For a mathematical programming model with multi-objectives, a general purpose model with a wide range of applications is shown below:
where
x represents decision variables that are vectors, and a vector with
k objective functions forms
. Finally, for constraints,
G(
x) denotes inequalities, and
H(
x) denotes equality.
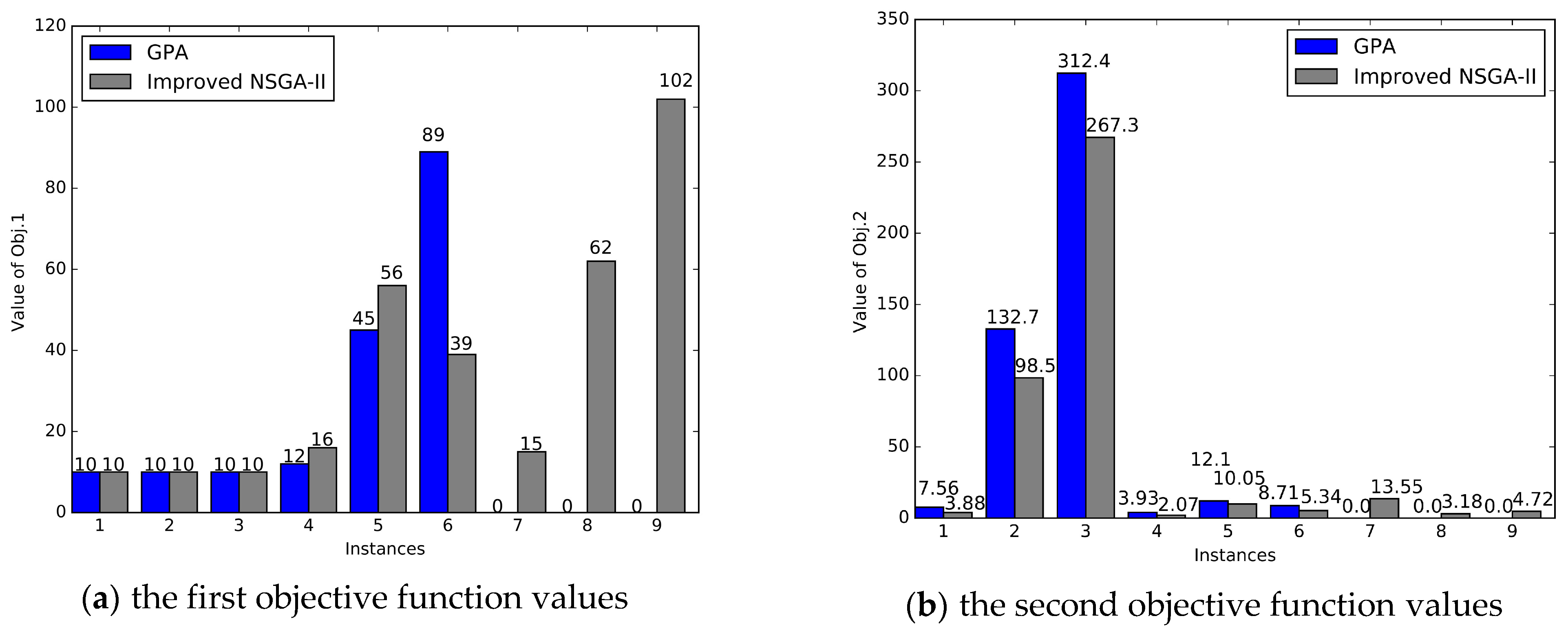
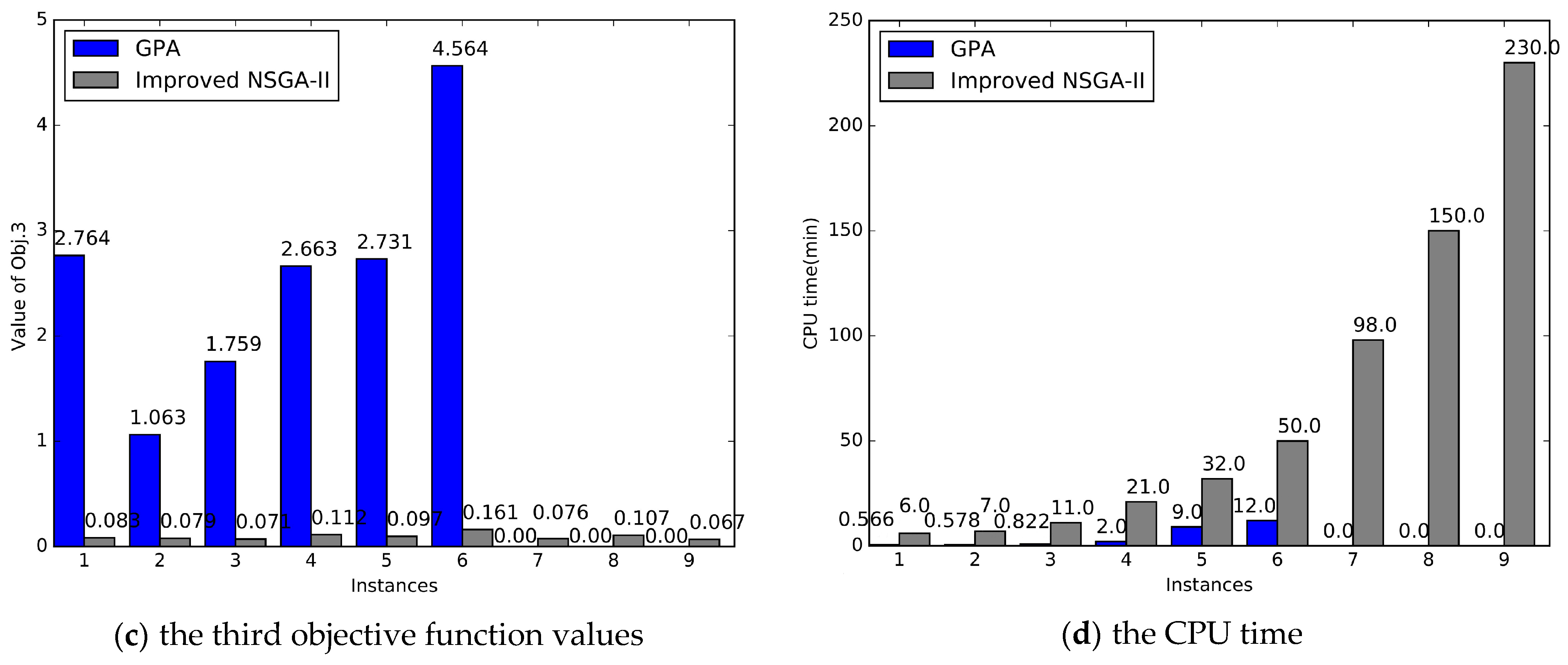
The solutions for multi-objective models are very broad. We conduct two approaches here to solve the models: the Goal Programming Approach (GPA) with ILOG CPLEX and the improved Non-dominated Sorting Genetic Algorithm II (NSGA-II) with MATLAB.
3.1. Goal Programming Approach (GPA)
When using the GPA to solve a multi-objective model, we must optimize the high-priority objectives first and then optimize the low-priority objectives. Thus, the Analytic Hierarchy Process (AHP) is proposed to determine the priority of the objectives.
3.1.1. Determining the Priority of the Objectives via AHP
AHP is a decision approach that decomposes decision-making elements into goals, criteria, and programs. On this basis, qualitative and quantitative analysis methods are used. The implementation of AHP is mainly divided into three steps: (1) build a hierarchical model, (2) construct a judgment matrix and calculate the weights of the four objectives, and (3) test the consistency of the judgment matrix.
