1. Introduction
Ongoing megatrends, such as climate change and urbanization, are projected to globally increase the exposure of populations to heat stress. Growing cities and the densification of cities may lead to a stronger urban heat island (UHI) effect, which may substantially exacerbate health impacts related to heat stress, especially during heatwaves, while on the other hand, reduce exposure to cold stress [
1]. In northern European countries, where severe heatwaves are less frequent than in hotter climates and effective cooling systems in buildings are not common, the UHI effect may be responsible for a large share of heat-related health impacts. In this article, we have modelled temperature–mortality relationships in the city of Helsinki and its wider surrounding region in southern Finland, the Helsinki-Uusimaa hospital district. Our main motivations were to assess, whether the temperature-related mortality would be higher in the capital, compared to the surrounding region, and whether the UHI would have an impact on the temperature-related mortality in Helsinki.
Temperature-mortality relationships are typically found to be U- or J-shaped, and according to earlier studies, this relation applies for Finland, as well [
2,
3,
4]. The major heatwaves in recent decades—in 2003, 2010, 2014 and 2018—have been evaluated to have each caused about 200 to 400 excess deaths in Finland [
5,
6]. Several multicountry studies on temperature-related mortality have used mortality and climate data from Helsinki, as well [
7,
8,
9,
10,
11]. In these studies, Helsinki has been considered as a representative city for the northern European climate or representative for Finland in general, without specific discussion on the role of UHI in temperature-related mortality. However, the UHI may lead to temperatures that are several degrees higher in cities than in surrounding rural areas, and consequently magnifies the exposure of the population to heat stress.
Urban climate studies have been concentrated on mapping or modelling the spatial distribution of the UHI with an aim to understand how characteristics of the cities modify the UHI in single cities. It has been concluded that the UHI effect varies with respect to the city size, land use, topographic factors, vegetation, urbanization and industrialization, season of the year and time of day, as well as with respect to the prevailing meteorological conditions [
12,
13]. Recently some multicity studies have studied the exposure to heat waves and cold waves in urban climates across Europe [
14], as well as the impact of urban characteristics on the vulnerability of the population to heat and cold stress [
15]. However, the universal quantification of the health burden associated with the UHI effect is complex. A study in the West Midlands, UK, assessed that the UHI contributed to almost half of the heat-related mortality [
16]. On the other hand, people acclimatize to their climatic conditions. For instance, a study in London suggested relatively complete acclimatization to the UHI effect on heat–related mortality, but less clear evidence for cold–related mortality [
17].
In Helsinki, Drebs [
18] has previously measured and mapped the UHI over a period of one year and found its intensity to be of about 1 °C in the city centre on an annual level, with a situational variation up to about 4 °C. Furthermore, Kazmierczak [
19] conducted a spatial analysis of social vulnerability to heat-related health impacts in Helsinki by using high-resolution spatial data on demographic and socioeconomic attributes of the population. The study inferred that exposure to high temperatures was high in many of the densely built areas of Helsinki. However, social vulnerability to heat, which is a combination of several indicators, was not especially high in most of the areas due to good adaptive capacity of the residents.
Especially in urban areas, the interaction between air quality and the UHI effect needs to be considered in health impact assessments, including temperature-related mortality. As with the UHI, air quality varies notably geographically, depending on the characteristics and patterns of human activities and the built environment. The near-ground concentrations of pollutant species also vary notably between urban and rural areas, e.g., [
20]. According to a review study [
21], temperature extremes modify the health effects of PM10 and O3 on both nonaccidental and cardiovascular mortality. A study on the Russian heatwave and wildfire in 2010 showed that interaction between high temperatures and air pollution from wildfires had an additive effect and contributed to more than 2000 excess deaths in Moscow [
22]. However, it has been found in previous studies that most of the health-relevant air pollutant concentrations in the Helsinki region were lower than the corresponding values in major central and southern European cities, e.g., in [
23,
24].
The overarching aim of this study was to assess the temperature-related mortality in Helsinki and its surrounding region, with special emphasis on heatwaves. In this study, the day is defined as hot when the daily mean temperature exceeds 20 °C. This criterion is based on the health impact studies [
2,
3,
4] and is used in issuing operational hot weather warnings in Finland. We also assessed the role of air quality in the temperature-related mortality in Helsinki. The specific objectives were:
To model the temperature–mortality relationships in the city of Helsinki and the wider Helsinki-Uusimaa hospital district (HUS) during the period 2000–2018, using distributed lag nonlinear modelling (DLNM).
To assess the deaths attributable to four intensive heatwaves, which occurred in 2003, 2010, 2014 and 2018, in Helsinki and its surroundings.
To evaluate the potential modifying effects of air quality on the temperature-mortality relationship in Helsinki.
This study does not specifically address the influence of the UHI on heat-related mortality in Helsinki, but in the end, we also discuss its potential role in explaining the outcomes.
2. Materials and Methods
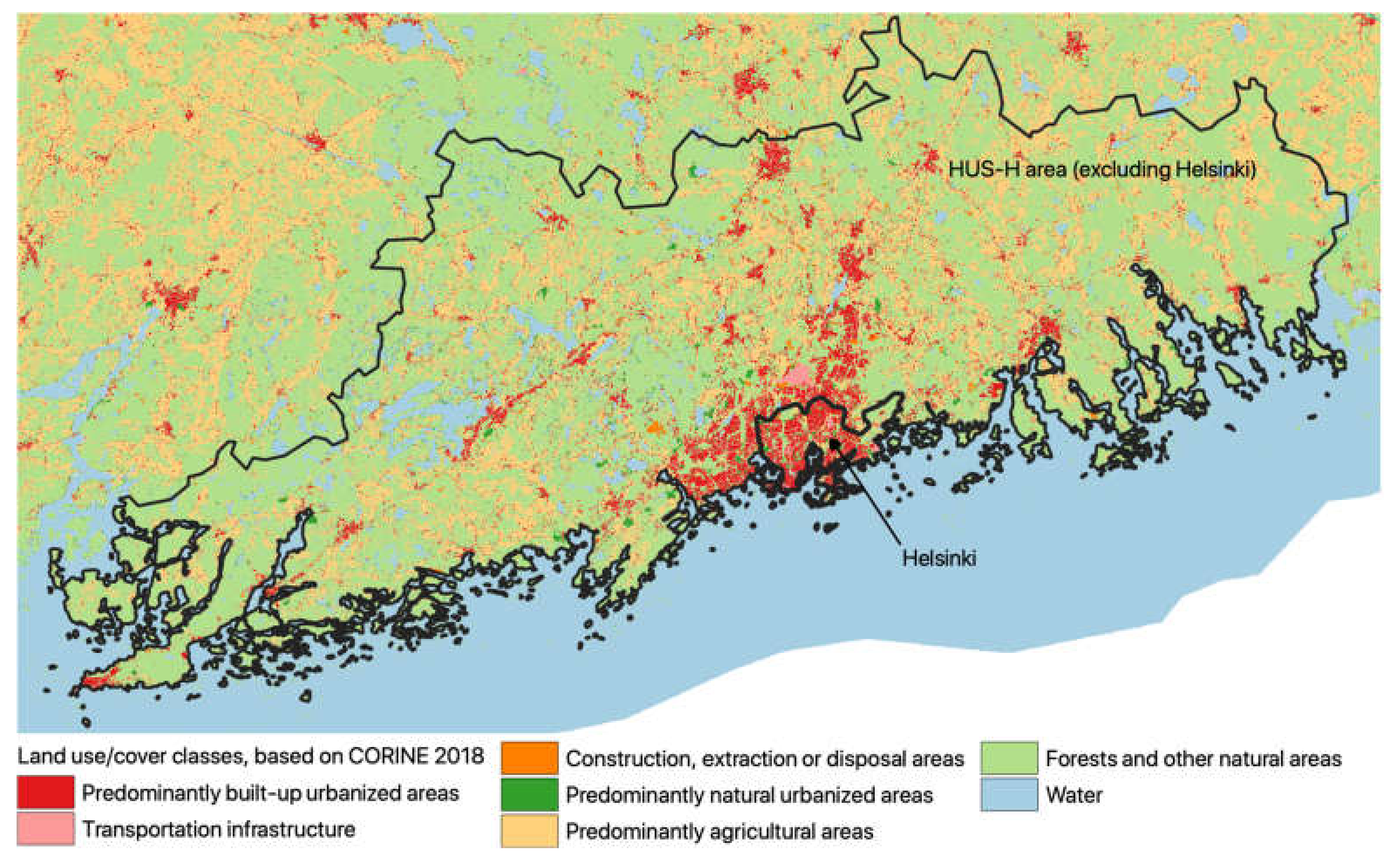
The Helsinki-Uusimaa hospital district (HUS) in southern Finland geographically covers a land area of about 9097 km
2. The capital of Finland, Helsinki, is located within the HUS hospital district by the coast of the Gulf of Finland (
Figure 1). The population in the study area has been growing about 10% per decade: during the study period, 2000–2018, the population in Helsinki increased approx. 18%, from 0.551 to 0.648 million and in HUS (including Helsinki) approx. 21%, from 1.376 to 1.667 million. The elderly population, 75 years or older, increased in Helsinki from 35,000 to 47,000 and in HUS from 69,000 to 117,000. Thus, the share of elderly population increased in Helsinki from 6.3 to 7.2 percent and in HUS from 5.0 to 7.0 percent during the study period. Even though the population in the HUS region surrounding Helsinki is also concentrated in towns and villages, the density of the population in the HUS region is substantially lower than that in the city of Helsinki. In particular, HUS is characterized by a large presence of agricultural, forest, and other natural land uses, in which small towns and villages are scattered in a discontinuous settlement pattern. In contrast, Helsinki is a large and relatively densely populated city, in which the predominant land uses are built-up categories with limited presence of extensive natural land uses.
