The Impact of Ambient PM2.5 on Emergency Ambulance Dispatches Due to Circulatory System Disease Modified by Season and Temperature in Shenzhen, China
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sites and Data Collection
2.2. Statistical Methods
2.2.1. Examining the Effect of Air Pollutants Modified by Season
2.2.2. Examining Effect of Air Pollutant Modified by Temperature
2.2.3. Different Test for Stratification Effects
2.2.4. Sensitivity Analysis
3. Result
3.1. Descriptive Analysis
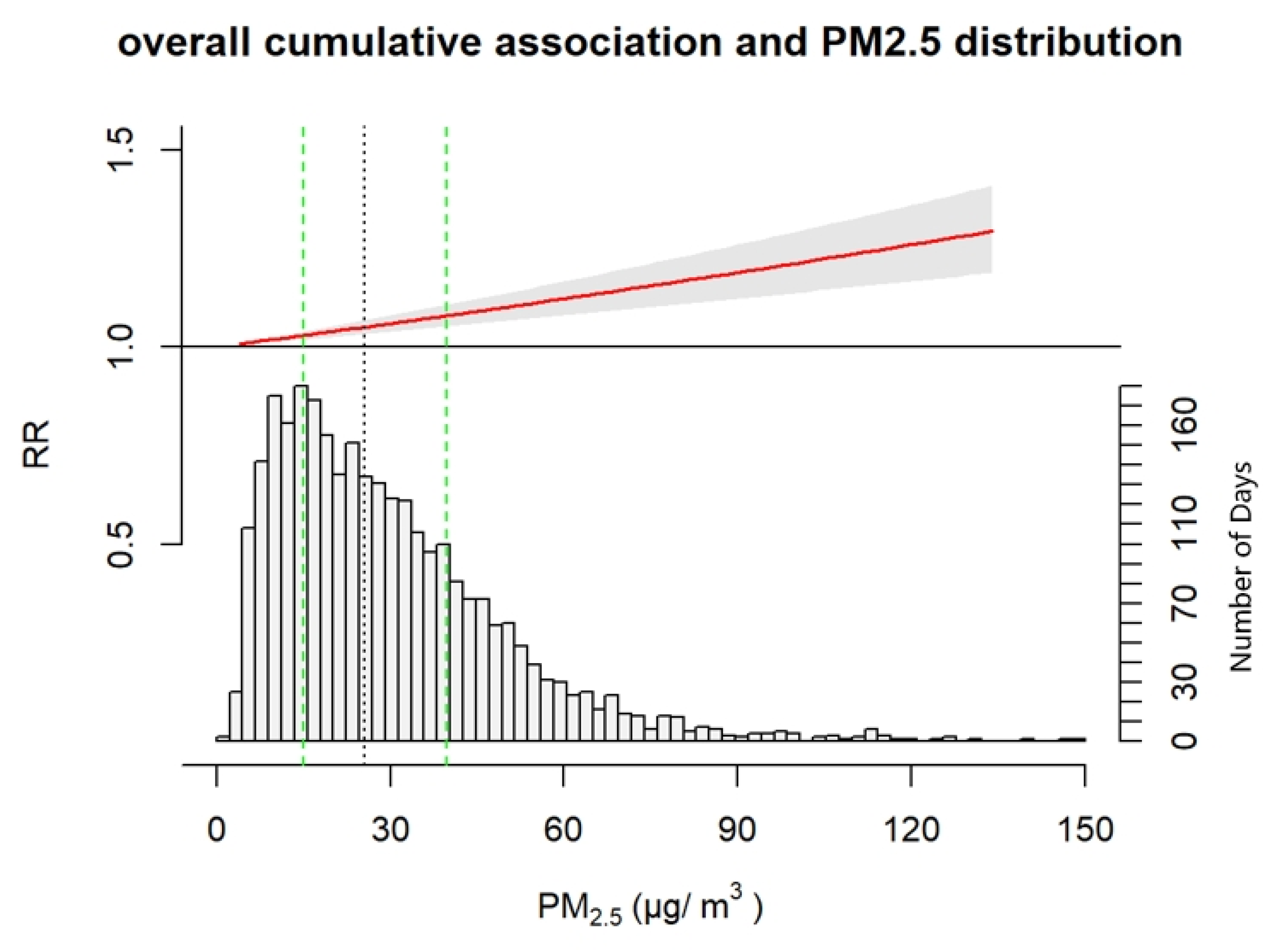
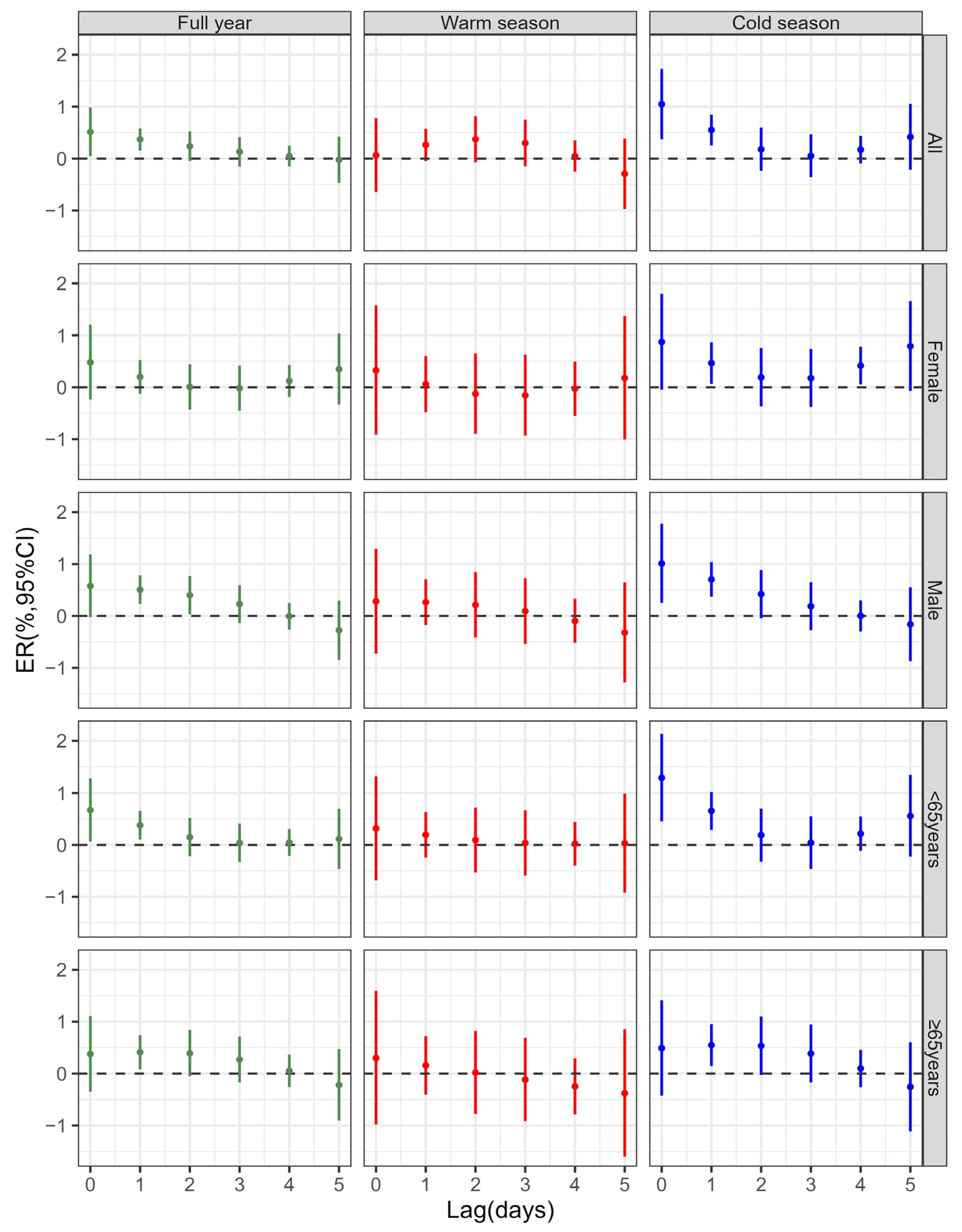
3.2. Effect of Air Pollutant Modified by Season
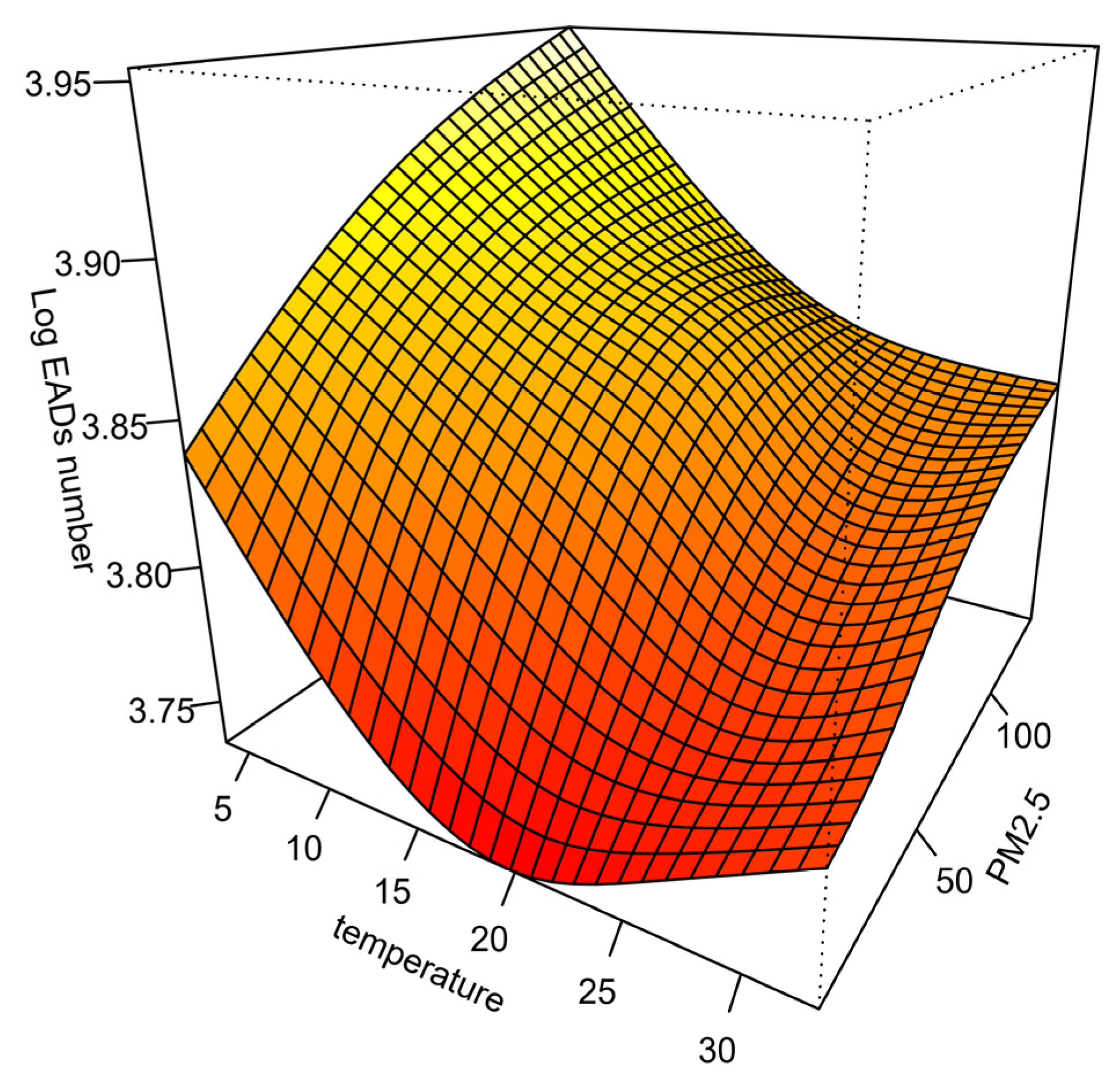
3.3. Effect of Air Pollutant Modified by Temperature
3.4. Sensitivity Analyses
4. Discussion
4.1. Association Between Air Pollutants and EADs
4.2. Air Pollution Effects Stratified by Season
4.3. Air Pollution Effects Stratified by Temperature
4.4. Vulnerable Subgroups
4.5. Potential Public Health Interventions
4.6. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- de Bont, J.; Jaganathan, S.; Dahlquist, M.; Persson, Å.; Stafoggia, M.; Ljungman, P. Ambient Air Pollution and Cardiovascular Diseases: An Umbrella Review of Systematic Reviews and Meta-Analyses. J. Intern. Med. 2022, 291, 779–800. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Chen, R.; Sera, F.; Vicedo-Cabrera, A.M.; Guo, Y.; Tong, S.; Coelho, M.S.Z.S.; Saldiva, P.H.N.; Lavigne, E.; Matus, P.; et al. Ambient Particulate Air Pollution and Daily Mortality in 652 Cities. N. Engl. J. Med. 2019, 381, 705–715. [Google Scholar] [CrossRef] [PubMed]
- Schraufnagel, D.E.; Balmes, J.R.; De Matteis, S.; Hoffman, B.; Kim, W.J.; Perez-Padilla, R.; Rice, M.; Sood, A.; Vanker, A.; Wuebbles, D.J. Health Benefits of Air Pollution Reduction. Ann. Am. Thorac. Soc. 2019, 16, 1478–1487. [Google Scholar] [CrossRef] [PubMed]
- Schwela, D. Air Pollution and Health in Urban Areas. Rev. Environ. Health 2000, 15, 13–42. [Google Scholar] [CrossRef]
- Khoshakhlagh, A.H.; Mohammadzadeh, M.; Gruszecka-Kosowska, A.; Oikonomou, E. Burden of Cardiovascular Disease Attributed to Air Pollution: A Systematic Review. Global Health 2024, 20, 37. [Google Scholar] [CrossRef] [PubMed]
- Crouse, D.L.; Peters, P.A.; Hystad, P.; Brook, J.R.; van Donkelaar, A.; Martin, R.V.; Villeneuve, P.J.; Jerrett, M.; Goldberg, M.S.; Pope, C.A.; et al. Ambient PM2.5, O3, and NO2 Exposures and Associations with Mortality over 16 Years of Follow-Up in the Canadian Census Health and Environment Cohort (CanCHEC). Environ. Health Perspect. 2015, 123, 1180–1186. [Google Scholar] [CrossRef] [PubMed]
