The Association between Household Air Pollution and Blood Pressure in Obuasi Municipality, Ghana
Abstract
1. Introduction
2. Methods
2.1. Study Design and Settings
2.2. Study Respondents and Sampling Procedure
2.3. Sample Size Calculation
2.4. Household Air Pollution Exposure Assessment
2.5. Covariates
2.6. Analysis
3. Results
3.1. Overall Demographics
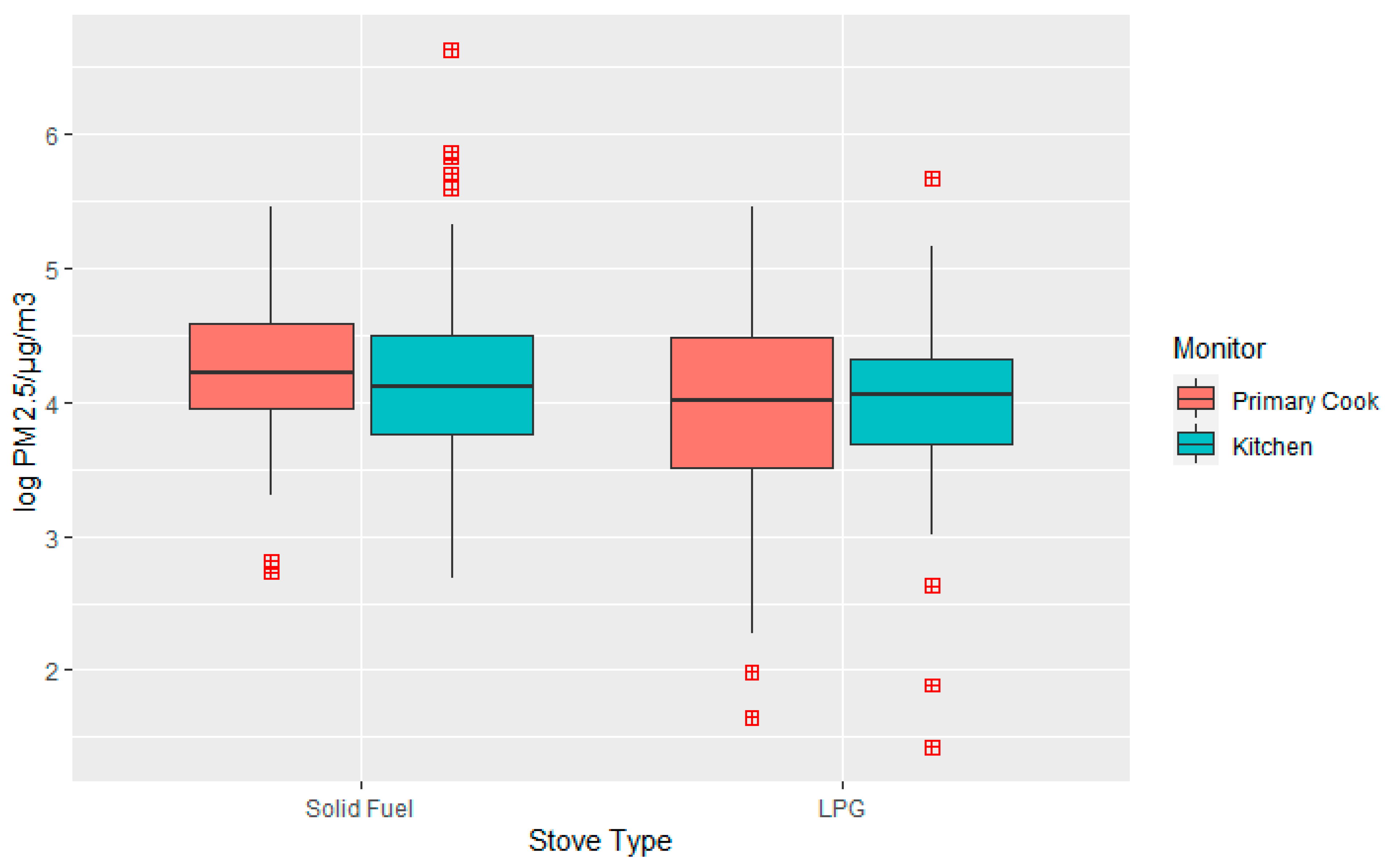
3.2. PM2.5 Concentration by Fuel Type
