Abstract
The impact of climate change on the physical environment, ecosystems, and human societies is increasingly recognized as the most important global challenge. Climate change may alter, among others, the thermal environment, the occurrence of extreme weather events, and the human exposure to physical, chemical, and biological pollutants, thus affecting human health with several potential outcomes. The impact of climate change on occupational health and safety has been receiving increasing attention in last years. In the European Union, the health and safety of workers is under the rule of Directive 89/391 and its daughters. In a changing climate, compliance with all requirements of the existing EU regulation entails an additional effort to implement preventive and protective measures. A central role in workers’ health protection is played by proper workers’ information and training, which is partly in charge of the occupational physicians. This paper provides a basic proposal on topics related to climate change to update workers’ information and training and to integrate the curricula of occupational physicians. Importantly, suitable information and training may contribute to promoting workers’ health and to implement adaptation measures, which are part of the individual, societal, and global responses to climate change.
1. Introduction
Climate Change (CC) is likely to be the current most important global challenge, not only for human safety, health, and wellbeing but also for the future of human civilization. There is now very little doubt on the anthropogenic causes of CC. The International Panel on Climate Change (IPCC) [1] periodically assesses the scientific evidence on CC, developing and updating models of climate evolution up to 2100, evaluating the impact on the physical environment, ecosystems, and human societies as well as discussing mitigation and adaptation measures. In its 6th assessment report [2], IPCC stresses the need to take actions globally in order to avoid global warming to exceed 1.5 °C with respect to the pre-industrial age. This goal has already been highlighted in a IPCC 2018 report [3] and is in line (being even more stringent) with the indications provided by the Paris agreement in 2015 [4].
For many years, the impact of CC on human health has been the subject of scientific papers and national and international reports [5,6,7,8,9,10,11,12,13,14,15,16]. A relevant example was given by the Lancet countdown, an international collaboration aimed at monitoring the health consequences of CC (see for instance Romanello et al. [17]), which periodically publishes ad hoc reports.
Heat strokes, accidents, renal failure, and cardiovascular and respiratory diseases induced or aggravated by heatwaves and/or severe/extreme meteorological events (like floods, storms, heavy rainfalls, droughts) (Section 3.3) are generally recognized in terms of increased rates of general and cause-specific mortalities, hospital admissions, and drug consumptions.
Mental health is stressed in Section 3.4 and displays an increasing link with CC. Reproductive health is increasingly recognized to be affected by CC with a multilevel action during pre-conception period, prenatal development, pregnancy outcome, and long-term consequences for the offspring (see for instance Yuzen et al., 2023 [18]).
Regarding a multifactorial, multi-stage, and long-term long latency disease like cancer, CC is projected to worsen the cancer burden, negatively acting along the entire pathway of cancer control (from etiology to treatment) [19].
In general, both well-recognized, short-term direct effects of CC on health and, even more, indirect effects, the last ones often characterized by a marked multifactorial etiology, long latencies and a more complex and partly unknown link with climate variables, are increasingly stressing the health systems worldwide. Health impact of CC may be worsened by a more difficult access to healthcare. The necessity to improve health systems, the question of economic costs, and the need of adequate risk management are recognized in the literature [20].
Issues regarding the necessity to extend and improve research, management, and communication on CC and human-health-related topics are repeatedly stressed in the literature (see for instance Ebi; Agache et al.; Campbell et al. [21,22,23]).
With respect to public health, the impact of CC on occupational health is an issue not so extensively investigated until now. Nonetheless, this issue is receiving increasing attention since 2009 [24], being explored in more detail at national and international levels in the subsequent years (see for instance D’Ovidio et al.; Schulte et al.; Schulte et al., 2023; Moda et al.; Ferrari et al. [25,26,27,28,29]).
EU regulation on occupational health and safety (Directive 89/391/EC, the so-called framework directive, and its daughters [30]) provides a coherent framework in order to protect workers’ health and safety through a proper risk assessment and management carried out by the employer. Measures to be implemented include the reduction or the elimination of exposure to risk factors existing in the workplace, the use of personal protective equipment (if requested), and workers’ health surveillance (if the worker is exposed to risks for which health surveillance is mandatory or on worker’s own request). Workers’ information and training on occupational risk factors of concern, as well as on related preventive and protective measures, is another pillar of occupational health and safety extensively recognized by EU regulation. This duty is in charge to the employer, but, some topics, especially those related to workers’ health protection and promotion, fall into the responsibility of the occupational physician.
This paper is neither a systematic or narrative review nor a study reporting original epidemiological or experimental results, but its objective is to stress the role of workers’ information and training in order to ensure a better management of the occupational risk factors potentially modulated by CC and, more generally, to support a more active role of occupational health practices in designing, implementing, and supporting strategies of adaptation to CC. As a preliminary input, a framework of basic concept and information on CC-related topics aimed at workers’ information and training is provided, which may be modulated and extended including additional and targeted information based on the activity sector, workplace involved, and specific job duties. In parallel, a proposal to integrate the degree and post-degree curricula of occupational physicians with CC-related topics is provided.
2. Methods
Recognition of occupational settings where workers were (or were to a greater extent) exposed to both direct and indirect effects of CC, reporting risk factors, the exposure to which may be (or is projected to be) modulated by CC. Moreover, EU regulation with regard to workers’ information and training will be stressed. Finally, a minimum set of information and advices on CC and occupational health and safety to be provided to the worker will be proposed, having in mind the need for both health promotion and adaptation to CC in working and living environments. Complementary to this is a proposal concerning the study curricula of occupational physicians, which should hopefully be integrated with CC-related topics.
3. Results
Issues related to CC are of concern for both indoor and outdoor workers.
3.1. Indoor Workers
CC affects indoor/outdoor exchanges, which, in turn, may potentially exacerbate heat stress of indoor workers or increase the exposure of the last ones to variable patterns of chemical pollutants, airborne infectious agents, or aeroallergens. However, the influence of CC on indoor air quality remains largely unknown [31], due to the number of factors involved, including those connected to building characteristics and socio-economic, cultural, and geographical features.
3.2. Outdoor Workers
Outdoor workers are more extensively involved in terms of CC impacts [28,32], as a number of occupational risk factors influenced by CC have a great relevance in outdoor settings. Therefore, considerations reported below refer primarily to outdoor workers.
There is not a shared definition of “outdoor worker” [33]. However, for the purposes of this paper, a worker is regarded as outdoor if the activity performed takes place outdoors, fully or for a significant fraction of the daily working time, having in mind that some working activities are mixed, conducted partly indoors and partly outdoors. The time spent outdoors may, therefore, be highly variable, as well as the exposure to typical outdoor occupational risk factors.
Despite the limitations, it is possible to indicate working sectors or jobs characterized by activities conducted outdoors or mostly outdoors (a non-exhaustive list is given in Table 1).

Table 1.
A non-exhaustive list of outdoor workers or jobs/activities conducted (or mostly conducted) outdoors *.
In addition to the “conventional” jobs/activities reported in Table 1, the ongoing energetic transition and the increasing need to protect, maintain, restore, or expand natural ecosystems will likely result in an growing number of workers employed in the so-called “green jobs”, largely conducted outdoors, as well as in a further diversification of these jobs. It must be emphasized that an increasing need of “green” activities is due to the current and future impacts of CC. Therefore, CC may potentially increase the exposure of “conventional” outdoor workers to outdoor occupational risk factors on one side and, on the other end, may indirectly expand and diversify the total number of workers that will operate outdoors or mostly outdoors due to the rising importance of green jobs [34,35,36].
Occupational exposures of outdoor workers are not fully overlapping. Apart from the time spent outdoors, each activity sector and/or job displays complex and variable patterns of multiple exposures. Moreover, rural outdoor settings differ from urban outdoor ones. For instance, in extra urban areas, air pollution is generally lower, and the contribution made by the urban heat island is absent. However, the vast majority of outdoor workers share exposure to a severe thermal environment, solar radiation (SR), air pollution (with highly variable patterns), vector-borne diseases, and aeroallergens.