- Karimi, B.; Moradzadeh, R.; Samadi, S. Air Pollution and COVID-19 Mortality and Hospitalization: An Ecological Study in Iran. Atmos. Pollut. Res. 2022, 13, 101463. [Google Scholar] [CrossRef] [PubMed]
- Orellano, P.; Reynoso, J.; Quaranta, N.; Bardach, A.; Ciapponi, A. Short-Term Exposure to Particulate Matter (PM10 and PM2.5), Nitrogen Dioxide (NO2), and Ozone (O3) and All-Cause and Cause-Specific Mortality: Systematic Review and Meta-Analysis. Environ. Int. 2020, 142, 105876. [Google Scholar] [CrossRef]
- Yao, M.; Wu, G.; Zhao, X.; Zhang, J. Estimating Health Burden and Economic Loss Attributable to Short-Term Exposure to Multiple Air Pollutants in China. Environ. Res. 2020, 183, 109184. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Yin, P.; Wang, L.; Liu, C.; Niu, Y.; Wang, W.; Jiang, Y.; Liu, Y.; Liu, J.; Qi, J.; et al. Association between Ambient Temperature and Mortality Risk and Burden: Time Series Study in 272 Main Chinese Cities. BMJ 2018, 363, k4306. [Google Scholar] [CrossRef]
- Healy, J.P.; Danesh Yazdi, M.; Wei, Y.; Qiu, X.; Shtein, A.; Dominici, F.; Shi, L.; Schwartz, J.D. Seasonal Temperature Variability and Mortality in the Medicare Population. Environ. Health Perspect. 2023, 131, 77002. [Google Scholar] [CrossRef] [PubMed]
- Nordio, F.; Zanobetti, A.; Colicino, E.; Kloog, I.; Schwartz, J. Changing Patterns of the Temperature–Mortality Association by Time and Location in the US, and Implications for Climate Change. Environ. Int. 2015, 81, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Fu, S.H.; Gasparrini, A.; Rodriguez, P.S.; Jha, P. Mortality Attributable to Hot and Cold Ambient Temperatures in India: A Nationally Representative Case-Crossover Study. PLoS Med. 2018, 15, e1002619. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Guo, M.; An, J.; Zhang, L.; Tan, P.; Tian, X.; Liu, L.; Zhao, Z.; Wang, X.; Liu, X.; et al. Associations between Ambient Air Pollution, Meteorology, and Daily Hospital Admissions for Ischemic Stroke: A Time-Stratified Case-Crossover Study in Beijing. Environ. Sci. Pollut. Res. 2022, 29, 53704–53717. [Google Scholar] [CrossRef]