Time series of the daily numbers of all-cause deaths in the HUS and Helsinki for 2000–2018 (19 years) and annual population were obtained from Statistics Finland. The studies were made for total all-age mortality and separately for the age group of 75 years or older (75+). As meteorological exposure data, we used daily mean ambient temperatures that were calculated as spatial averages for the study areas from the gridded temperature data set on the spatial resolution of 10 × 10 km
2. These data are produced operationally at the Finnish Meteorological Institute (FMI) from the station-wise temperature observations by kriging-interpolation that also takes into account the elevation and the share of water bodies [
25].
Temperature–mortality relationships were modelled by applying distributed lag nonlinear model (DLNM) and quasi-Poisson distribution for the daily number of deaths [
26,
27]. The exposure to temperature was chosen as quadratic B-spline with three equally placed knots for the range of daily mean temperature, and the delayed impact of temperature for 25 days was modelled using 2 knots for the lag on the logarithmic scale. These numbers of knots were based on the findings of our earlier studies and use of the Akaike Information Criterion (AIC) in the selection of the best model [
4]. Long-term trends and seasonal variation were controlled by natural cubic splines with 7 degrees of freedom (df) per year and a day-of-the-week effect was included as a categorical variable.
The temperature–mortality relationships were modelled separately for the whole population and for the elderly (75+) in Helsinki and in the surrounding HUS area, data from Helsinki excluded (denoted in the following as HUS-H). In addition, temperature–mortality modelling was conducted on the whole HUS area, thus including data from Helsinki (see
Supplementary Material). The modelled relationships are presented graphically, and in addition, the relative risks of mortality (RR) at daily mean temperatures of +24, +20, −15 and −20 °C are given in a table. The first two temperatures are used as the thresholds for heat warnings and the remaining values are relevant for cold warnings in Finland, issued by the operational weather forecasting at FMI.
Based on the modelled temperature–mortality relationships, we assessed attributable deaths to selected heatwaves using methods developed by Gasparrini and Leone [
28]. The four major heatwaves, with substantial and previously demonstrated increases in mortality, took place in Finland in the summers of 2003, 2010, 2014 and 2018 [
5,
6]. In this study we compared the mortalities in Helsinki and the surrounding HUS-H area during these heatwaves.
As a sensitivity study, we also modelled the relationships in Helsinki using as an exposure term the daily mean temperatures measured at the Helsinki-Kaisaniemi weather station that is located in a park in downtown Helsinki (see
Supplementary Material).
Air quality may potentially be an important factor with regard to the differences in temperature-related mortality, especially in urban areas. Therefore, the temperature–mortality relationships in Helsinki were also modelled, taking into account the temporal variations of air quality. We considered ozone (O3), as well as respirable (PM10) and fine (PM2.5) particulate matter, measured at the urban background station in Kallio, maintained by the Helsinki Region Environmental Services Authority. The air quality data were included into the model as a confounding factor, using 2-day running mean values of O3, PM10 and PM2.5. This modelling was conducted for various alternative cases: first, by selecting only one of the air quality variables (i.e., a single pollutant concentration) in the analysis, and second, by selecting two air quality variables: O3 and one of the selected particulate matter measures (PM10 or PM2.5).
The analysis was conducted in the R statistical software language and environment with the library “dlnm” [
27,
29].
3. Results
The number of daily all-cause deaths in Helsinki varied between 2 and 31, with a median of 14, and in the surrounding HUS-H area (HUS excluding Helsinki) between 4 and 37 with a median of 16, respectively. Most of the deaths occurred among the elderly: in Helsinki the daily deaths of those aged 75+ varied between 0 and 25, with median of 8 and in HUS-H between 0 and 25 with median of 9. The range of the spatial average of the daily mean temperature, that was used in the modelling, was in Helsinki from −23.7 to 25.9 °C and in HUS-H from −24.9 to 25.7 °C. The highest spatial average of the daily maximum temperature in the study period was in Helsinki 30.8 °C and in HUS-H 31.5 °C, while the lowest daily minimum temperature in Helsinki was −29.1 °C and in HUS-H −30.3 °C. Thus, the temperature ranges were very similar in both regions (Helsinki and HUS-H).
