Participation and Engagement of Public Health Stakeholders in Climate and Health Adaptation
Abstract
:1. Introduction
1.1. Stakeholder Participation at the Intersection of Climate and Health
1.2. Role of Public Health in Climate-Sensitive Hazard Work
1.3. Engaging Stakeholders
2. Experiments
2.1. Maricopa County Department of Public Health (MCDPH)
2.2. Climate Assessment for the Southwest (CLIMAS)
2.3. Stakeholder Mapping
3. Results
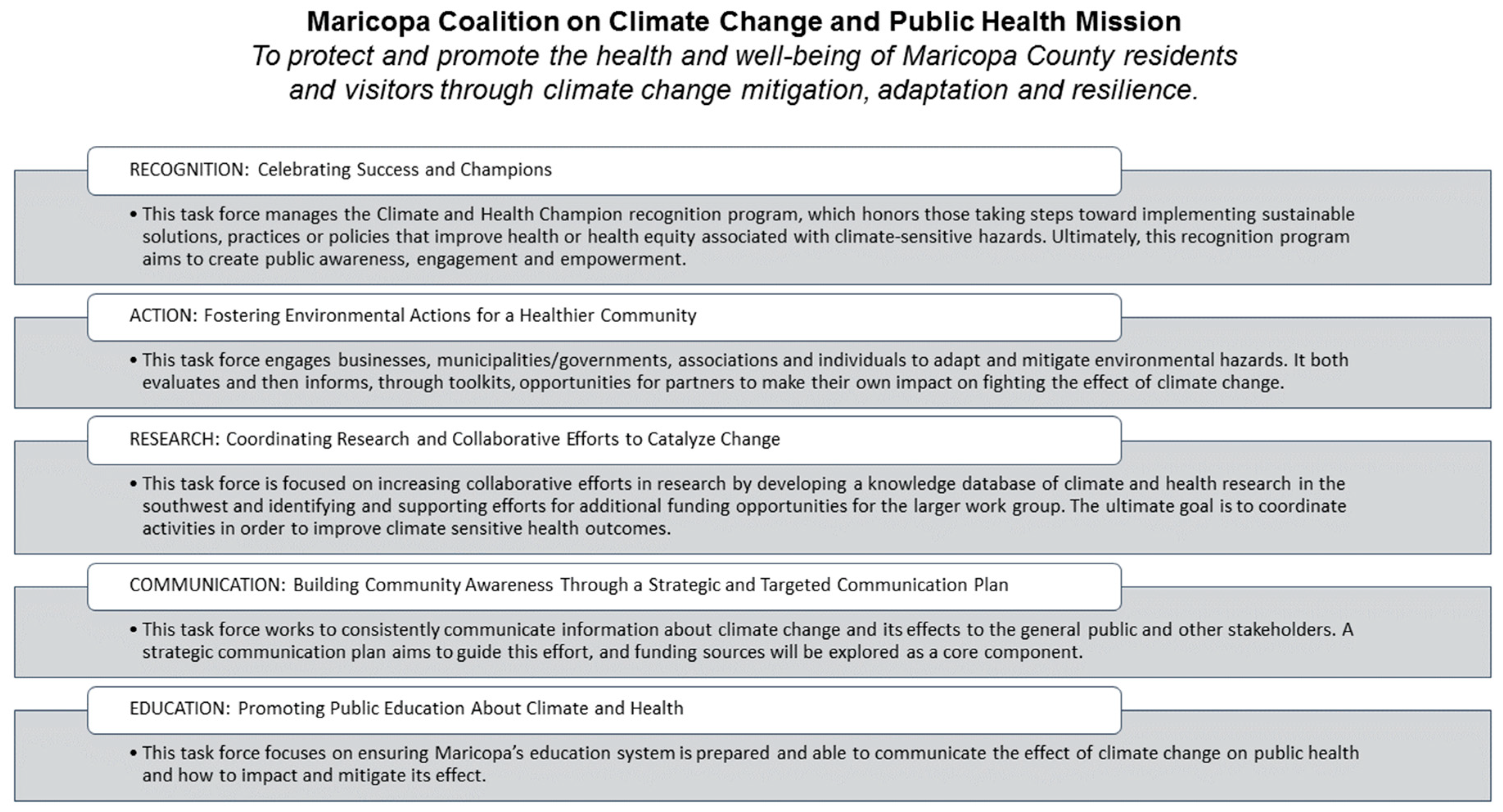
3.1. Maricopa County Department of Public Health (MCDPH)
3.2. Climate Assessment for the Southwest (CLIMAS)
3.3. Maintaining Stakeholder Lists
3.3.1. Maricopa County Department of Public Health (MCDPH)
3.3.2. Climate Assessment for the Southwest (CLIMAS)
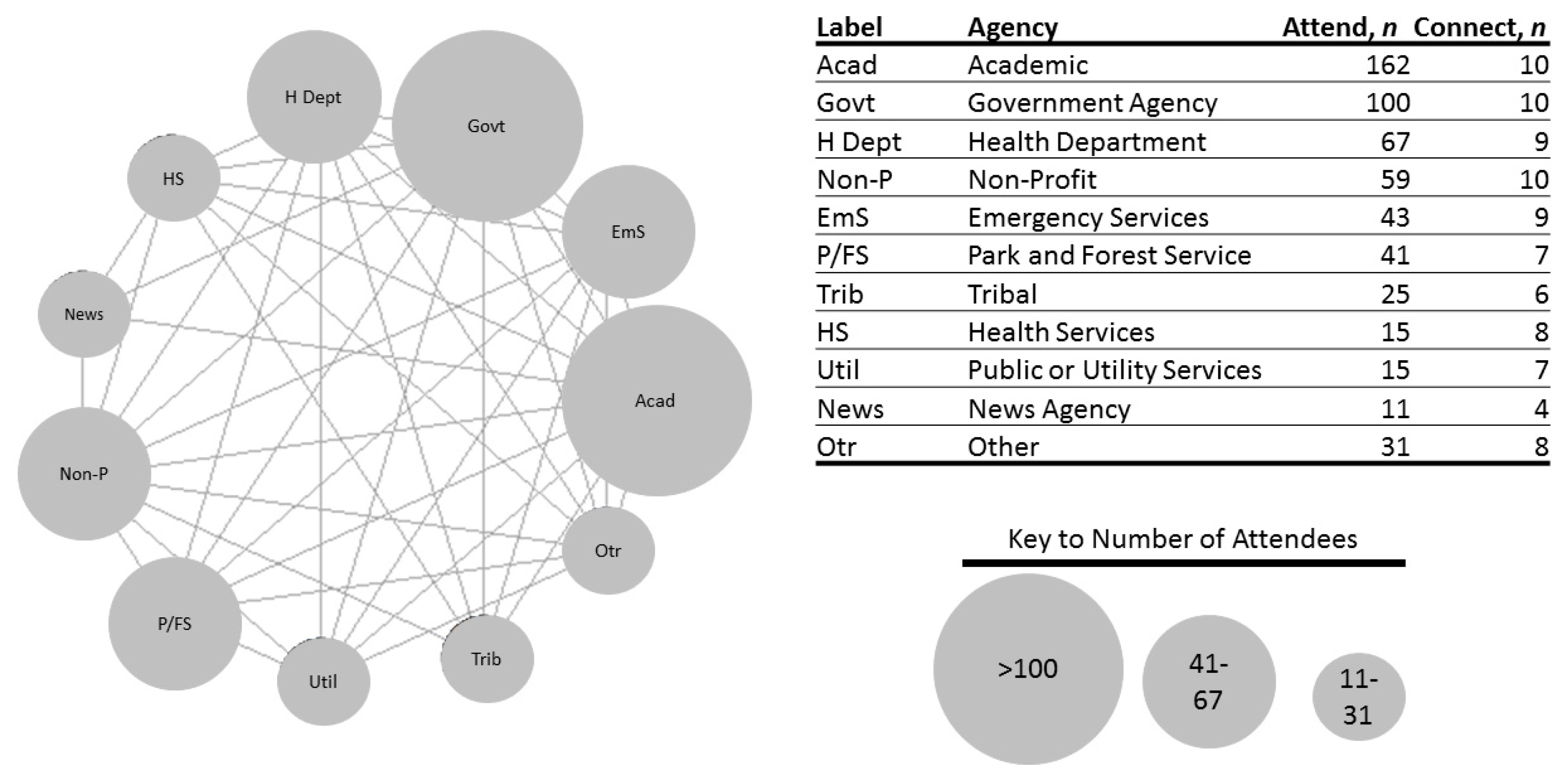
3.4. Stakeholder Mapping
4. Discussion
Gap Analysis and Platform Description
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Marinucci, G.D.; Luber, G.; Uejio, C.K.; Saha, S.; Hess, J.J. Building resilience against climate effects-a novel framework to facilitate climate readiness in public health agencies. Int. J. Environ. Res. Public Health 2014, 11, 6433–6458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eidson, M.; Clancy, K.A.; Birkhead, G.S. Public health climate change adaptation planning using stakeholder feedback. J. Public Heal. Manag. Pract. 2016, 22, E11–E19. [Google Scholar] [CrossRef] [PubMed]
- Rudolph, L.; Harrison, C.; Buckley, L.; North, S. Climate Change, Health, and Equity: A Guide for Local Health Departments; American Public Health Association: Oakland, CA, USA, 2018. [Google Scholar]
- Fery, P.; Speiser, M. Let’s Lead on Climate; ecoAmerica: Washington, DC, USA, 2017. [Google Scholar]
- Haines, A.; Ebi, K. The Imperative for Climate Action to Protect Health. N. Engl. J. Med. 2018, 1, 1–17. [Google Scholar] [CrossRef] [PubMed]
- APHA. Adaptation in Action Part II 2018: Updated Grantee Sucess Stories from CDC’s Climate and Health Program; American Public Health Association: Washington, DC, USA, 2018; p. 35. [Google Scholar]
