Indoor Air Quality in Healthcare and Care Facilities: Chemical Pollutants and Microbiological Contaminants
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Sites and Sampling Period
2.2. Building Characteristics
2.3. Sampling Strategies
2.4. Ambient Parameters and PM Measurement
2.5. VOCs and SVOCs Sampling and Analyses
2.6. Microbiological Sampling and Analyses
2.7. Duplicates and Field Blanks
2.8. Statistical Analysis
3. Results
3.1. Ambient Parameters
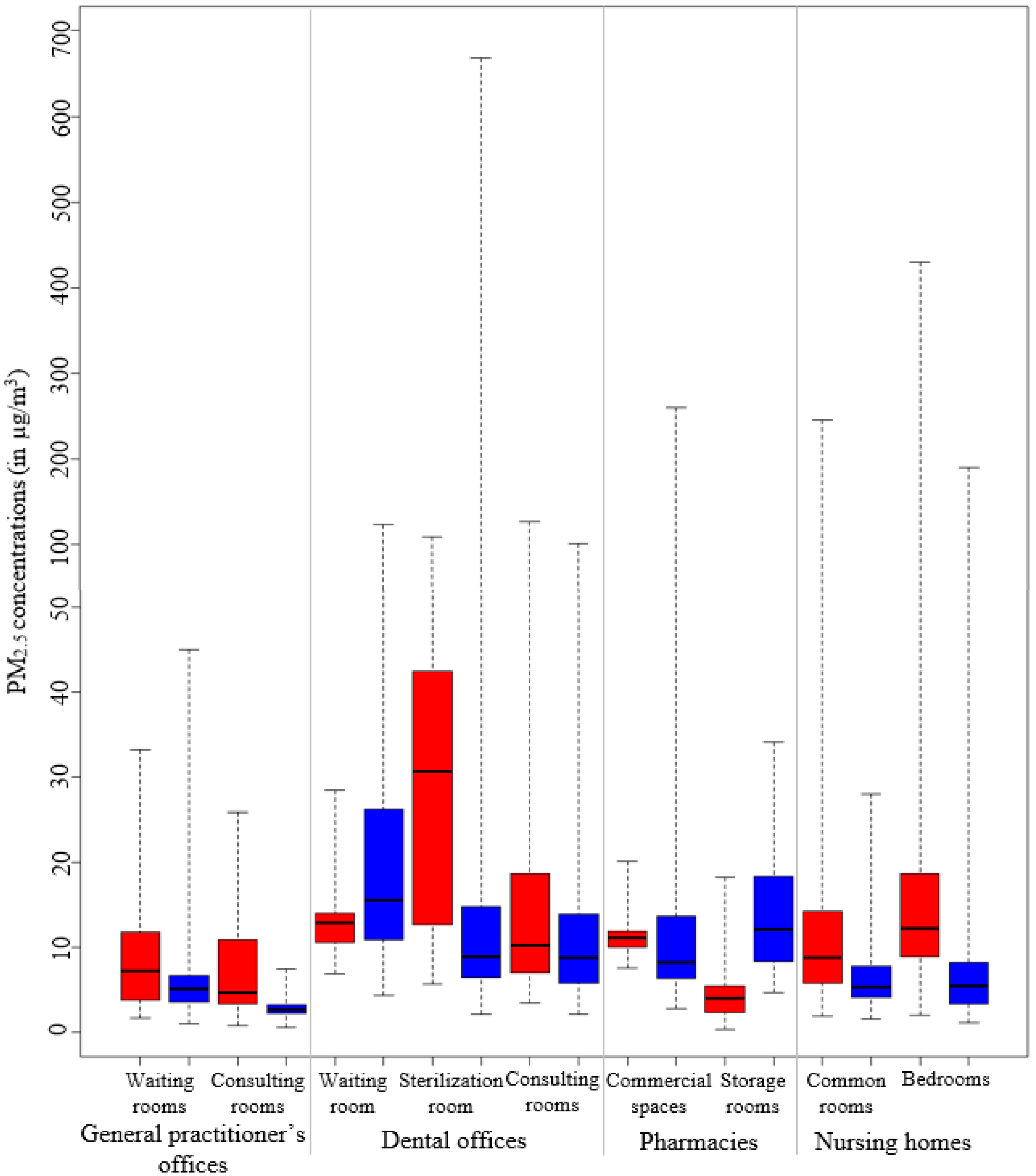
3.2. Particulate Matter
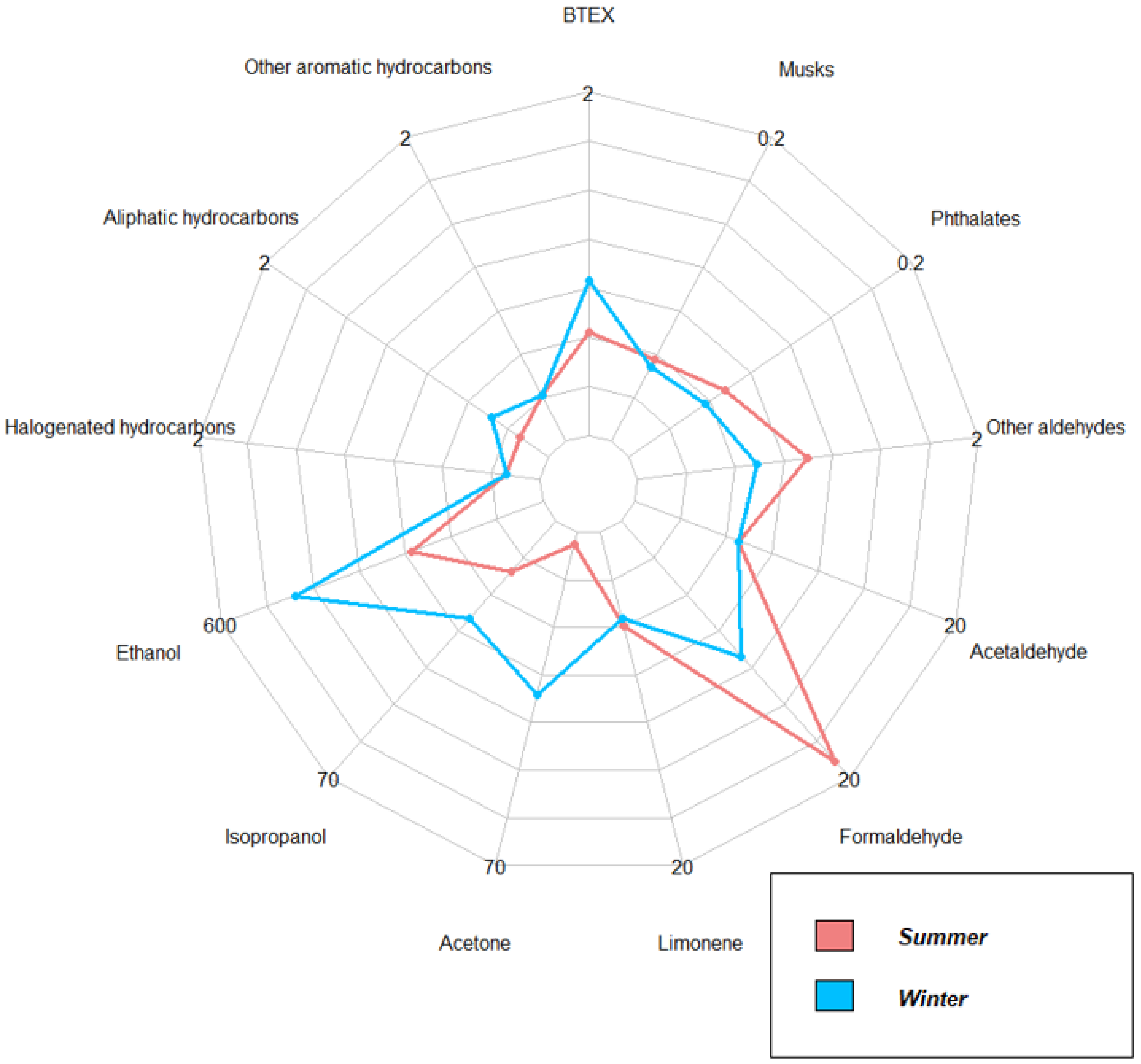
3.3. Organic Compounds: VOCs and SVOCs
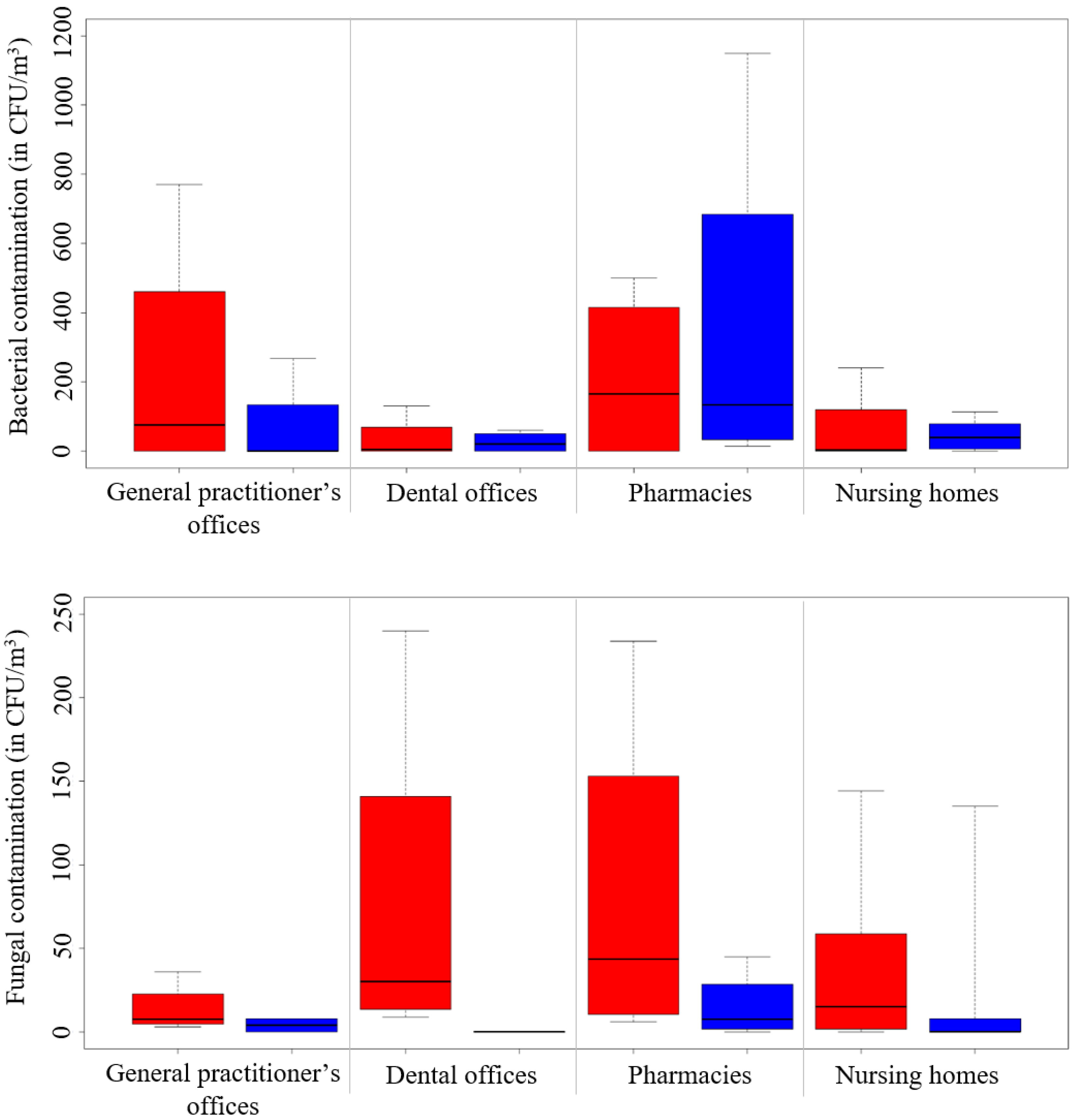
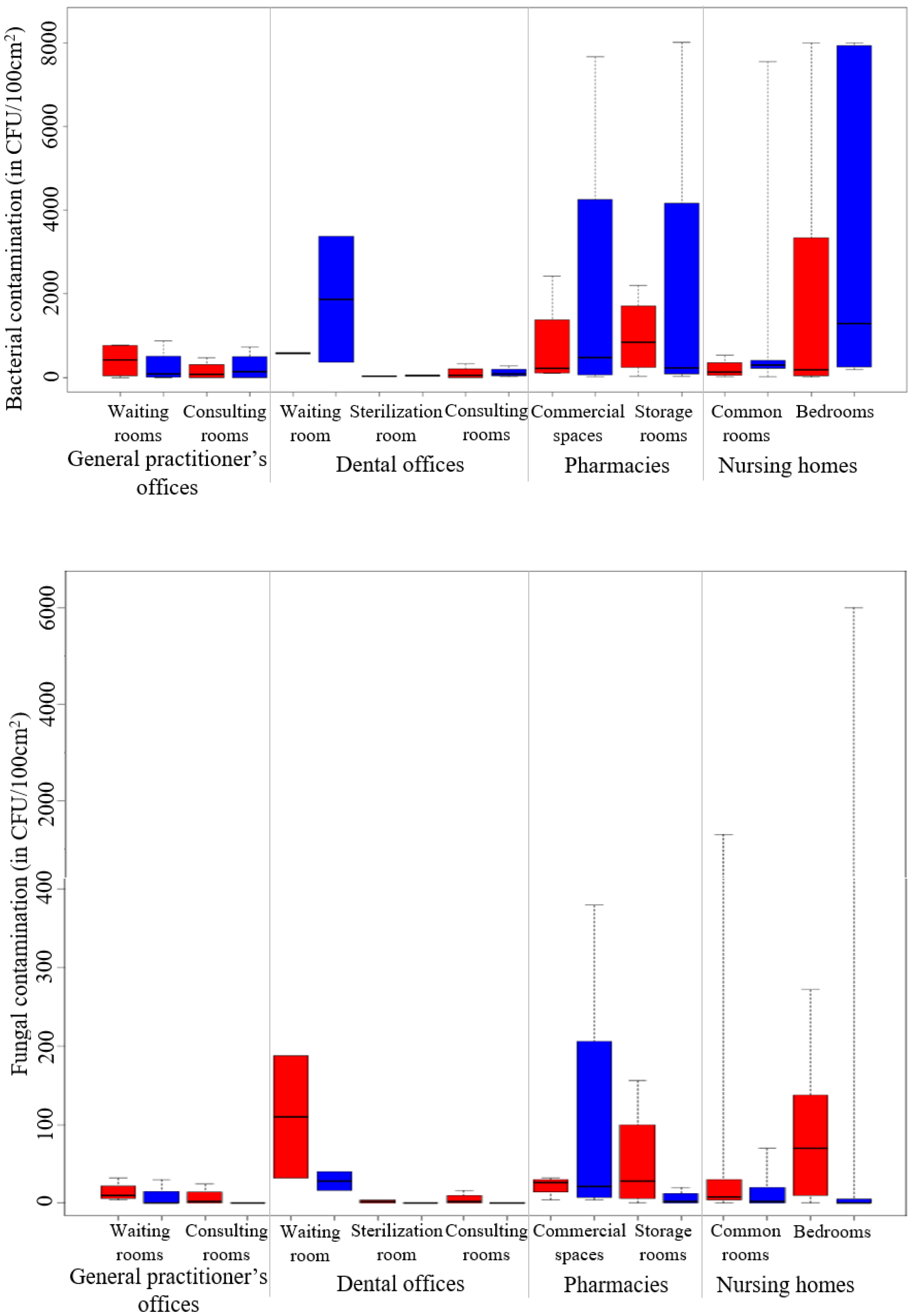
3.4. Microorganisms: Bacteria and Fungi
4. Discussion
4.1. Ambient Parameters
4.2. Particulate Matter (PM2.5)
4.3. Volatile Organic Compounds (VOCs)
4.4. Semi-Volatile Organic Compounds (SVOCs)
4.5. Microorganisms: Bacteria and Fungi
4.6. Strengths and Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Paciência, I.; Madureira, J.; Rufo, J.; Moreira, A.; Fernandes, E. A systematic review of evidence and implications of spatial and seasonal variations of volatile organic compounds (VOC) in indoor human environments. J. Toxicol. Environ. Health B Crit. Rev. 2016, 19, 47–64. [Google Scholar] [CrossRef] [PubMed]
- Huang, Q.; Marzouk, T.; Cirligeanu, R.; Malmstrom, H.; Eliav, E.; Ren, Y.F. Ventilation assessment by carbon dioxide levels in dental treatment rooms. J. Dent. Res. 2021, 100, 810–816. [Google Scholar] [CrossRef]
- Tzoutzas, I.; Maltezou, H.C.; Barmparesos, N.; Tasios, P.; Efthymiou, C.; Assimakopoulos, M.N.; Tseroni, M.; Vorou, R.; Tzermpos, F.; Antoniadou, M.; et al. Indoor Air Quality evaluation using mechanical ventilation and portable air purifiers in an academic dentistry clinic during the COVID-19 pandemic in Greece. Int. J. Environ. Res. Public Health 2021, 18, 8886. [Google Scholar] [CrossRef] [PubMed]
- Helmis, C.G.; Tzoutzas, J.; Flocas, H.A.; Halios, C.H.; Assimakopoulos, V.D.; Stathopoulou, O.I.; Panis, V.; Apostolatou, M. Emissions of total volatile organic compounds and indoor environment assessment in dental clinics in Athens, Greece. Int. Dent. J. 2008, 58, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.H.; Roh, J.; Park, W.M. Evaluation of PM10, CO2, airborne bacteria, TVOCs, and formaldehyde in facilities for susceptible populations in South Korea. Environ. Pollut. 2018, 242, 700–708. [Google Scholar] [CrossRef] [PubMed]