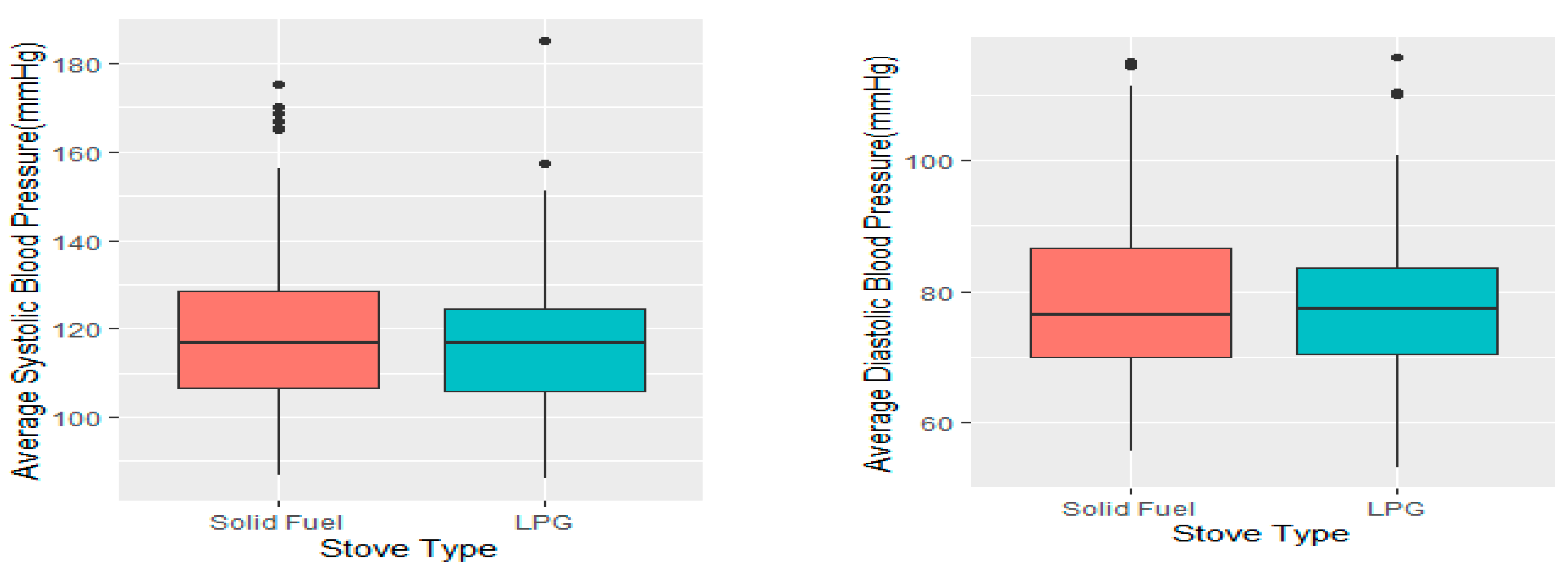
3.3. Average Systolic and Diastolic Blood Pressure
3.4. Relationship between Type of Fuel Use and Blood Pressure
3.5. Exposure–Response Relationship between PM2.5 Exposure and Blood Pressure
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Household Air Pollution and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/household-air-pollution-and-health (accessed on 30 November 2021).
