The Cost of Heat: Health and Economic Burdens in Three Brazilian Cities
Abstract
1. Introduction
2. Materials and Methods
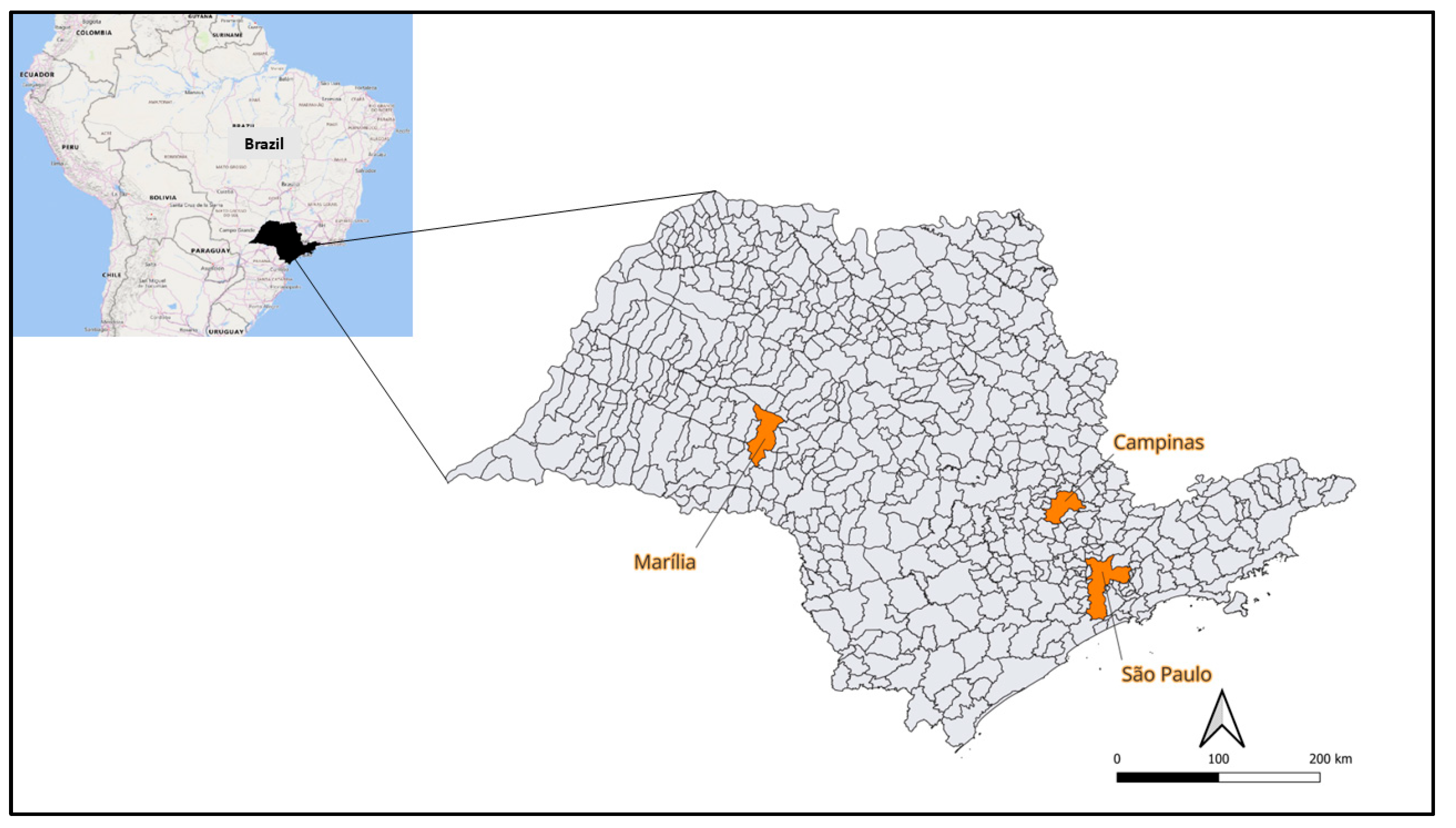
2.1. Study Area
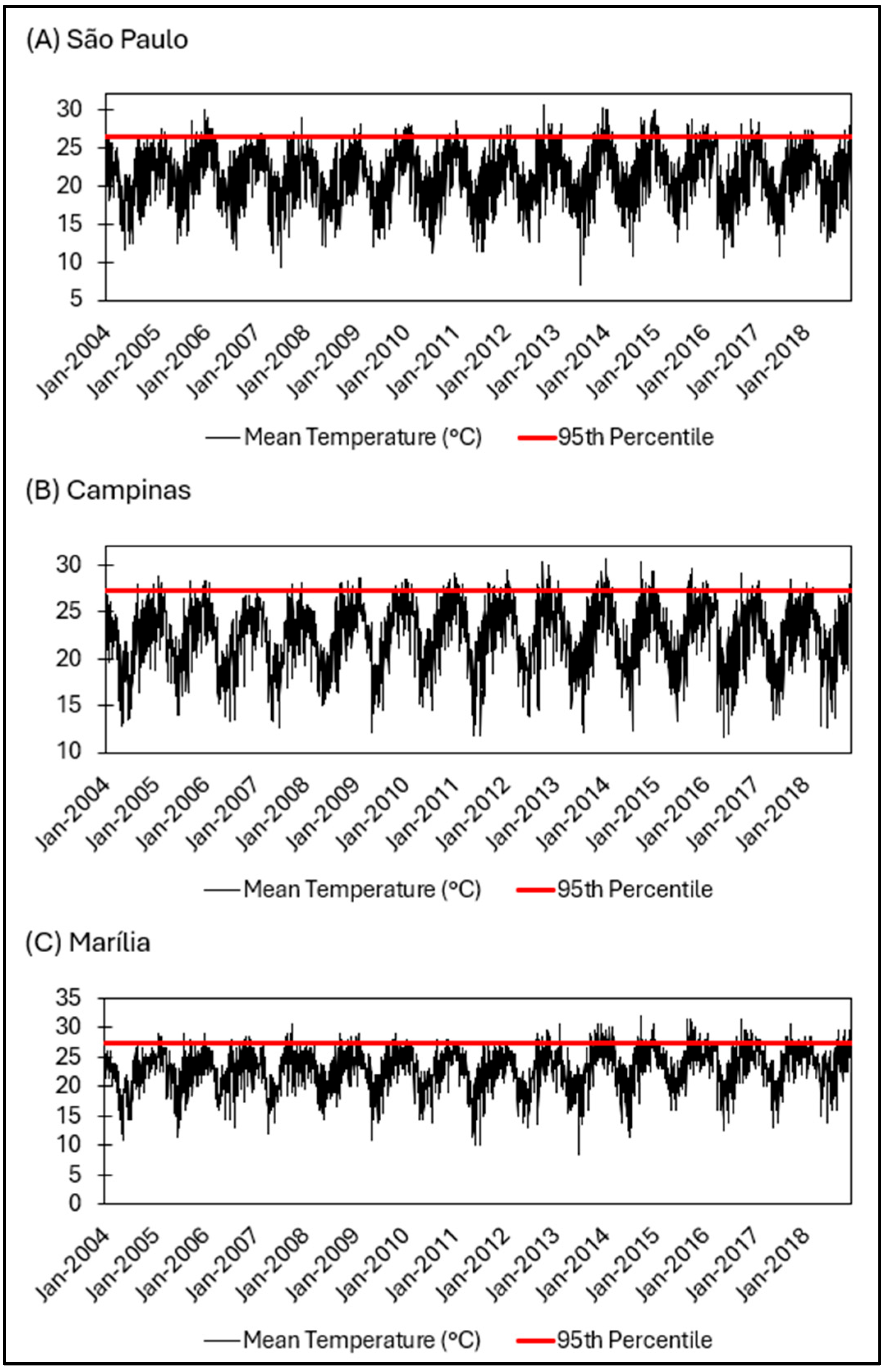
2.2. Meteorological Data
2.3. Mortality Data
