Gardens of Historic Mental Health Hospitals and Their Potential Use for Green Therapy Purposes
Abstract
1. Introduction
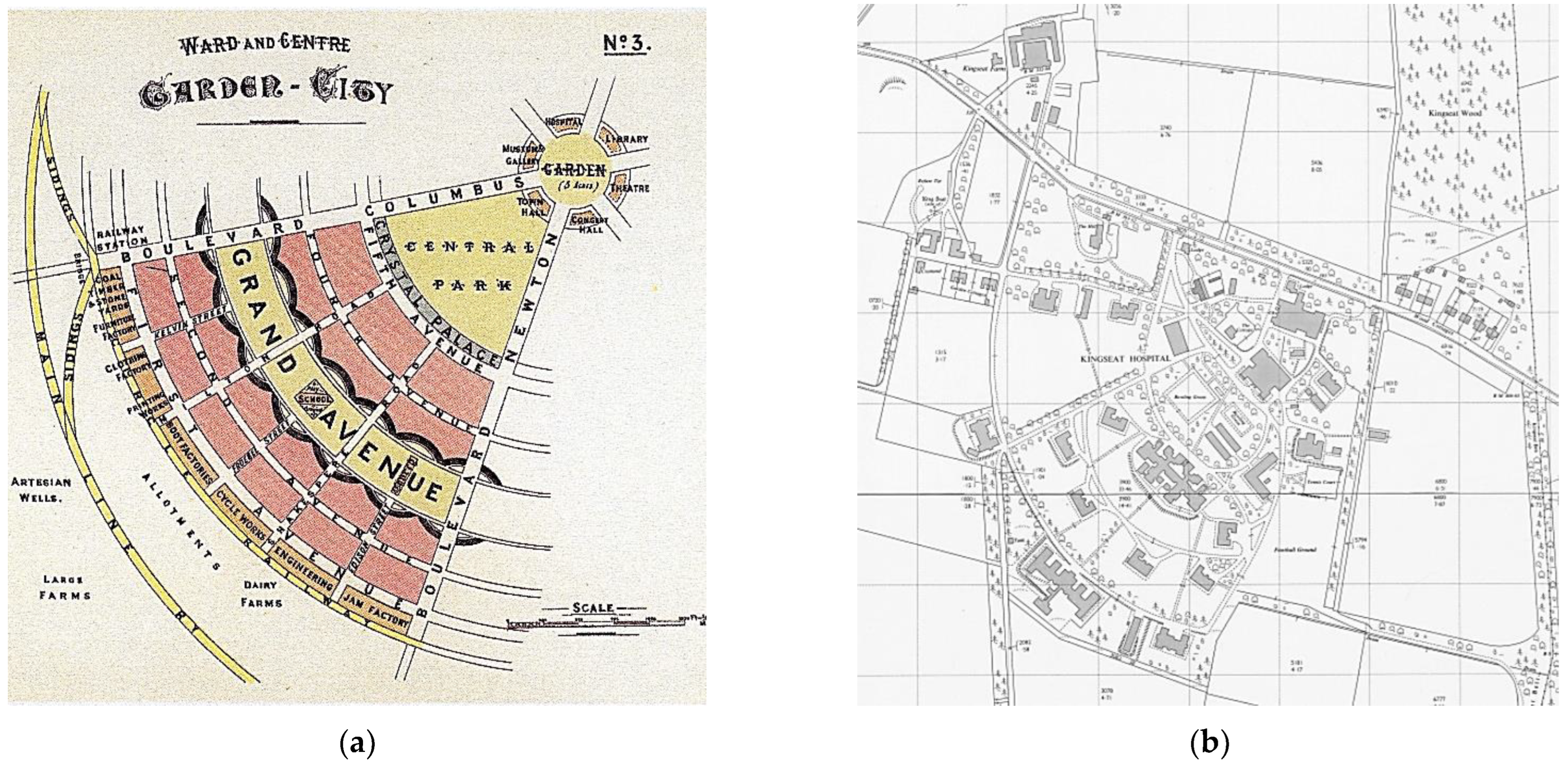
1.1. Historic Psychiatric Hospitals and Their Gardens—From Lunatic Asylum to Contemporary Mental Health Centres
1.2. Aim of the Study
2. Materials and Methods
Case Study Choice and Location
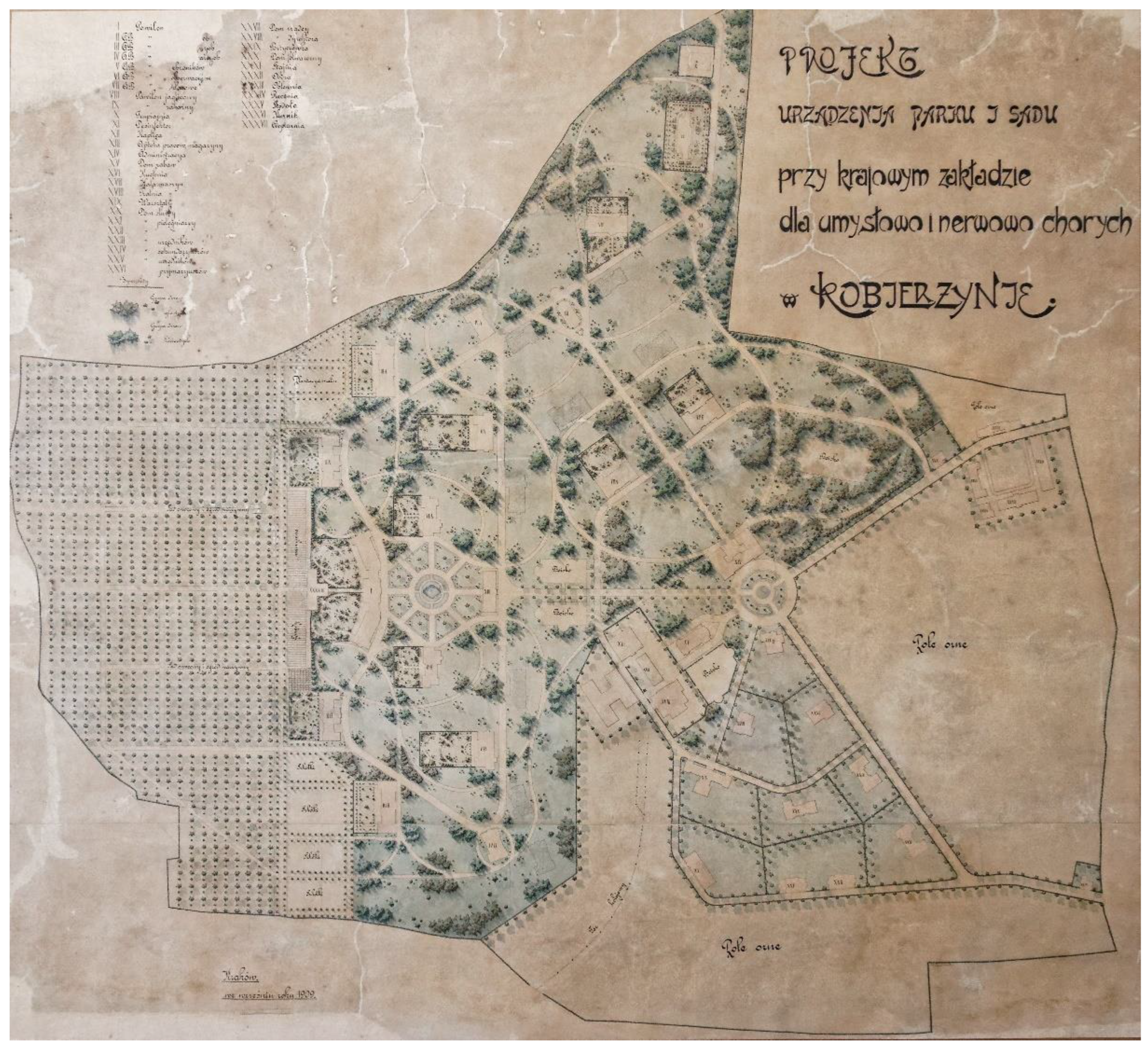
- The Babiński Specialized Hospital in the southern suburb of Kraków, former second National Institute for the Nervous and Mentally Ill, Kraków-Kobierzyn (Małopolska Voivodeship, Poland);
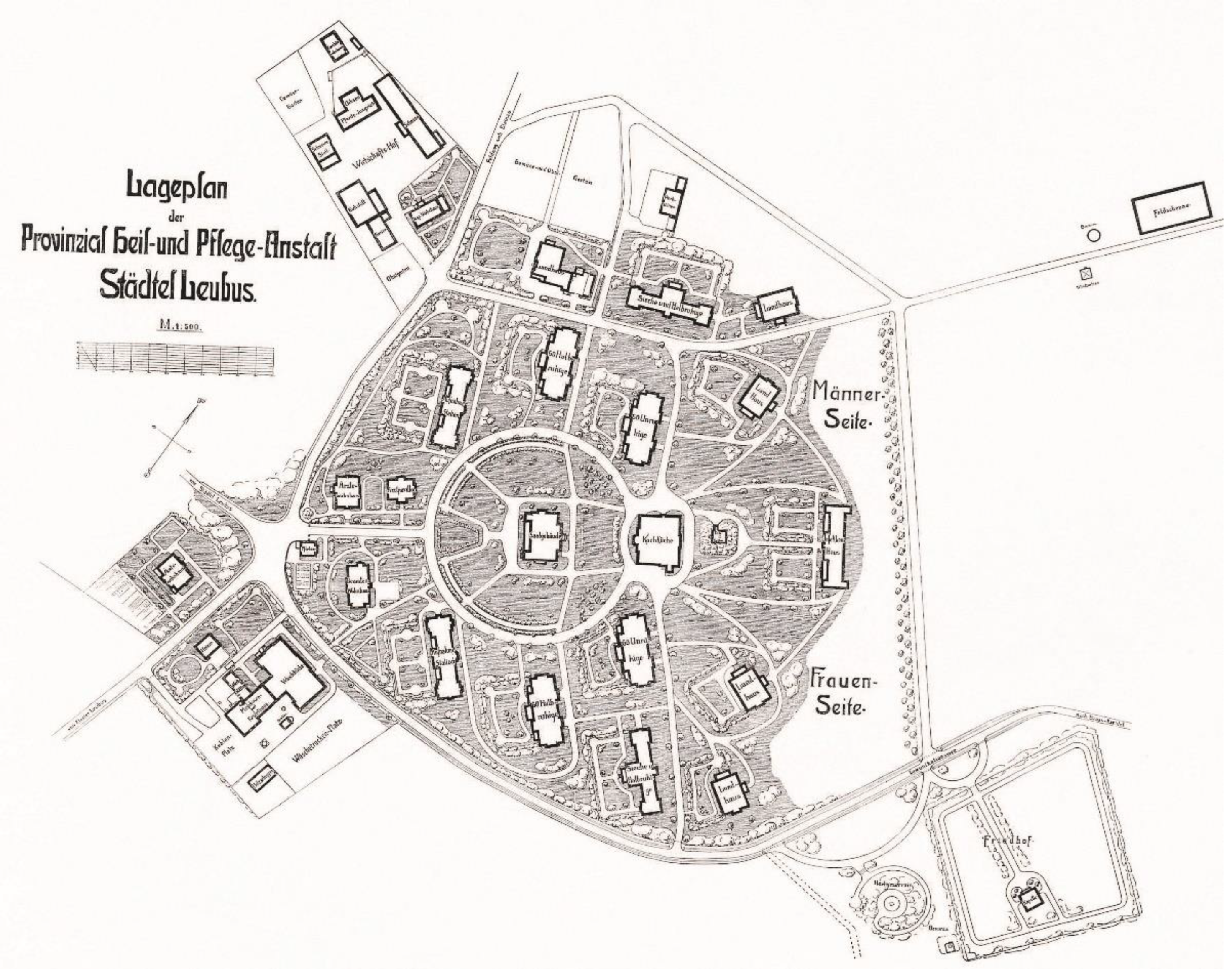
- The Voivodeship Mental Hospital Lubiąż, former Provincial Hospital for the Nervously and Mentally Ill (so-called ‘New Institution’, to differentiate it from the old hospital situated in a former Cistercian abbey), Lubiąż (Lower Silesia Voivideship, Poland);
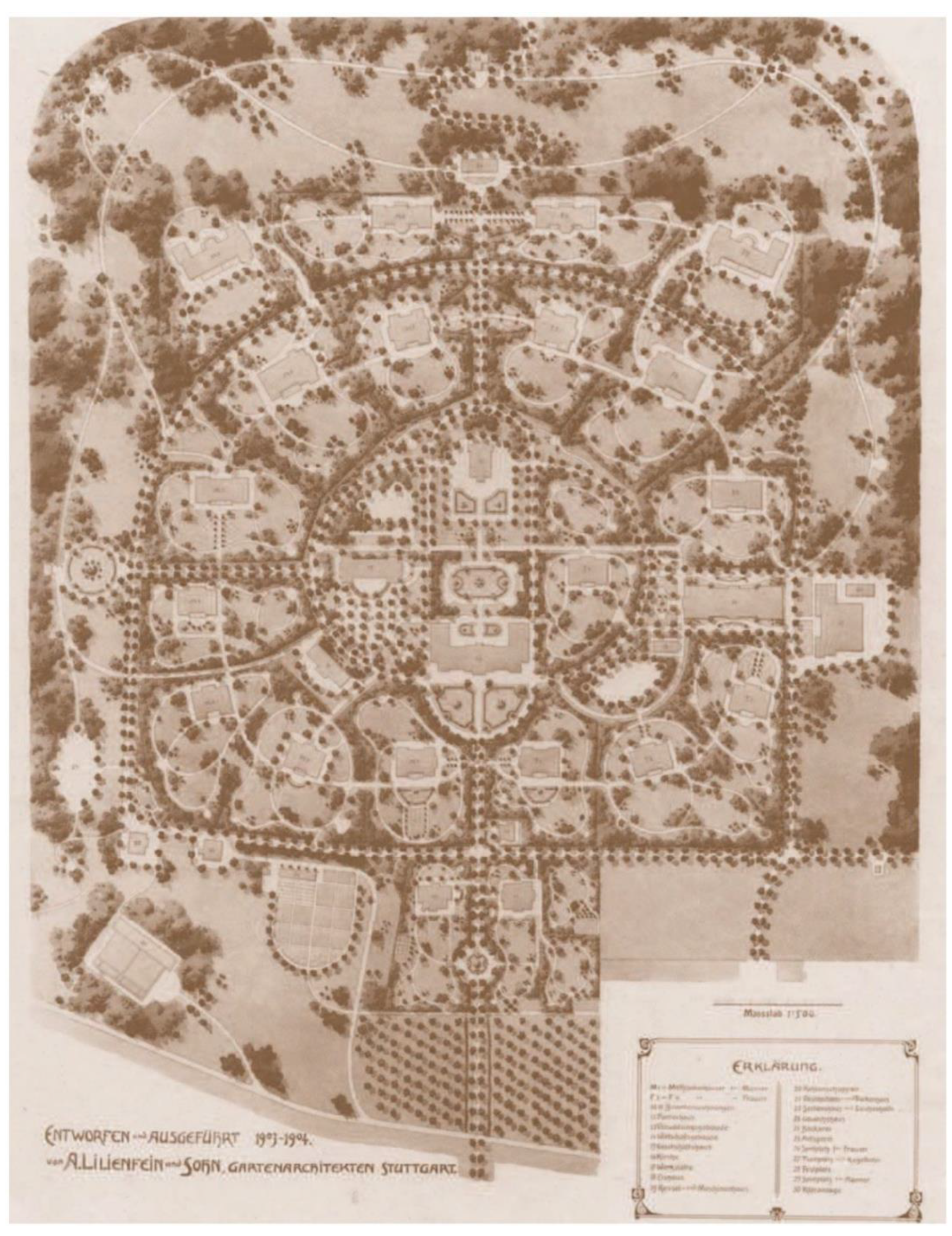
- Klinikum am Weissenhof Centre for Psychiatry Weinsberg, former Königliche Heilanstalt Weinsberg, Staatliche Irrenanstalt, Weissenhof-Weinsberg (Baden-Würtemberg, Germany).
3. Results
3.1. An Overview of Connections to Nature and Green Therapies Historically Used in Mental Hospitals from the Turn of the 19th and 20th Centuries
The cultivation of the gardens, and of the ground called the farm, as well as of the extensive ornamental ground in front of the asylum, is entirely effected by the labour of numerous male patients, superintended by gardeners, or by steady workmen. The cheerfulness with which their work is performed, and the satisfaction with which, at stated hours, they assemble for their allowance of beer, sufficiently attest that calming and remedial influences are thus exercised [84] (p. 51).
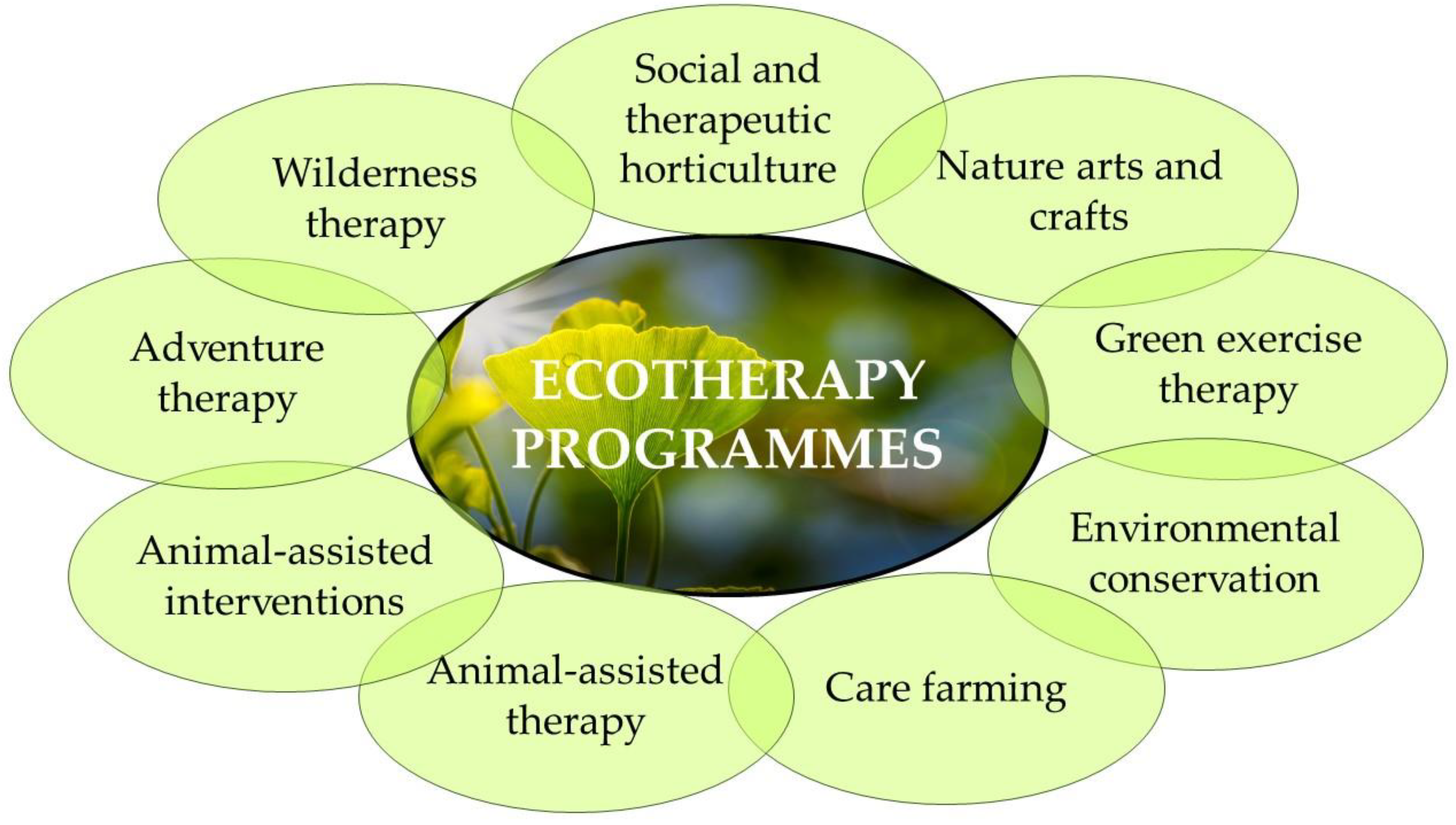
3.2. Nature and Green Therapies Supporting Mental Health and Well-Being Nowadays
- Social and therapeutic horticulture (passive: simply spending time and admiring gardens and plants; or active: focused on gardening, tending the food-growing plants. May also take place indoors, in greenhouses);
