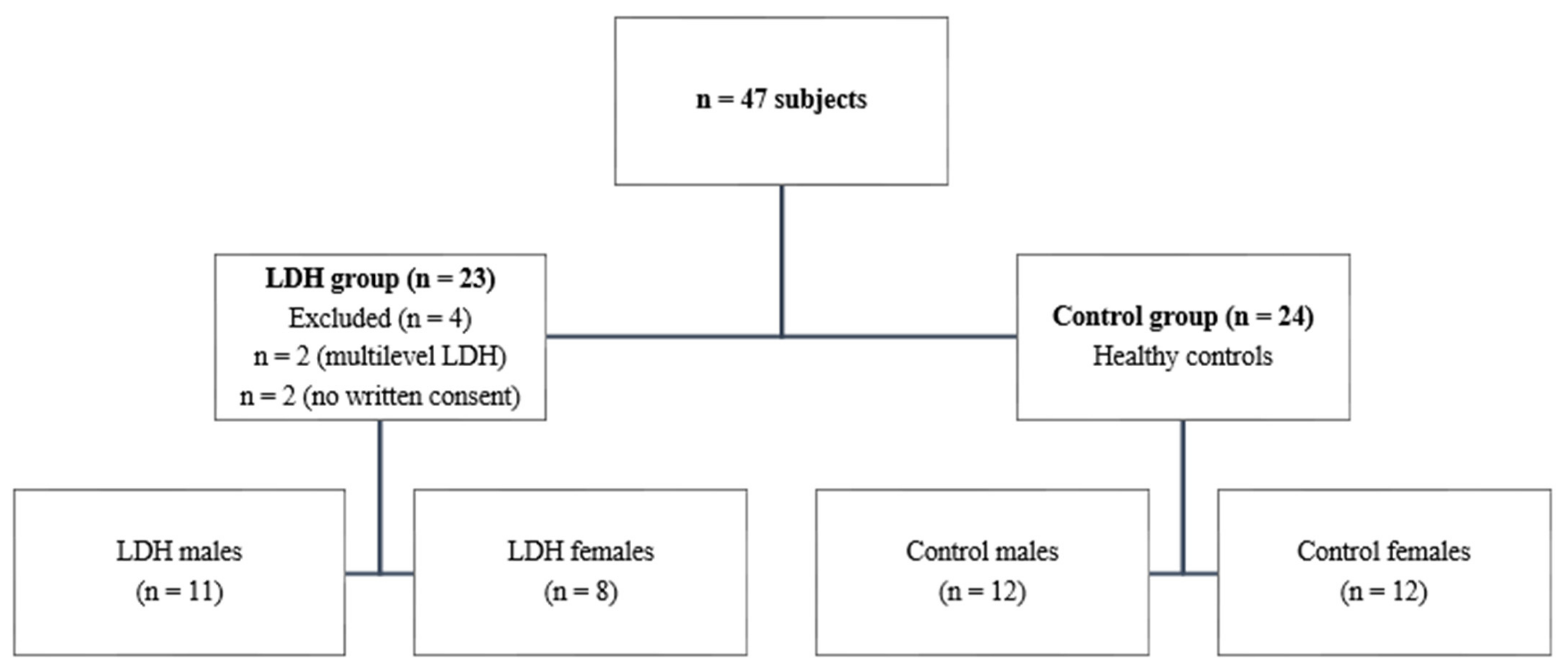
People (n = 47) seeking treatment for their LDH were recruited from the private physiotherapy clinic and the university in the period between June and August 2020. The study was registered before the enrollment (NCT04417855) number was obtained. Before the initiation of the study, each subject was informed regarding the study form and their right to refuse to participate or to withdraw at any time. All participants provided their informed consent prior to enrolment in the study, and the study procedures were approved by the Ethics Committee of the University School of Physical Education (Wroclaw, Poland) (14/2020). Several inclusion criteria were set including being aged between 18 and 35 years; reported pain of at least 2/10 on the Numeric Rating Scale (NPRS), which resulted in subjective disability within daily living activities; single-segment lumbar herniated disc confirmed by magnetic resonance imaging (MRI); and no acute stage of the pathology. Exclusion criteria were serious spinal pathology (i.e., metastatic disease, fracture), severe spinal deformity, spinal surgery history, pregnancy, or other disorders that would affect the outcome. The control group was formed of 24 healthy, asymptomatic individuals within the same exclusion criteria (Figure 1). Participant demographics are presented in Table 1.