3.3. Thermal Environment, Meteorological Conditions, and Productivity
An increase in the mean global surface temperature due to the ongoing CC, now about 1.1 °C above that of the preindustrial age, has multiple consequences, among which the intensifications of the extreme meteorological events are of paramount importance. This means, for instance, the occurrence of more frequent, intense, and long-lasting heat waves. In parallel, events like storms, floods, tornados, and, to some extent, hurricanes or, on the opposite, droughts increase in both frequency and intensity [20,37]. Heat waves contribute to the progressive desertification of drylands worldwide, but a typical, short-term, and alarming by-product of heat waves is an intensification of wildfires [38,39]. The effects of wildfires are generally severe by themselves but may be amplified in urban areas, where an additional temperature increase (even several degrees) may occur due to the so-called “heat island effect” [40], a widespread phenomenon involving a growing number of urban settings across different latitudes and altitudes over time [41]. Outdoor workers are then exposed to a potentially higher thermal stress. To stay and work in a severe hot thermal environment, especially when relative humidity is high, leads to a higher risk of accidents at work, dehydration (with an increased risk for renal failure), heat stroke, exacerbation of clinical features of pre-existing diseases (like cardiovascular, lung and renal diseases), higher hospitalization, and mortality rates [42,43,44]. Moreover, a significant loss of productivity and a large economic burden is expected [45], especially in sectors like agriculture and construction [43].
An early onset of the summer season and/or an early occurrence of heat waves in temperate zones is another reason for concern. In fact, the body experiences an abrupt transition to a hot and wet weather, with no time to adapt to the new microclimatic conditions and a consequent higher risk of thermal stress or thermal exhaustion, especially when an individual is employed in an outdoor activity. The exposure to wind, rain, and to sudden changes in weather conditions may increase the risk of accidents at work, worsen pre-existing respiratory and cardiovascular diseases, and increase the individual susceptibility to respiratory infections.
3.4. Mental Health
A prolonged thermal stress or too-frequent weather changes may also lead to disclosing latent psychiatric disorders or exacerbating existing ones [12,14,46], especially if social and economic disadvantages, marginalization, substance abuse, and CC-induced alterations of the living environment occur. The impact of CC on mental health is likely to be relevant in occupational health, given the potential safety and health consequences of psychiatric disorders in occupational settings. Emotional responses to CC concerns may induce climate anxiety [7], a feature that needs to be further explored due to its potential consequences on health and well-being as well as to individual and collective choices.
A growing number of papers deal with CC and farmers’ mental health (see for instance Polain et al., 2011; Ellis and Albrecht, 2017; Talukder et al., 2021; Nagai, 2023 [47,48,49,50]), especially in countries like Australia and in Asia, and with particular reference to smallholder farmers. Rural workers, especially the aged ones, are at higher risk for anxiety, depression, post-traumatic stress disorders and other forms of mental disorders in relation to rapid environmental changes (including CC) involving their living and working environments, given the uncertainties due to the impact of extreme events like droughts and floods on food production, dwellings, conventional lifestyles, etc.
3.5. Solar Radiation
SR is crucial for human health, having direct effects on the body (especially on skin and eye) and indirectly affecting both thermal environment and human exposure to some chemical pollutants, disease vectors, and biological agents. Accordingly, SR will be stressed in more detail in the following.
SR on earth surface contains approximately 50% of Infrared Radiation (IR), 45% of visible radiation, and about 5–6% of Ultra Violet Radiation (UVR) (the 95% of which is UVA, and 5% is UVB at noon—the ozone layer completely blocks UVC in the stratosphere).
Exposure to SR may vary as a function of daytime, latitude, altitude, season, air pollution, total time spent outdoors, and implementation of preventive and protective collective and individual measures [51,52,53]. Prolonged heat waves or changes in cloudiness due to CC are additional factors affecting the exposure to SR [54]. The interplay between CC and stratospheric ozone cycles of depletion and recovery may increase the net solar UVR even at mid latitudes, although to a substantially lesser extent, with respect to Polar Regions. CC is projected to delay the stratospheric ozone recovery. The beneficial trend in ozone recovery was due to the ban of ozone-depleting substances following the implementation of the Montreal protocol [55,56].
This does not necessarily lead to a net increase in SR exposure, especially if general population and sun-exposed workers adopt or largely adopt the appropriate protective measures: avoiding sun exposure in the central hours of the day; shadow seeking; sun shielding by using gazebos, curtains, etc.; appropriate clothing; and use of large-brimmed hats, sunglasses, and sunscreens, etc. However, outdoor workers are at higher risk of a prolonged exposure, with respect to the general public, if the duly preventive and protective measures are not fully implemented. It must be emphasized that SR tends to be an underestimated risk for outdoor workers [57]. Moreover, the implementation of progressively lower exposure limits for classes of air pollutants like particulate matter may contribute to a further increase in SR exposure due to the lack of the shielding power exerted by airborne particulates with regard to SR.
Exposure to SR may induce both acute and long-lasting effects on the skin and eyes [54,58]. Among acute effects on the skin’s photoerythema, tanning and thickness of the corneous layer are to be included. Moreover, SR may induce or exacerbate the clinical features of the so-called photodermatosis (some of them arising from genetic defects or being linked to immune system alterations) and is responsible for phototoxic and photoallergic reactions. UVB and, to a lesser extent, UVA are involved in exacerbation of photodermatosis. However, some photodermatosis (e.g., the solar urticaria) and a subset of phototoxic and photoallergic reactions may be triggered even by visible radiation.
SR as a whole and the separate spectral bands UVA, UVB, and UVC were assessed to be carcinogenic to humans by the International Agency for Research on Cancer (IARC) [40]. Exposure to SR is associated with an increased risk of Basal Cell Carcinoma (BCC) of the skin, Squamous Cell Carcinoma (SSC) of the skin, and Cutaneous Malignant Melanoma (CMM). The association with ocular melanoma is still an object of debate. Outdoor workers are at a higher risk of BCC and SCC [59], as well as of the precancerous lesions of SSC, i.e., actinic keratosis.
The eye is affected by SR both acutely (induction of photokeratitis, photokeratoconjunctivitis, and photoretinitis) and chronically (induction of pinguecola, pterygium, cataracts, and macular degeneration). Again, UVB and UVA are largely involved, but macular degeneration is generally associated with long-term (even lifetime) exposure to shortwave, visible radiation, i.e., blue and violet light. Outdoor workers are shown to be at higher risk for both cataracts, especially the cortical type, and macular degeneration, although studies are not fully concordant, and the dose–response relationship as well as the magnitude of the additional risk with respect to the general population are difficult to assess [60,61].
Solar UVR may exert modulatory effects on the immune system. The complete picture of UV-induced immune effects and related action mechanisms are complex and not yet fully elucidated [62]. Summarizing the current knowledge, it may be stated that UVR stimulates innate immune responses while tending to inhibit acquired immunity. UVR modulates the immune system at both the local and systemic levels, but the potential consequences are not yet clear and are object of research activity. Among the topics under study, increased susceptibility to infections, decreased efficacy of vaccines, increased risk of skin- and non-skin cancers, or, as a positive outcome, the attenuation of clinical features of autoimmune and allergic diseases have to be mentioned. Similarly, the health outcomes due to interplay between SR, CC, and exposure to occupational pollutants with immunotoxic properties have not yet been adequately addressed [63].
The individual susceptibility to the adverse effects of SR varies greatly, depending on the phototype (phototypes I and II are the most sensible), conditions like albinism, pre-existing skin and eye diseases, co-exposure to photoactive substances, etc.