- Li, Y.; Ma, Z.; Zheng, C.; Shang, Y. Ambient Temperature Enhanced Acute Cardiovascular-Respiratory Mortality Effects of PM2.5 in Beijing, China. Int. J. Biometeorol. 2015, 59, 1761–1770. [Google Scholar] [CrossRef]
- Stafoggia, M.; Schwartz, J.; Forastiere, F.; Perucci, C.A. SISTI Group Does Temperature Modify the Association between Air Pollution and Mortality? A Multicity Case-Crossover Analysis in Italy. Am. J. Epidemiol. 2008, 167, 1476–1485. [Google Scholar] [CrossRef] [PubMed]
- Chan, E.Y.; Goggins, W.B.; Yue, J.S.; Lee, P. Hospital Admissions as a Function of Temperature, Other Weather Phenomena and Pollution Levels in an Urban Setting in China. Bull. World Health Organ. 2013, 91, 576. [Google Scholar] [CrossRef] [PubMed]
- Rai, M.; Stafoggia, M.; de’Donato, F.; Scortichini, M.; Zafeiratou, S.; Vazquez Fernandez, L.; Zhang, S.; Katsouyanni, K.; Samoli, E.; Rao, S.; et al. Heat-Related Cardiorespiratory Mortality: Effect Modification by Air Pollution across 482 Cities from 24 Countries. Environ. Int. 2023, 174, 107825. [Google Scholar] [CrossRef] [PubMed]
- Duan, Y.; Liao, Y.; Li, H.; Yan, S.; Zhao, Z.; Yu, S.; Fu, Y.; Wang, Z.; Yin, P.; Cheng, J.; et al. Effect of Changes in Season and Temperature on Cardiovascular Mortality Associated with Nitrogen Dioxide Air Pollution in Shenzhen, China. Sci. Total Environ. 2019, 697, 134051. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Huang, S.; Tian, Y.; Ji, J.; Zhang, Y.; Hu, J.; Lv, Z.; Liu, N.; Wang, P.; Yin, P.; et al. Short-Term Exposure to Nitrogen Dioxide and Ischemic Stroke Incidence in Shenzhen, China: Modification Effects by Season and Temperature. Ecotoxicol. Environ. Saf. 2022, 239, 113644. [Google Scholar] [CrossRef] [PubMed]
- Peng, R.D.; Dominici, F.; Louis, T.A. Model Choice in Time Series Studies of Air Pollution and Mortality. J. R. Stat.Soc. Ser. A (Stat.Soc.) 2006, 169, 179–203. [Google Scholar] [CrossRef]
- Lu, F.; Zhou, L.; Xu, Y.; Zheng, T.; Guo, Y.; Wellenius, G.A.; Bassig, B.A.; Chen, X.; Wang, H.; Zheng, X. Short-Term Effects of Air Pollution on Daily Mortality and Years of Life Lost in Nanjing, China. Sci. Total Environ. 2015, 536, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Luo, K.; Li, R.; Wang, Z.; Zhang, R.; Xu, Q. Effect Modification of the Association between Temperature Variability and Daily Cardiovascular Mortality by Air Pollutants in Three Chinese Cities. Environ. Pollut. 2017, 230, 989–999. [Google Scholar] [CrossRef] [PubMed]