- Almeida-Silva, M.; Almeida, S.M.; Pegas, P.N.; Nunes, T.; Alves, C.A.; Wolterbeek, H.T. Exposure and dose assessment to particle components among an elderly population. Atmos. Environ. 2015, 102, 156–166. [Google Scholar] [CrossRef]
- Bentayeb, M.; Norback, D.; Bednarek, M.; Bernard, A.; Cai, G.; Cerrai, S.; Eleftheriou, K.K.; Gratziou, C.; Holst, G.J.; Lavaud, F.; et al. Indoor air quality, ventilation and respiratory health in elderly residents living in nursing homes in Europe. Eur. Respir J. 2015, 45, 1228–1238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, H.H.; Lee, G.W.; Yang, J.Y.; Jeon, J.M.; Lee, W.S.; Lim, J.Y.; Lee, H.S.; Gwak, Y.K.; Shin, D.C.; Lim, Y.W. Indoor exposure and health risk of polycyclic aromatic hydrocarbons (PAHs) via public facilities PM2.5, Korea (II). Asian J. Atmos. Env. 2014, 8, 35–47. [Google Scholar] [CrossRef] [Green Version]
- Matz, C.J.; Stieb, D.M.; Davis, K.; Egyed, M.; Rose, A.; Chou, B.; Brion, O. Effects of age, season, gender and urban-rural status on time-activity: CanadianHuman Activity Pattern Survey 2 (CHAPS 2). Int. J. Environ. Res. Public Health 2014, 11, 2108–2124. [Google Scholar] [CrossRef] [Green Version]
- Schweizer, C.; Edwards, R.D.; Bayer-Oglesby, L.; Gauderman, W.J.; Ilacqua, V.; Jantunen, M.J.; Lai, H.K.; Nieuwenhuijsen, M.; Künzli, N. Indoor time-microenvironment-activity patterns in seven regions of Europe. J. Expo. Sci. Environ. Epidemiol. 2007, 17, 170–181. [Google Scholar] [CrossRef] [Green Version]
- Le Cann, P.; Bonvallot, N.; Glorennec, P.; Deguen, S.; Goeury, C.; Le Bot, B. Indoor environment and children’s health: Recent developments in chemical, biological, physical and social aspects. Int. J. Hyg. Environ. Health 2011, 215, 1–18. [Google Scholar] [CrossRef]
- Sérafin, G.; Blondeau, P.; Mandin, C. Indoor air pollutant health prioritization in office buildings. Indoor Air 2021, 31, 646–659. [Google Scholar] [CrossRef]
- Pelletier, M.; Bonvallot, N.; Ramalho, O.; Mandin, C.; Wei, W.; Raffy, G.; Mercier, F.; Blanchard, O.; Le Bot, B.; Glorennec, P. Indoor residential exposure to semivolatile organic compounds in France. Environ. Int. 2017, 109, 81–88. [Google Scholar] [CrossRef]