Exposure to SR, on the opposite, may exert beneficial effects to health, the best-known being the vitamin D3 synthesis, a substance having a pleiotropic activity on human physiology, well beyond the regulation of calcium metabolism [58,64,65]. There is an ongoing debate on how much vitamin D is necessary to restore, maintain, or improve a good health status in relation to individual features, but emerging evidence indicates that SR may have health benefits regardless of vitamin D3. These ones include a potential protective effects on some internal cancers, lowering of blood pressure, regulation of circadian rhythms, and, in general, improvement of wellness sensation.
A growing body of data indicate that other bands of SR, especially visible radiation and, even more, near-infrared radiation (or IRA), may be important in modulating the biological effects of solar UVB and UVA at the skin and even the eye level [64]. Moreover, apart the evident and well-known role of light in vision physiology, visible radiation may promote the formation of Reactive Oxygen Species (ROS) in the skin tissue [33,64], as the IRA does. The biological significance of ROS production by visible and IR radiation may be potentially beneficial or adverse, depending on cells/tissues involved, radiation doses and dose rates, time course of ROS synthesis ad removal, and other not-well-established parameters. Finally, there is evidence that ambient temperature may enhance the carcinogenic potential of UV radiation on keratinocytes [33,66,67,68].
The ongoing CC is projected to increase the incidence of skin cancer in the following years and decades [55]. This is likely to be due to the combined effects of an increased exposure to SR, changes in ambient temperature, and altered patterns of exposure to air pollutants, some of which have carcinogenic properties. Although the evidence is still lacking, it is reasonable to forecast that the combined effect of CC and SR will lead to an increased incidence of eye diseases.
It is difficult to assess the balance between adverse and beneficial effects of SR on individual level as a function of a certain amount of exposure to SR, being crucial in this regard both the individual susceptibility and many co-exposures (or, more extensively, the individual “exposome”). However, it is conceivable that outdoor workers, given the generally strong amount of exposure to SR, a potential severe thermal environment and multiple co-exposures to physical, chemical, and biological agents, are likely to have a net balance shift towards adverse effects. Uncertainties persist regarding the impact on different health outcomes due to future exposure to SR interacting with CC and ozone depletion/recovery [56].
3.6. Air Pollution
Qualitative and quantitative patterns of air pollutants depend on the type, number, and localization of the sources of pollution and may vary greatly [69]. Some factors affecting airborne concentration of chemical pollutants display oscillatory patterns (for instance, following the daily and seasonal solar cycle and the day–night variations in vehicular traffic). The superimposition of CC makes this framework more complex, depending on both CC scenario and projections of future emissions of air pollutants [70]. However, it is likely that CC contributes (and will contribute) to increase human exposure to pollutants like ozone and fine particulate matter (PM), both directly and indirectly.
A sustained increase in ambient temperature can result in a higher airborne concentration of Volatile Organic Compounds (VOCs) and Polycyclic Aromatic Hydrocarbons (PAHs), the last ones known to be carcinogenic for the lungs, skin, and bladder [71]. It must be emphasized that both outdoor atmospheric pollution and outdoor PM were evaluated by IARC as carcinogenic to humans (group 1 of the IARC classification of the carcinogenic evidence) in relation to lung cancer [72].
Ozone is a secondary air pollutant formed by photochemical reactions involving primary pollutants. Its concentration depends on both the amount(s) of primary air pollutants (e.g., NO2) and the intensity of SR. A prolonged and more-intense solar irradiation of the troposphere due to CC is likely to result in higher and more persistent tropospheric ozone concentrations. Ozone is responsible for airways irritation, exacerbation of pre-existing respiratory diseases, as well as hospitalizations, and deaths [73,74,75,76,77,78].
Exposure to PM is associated with an increased risk of respiratory, cardiovascular, and neoplastic diseases, but there are concerns for other health outcomes [79,80]. Fine (<10 µm—PM10) and ultrafine (<2.5 µm—PM2.5) PM once inhaled may reach pulmonary alveoli. A significant fraction of alveolar PM (especially PM2.5) translocases into the blood stream and, through this route, is able to reach a number of tissues and organs. Nanoparticulate (<0.1 µm—NP or PM0.1) matter displays an even higher capability to penetrate lower respiratory airways and blood streams; an intense research activity on the health effects due to NP exposure is ongoing, especially for potential long-term effects and including non-neoplastic ones.
Exposure of outdoor workers to PM depends on the type, localization, and intensity of anthropogenic sources as well as the job(s) performed and the time spent outdoors. Weather conditions modulate human exposure to airborne PM in outdoor settings. For instance, wind and rain may remove or dilute the suspended PM. As a consequence, if CC determines a higher frequency, intensity, and duration of heatwaves, this is likely to translate into an increased exposure to PM. On the opposite, if the local consequences of CC are in terms of increased rain, storms, or floods, then the exposure to PM is projected to decrease. As in other cases (see for instance the exposure to SR), the net effect of CC is difficult to predict, being largely affected by local conditions.
Other concerns linked to workers’ exposure to airborne chemical pollutants are related to the impact of CC on occupational exposure to pesticides [81].
For completeness and relevance, there are at least two situations involving outdoor workers where CC may lead to a net increase in the exposure to air pollutants within large areas of terrestrial surface.
The former refers to wildfires [38,39], whose frequencies, extensions, and durations are shown to be dramatically increased in both temperate and non-temperate zones in recent years. Wildfires produce a number of pollutants (among others, CO, VOCs, PM10, PM2.5, and NP), which may be transported by atmospheric circulation over great distances and can add to the anthropogenic ones, especially in urban and industrial areas.
The latter situation is linked to the combined effects of changed patterns of atmospheric circulation and the progressive extension of arid or desert areas. This may lead to a higher spread of dust and sand particulate over the inhabited areas during desert storms, with a consequent higher exposure of residents and a potential impact on health, especially in terms of respiratory and cardiovascular diseases [82,83].
3.7. Communicable Diseases
CC may increase the exposure to vector-borne diseases [84,85,86] due to the modifications in vector habitats. The last ones may expand to higher latitudes, given the increased mean temperatures, the changing patterns of humidity, and the anticipation of the spring and summer seasons. Concerns are predominantly related to arboviruses infections. CC may indirectly affect the occurrence of gastro-enteric infectious diseases altering the quality of water and food supplies or may promote respiratory and non-respiratory infections if exposure to increased humidity, rainfalls, floods, storms, and droughts occurs [87]. Altogether, over half of human infectious diseases can be aggravated by CC [88].
Moreover, the destruction of forest habitats is a direct consequence of anthropic activities but is exacerbated by CC. It promotes the contact between humans and disease-vectors on one side and the proximity of humans to wild mammalian or avian species on the other side. The last scenario may increase the likelihood of spill-overs [89]. Although not proven, it is not unlikely that a similar mechanism was implied in the origin of the SARS-CoV-2 pandemics [90].
The increased or decreased exposure to risk factors modulated by CC may affect the risk of airborne, foodborne, or waterborne infections through other mechanisms. For instance, increased killing activities of pathogens due to UVR and other spectral bands of SR if the exposure to SR effectively increases are conceivable. On the other hand, SR may exert local and systemic immunosuppressive effects, as previously stated, and it is problematic to predict how this modulates the real risk of infections.
3.8. Allergic Diseases
CC is a factor exacerbating the occurrence and/or severity of allergic diseases [91,92,93], with an emphasis on respiratory allergic diseases (asthma in particular). For instance, an early spring and a more prolonged flowering season increase the exposure to allergens like pollens, both quantitatively and qualitatively. The episodes of the so-called “thunderstorm asthma”, due to a higher exposure to allergenic proteins of pollens caused by the osmotic rupture of pollen grains during rainfalls or thunderstorms, have been shown to increase during extreme meteorological events, the frequency and intensity of which is, as previously mentioned, affected by CC. Airborne pollutants like O3, NO2, and others may interact with molecular components of pollen grains (especially proteins), producing chemical conjugates that enhance the allergenic potential of the original pollen biomolecules in many cases. Molds are a well-known source of respiratory allergies. Moist environments due to frequent and prolonged rainfalls (or flood in some cases) promote the growth of molds and, especially in previously degraded or not adequately protected living and working settings, may increase the risk of allergy occurrence or exacerbation. It occurs primarily or exclusively in indoor settings.