- Dockery, D.W.; Pope, C.A.; Xu, X.; Spengler, J.D.; Ware, J.H.; Fay, M.E.; Ferris, B.G., Jr.; Speizer, F.E. An association between air pollution and mortality in six US cities. N. Engl. J. Med. 1993, 329, 1753–1759. [Google Scholar] [CrossRef] [PubMed]
- Hoek, G.; Brunekreef, B.; Goldbohm, S.; Fischer, P.; van den Brandt, P.A. Association between mortality and indicators of traffic-related air pollution in the Netherlands: A cohort study. Lancet 2002, 360, 1203–1209. [Google Scholar] [CrossRef]
- Lin, H.H.; Murray, M.; Cohen, T.; Colijn, C.; Ezzati, M. Effects of smoking and solid-fuel use on COPD, lung cancer, and tuberculosis in China: A time-based, multiple risk factor, modelling study. Lancet 2008, 372, 1473–1483. [Google Scholar] [CrossRef] [PubMed]
- Gakidou, E.; Afshin, A.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abdulle, A.M.; Abera, S.F.; Aboyans, V.; et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1345–1422. [Google Scholar] [CrossRef]
- Zhou, B.; Bentham, J.; Di Cesare, M.; Bixby, H.; Danaei, G.; Cowan, M.J.; Paciorek, C.J.; Singh, G.; Hajifathalian, K.; Bennett, J.E.; et al. Worldwide trends in blood pressure from 1975 to 2015: A pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet 2017, 389, 37–55. [Google Scholar] [CrossRef] [PubMed]
- Kearney, P.M.; Whelton, M.; Reynolds, K.; Muntner, P.; Whelton, P.K.; He, J. Global burden of hypertension: Analysis of worldwide data. Lancet 2005, 365, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Opie, L.H.; Seedat, Y.K. Hypertension in sub-Saharan African populations. Circulation 2005, 112, 3562–3568. [Google Scholar] [CrossRef]
- Ataklte, F.; Erqou, S.; Kaptoge, S.; Taye, B.; Echouffo-Tcheugui, J.B.; Kengne, A.P. Burden of undiagnosed hypertension in sub-saharan Africa: A systematic review and meta-analysis. Hypertension 2015, 65, 291–298. [Google Scholar] [CrossRef]
- Bosu, W.K.; Bosu, D.K. Prevalence, awareness and control of hypertension in Ghana: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0248137. [Google Scholar] [CrossRef]
- Brook, R.D.; Weder, A.B.; Rajagopalan, S. “Environmental hypertensionology” the effects of environmental factors on blood pressure in clinical practice and research. J. Clin. Hypertens. 2011, 13, 836–842. [Google Scholar] [CrossRef]
- Ghana Statistical Service. Ghana Living Standards Survey Main Report (GLSS 7); Ghana Statistical Service: Accra, Ghana, 2019. [Google Scholar]
- Mensah Mustapha. Cylinder Recirculation Model: Ensures Household Energy Efficiency and Sustainability. 2021. Available online: https://thebftonline.com/2021/10/07/cylinder-recirculation-model-ensures-household-energy-efficiency-and-sustainability/ (accessed on 30 September 2022).
- Ghana Statistical Service. 2010 Population and Housing Census, District Analytical Report, Obuasi Municipality; Ghana Statistical Service: Accra, Ghana, 2014. [Google Scholar]
- Shupler, M.; Baame, M.; Nix, E.; Tawiah, T.; Lorenzetti, F.; Saah, J.; de Cuevas, R.A.; Sang, E.; Puzzolo, E.; Mangeni, J.; et al. Multiple aspects of energy poverty are associated with lower mental health-related quality of life: A modelling study in three peri-urban African communities. SSM Ment. Health 2022, 2, 100103. [Google Scholar] [CrossRef]
- Shupler, M.; Mangeni, J.; Tawiah, T.; Sang, E.; Baame, M.; de Cuevas, R.A.; Nix, E.; Betang, E.; Saah, J.; Twumasi, M.; et al. Modelling of supply and demand-side determinants of liquefied petroleum gas consumption in peri-urban Cameroon, Ghana and Kenya. Nat. Energy 2021, 6, 1198–1210. [Google Scholar] [CrossRef]
- Ofori, S.N.; Fobil, J.N.; Odia, O.J. Household biomass fuel use, blood pressure and carotid intima media thickness; a cross sectional study of rural dwelling women in Southern Nigeria. Environ. Pollut. 2018, 242, 390–397. [Google Scholar] [CrossRef]
- REDCap. Available online: https://projectredcap.org/software/ (accessed on 6 April 2022).
- American Heart Association. Monitoring Your Blood Pressure at Home. Available online: https://www.heart.org/en/health-topics/high-blood-pressure/understanding-blood-pressure-readings/monitoring-your-blood-pressure-at-home (accessed on 30 September 2022).