Figure 1.
Flow diagram of the study, illustrating derivation of the sample size. LDH—lumbar disc herniation.

Table 1.
Participant demographics.
2.2. Procedure
All participants underwent dynamic lumbopelvic and gait measures with G-Walk (GW) by BTS Engineering. GW is a wearable device equipped with a 3-axis 16-bit accelerometer, gyro, and magnetometer in wireless Bluetooth communication with a G-Studio Software running on a PC measuring temporospatial gait analysis. The device was positioned on the fifth lumbar (L5) level during 6-m walking test (6MWT). The test was performed three times in a row, and the mean value of these was used. Every patient was tested in the same room on a flat surface with a standardized chair and margin line position. As for the 6MWT test, a 6-m margin was set. The outcome measures were performed on patients during normal gait without any walking aids. Recent literature proved the G-Sensor to be suitable for the assessment of physical activity [23,24]. This study evaluated the following spatiotemporal gait parameters: symmetry index (%), walking cadence (steps/min), walking speed (m/s); three-dimensional pelvic symmetry: pelvic tilt index (%), pelvic obliquity index (%), pelvic rotation index (%). Normal values according to the guidelines of the manufacturer, BTS Bioengineering, were given in Table 2. The BTS G-Walk device is based on works based on the correlation coefficient between the mean left and right normalized anteroposterior acceleration signal [25].

Table 2.
Mean, standard deviation (SD), and medians of gait kinematics within and between the groups (t-test and Mann–Whitney test) and normative values for preferred speed.
2.3. Assessment of Function
The ODI questionnaire was used to assess the subjective level of disability. It contains 10 sections related to daily activities, scored 0–5 points each. The overall score is interpreted as the following: from minimal disability (0–20%) to crippled/bed-bound (80–100%) [26]. This questionnaire was used in the Polish language version.
2.4. Statistical Analysis
All statistical calculations were performed using Statistica 12.5 software, developed by StatSoft. Power analysis (0.8) and sample size determination were performed before the study. With the assumption of a clinically significant effect size of a 10% asymmetry index in gait kinematics [13], the sample size of 20 participants was found to be sufficiently acceptable to provide a study design at p < 0.05. The Shapiro–Wilk test was used for the calculation of normality. Descriptive statistics, mean and standard deviations, and medians were presented for the groups. Cohen’s d statistics were calculated [27]. The parametric t-test was used to calculate the differences between the LDH group and the control group in walking cadence and speed, and the nonparametric Mann–Whitney U test for the kinematic variables. Spearman’s Rho analysis was used to determine the correlation between the variables.
3. Results
The Shapiro–Wilk test revealed the normal distribution of the results of both groups in speed (W = 0.92–0.96, p = 0.14–0.17) and cadence (W = 0.93–0.96, p = 0.21–32) only. There were no significant differences in kinematic parameters of gait between males and females in both groups (p > 0.05). Patients in the LDH group were significantly older than in the control group (p < 0.0001). There were no differences in body mass, height, or BMI index between the groups (p > 0.05) (Table 1).
There were only three differences between the control and LDH group. The LDH group presented a significantly higher speed of gait than the control group (p = 0.02; d = 0.75), but cadence was the same in both groups (p > 0.05). The symmetry index of pelvis tilt was significantly lower in LDH patients than in the control group (p = 0.01; d = 0.769). The symmetry index of rotation was significantly lower in LDH patients than in the control group (p = 0.04; d = 0.02) (Table 2).
There were no differences between the groups in the symmetry index of pelvis obliquity and symmetry index of gait (p > 0.05). There were no differences between groups in stride stance or swing duration in the left and right side (p > 0.05). There were also no differences between groups in double and single support in the left and right side (p > 0.05) (Table 2). The suggested normative values for spatiotemporal parameters are included in Table 2 [28].