- Fournier, K.; Glorennec, P.; Bonvallot, N. An exposure-based framework for grouping pollutants for a cumulative risk assessment approach: Case study of indoor semi-volatile organic compounds. Environ. Res. 2014, 130, 20–28. [Google Scholar] [CrossRef] [Green Version]
- Tsai, W.T. An overview of health hazards of volatile organic compounds regulated as indoor air pollutants. Rev. Environ. Health 2019, 34, 81–89. [Google Scholar] [CrossRef]
- Bessonneau, V.; Mosqueron, L.; Berrubé, A.; Mukensturm, G.; Buffet-Bataillon, S.; Gangneux, J.P.; Thomas, O. VOC contamination in hospital, from stationary sampling of a large panel of compounds, in view of healthcare workers and patients exposure assessment. PLoS ONE 2013, 8, e55535. [Google Scholar] [CrossRef] [PubMed]
- Zabiegala, B. Organic compounds in indoor environments. Pol. J. Environ. Stud. 2006, 15, 383–393. [Google Scholar]
- Zhang, M.; Zhang, S.; Feng, G.; Su, H.; Zhu, F.; Ren, M.; Cai, Z. Indoor airborne particle sources and outdoor haze days effect in urban office areas in Guangzhou. Environ. Res. 2017, 154, 60–65. [Google Scholar] [CrossRef]
- Benabed, A.; Limam, K. Resuspension of Indoor Particles Due to Human Foot Motion. Energy Procedia 2017, 139, 242–247. [Google Scholar] [CrossRef]
- Kim, K.-H.; Kabir, E.; Kabir, S. A review on the human health impact of airborne particulate matter. Environ. Int. 2015, 74, 136–143. [Google Scholar] [CrossRef]
- Gangneux, J.P.; Bougnoux, M.E.; Hennequin, C.; Godet, C.; Chandenier, J.; Denning, D.W.; Dupont, B.; LIFE Program, the Société Française de Mycologie Médicale SFMM-Study Group. An estimation of burden of serious fungal infections in France. J. Mycol. Med. 2016, 26, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Zemouri, C.; de Soet, H.; Crielaard, W.; Laheij, A. A scoping review on bio-aerosols in healthcare and the dental environment. PLoS ONE 2017, 12, e0178007. [Google Scholar] [CrossRef] [PubMed]
- Beggs, C.; Knibbs, L.D.; Johnson, G.R.; Morawska, L. Environmental contamination and hospital-acquired infection: Factors that are easily overlooked. Indoor Air 2015, 25, 462–474. [Google Scholar] [CrossRef] [Green Version]
- Kurita, H.; Kurashina, K.; Honda, T. Nosocomial transmission of methicillin-resistant Staphylococcus aureus via the surfaces of the dental operatory. Br. Dent. J. 2006, 201, 297–300. [Google Scholar] [CrossRef] [Green Version]