- Du, W.; Wang, J.; Zhang, S.; Fu, N.; Yang, F.; Wang, G.; Wang, Z.; Mao, K.; Shen, G.; Qi, M.; et al. Impacts of Chinese spring festival on household PM2.5 pollution and blood pressure of rural residents. Indoor Air 2021, 31, 1072–1083. [Google Scholar] [PubMed]
- Okello, G.; Devereux, G.; Semple, S. Women and girls in resource poor countries experience much greater exposure to household air pollutants than men: Results from Uganda and Ethiopia. Environ. Int. 2018, 119, 429–437. [Google Scholar] [CrossRef] [PubMed]
- Van Vliet, E.D.; Asante, K.; Jack, D.W.; Kinney, P.L.; Whyatt, R.M.; Chillrud, S.N.; Abokyi, L.; Zandoh, C.; Owusu-Agyei, R.M. Personal exposures to fine particulate matter and black carbon in households cooking with biomass fuels in rural Ghana. Environ. Res. 2013, 127, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Dionisio, K.; Howie, S.R.C.; Dominici, F.; Fornace, K.; Spengler, J.D.; Adegbola, R.A.; Ezzati, M. Household Concentrations and Exposure of Children to Particulate Matter from Biomass Fuels in The Gambia. Environ. Sci. Technol. 2012, 46, 3519–3527. [Google Scholar] [CrossRef]
- Gould, C.; Schlesinger, S.; Toasa, A.O.; Thurber, M.; Waters, W.F.; Graham, J.P.; Jack, D. Government policy, clean fuel access, and persistent fuel stacking in Ecuador. Energy Sustain. Dev. 2018, 46, 111–122. [Google Scholar] [CrossRef]
- Abdulai, M.A.; Afari-Asiedu, S.; Carrion, D.; Ae-Ngibise, K.A.; Gyaase, S.; Mohammed, M.; Agyei, O.; Boamah-Kaali, E.; Tawiah, T.; Dwommoh, R.; et al. Experiences with the Mass Distribution of LPG Stoves in Rural Communities of Ghana. EcoHealth 2018, 15, 757–767. [Google Scholar] [CrossRef]
- Shankar, A.V.; Quinn, A.K.; Dickinson, K.L.; Williams, K.N.; Masera, O.; Charron, D.; Jack, D.; Hyman, J.; Pillarisetti, A.; Bailis, R.; et al. Everybody stacks: Lessons from household energy case studies to inform design principles for clean energy transitions. Energy Policy 2020, 141, 111468. [Google Scholar] [CrossRef]
- Karanasiou, A.; Alastuey, A.; Amato, F.; Renzi, M.; Stafoggia, M.; Tobias, A.; Reche, C.; Forastiere, F.; Gumy, S.; Mudu, P.; et al. Short-term health effects from outdoor exposure to biomass burning emissions: A review. Sci. Total. Environ. 2021, 781, 146739. [Google Scholar] [CrossRef] [PubMed]
- Amegah, A.K.; Jaakkola, J.J.; Quansah, R.; Norgbe, G.K.; Dzodzomenyo, M. Cooking fuel choices and garbage burning practices as determinants of birth weight: A cross-sectional study in Accra, Ghana. Environ. Health 2012, 11, 78. [Google Scholar] [CrossRef] [PubMed]
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo, J.L., Jr.; Jones, D.W.; Materson, B.J.; Oparil, S.; Wright, J.T., Jr.; et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. JAMA 2003, 289, 2560–2572. [Google Scholar] [CrossRef] [PubMed]
- Ye, W.; Steenland, K.; Quinn, A.; Liao, J.; Balakrishnan, K.; Rosa, G.; Ndagijimana, F.; Ntivuguruzwa, J.d.D.; Thompson, L.M.; McCracken, J.P.; et al. Effects of a liquefied petroleum gas stove intervention on gestational blood pressure: Intention-to-treat and exposure-response findings from the HAPIN trial. Hypertension 2022, 79, 1887–1898. [Google Scholar] [CrossRef] [PubMed]