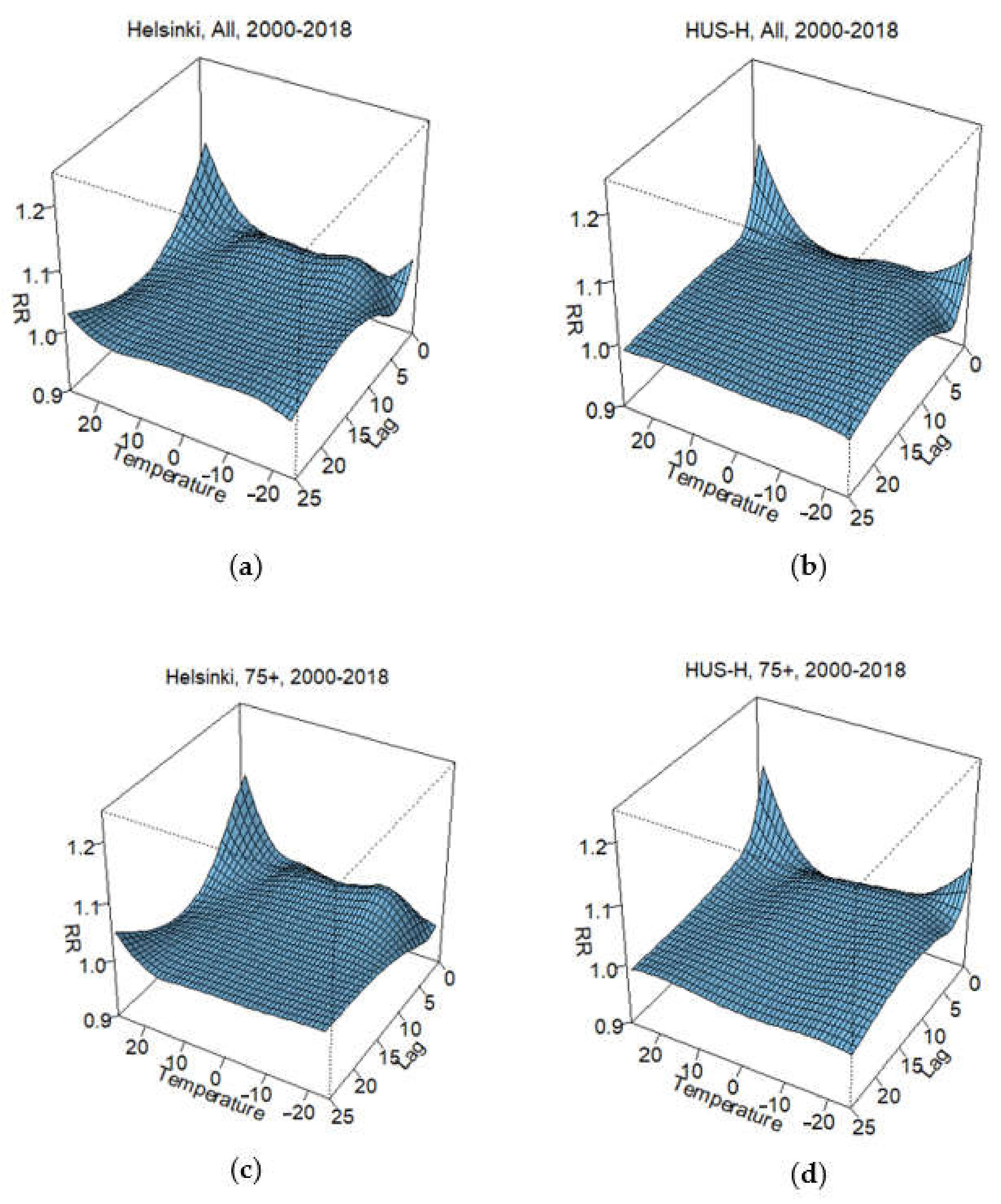
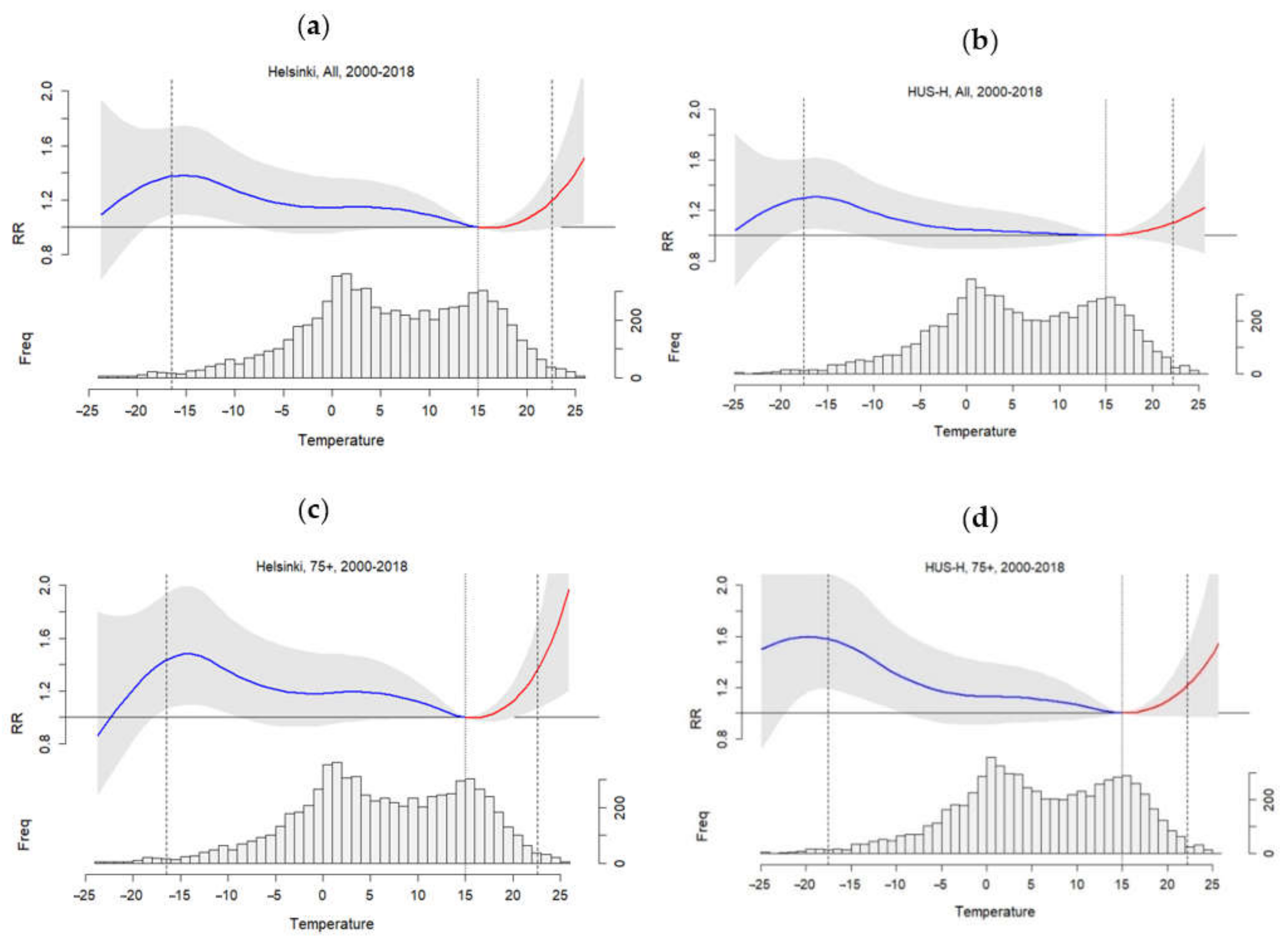
The modelled temperature dependences of all-age and elderly (75+ years) mortality in Helsinki and HUS-H are presented in
Figure 2 and
Figure 3. The 3D visualizations in
Figure 2 show how the modelled relative risk (RR) of mortality varies against both the daily mean temperature range and the lags that range from 0 to 25 days. The graphs in
Figure 3 present overall mortality risk at different temperatures, thus, delayed impacts are aggregated in these graphs. Below the graphs, the frequency distributions of the daily mean temperatures visualize how often various temperatures were observed during the study period. The shapes of the modelled temperature–mortality relationships in
Figure 3 appeared to be fairly similar in all four considered cases. However, the magnitudes of the risks vary according to the age group and the area. The increases in the heat-related mortality risks with increasing temperature were steeper in Helsinki than in HUS-H. Exposure to cold stress increased the risks at the daily level less than that of the heat stress. Based on
Figure 2, at hot extremes, the highest mortality risks were found on the same day and the risks gradually decreased during the next few days. The consequences of cold stress appeared with a longer lag (up to 25 days), also leading to fairly high overall risk for cold-related mortality.
Table 1 shows RR at temperatures relevant for issuing heat and cold warnings in southern Finland. The heat-related RR among the elderly was almost double compared to the all-age risks at the same temperatures; e.g., in Helsinki the all-age RR was 1.06 when the RR of the elderly was 1.12 at the temperature of +20 °C. The cold-related RR of the elderly were also substantially higher than the all-age RR; e.g., in Helsinki, all-age RR was 1.38, while the RR of the elderly was 1.47 at −15 °C. However, at very cold extremes in Helsinki, the all-age mortality risk appeared higher than the risk of the elderly. When compared regionally, both all-age and elderly heat-related risks were higher in Helsinki than in the surrounding HUS-H; e.g., at +24 °C, the all-age RR was 1.30 in Helsinki and 1.16 in HUS-H. Cold-related risks were higher in HUS-H among the elderly, while the all-age risk appeared higher in Helsinki. However, as indicated by the 95% confidence intervals, uncertainties were substantial around the risk estimates at the highest and lowest considered temperatures.