- Green exercise therapy (doing exercise in green spaces: yoga, walking, running, or cycling);
- Care farming (the therapeutic use of agricultural landscape and farming practices such as growing crops, looking after farm animals, or helping to manage woodland);
- Animal-assisted interventions (spending relaxed time in contact with animals in spaces like farms, especially introduced in groups of young patients);
- Animal-assisted therapy (meant as building a therapeutic relationship with animals, especially dogs and horses);
- Environmental conservation (activities focused on protecting and caring for natural spaces, often combining physical exercise with conservation tasks);
- Nature arts and crafts (creating art in green spaces, or with nature and natural materials, such as painting, sculpture, and creating land-art, and also referring to use of the environment as inspiration);
- Adventure therapy (focused on adventurous physical group activities like rafting or rock climbing);
3.3. A spectrum of Green Therapies Conducted in Selected Contemporary Facilities Operating within the Walls of Historic Psychiatric Hospitals
3.3.1. Kobierzyn, Krakow
3.3.2. Lubiąż
3.3.3. Weissenhof Weinsberg Klinikum
4. Discussion
Ecotherapy Programmes and Their Relation to a Historic Mental Hospital Therapeutic Landscape
5. Conclusions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gerard, D.L. Chiarugi and Pinel considered: Soul’s brain/person’s mind. J. Hist. Behav. Sci. 1997, 33, 381–403. [Google Scholar] [CrossRef]
- Pinel, P. Traité Médico-Philosophique sur L’aliénation Mentale ou la Manie; Caille & Ravier: Paris, France, 1801. [Google Scholar]
- Tuke, S. Description of the Retreat, an Institution near York, for Insane Persons of the Society of Friends: Containing an Account of Its Origin and Progress, the Modes of Treatment, and a Statement of Cases; Isaac Peirce: Philadelphia, PA, USA, 1813. [Google Scholar]