4. Discussion
CC is a meta-risk factor superimposing on and interacting with several physical, chemical, and biological agents found in both outdoor and indoor settings. Figure 1 is an oversimplified picture of the mutual interactions among CC, stratospheric ozone, urban environment, pollution, and other determinants of health status, ultimately affecting, in a poorly predictable manner, outdoor and indoor workers’ health statuses.
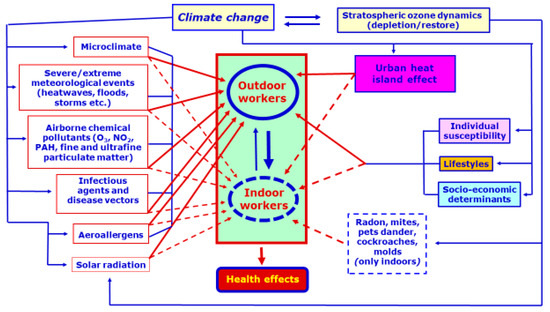
Figure 1.
An essential scheme showing the very complex and only partially known interactions between climate change, stratospheric ozone, and urban heat islands, with regard to occupational exposure to physical, chemical, and biological agents in both outdoor and indoor settings. The figure’s content is qualitative. A quick view highlights that most of the reported risk factors acts (directly or indirectly) in both outdoor and indoor environment(s), with the exception of pollutants typical of the indoor environment(s) (e.g., radon and molds). Different types of risk factors may interact and modulate each other (for instance increasing or decreasing their concentration into the environment or their action on biological targets), and this is represented by a blue line, with some dashes connecting the different classes of physical, chemical, and biological agents. In this context, the so-called “Urban heat island” may act on both outdoor and indoor settings, with the exception of those located in extra urban areas, potentially amplifying the effects due to a severe thermal environment and, indirectly, to other risk factors. Urban heat island may also modify, among others, individual lifestyles. In summary, workers’ health is affected by multiple exposures. The final health outcome(s) is (are) qualitatively and quantitatively dependent on activity sector, job performed, time spent indoors/outdoors, agents to which workers are exposed, their relative and changing concentrations, and their interactions. Health effects on the single worker are modulated by individual susceptibility, lifestyles, and socio-economic determinants (reported in the figure). The continuous blue circle represents the generality of the outdoor setting (with the outdoor workers), whereas the dotted blue circle indicates the generality of indoor settings (with the indoor workers). Importantly, exchanges between outdoors and indoors do exist and are represented in the figure by two blue arrows in opposite directions. Exchanges are principally due to air flowing and to people movement inward or outward (not represented in the figure). People act as carriers of, for instance, biological agents and/or allergens like pollen. The figure indicates that the general gradient of exchange is usually inward (thicker arrow), i.e., toward indoor settings, due to the higher outdoor concentration of several chemical and biological pollutants. Continuous red arrows mark what refers to the outdoors (with the exception of the red arrow indicating health effects, which is cumulative), whereas, for the indoors, dotted red arrows were chosen.
CC is challenging occupational health and safety, requiring, in many cases, an adjustment of both risk assessment in the workplaces and implementation of preventive/protective measure to reduce or eliminate occupational risk factors.
The Total Worker Health (TWH), a program launched by NIOSH in 2011 and defined “as policies, programs, and practices that integrate protection from work-related safety and health hazards with promotion of injury and illness-prevention efforts to advance worker well-being” [94,95] may be regarded as a starting point to implement issues on occupational health and safety in a changing climate.
In fact, today and increasingly in the future worker’s health and well-being promotion has to include CC instances. Moreover, it must be kept in mind that CC does not only affect workers in working hours but also during the leisure time (at home, on holidays, etc.). Consequently, non-occupational exposure to physical, chemical, and biological agents (which is generally lower but sometimes may be higher than in the workplace) may add to and interact with the occupational one.
Migration due to CC is a crucial issue for developed countries and future geopolitical scenarios. Migrants’ health is a central topic in this regard (see for instance Bellizzi et al., 2023; McMichael, 2023 [96,97]), and, in addition to concerns due to inherently more susceptible populations to a series of new and consolidated health risks, new opportunities emerge in terms of a further support to adaptation measures and of a better resilience to climate and environmental challenges. Occupational health and safety of migrant workers in a changing climate poses additional challenges, starting from those connected to heat stress [98], requiring to build or improve an interface between native and migrant workers in a more general framework aimed at promoting decent work [99].
Ageing workers are of particular concern with regard to CC. In developed countries, demographic trends and the tendency to delay workers’ retirement contribute to a progressive ageing of the workforce. Elderly workers tend to be less productive, more prone to work accidents, and to develop multifactorial diseases but may be important sources of opportunities [100]. However, they tend to be less resilient to environmental and climate changes, especially if they are sudden.
The above considerations strengthen the need to address and re-address proper risk assessments and management strategies in the workplaces, especially if CC concerns are to be taken into account, and makes the framework depicted until now even more complex.
The impact of CC on occupational health and safety emphasizes the role of occupational health professionals (see for instance Patil and Jeffery [101]). The role of workers’ information and training is of increasing importance, and topics related to CC cannot longer be ignored. The occupational physician plays an important role in workers’ information and training, as recognized by EU Regulation (directive 89/391 and the so-called “daughters directives”). The occupational physician is responsible of the health surveillance of the worker(s) at risk and informs the worker(s) surveyed about contents, results, and meanings of health surveillance practices, also dealing with the matter of workers’ health protection and promotion. In order to fully achieve the goal of proper, complete, updated, and useful information and training of a heterogeneous and changing workforce in workplaces characterized by occupational risk profiles increasingly affected by CC, the curricula of occupational physicians should include, during the degree or post-degree studies, concepts, notions, and operative approaches on the ongoing CC and its impact on the environment as well as on public and occupational health.
This is in line with a growing need to outline the role of health professionals in relation to CC, with particular reference to medical education and medical practice, as reported in the recent literature [102,103,104,105,106,107,108]. The impact of CC on medical ethics is also increasingly recognized. The aim is to obtain a suitable emergency management, a more effective treatment of both acute and chronic diseases impacted by CC, and the enforcement of the framework to educate people to healthy lifestyles and adaptive behaviors.
Occupational medicine pertains to the wider area of public health, which is primarily involved, together with environmental health, in the assessment and management of CC health impact. Moreover, in the EU Regulation the occupational physician plays many roles. A central duty of the occupational physician, in addition to health surveillance and workers’ information/training, is to contribute to the risk assessment in the workplace, acting as an employer’s advisor in practice. However, the authors argue that all medical specialties play an important, although complementary, role in the assessment and management of the health impact of CC. For instance, clinicians are requested to have a growing competence and practice in recognizing and treating clinical features induced or aggravated by CC-related effects, especially the indirect ones. In fact, while it is relatively easy to recognize and treat, for instance, heat stroke, it could be more difficult to address climate-induced or aggravated health effects whose causal agent is chemical or biological. Such difficulties may also arise in the case of the effects potentially linked to exposures erroneously regarded as low (for instance, on the basis of extrapolations from similar situations assessed in the past with no or less CC impact), as well as if long-term effects are involved.
An indicative proposal to include CC into the curricula of occupational physicians is reported in Table 2, whereas a parallel proposal on the CC-related content of workers’ information and training is given in Table 3. Periodic assessment of the effectiveness of workers’ information and training including CC topics has to be envisaged.

Table 2.
Proposal for integrating the curricula of occupational physicians with climate change (CC) related skills.

Table 3.
Concepts and notions on climate change (CC) suggested to be included into workers’ mandatory information and training within occupational safety and health management.