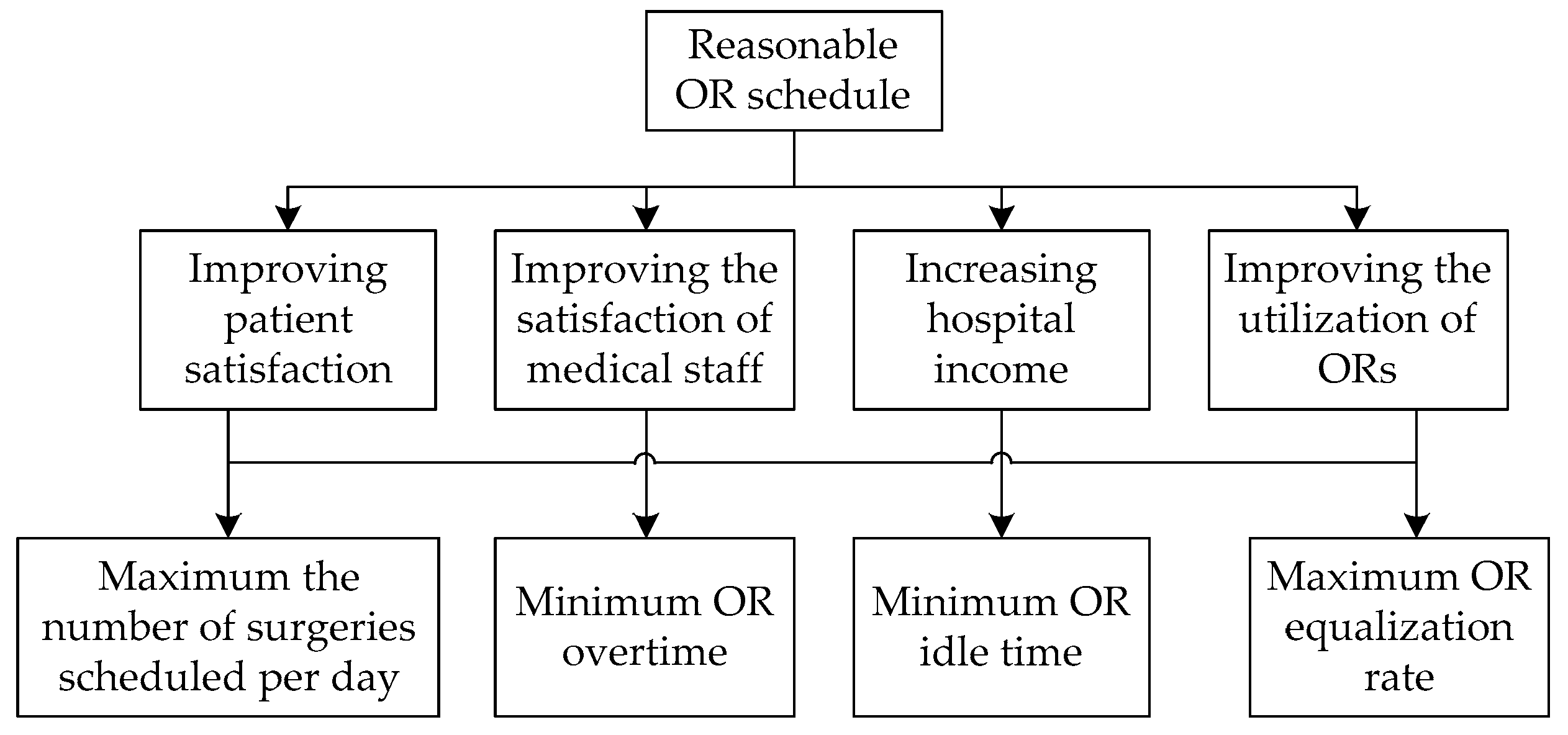
First, by dividing the decision objectives, the factors considered, and the decision objects into the objective layer, the standard layer, and the decision layer according to the mutual relationship between them, the hierarchical structure diagram is drawn (
Figure 1). In this section, minimizing overtime and idle time should be considered separately, and the three objectives can be divided into four.
Second, the most important step is to construct a comparison judgment matrix by pairwise comparison to obtain the priority of each objective. We need to make a pairwise comparison between the elements of each layer to construct a comparison judgment matrix. For one element, we get the pairwise comparison judgment matrix
, where
aij represents the relative importance scale between the two indicators. The relative importance scales are mainly based on 1 to 9 and their reciprocals as a scale to reflect their importance. The method of scaling is shown in
Table 3.
In our paper, according to the scores of the doctors and nurses in the hospital SMC, the importance of the comparison between the indicators is made, and then the comparison matrix of the layers is compared according to the 1–9 matrix. The final judgment matrix comparing the decision-making layers is shown in
Table 4: That is, the pairwise comparison of the two pairs is performed in the 4 x 4 judgment matrix. First, the values in the judgment matrix are multiplied by rows, and then the values obtained in the first step are raised to the fourth power. Next, these values are normalized: That is, the relative importance
ωi of these four indicators is obtained.