- Rutherford, S. The Landscapes of Public Lunatic Asylums in England, 1808–1914. Ph.D. Thesis, de Montfort University, Leicester, UK, 2003. Available online: https://www.dora.dmu.ac.uk/handle/2086/4783 (accessed on 12 August 2022).
- Rutherford, S. The Victorian Asylum; Shire Publications: Oxford, UK, 2008. [Google Scholar]
- Rutherford, S. Landscapes for the Mind and Body, Context 72, December 2001, The Institute of Historic Building Conservation. Available online: http://ihbc.org.uk/context_archive/72/landscapes/hospital.html (accessed on 12 August 2022).
- Mercier, C. Lunatic Asylums, their Organisation and Management; Griffin: London, UK, 1894; pp. 100–114. [Google Scholar]
- Allmond, G. The First Garden City? Environment and utopianism in an Edwardian institution for the insane poor. J. Hist. Geogr. 2017, 56, 101–112. [Google Scholar] [CrossRef]
- Mues, A. Eine Gartenstadt für Psychisch Kranke—Die Baugeschichte der Heil- und Pflegeanstalt Wiesloch, Wiesloch—Beiträge zur Geschichte; Band 2: Ubstadt-Weiher, Germany, 2001; pp. 290–304. [Google Scholar]
- Howard, Ebenezer, To-morrow: A Peaceful Path to Real Reform, London: Swan Sonnenschein & Co., Ltd., 1898. Available online: https://commons.wikimedia.org/wiki/File:Diagram_No.3_(Howard,_Ebenezer,_To-morrow.).jpg (accessed on 12 August 2022).
- Shorter, E. A history of Psychiatry: From the Era of the Asylum to the Age of Prozac; John Wiley & Sons: New York, NY, USA, 1997. [Google Scholar]
- Leff, J. Care in the Community: Illusion or Reality? John Wiley & Sons: Chichester, UK, 1997. [Google Scholar]
- Whitley, R. The Antipsychiatry Movement: Dead, Diminishing, or Developing? Psychiatr. Serv. 2012, 63, 1039–1041. [Google Scholar] [CrossRef] [PubMed]
- Proceedings of a Conference Held at Church House, Westminster, London, on 9m and 10th March, 1961, p. 5. In The Speeches of John Enoch Powell, p. 36. Available online: http://enochpowell.info/wp-content/uploads/Speeches/1957-1961.pdf (accessed on 31 March 2022).
- Killaspy, H. From the asylum to community care: Learning from experience. Br. Med. Bull. 2006, 79–80, 245–258. [Google Scholar] [CrossRef] [PubMed]