5. Conclusions
Considerations expressed in this paper depict a growing complexity in risk assessment procedures for a lot of workplaces and working activities, primarily outdoors. This complexity is increasingly drawn by CC and adds to the need to assess the impact of multiple exposure and to the expanding necessity to predict health outcomes at an individual level. This scenario makes the management of occupational health and safety increasingly dependent on the implementation of emerging methods and approaches, namely, the concept of “exposome”, big data analysis, and “omics” techniques (see for instance Dini et al.; Abdelzaher et al. [109,110]). This should allow, among others, to develop suitable biomarkers of exposure, effect, and susceptibility.
CC is, undoubtedly, a strong additional reason to explore the implementation of these tools in occupational health and safety, in an effort to reduce the time elapsing between the availability of a particular tool or a combination of tools and its/their successful application(s) in real occupational settings. Moreover, it must be kept in mind that catastrophic scenarios linked to CC [111], e.g., the increase of three or more degrees in mean global surface temperature in relatively closed time horizons, although not so likely, may not be excluded and have to be taken into account to forecast appropriate responses at individual, societal, national, and international levels. Evidently, catastrophic scenarios would represent unprecedented challenges for the management of occupational health and safety.
Workers’ information and training are likely to become even more crucial in this regard. The same may be assumed in relation to targeted competence acquired by occupational physicians. As workers’ information and training must emphasize, among other factors, the importance of healthy lifestyles, their purposes go beyond the awareness of occupational hazards and the correct implementation of both collective and individual preventive and protective measures. In more general terms, they concur to improve individual and collective adaptation to CC.
Author Contributions
Conceptualization: C.G. and M.C.D.; Methodology: C.G., A.L. and M.C.D.; Formal analysis: C.G. and A.L.; Investigation: C.G., A.L. and M.C.D.; Data curation: C.G., A.L. and M.C.D.; Writing—original draft preparation: C.G.; Writing—review and editing: C.G., A.L. and M.C.D.; Visualization: C.G. and M.C.D.; Supervision: C.G., A.L. and M.C.D.; Project administration: C.G. and M.C.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data supporting reported results can be provided on request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- The Intergovernmental Panel on Climate Change (IPCC). Available online: https://www.ipcc.ch/about/ (accessed on 24 May 2023).
- IPCC Sixth Assessment Report. Available online: https://www.ipcc.ch/assessment-report/ar6/ (accessed on 24 May 2023).
- IPCC Special Report—Global Warming of 1.5 °C. Available online: https://www.ipcc.ch/sr15/ (accessed on 24 May 2023).
- The Paris Agreement. What Is the Paris Agreement? Available online: https://unfccc.int/process-and-meetings/the-paris-agreement (accessed on 24 May 2023).
- Tong, S.; Ebi, K. Preventing and mitigating health risks of climate change. Environ. Res. 2019, 174, 9–13. [Google Scholar] [CrossRef]
- Nogueira, L.M.; Crane, T.E.; Ortiz, A.P.; D’Angelo, H.; Neta, G. Climate change and cancer. Cancer Epidemiol. Biomarkers Prev. 2023, 32, 869–875. [Google Scholar] [CrossRef]
- Clayton, S. Climate anxiety: Psychological responses to climate change. J. Anxiety Disord. 2020, 74, 102263. [Google Scholar] [CrossRef]
- Wynkoop, W. Climate change, air pollution & health. Explore 2020, 16, 131–132. [Google Scholar] [CrossRef] [PubMed]
- Clarke, B.; Otto, F.; Stuart-Smith, R.; Harrington, L. Extreme weather impacts of climate change: An attribution perspective. Environ. Res.:Climate 2022, 1, 012001. [Google Scholar] [CrossRef]
- World Health Organization. WHO Global Strategy on Health, Environment and Climate Change the Transformation Needed to Improve Lives and Wellbeing Sustainably through Healthy Environments; WHO: Geneva, Switzerland, 2020; ISBN 978-92-4-000037-7 (electronic version); 978-92-4-000152-7 (print version). [Google Scholar]
- Dasandi, N.; Cai, W.; Friberg, P.; Jankin, S.; Kuylenstierna, J.; Nilsson, M. The inclusion of health in major global reports on climate change and biodiversity. BMJ Glob. Health 2022, 7, e008731. [Google Scholar] [CrossRef] [PubMed]
- Hwong, A.R.; Wang, M.; Khan, H.; Chagwedera, N.; Grzenda, A.; Doty, B.; Benton, T.; Alpert, J.; Clarke, D.; Compton, W.M. Climate change and mental health research methods, gaps, and priorities: A scoping review. Lancet Planet. Health 2022, 6, e281–e291. [Google Scholar] [CrossRef]
- Segal, T.R.; Giudice, L.C. Systematic review of climate change effects on reproductive health. Fertil. Steril. 2022, 118, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Lawrance, E.L.; Thompsond, R.; Newberry Le Vaya, J.; Pagee, L.; Jennings, N. The impact of climate change on mental health and emotional wellbeing: A narrative review of current evidence, and its implications. Int. Rev. Psychiatry 2022, 34, 443–498. [Google Scholar] [CrossRef]
- Khraishah, H.; Alahmad, B.; Ostergard, R.L., Jr.; AlAshqar, A.; Albaghdadi, M.; Vellanki, N.; Chowdhury, M.M.; Al-Kindi, S.G.; Zanobetti, A.; Gasparrini, A.; et al. Climate change and cardiovascular disease: Implications for global health. Nat. Rev. Cardiol. 2022, 19, 798–812. [Google Scholar] [CrossRef]
- Louis, S.; Carlson, A.K.; Suresh, A.; Rim, J.; Mays, M.A.; Ontaneda, D.; Dhawan, A. Impacts of climate change and air pollution on neurologic health, disease, and practice—A scoping review. Neurology 2023, 100, 474–483. [Google Scholar] [CrossRef] [PubMed]
- Romanello, M.; McGushin, A.; Di Napoli, C.; Drummond, P.; Hughes, N.; Jamart, L.; Kennard, H.; Lampard, P.; Solano Rodriguez, B.; Arnell, N.; et al. The 2021 report of the Lancet Countdown on health and climate change: Code red for a healthy future. Lancet 2021, 398, 1619–1662. [Google Scholar] [CrossRef] [PubMed]
- Yüzen, D.; Graf, I.; Diemert, A.; Arck, P.C. Climate change and pregnancy complications: From hormones to the immune response. Front. Endocrinol. 2023, 14, 1149284. [Google Scholar] [CrossRef]
- Hiatt, R.A.; Beyeler, N. Cancer and climate change. Lancet Oncol. 2020, 21, e519–e527. [Google Scholar] [CrossRef]
- Ebi, K.L.; Vanos, J.; Baldwin, J.W.; Bell, J.E.; Hondula, D.M.; Errett, N.A.; Hayes, K.; Reid, C.E.; Saha, S.; Spector, J.; et al. Extreme weather and climate change: Population health and health system implications. Annu. Rev. Public Health 2021, 42, 293–315. [Google Scholar] [CrossRef]
- Ebi, K.L. Managing climate change risks is imperative for human health. Nat. Rev. Nephrol. 2022, 18, 74–75. [Google Scholar] [CrossRef]
- Agache, I.; Sampath, V.; Aguilera, J.; Akdis, C.A.; Akdis, M.; Barry, M.; Bouagnom, A.; Chinthrajah, S.; Collins, W.; Dulitzki, C.; et al. Climate change and global health: A call to more research and more action. Allergy 2022, 77, 1389–1407. [Google Scholar] [CrossRef]
- Campbell, E.; Uppalapati, S.S.; Kotcher, J.; Maibach, E. Communication research to improve engagement with climate change and human health: A review. Front. Public Health 2023, 10, 1086858. [Google Scholar] [CrossRef] [PubMed]
- Schulte, P.A.; Chun, H.K. Climate change and occupational safety and health: Establishing a preliminary framework. J. Occup. Environ. Hyg. 2009, 6, 542–554. [Google Scholar] [CrossRef]
- D’Ovidio, M.C.; Grandi, C.; Polichetti, A.; Iavicoli, S. Monographic section: Climate change and occupational health. Ann. Ist. Super. Sanità 2016, 52, 323–343. [Google Scholar]
- Schulte, P.A.; Bhattacharya, A.; Butler, C.R.; Chun, H.K.; Jacklitsch, B.; Jacobs, T.; Kiefer, M.; Lincoln, J.; Pendergrass, S.; Shire, J.; et al. Advancing the framework for considering the effects of climate change on worker safety and health. J. Occup. Environ. Hyg. 2016, 13, 847–865. [Google Scholar] [CrossRef] [PubMed]
- Schulte, P.A.; Jacklitsch, B.L.; Bhattacharya, A.; Chun, H.; Edwards, N.; Elliott, K.C.; Flynn, M.A.; Guerin, R.; Hodson, L.; Lincoln, J.M.; et al. Updated assessment of occupational safety and health hazards of climate change. J. Occup. Environ. Hyg. 2023, 20, 183–206. [Google Scholar] [CrossRef] [PubMed]
- Moda, H.M.; Filho, W.L.; Minhas, A. Impacts of climate change on outdoor workers and their safety: Some research priorities. Int. J. Environ. Res. Public Health 2019, 16, 3458. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, G.N.; Lapasini Leal, G.C.; Thom de Souza, R.C.; Cardoza Galdamez, E.V. Impact of climate change on occupational health and safety: A review of methodological approaches. Work 2023, 74, 485–499. [Google Scholar] [CrossRef] [PubMed]
- Council Directive of 12 June 1989 on the Introduction of Measures to Encourage Improvements in the Safety and Health of Workers (89/391/EEC); Official Journal of the European Comminities 29.6.89 No L 183/1; Official Journal of the European Comminities: Brussels, Belgium, 1989.