- Roach, M.; Austhof, E.; Berisha, V.; Brown, H.; Carr, D.; Harlow-Smith, L.; Hondula, D.; Snyder, K. Addendum to the Arizona Climate and Health Adaptation Plan. In A report prepared for the United States Centers for Disease Control and Prevention Climate-Ready States and Cities Initiative; Arizona Department of Health Services: Phoenix, AZ, USA, 2018. [Google Scholar]
- Masson-Delmotte, V.; Zhai, P.; Pörtner, H.-O.; Roberts, D.; Skea, J.; Shukla, P.R.; Pirani, A.; Moufouma-Okia, W.; Péan, C.; Pidcock, R.; et al. IPCC, 2018: Summary for Policymakers. In Global warming of 1.5 °C. An IPCC Special Report on the Impacts of Global Warming of 1.5°C above Pre-Industrial Levels and Related Global Greenhouse Gas Emission Pathways, in the Context of Strengthening the Global Response to the Threat of Climate Change, Sustainable Development, and Efforts to Eradicate Poverty; The Intergovernmental Panel on Climate Change: Geneva, Switzerland, 2018. [Google Scholar]
- Guyer, H.E.; Putnam, H.F.; Roach, M.; Iñiguez, P.; Hondula, D.M.; Guyer, H.E.; Putnam, H.F.; Roach, M.; Iñiguez, P.; Hondula, D.M. Cross-Sector Management of Extreme Heat Risks in Arizona. Bull. Am. Meteorol. Soc. 2019, 100, ES101–ES104. [Google Scholar] [CrossRef]
- Woolgar, S. Social basis of interactive social science. Sci. Public Policy 2000, 27, 165–173. [Google Scholar] [CrossRef]
- Scott, A.; Skea, J.; Robinson, J.; Shove, E. Designing “Interactive” Environmental Research for Wider Social Relevance; Global Environmental Change Programme: Brighton, UK, 1999. [Google Scholar]
- Owen, G.; Ferguson, D.B.; McMahan, B. Contextualizing climate science: Applying social learning systems theory to knowledge production, climate services, and use-inspired research. Clim. Chang. 2019, 157, 151–170. [Google Scholar] [CrossRef]
- Lemos, M.C.; Morehouse, B.J. The co-production of science and policy in integrated climate assessments. Glob. Environ. Chang. 2005, 15, 57–68. [Google Scholar] [CrossRef]