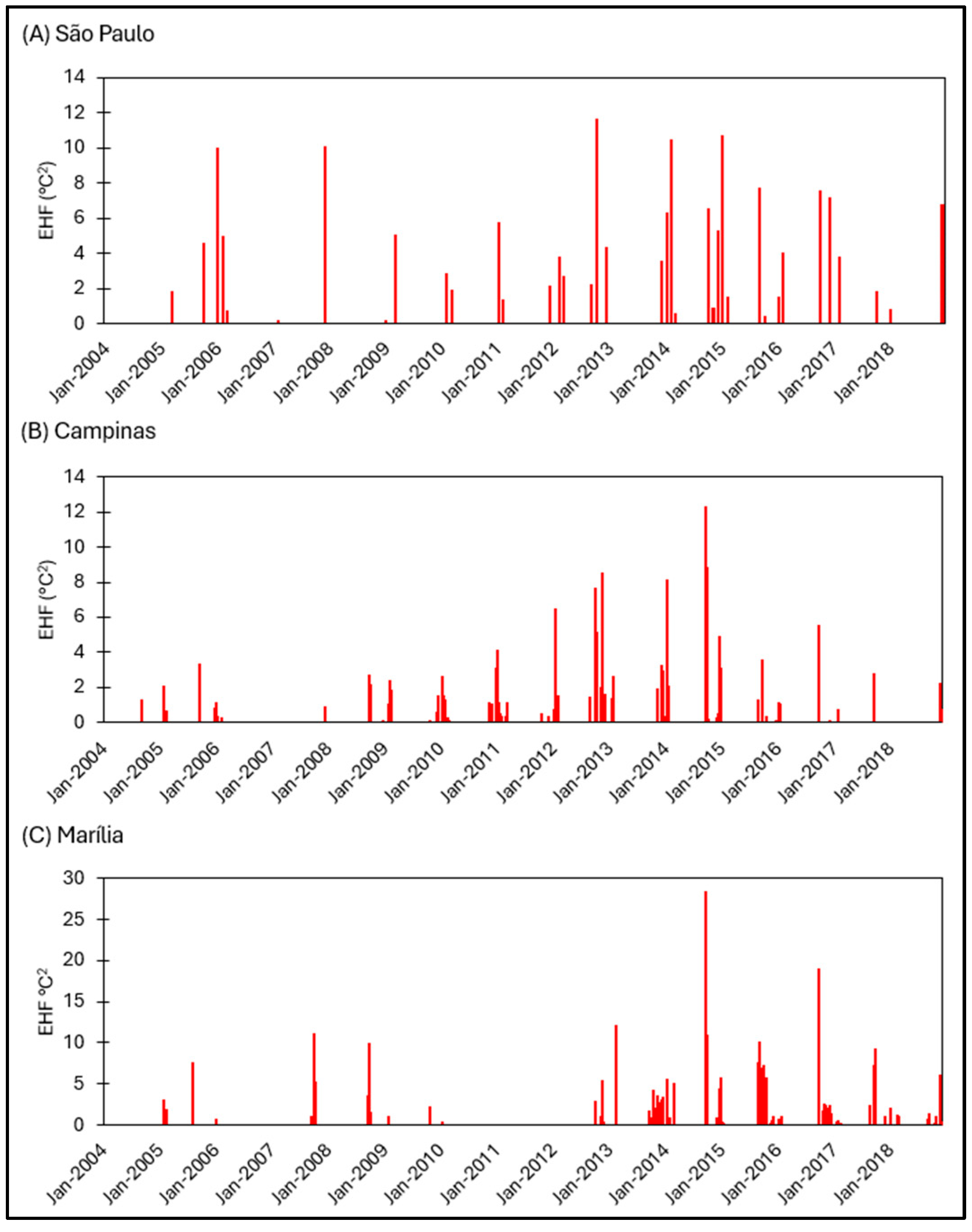
2.4. Excess Heat Factor
2.5. Generalized Linear Model (GLM)
2.6. Valuation of Mortality Risk
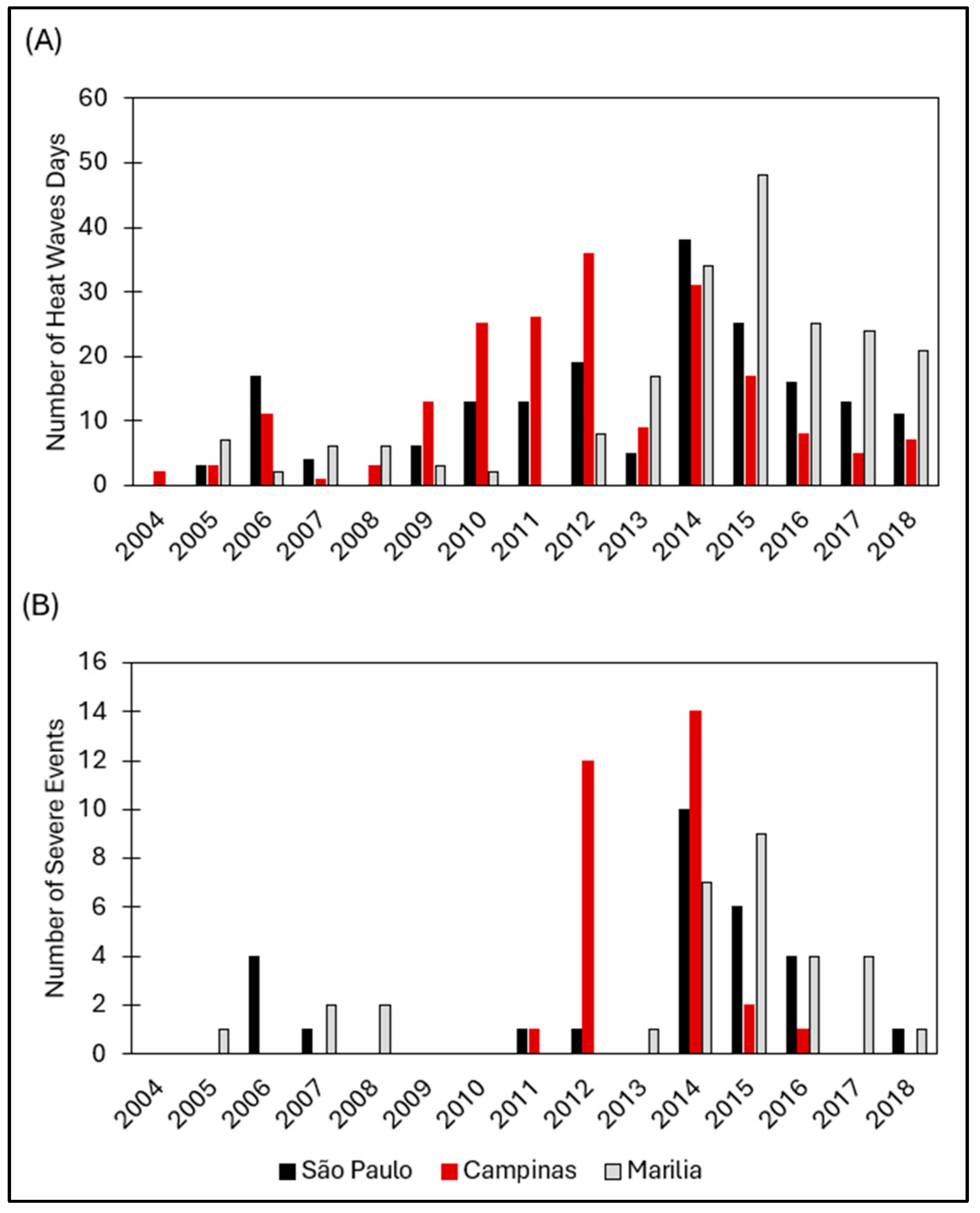
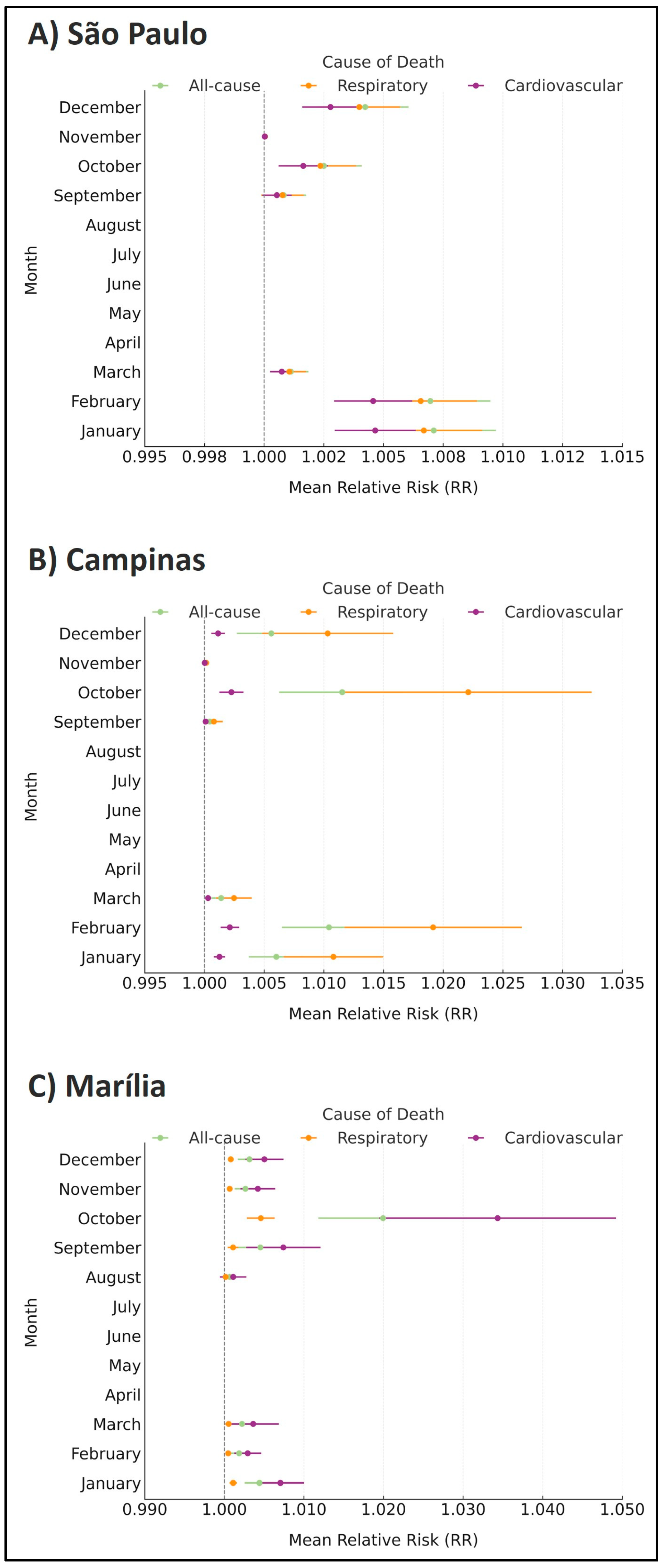
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| EHF | excess heat factor |
| RR | relative risk |
| DMT | daily mean temperature |
| VSL | value of statistical life |
| GLM | generalized linear model |
References
- IPCC. Climate Change 2022: Mitigation of Climate Change. Summary for Policymakers. Working Group III Contribution to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change; Intergovernmental Panel on Climate Change: Geneva, Switzerland, 2022; Available online: https://www.ipcc.ch/report/ar6/wg3/downloads/report/IPCC_AR6_WGIII_SPM.pdf (accessed on 20 February 2023).