- Mansouri, A.; Wei, W.; Alessandrini, J.M.; Mandin, C.; Blondeau, P. Impact of climate change on indoor air quality: A review. Int. J. Environ. Res. Public Health 2022, 19, 15616. [Google Scholar] [CrossRef] [PubMed]
- Habibi, P.; Moradi, G.; Dehghan, H.; Moradi, A.; Heydari, A. The impacts of climate change on occupational heat strain in outdoor workers: A systematic review. Urban Clim. 2021, 36, 100770. [Google Scholar] [CrossRef]
- Grandi, C.; D’Ovidio, M.C. Balance between health risks and benefits for outdoor workers exposed to solar radiation: An overview on the role of near infrared radiation alone and in combination with other solar spectral bands. Int. J. Environ. Res. Public Health 2020, 17, 1357. [Google Scholar] [CrossRef]
- Valenti, A.; Gagliardi, D.; Fortuna, G.; Iavicoli, S. Towards a greener labour market: Occupational health and safety implications. Ann. Ist. Super. Sanità 2016, 52, 415–423. [Google Scholar] [CrossRef]
- Stanef-Puicà, M.R.; Badea, L.; Serban-Oprescu, G.L.; Serban-Oprescu, A.T.; Frâncu, L.G.; Cretu, A. Green jobs—A literature review. Int. J. Environ. Res. Public Health 2022, 19, 7998. [Google Scholar] [CrossRef]
- Kozar, Ł.J.; Sulich, A. Green Jobs: Bibliometric Review. Int. J. Environ. Res. Public Health 2023, 20, 2886. [Google Scholar] [CrossRef]
- Weilnhammer, V.; Schmid, J.; Mittermeier, I.; Schreiber, F.; Jiang, L.; Pastuhovic, V.; Herr, C.; Heinze, S. Extreme weather events in europe and their health consequences—A systematic review. Int. J. Hyg. Environ. Health 2021, 233, 113688. [Google Scholar] [CrossRef] [PubMed]
- Balmes, J.R. The changing nature of wildfires impacts on the health of the public. Clin. Chest Med. 2020, 41, 771–776. [Google Scholar] [CrossRef] [PubMed]
- Akdis, C.A.; Nadeau, K.C. Human and planetary health on fire. Nat. Rev. Immunol. 2022, 22, 651–652. [Google Scholar] [CrossRef]
- Yuan, Y.; Li, C.; Geng, X.; Yu, Z.; Fan, Z.; Wang, X. Natural-anthropogenic environment interactively causes the surface urban heat island intensity variations in global climate zones. Environ. Int. 2022, 170, 107574. [Google Scholar] [CrossRef]
- Ren, Y.; Lafortezza, R.; Giannico, V.; Sanesi, G.; Zhang, X.; Xu, X. The unrelenting global expansion of the urban heat island over the last century. Sci. Total Environ. 2023, 880, 163276. [Google Scholar] [CrossRef] [PubMed]
- Binazzi, A.; Levi, M.; Bonafede, M.; Bugani, M.; Messeri, A.; Morabito, M.; Marinaccio, A.; Baldasseroni, A. Evaluation of the impact of heat stress on the occurrence of occupational injuries: Meta-analysis of observational studies. Am. J. Ind. Med. 2019, 62, 233–243. [Google Scholar] [CrossRef]
- Levi, M.; Kjellstrom, T.; Baldasseroni, A. Impact of climate change on occupational health and productivity: A systematic literature review focusing on workplace heat. Med. Lav. 2018, 109, 163–179. [Google Scholar] [CrossRef]
- Johnson, R.J.; Sanchez-Lozada, L.G.; Newman, L.S.; Lanaspa, M.A.; Diaz, H.F.; Lemery, J.; Rodriguez-Iturbe, B.; Tolan, D.R.; Butler-Dawson, J.; Sato, Y.; et al. Climate change and the kidney. Ann. Nutr. Metab. 2019, 74, 38–44. [Google Scholar] [CrossRef]
- Borg, M.A.; Xiang, J.; Anikeeva, O.; Pisaniello, D.; Hansen, A.; Zander, K.; Dear, K.; Sim, M.R.; Bi, P. Occupational heat stress and economic burden: A review of global evidence. Environ. Res. 2021, 195, 110781. [Google Scholar] [CrossRef]
- Ramadan, A.M.H.; Ataallah, A.G. Are climate change and mental health correlated? Gen. Psychiatry 2021, 34, e100648. [Google Scholar] [CrossRef]
- Polain, J.D.; Berry, H.L.; Hoskin, J.O. Rapid change, climate adversity and the next ‘big dry’: Older farmers’ mental health.ajr_1219 23 Aust. J. Rural. Health 2011, 19, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Ellis, N.R.; Albrecht, G.A. Climate change threats to family farmers’ sense of place and mental wellbeing: A case study from the Western Australian Wheatbelt. Soc. Sci. Med. 2017, 175, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Talukder, B.; van Loon, G.W.; Hipel, K.W.; Chiotha, S.; Orbinski, J. Health impacts of climate change on smallholder farmers. One Health 2021, 13, 100258. [Google Scholar] [CrossRef] [PubMed]
- Nagai, K. Environmental changes and mental distress in rural communities. J. Rural. Med. 2023, 18, 159–161. [Google Scholar] [CrossRef]
- Godar, D.E. UV doses worldwide. Photochem. Photobiol. 2005, 81, 736–749. [Google Scholar] [CrossRef]
- Milon, A.; Sottas, P.E.; Bulliard, J.L.; Vernez, D. Effective exposure to solar UV in building workers: Influence of local and individual factors. J. Expo. Sci. Environ. Epidemiol. 2007, 17, 58–68. [Google Scholar] [CrossRef]
- International Agency for Research on Cancer. A Review of Human Carcinogens. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Vol. 100 D—Radiation; IARC: Lyon, France, 2012. [Google Scholar]
- Grandi, C.; Borra, M.; Militello, A.; Polichetti, A. Impact of climate change on occupational exposure to solar radiation. Ann. Ist. Super. Sanità 2016, 52, 343–356. [Google Scholar] [CrossRef]
- Rawlings Parker, E. The influence of climate change on skin cancer incidence—A review of the evidence. Int. J. Women’s Dermatol. 2021, 7, 17–27. [Google Scholar] [CrossRef]
- Barnes, P.W.; Robson, T.M.; Neale, P.J.; Williamson, C.E.; Zepp, R.G.; Madronich, S.; Wilson, S.R.; Andrady, A.L.; Heikkilä, A.M.; Bernhard, G.H.; et al. Environmental effects of stratospheric ozone depletion, UV radiation, and interactions with climate change: UNEP Environmental Effects Assessment Panel, Update 2021. Photochem. Photobiol. Sci. 2022, 21, 275–301. [Google Scholar] [CrossRef]
- Modenese, A.; Korpinen, L.; Gobba, F. Solar radiation exposure and outdoor work: An underestimated occupational risk. Int. J. Environ. Res. Public Health 2018, 15, 2063. [Google Scholar] [CrossRef]
- Neale, R.E.; Lucas, R.M.; Byrne, S.N.; Hollestein, L.; Rhodes, L.E.; Yazar, S.; Young, A.R.; Berwick, M.; Ireland, R.A.; Olsen, C.M. The effects of exposure to solar radiation on human health. Photochem. Photobiol. Sci. 2023, 22, 1011–1047. [Google Scholar] [CrossRef]