- Baurès, E.; Blanchard, O.; Mercier, F.; Surget, E.; le Cann, P.; Rivier, A.; Gangneux, J.P.; Florentin, A. Indoor air quality in two French hospitals: Measurement of chemical and microbiological contaminants. Sci. Total Environ. 2018, 642, 168–179. [Google Scholar] [CrossRef]
- Ribéron, J.; Ramalho, O.; Derbez, M.; Berthineau, B.; Wyart, G.; Kirchner, S.; Mandin, M. Air stuffiness index: From schools to dwellings. Pollut. Atmosphérique 2016, 228, 1–12. [Google Scholar]
- Dallongeville, A.; Costet, N.; Zmirou-Navier, D.; Le Bot, B.; Chevrier, C.; Deguen, S.; Annesi-Maesano, I.; Blanchard, O. Volatile and semi-volatile organic compounds of respiratory health relevance in French dwellings. Indoor Air 2016, 26, 426–438. [Google Scholar] [CrossRef]
- Mandin, C.; Trantallidi, M.; Cattaneo, A.; Canha, N.; Mihucz, V.G.; Szigeti, T.; Mabilia, R.; Perreca, E.; Spinazzè, A.; Fossati, S.; et al. Assessment of indoor air quality in office buildings across Europe-The OFFICAIR study. Sci. Total Environ. 2017, 579, 169–178. [Google Scholar] [CrossRef] [Green Version]
- Mosqueron, L.; Momas, I.; Le Moullec, Y. Personal exposure of Paris office workers to nitrogen dioxide and fine particles. Occup. Environ. Med. 2002, 59, 550–555. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Langer, S.; Ramalho, O.; Derbez, M.; Ribéron, J.; Kirchner, S.; Mandin, C. Indoor environmental quality in French dwellings and building characteristics. Atmos. Environ. 2016, 128, 82–91. [Google Scholar] [CrossRef]
- Shao, Z.; Yin, X.; Bi, J.; Ma, Z.; Wang, J. Spatiotemporal variations of indoor PM2.5 concentrations in Nanjing, China. Int. J. Environ. Res. Public Health 2019, 16, 144. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization (WHO). WHO Global Air Quality Guidelines: Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide; World Health Organization: Geneva, Swiss, 2021. [Google Scholar]
- Liang, W.; Yang, S.; Yang, X. Long-term formaldehyde emissions from medium-density fiberboard in a full-scale experimental room: Emission characteristics and the effects of temperature and humidity. Environ. Sci. Technol. 2015, 49, 10349–10356. [Google Scholar] [CrossRef]
- Guo, H.; Kwok, N.H.; Cheng, H.R.; Lee, S.C.; Hung, W.T.; Li, Y.S. Formaldehyde and volatile organic compounds in Hong Kong homes: Concentrations and impact factors. Indoor Air 2009, 19, 206–217. [Google Scholar] [CrossRef]