Last, a consistency check of the judgment matrix is required when the relative importance is obtained. The indicators for checking the consistency are C.I. = (λ − n)/(n − 1), where λ is the largest eigenvalue. For all , there is , and n is the matrix dimension. This stipulates that when C.I. = 0, there is complete consistency, and when C.I. is close to 0, there is satisfactory consistency. The larger the C.I., the more serious the inconsistency is. From above, it can be concluded that C.I. = 0.0045 is close to 0, so it can be said that the consistency of the judgment matrix is acceptable.
Therefore, the priority of the objectives can be obtained, that is, the maximum number of surgeries scheduled per day, minimum OR overtime, minimum OR idle time, and maximum OR equalization rate. The priority is P1 > P2 > P3 > P4.
3.1.2. Transforming Models via GPA
The main idea of the GPA is to treat the objective functions and constraints all as constraints and then divide the constraints into two categories. One is treated with strict equality or inequality constraints that should be satisfied, and the other is called a flexible constraint that can be satisfied without strict requirements. For models in Phase 2, Equations (10–15) are the first one. Besides, four objectives can be viewed as four flexible constraints. For flexible constraints, we convert them into an equality constraint by setting a deviation variable.
A deviation variable represents the difference between the calculated value and the objective value, and , respectively: If , then and . That is, is the part of exceeding , so that is a positive deviation variable. If , then and . That is, is the part of that does not reach , so is called a negative deviation variable. If , then .
For practical problems, if the calculated value desires to exceed the objective value as much as possible, the negative deviation variable is minimized, , while on the contrary, the positive deviation variable is minimized, . If is as close as possible to , while minimizing positive and negative deviation variables, .
Consequently, the four flexible constraints are converted into the following expressions:
(1) Arranging as many surgeries as possible every day to make them exceed the number of surgeries “
Num”, as is possible,
(2) Guaranteeing there is no overtime in the ORs, as is possible,
(3) Guaranteeing there is no idle time in the ORs, as is possible,
(4) Making the total utilization time between the ORs as uniform as possible,
The corresponding objective function is as follows:
3.2. Improved Nondominated Sorting Genetic Algorithm II (NSGA-II)
For the general formulation of multi-objective mathematical programming in
Section 3, there are
n design variables. Combining the design variables, the collection of these combinations constitutes the search space. In the search space, if there is a region that satisfies all the constraints, then this region becomes a feasible domain, denoted by
X.
When using the Pareto optimization to process the multi-objective models, for each solution x∈X corresponding to the vector objective function , the trade-off is generally made in the k objective functions at the time of selection. If a multi-objective function has only two objective functions f1 and f2, we define the solution x1 to dominate x2 as follows: . If all solutions are not dominated by any other solutions in X, then this set constitutes the Pareto optimal front. However, in general, it can only be local Pareto optimality, and there is no guarantee that global Pareto optimality will be obtained. We use the following definitions to describe this more clearly:
Definition 1. For the vector objective function , there are two decision vector variables . means that dominates , if and only if , and , where and are the objective function values for the ith and jth objective;
Definition 2. For the vector objective function , if point is defined as globally Pareto optimal if and only if , does not exist. Where is globally efficient, this means that is efficient in the entire feasible space, and is called a globally efficient point. The image of the set of globally efficient points is called a Pareto front;
Definition 3. For the vector objective function , if point is defined as locally Pareto optimal if and only if there exists an open neighborhood of , and there is no when . is called locally efficient, which means that is efficient in the locally feasible space. The image of the set of locally efficient points () is called a local Pareto front.
When dealing with multi-objective programming models, heuristic algorithms are often used, and genetic algorithms are ones in which good solutions can be obtained. Among them, we chose the Non-dominated Sorting Genetic Algorithm II (NSGA-II) to deal with our models, which was proposed by Srinivas and Deb [
38] on the basis of a non-dominated sorting genetic algorithm (NSGA). The NSGA ([
39]) is a non-dominated algorithm used to solve multi-objective optimization, and its basic principle is mainly based on a genetic algorithm. The algorithm is efficient, but there are also some application deficiencies, such as its lack of elitism, its computational complexity, and the selection of optimal parameter values
for sharing parameters. In response to some of the shortcomings of the NSGA mentioned above, Reference [
38] developed an improved version of the NSGA, called the NSGA-II, which is a more expensive dominated sorting algorithm that improves the deficiencies of the NSGA and is now the most widely used. Simultaneously, it is one of the heuristic evolutionary algorithms that find Pareto optimal solutions for multi-objective programming models.