- Young, B.N.; Clark, M.L.; Rajkumar, S.; Benka-Coker, M.L.; Bachand, A.; Brook, R.D.; Nelson, T.L.; Volckens, J.; Reynolds, S.J.; L’Orange, C.; et al. Exposure to household air pollution from biomass cookstoves and blood pressure among women in rural Honduras: A cross-sectional study. Indoor Air 2018, 29, 130–142. [Google Scholar] [CrossRef] [PubMed]
- Abba, M.S.; Nduka, C.U.; Anjorin, S.; Uthman, O.A. Household Air Pollution and High Blood Pressure: A Secondary Analysis of the 2016 Albania Demographic Health and Survey Dataset. Int. J. Environ. Res. Public Health 2022, 19, 2611. [Google Scholar] [CrossRef]
- Juntarawijit, C.; Juntarawijit, Y. Cooking with biomass fuel and cardiovascular disease: A cross-sectional study among rural villagers in Phitsanulok, Thailand. F1000Research 2020, 9, 307. [Google Scholar]
- Peña, M.B.; Romero, K.M.; Velazquez, E.J.; Davila-Roman, V.G.; Gilman, R.H.; Wise, R.; Miranda, J.J.; Checkley, W. Relationship Between Daily Exposure to Biomass Fuel Smoke and Blood Pressure in High-Altitude Peru. Hypertension 2015, 65, 1134–1140. [Google Scholar] [CrossRef]
- Quinn, A.K.; Ae-Ngibise, K.A.; Kinney, P.L.; Kaali, S.; Wylie, B.J.; Boamah, E.; Shimbo, D.; Agyei, O.; Chillrud, S.N.; Mujtaba, M.; et al. Ambulatory monitoring demonstrates an acute association between cookstove-related carbon monoxide and blood pressure in a Ghanaian cohort. Environ. Health 2017, 16, 76. [Google Scholar] [CrossRef]
| Characteristics | Fuel Type | Total | |
|---|---|---|---|
| SFs n (%) | LPG n (%) | n (%) | |
| Sex | |||
| Female | 175 (98.9) | 166 (96.0) | 341 (97.4) |
| Male | 2 (1.1) | 7 (4.1) | 9 (2.6) |
| Age group | |||
| 18–30 years | 67 (37.8) | 69 (39.9) | 136 (38.9) |
| 31–40 years | 56 (31.6) | 66 (38.2) | 122 (34.9) |
| >40 years | 54 (30.5) | 38 (22.0) | 92 (26.3) |
| Marital status | |||
| Married | 101 (57.1) | 109 (63.0) | 210 (60.0) |
| Unmarried | 76 (42.9) | 64 (37.0) | 140 (40.0) |
| Household head regular cash income | |||
| Yes | 124 (70.1) | 127 (73.4) | 251 (71.7) |
| No | 53 (29.9) | 46 (26.6) | 99 (28.3) |
| Household average monthly income * | |||
| <GH500 (USD 82) | 68 (38.4) | 41 (23.7) | 109 (31.1) |
| GH501–1000 (USD 82–172) | 55 (31.1) | 55 (31.8) | 110 (31.4) |
| >GH1000 (USD 172) | 36 (20.3) | 65 (37.6) | 101 (28.9) |
| Don’t know | 18 (10.1) | 12 (6.9) | 30 (8.6) |
| Primary cook occupation | |||
| Farming | 34 (19.2) | 9 (5.2) | 43 (12.3) |
| Employed | 12 (6.8) | 27 (15.6) | 39 (11.1) |
| Own business | 92 (52.0) | 102 (59.0) | 194 (55.4) |
| Unemployed | 37 (20.9) | 31 (17.9) | 68 (19.4) |
| Other | 2 (1.1) | 4 (2.3) | 6 (1.7) |
| Educational status | |||
| Informal education | 31 (17.5) | 12 (6.9) | 43 (12.3) |
| Formal education | 146 (82.5) | 161 (93.1) | 307 (87.7) |
| Cooking location | |||
| In main house: no separate room | 4 (2.3) | 7 (4.1) | 11 (3.1) |
| In main house: separate room | 23 (13.0) | 42 (24.3) | 65 (18.6) |
| Outside main house: in separate room | 10 (5.7) | 2 (1.2) | 12 (3.4) |
| Outside main house: open air | 32 (18.1) | 7 (4.1) | 39 (11.1) |
| On veranda or covered porch | 108 (61.0) | 115 (66.5) | 223 (63.7) |