- Taylor, B. The demise of the asylum in late twentieth-century britain: A personal history. Trans. R. Hist. Soc. 2011, 21, 193–215. [Google Scholar] [CrossRef]
- Lowin, A.; Knapp, M.; Beecham, J. Uses of Old Long-Stay Hospital Buildings, Psychiatr. Bull. 1998, 22, 129–130. [Google Scholar]
- SAVE, Mind over Matter: A Study of the Country’s Threatened Mental Asylums; SAVE Britain’s Heritage: London, UK, 1995.
- Chaplin, R.; Peters, S. Executives have taken over the asylum: The fate of 71 psychiatric hospitals. Psychiatr. Bull. 2003, 27, 227–229. [Google Scholar] [CrossRef]
- Jacobson, D.R. Mapping the location, design and decline of London’s psychiatric asylums (1831–2012). J. Maps 2016, 12, 684–694. [Google Scholar] [CrossRef]
- Dumont, M.P.; Dumont, D.M. Deinstitutionalization in the United States and Italy: A Historical Survey. Int. J. Ment. Health 2008, 37, 61–70. [Google Scholar] [CrossRef]
- Lamb, H.R.; Bachrach, L.L. Some perspectives on deinstitutionalization. Psychiatr. Serv. 2001, 52, 1039–1045. [Google Scholar] [CrossRef]
- Joseph, A.; Kearns, R.; Moon, G. Re-Imagining Psychiatric Asylum Spaces through Residential Redevelopment: Strategic Forgetting and Selective Remembrance. Hous. Stud. 2013, 28, 135–153. [Google Scholar] [CrossRef]
- Vermorel, H.; Vermorel, M. De l’asile à la politique de secteur: L’évolution des institutions et des soins psychiatriques à Bassens. Inf. Psychiatr. 2012, 88, 759–770. [Google Scholar] [CrossRef]
- Gusset, S.; Seglias, L.; Lengwiler, M. Versorgen, behandeln, pflegen: Geschichte der Psychiatrie in Graubünden. In Quellen und Forschungen zur Bündner Geschichte; Band 38, Herausgegeben vom Staatsarchiv Graubünden; Florian Hitz, Schwabe: Basel, Switzerland, 2021. [Google Scholar]
- Wolf, G., Ed.; Geschäftsbericht Zentren für Psychiatrie in Baden-Württemberg 2021; Zentren für Psychiatrie Baden-Württemberg, 2021. Available online: https://docplayer.org/215123331-Geschaeftsbericht-zentren-fuer-psychiatrie-in-baden-wuerttemberg.html (accessed on 10 July 2022).