There was a significant correlation between pelvis obliquity and pelvis rotation symmetry index only in the control group. There were no correlations between ODI and the symmetry indexes of the pelvis in the LDH group (Table 3).

Table 3.
Spearman’s rho correlation between the measured parameters in both groups.
4. Discussion
While LBP affects the majority of adults in society, with its common symptoms causing functional disability, its clinical background still remains an object of interest for many researchers. Gait stands among the main daily living activities and throughout significant pain and other neurophysiological impairments caused by LBP, it can be challenging for people regardless of their age [29]. In our study, we compared lumbopelvic biomechanics in LDH people and healthy individuals in the control group in basic everyday living tasks using the 6MWT and TUG tests.
Similar to other researchers, we confirmed the differences in lower back region dynamic parameters [30,31]. Our findings focus mainly on three variables that were significantly different between the groups. LDH patients completed the procedure with higher speed than the controls, while the cadence was similar and not statistically significant. This mechanism is present probably due to poorer body control of the lower back region and to larger pelvis rotation than healthy controls, which makes gait also non-ergonomic. This was also confirmed by Dieen et al. [32]. Madadi-Shad et al. also found it to be similar; however, no females were recruited to the experiment, and the LBP term was not precisely specified [31]. The opposite result, decreased spatiotemporal gait parameters, was obtained by Bonab et al. in their study within LDH group; however, the difference could be related to the age of the research group (25–65) which should be taken into account and improved in further research [33].
Our study also revealed that a herniated lumbar disc significantly affects the pelvis tilt parameter. Lower scores obtained by the LDH individuals showed worse lumbopelvic region control in the sagittal plane during walking and the need for more compensation mechanisms in other body regions, what could increase the walking speed variable. Similar observations were recorded by Huang et al.; moreover, they experienced more compensation in the extremities and thoracic region of the spine [34]. The compensation phenomenon was also described by Winiarski et al. [13,35]. Recently, Rum et al. evaluated the correlation of LBP with gait kinematics and showed that LBP causes wider and more variable trunk motion, which is similar to our observation [36]. Furthermore, Gombatto et al. observed differences in lumbar subregion motion in people with LBP [37]. They showed that there can be less upper lumbar motion than in healthy controls. This confirms that the adjacent regions’ compensation can also be related to increased back muscle activity in the majority of individuals with LBP [1]. Restriction of lumbar region motion in daily living activities was also confirmed by Kuai et al. [11]. They also point to the correlation of restriction with the pelvis kinematics.
Another variable related to the previous two is the symmetry index of rotation which has given a lower score in people with LDH. The correlation calculations were found to be statistically significant between pelvis rotation and obliquity, but only in healthy controls. The LDH people did not show this kind of synergy in the lumbopelvic region. These proved that their pelvis kinematics are less efficient due to poor proprioception and probably pain-avoiding mechanisms. That background was confirmed in a different study where we observed that chronic pain intensity played an important role in decreasing ground reaction peak force and increasing time to peak in the sit-to-stand task in LBP patients [38]. This study suggested three main directions for rehabilitation programs: pain reduction, postural improvement, and the coordination of the sit-to-stand strategy. Gait disturbances of kinematic pelvis asymmetry in the LDH group appear to be one more clinical problem to resolve in transfer ability.
Our study did not reveal differences in other lumbopelvic parameters in LDH people and healthy controls. This might be due to the young age (18–35) and/or the subacute chronic stage of the disease. Although we did not find differences in other analyzed parameters, the LDH needs further research on gait and lumbopelvic biomechanics.
Limitations and Future Directions
The patient’s age and the exact duration of the disability could be important factors in the chronification process that might affect the kinematic lumbopelvic pattern observed in gait LDH patients. We did not obtain the information about the exact duration of the disability. Due to the loss of proprioception, it could be a substantial factor in further analysis. The observational group (LDH) size needs to be expanded to show more statistical differences between the parameters. The LDH topic lacks the literature necessary to answer many questions, such as if the direction of migrated disc material could be important in understanding gait biomechanics and the influence of daily living activities, taking into account its pathological factors. While the correlation of radiological imaging and patients’ clinical outcome remains challenging due to many factors, expanded clinical examination is needed. In addition, no follow-up in gait reeducation was included in our study and should be improved in further research.