- Ren, C.; Williams, G.M.; Mengersen, K.; Morawska, L.; Tong, S. Does Temperature Modify Short-Term Effects of Ozone on Total Mortality in 60 Large Eastern US Communities? An Assessment Using the NMMAPS Data. Environ. Int. 2008, 34, 451–458. [Google Scholar] [CrossRef]
- Ren, C.; Tong, S. Temperature Modifies the Health Effects of Particulate Matter in Brisbane, Australia. Int. J. Biometeorol. 2006, 51, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Yu, I.T.; Qiu, H.; Wang, X.; Tian, L.; Tse, L.A. Synergy between Particles and Nitrogen Dioxide on Emergency Hospital Admissions for Cardiac Diseases in Hong Kong. Int. J. Cardiol. 2013, 168, 2831–2836. [Google Scholar] [CrossRef] [PubMed]
- Altman, D.G.; Bland, J.M. Interaction Revisited: The Difference between Two Estimates. BMJ 2003, 326, 219. [Google Scholar] [CrossRef]
- Ai, S.; Wang, C.; Qian, Z.M.; Cui, Y.; Liu, Y.; Acharya, B.K.; Sun, X.; Hinyard, L.; Jansson, D.R.; Qin, L.; et al. Hourly Associations between Ambient Air Pollution and Emergency Ambulance Calls in One Central Chinese City: Implications for Hourly Air Quality Standards. Sci. Total Environ. 2019, 696, 133956. [Google Scholar] [CrossRef] [PubMed]
- Michikawa, T.; Sasaki, J.; Yamazaki, S.; Takami, A.; Asakura, K.; Imamura, H.; Ueda, K.; Saito, S.; Hoshi, J.; Yoshino, A.; et al. A Case-Crossover Analysis of the Association between Exposure to Total PM2.5 and Its Chemical Components and Emergency Ambulance Dispatches in Tokyo. Environ. Sci. Technol. 2022, 56, 7319–7327. [Google Scholar] [CrossRef]
- You, X.; Cao, X.; Guo, Y.; Wang, D.; Qiu, W.; Zhou, C.; Zhou, M.; Chen, W.; Zhang, X. Associations between Short-Term PM2.5 Exposure and Daily Hospital Admissions for Circulatory System Diseases in Ganzhou, China: A Time Series Study. Front. Public. Health 2023, 11, 1134516. [Google Scholar] [CrossRef]
- Kramer, A.L.; Liu, J.; Li, L.; Connolly, R.; Barbato, M.; Zhu, Y. Environmental Justice Analysis of Wildfire-Related PM2.5 Exposure Using Low-Cost Sensors in California. Sci. Total Environ. 2023, 856, 159218. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Zhang, Y.; Chen, C.; Sun, Q.; Wang, Y.; Du, H.; Wang, J.; Zhong, Y.; Shi, W.; Li, T.; et al. Impact of Heavy PM2.5 Pollution Events on Mortality in 250 Chinese Counties. Environ. Sci. Technol. 2022, 56, 8299–8307. [Google Scholar] [CrossRef]
