COVID-19 Lockdown Air Pollution Reduction: Did It Impact the Number of COPD Hospitalizations?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Time Frame
2.2. Study Population
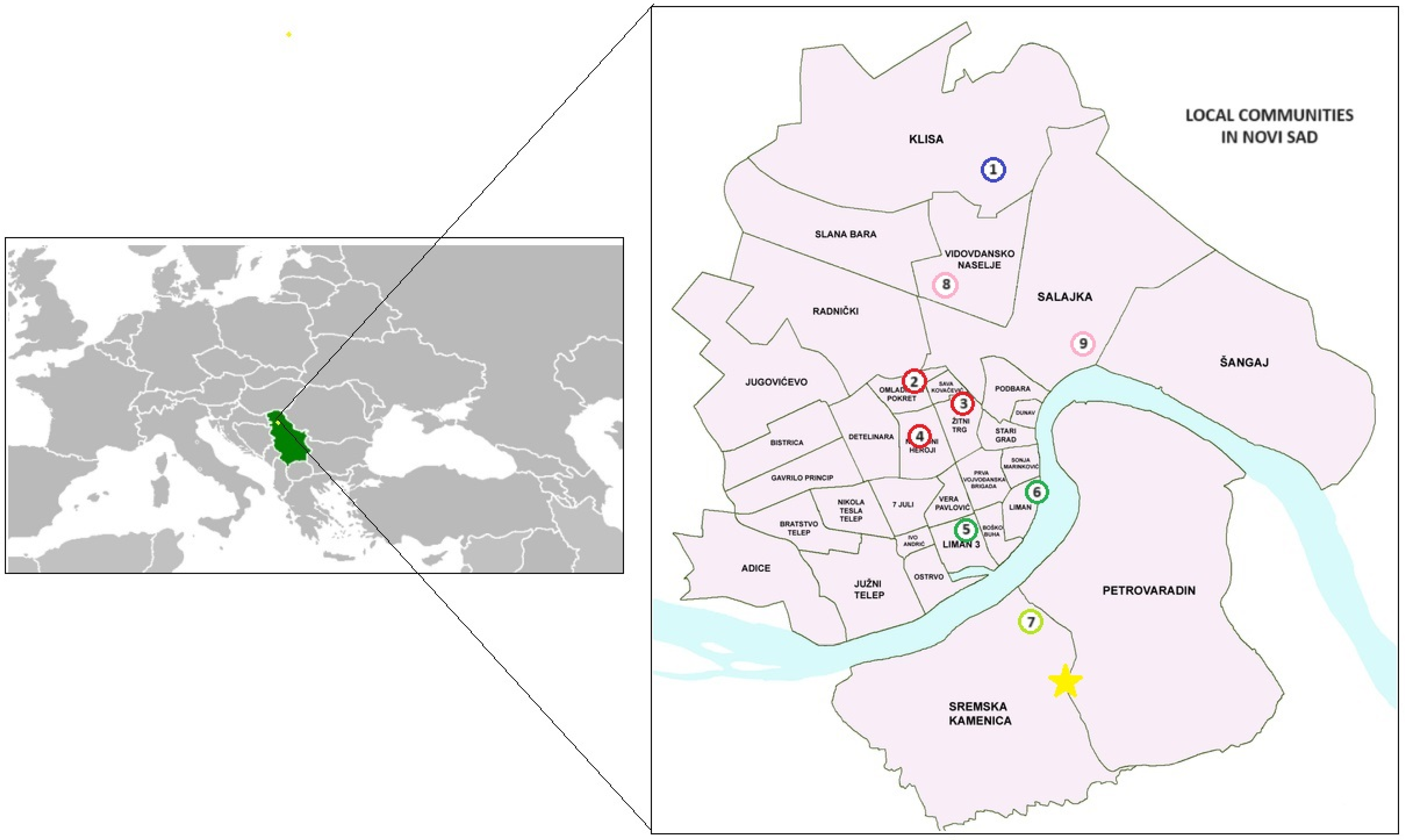
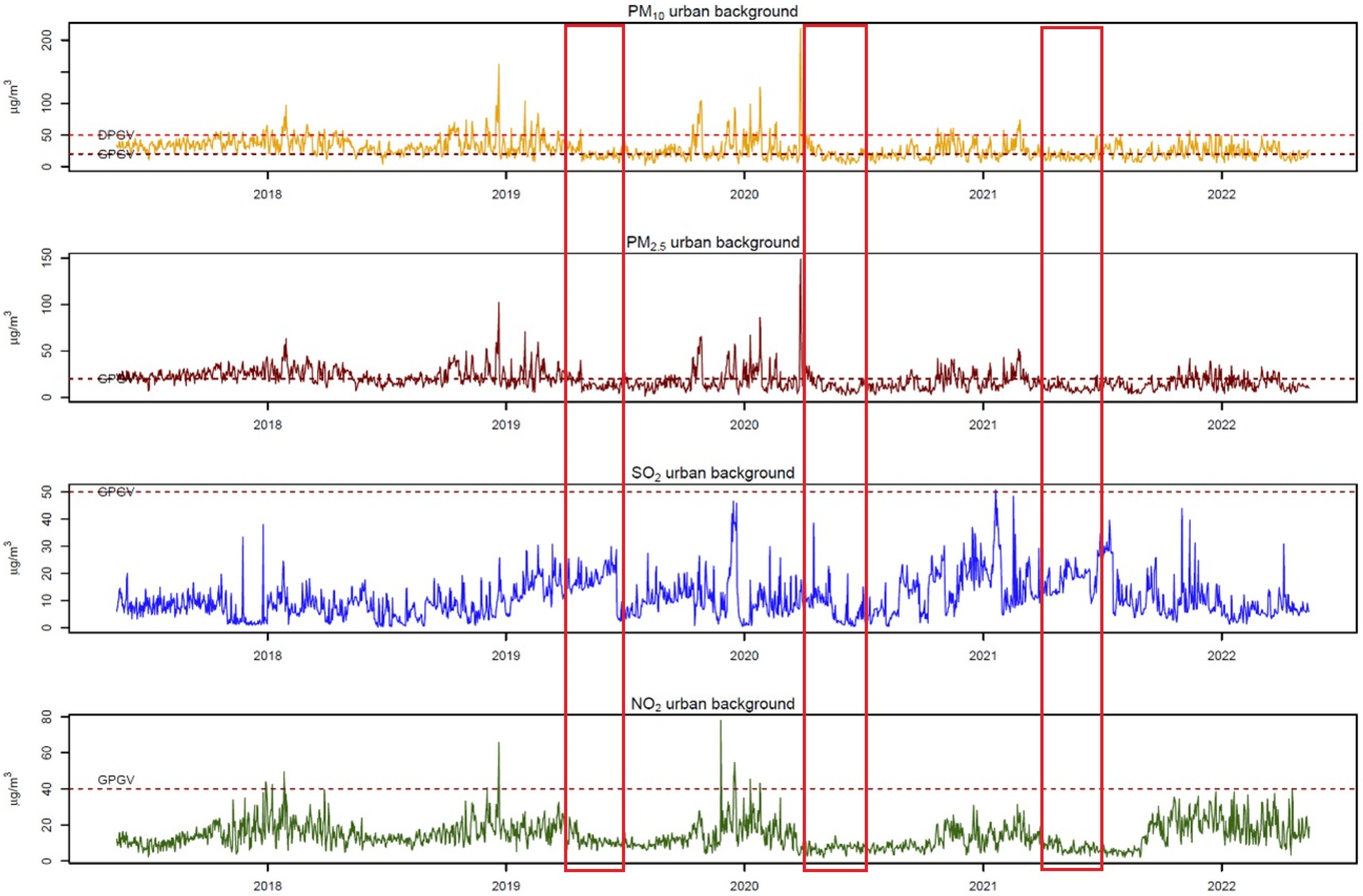
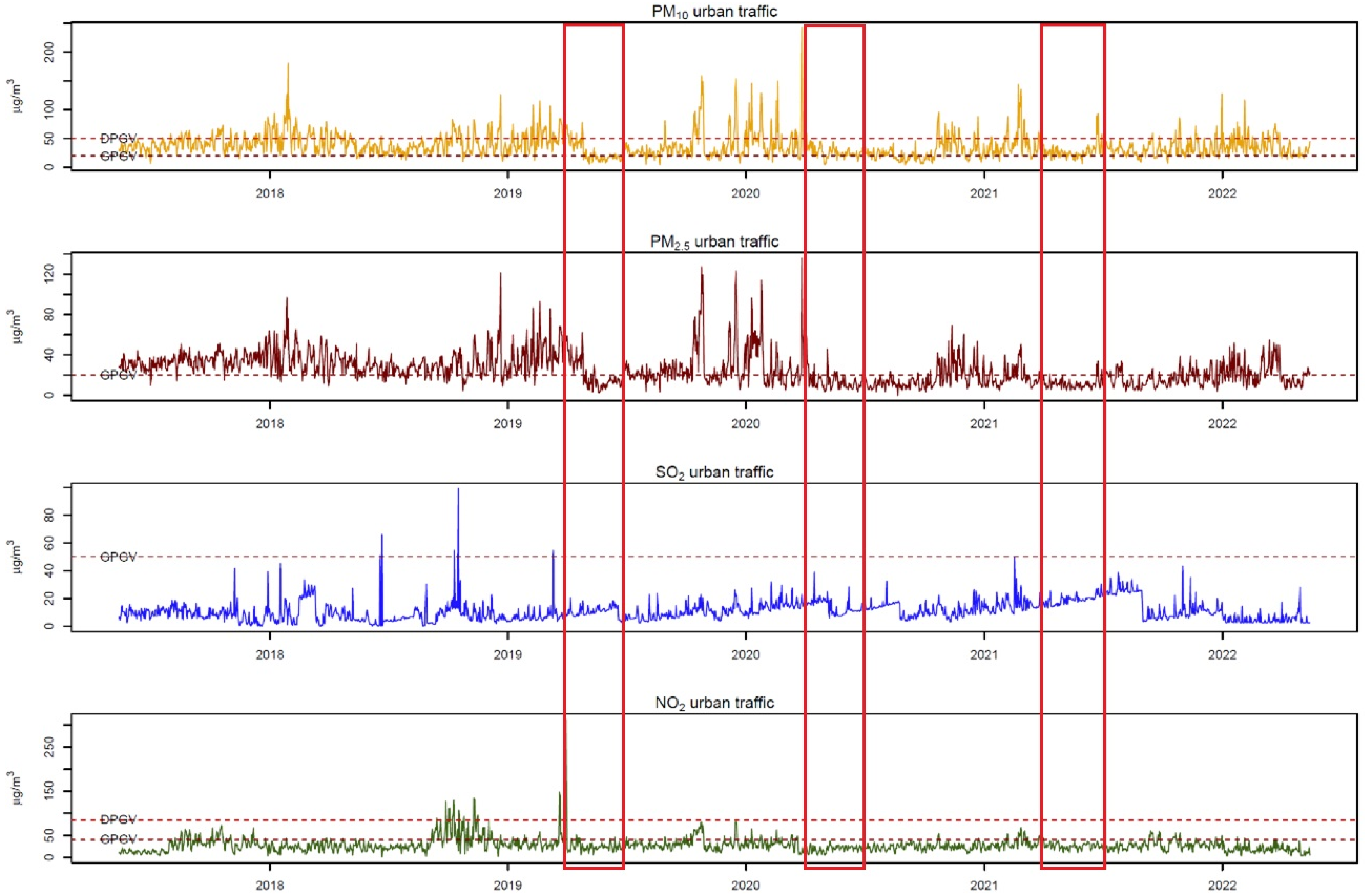
2.3. Study Location and Air Pollution Data
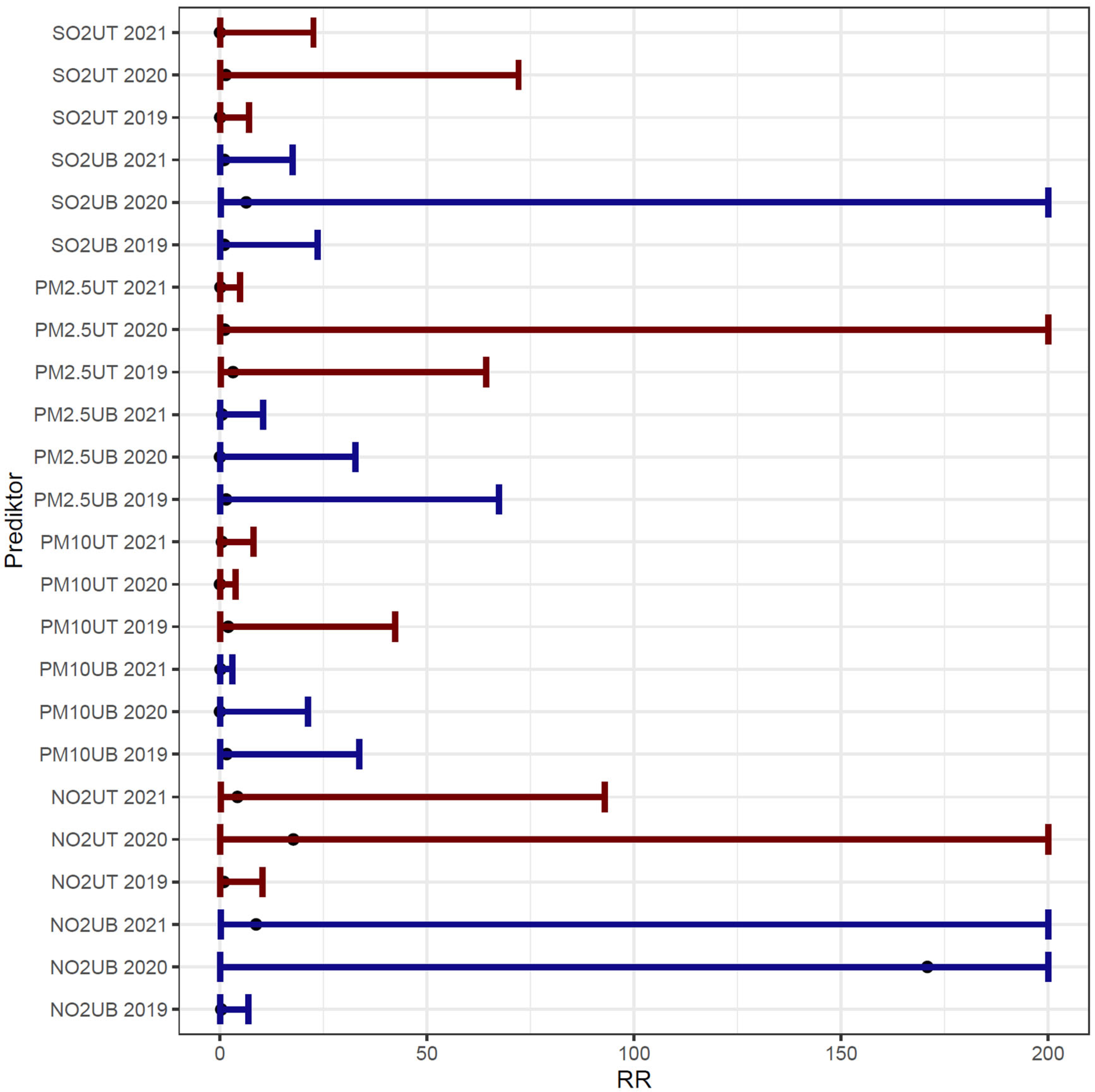
2.4. Statistical Analysis
3. Results
Descriptive Statistics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jevtic, M.; Matkovic, V.; van den Hazel, P.; Bouland, C. Environment-lockdown, air pollution and related diseases: Could we learn something and make it last? Eur. J. Public Health 2021, 31 (Suppl. S4), iv36–iv39. [Google Scholar] [CrossRef] [PubMed]
- Primorac, D.; Roberts, R.J. The impact of COVID-19 on sustainable development. Croat. Med. J. 2022, 63, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; Liu, Y.; Ya, B.; He, J.; Leng, T.; Sun, Y.; Xin, Q. Latest Effective Measures to Combat COVID-19: A Review. Iran. J. Public Health 2021, 50, 640–648. [Google Scholar] [CrossRef] [PubMed]