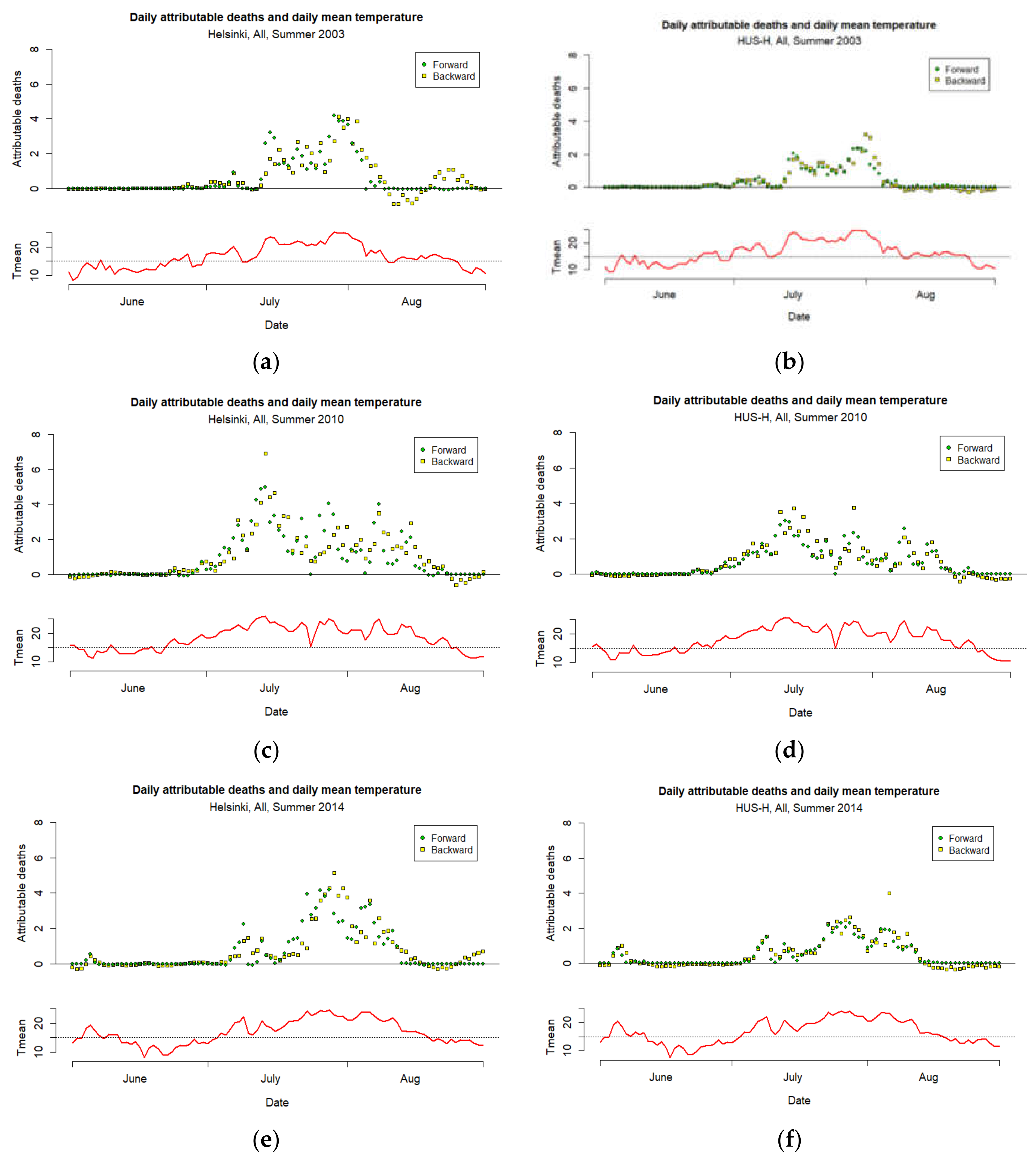
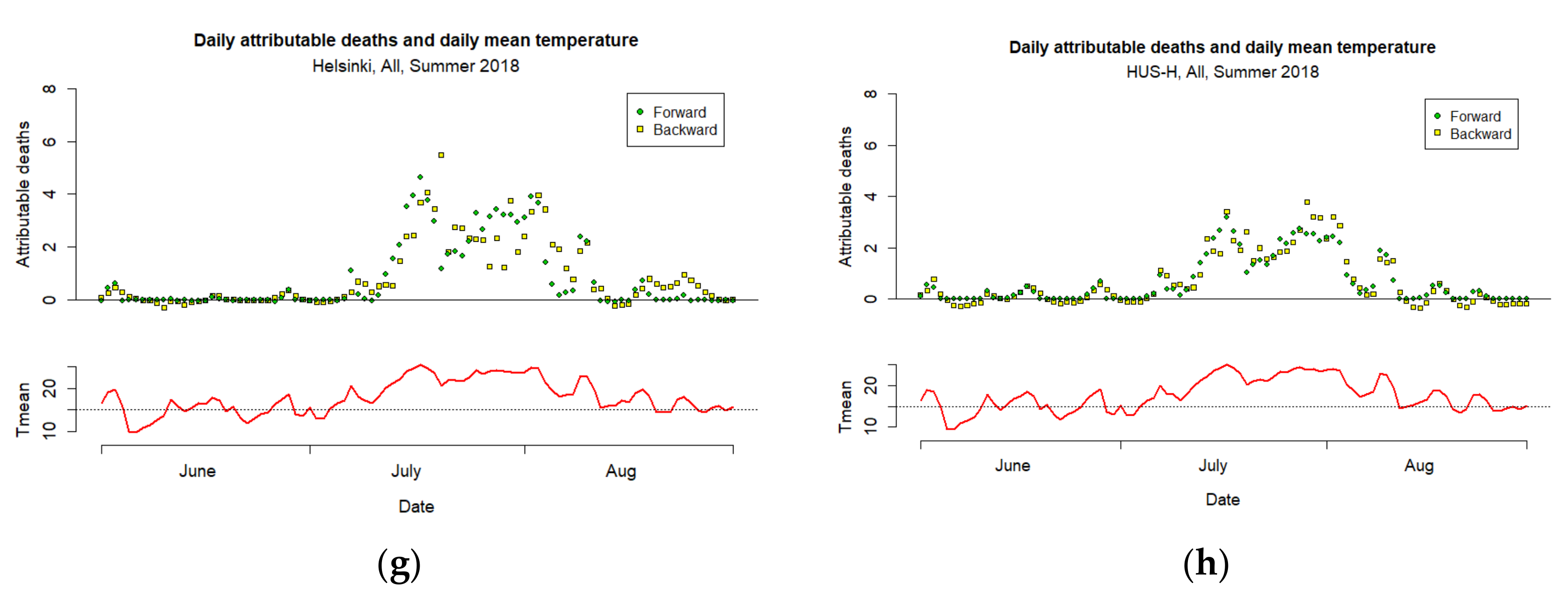
Based on the modelled all-age temperature–mortality relationships,
Figure 4 illustrates heat-related attributable all-age deaths during the four intensive heatwaves in the summers of 2003, 2010, 2014 and 2018 in Helsinki and the surrounding HUS-H. All these heatwaves took place in July–early August and resulted in substantial increases in the number of deaths for a period of a few weeks. In the visualizations, the “forward” perspective refers to the prediction of the number of deaths based on the temperatures, and “backward” to the prediction in which the number of deaths was explained by the temperatures of the previous days.