- Meadow, A.M.; Ferguson, D.B.; Guido, Z.; Horangic, A.; Owen, G.; Wall, T. Moving toward the Deliberate Coproduction of Climate Science Knowledge. Weather. Clim. Soc. 2015, 7, 179–191. [Google Scholar] [CrossRef] [Green Version]
- Wine, O.; Ambrose, S.; Campbell, S.; Villeneuve, P.J.; Burns, K.K.; Vargas, A.O. Key Components of Collaborative Research in the Context of Environmental Health: A Scoping Review. J. Res. Pract. 2017, 13, R2. [Google Scholar]
- Younger, M.; Morrow-Almeida, H.R.; Vindigni, S.M.; Dannenberg, A.L. The Built Environment, Climate Change, and Health. Am. J. Prev. Med. 2008, 35, 517–526. [Google Scholar] [CrossRef] [PubMed]
- Leiserowitz, A.; Maibach, E.; Rosenthal, S.; Kotcher, J.; Bergquist, P.; Ballew, M.; Goldberg, M.; Gustafson, A. Climate Change in the American Mind: April 2019; Yale Program on Climate Change Communication: New Haven, CT, USA, 2019. [Google Scholar]
- Myers, T.A.; Nisbet, M.C.; Maibach, E.W.; Leiserowitz, A.A. A public health frame arouses hopeful emotions about climate change. Clim. Chang. 2012, 113, 1105–1112. [Google Scholar] [CrossRef] [Green Version]
- Woodruff, S.C.; Stults, M. Numerous strategies but limited implementation guidance in US local adaptation plans. Nat. Clim. Chang. 2016, 6, 796–802. [Google Scholar] [CrossRef]
- Araos, M.; Austin, S.E.; Berrang-Ford, L.; Ford, J.D. Public Health Adaptation to Climate Change in Large Cities. Int. J. Heal. Serv. 2016, 46, 53–78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schramm, P.J.; Uejio, C.K.; Hess, J.J.; Marinucci, G.D.; Luber, G. Climate Models and the Use of Climate Projections: A Brief Overview for Health Departments; National Center for Environmental Health, Centers for Disease Control and Prevention: Atlanta, GA, USA, 2014. [Google Scholar]
- ADHS. Extreme Weather and Public Health—About Us. Available online: https://www.azdhs.gov/preparedness/epidemiology-disease-control/extreme-weather/index.php#about-us (accessed on 26 July 2019).