- Kumari, P.; Toshniwal, D. Impact of lockdown measures during COVID-19 on air quality- A case study of India. Int. J. Environ. Health Res. 2022, 32, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Wetchayont, P. Investigation on the impacts of COVID-19 lockdown and influencing factors on air quality in greater Bangkok, Thailand. Adv. Meteorol. 2021, 2021, 6697707. [Google Scholar] [CrossRef]
- Mostafa, M.K.; Gamal, G.; Wafiq, A. The impact of COVID 19 on air pollution levels and other environmental indicators—A case study of Egypt. J. Environ. Manag. 2021, 277, 111496. [Google Scholar] [CrossRef] [PubMed]
- Yumin, L.; Shiyuan, L.; Ling, H.; Ziyi, L.; Yonghui, Z.; Li, L.; Yangjun, W.; Kangjuan, L. The casual effects of COVID-19 lockdown on air quality and short-term health impacts in China. Environ. Pollut. 2021, 290, 117988. [Google Scholar] [CrossRef] [PubMed]
- Dragic, N.; Bijelovic, S.; Jevtic, M.; Velicki, R.; Radic, I. Short-term health effects of air quality changes during the COVID-19 pandemic in the City of Novi Sad, the Republic of Serbia. Int. J. Occup. Med. Environ. Health 2021, 34, 223–237. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Wang, M.; Huang, C.; Kinney, P.L.; Anastas, P.T. Air pollution reduction and mortality benefit during the COVID-19 outbreak in China. Lancet Planet. Health 2020, 4, e210–e212. [Google Scholar] [CrossRef]
- Khomsi, K.; Najmi, H.; Amghar, H.; Chelhaoui, Y.; Souhaili, Z. COVID-19 national lockdown in morocco: Impacts on air quality and public health. One Health 2021, 11, 100200. [Google Scholar] [CrossRef]
- Mitreska Jovanovska, E.; Batz, V.; Lameski, P.; Zdravevski, E.; Herzog, M.A.; Trajkovik, V. Methods for Urban Air Pollution Measurement and Forecasting: Challenges, Opportunities, and Solutions. Atmosphere 2023, 14, 1441. [Google Scholar] [CrossRef]
- Javorac, J.; Živanović, D.; Ilić, M.; Lečić, S.K.; Milenković, A.; Dragić, N.; Bijelović, S.; Savić, N.; Vereš, K.T.; Smuđa, M.; et al. The Influence of Air Pollution on Non-Infectious Hospitalizations for Severe Acute Exacerbations of Chronic Obstructive Pulmonary Disease: A Time-Series from Serbia. Atmosphere 2023, 14, 730. [Google Scholar] [CrossRef]