5. Conclusions
An important conclusion that can be drawn from this paper is that the lumbopelvic biomechanics show differences in pelvis tilt and the symmetry index of rotation parameters between LDH and healthy controls. In conclusion, LDH affects the gait kinematics causing three-dimensional disorders and lack of synergy. This is probably due to pain avoidance behaviors and the compensation mechanisms of the adjacent body region. No differences were found in other parameters, and further research is needed.
Author Contributions
Conceptualization, T.K. and T.S.; methodology, T.K and T.S.; software, T.K.; validation, T.S.; formal analysis, T.K.; investigation, T.K.; resources, T.K.; data curation, T.S.; writing—original draft preparation, T.K. and T.S.; writing—review and editing, T.K. and T.S.; visualization, T.K.; supervision, T.S.; project administration, T.K. All authors have read and agreed to the published version of the manuscript.
Funding
No funding has contributed to this conception of this manuscript.
Data Availability Statement
The data presented in this study are available on request from corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lima, M.; Ferreira, A.S.; Reis, F.J.J.; Paes, V.; Meziat-Filho, N. Chronic low back pain and back muscle activity during functional tasks. Gait Posture 2018, 61, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Kuai, S.; Liao, Z.; Zhou, W.; Guan, X.; Ji, R.; Zhang, R.; Guo, D.; Liu, W. The Effect of Lumbar Disc Herniation on Musculoskeletal Loadings in the Spinal Region During Level Walking and Stair Climbing. Med. Sci. Monit. 2017, 23, 3869–3877. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.-Y.; Choi, J.-D.; Kim, S.-Y.; Oh, D.-W.; Kim, J.-K.; Park, J.-W. Comparison between muscle activation measured by electromyography and muscle thickness measured using ultrasonography for effective muscle assessment. J. Electromyogr. Kinesiol. 2014, 24, 614–620. [Google Scholar] [CrossRef] [PubMed]
- Kuligowski, T.; Dębiec-Bąk, A.; Skrzek, A. Effectiveness of traction in young patients representing different stages of degenerative disc disease. Ortop. Traumatol. Rehabil. 2019, 21, 187–195. [Google Scholar] [CrossRef]
- Kuligowski, T.; Dȩbiec-Ba̧k, A.; Skrzek, A. Mobilisation efficacy in young patients with different stages of degenerative disc disease. J. Back Musculoskelet. Rehabil. 2020, 33, 913–918. [Google Scholar] [CrossRef]
- Kuligowski, T.; Cieślik, B.; Nowicka, Z. Functional outcomes in relation with the progression level in young degenerative disc disease patients. Fizjoterapia 2017, 24, 9–12. [Google Scholar] [CrossRef]
- Yazdani, S.; Dizji, E.; Alizadeh, F.; Hassanlouei, H. Effect of chronic idiopathic low back pain on the kinetic gait characteristics in different foot masks. J. Biomech. 2018, 79, 243–247. [Google Scholar] [CrossRef]
- Koch, C.; Hänsel, F. Chronic non-specific low back pain and motor control during gait. Front. Psychol. 2018, 9, 2236. [Google Scholar] [CrossRef]
- Bagheri, R.; Parhampour, B.; Pourahmadi, M.; Fazeli, S.H.; Takamjani, I.E.; Akbari, M.; Dadgoo, M. The effect of core stabilization exercises on trunk–pelvis three-dimensional kinematics during gait in non-specific chronic low back pain. Spine 2019, 44, 927–936. [Google Scholar] [CrossRef]
- Laird, R.A.; Gilbert, J.; Kent, P.; Keating, J.L. Comparing lumbo-pelvic kinematics in people with and without back pain: A systematic review and meta-analysis. BMC Musculoskelet. Disord. 2014, 15, 229. [Google Scholar] [CrossRef]