Table 2 summarizes the number of attributable deaths and related mortality (defined as cases for 100,000 inhabitants: 1/100,000) during the heatwaves. Furthermore, the ratios of the attributable mortality in Helsinki to the mortality in HUS-H are also given.
The results prove that the heat-related mortality risks during these heatwaves were substantially higher in Helsinki, compared with those in the surrounding HUS-H region. According to the number of heat-related attributable deaths and mortality rates, the most severe heatwave was the one in 2010, followed by the heatwaves in 2018, 2014 and 2003. Based on the modelling of the number of attributable deaths during these heatwaves varied in Helsinki between 52 and 93 and in HUS-H between 31 and 58; the heat-related mortality (1/100,000) in Helsinki varied from 9.3 to 15.9, while the heat-related mortality in the surrounding HUS-H region varied from 3.6 to 6.2. Thus, the mortality attributable to the heatwaves was about 2.5-times higher in Helsinki than in HUS-H.
Controlling the temperature–mortality relationship in Helsinki in 2000–2018 by air quality observations revised the temperature related mortality risks only slightly.
Table 3 shows how the relative risk of all-age mortality in Helsinki varied in different model versions that, in addition to temperature, also included exposures to the concentrations of O
3, PM
10 and PM
2.5 concentration. The inclusion of air quality variables did not significantly alter the modelled temperature–mortality relationships, noting the wide confidence intervals of the modelled relationships. However, from the chosen air quality variables, O
3 concentration appeared to have some influence on the risks associated with temperature. Thus, the results suggest that the mortality risks related to heat or cold stress were indeed predominantly driven by ambient temperature, with no or marginal amplification effects of air quality in the Helsinki case.
In the
Supplementary Material we have provided results on the modelling of the temperature–mortality relationships for the whole HUS region, thus Helsinki included (
Figures S1–S3). As a sensitivity analysis of the modelling to the selected data for the exposure, we have also provided outcomes of the modelled relationship using temperature data that are measured in the Helsinki-Kaisaniemi weather station (
Figures S4–S6). Because this FMI weather station is located in the middle of a park (Kaisaniemi) in central Helsinki, it cannot be considered representative either for the whole of Helsinki nor for the densely built areas in Helsinki.
Table S1 reports relative mortality risks at selected temperatures and
Table S2 attributable deaths and mortality to the four heatwaves accordingly.
4. Discussion
The modelled temperature–mortality relationships in 2000–2018, and the case studies on the deaths attributable to four intensive heatwaves, showed differences in temperature-related mortality between the more urbanized Helsinki and the surrounding more rural Helsinki-Uusimaa region. The higher heat-related risks in Helsinki compared to the surrounding HUS-H area could be caused (i) partly by the differences in exposure to high ambient temperatures, and (ii) partly by the differences in adaptive capacity and vulnerability of the population due to the sociodemographic factors, housing and differences between urban and predominantly rural environments. However, it is not possible to assess the relative importance of these factors on the basis of this study.
This study did not specifically address the influence of the UHI on heat-related mortality. However, it has been previously estimated, e.g., that the UHI could have contributed to almost half of the heat-related mortality in the West Midlands in the UK [
16]. We conjecture that the UHI effect may also partly explain the differences in mortality between Helsinki and its surrounding area. The higher temperatures in the more densely built and populated city of Helsinki, compared to the HUS-H region, magnifies the heat stress, and this could result in a relatively higher mortality. The implication is that the land use mix—if taken as a proxy variable—may have a role in temperature-related mortality, although the causal mechanism has to be clarified in future research. In addition, there are also other mechanisms, which influence the heat-related mortalities. These can relate to differences in lifestyles in different settlement types, or to differences in vulnerability characteristics, since households with different demographic characteristics are commonly located in different parts of a metropolitan region.
Furthermore, it is possible that the gridded temperature dataset used in the modelling is too coarse for estimating the actual exposure to the heat stress. Therefore, an urban climate model would be needed for more accurately describing the intensity and finer resolution spatial distribution of the UHI and related heat stress. The first results using the SURFEX air-surface interaction model in Vantaa (medium-sized city within the Helsinki Metropolitan Area) showed as a measure of the UHI effect; e.g., in July a typical temperature difference of 1–2.5 °C between the commercial centre of Vantaa and the nearby National Park in July [
30].
It is worth noting that the chosen method using spatially average temperature as an exposure term does not fully describe the actual exposure of people to thermal stress. An alternative could be the use of population-weighted spatial average temperature as an exposure term, as has been used in some other studies [
16]. However, because the mortality risk also depends on vulnerability of the population to thermal stress, and thus, on the spatial distributions of several factors that affect the vulnerability, use of population-weighted temperature would not adequately solve the problem either. The results clearly show a need for data sets that also include sensitive data from population—such as places of residence and death, social background information etc.—in order to determine both better exposure to thermal stress and social vulnerability. Unfortunately, the information is scarce on the behavioural and social factors, which affect exposure and resilience to heat stress and recovery from it. The inclusion of such effects would require the information on the detailed demographic and diurnal mobility or time-use data in the modelling.
Ambient temperatures within Helsinki and the wider Helsinki-Uusimaa hospital district may vary remarkably, both spatially and temporally. The actual temperature values depend on the weather situation, especially related to the wind direction and impacts of the sea, which vary seasonally in a coastal area. For instance, in summer, a cool breeze from the sea may modify the spatial distribution of UHI in Helsinki and reduce the exposure to the heat stress during heatwaves.
Cold-related mortality risks appeared to be more complex than heat-related mortality. For instance, among the elderly the cold-related mortality risks are higher in HUS-H than in Helsinki, and this difference could partly be explained by less exposure to cold stress in the urban areas. However, behavioural factors probably explain part of the differences. For instance, the elderly in Helsinki may spend less time outdoors during extremely cold weather conditions.
This is the first study assessing the differences in temperature-related mortality in urban and rural environments in Finland. The results show that these impacts are substantially different in the urban area, compared to more rural regions. Such differences should, therefore, be considered in urban planning and climate change adaptation plans. However, the modelling with DLNM is sensitive to the number of daily deaths and the modelling strategy, hence the quantitative results should be interpreted with care. Large uncertainties in the modelled temperature–mortality differences refer to both genuine stochasticity and a fair amount of nonexplained variability attributable to nonobserved factors. We used spatially aggregated daily temperature data, which would not be applicable for assessing the exposure to heat or cold stress at an individual level. On the other hand, this study is in agreement with the findings of the earlier studies on the Finnish population [
3,
4] and extends these with respect to the health impacts in the urban area.
Helsinki has been a growing and quickly developing city for the past couple of decades; these developments have resulted in diminished green areas, which has contributed to an intensifying UHI. In future research, information on the characteristics of the city and the UHI should be combined with social vulnerability mapping, to better understand the health risks related to heat and cold stress. Research towards this direction has been taken, for instance, in the study of Masson et al. [
31]. This will introduce practical knowledge that can be used by practitioners in various stages of urban planning and development.
A second strategic element can be introduced by including climate change scenarios and urban growth forecasts, e.g., in [
32], allowing strategic planners to compare the implications of various urban growth pathways in a changing climate. Both elements—on one hand, the influence of the built-up and social urban environment on temperature-related mortality and, on the other hand, the introduction of future pathway thinking—are approaches that have been long used by designers in cities with more extreme thermal climates, e.g., [
33]. The reintroduction of climate considerations in architectural and urban design is thus a promising addition to our efforts for well-informed, comprehensive adaptation planning.
5. Conclusions
This study reports the modelling of the temperature–mortality relationships and simulations of heatwaves in the city of Helsinki and in the surrounding Helsinki-Uusimaa hospital district. The results demonstrated that the heat-related mortality risks are clearly higher in Helsinki compared with the surrounding mainly rural region, and we conjecture that the relatively higher mortality values could be partly attributable to UHI in Helsinki. Yet, to confirm this attribution, follow-up research is necessary.