- Evangelopoulos, D.; Chatzidiakou, L.; Walton, H.; Katsouyanni, K.; Kelly, F.J.; Quint, J.K.; Jones, R.L.; Barratt, B. Personal exposure to air pollution and respiratory health of COPD patients in London. Eur. Respir. J. 2021, 58, 2003432. [Google Scholar] [CrossRef] [PubMed]
- Benaissa, F.; Alkama, R.; Annesi-Maesano, I. Assessment of Air Pollution Impacts on Population Health in Bejaia City, Northern Algeria. Iran. J. Public Health 2014, 43, 1221–1228. [Google Scholar] [PubMed]
- Liang, L.; Cai, Y.; Barratt, B.; Lyu, B.; Chan, Q.; Hansell, A.L.; Xie, W.; Zhang, D.; Kelly, F.J.; Tong, Z. Associations between daily air quality and hospitalisations for acute exacerbation of chronic obstructive pulmonary disease in Beijing, 2013–2017: An ecological analysis. Lancet Planet Health 2019, 3, e270–e279. [Google Scholar] [CrossRef] [PubMed]
- Yan, P.; Liu, P.; Lin, R.; Xiao, K.; Xie, S.; Wang, K.; Zhang, Y.; He, X.; Zhao, S.; Zhang, X.; et al. Effect of ambient air quality on exacerbation of COPD in patients and its potential mechanism. Int. J. Chronic Obstr. Pulm. Dis. 2019, 14, 1517–1526. [Google Scholar] [CrossRef] [PubMed]