- Staniewska, A. Zagrożenia parków i ogrodów towarzyszących dawnym szpitalom psychiatrycznym w Polsce. In Dziedzictwo Zagrożone, Ogrody Historyczne w Polsce, Hodor, K., Łakomy, K., Eds.; Politechnika Krakowska: Kraków, Poland, 2015; pp. 102–120. [Google Scholar]
- Rosenberg, C.E. Epilogue: Airs, Waters, Places. A Status Report. Bull. Hist. Med. 2012, 86, 661–670, Project MUSE. [Google Scholar] [CrossRef] [PubMed]
- Gesler, W.M. Therapeutic landscapes: Medical issues in the light of the new cultural geography. Soc. Sci. Med. 1992, 34, 735–746. [Google Scholar] [CrossRef]
- Williams, A. Therapeutic landscapes in holistic medicine. Soc. Sci. Med. 1998, 46, 1193–1203. [Google Scholar] [CrossRef]
- Appleton, J. The Experience of Landscape; John Wiley & Sons: London, UK, 1975. [Google Scholar]
- Kaplan, S. The restorative benefits of nature: Toward an integrative framework. J. Environ. Psychol. 1995, 15, 169–182. [Google Scholar] [CrossRef]
- Kaplan, R.; Kaplan, S. The Experience of Nature: A Psychological Perspective; Cambridge University Press: Cambridge, UK, 1989. [Google Scholar]
- Ulrich, R.S. View Through a Window May Influence Recovery. Science 1984, 224, 224–225. [Google Scholar] [CrossRef]
- Ulrich, R.S. Visual landscapes and psychological well-being. Landsc Res. 1979, 4, 17–23. [Google Scholar] [CrossRef]
- Ulrich, R.S. Human responses to vegetation and landscapes. Landsc. Urban Plan. 1986, 13, 29–44. [Google Scholar] [CrossRef]
- Dushkova, D.; Ignatieva, M. New Trends in Urban Environmental Health Research: From Geography of Diseases To Therapeutic Landscapes and Healing Gardens. Geogr. Environ. Sustain. 2020, 13, 159–171. [Google Scholar] [CrossRef]
- Saratsi, E.; White, J.; Holyoak, V. Taking Account of Heritage Values of Urban Parks and Gardens; Living with Environmental Change Policy and Practice Notes; Note No.36; Living With Environmental Change Polaris House, North Star Avenue: Wiltshire, UK, September 2016. [Google Scholar] [CrossRef]
- Gilmore, A. The park and the commons: Vernacular spaces for everyday participation and cultural value. Cult. Trends 2017, 26, 34–46. [Google Scholar] [CrossRef]
- Mell, I.C. Green infrastructure: Reflections on past, present and future praxis. Landsc. Res. 2017, 42, 135–145. [Google Scholar] [CrossRef]
- Swensen, G.; Krokann Berg, S. The ‘garden city’ in the green infrastructure of the future: Learning from the past. Landsc. Res. 2020, 45, 802–818. [Google Scholar] [CrossRef]
- Cameron, T.; Blanuša, J.; Taylor, E.; Salisbury, A.; Halstead, A.J.; Henricot, B.; Thompson, K. The domestic garden—Its contribution to urban green infrastructure. Urban For. Urban Green. 2012, 11, 129–137. [Google Scholar] [CrossRef]
- Ying, J.; Zhang, X.; Zhang, Y.; Bilan, S. Green infrastructure: Systematic literature review. Econ. Res. -Ekon. Istraživanja 2022, 35, 343–366. [Google Scholar] [CrossRef]
- Hartig, T.; Mitchell, R.; de Vries, S.; Frumkin, H. Nature and health. Annu. Rev. Public Health 2014, 35, 207–228. [Google Scholar] [CrossRef]
- Hartig, T. Restorative Environments. In Encyclopedia of Applied Psychology; Spielberger, C., Ed.; Academic Press: San Diego, CA, USA, 2004; pp. 273–279. [Google Scholar] [CrossRef]
- Hartig, T. Restoration in Nature: Beyond the Conventional Narrative. In Nature and Psychology, Schutte, A.R., Torquati, J.C., Stevens, J.R., Eds.; Nebraska Symposium on Motivation; Springer: Cham, Switzerland, 2021; Volume 67, pp. 89–151. [Google Scholar] [CrossRef]
- Annerstedt van den Bosch, M.; Depledge, M.H. Healthy people with nature in mind. BMC Public Health 2015, 15, 1232. [Google Scholar] [CrossRef]
- van den Bosch, M.; Ode Sang, Å. Urban natural environments as nature-based solutions for improved public health—A systematic review of reviews. Environ. Res. 2017, 158, 373–384. [Google Scholar] [CrossRef]
- Twohig-Bennett, C.; Jones, A. The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace exposure and health outcomes. Environ Res. 2018, 166, 628–637. [Google Scholar] [CrossRef]
- Kondo, M.C.; Fluehr, J.M.; McKeon, T.; Branas, C.C. Urban Green Space and Its Impact on Human Health. Int. J. Environ. Res. Public Health 2018, 15, 445. [Google Scholar] [CrossRef]
- Chen, K.; Zhang, T.; Liu, F.; Zhang, Y.; Song, Y. How Does Urban Green Space Impact Residents’ Mental Health: A Literature Review of Mediators. Int. J. Environ. Res. Public Health 2021, 18, 11746. [Google Scholar] [CrossRef] [PubMed]
- Maas, J.; Verheij, R.A.; Groenewegen, P.P.; de Vries, S.; Spreeuwenberg, P. Green space, urbanity, and health: How strong is the relation? J. Epidemiol. Community Health 2006, 60, 587–592. [Google Scholar] [CrossRef] [PubMed]
- Berman, M.G.; Kross, E.; Krpan, K.M.; Askren, M.K.; Burson, A.; Deldin, P.J.; Kaplan, S.; Sherdell, L.; Gotlib, I.H.; Jonides, J. Interacting with nature improves cognition and affect for individuals with depression. J. Affect. Disord. 2012, 140, 300–305. [Google Scholar] [CrossRef] [PubMed]
- van den Berg, M.; van Poppel, M.; van Kamp, I.; Andrusaityte, S.; Balseviciene, B.; Cirach, M.; Danileviciute, A.; Ellis, N.; Hurst, G.; Masterson, D.; et al. Visiting green space is associated with mental health and vitality: A cross-sectional study in four European cities. Health Place 2016, 38, 8–15. [Google Scholar] [CrossRef]
- van den Berg, M.M.; van Poppel, M.; van Kamp, I.; Ruijsbroek, A.; Triguero-Mas, M.; Gid-low, C.; Nieuwenhuijsen, M.J.; Gražulevičiene, R.; van Mechelen, W.; Kruize, H.; et al. Do Physical Activity, Social Cohesion, and Loneliness Mediate the Association Between Time Spent Visiting Green Space and Mental Health? Environ. Behav. 2019, 51, 144–166. [Google Scholar] [CrossRef]
- Roscoe, C.; Sheridan, C.; Geneshka, M.; Hodgson, S.; Vineis, P.; Gulliver, J.; Fecht, D. Green Walkability and Physical Activity in UK Biobank: A Cross-Sectional Analysis of Adults in Greater London. Int. J. Environ. Res. Public Health 2022, 19, 4247. [Google Scholar] [CrossRef]
- WHO. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-disorders (accessed on 22 June 2022).