- Spinazzè, A.; Campagnolo, D.; Cattaneo, A.; Urso, P.; Sakellaris, I.A.; Saraga, D.E.; Mandin, C.; Canha, N.; Mabilia, R.; Perreca, E.; et al. Indoor gaseous air pollutants determinants in office buildings-The OFFICAIR project. Indoor Air 2020, 30, 76–87. [Google Scholar] [CrossRef]
- Campagnolo, D.; Saraga, D.E.; Cattaneo, A.; Spinazzè, A.; Mandin, C.; Mabilia, R.; Perreca, E.; Sakellaris, I.; Canha, N.; Mihucz, V.G.; et al. VOCs and aldehydes source identification in European office buildings-The OFFICAIR study. Build. Environ. 2017, 115, 18–24. [Google Scholar] [CrossRef]
- Xiong, J.; Zhang, P.; Huang, S.; Zhang, Y. Comprehensive influence of environmental factors on the emission rate of formaldehyde and VOCs in building materials: Correlation development and exposure assessment. Environ. Res. 2016, 151, 734–741. [Google Scholar] [CrossRef]
- Bornehag, C.G.; Lundgren, B.; Weschler, C.J.; Sigsgaard, T.; Hagerhed-Engman, L.; Sundell, J. Phthalates in indoor dust and their association with building characteristics. Environ. Health Perspect. 2005, 113, 1399–1404. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clausen, P.A.; Liu, Z.; Kofoed-Sørensen, V.; Little, J.; Wolkoff, P. Influence of temperature on the emission of di-(2-ethylhexyl)phthalate (DEHP) from PVC flooring in the emission cell FLEC. Environ. Sci. Technol. 2012, 46, 909–915. [Google Scholar] [CrossRef] [PubMed]
- Castiglia, P.; Liguori, G.; Montagna, M.T.; Napoli, C.; Pasquarella, C.; Bergomi, M.; Fabiani, L.; Monarca, S.; Petti, S.; SItI Working Group Hygiene in Dentistry. Italian multicenter study on infection hazards during dental practice: Control of environmental microbial contamination in public dental surgeries. BMC Public Health 2008, 8, 187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kobza, J.; Pastuszka, J.S.; Bragoszewska, E. Do exposures to aerosols pose a risk to dental professionals? Occup. Med. 2018, 68, 454–458. [Google Scholar] [CrossRef] [Green Version]
- Mendes, A.; Pereira, C.; Mendes, D.; Aguiar, L.; Neves, P.; Silva, S.; Batterman, S.; Teixeira, J.P. Indoor air quality and thermal comfort-results of a pilot study in elderly care centers in Portugal. J. Toxicol. Environ. Health Part A 2013, 76, 333–344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brągoszewska, E.; Biedroń, I. Indoor Air Quality and Potential Health Risk Impacts of Exposure to Antibiotic Resistant Bacteria in an Office Rooms in Southern Poland. Int. J. Environ. Res. Public Health 2018, 15, 2604. [Google Scholar] [CrossRef] [Green Version]