- Burney, P.G.; Patel, J.; Newson, R.; Minelli, C.; Naghavi, M. Global and regional trends in COPD mortality, 1990–2010. Eur. Respir. J. 2015, 45, 1239–1247. [Google Scholar] [CrossRef] [PubMed]
- Jung, Y.J.; Kim, E.J.; Heo, J.Y.; Choi, Y.H.; Kim, D.J.; Ha, K.H. Short-Term Air Pollution Exposure and Risk of Acute Exacerbation of Chronic Obstructive Pulmonary Disease in Korea: A National Time-Stratified Case-Crossover Study. Int. J. Environ. Res. Public Health 2022, 19, 2823. [Google Scholar] [CrossRef] [PubMed]
- Dragić, N. Impact of Ambient Suspended Particles “PM2.5” on Mortality, Cardiovascular and Respiratory Morbidity of Adults in the City of Novi Sad. Ph.D. Thesis, University of Novi Sad, Faculty of Medicine, Novi Sad, Serbia, 2019. [Google Scholar]
- Gradska Uprava za Zaštitu Životne Sredine. Available online: https://environovisad.rs/laravel-filemanager/files/shares/%D0%94%D0%BE%D0%BA%D1%83%D0%BC%D0%B5%D0%BD%D1%82%D0%B8/Program%20kontrole%20kvaliteta%20vazduha%20na%20teritoriji%20grada%20Novog%20Sada%20u%202023.%20i%202024.%20godini.pdf (accessed on 1 May 2024).