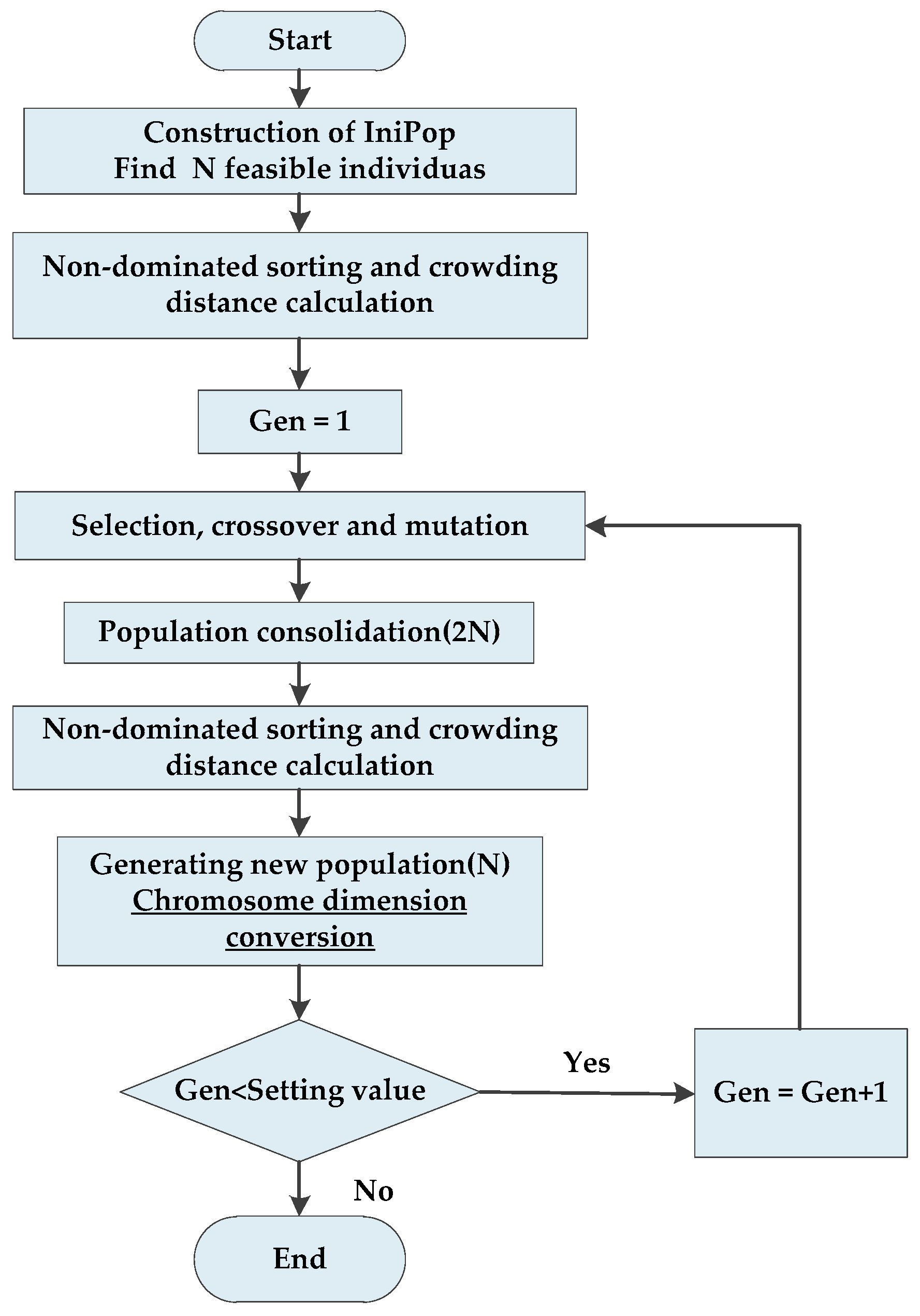
The NSGA-II is based on an elite principle, and it adopts an explicit diversity retention mechanism and emphasizes non-dominated solutions. Initial populations of size
N are generated randomly, and then a first-generation offspring population is obtained by the selection, crossover, and mutation of the genetic algorithm after non-dominant sequencing. Second, it is different from the first generation in following generations. It mainly combines the populations of the parent and the offspring, and after they are quickly non-dominated, it calculates the crowding degree of the individual in the non-dominant layer. The appropriate individuals are selected by non-dominant relationships and the results of individual crowding degrees to form a new population. At last, a new subpopulation is created by the basic operation of the genetic algorithm. Then these operations repeat until the conditions for program termination are satisfied. The specific implementation process of the NSGA-II is depicted in
Figure 2.