- Bragoszewska, E.; Mainka, A.; Pastuszka, J.S.; Lizonczyk, K.; Desta, Y.G. Assessment of bacterial aerosol in a preschool, primary school and high school in Poland. Atmosphere 2018, 9, 87. [Google Scholar] [CrossRef] [Green Version]
- Fu Shaw, L.; Chen, I.H.; Chen, C.S.; Wu, H.H.; Lai, L.S.; Chen, Y.Y.; Wang, F.D. Factors influencing microbial colonies in the air of operating rooms. BMC Infect Dis. 2018, 18, 4. [Google Scholar] [CrossRef] [Green Version]
- Chang, C.W.; Ting, Y.T.; Horng, Y.J. Collection efficiency of liquid-based samplers for fungi in indoor air. Indoor Air 2019, 29, 380–389. [Google Scholar] [CrossRef]
- Chang, C.W.; Wang, L.J. Impact of culture media and sampling methods on Staphylococcus aureus aerosols. Indoor Air 2015, 25, 488–498. [Google Scholar] [CrossRef] [PubMed]
- Adams, R.I.; Bateman, A.C.; Bik, H.M.; Meadow, J.F. Microbiota of the indoor environment: A meta-analysis. Microbiome 2015, 3, 49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stephens, B. What have we learned about the microbiomes of indoor environments? mSystems 2016, 1, e00083-16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sautour, M.; Sixt, N.; Dalle, F.; L’Ollivier, C.; Fourquenet, V.; Calinon, C.; Paul, K.; Valvin, S.; Maurel, A.; Aho, S.; et al. Profiles and seasonal distribution of airborne fungi in indoor and outdoor environments at a French hospital. Sci. Total Environ. 2009, 407, 3766–3771. [Google Scholar] [CrossRef]
- Gołofit-Szymczak, M.; Górny, R.L. Microbiological air quality in office buildings equipped with dventilation systems. Indoor Air 2018, 28, 792–805. [Google Scholar] [CrossRef]
- Fujiyoshi, S.; Tanaka, D.; Maruyama, F. Transmission of airborne bacteria across built environments and its measurement standards: A review. Front. Microbiol. 2017, 8, 2336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al Maghlouth, A.; Al Yousef, Y.; Al-Bagieh, N.H. Qualitative and quantitative analysis of microbial aerosols in selected areas within the College of Dentistry, King Saud University. Quintessence Int. 2007, 38, e222–e228. [Google Scholar] [PubMed]