- Kim, S.; Lee, J.-T. Short-Term Exposure to PM10 and Cardiovascular Hospitalization in Persons with and without Disabilities: Invisible Population in Air Pollution Epidemiology. Sci. Total Environ. 2022, 848, 157717. [Google Scholar] [CrossRef] [PubMed]
- Feng, W.; Li, H.; Wang, S.; Van Halm-Lutterodt, N.; An, J.; Liu, Y.; Liu, M.; Wang, X.; Guo, X. Short-Term PM10 and Emergency Department Admissions for Selective Cardiovascular and Respiratory Diseases in Beijing, China. Sci. Total Environ. 2019, 657, 213–221. [Google Scholar] [CrossRef]
- Zhu, F.; Yu, H.; Fan, X.; Ding, Z.; Wang, Q.; Zhou, J. Particulate Air Pollution and Cardiovascular Disease Mortality in Jiangsu Province, China: A Time-Series Analysis between 2015 and 2021. Front Public Health 2023, 11, 1218479. [Google Scholar] [CrossRef]
- Manou-Stathopoulou, V.; Goodwin, C.D.; Patterson, T.; Redwood, S.R.; Marber, M.S.; Williams, R.P. The Effects of Cold and Exercise on the Cardiovascular System. Heart 2015, 101, 808–820. [Google Scholar] [CrossRef]
- Boonarkart, C.; Suptawiwat, O.; Sakorn, K.; Puthavathana, P.; Auewarakul, P. Exposure to Cold Impairs Interferon-Induced Antiviral Defense. Arch. Virol. 2017, 162, 2231–2237. [Google Scholar] [CrossRef] [PubMed]
- He, F.; Liao, B.; Pu, J.; Li, C.; Zheng, M.; Huang, L.; Zhou, Y.; Zhao, D.; Li, B.; Ran, P. Exposure to Ambient Particulate Matter Induced COPD in a Rat Model and a Description of the Underlying Mechanism. Sci. Rep. 2017, 7, 45666. [Google Scholar] [CrossRef] [PubMed]
- Juan, Y.; Haiqiao, W.; Xie, W.; Huaping, H.; Zhong, H.; Xiangdong, Z.; Kolosov, V.P.; Perelman, J.M. Cold-Inducible RNA-Binding Protein Mediates Airway Inflammation and Mucus Hypersecretion through a Post-Transcriptional Regulatory Mechanism under Cold Stress. Int. J. Biochem. Cell Biol. 2016, 78, 335–348. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Zhou, M.; Cai, Y.; Zhang, Y.; Pan, X. Does Temperature Enhance Acute Mortality Effects of Ambient Particle Pollution in Tianjin City, China. Sci. Total Environ. 2011, 409, 1811–1817. [Google Scholar] [CrossRef] [PubMed]
- Tian, L.; Liang, F.; Guo, Q.; Chen, S.; Xiao, S.; Wu, Z.; Jin, X.; Pan, X. The Effects of Interaction between Particulate Matter and Temperature on Mortality in Beijing, China. Environ. Sci. Process Impacts 2018, 20, 395–405. [Google Scholar] [CrossRef]
- Kysely, J.; Pokorna, L.; Kyncl, J.; Kriz, B. Excess Cardiovascular Mortality Associated with Cold Spells in the Czech Republic. BMC Public Health 2009, 9, 19. [Google Scholar] [CrossRef] [PubMed]