- Watts, N.; Amann, M.; Arnell, N.; Ayeb-Karlsson, S.; Belesova, K.; Boykoff, M.; Byass, P.; Cai, W.; Campbell-Lendrum, D.; Capstick, S.; et al. The 2019 Report of The Lancet Countdown on Health and Climate Change: Ensuring That the Health of a Child Born Today Is Not Defined by a Changing Climate. Lancet 2019, 394, 1836–1878. [Google Scholar] [CrossRef] [PubMed]
- Goshua, A.; Gomez, J.; Erny, B.; Burke, M.; Luby, S.; Sokolow, S.; LaBeaud, A.D.; Auerbach, P.; Gisondi, M.A.; Nadeau, K. Addressing Climate Change and Its Effects on Human Health: A Call to Action for Medical Schools. Acad. Med. 2021, 96, 324–328. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.; Guo, Y.; Ye, T.; Gasparrini, A.; Tong, S.; Overcenco, A.; Urban, A.; Schneider, A.; Entezari, A.; Vicedo-Cabrera, A.M.; et al. Global, Regional, and National Burden of Mortality Associated with Non-Optimal Ambient Temperatures from 2000 to 2019: A Three-Stage Modelling Study. Lancet Planet. Health 2021, 5, e415–e425. [Google Scholar] [CrossRef]
- Hartinger, S.M.; Palmeiro-Silva, Y.K.; Llerena-Cayo, C.; Blanco-Villafuerte, L.; Escobar, L.E.; Diaz, A.; Sarmiento, J.H.; Lescano, A.G.; Melo, O.; Rojas-Rueda, D.; et al. The 2023 Latin America Report of the Lancet Countdown on Health and Climate Change: The Imperative for Health-Centred Climate-Resilient Development. Lancet Reg. Health Am. 2024, 33, 100746. [Google Scholar] [CrossRef] [PubMed]
- Miraglia, S.G.E.K.; Tavella, R.A.; Debone, D. Unprecedented Air Quality Crisis: The Impact of Widespread Fires on Air Pollution in São Paulo. Air Qual. Atmos. Health 2025, 18, 1257–1262. [Google Scholar] [CrossRef]
- Huynen, M.M.; Martens, P.; Schram, D.; Weijenberg, M.P.; Kunst, A.E. The Impact of Heat Waves and Cold Spells on Mortality Rates in the Dutch Population. Environ. Health Perspect. 2001, 109, 463–470. [Google Scholar] [CrossRef]
- Habeeb, D.; Vargo, J.; Stone, B. Rising Heat Wave Trends in Large US Cities. Nat. Hazards 2015, 76, 1651–1665. [Google Scholar] [CrossRef]
- Cui, Y.; Yin, F.; Deng, Y.; Volinn, E.; Chen, F.; Ji, K.; Zeng, J.; Zhao, X.; Li, X. Heat or Cold: Which One Exerts Greater Deleterious Effects on Health in a Basin Climate City? Impact of Ambient Temperature on Mortality in Chengdu, China. Int. J. Environ. Res. Public Health 2016, 13, 1212. [Google Scholar] [CrossRef]
- Guo, Y.; Gasparrini, A.; Armstrong, B.G.; Tawatsupa, B.; Tobias, A.; Lavigne, E.; Coelho, M.S.Z.S.; Pan, X.; Kim, H.; Hashizume, M.; et al. Heat Wave and Mortality: A Multicountry, Multicommunity Study. Environ. Health Perspect. 2017, 125, 087006. [Google Scholar] [CrossRef]
- Lin, Y.K.; Maharani, A.T.; Chang, F.T.; Wang, Y.C. Mortality and Morbidity Associated with Ambient Temperatures in Taiwan. Sci. Total Environ. 2019, 651, 210–217. [Google Scholar] [CrossRef]
- Ferguson, L.; Anna, M. The Impact of Heat Adaptation on Socioeconomically Vulnerable Populations. In Mitigation and Adaptation of Urban Overheating; Elsevier: Amsterdam, The Netherlands, 2024; pp. 277–293. [Google Scholar] [CrossRef]
- Hutton, A.; Maud, K.; Giggins, H.; Skipp, M.; Verdon-Kidd, D. Are We Adequately Promoting Climate Change Adaptation to Address the Increasing Heatwaves Affecting the Elderly? Int. J. Disaster Risk Sci. 2025, 16, 182–189. [Google Scholar] [CrossRef]
- Zhou, Y.; Larochelle, L.; Khan, F.A.; Pilote, L. Sex Differences in the Impact of Extreme Heat on Cardiovascular Disease Outcomes: A Systematic Review and Meta-Analysis. Environ. Health 2025, 24, 20. [Google Scholar] [CrossRef]