Before we started the formal experiment, we did some preliminary pre-experimental calculations. We found that when the generations of the iteration are too high, for example, 100,000, the NSGA-II usually cannot find a feasible solution because the dimension of the search space is too high. Moreover, for most evaluation functions, the decision variables are one-dimensional, but in our paper, is three-dimensional. Therefore, in order to improve the performance of the NSGA-II in finding a Pareto solution, we designed the following improved algorithm. The following is a detailed description of some of the key steps in the proposed algorithm.
3.2.1. Initial Population
In order to improve the quality of the Pareto solution and reduce the optimization time, we improved the initialization phase and defined a new initialization process, mainly by adding constraints to randomly generate the initial population
IniPop. More specifically, the constraints in (10–15) are imposed on the initialization function, so that the generated chromosomes are the feasible solutions that satisfy the proposed model constraints, thus forming the initial population of
N feasible solutions. The initial population generated affects the convergence of the algorithm: It is also better and more meaningful than the purely randomly generated population of the NSGA-II, and
IniPop is also a good seed for the solution of the next generation. On the basis of initialization, the population evolves until the defined number of generations. The pseudo code of the construction process of the initial population
IniPop is shown in
Table 5.
3.2.2. Non-Dominant Sorting and Crowding Distance Calculation
The initial population is sorted using a non-dominated sort. This process returns the sorting value and the crowding distance corresponding to each individual, which is a two-column matrix, and adds sorting values and crowding distances to the chromosome matrix. What is obtained at last is a population matrix that already contains rank and crowding distance and that has been sorted by sorting rank.
3.2.3. Selection, Crossover, and Mutation
The selection process uses a tournament selection approach, which randomly selects two individuals at a time and preferentially selects individuals with a high ranking. If the ranking is the same, it prefers to select individuals with a large crowding distance.
The crossover algorithm selects the simulated binary crossover (SBX). SBX mainly simulates the principle of a single-point crossover based on binary strings and applies it to chromosomes expressed in real numbers. The two parent chromosomes are cross-operated to produce two progeny chromosomes, so that the relevant pattern information of the parent chromosome is protected in the subchromosomes. The mutation uses a general polynomial mutation.
3.2.4. Generating New Populations (Elite Strategy)
The elite strategy keeps the good individuals in the parent directly within the offspring to prevent the obtained Pareto optimal solution from being lost. First, the parent population and the child population are synthesized into a population . Then, a new parent population from the population is generated according to the following rules:
(1) According to the order of Pareto rank from low to high, the whole layer population is put into the parent population until a layer of the individual cannot be put into the parent population ;
(2) The individuals of the layer are sorted according to the crowding distance from large to small and then placed in the parent population until the parent population fills up.
3.2.5. Evaluation Function Stage
Generally, a chromosome is one-dimensional, but in our paper, the decision variable is three-dimensional. Thus, we proposed a new conversion method after generating a new population (replace chromosome): When a new population is generated, we convert one-dimensional variables into three-dimensional variables using the corresponding rules of the design based on solid geometry properties. The one-dimensional vectors are divided into multidimensional cube vectors of in order to calculating fitness values.
Meanwhile, after the feasible chromosomes undergo crossover, mutation, and other processes, they may be not feasible. Thus, in order to get a completely feasible solution again, we judge if the obtained chromosomes are feasible in the evaluation function calculation stage. If they meet all the constraints, the evaluation objective values are calculated, and if not, they re-enter initialization.