- Xu, Q.; Wang, S.; Guo, Y.; Wang, C.; Huang, F.; Li, X.; Gao, Q.; Wu, L.; Tao, L.; Guo, J.; et al. Acute Exposure to Fine Particulate Matter and Cardiovascular Hospital Emergency Room Visits in Beijing, China. Environ. Pollut. 2017, 220, 317–327. [Google Scholar] [CrossRef]
- Yang, Q.; Chen, Y.; Shi, Y.; Burnett, R.T.; McGrail, K.M.; Krewski, D. Association between Ozone and Respiratory Admissions among Children and the Elderly in Vancouver, Canada. Inhal. Toxicol. 2003, 15, 1297–1308. [Google Scholar] [CrossRef] [PubMed]

| Variables | Mean | SD | Percentile | ||||
|---|---|---|---|---|---|---|---|
| Min | P25 | Median | P75 | Max | |||
| Temperature (°C) | |||||||
| Full year | 23.56 | 5.31 | 3.50 | 19.60 | 24.70 | 28.10 | 33.00 |
| Cold season (Nov.–Apr.) | 18.30 | 4.03 | 3.50 | 16.60 | 19.60 | 22.40 | 28.00 |
| Warm season (May–Oct.) | 27.76 | 2.09 | 18.80 | 26.50 | 28.10 | 29.40 | 33.00 |
| Low temperature | 18.10 | 3.76 | 3.50 | 16.60 | 19.60 | 22.20 | 24.60 |
| High temperature | 27.97 | 1.68 | 24.70 | 26.60 | 28.10 | 29.40 | 33.00 |
| Relative humidity (%) | |||||||
| Full year | 75.72 | 12.88 | 19.00 | 70.00 | 78.00 | 84.00 | 100.00 |
| Cold season (Nov.–Apr.) | 72.64 | 14.55 | 19.00 | 65.00 | 75.00 | 83.00 | 100.00 |
| Warm season (May–Oct.) | 78.75 | 10.12 | 34.00 | 73.00 | 80.00 | 86.00 | 100.00 |
| Low temperature (<Median) | 72.09 | 14.98 | 19.00 | 64.00 | 74.50 | 83.00 | 100.00 |
| High temperature (≥Median) | 79.29 | 9.07 | 39.00 | 74.00 | 80.00 | 85.00 | 100.00 |
| PM10 (μg/m3) | |||||||
| Full year | 61.02 | 44.65 | 5.55 | 30.00 | 49.13 | 74.75 | 336.83 |
| Cold season (Nov.–Apr.) | 73.36 | 48.45 | 5.55 | 40.27 | 59.41 | 91.00 | 336.83 |
| Warm season (May–Oct.) | 48.86 | 36.72 | 8.70 | 23.78 | 37.00 | 61.08 | 266.00 |
| Low temperature (<Median) | 73.24 | 48.72 | 5.55 | 40.65 | 59.00 | 88.93 | 336.83 |
| High temperature (≥Median) | 48.95 | 36.42 | 8.70 | 23.86 | 36.54 | 62.45 | 253.57 |
| PM2.5 (μg/m3) | |||||||
| Full year | 28.63 | 17.76 | 3.91 | 15.40 | 24.89 | 37.55 | 135.60 |
| Cold season (Nov.–Apr.) | 35.99 | 18.15 | 4.00 | 23.40 | 32.36 | 44.00 | 135.60 |
| Warm season (May–Oct.) | 21.38 | 14.00 | 3.91 | 11.43 | 17.05 | 27.35 | 101.00 |
| Low temperature | 36.40 | 18.40 | 4.00 | 23.45 | 32.60 | 44.50 | 135.60 |
| High temperature | 20.96 | 13.21 | 3.91 | 11.43 | 16.86 | 27.00 | 101.00 |
| NO2 (μg/m3) | |||||||