- Gasparrini, A. Distributed Lag Linear and Non-Linear Models in R: The Package dlnm. J. Stat. Softw. 2011, 43, 1–20. [Google Scholar] [CrossRef]
- Belis, C.; Djatkov, D.; Lettieri, T.; Jones, A.; Wojda, P.; Banja, M.; Muntean, M.; Paunovic, M.; Niegowska, M.Z.; Marinov, D.; et al. Status of Environment and Climate in the Western Balkans: Benchmarking the Accession Process Progress on Environment; Publications Office of the European Union: Luxembourg, 2022. [Google Scholar]
- Muhammad, S.; Long, X.; Salman, M. COVID-19 pandemic and environmental pollution: A blessing in disguise? Sci. Total Environ. 2020, 728, 138820. [Google Scholar] [CrossRef]
- Berman, J.D.; Ebisu, K. Changes in U.S. air pollution during the COVID-19 pandemic. Sci. Total Environ. 2020, 739, 139864. [Google Scholar] [CrossRef]
- Ropkins, K.; Tate, J.E. Early observations on the impact of the COVID-19 lockdown on air quality trends across the UK. Sci. Total Environ. 2021, 754, 142374. [Google Scholar] [CrossRef] [PubMed]
- Montiel-Lopez, F.; Rodríguez-Ramírez, D.; Cassou-Martínez, M.; Miranda-Márquez, M.C.; González-González, C.; Sansores, R.H.; Mayar-Maya, M.E.; Pérez-Padilla, R.; Robles-Hernández, R.E.; Thirion-Romero, I.; et al. Air quality in Mexico City during the COVID-19 lockdown possibly decreased COPD exacerbations. ERJ Open Res. 2022, 8, 00183–02022. [Google Scholar] [CrossRef] [PubMed]
- Vultaggio, M.; Varrica, D.; Alaimo, M.G. Impact on Air Quality of the COVID-19 Lockdown in the Urban Area of Palermo (Italy). Int. J. Environ. Res. Public Health 2020, 17, 7375. [Google Scholar] [CrossRef] [PubMed]
- Kerimray, A.; Baimatova, N.; Ibragimova, O.P.; Bukenov, B.; Kenessov, B.; Plotitsyn, P.; Karaca, F. Assessing air quality changes in large cities during COVID-19 lockdowns: The impacts of traffic-free urban conditions in Almaty, Kazakhstan. Sci. Total Environ. 2020, 730, 139179. [Google Scholar] [CrossRef] [PubMed]
- Kyriakopoulos, C.; Gogali, A.; Exarchos, K.; Potonos, D.; Tatsis, K.; Apollonatou, V.; Loukides, S.; Papiris, S.; Sigala, I.; Katsaounou, P.; et al. Reduction in Hospitalizations for Respiratory Diseases during the First COVID-19 Wave in Greece. Respiration 2021, 100, 588–593. [Google Scholar] [CrossRef] [PubMed]
- Sarc, I.; Dolinar, A.L.; Morgan, T.; Sambt, J.; Ziherl, K.; Gavric, D.; Selb, J.; Rozman, A.; Bonca, P.D. Mortality, seasonal variation, and susceptibility to acute exacerbation of COPD in the pandemic year: A nationwide population study. Ther. Adv. Respir. Dis. 2022, 16, 17534666221081047. [Google Scholar] [CrossRef] [PubMed]
- Chan, K.P.F.; Ma, T.F.; Kwok, W.C.; Leung, J.K.C.; Chiang, K.Y.; Ho, J.C.M.; Lam, D.C.L.; Tam, T.C.C.; Ip, M.S.M.; Ho, P.L. Significant reduction in hospital admissions for acute exacerbation of chronic obstructive pulmonary disease in Hong Kong during coronavirus disease 2019 pandemic. Respir. Med. 2020, 171, 106085. [Google Scholar] [CrossRef] [PubMed]
- Alsallakh, M.A.; Sivakumaran, S.; Kennedy, S.; Vasileiou, E.; Lyons, R.A.; Robertson, C.; Sheikh, A.; Davies, G.A.; EAVE II Collaborators. Impact of COVID-19 lockdown on the incidence and mortality of acute exacerbations of chronic obstructive pulmonary disease: National interrupted time series analyses for Scotland and Wales. BMC Med. 2021, 19, 124. [Google Scholar] [CrossRef]