- Institute of Health Metrics and Evaluation. Global Health Data Exchange (GHDx). Available online: https://vizhub.healthdata.org/gbd-results (accessed on 22 June 2022).
- Reinert, M.; Fritze, D.; Nguyen, T. The State of Mental Health in America 2022, Mental Health America, Alexandria VA 2021; p. 20. Available online: https://mhanational.org/issues/state-mental-health-america (accessed on 22 June 2022).
- Halbreich, U. Stress-related physical and mental disorders: A new paradigm. BJPsych Adv. 2021, 27, 145–152. [Google Scholar] [CrossRef]
- World Health Organization. Mental health atlas 2020. World Health Organization. 2021. Available online: https://apps.who.int/iris/handle/10665/345946.License: CC BY-NC-SA 3.0 IGO (accessed on 22 June 2022).
- Han, A.R.; Park, S.A.; Ahn, B.E. Reduced stress and improved physical functional ability in elderly with mental health problems following a horticultural therapy program. Complementary Ther. Med. 2018, 38, 19–23. [Google Scholar] [CrossRef]
- Overbey, T.A.; Diekmann, F.; Lekies, K.S. Nature-based interventions for vulnerable youth: A scoping review. Int. J. Environ. Health Res. 2021, 1–39. [Google Scholar] [CrossRef]
- Siu, A.; Kam, M.; Mok, I. Horticultural Therapy Program for People with Mental Illness: A Mixed-Method Evaluation. Int. J. Environ. Res. Public Health 2020, 17, 711. [Google Scholar] [CrossRef]
- Gonzalez, M.T.; Hartig, T.; Patil, G.G.; Martinsen, E.W.; Kirkevold, M. Therapeutic horticulture in clinical depression: A prospective study of active components. J. Adv. Nurs. 2010, 66, 2002–2013. [Google Scholar] [CrossRef] [PubMed]
- Detweiler, M.B.; Self, J.A.; Lane, S.; Spencer, L.; Lutgens, B.; Kim, D.Y.; Halling, M.H.; Rudder, T.C.; Lehmann, L.P. Horticultural therapy: A pilot study on modulating cortisol levels and indices of substance craving, posttraumatic stress disorder, depression, and quality of life in veterans. Altern. Ther. Health Med. 2015, 21, 36–41, PMID: 26030115. [Google Scholar]
- Wise, J. Digging for Victory. Horticultural therapy with Veterans for Post-Traumatic Growth; Routledge: London, UK, 2015. [Google Scholar]
- Poulsen, D.V.; Stigsdotter, U.K.; Refshage, A.D. Whatever happened to the soldiers? Nature-assisted therapies for veterans diagnosed with post-traumatic stress disorder: A literature review. Urban For. Urban Green. 2015, 14, 438–445. [Google Scholar] [CrossRef]
- Eichholz, C. Therapeutic Horticulture as a Healing Tool for Veterans. Dissertation, University of Pennsylvania, Philadelphia, PA, USA, 2020. Pennsylvania US. Available online: https://repository.upenn.edu/edissertations_sp2/142 (accessed on 17 February 2022).
- Murroni, V.; Cavalli, R.; Basso, A.; Borella, E.; Meneghetti, C.; Melendugno, A.; Pazzaglia, F. Effectiveness of Therapeutic Gardens for People with D dementia: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 9595. [Google Scholar] [CrossRef] [PubMed]
- Bourdon, E.; Belmin, J. Enriched gardens improve cognition and independence of nursing home residents with dementia: A pilot controlled trial. Alzheimer’s Res. Ther. 2021, 13, 116. [Google Scholar] [CrossRef]
- Cooper-Marcus, C.; Barnes, M. Gardens in Healthcare Facilities: Uses, Therapeutic Benefits, and Design Recommendations; The Center for Health Design: Martinez, CA, USA, 1995. [Google Scholar]
- Cooper-Marcus, C.; Barnes, M. Healing Gardens: Therapeutic Benefits and Design Recommendations; John Wiley: New York, NY, USA, 1999. [Google Scholar]
- Gierlach-Spriggs, N.; Kaufman, R.E.; Warner, S.B., Jr. Restorative Garden: The Healing Landscape; Yale University Press: New Haven, CT, USA, 1998. [Google Scholar]
- Stigsdotter, U.; Grahn, P. What makes a garden a healing garden? J. Ther. Hortic. 2002, 13, 60–69. [Google Scholar]
- Trojanowska, M. Parki i Ogrody Terapeutyczne; Wydawnictwo Naukowe PWN: Warszawa, Polandm, 2017. [Google Scholar]
- Staniewska, A. Obłędne Ogrody: Idea Krajobrazu Terapeutycznego w Kompozycji Zespołów Szpitali Psychiatrycznych XIX i Początku XX Wieku; Wydawnictwo Politechniki Krakowskiej: Kraków, Poland, 2020. [Google Scholar]
- Babbie, E. The Practice of Social Research; Wadsworth: Belmont, CA, USA, 1992. [Google Scholar]
- Kvale, S. Doing Interviews; SAGE Publications Ltd.: London, UK, 2007; pp. 2–10. [Google Scholar] [CrossRef]
- Jamshed, S. Qualitative research method-interviewing and observation. J. Basic Clin. Pharm. 2014, 5, 87–88. [Google Scholar] [CrossRef]
- Curran, K.; Zimmermann, N. The Dynamics of Collaboration in Heritage Science. Stud. Conserv. 2022, 67, 136–149. [Google Scholar] [CrossRef]
- McGrath, C.; Palmgren, P.J.; Liljedahl, M. Twelve tips for conducting qualitative research interviews. Med. Teach. 2019, 41, 1002–1006. [Google Scholar] [CrossRef]
- Fontana, A.; Frey, J.H. The interview: From neutral stance to political involvement. In The SAGE Handbook of Qualitative Research; Denzin, N.K., Lincoln, Y.S., Eds.; Sage: Thousand Oaks, CA, USA, 2005; pp. 695–727. [Google Scholar]
- Conolly, J.M. The Construction and Government of Lunatic Asylums and Hospitals for the Insane; J. Churchill: London, UK, 1847. [Google Scholar]
- Suggestions and Instructions in reference to Sites, Construction, and Arrangement of Buildings, and Plans of Lunatic Asylums, Issued by the Commissioners in Lunacy. J. Ment. Sci. 1871, 16, 627–631. [CrossRef]
- Browne, W.A.F. What Asylums Were, Are, and Ought to Be Being the Substance of Five Lectures Delivered before the Managers of the Montrose Royal Lunatic Asylum; A.C. Black: Edinburgh, UK, 1837. [Google Scholar]
- Parchappe, M. Des Principes à Suivre Dans la Fondation et la Construction des Asiles d’Aliénés; Librairie de Victor Masson: Paris, France, 1853. [Google Scholar]
- Roller, C.F.W. Die Irrenanstalt Nach allen ihren Beziehungen dargestellt. Mit Lithographischen und Colorirten Plane; Müller: Karlsruhe, Germany, 1831; pp. 114–115. [Google Scholar]
- Hickman, C. Therapeutic Landscapes. A History of English Hospital Gardens Since 1800; Manchester University Press: Manchester, UK, 2013. [Google Scholar]
- Zagórski, R. O Zakładzie dla umysłowo i nerwowo chorych w Kobierzynie. Zarys rozwoju Zakładu pod koniec 1924 roku. Pol. Gaz. Lek. 1925, 18, 420–423. [Google Scholar]
- Beveridge, A. What became of Arthur Conan Doyle’s father? The last years of Charles Altamont Doyle. J. R. Coll. Phys. Edinb. 2006, 36, 264–270. Available online: https://www.rcpe.ac.uk/sites/default/files/u_beveridge2.pdf (accessed on 12 August 2022).