| Full year | 34.49 | 16.15 | 6.73 | 23.75 | 31.44 | 41.29 | 139.40 |
| Cold season (Nov.–Apr.) | 39.43 | 18.48 | 9.55 | 27.00 | 35.23 | 48.00 | 139.40 |
| Warm season (May–Oct.) | 29.62 | 11.57 | 6.73 | 21.23 | 27.82 | 36.00 | 83.80 |
| Low temperature (<Median) | 39.25 | 18.57 | 9.55 | 26.45 | 35.25 | 48.00 | 139.40 |
| High temperature (≥Median) | 29.79 | 11.56 | 6.73 | 21.45 | 28.00 | 36.00 | 83.80 |
| SO2 (μg/m3) | |||||||
| Full year | 8.21 | 3.75 | 3.09 | 5.86 | 7.36 | 9.50 | 54.20 |
| Cold season (Nov.–Apr.) | 8.78 | 4.45 | 3.09 | 6.00 | 7.60 | 10.17 | 54.20 |
| Warm season (May–Oct.) | 7.64 | 2.78 | 3.20 | 5.73 | 7.17 | 8.86 | 28.80 |
| Low temperature (<Median) | 8.77 | 4.48 | 3.09 | 6.00 | 7.50 | 10.17 | 54.20 |
| High temperature (≥Median) | 7.66 | 2.74 | 3.20 | 5.73 | 7.29 | 8.86 | 28.80 |
| Emergency ambulance dispatches | |||||||
| All-cause | |||||||
| Full year | 398.31 | 86.56 | 173.00 | 335.00 | 390.00 | 457.00 | 776.00 |
| Cold season (Nov.–Apr.) | 383.06 | 91.67 | 173.00 | 316.00 | 373.00 | 447.00 | 753.00 |
| Warm season (May–Oct.) | 413.40 | 78.35 | 236.00 | 351.00 | 404.00 | 470.00 | 776.00 |
| Low temperature (<Median) | 382.02 | 92.35 | 173.00 | 313.00 | 372.50 | 445.00 | 753.00 |
| High temperature (≥Median) | 414.47 | 77.09 | 237.00 | 353.00 | 405.00 | 471.00 | 776.00 |
| Circulatory system disease | |||||||
| Full year | 39.47 | 10.10 | 15.00 | 32.00 | 39.00 | 46.00 | 84.00 |
| Cold season (Nov.–Apr.) | 41.16 | 10.51 | 15.00 | 34.00 | 40.00 | 48.00 | 84.00 |
| Warm season (May–Oct.) | 37.81 | 9.39 | 15.00 | 31.00 | 37.00 | 44.00 | 73.00 |
| Low temperature (<Median) | 41.15 | 10.44 | 15.00 | 34.00 | 41.00 | 48.00 | 84.00 |
| High temperature (≥Median) | 37.82 | 9.47 | 15.00 | 31.00 | 37.00 | 44.00 | 77.00 |
| Group | Percentage Change in EADs(95%CI) b | ||||
|---|---|---|---|---|---|
| Lag0–1 | Lag0–2 | Lag0–3 | Lag0–4 | Lag0–5 | |
| Full year | |||||
| All a | 0.88 (0.26, 1.51) | 1.12 (0.47, 1.78) | 1.26 (0.54, 1.97) | 1.30 (0.56, 2.05) | 1.28 (0.48, 2.08) |
| Male | 1.08 (0.28, 1.89) | 1.49 (0.65, 2.33) | 1.72 (0.80, 2.64) | 1.71 (0.76, 2.67) | 1.43 (0.41, 2.46) |
| Female | 0.68 (−0.27, 1.64) | 0.68 (−0.31, 1.69) | 0.66 (−0.42, 1.76) | 0.79 (−0.34, 1.92) | 1.14 (−0.09, 2.37) |
| <65 years | 1.05 (0.24, 1.87) | 1.20 (0.36, 2.05) | 1.24 (0.32, 2.17) | 1.28 (0.33, 2.25) | 1.40 (0.36, 2.45) |
| ≥65 years | 0.79 (−0.18, 1.77) | 1.18 (0.17, 2.20) | 1.46 (0.35, 2.57) | 1.51 (0.36, 2.66) | 1.28 (0.05, 2.54) |