- Basu, R.; Samet, J.M. Relation between Elevated Ambient Temperature and Mortality: A Review of the Epidemiologic Evidence. Epidemiol. Rev. 2002, 24, 190–202. [Google Scholar] [CrossRef] [PubMed]
- Basu, R. High Ambient Temperature and Mortality: A Review of Epidemiologic Studies from 2001 to 2008. Environ. Health 2009, 8, 40. [Google Scholar] [CrossRef] [PubMed]
- Bell, M.L.; O’Neill, M.S.; Ranjit, N.; Borja-Aburto, V.H.; Cifuentes, L.A.; Gouveia, N.C. Vulnerability to Heat-Related Mortality in Latin America: A Case-Crossover Study in São Paulo, Brazil, Santiago, Chile and Mexico City, Mexico. Int. J. Epidemiol. 2008, 37, 796–804. [Google Scholar] [CrossRef]
- Xu, Z.; FitzGerald, G.; Guo, Y.; Jalaludin, B.; Tong, S. Impact of Heatwave on Mortality under Different Heatwave Definitions: A Systematic Review and Meta-Analysis. Environ. Int. 2016, 89–90, 193–203. [Google Scholar] [CrossRef]
- Bettaieb, J.; Toumi, A.; Leffondre, K.; Chlif, S.; Salah, A.B. High Temperature Effect on Daily All-Cause Mortality in Tunis 2005–2007. Rev. Epidemiol. Sante Publique 2020, 68, 37–43. [Google Scholar] [CrossRef]
- de Visser, M.; Kunst, A.E.; Fleischmann, M. Geographic and Socioeconomic Differences in Heat-Related Mortality among the Dutch Population: A Time Series Analysis. BMJ Open 2022, 12, e058185. [Google Scholar] [CrossRef]
- Gasparrini, A.; Guo, Y.; Hashizume, M.; Kinney, P.L.; Petkova, E.P.; Lavigne, E.; Zanobetti, A.; Schwartz, J.D.; Tobias, A.; Leone, M.; et al. Temporal Variation in Heat-Mortality Associations: A Multicountry Study. Environ. Health Perspect. 2015, 123, 1200–1207. [Google Scholar] [CrossRef]
- Sera, F.; Armstrong, B.; Tobias, A.; Vicedo-Cabrera, A.M.; Åström, C.; Bell, M.L.; Chen, B.Y.; de Sousa Zanotti Stagliorio Coelho, M.; Matus Correa, P.; Cruz, J.C.; et al. How Urban Characteristics Affect Vulnerability to Heat and Cold: A Multi-Country Analysis. Int. J. Epidemiol. 2019, 48, 1101–1112. [Google Scholar] [CrossRef]
- Nairn, J.R.; Fawcett, R.J.B. The Excess Heat Factor: A Metric for Heatwave Intensity and Its Use in Classifying Heatwave Severity. Int. J. Environ. Res. Public Health 2015, 12, 227–253. [Google Scholar] [CrossRef]
- Alberini, A.; Hunt, A.; Markandya, A. Willingness to Pay to Reduce Mortality Risks: Evidence from a Three-Country Contingent Valuation Study. Environ. Resour. Econ. 2006, 33, 251–264. [Google Scholar] [CrossRef]
- Ding, D.; Xing, J.; Wang, S.; Liu, K.; Hao, J. Estimated Contributions of Emissions Controls, Meteorological Factors, Population Growth, and Changes in Baseline Mortality to Reductions in Ambient PM2.5 and PM2.5-Related Mortality in China, 2013–2017. Environ. Health Perspect. 2019, 127, 067009. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, P.; Davidson, K.; Fulcher, C.; Fann, N.; Zawacki, M.; Baker, K.R. Monetized Health Benefits Attributable to Mobile Source Emission Reductions across the United States in 2025. Sci. Total Environ. 2019, 650, 2490–2498. [Google Scholar] [CrossRef] [PubMed]
- Debone, D.; Leirião, L.F.L.; Miraglia, S.G.E.K. Air Quality and Health Impact Assessment of a Truckers’ Strike in São Paulo State, Brazil: A Case Study. Urban Clim. 2020, 34, 100687. [Google Scholar] [CrossRef]
- IBGE. Brazilian Institute of Statistics and Geography. 2023. Available online: https://cidades.ibge.gov.br/brasil/sp/sao-paulo/panorama (accessed on 20 February 2023).