- Tan, J.Y.; Conceicao, E.P.; Wee, L.E.; Sim, X.Y.J.; Venkatachalam, I. COVID-19 public health measures: A reduction in hospital admissions for COPD exacerbations. Thorax 2021, 76, 512–513. [Google Scholar] [CrossRef]
- Pappe, E.; Hammerich, R.; Saccomanno, J.; Sgarbossa, T.; Pohrt, A.; Schmidt, B.; Grah, C.; Eisenmann, S.; Holland, A.; Eggeling, S.; et al. Impact of COVID-19 on Hospital Admissions, Health Status, and Behavioral Changes of Patients with COPD. Chronic Obstr. Pulm. Dis. 2023, 10, 211–223. [Google Scholar] [PubMed]
- Ilić, M.; Javorac, J.; Milenković, A.; Živanović, D.; Miljković, D.; Lečić, S.K.; Savić, N.; Vereš, K.T.; Kovačević, D.; Vujičić, E.; et al. Home-Based Spirometry in Patients with Interstitial Lung Diseases: A RealLife Pilot “FACT” Study from Serbia. J. Pers. Med. 2023, 13, 793. [Google Scholar] [CrossRef]
- Docherty, A.B.; Harrison, E.M.; Green, C.A.; Hardwick, H.E.; Pius, R.; Norman, L.; Holden, K.A.; Read, J.M.; Dondelinger, F.; Carson, G.; et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: Prospective observational cohort study. BMJ 2020, 369, m1985. [Google Scholar] [CrossRef]
- Poucineau, J.; Delory, T.; Lapidus, N.; Hejblum, G.; Chouaïd, C.; Le Cœur, S.; Khlat, M. Hospital admissions and mortality for acute exacerbations of COPD during the COVID-19 pandemic: A nationwide study in France. Front. Med. (Lausanne) 2022, 9, 995016. [Google Scholar] [CrossRef]
- Quintyne, K.I.; Kelly, C.; Sheridan, A.; Kenny, P.; O’Dwyer, M. COVID-19 transport restrictions in Ireland: Impact on air quality and respiratory hospital admissions. Public Health 2021, 198, 156–160. [Google Scholar] [CrossRef]
- Kelly, C.; Kenny, P.; O’Dwyer, M.; Quintyne, K.I. Ambient air pollutant concentrations and asthma-related hospital admissions during COVID-19 transport restrictions. Public Health 2022, 211, 66–71. [Google Scholar] [CrossRef]
- Aix, M.L.; Petit, P.; Bicout, D.J. Air pollution and health impacts during the COVID-19 lockdowns in Grenoble, France. Environ. Pollut. 2022, 303, 119134. [Google Scholar] [CrossRef]
- Anbari, K.; Sicard, P.; Omidi Khaniabadi, Y.; Raja Naqvi, H.; Rashidi, R. Assessing the effect of COVID-19 pandemic on air quality change and human health outcomes in a capital city, southwestern Iran. Int. J. Environ. Health Res. 2023, 33, 1716–1727. [Google Scholar] [CrossRef] [PubMed]
- Ghobakhloo, S.; Khoshakhlagh, A.H.; Mostafaii, G.R.; Chuang, K.J.; Gruszecka-Kosowska, A.; Hosseinnia, P. Critical air pollutant assessments and health effects attributed to PM2.5 during and after COVID-19 lockdowns in Iran: Application of AirQ+ models. Front. Public Health 2023, 11, 1120694. [Google Scholar] [CrossRef] [PubMed]
- Ling, C.; Li, Y. Substantial Changes of Gaseous Pollutants and Health Effects During the COVID-19 Lockdown Period Across China. Geohealth 2021, 5, e2021GH000408. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Liu, Z.; Li, H.; Wang, Y.; Li, Y.; Zhu, Y.; Ooi, M.C.G.; An, J.; Shang, Y.; Zhang, D.; et al. The Silver Lining of COVID-19: Estimation of Short-Term Health Impacts Due to Lockdown in the Yangtze River Delta Region, China. Geohealth 2020, 4, e2020GH000272. [Google Scholar] [CrossRef] [PubMed]