| Cold season | |||||
| All | 1.60 (0.71, 2.50) | 1.78 (0.88, 2.69) | 1.83 (0.86, 2.82) | 2.01 (1.04, 2.98) | 2.43 (1.47, 3.40) † |
| Male | 1.72 (0.72, 2.72) | 2.15 (1.13, 3.17) | 2.34 (1.24, 3.44) | 2.33 (1.26, 3.42) | 2.17 (1.10, 3.25) † |
| Female | 1.34 (0.14, 2.56) | 1.53 (0.31, 2.77) | 1.71 (0.39, 3.04) | 2.13 (0.83, 3.45) † | 2.94 (1.63, 4.26) † |
| <65 years | 1.96 (0.86, 3.06) | 2.15 (1.03, 3.27) | 2.19 (0.99, 3.40) | 2.41 (1.22, 3.61) † | 2.98 (1.79, 4.18) † |
| ≥65 years | 1.04 (−0.16, 2.25) | 1.58 (0.36, 2.82) | 1.97 (0.65, 3.31) | 2.07 (0.77, 3.39) | 1.81 (0.52, 3.12) |
| Warm season | |||||
| All | 0.33 (−0.60, 1.26) | 0.70 (−0.25, 1.65) | 1.00 (−0.02, 2.03) | 1.02 (−0.04, 2.06) | 0.75 (−0.25, 1.76) |
| Male | 0.54 (−0.76, 1.87) | 0.76 (−0.57, 2.10) | 0.85 (−0.57, 2.30) | 0.75 (−0.64, 2.16) | 0.43 (−0.92, 1.80) |
| Female | 0.38 (−1.22, 2.02) | 0.26 (−1.36, 1.90) | 0.10 (−1.64, 1.87) | 0.07 (−1.63, 1.80) | 0.24 (−1.42, 1.94) |
| <65 years | 0.51 (−0.79, 1.82) | 0.60 (−0.70, 1.93) | 0.64 (−0.77, 2.07) | 0.66 (−0.71, 2.06) | 0.69 (−0.66, 2.05) |
| ≥65 years | 0.46 (−1.21, 2.15) | 0.47 (−1.21, 2.19) | 0.35 (−1.45, 2.19) | 0.10 (−1.66, 1.90) | −0.27 (−1.99, 1.47) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cui, X.; Tian, Y.; Yin, Z.; Huang, S.; Yin, P. The Impact of Ambient PM2.5 on Emergency Ambulance Dispatches Due to Circulatory System Disease Modified by Season and Temperature in Shenzhen, China. Atmosphere 2025, 16, 198. https://doi.org/10.3390/atmos16020198
Cui X, Tian Y, Yin Z, Huang S, Yin P. The Impact of Ambient PM2.5 on Emergency Ambulance Dispatches Due to Circulatory System Disease Modified by Season and Temperature in Shenzhen, China. Atmosphere. 2025; 16(2):198. https://doi.org/10.3390/atmos16020198
Chicago/Turabian StyleCui, Xuanye, Yuchen Tian, Ziming Yin, Suli Huang, and Ping Yin. 2025. "The Impact of Ambient PM2.5 on Emergency Ambulance Dispatches Due to Circulatory System Disease Modified by Season and Temperature in Shenzhen, China" Atmosphere 16, no. 2: 198. https://doi.org/10.3390/atmos16020198
APA StyleCui, X., Tian, Y., Yin, Z., Huang, S., & Yin, P. (2025). The Impact of Ambient PM2.5 on Emergency Ambulance Dispatches Due to Circulatory System Disease Modified by Season and Temperature in Shenzhen, China. Atmosphere, 16(2), 198. https://doi.org/10.3390/atmos16020198