- Hefzy, E.M.; Wegdan, A.A.; Abdel Wahed, W.Y. Hospital outpatient clinics as a potential hazard for healthcare associated infections. J. Infect. Public Health 2016, 9, 88–97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grevskott, D.H.; Svanevik, C.S.; Wester, A.L.; Lunestad, B.T. The species accuracy of the Most Probable Number (MPN) European Union reference method for enumeration of Escherichia coli in marine bivalves. J. Microbiol. Methods 2016, 131, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Gangneux, J.P.; Sassi, M.; Lemire, P.; Le Cann, P. Metagenomic Characterization of Indoor Dust Bacterial and Fungal Microbiota in Homes of Asthma and Non-asthma Patients Using Next Generation Se-quencing. Front. Microbiol. 2020, 11, 1671. [Google Scholar] [CrossRef]

| Compounds | Sampling | Sampling Time and Flow Rate | Analysis Methods |
|---|---|---|---|
| Carbon dioxide (CO2) | Passive Class’Air® | 4.5 days | Non-dispersive infrared technology: Class’Air® |
| Particles (PM2.5) | Active pDR1500® | 2.25 days 1.5 L/min | Optic particles count: pDR1500® |
| Aldehydes | Passive 2,4-DNPH cartridge Radielo™ | 4.5 days | HPLC/DAD |
| Other VOCs | Active Carbopack™/Carboxen® tube | 3 h 50 mL/min | Thermal desorption and GC/MS |
| SVOCs | Active Polyurethane foam and quartz filter | 4.5 days 2 L/min | Pressurized liquid extraction and GC/MS/MS |
| Hydrogen peroxide | Active Closed-face cartridge | 6–8 h 1 L/min | Chemical desorption and photometer |
| Microbiological (bacteria and fungi) | Coriolis® air sampler Swabs for surfaces | 10 min–100 L/min Spot sample (100 cm2) | Cultures MALDI-TOF MS or API test |
| Family of Compounds (Number) | Organic Compound |
|---|---|
| Volatile organic compounds (VOCs) (39) | |
| Aromatic hydrocarbons (9) | benzene, ethylbenzene, styrene, toluene, o-xylene, mp-xylenes, 1,2,4-trimethylbenzene, naphthalene, phenol |
| Aliphatic hydrocarbons (3) | n-decane, n-undecane, n-heptane |
| Halogenated hydrocarbons (8) | 1,1,1-trichloroethane, 1,4-dichlorobenzene, trichloroethylene, tetrachloroethylene, bromodichloromethane, dibromochloromethane, tribromomethane, trichloromethane |
| Alcohols (5) | 2-ethyl-1-hexanol, phenoxyethanol, ethanol, isopropanol, n-propanol |
| Ketones (2) | acetone, 2-butanone |
| Terpenes (1) | limonene |
| Ethers (3) | ether, 2-ethoxyethanol, 2-butoxyethanol |