- Ko, F.W.S.; Lau, L.H.S.; Ng, S.S.; Yip, T.C.F.; Wong, G.L.H.; Chan, K.P.; Chan, T.O.; Hui, D.S.C. Respiratory admissions before and during the COVID-19 pandemic with mediation analysis of air pollutants, mask-wearing and influenza rates. Respirology 2023, 28, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Sigala, I.; Giannakas, T.; Giannakoulis, V.G.; Zervas, E.; Brinia, A.; Gianiou, N.; Asimakos, A.; Dima, E.; Kalomenidis, I.; Katsaounou, P. Effect of COVID-19-Related Lockdown οn Hospital Admissions for Asthma and COPD Exacerbations: Associations with Air Pollution and Patient Characteristics. J. Pers. Med. 2021, 11, 867. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Baumgartner, J.; Harper, S.; Zhang, X.; Sternbach, T.; Barrington-Leigh, C.; Brehmer, C.; Robinson, B.; Shen, G.; Zhang, Y.; et al. Field measurements of indoor and community air quality in rural Beijing before, during, and after the COVID-19 lockdown. Indoor Air 2022, 32, e13095. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhao, B.; Jiang, Y.; Xing, J.; Sahu, S.K.; Zheng, H.; Ding, D.; Cao, S.; Han, L.; Yan, C.; et al. Non-negligible contributions to human health from increased household air pollution exposure during the COVID-19 lockdown in China. Environ. Int. 2022, 158, 106918. [Google Scholar] [CrossRef] [PubMed]
| Year | AECOPD Hospitalizations | ||
|---|---|---|---|
| Non-Infectious | Infectious | Total | |
| 2019 | 49 | 72 | 121 |
| 2020 (lockdown) | 22 | 23 | 45 |
| 2021 | 41 | 45 | 86 |
| Air Pollutant | March–June | p a 2019 vs. 2020 | p a 2020 vs. 2021 | ||
|---|---|---|---|---|---|
| 2019 | 2020 | 2021 | |||
| PM10(UB) (μm/m3) | 24.64 | 22.86 | 18.25 | 0.08540 | 0.02672 * |
| PM10(UT) (μm/m3) | 34.03 | 31.71 | 30.30 | 0.17960 | 0.30698 |
| PM2.5(UB) (μm/m3) | 17.00 | 15.58 | 12.12 | 0.08967 | 0.01672 * |
| PM2.5(UT) (μm/m3) | 26.86 | 16.85 | 12.46 | <0.00001 * | 0.00162 * |
| SO2(UB) (μm/m3) | 16.58 | 8.14 | 17.25 | <0.00001 * | <0.00001 * |
| SO2(UT) (μm/m3) | 10.31 | 14.58 | 18.12 | <0.00001 * | <0.00001 * |
| NO2(UB) (μm/m3) | 13.71 | 8.20 | 9.23 | <0.00001 * | 0.02942 * |
| NO2(UT) (μm/m3) | 35.32 | 20.68 | 28.04 | 0.00019 * | <0.00001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Javorac, J.; Živanović, D.; Ilić, M.; Mijatović Jovin, V.; Stojkov, S.; Smuđa, M.; Minaković, I.; Kolarš, B.; Ćućuz, V.; Jevtić, M. COVID-19 Lockdown Air Pollution Reduction: Did It Impact the Number of COPD Hospitalizations? Atmosphere 2024, 15, 593. https://doi.org/10.3390/atmos15050593
Javorac J, Živanović D, Ilić M, Mijatović Jovin V, Stojkov S, Smuđa M, Minaković I, Kolarš B, Ćućuz V, Jevtić M. COVID-19 Lockdown Air Pollution Reduction: Did It Impact the Number of COPD Hospitalizations? Atmosphere. 2024; 15(5):593. https://doi.org/10.3390/atmos15050593
Chicago/Turabian StyleJavorac, Jovan, Dejan Živanović, Miroslav Ilić, Vesna Mijatović Jovin, Svetlana Stojkov, Mirjana Smuđa, Ivana Minaković, Bela Kolarš, Veljko Ćućuz, and Marija Jevtić. 2024. "COVID-19 Lockdown Air Pollution Reduction: Did It Impact the Number of COPD Hospitalizations?" Atmosphere 15, no. 5: 593. https://doi.org/10.3390/atmos15050593
APA StyleJavorac, J., Živanović, D., Ilić, M., Mijatović Jovin, V., Stojkov, S., Smuđa, M., Minaković, I., Kolarš, B., Ćućuz, V., & Jevtić, M. (2024). COVID-19 Lockdown Air Pollution Reduction: Did It Impact the Number of COPD Hospitalizations? Atmosphere, 15(5), 593. https://doi.org/10.3390/atmos15050593