In the modelling, as an exposure term we applied the gridded observational temperature data on a resolution of 10 × 10 km
2, which does not resolve the fine-scale spatial variations of the exposure to heat or cold stress in an urban area. The higher heat-related mortality in Helsinki suggests that this fairly coarse resolution gridded temperature data underestimated the actual exposure to the heat stress. For a detailed investigation of the spatial distribution of the UHI and related health impacts, one would need to use an urban climate model [
31].
Short-term health impacts of air quality in Helsinki were found to be substantially smaller, compared with those of the thermal stress. This was probably caused by the relatively low pollutant concentrations in Helsinki, compared with, e.g., most major cities in central or southern Europe. However, this effect can be substantial for many other cities, and also in Helsinki during specific episodic periods. We therefore recommend including the effects of air quality on the temperature–mortality relationships as a confounding factor.
Future challenges remain to understand (i) how the magnitude and spatial distribution of UHI varies in terms of the weather situations and (ii) how the exposure to thermal stress varies among vulnerable population subgroups. Further studies are also needed to understand the role of social vulnerability and the demographic factors in explaining the relatively higher heat-related mortality in Helsinki, as compared with the surrounding and mostly rural region.
Tailored climate services would be relevant in communicating the complexity of health risks related to temperature extremes in urban areas. The findings and conclusions of this study can be used in urban planning, in the urban and neighbourhood design, and in designing climate change adaptation plans.
Supplementary Materials
The following are available online at
https://www.mdpi.com/2073-4433/12/1/46/s1, Figure S1: Relative risk (RR) of all-cause mortality as a function of daily mean temperature and lag (days) in the Helsinki-Uusimaa hospital district (HUS) in 2000–2018. Figure S2: Overall cumulative mortality risks (RR) as a function or daily mean temperature and frequency distribution of daily mean temperature in 2000–2018 in the Helsinki-Uusimaa hospital district (HUS). Figure S3: Daily deaths attributable to heat in summers 2003, 2010, 2014 and 2018 and daily mean temperature in HUS based on the modelled temperature–mortality relationship during 2000–2018. Figure S4: Relative risk (RR) of all-cause mortality as a function of daily mean temperature and lag (days) in Helsinki in 2000–2018. Temperature data from the Helsinki-Kaisaniemi weather station. Figure S5: Overall cumulative mortality risks (RR) as a function or daily mean temperature and frequency distribution of daily mean temperature in Helsinki in 2000–2018. Figure S6: Daily deaths attributable to heat in summers 2003, 2010, 2014 and 2018 and daily mean temperature in Helsinki based on the modelled temperature–mortality relationship during 2000–2018. Table S1: Relative risks (RR) of all-age and 75+ mortality (with 95% confidence interval) at selected daily mean temperatures (Tmean) in Helsinki and in Helsinki-Uusimaa hospital district based on modelled temperature–mortality relationship 2000–2018 visualized in Figures S2 and S5. Table S2: Number of deaths and mortality (1/100,000) attributable to daily mean temperature exceeding +20 °C during heatwaves in the city of Helsinki and Helsinki-Uusimaa hospital district (HUS) in 2003, 2010, 2014 and 2018, based on simulation visualized in Figures S3 and S6.
Author Contributions
Conceptualization, R.R., J.K. and K.J.; methodology, R.R.; software, R.R.; validation, R.R.; formal analysis, R.R.; investigation, R.R.; resources, R.R., A.V.; data curation, R.R.; writing—original draft preparation, R.R.; writing—review and editing, all authors; visualization, R.R., A.V., supervision, J.K., K.J., S.K.; project administration, A.P., J.K., R.R., K.J.; funding acquisition A.P., J.K., R.R., K.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by following projects: URCLIM (Advance on Urban Climate Services—EU Era4CS, grant number 690462), EXHAUSTION (Exposure to heat and air pollution in Europe—cardio-pulmonary impacts and benefits of mitigation and adaptation—EU Horizon2020, grant number 820655), CHAMPS (Climate change and Health: Adapting to Mental, Physical and Societal challenges, project number 329225) and HEATCLIM (Heat and health in the changing climate, project number 329307) within the CLIHE-programme (Climate change and health, Academy of Finland), and GLORIA (Global health risks related to atmospheric composition and weather—Academy of Finland, project number 310373).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Patient consent was not required because in this study no individual data have been used or produced, nor can the data be linked to individuals.
Data Availability Statement
Daily mortality data was obtained from Statistics Finland and are available from the authors with the permission of Statistics Finland. Publicly available gridded temperature datasets were used in this study. This data can be found here:
https://paituli.csc.fi. Publicly available air quality datasets can be found here:
https://www.ilmatieteenlaitos.fi/havaintojen-lataus.
Acknowledgments
We also thank Pentti Pirinen from the Finnish Meteorological Institute for providing the gridded temperature dataset for the research.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Heaviside, C.; Macintyre, H.; Vardoulakis, S. The Urban Heat Island: Implications for Health in a Changing Environment. Curr. Environ. Heal. Rep. 2017, 4, 296–305. [Google Scholar] [CrossRef] [PubMed]
- Näyhä, S. Environmental temperature and mortality. Int. J. Circumpolar Health 2005, 64, 451–458. [Google Scholar] [CrossRef] [PubMed]
- Ruuhela, R.; Jylhä, K.; Lanki, T.; Tiittanen, P.; Matzarakis, A. Biometeorological assessment of mortality related to extreme temperatures in Helsinki region, Finland, 1972–2014. Int. J. Environ. Res. Public Health 2017, 14, 944. [Google Scholar] [CrossRef] [PubMed]
- Ruuhela, R.; Hyvärinen, O.; Jylhä, K. Regional Assessment of Temperature-Related Mortality in Finland. Int. J. Environ. Res. Public Health 2018, 15, 406. [Google Scholar] [CrossRef] [PubMed]
- Kollanus, V.; Lanki, T. 2000-Luvun Pitkittyneiden Helleaaltojen Kuolleisuusvaikutukset Suomessa. (Mortality Effects of Prolonged Heat Waves in the 2000s in Finland. Summary in English). Duodecim 2014, 983–990. Available online: http://www.terveysportti.fi/xmedia/duo/duo11638.pdf (accessed on 10 June 2020).
- Finnish Institute for Health and Welfare (THL). 2019. Available online: https://thl.fi/en/web/thlfi-en/-/last-summer-s-heat-wave-increased-the-mortality-of-older-people-prepare-for-hot-weather-in-time (accessed on 10 June 2020).