- INMET. Instituto Nacional de Meteorologia. Gráficos Climatológicos. 2020. Available online: https://clima.inmet.gov.br/GraficosClimatologicos/SP/83781 (accessed on 20 February 2023).
- AGRITEMPO. Brazilian Agro-Meteorological Monitoring System. Monitoring. São Paulo State. 2020. Available online: https://www.agritempo.gov.br/br/estado/SP/monitoramento/ (accessed on 20 February 2023).
- DATASUS. Brazilian Health System Database (TABNET). 2020. Available online: https://datasus.saude.gov.br/mortalidade-desde-1996-pela-cid-10 (accessed on 20 February 2023).
- Nairn, J.; Ostendorf, B.; Bi, P. Performance of Excess Heat Factor Severity as a Global Heatwave Health Impact Index. Int. J. Environ. Res. Public Health 2018, 15, 2494. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, A.; Lopes, A.; Soares, A. Excess Heat Factor Climatology, Trends, and Exposure across European Functional Urban Areas. Weather Clim. Extremes 2022, 36, 100455. [Google Scholar] [CrossRef]
- Langlois, N.; Herbst, J.; Mason, K.; Nairn, J.; Byard, R.W. Using the Excess Heat Factor (EHF) to Predict the Risk of Heat-Related Deaths. J. Forensic Legal Med. 2013, 20, 408–411. [Google Scholar] [CrossRef]
- OECD. Mortality Risk Valuation in Environment, Health and Transport Policies; OECD Publishing: Paris, France, 2012; p. 140. [Google Scholar] [CrossRef]
- dos Santos, D.M.; Libonati, R.; Garcia, B.N.; Geirinhas, J.L.; Salvi, B.B.; Lima e Silva, E.; Rodrigues, J.A.; Peres, L.F.; Russo, A.; Gracie, R.; et al. Twenty-First-Century Demographic and Social Inequalities of Heat-Related Deaths in Brazilian Urban Areas. PLoS ONE 2024, 19, e0295766. [Google Scholar] [CrossRef]
- Geirinhas, J.L.; Russo, A.; Libonati, R.; Trigo, R.M.; Castro, L.C.O.; Peres, L.F.; Magalhães, M.A.F.M.; Nunes, B. Heat-Related Mortality at the Beginning of the Twenty-First Century in Rio de Janeiro, Brazil. Int. J. Biometeorol. 2020, 64, 1319–1332. [Google Scholar] [CrossRef]
- Perkins-Kirkpatrick, S.E.; Lewis, S.C. Increasing Trends in Regional Heatwaves. Nat. Commun. 2020, 11, 3357. [Google Scholar] [CrossRef] [PubMed]
- Heaviside, C.; Tsangari, H.; Paschalidou, A.; Vardoulakis, S.; Kassomenos, P.; Georgiou, K.E.; Yamasaki, E.N. Heat-Related Mortality in Cyprus for Current and Future Climate Scenarios. Sci. Total Environ. 2016, 569–570, 627–633. [Google Scholar] [CrossRef] [PubMed]
- Mitropoulos, D.; Pytharoulis, I.; Zanis, P.; Anagnostopoulou, C. Synoptic Analysis and Subseasonal Predictability of an Early Heatwave in the Eastern Mediterranean. Atmosphere 2024, 15, 442. [Google Scholar] [CrossRef]
- Rathi, S.K.; Sodani, P.R.; Joshi, S. Summer Temperature and All-Cause Mortality from 2006 to 2015 for Smart City Jaipur, India. J. Health Manag. 2021, 23, 294–301. [Google Scholar] [CrossRef]
- Arsad, F.S.; Hod, R.; Ahmad, N.; Ismail, R.; Mohamed, N.; Baharom, M.; Osman, Y.; Radi, M.F.M.; Tangang, F. The Impact of Heatwaves on Mortality and Morbidity and the Associated Vulnerability Factors: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 16356. [Google Scholar] [CrossRef]
- Weinberger, K.R.; Harris, D.; Spangler, K.R.; Zanobetti, A.; Wellenius, G.A. Estimating the Number of Excess Deaths Attributable to Heat in 297 United States Counties. Environ. Epidemiol. 2020, 4, e096. [Google Scholar] [CrossRef]
- Patel, D.; Jian, L.; Xiao, J.; Jansz, J.; Yun, G.; Robertson, A. Joint Effect of Heatwaves and Air Quality on Emergency Department Attendances for Vulnerable Population in Perth, Western Australia, 2006 to 2015. Environ. Res. 2019, 174, 80–87. [Google Scholar] [CrossRef]