- Loney, T.; Paulo, M.S.; Modenese, A.; Gobba, F.; Tenkate, T.; Whiteman, D.C.; Green, A.C.; John, S.M. Global evidence on occupational sun exposure and keratinocyte cancers: A systematic review. Br. J. Dermatol. 2021, 184, 208–218. [Google Scholar] [CrossRef]
- Modenese, A.; Gobba, F. Cataract frequency and subtypes involved in workers assessed for their solar radiation exposure: A systematic review. Acta Ophthalmol. 2018, 96, 779–788. [Google Scholar] [CrossRef]
- Modenese, A.; Gobba, F. Macular degeneration and occupational risk factors: A systematic review. Int. Arch. Occup. Environ. Health 2019, 92, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Bernard, J.J.; Gallo, R.L.; Krutmann, J. Photoimmunology: How ultraviolet radiation affects the immune system. Nat. Rev. Immunol. 2019, 19, 688–701. [Google Scholar] [CrossRef]
- Grandi, C.; D’Ovidio, M.C. The interplay between solar radiation, climate change and immunotoxicants in relation to immune response modulation: A concern for outdoor workers’ health. Am. J. Health Res. 2018, 6, 138–149. [Google Scholar]
- Shin, D.W. Various biological effects of solar radiation on skin and their mechanisms: Implications for phototherapy. Anim. Cells Syst. 2020, 24, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Umar, S.A.; Tasduq, S.A. Ozone layer depletion and emerging public health concerns—An update on epidemiological perspective of the ambivalent effects of ultraviolet radiation exposure. Front. Oncol. 2022, 12, 866733. [Google Scholar] [CrossRef]
- Van der Leun, J.C.; Piacentini, R.D.; de Gruijl, F.R. Climate change and human skin cancer. Photochem. Photobiol. Sci. 2008, 7, 730–733. [Google Scholar] [CrossRef]
- Calapre, L.; Gray, E.S.; Ziman, M. Heat stress: A risk factor for skin carcinogenesis. Cancer Lett. 2013, 337, 35–40. [Google Scholar] [CrossRef]
- Calapre, L.; Gray, E.S.; Kurdykowski, S.; David, A.; Hart, P.; Descargues, P.; Ziman, M. Heat-mediated reduction of apoptosis in UVB-damaged keratinocytes in vitro and in human skin ex vivo. BMC Dermatol. 2016, 16, 6. [Google Scholar] [CrossRef]
- Manisalidis, I.; Stavropoulou, E.; Stavropoulos, A.; Bezirtzoglou, E. Environmental and health impacts of air pollution: A review. Front. Public Health 2020, 8, 14. [Google Scholar] [CrossRef] [PubMed]
- Orru, H.; Ebi, K.L.; Forsberg, B. The interplay of climate change and air pollution on health. Curr. Environ. Health Rep. 2017, 4, 504–513. [Google Scholar] [CrossRef]
- Mallah, A.M.; Changxing, L.; Mallah, A.M.; Noreen, S.; Liu, Y.; Saeed, M.; Xi, H.; Ahmed, B.; Feng, F.; Mirjat, A.A.; et al. Polycyclic aromatic hydrocarbon and its effects on human health: An overeview. Chemosphere 2022, 296, 133948. [Google Scholar] [CrossRef]
- International Agency for Research on Cancer. IARC monographs on the Evaluation of Carcinogenic Risks to Humans. Vol. 109—Outdoor Air Pollution; IARC: Lyon, France, 2016. [Google Scholar]
- Nuvolone, D.; Petri, D.; Voller, F. The effects of ozone on human health. Environ. Sci. Pollut. Res. Int. 2018, 25, 8074–8088. [Google Scholar] [CrossRef] [PubMed]
- Lim, C.C.; Hayes, R.B.; Ahn, J.; Shao, Y.; Silverman, D.T.; Jones, R.R.; Garcia, C.; Bell, M.L.; Thurston, G.D. Long-term exposure to ozone and cause-specific mortality risk in the United States. Am. J. Respir. Crit. Care Med. 2019, 200, 1022–1031. [Google Scholar] [CrossRef]
- Kim, S.Y.; Kim, E.; Kim, W.J. Health effects of ozone on respiratory diseases. Tuberc. Respir. Dis. 2020, 83, S6–S11. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.Y.; Orellano, P.; Lin, H.L.; Jiang, M.; Guan, W.J. Short-term exposure to ozone, nitrogen dioxide, and sulphur dioxide and emergency department visits and hospital admissions due to asthma: A systematic review and meta-analysis. Environ. Int. 2021, 150, 106435. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, C.E.; Kesic, M.J.; Hernandez, M.L. Ozone in the development of pediatric asthma and atopic disease. Immunol Allergy Clin. N. Am. 2022, 42, 701–713. [Google Scholar] [CrossRef]
- Balmes, J.R. Long-term exposure to ozone and small airways: A large impact? Am. J. Respir. Crit. Care Med. 2022, 205, 384–385. [Google Scholar] [CrossRef]
- Kim, K.H.; Kabir, E.; Kabir, S. A review on the human health impact of airborne particulate matter. Environ. Int. 2015, 74, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Pryor, J.T.; Cowley, L.O.; Simonds, S.E. The physiological effects of air pollution: Particulate matter, physiology and disease. Front. Public Health 2022, 10, 882569. [Google Scholar] [CrossRef] [PubMed]
- Gatto, M.P.; Cabella, R.; Gherardi, M. Climate change: The potential impact on occupational exposure to pesticides. Ann. Ist. Super. Sanità 2016, 52, 374–385. [Google Scholar] [CrossRef]
- Fussell, J.C.; Kelly, F.J. Mechanisms underlying the health effects of desert sand dust. Environ. Int. 2021, 157, 106790. [Google Scholar] [CrossRef]
- Sadeghimoghaddam, A.; Khankeh, H.; Norozi, M.; Fateh, A.; Farrokhi, M. Investigating the effects of dust storms on morbidity and mortality due to cardiovascular and respiratory diseases: A systematic review. J. Educ. Health Promot. 2021, 10, 191. [Google Scholar]
- Vonesch, N.; D’Ovidio, M.C.; Melis, P.; Remoli, M.E.; Ciufolini, M.G.; Tomao, P. Climate change, vector-borne diseases and working population. Ann. Ist. Super. Sanità 2016, 52, 397–405. [Google Scholar] [CrossRef]
- Caminade, C.; McIntyre, K.M.; Jones, A.E. Impact of recent and future climate change on vector-borne diseases. Ann. N. Y. Acad. Sci. 2019, 1436, 157–173. [Google Scholar] [CrossRef]
- Chala, B.; Hamde, F. Emerging and re-emerging vector-borne infectious diseases and the challenges for control: A review. Front. Public Health 2021, 9, 715759. [Google Scholar] [CrossRef]
- Semenza, J.C.; Rocklov, J.; Ebi, K.L. Climate change and cascading risks from infectious disease. Infect. Dis. Ther. 2022, 11, 1371–1390. [Google Scholar] [CrossRef]