- Baccini, M.; Biggeri, A.; Accetta, G.; Kosatsky, T.; Katsouyanni, K.; Analitis, A.; Anderson, H.R.; Bisanti, L.; D’Iippoliti, D.; Danova, J.; et al. Heat effects on mortality in 15 European cities. Epidemiology 2008, 19, 711–719. [Google Scholar] [CrossRef]
- De’Donato, F.K.; Leone, M.; Scortichini, M.; De Sario, M.; Katsouyanni, K.; Lanki, T.; Basagaña, X.; Ballester, F.; Åström, C.; Paldy, A.; et al. Changes in the effect of heat on mortality in the last 20 years in nine European cities. Results from the PHASE project. Int. J. Environ. Res. Public Health 2015, 12, 15567–15583. [Google Scholar] [CrossRef]
- Gasparrini, A.; Guo, Y.; Sera, F.; Vicedo-Cabrera, A.M.; Huber, V.; Tong, S.; de Sousa Zanotti Stagliorio Coelho, M.; Nascimento Saldiva, P.H.; Lavigne, E.; Matus Correa, P.; et al. Projections of temperature-related excess mortality under climate change scenarios. Lancet Planet. Health 2017, 1, 360–367. [Google Scholar] [CrossRef]
- Gosling, S.; Hondula, D.; Bunker, A.; Ibarreta, D.; Liu, J.; Zhang, X.; Sauerborn, R. Adaptation to climate change: A comparative analysis of modelling methods for heat-related mortality. Environ. Health Perspect. 2017, 125. [Google Scholar] [CrossRef]
- Kendrovski, V.; Baccini, M.; Martinez, G.S.; Paunovic, E.; Menne, B. Quantifying Projected Heat Mortality Impacts under 21st-Century Warming Conditions for Selected European Countries. Int. J. Environ. Res. Public Health 2017, 14, 729. [Google Scholar] [CrossRef]
- Tzavali, A.; Paravantis, J.P.; Mihalakakou, G.; Fotiadi, A.; Stigka, E. Urban heat island intensity: A literature review. Fresenius Environ. Bull. 2015, 24, 4537–4554. [Google Scholar]
- Santamouris, M. Analyzing the heat island magnitude and characteristics in one hundred Asian and Australian cities and regions. Sci. Total Environ. 2015, 512, 582–598. [Google Scholar] [CrossRef] [PubMed]
- Smid, M.; Russo, S.; Costa, A.C.; Granell, C.; Pebesma, E. Urban Climate Ranking European capitals by exposure to heat waves and cold waves. Urban Clim. 2019, 27, 388–402. [Google Scholar] [CrossRef]
- Sera, F.; Armstrong, B.; Tobias, A.; Vicedo-cabrera, A.M.; Christofer, A.; Bell, M.L.; Chen, B.; De Sousa, M.; Stagliorio, Z.; Correa, P.M.; et al. How urban characteristics affect vulnerability to heat and cold: A multi-country analysis. Int. J. Epidemiol. 2019, 48, 1101–1112. [Google Scholar] [CrossRef] [PubMed]
- Heaviside, C.; Vardoulakis, S.; Cai, X.M. Attribution of mortality to the urban heat island during heatwaves in the West Midlands, UK. Environ. Health 2016, 15. [Google Scholar] [CrossRef] [PubMed]
- Milojevic, A.; Armstrong, B.G.; Gasparrini, A.; Bohnenstengel, S.I.; Barratt, B.; Wilkinson, P. Methods to Estimate Acclimatization to Urban Heat Island Effects on Heat- and Cold-Related Mortality. Environ. Health Perspect. 2016. [Google Scholar] [CrossRef]
- Drebs, A. Helsingin Lämpösaareke Ajallisena ja Paikallisena Ilmiönä. (Helsinki Urban Heat Island as Temporal and Spatial Phenomena, Abstract in English). Master’s Thesis, University of Helsinki, Helsinki, Finland, 2011. Available online: http://urn.fi/URN:NBN:fi-fe201201121058 (accessed on 10 June 2020).
- Kazmierczak, A. Analysis of Social Vulnerability to Climate Change in Helsinki Metropolitan Area. Final Report 2015. Helsinki Region Environmental Services Authority. Available online: https://www.hsy.fi/sites/Esitteet/EsitteetKatalogi/Raportit/HSY-Ilmastolahtoinen-sosiaalinen-haavoittuvuus.pdf (accessed on 10 June 2020).
- Van Donkelaar, A.; Martin, R.V.; Brauer, M.; Hsu, N.C.; Kahn, R.A.; Levy, R.C.; Lyapustin, A.; Sayer, A.M.; Winker, D.M. Global Estimates of Fine Particulate Matter using a Combined Geophysical-Statistical Method with Information from Satellites, Models, and Monitors. Environ. Sci. Technol. 2016, 50, 3762–3772. [Google Scholar] [CrossRef]
- Li, J.; Woodward, A.; Hou, X.Y.; Zhu, T.; Zhang, J.; Brown, H.; Yang, J.; Qin, R.; Gao, J.; Gu, S.; et al. Modification of the effects of air pollutants on mortality by temperature: A systematic review and meta-analysis. Sci. Total Environ. 2017, 575, 1556–1570. [Google Scholar] [CrossRef]
- Shaposhnikov, D.; Revich, B.; Bellander, T.; Bedada, G.B.; Bottai, M.; Kharkova, T.; Kvasha, E.; Lezina, E.; Lind, T.; Semutnikova, E.; et al. Mortality Related to Air Pollution with the Moscow Heat Wave and Wildfire of 2010. Epidemiology 2014, 25, 359–364. [Google Scholar] [CrossRef]
- Kukkonen, J.; López-Aparicio, S.; Segersson, D.; Geels, C.; Kangas, L.; Kauhaniemi, M.; Maragkidou, A.; Jensen, A.; Assmuth, T.; Karppinen, A.; et al. The influence of residential wood combustion on the concentrations of PM2.5 in four Nordic cities. Atmos. Chem. Phys. 2020, 20, 4333–4365. [Google Scholar] [CrossRef]
- Kukkonen, J.; Karl, M.; Keuken, M.P.; Denier Van Der Gon, H.A.C.; Denby, B.R.; Singh, V.; Douros, J.; Manders, A.; Samaras, Z.; Moussiopoulos, N.; et al. Modelling the dispersion of particle numbers in five European cities. Geosci. Model Dev. 2016, 9, 451–478. [Google Scholar] [CrossRef]
- Aalto, J.; Pirinen, P.; Jylhä, K. New gridded daily climatology of Finland: Permutation-based uncertainty estimates and temporal trends in climate. J. Geophys. Res. Atmos. 2016, 121, 3807–3823. [Google Scholar] [CrossRef]
- Gasparrini, A.; Armstrong, B.; Kenward, M.G. Distributed lag non-linear models. Stat. Med. 2010, 29, 2224–2234. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A. Distributed Lag Linear and Non-Linear Models in R: The Package dlnm. J. Stat. Softw. 2011, 43, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A.; Leone, M. Attributable risk from distributed lag models. BMC Med. Res. Methodol. 2014, 14, 55. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020; Available online: https://www.R-project.org (accessed on 10 June 2020).
- Saranko, O.; Fortelius, C.; Jylhä, K.; Ruosteenoja, K.; Brattich, E.; Di Sabatino, S.; Nurmi, V. Impacts of town characteristics on the changing urban climate in Vantaa. Sci. Total Environ. 2020, 727, 138471. [Google Scholar] [CrossRef]
- Masson, V.; Heldens, W.; Bocher, E.; Bonhomme, M.; Bucher, B.; Burmeister, C.; de Munck, C.; Esch, T.; Hidalgo, J.; Kanani-Sühring, F.; et al. City-descriptive input data for urban climate models: Model requirements, data sources and challenges. Urban Clim. 2020, 31, 100536. [Google Scholar] [CrossRef]
- Votsis, A. Utilizing a cellular automaton model to explore the influence of coastal flood adaptation strategies on Helsinki’s urbanization patterns. Comput. Environ. Urban Syst. 2017, 64, 344–355. [Google Scholar] [CrossRef]
- Givoni, B. Climate Considerations in Building and Urban Design; John Wiley & Sons: Hoboken, NJ, USA, 1998. [Google Scholar]
Figure 1.
Overview of simplified CORINE 2018 land use/cover categories in the study areas: HUS is indicated by the outer black border; Helsinki by the inner black border; HUS-H area (HUS excluding Helsinki) by the area between the outer and inner borders. Land use/cover categories are indicated in the legend: red, orange or purple colours indicate predominantly urbanised areas, whereas yellow, green and blue colours indicate predominantly rural or natural areas.
Figure 1.
Overview of simplified CORINE 2018 land use/cover categories in the study areas: HUS is indicated by the outer black border; Helsinki by the inner black border; HUS-H area (HUS excluding Helsinki) by the area between the outer and inner borders. Land use/cover categories are indicated in the legend: red, orange or purple colours indicate predominantly urbanised areas, whereas yellow, green and blue colours indicate predominantly rural or natural areas.