- Helping North America Communities Adapt to Climate Change: A Pilot Syndromic Surveillance System for Extreme Heat Events|Commission for Environmental Cooperation. Available online: http://www.cec.org/our-work/projects/helping-north-america-communities-adapt-climate-change-pilot-syndromic-surveillance-system-extreme-heat-events (accessed on 3 February 2020).
- Roach, M.; Barrett, E.; Brown, H.; Dufour, B.; Hondula, D.M.; Putnam, H.; Sosa, B. Climate and Health Adaptation Plan 2017; Arizona Department of Health Services: Phoenix, AZ, USA, 2017.
- Southwest Adaptation Forum. Available online: https://www.swcasc.arizona.edu/events/16751-southwest-adaptation-forum (accessed on 3 February 2020).
- UA Joins Research Coalition on Climate. Available online: https://uanews.arizona.edu/story/ua-joins-research-coalition-climate (accessed on 3 February 2020).
- ADEMA. State of Arizona Hazard Mitigation Plan; Arizona Department of Emergency and Military Affairs: Phoenix, AZ, USA, 2018.
- White, J.R.; Berisha, V.; Lane, K.; Ménager, H.; Gettel, A.; Braun, C.R. Evaluation of a Novel Syndromic Surveillance Query for Heat-Related Illness Using Hospital Data From Maricopa County, Arizona, 2015. Public Health Rep. 2017, 132, 31S–39S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- US Department of Commerce, NOAA, N.W.S. NWS Forecast Office Tucson, AZ. Available online: https://www.weather.gov/twc/ (accessed on 13 June 2018).
- Roach, M.; Brown, H.E.; Wilder, M.; Smith, G.R.; Chambers, S.; Patten, I.E.; Rabby, Q. Assessment of Climate and Health Impacts on Vector-Borne Diseases and Valley Fever in Arizona; Arizona Department of Health Services: Phoenix, AZ, USA, 2017.
- Berisha, V.; Hondula, D.; Roach, M.; White, J.R.; McKinney, B.; Bentz, D.; Mohamed, A.; Uebelherr, J.; Goodin, K.; Berisha, V.; et al. Assessing Adaptation Strategies for Extreme Heat: A Public Health Evaluation of Cooling Centers in Maricopa County, Arizona. Weather. Clim. Soc. 2017, 9, 71–80. [Google Scholar] [CrossRef]
- Kent, D.C.; Garcia, R.Z.; Packard, S.; Briggs, G.; Hill, C.; Griffin, S.; Bedrick, E.; Collier, K.; Roach, M. Enhanced Surveillance of Heat-Related Illness in Pinal County. Online J. Public Health Inform. 2018, 10, 1. [Google Scholar] [CrossRef] [Green Version]
- Putnam, H.; Hondula, D.M.; Urban, A.; Berisha, V.; Iñiguez, P.; Roach, M. It’s not the heat, it’s the vulnerability: Attribution of the 2016 spike in heat-associated deaths in Maricopa County, Arizona. Environ. Res. Lett. 2018, 13, 094022. [Google Scholar] [CrossRef] [Green Version]
- GAO. Climate Change: HHS Could Take Further Steps to Enhance Understanding of Public Health Risks; US Government Accountability Office: Washington, DC, USA, 2015.
- U.S. Census Bureau QuickFacts: Maricopa County, Arizona. Available online: https://www.census.gov/quickfacts/maricopacountyarizona (accessed on 7 February 2019).