- Mora, C.; McKenzie, T.; Gaw, I.M.; Dean, J.M.; von Hammerstein, H.; Knudson, T.A.; Setter, R.O.; Smith, C.Z.; Webster, K.M.; Patz, J.A.; et al. Over half of known human pathogenic diseases can be aggravated by climate change. Nat. Clim. Chang. 2022, 12, 869–875. [Google Scholar] [CrossRef]
- Carlson, C.J.; Albery, G.F.; Merow, C.; Trisos, C.H.; Zipfel, C.M.; Eskew, E.A.; Olival, K.J.; Ross, N.; Bansal, S. Climate change increases cross-species viral transmission risk. Nature 2022, 607, 555–562. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Rouse, B.T.; Sarangi, P.P. Did climate change influence the emergence, transmission, and expression of the Covid-19 pandemic? Front. Med. 2021, 8, 769208. [Google Scholar] [CrossRef] [PubMed]
- D’Ovidio, M.C.; Annesi-Maesano, I.; D’Amato, G.; Cecchi, L. Climate change and occupational allergies: An overview on biological pollution, exposure and prevention. Ann. Ist. Super. Sanità 2016, 52, 406–414. [Google Scholar] [CrossRef]
- Pacheco, S.E.; Guidos-Fogelbach, G.; Annesi-Maesano, I.; Pawankar, R.; D’Amato, G.; Latour-Staffeld, P.; Urrutia-Pereira, M.; Kesic, M.J.; Hernandez, M.L.; American Academy of Allergy, Asthma & Immunology Environmental Exposures and Respiratory Health Committee. Climate change and global issues in allergy and Immunology. J. Allergy Clin. Immunol. 2021, 148, 1366–1377. [Google Scholar] [CrossRef]
- Rorie, A. Climate change factors and the aerobiology effect. Immunol. Allergy Clin. N. Am. 2022, 42, 771–786. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Occupational Safety and health (NIOSH). What Is Total Worker Health®? Available online: https://www.cdc.gov/niosh/twh/totalhealth.html (accessed on 1 January 2023).
- Magnavita, N. Workplace health promotion embedded in medical surveillance: The Italian way to Total Worker Health program. Int. J. Environ. Res. Public Health 2023, 20, 3659. [Google Scholar] [CrossRef]
- Bellizzi, S.; Popescu, C.; Panu Napodano, C.M.; Fiamma, M.; Cegolon, L. Global health, climate change and migration: The need for recognition of “climate refugees”. J. Glob. Health 2023, 13, 03011. [Google Scholar] [CrossRef]
- McMichael, C. Climatic and environmental change, migration, and health. Annu. Rev. Public Health 2023, 44, 171–191. [Google Scholar] [CrossRef]
- Messeri, A.; Morabito, M.; Bonafede, M.; Bugani, M.; Levi, M.; Baldasseroni, A.; Binazzi, A.; Gozzini, B.; Orlandini, S.; Nybo, L.; et al. Heat stress perception among native and migrant workers in Italian industries—Case studies from the construction and agricultural sectors. Int. J. Environ. Res. Public Health 2019, 16, 1090. [Google Scholar] [CrossRef]
- Schulte, P.A.; Iavicoli, I.; Fontana, L.; Leka, S.; Dollard, M.F.; Salmen-Navarro, A.; Salles, F.J.; Olympio, K.P.K.; Lucchini, R.; Fingerhut, M.; et al. Occupational safety and health staging framework for decent Work. Int. J. Environ. Res. Public Health 2022, 19, 10842. [Google Scholar] [CrossRef]
- Husic, J.B.; Melero, F.J.; Barakovic, S.; Lameski, P.; Zdravevski, E.; Maresova, P.; Krejcar, O.; Chorbev, I.; Garcia, N.M.; Trajkovik, V. Aging at work: A review of recent trends and future directions. Int. J. Environ. Res. Public Health 2020, 17, 7659. [Google Scholar] [CrossRef]
- Patil, M.; Jeffery, K.J. What does climate change mean for occupational health professionals? Occup. Med. 2020, 70, 386–388. [Google Scholar] [CrossRef] [PubMed]
- Giudice, L.C.; Llamas-Clark, E.F.; DeNicola, N.; Pandipati, S.; Zlatnik, M.G.; Decena, D.C.D.; Woodruff, T.J.; Conry, J.A. The FIGO Committee on Climate Change and Toxic Environmental Exposures. Climate change, women’s health, and the role of obstetricians and gynecologists in leadership. Int. J. Gynecol. Obstet. 2021, 155, 345–356. [Google Scholar] [CrossRef] [PubMed]
- Goshua, A.; Gomez, J.; Erny, B.; Burke, M.; Luby, S.; Sokolow, S.; LaBeaud, D.; Auerbach, P.; Gisondi, M.A.; Nadeau, K. Addressing climate change and its effects on human health: A call to action for medical schools. Acad. Med. 2021, 96, 324–328. [Google Scholar] [CrossRef]
- Fadadu, R.P.; Jayaraman, T.; Teherani, A. Climate and health education for medical students. Clin. Teach. 2021, 18, 362–364. [Google Scholar] [CrossRef]
- Pillai, P.; Patz, J.A.; Seibert, C.S. Climate change and environmental health must be integrated into medical education. Acad. Med. 2021, 96, 1501–1502. [Google Scholar] [CrossRef]
- Auckland, C.; Blumenthal-Barby, J.; Boyd, K.; Earp, B.D.; Frith, L.; Fritz, Z.; McMillan, J.; Shahvisi, A.; Suleman, M. Medical ethics and the climate change emergency. J. Med. Ethics 2022, 48, 939–940. [Google Scholar] [CrossRef]
- Pass Philipsborn, R.; Sheffield, P.; White, A.; Osta, A.; Anderson, M.S.; Bernstein, A. Climate change and the practice of medicine: Essentials for resident education. Acad. Med. 2021, 96, 355–367. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, J.K.; Lowe, K.E.; Gordon, I.O.; Colbert, C.Y.; Salas, R.N.; Bernstein, A.; Utech, J.; Natowicz, M.R.; Mehta, N.; Isaacson, J.H. Climate change and medical education: An integrative model. Acad. Med. 2022, 97, 188–192. [Google Scholar] [CrossRef]
- Dini, G.; Bragazzi, N.L.; Montecucco, A.; Toletone, A.; Debarbieri, N.; Durando, P. Big Data in occupational medicine: The convergence of -omics sciences, participatory research and e-health. Med. Lav. 2019, 110, 102–114. [Google Scholar] [CrossRef]
- Abdelzaher, H.; Tawfik, S.M.; Nour, A.; Abdelkader, S.; Tarek Elbalkiny, S.; Abdelkader, M.; Abbas, W.A.; Abdelnaser, A. Climate change, human health, and the exposome: Utilizing OMIC technologies to navigate an era of uncertainty. Front. Public Health 2022, 10, 973000. [Google Scholar] [CrossRef] [PubMed]
- Kemp, L.; Xuc, C.; Depledge, J.; Ebi, K.L.; Gibbins, G.; Kohler, T.A.; Rockstrom, J.; Scheffer, M.; Schellnhuber, H.J.; Steffen, W.; et al. Climate endgame: Exploring catastrophic climate change scenarios. Proc. Natl. Acad. Sci. USA 2022, 119, e2108146119. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).