Figure 2.
Relative risk (RR) of all-cause mortality as a function of daily mean temperature and lag (days) in the city of Helsinki (a,c) and Helsinki-Uusimaa hospital district without Helsinki (HUS-H, (b,d) in 2000–2018. In the upper panels (a,b), all ages and in the lower panels (c,d) 75+ relationships. The RR is with respect to the mortality at +15 °C.
Figure 2.
Relative risk (RR) of all-cause mortality as a function of daily mean temperature and lag (days) in the city of Helsinki (a,c) and Helsinki-Uusimaa hospital district without Helsinki (HUS-H, (b,d) in 2000–2018. In the upper panels (a,b), all ages and in the lower panels (c,d) 75+ relationships. The RR is with respect to the mortality at +15 °C.
Figure 3.
Overall cumulative mortality risks (RR) as a function or daily mean temperature and frequency distribution of daily mean temperature in 2000–2018. The association in Helsinki on left (a,c) and Helsinki-Uusimaa hospital district without Helsinki (HUS-H) on right (b,c). In the upper panels all ages (a,b) and in the lower panels 75+ associations (c,d). The grey areas illustrate the 95% confidence intervals of the modelled relationships. The RR is with respect to the mortality at +15 °C (vertical dotted line), the red part of the curve illustrates heat-related mortality risk and the blue part of the curve cold-related mortality risk. The vertical dashed lines indicate 1st and 99th percentile of the daily mean temperature frequency distribution.
Figure 3.
Overall cumulative mortality risks (RR) as a function or daily mean temperature and frequency distribution of daily mean temperature in 2000–2018. The association in Helsinki on left (a,c) and Helsinki-Uusimaa hospital district without Helsinki (HUS-H) on right (b,c). In the upper panels all ages (a,b) and in the lower panels 75+ associations (c,d). The grey areas illustrate the 95% confidence intervals of the modelled relationships. The RR is with respect to the mortality at +15 °C (vertical dotted line), the red part of the curve illustrates heat-related mortality risk and the blue part of the curve cold-related mortality risk. The vertical dashed lines indicate 1st and 99th percentile of the daily mean temperature frequency distribution.
Figure 4.
Daily deaths attributable to heat in summers 2003, 2010, 2014 and 2018 and daily mean temperature in Helsinki (a,c,e,g) and Helsinki-Uusimaa hospital district without Helsinki HUS-H, (b,d,f,h). These estimates were based on the modelled temperature–mortality relationships during 2000–2018, in which the impact of heat on mortality risk lasted for a few days. “Forward” refers to the prediction of the number of deaths based on the temperatures, and “backward” to the perspective in which the number of deaths was explained by the temperatures of the previous few days.
Figure 4.
Daily deaths attributable to heat in summers 2003, 2010, 2014 and 2018 and daily mean temperature in Helsinki (a,c,e,g) and Helsinki-Uusimaa hospital district without Helsinki HUS-H, (b,d,f,h). These estimates were based on the modelled temperature–mortality relationships during 2000–2018, in which the impact of heat on mortality risk lasted for a few days. “Forward” refers to the prediction of the number of deaths based on the temperatures, and “backward” to the perspective in which the number of deaths was explained by the temperatures of the previous few days.
Table 1.
Relative risks (RR) of all ages and 75+ mortality (with 95% confidence interval) at selected daily mean temperatures (Tmean) in Helsinki and in the surrounding Helsinki-Uusimaa hospital district (HUS-H) based on modelled temperature–mortality relationship 2000–2018.
Table 1.
Relative risks (RR) of all ages and 75+ mortality (with 95% confidence interval) at selected daily mean temperatures (Tmean) in Helsinki and in the surrounding Helsinki-Uusimaa hospital district (HUS-H) based on modelled temperature–mortality relationship 2000–2018.
| | RR—All | | RR—75+ | |
|---|
| Tmean (°C) | Helsinki | HUS-H | Helsinki | HUS-H |
|---|
| +24 | 1.30 (1.01–1.69) | 1.16 (0.90–1.45) | 1.56 (1.11–2.19) | 1.36 (0.97–1.90) |
| +20 | 1.06 (0.97–1.16) | 1.05 (0.96–1.15) | 1.12 (1.00–1.26) | 1.10 (0.97–1.23) |
| −15 | 1.38 (1.09–1.74) | 1.30 (1.05–1.61) | 1.47 (1.09–1.99) | 1.52 (1.44–2.01) |
| −20 | 1.28 (0.95–1.73) | 1.25 (0.98–1.60) | 1.21 (0.82–1.78) | 1.60 (1.16–2.20) |
Table 2.
Number of deaths and mortality (1/100,000) attributable to daily mean temperature exceeding +20 °C during heatwaves in Helsinki and in the surrounding Helsinki-Uusimaa hospital district (HUS-H; Helsinki excluded) in 2003, 2010, 2014 and 2018. The different values are forward/backward perspectives of the estimates, as visualized in
Figure 4. Ratios of the mortality in Helsinki to the mortality in HUS-H are given in the last column.
Table 2.
Number of deaths and mortality (1/100,000) attributable to daily mean temperature exceeding +20 °C during heatwaves in Helsinki and in the surrounding Helsinki-Uusimaa hospital district (HUS-H; Helsinki excluded) in 2003, 2010, 2014 and 2018. The different values are forward/backward perspectives of the estimates, as visualized in
Figure 4. Ratios of the mortality in Helsinki to the mortality in HUS-H are given in the last column.
| | Deaths | | Mortality | | |
|---|
| Year | Helsinki | HUS-H | Helsinki | HUS-H | Ratio of Mortalities |
|---|
| 2003 | 52/56 | 31/32 | 9.3/10.0 | 3.6/3.7 | 2.6/2.7 |
| 2010 | 86/93 | 55/58 | 14.7/15.9 | 5.9/6.2 | 2.5/2.6 |
| 2014 | 65/67 | 39/42 | 10.5/10.9 | 4.0/4.3 | 2.6/2.5 |
| 2018 | 72/78 | 52/53 | 11.2/12.1 | 5.1/5.2 | 2.2/2.3 |
Table 3.
Relative Risks (RR, 95% CI) of all-age mortality in Helsinki at various values of daily mean temperature (T) based on modelling temperature–mortality relationships with and without taking into account the air quality variables O3, PM10 and PM2.5.
Table 3.
Relative Risks (RR, 95% CI) of all-age mortality in Helsinki at various values of daily mean temperature (T) based on modelling temperature–mortality relationships with and without taking into account the air quality variables O3, PM10 and PM2.5.
| Exposure | RR at +24 °C | RR at +20 °C | RR at −15 °C | RR at −20 °C |
|---|
| T | 1.30 (1.01–1.67) | 1.06 (0.97–1.16) | 1.38 (1.09–1.74) | 1.28 (0.95–1.73) |
| T, O3 | 1.26 (0.97–1.64) | 1.05 (0.96–1.15) | 1.40 (1.11–1.77) | 1.31 (0.97–1.77) |
| T, PM10 | 1.31 (1.01–1.69) | 1.06 (0.97–1.17) | 1.38 (1.09–1.74) | 1.28 (0.95–1.73) |
| T, PM2.5 | 1.30 (1.01–1.69) | 1.06 (0.97–1.16) | 1.38 (1.09–1.75) | 1.28 (0.95–1.74) |
| T, O3, PM10 | 1.27 (0.97–1.65) | 1.05 (0.96–1.15) | 1.40 (1.11–1.77) | 1.31 (0.97–1.77) |
| T, O3, PM2.5 | 1.27 (0.97–1.65) | 1.05 (0.96–1.15) | 1.40 (1.11–1.77) | 1.31 (0.97–1.77) |
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).