| BMI category (kg/m2) | |||
| Underweight (BMI < 18.5) | 4 (2.3) | 1 (0.6) | 5 (1.4) |
| Normal (BMI ≥ 18.5–<25) | 60 (33.9) | 37 (21.4) | 97 (27.7) |
| Overweight (BMI ≥ 25–<30) | 58 (32.8) | 70 (40.5) | 128 (36.6) |
| Obese (BMI ≥ 30) | 52 (29.4) | 60 (34.7) | 112 (32.0) |
| Missing | 3 (1.7) | 5 (2.9) | 8 (2.3) |
| Physically active | |||
| Yes | 94 (53.1) | 111 (64.2) | 205 (58.6) |
| No | 83 (46.9) | 62 (35.8) | 145 (41.4) |
| Emotionally stressed | |||
| Yes | 162 (91.5) | 160 (92.5) | 322 (92.0) |
| No | 15 (8.5) | 13 (7.5) | 28 (8.0 |
| History of known hypertension status | |||
| Yes | 21 (11.9) | 13 (7.5) | 34 (9.7) |
| No | 156 (88.1) | 160 (92.5) | 316 (90.3) |
| Prevalence of heart disease | |||
| Yes | 2 (1.1) | 5 (2.9) | 7 (2.0) |
| No | 175 (98.9) | 168 (97.1) | 343 (98.0) |
| Currently consumed alcohol | |||
| Yes | 9 (5.1) | 9 (5.2) | 18 (5.1) |
| No | 168 (94.9) | 164 (94.8) | 332 (94.9) |
| Does a household member smoke cigarettes? | |||
| Yes | 9 (5.1) | 6 (3.5) | 15 (4.3) |
| No | 168 (94.9) | 167 (96.5) | 335 (95.7) |
| Average heart rate (mean; min–max) (bpm) | 80.8 (55.3–113.3) | 80.5 (45.7–141.7) | 80.6 (45.7–141.7) |
| Outcome per Fuel Type | Coefficient (mmHg) | 95% CI | p-Value | |
|---|---|---|---|---|
| Model 1 | Pre-hypertension | |||
| SFs | Reference | |||
| LPG | 0.28 | −0.23; 0.79 | 0.279 | |
| Model 2 | Stage one hypertension | |||
| SFs | Reference | |||
| LPG | −0.24 | −1.02; 0.53 | 0.542 | |
| Model 3 | Stage two hypertension | |||
| SFs | Reference | |||
| LPG | −0.76 | −1.97; 0.44 | 0.215 |
| Model | Coefficient (mmHg) | 95% CI (mmHg) | p-Value | |
|---|---|---|---|---|
| Systolic blood pressure | ||||
| Adjusted | Log (PM2.5) | −2.42 | −8.65; 3.80 | 0.438 * |
| Diastolic blood pressure | ||||
| Adjusted | Log (PM2.5) | −0.28 | −5.04; 4.48 | 0.960 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tawiah, T.; Shupler, M.; Gyaase, S.; Anderson de Cuevas, R.; Saah, J.; Nix, E.; Twumasi, M.; Quansah, R.; Puzzolo, E.; Pope, D.; et al. The Association between Household Air Pollution and Blood Pressure in Obuasi Municipality, Ghana. Atmosphere 2022, 13, 2033. https://doi.org/10.3390/atmos13122033
Tawiah T, Shupler M, Gyaase S, Anderson de Cuevas R, Saah J, Nix E, Twumasi M, Quansah R, Puzzolo E, Pope D, et al. The Association between Household Air Pollution and Blood Pressure in Obuasi Municipality, Ghana. Atmosphere. 2022; 13(12):2033. https://doi.org/10.3390/atmos13122033
Chicago/Turabian StyleTawiah, Theresa, Matthew Shupler, Stephaney Gyaase, Rachel Anderson de Cuevas, Jason Saah, Emily Nix, Mieks Twumasi, Reginald Quansah, Elisa Puzzolo, Daniel Pope, and et al. 2022. "The Association between Household Air Pollution and Blood Pressure in Obuasi Municipality, Ghana" Atmosphere 13, no. 12: 2033. https://doi.org/10.3390/atmos13122033
APA StyleTawiah, T., Shupler, M., Gyaase, S., Anderson de Cuevas, R., Saah, J., Nix, E., Twumasi, M., Quansah, R., Puzzolo, E., Pope, D., & Asante, K. P. (2022). The Association between Household Air Pollution and Blood Pressure in Obuasi Municipality, Ghana. Atmosphere, 13(12), 2033. https://doi.org/10.3390/atmos13122033