- Campbell, S.L.; Remenyi, T.; Williamson, G.J.; Rollins, D.; White, C.J.; Johnston, F.H. Ambulance Dispatches and Heatwaves in Tasmania, Australia: A Case-Crossover Analysis. Environ. Res. 2021, 202, 111655. [Google Scholar] [CrossRef]
- Vicedo-Cabrera, A.M.; Scovronick, N.; Sera, F.; Royé, D.; Schneider, R.; Tobias, A.; Åström, C.; Guo, Y.; Honda, Y.; Hondula, D.M.; et al. The Burden of Heat-Related Mortality Attributable to Recent Human-Induced Climate Change. Nat. Clim. Change 2021, 11, 492–500. [Google Scholar] [CrossRef]
- Adélaïde, L.; Chanel, O.; Pascal, M. Health Effects from Heat Waves in France: An Economic Evaluation. Eur. J. Health Econ. 2022, 23, 119–131. [Google Scholar] [CrossRef]
- Cheng, J.; Xu, Z.; Bambrick, H.; Su, H.; Tong, S.; Hu, W. Heatwave and Elderly Mortality: An Evaluation of Death Burden and Health Costs Considering Short-Term Mortality Displacement. Environ. Int. 2018, 115, 334–342. [Google Scholar] [CrossRef] [PubMed]
- Sousa, P.M.; Trigo, R.M.; Russo, A.; Geirinhas, J.L.; Rodrigues, A.; Silva, S.; Torres, A. Heat-Related Mortality Amplified during the COVID-19 Pandemic. Int. J. Biometeorol. 2022, 66, 457–468. [Google Scholar] [CrossRef] [PubMed]
- Caruso, G.; de Marcos, I.; Noy, I. Climate Changes Affect Human Capital. Econ. Disasters Clim. Change 2024, 8, 157–196. [Google Scholar] [CrossRef]
- de Sario, M.; de’Donato, F.K.; Bonafede, M.; Marinaccio, A.; Levi, M.; Ariani, F.; Morabito, M.; Michelozzi, P. Occupational Heat Stress, Heat-Related Effects and the Related Social and Economic Loss: A Scoping Literature Review. Front. Public Health 2023, 11, 1173553. [Google Scholar] [CrossRef]
| Region | VSL (Million USD Range) a | VSL (Million USD—Selected Value) |
|---|---|---|
| Europe | 1.5–4.5 | 3 |
| USA (EPA) | 1–10 | 7.5 |
| Great Britain | -- | 2.1 b |
| Adopted for Brazil | -- | 2.6 |
| Cause of Death | RRs [95% CI] | AFs | Monetary Valuation (Million USD) | |
|---|---|---|---|---|
| São Paulo | Total | 1.0018 [1.0015; 1.0022] | 1960 | 5096 |
| Respiratory | 1.0017 [1.0014; 1.0021] | 239 | 621.4 | |
| Cardiovascular | 1.0012 [1.0010; 1.0015] | 415 | 1079 | |
| Campinas | Total | 1.0029 [1.0023; 1.0036] | 286 | 743.6 |
| Respiratory | 1.0054 [1.0042; 1.0066] | 78 | 202.8 | |
| Cardiovascular | 1.0006 [1.0005; 1.0007] | 18 | 46.8 | |
| Marília | Total | 1.0033 [1.0025; 1.0041] | 73 | 189.8 |
| Respiratory | 1.0008 [1.0006; 1.0010] | 2 | 5.2 | |
| Cardiovascular | 1.0055 [1.0041; 1.0069] | 36 | 93.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Debone, D.; do Rosário, N.M.É.; Miraglia, S.G.E.K. The Cost of Heat: Health and Economic Burdens in Three Brazilian Cities. Atmosphere 2025, 16, 755. https://doi.org/10.3390/atmos16070755
Debone D, do Rosário NMÉ, Miraglia SGEK. The Cost of Heat: Health and Economic Burdens in Three Brazilian Cities. Atmosphere. 2025; 16(7):755. https://doi.org/10.3390/atmos16070755
Chicago/Turabian StyleDebone, Daniela, Nilton Manuel Évora do Rosário, and Simone Georges El Khouri Miraglia. 2025. "The Cost of Heat: Health and Economic Burdens in Three Brazilian Cities" Atmosphere 16, no. 7: 755. https://doi.org/10.3390/atmos16070755
APA StyleDebone, D., do Rosário, N. M. É., & Miraglia, S. G. E. K. (2025). The Cost of Heat: Health and Economic Burdens in Three Brazilian Cities. Atmosphere, 16(7), 755. https://doi.org/10.3390/atmos16070755