- Montès, J.-F. Le monde clos, ou la raison médico-économique. Sci. Soc. Et St. 1993, 11, 41–69. [Google Scholar] [CrossRef]
- Vanja, C. Von der herzoglihen Irrenanstalt zum modernen Gesundheitskonzern. Die Geschichte der nassauischen Pscyhiatrie, In Nassauische Annalen, Jahrbuch des Vereins für Nassauische Altertumskunde und Geschichtsforschung; Bd123_Sonderband: Wiesbaden, Germany, 2021; pp. 603–634. [Google Scholar]
- Roszak, T.; Gomes, M.E.; Kanner, A.D. (Eds.) Ecopsychology: Restoring the Earth, Healing the Mind; Sierra Club Books: Berkeley, CA, USA.; Los Angeles, CA, USA.; London, UK, 1995. [Google Scholar]
- Summers, J.K.; Vivian, D.N. Ecotherapy—A Forgotten Ecosystem Service: A Review. Front. Psychol. 2018, 9, 1389. [Google Scholar] [CrossRef]
- Buzzell, L.; Craig, C. Ecotherapy: Healing with Nature in Mind; Sierra Club Books: San Francisco, CA, USA, 2009. [Google Scholar]
- Bragg, R.; Wood, C.; Barton, J. Ecominds Effects on Mental Wellbeing. An Evaluation for Mind; MIND: London, UK, 2013; Available online: https://www.bl.uk/collection-items/ecominds-effects-on-mental-wellbeing-an-evaluation-for-mind (accessed on 12 August 2022).
- Ecotherapy, MIND 2021. Available online: https://www.mind.org.uk/media/9661/ecotherapy-2021-pdf-for-download-pdf-version.pdf (accessed on 12 August 2022).
- Chaudhury, P.; Banerjee, D. Recovering with Nature: A Review of Ecotherapy and Implications for the COVID-19 Pandemic. Front. Public Health 2020, 8, 604440. [Google Scholar] [CrossRef]
- Danilczyk, L.; et al. Kraków—Kobierzyn, ul. Babińskiego 29, Zespół Szpitala Psychiatrycznego. Studium Urbanistyczno-Konserwatorskie. unpublished material in Babiński Clinical Hospital archive, Kraków, 1988. [Google Scholar]
- Staniewska, A.; Petryshyn, H.; Lukashchuk, H.; Kliusa, T.; Koprynia, K. Values of the historical parks and gardens of psychiatric hospitals in Kulparków and Kobierzyn as the basis for their revalorization, Wiadomości Konserw. J. Herit. Conserv. 2021, 67, 22–34. Available online: https://repozytorium.biblos.pk.edu.pl/redo/resources/44675/file/resourceFiles/StaniewskaA_WaloryHistorycznych.pdf (accessed on 12 August 2022). [CrossRef]
- Filek, E. (Babiński Clinical Hospital, Kraków, Poland). Personal communication, 2021.
- Bóbr, E. (Babiński Clinical Hospital, Kraków, Poland). Personal communication, 2021.
- Kiejna, A.; Wójtowicz, M. Prowincjalny Psychiatryczny Zakład Leczniczo-Opiekuńczy w Lubiążu 1830–1912/Provinzial Heil- und Pflegeirrenanstalt zu Leubus/Schlesien: 1830–1912; Fundacja Ochrony Zdrowia Psychicznego: Wrocław, Poland, 2002. [Google Scholar]
- Bresler, J. (Ed.) Deutsche Heil- und Pflegeanstalten für Psychischkranke in Wort und Bild; Band 1, Marhold: Halle an der Salle, Germany, 1910. [Google Scholar]
- Hohendorf, G.; Rotzoll, M.; Richter, P.; Eckart, W.; Mundt, C. Die Opfer der nationalsozialistischen “Euthanasie-Aktion T4”. Der Nervenarzt 2002, 73, 1065–1074. [Google Scholar] [CrossRef]
- Kacalak, J. Wojewódzki Szpital dla Nerwowo i Psychicznie Chorych w Lubiążu na przełomie wieków; Oscar Marand P. Spiżak: Warszawa, Poland, 2008. [Google Scholar]
- Kukułka, A. (Lubiąż Psychiatric Hospital). Personal communication, 2021.
- Festschrift „100-Jahre“. Von der Königlichen Heilanstalt Weinsberg zum Klinikum am Weissenhof 1903–2003; Knaebel, D., Zenth, U., Eds.; Klinikum am Weissenhof: Weinsberg, Germany, 2003. [Google Scholar]
- Brochure: Der Grüne Kompass, Klinikum am Weissenhof, Weinsberg 2021. p. 16. Available online: https://www.klinikum-weissenhof.de/fileadmin/user_upload/Weinsberg/News_Veranstaltungen/Gruener_Kompass_KaW.pdf (accessed on 18 November 2021).
- Lager, S. (Zentrum für Psychiatrie Weinsberg). Personal communication, 2021.