- MCDPH. Climate and Health Strategic Plan for Maricopa County; Maricopa County Department of Public Health: Phoenix, AZ, USA, 2018. [Google Scholar]
- Meadow, A.M. An Ethnohistory of the NOAA RISA Program; Climate Assessment for the Southwest University of Arizona: Tucson, AZ, USA, 2017. [Google Scholar]
- Roach, M.; Brown, H.E.; Clark, R.; Hondula, D.; Lega, J.; Rabby, Q.; Schweers, N.; Tabor, J. Projections of Climate Impacts on Vector-Borne Diseases and Valley Fever in Arizona; Arizona Department of Health Services: Phoenix, AZ, USA, 2017.
- Arkin, E.B.; Bauer, C.; Burklow, J.; Doner, L.; Edgar, T.; Flay, B.R.; Freimuth, V.S.; Gallivan, J.; Glanz, K.; Glassman, B.; et al. Making Health Communication Programs Work, 2nd ed.; National Institutes of Health National Cancer Institute: Bethesda, MD, USA, 1989. [Google Scholar]
- Ebi, K.L. Public Health Responses to the Risks of Climate Variability and Change in the United States. J. Occup. Environ. Med. 2009, 51, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Ebi, K.L.; Burton, I. Identifying practical adaptation options: An approach to address climate change-related health risks. Environ. Sci. Policy 2008, 11, 359–369. [Google Scholar] [CrossRef]
- The Human Cost of Heat | AZ Central. Available online: https://static.azcentral.com/human-cost-heat/ (accessed on 3 February 2020).
- Ebi, K.L.; Balbus, J.; Kinney, P.L.; Lipp, E.; Mills, D.; O’Neill, M.S.; Wilson, M.L. U.S. Funding Is Insufficient to Address the Human Health Impacts of and Public Health Responses to Climate Variability and Change. Environ. Health Perspect. 2009, 117, 857–862. [Google Scholar] [CrossRef] [PubMed]
| Title of Project | Project Reference | Stakeholders Involved |
|---|---|---|
| Evaluation of a Novel Syndromic Surveillance Query for Heat-Related Illness Using Hospital Data from Maricopa County, Arizona, 2015 | [28] | Maricopa County Department of Public Health (Maricopa) * |
| Climate and Health Adaptation Plan; and addendum | [7,24] | Arizona Department of Health Services (ADHS) *, Maricopa, University of Arizona (UA), Arizona State University (ASU), Pinal County Public Health Services District (Pinal), Yuma County Health Services District (Yuma) |
| Special Weather Briefings and Statements from National Weather Service Forecast Offices in Arizona | [29] | National Weather Service (NWS) * |
| Assessment of Climate and Health Impacts on Vector-Borne Diseases and Valley Fever in Arizona 2017 | [30] | UA *, ADHS |
| Assessing Adaptation Strategies for Extreme Heat: A Public Health Evaluation of Cooling Centers in Maricopa County, Arizona | [31] | Maricopa *, ADHS, ASU |
| Enhanced Surveillance of Heat-Related Illness in Pinal County | [32] | Pinal *, ADHS, UA |
| It’s not the heat, it’s the vulnerability: attribution of the 2016 spike in heat-associated deaths in Maricopa County, Arizona | [33] | ASU *, ADHS, Maricopa, NWS |
| Cross-Sector Management of Extreme Heat Risks in Arizona | [9] | ASU *, ADHS, Maricopa, NWS |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Austhof, E.; Berisha, V.; McMahan, B.; Owen, G.; Keith, L.; Roach, M.; Brown, H.E. Participation and Engagement of Public Health Stakeholders in Climate and Health Adaptation. Atmosphere 2020, 11, 265. https://doi.org/10.3390/atmos11030265
Austhof E, Berisha V, McMahan B, Owen G, Keith L, Roach M, Brown HE. Participation and Engagement of Public Health Stakeholders in Climate and Health Adaptation. Atmosphere. 2020; 11(3):265. https://doi.org/10.3390/atmos11030265
Chicago/Turabian StyleAusthof, Erika, Vjollca Berisha, Ben McMahan, Gigi Owen, Ladd Keith, Matthew Roach, and Heidi E. Brown. 2020. "Participation and Engagement of Public Health Stakeholders in Climate and Health Adaptation" Atmosphere 11, no. 3: 265. https://doi.org/10.3390/atmos11030265
APA StyleAusthof, E., Berisha, V., McMahan, B., Owen, G., Keith, L., Roach, M., & Brown, H. E. (2020). Participation and Engagement of Public Health Stakeholders in Climate and Health Adaptation. Atmosphere, 11(3), 265. https://doi.org/10.3390/atmos11030265