- Kuai, S.; Zhou, W.; Liao, Z.; Ji, R.; Guo, D.; Zhang, R.; Liu, W. Influences of lumbar disc herniation on the kinematics in multi-segmental spine, pelvis, and lower extremities during five activities of daily living. BMC Musculoskelet. Disord. 2017, 18, 216. [Google Scholar] [CrossRef]
- Kuai, S.; Guan, X.; Liu, W.; Ji, R.; Xiong, J.; Wang, D.; Zhou, W. Prediction of the spinal musculoskeletal loadings during level walking and stair climbing after two types of simulated interventions in patients with lumbar disc herniation. J. Health Eng. 2019, 2019, 6406813. [Google Scholar] [CrossRef]
- Winiarski, S.; Rutkowska-Kucharska, A.; Pozowski, A.; Aleksandrowicz, K. A new method of evaluating the symmetry of movement used to assess the gait of patients after unilateral total hip replacement. Appl. Bionics Biomech. 2019, 2019, 7863674. [Google Scholar] [CrossRef]
- Misir, A.; Kizkapan, T.B.; Tas, S.K.; Yildiz, K.I.; Ozcamdalli, M.; Yetis, M. Lumbar spine posture and spinopelvic parameters change in various standing and sitting postures. Eur. Spine J. 2019, 28, 1072–1081. [Google Scholar] [CrossRef]
- Corniola, M.-V.; Stienen, M.N.; Joswig, H.; Smoll, N.R.; Schaller, K.; Hildebrandt, G.; Gautschi, O.P. Correlation of pain, functional impairment, and health-related quality of life with radiological grading scales of lumbar degenerative disc disease. Acta Neurochir. 2016, 158, 499–505. [Google Scholar] [CrossRef]
- Joswig, H.; Stienen, M.N.; Smoll, N.R.; Corniola, M.V.; Chau, I.; Schaller, K.; Hildebrandt, G.; Gautschi, O.P. Patients’ preference of the timed up and go test or patient-reported outcome measures before and after surgery for lumbar degenerative disk disease. World Neurosurg. 2017, 99, 26–30. [Google Scholar] [CrossRef]
- Bennell, K.L.; Dobson, F.; Hinman, R.S. Measures of physical performance assessments: Self-Paced Walk Test (SPWT), Stair Climb Test (SCT), Six-Minute Walk Test (6MWT), Chair Stand Test (CST), Timed Up & Go (TUG), Sock Test, Lift and Carry Test (LCT), and Car Task. Arthritis Care Res. 2011, 63, S350–S370. [Google Scholar] [CrossRef]
- Bohannon, R.W. Reference values for the timed up and go test: A descriptive meta-analysis. J. Geriatr. Phys. Ther. 2006, 29, 64–68. [Google Scholar] [CrossRef]
- Christopher, A.; Kraft, E.; Olenick, H.; Kiesling, R.; Doty, A. The reliability and validity of the timed up and go as a clinical tool in individuals with and without disabilities across a lifespan: A systematic review. Disabil. Rehabil. 2019, 1–15. [Google Scholar] [CrossRef]
- D’Addio, G.; Donisi, L.; Pagano, G.; Improta, G.; Biancardi, A.; Cesarelli, M. Agreement between opal and G-walk wearable inertial systems in gait analysis on normal and pathological subjects. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBS, Berlin, Germany, 23–27 July 2019; pp. 3286–3289. [Google Scholar]
- Gautschi, O.P.; Smoll, N.R.; Joswig, H.; Corniola, M.V.; Schaller, K.; Hildebrandt, G.; Stienen, M.N. Influence of age on pain intensity, functional impairment and health-related quality of life before and after surgery for lumbar degenerative disc disease. Clin. Neurol. Neurosurg. 2016, 150, 33–39. [Google Scholar] [CrossRef]
- Sadeghi, H.; Allard, P.; Prince, F.; Labelle, H. Symmetry and limb dominance in able-bodied gait: A review. Gait Posture 2000, 12, 34–45. [Google Scholar] [CrossRef]