- AHTA. Definitions and Positions Paper, 2 Mar 2022. Available online: https://www.ahta.org/assets/docs/definitions%20and%20positions%20final%206.17.pdf (accessed on 11 August 2022).
- Internationalen Gesellschaft Gartentherapie, e.V. Available online: https://www.iggt.eu (accessed on 12 August 2022).
- Schweizerische Gesellschaft Gartentherapie und Gartenagogik, SGGTA. Available online: https://www.gartentherapie.ch (accessed on 12 August 2022).
- Grahn, P.; Tenngart Ivarsson, C.; Stigsdotter, U.; Bengtsson, I.-L. Using affordances as a health-promoting tool in a therapeutic garden. In Innovative Approaches to Researching Landscape and Health: Open Space: People Space 2, Ward Thompson, C., Aspinall, P., Bell, S., Eds.; Routledge: New York, NY, USA, 2010; pp. 116–154. [Google Scholar] [CrossRef]
- Trojanowska, M. A universal standard for health-promoting places. Example of assessment—On the basis of a case study of Rahway River Park. Bud. I Archit. 2021, 20, 57–82. [Google Scholar] [CrossRef]
- La Cooperativa Agricola Monte San Pantaleone. Available online: https://www.agricolamontesanpantaleone.it (accessed on 12 August 2022).
- Pieren, M.; Zoellner, S.; Tromm, P. Jubiläumspublikation der Psychiatrischen Dienste Graubünden 2017: 125 Jahre Klinik Waldhaus Chur, Hochschule für Technik und Wirtschaft, Psychiatrische Dienste Graubünden, Chur 2017. Available online: https://www.fhgr.ch/fileadmin/news/news-institute_und_zentren/news-2017_10_10-Jubilaeumspublikation_PDGR.pdf (accessed on 12 August 2022).
- ARBES. Available online: https://arbes.ch/de/arbeiten-bei-der-arbes/anlage-park-chur (accessed on 12 August 2022).
- Bildarchiv/Stiftung Luftbild Schweiz/Fotograf: Friedli, Werner LBS_H1-010108. Available online: http://doi.org/10.3932/ethz-a-000352242 (accessed on 12 August 2022).
- Psychiatrische Dienste Graubünden Klinik Waldhaus. Available online: https://upload.wikimedia.org/wikipedia/commons/3/33/Klinik_waldhaus_img2.JPG (accessed on 12 August 2022).
- Krzeptowska-Moszkowicz, I.; Moszkowicz, Ł.; Porada, K. Evolution of the Concept of Sensory Gardens in the Generally Accessible Space of a Large City: Analysis of Multiple Cases from Kraków (Poland) Using the Therapeutic Space Attribute Rating Method. Sustainability 2021, 13, 5904. [Google Scholar] [CrossRef]
- Soga, M.; Gaston, K.J.; Yamaura, Y. Gardening is beneficial for health: A meta-analysis. Prev. Med. Rep. 2016, 5, 92–99. [Google Scholar] [CrossRef]
- Beyer, K.M.; Kaltenbach, A.; Szabo, A.; Bogar, S.; Nieto, F.J.; Malecji, K.M. Exposure to neighborhood green space and mental health: Evidence from the survey of the health of Wisconsin. Int. J. Environ. Res. Public Health 2014, 11, 3453–3472. [Google Scholar] [CrossRef] [PubMed]
- Spennemann, D.H.R. The Nexus between Cultural Heritage Management and the Mental Health of Urban Communities. Land 2022, 11, 304. [Google Scholar] [CrossRef]

| Kraków-Kobierzyn | Lubiąż | Weissenhof-Weinsberg | |
|---|---|---|---|
| Historic name | The second National Institute for the Nervous and Mentally Ill | Provincial treatment and care facility in the town of Lubiąż | Königliche Heilanstalt Weinsberg, Staatliche Irrenanstalt |
| Contemporary surface in ha | 48 ha | 21 ha | 45 ha |
| Construction dates | 1909-1919 | 1902-1910 | 1900-1903 |
| Architects involved | Władysław Klimczak | Eduard Blümner | Carl Hees |
| Landscape architects | Wiktor Żochowski | nn | Albrecht Lilienfein und Sohn |
| Connection to Nature in Historic Mental Health Institutions | |
|---|---|
| In the Past | Nowadays |
| The garden setting of the asylum, located beyond city boundaries, is considered a space of mental escape from illness, and an environment supporting recovery. | Location on the outskirts of cities still considered as pleasant, but often surrounded by residential areas and urban sprawl. |
| Distant views from the institution showing picturesque landscapes. | Views become limited because of contemporary urban development—nevertheless, the most important can be preserved. |
| Gardens as places of physical exercise (gymnastics and walks); daily routine in utility and kitchen gardens; places of occupational therapy; terraces in the sun as therapy for tuberculosis. | Meditation and rest in the gardens; gardening therapy in the ward gardens; social activities—talks and therapeutic group meetings in the open air; therapeutic walks in the parks and woods surrounding the institution. |
| Orchards and arable land for food production as therapeutic work and an economic necessity. | Limited therapeutic farming/agricultural activities and animal tending. |
| Private gardens of the employees of the institution who lived onsite. | Hospital gardens as sites of regeneration during short breaks for employees. |
| Ecotherapy Programme Opportunities in Historic Mental Hospitals | |
|---|---|
| Elements of Landscape Composition of Historic Mental Hospital Sites | Potential Therapeutic Use for Ecotherapy Programmes |
| Gardens at the wards. | Social and therapeutic horticulture; nature arts and crafts; green exercise therapy (yoga and open-air gyms). |
| Ornamental grounds and representative entrance areas. | Social and therapeutic horticulture; nature arts and crafts. |
| Landscape park. | Environmental conservation; nature arts and crafts; green exercise therapy (walking). |
| Hospital farm. | Care farming; animal-assisted interventions; animal-assisted therapy. |
| Former kitchen garden (including historic and new glasshouses), orchards, and arable land. | Social and therapeutic horticulture; nature arts and crafts; care farming. |
| Private gardens of the employees of the institution who lived onsite. | Social and therapeutic horticulture; nature arts and crafts. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Staniewska, A. Gardens of Historic Mental Health Hospitals and Their Potential Use for Green Therapy Purposes. Land 2022, 11, 1618. https://doi.org/10.3390/land11101618
Staniewska A. Gardens of Historic Mental Health Hospitals and Their Potential Use for Green Therapy Purposes. Land. 2022; 11(10):1618. https://doi.org/10.3390/land11101618
Chicago/Turabian StyleStaniewska, Anna. 2022. "Gardens of Historic Mental Health Hospitals and Their Potential Use for Green Therapy Purposes" Land 11, no. 10: 1618. https://doi.org/10.3390/land11101618
APA StyleStaniewska, A. (2022). Gardens of Historic Mental Health Hospitals and Their Potential Use for Green Therapy Purposes. Land, 11(10), 1618. https://doi.org/10.3390/land11101618