| Peroxides (1) | hydrogen peroxide |
| Aldehydes (7) | formaldehyde, acetaldehyde, propionaldehyde, butyraldheyde, isovaleraldehyde, valeraldehyde, hexaldehyde |
| Semi-volatile organic compounds (SVOCs) (13) | |
| Phthalates (6) | di(2-ethylhexyl)phthalate (DEHP), diethylphthalate (DEP), dibutylphthalate (DBP), diisobutyltphthalate (DiBP), benzylbutylphthalate (BBP), diisononylphthalate (DiNP) |
| Musk (2) | tonalide, galaxolide |
| Pyrethroids (5) | cyfluthrine, cypermethrine, deltamethrine, permethrine, tetramethrine |
| Facilities | Rooms | Day (8 am to 8 pm) | Night (8 pm to 8 am) | ||
|---|---|---|---|---|---|
| Summer | Winter | Summer | Winter | ||
| General practitioner’s offices (n = 2) | Waiting rooms | 0 | 1 | 0 | 0 |
| Consulting rooms | 2 | 2 | 1 | 1 | |
| Dental offices (n = 2) | Waiting room | 0 | 0 | 0 | 0 |
| Sterilization room | 2 | 2 | 1 | 0 | |
| Consulting rooms | 2 | 2 | 1 | 1 | |
| Pharmacies (n = 2) | Commercial spaces | 0 | 0 | 0 | 0 |
| Storage rooms | 1 | 0 | 0 | 0 | |
| Nursing homes (n = 4) | Common rooms | 0 | 0 | 0 | 0 |
| Bedrooms | 0 | 0 | 1 | 0 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baudet, A.; Baurès, E.; Guegan, H.; Blanchard, O.; Guillaso, M.; Le Cann, P.; Gangneux, J.-P.; Florentin, A. Indoor Air Quality in Healthcare and Care Facilities: Chemical Pollutants and Microbiological Contaminants. Atmosphere 2021, 12, 1337. https://doi.org/10.3390/atmos12101337
Baudet A, Baurès E, Guegan H, Blanchard O, Guillaso M, Le Cann P, Gangneux J-P, Florentin A. Indoor Air Quality in Healthcare and Care Facilities: Chemical Pollutants and Microbiological Contaminants. Atmosphere. 2021; 12(10):1337. https://doi.org/10.3390/atmos12101337
Chicago/Turabian StyleBaudet, Alexandre, Estelle Baurès, Hélène Guegan, Olivier Blanchard, Monique Guillaso, Pierre Le Cann, Jean-Pierre Gangneux, and Arnaud Florentin. 2021. "Indoor Air Quality in Healthcare and Care Facilities: Chemical Pollutants and Microbiological Contaminants" Atmosphere 12, no. 10: 1337. https://doi.org/10.3390/atmos12101337
APA StyleBaudet, A., Baurès, E., Guegan, H., Blanchard, O., Guillaso, M., Le Cann, P., Gangneux, J.-P., & Florentin, A. (2021). Indoor Air Quality in Healthcare and Care Facilities: Chemical Pollutants and Microbiological Contaminants. Atmosphere, 12(10), 1337. https://doi.org/10.3390/atmos12101337