- Del Din, S.; Godfrey, A.; Rochester, L. Validation of an accelerometer to quantify a comprehensive battery of gait characteristics in healthy older adults and Parkinson’s disease: Toward clinical and at home use. IEEE J. Biomed. Health Inform. 2015, 20, 838–847. [Google Scholar] [CrossRef] [PubMed]
- Sankar Pandi, S.K.; Baldwin, A.J.; Ray, J.; Mazzà, C. Reliability of inertial sensors in the assessment of patients with vestibular disorders: A feasibility study. BMC Ear Nose Throat Disord. 2017, 17. [Google Scholar] [CrossRef]
- Latajka, A.; Woźniewski, M.; Malicka, I. Influence of surgical treatment of selected malignant tumours on gait kinematics—A pilot study. Physiother. Q. 2018, 26, 33–39. [Google Scholar] [CrossRef]
- Fairbank, J.C.T.; Pynsent, P.B. The oswestry disability index. Spine 2000, 25, 2940–2953. [Google Scholar] [CrossRef]
- Ellis, P.D. The Essential Guide to Effect Sizes; Cambridge University Press: Cambridge, UK, 2010. [Google Scholar]
- Pietraszewski, B.; Winiarski, S.; Jaroszczuk, S. Three-dimensional human gait pattern—reference data for normal men. Acta Bioeng. Biomech. 2012, 14, 9–16. [Google Scholar]
- Clark, D.J. Automaticity of walking: Functional significance, mechanisms, measurement and rehabilitation strategies. Front. Hum. Neurosci. 2015, 9, 246. [Google Scholar] [CrossRef]
- Cimolin, V.; Vismara, L.; Galli, M.; Zaina, F.; Negrini, S.; Capodaglio, P. Effects of obesity and chronic low back pain on gait. J. Neuroeng. Rehabil. 2011, 8, 55. [Google Scholar] [CrossRef]
- Madadi-Shad, M.; Jafarnezhadgero, A.A.; Sheikhalizade, H.; Dionisio, V.C. Effect of a corrective exercise program on gait kinetics and muscle activities in older adults with both low back pain and pronated feet: A double-blind, randomized controlled trial. Gait Posture 2020, 76, 339–345. [Google Scholar] [CrossRef]
- Van Dieën, J.H.; Prins, M.R.; Bruijn, S.M.; Wu, W.H.; Liang, B.; Lamoth, C.J.; Meijer, O.G. Coordination of axial trunk rotations during gait in low back pain. A narrative review. J. Hum. Kinet 2021, 76, 35–50. [Google Scholar]
- Bonab, M.A.R.; Colak, T.K.; Toktas, Z.O.; Konya, D. Assessment of spatiotemporal gait parameters in patients with lumbar disc herniation and patients with chronic mechanical low back pain. Turk. Neurosurg. 2020, 30, 277–284. [Google Scholar] [CrossRef]
- Huang, Y.P.; Bruijn, S.M.; Lin, J.H.; Meijer, O.G.; Wu, W.H.; Abbasi-Bafghi, H.; Lin, X.C.; Van Dieën, J.H. Gait adaptations in low back pain patients with lumbar disc herniation: Trunk coordination and arm swing. Eur. Spine J. 2011, 20, 491–499. [Google Scholar] [CrossRef]
- Winiarski, S.; Pietraszewska, J.; Pietraszewski, B. Three-dimensional human gait pattern: Reference data for young, active women walking with low, preferred, and high speeds. BioMed Res. Int. 2019, 2019, 9232430. [Google Scholar] [CrossRef]
- Rum, L.; Brasiliano, P.; Vannozzi, G.; Laudani, L.; Macaluso, A. Non-specific chronic low back pain elicits kinematic and neuromuscular changes in walking and gait termination. Gait Posture 2021, 84, 238–244. [Google Scholar] [CrossRef]
- Gombatto, S.P.; Brock, T.; DeLork, A.; Jones, G.; Madden, E.; Rinere, C. Lumbar spine kinematics during walking in people with and people without low back pain. Gait Posture 2015, 42, 539–544. [Google Scholar] [CrossRef]
- Sipko, T.; Glibowski, E.; Barczyk-Pawelec, K.; Kuczyński, M. The effect of chronic pain intensity on sit-to-stand strategy in patients with herniated lumbar disks. J. Manip. Physiol. Ther. 2016, 39, 169–175. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).