From Metabolic to Epigenetic Memory: The Impact of Hyperglycemia-Induced Epigenetic Signature on Kidney Disease Progression and Complications
Abstract
1. Introduction
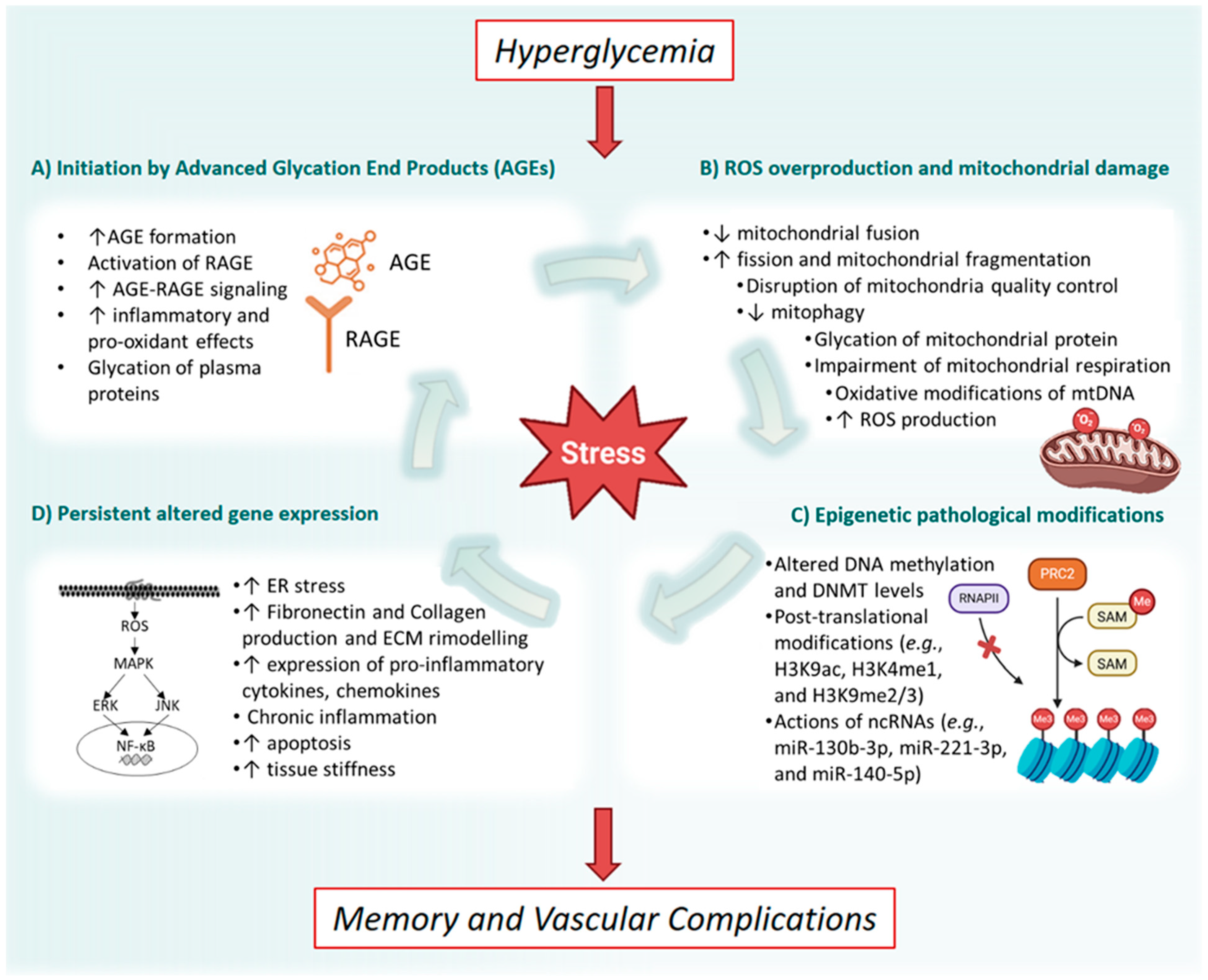
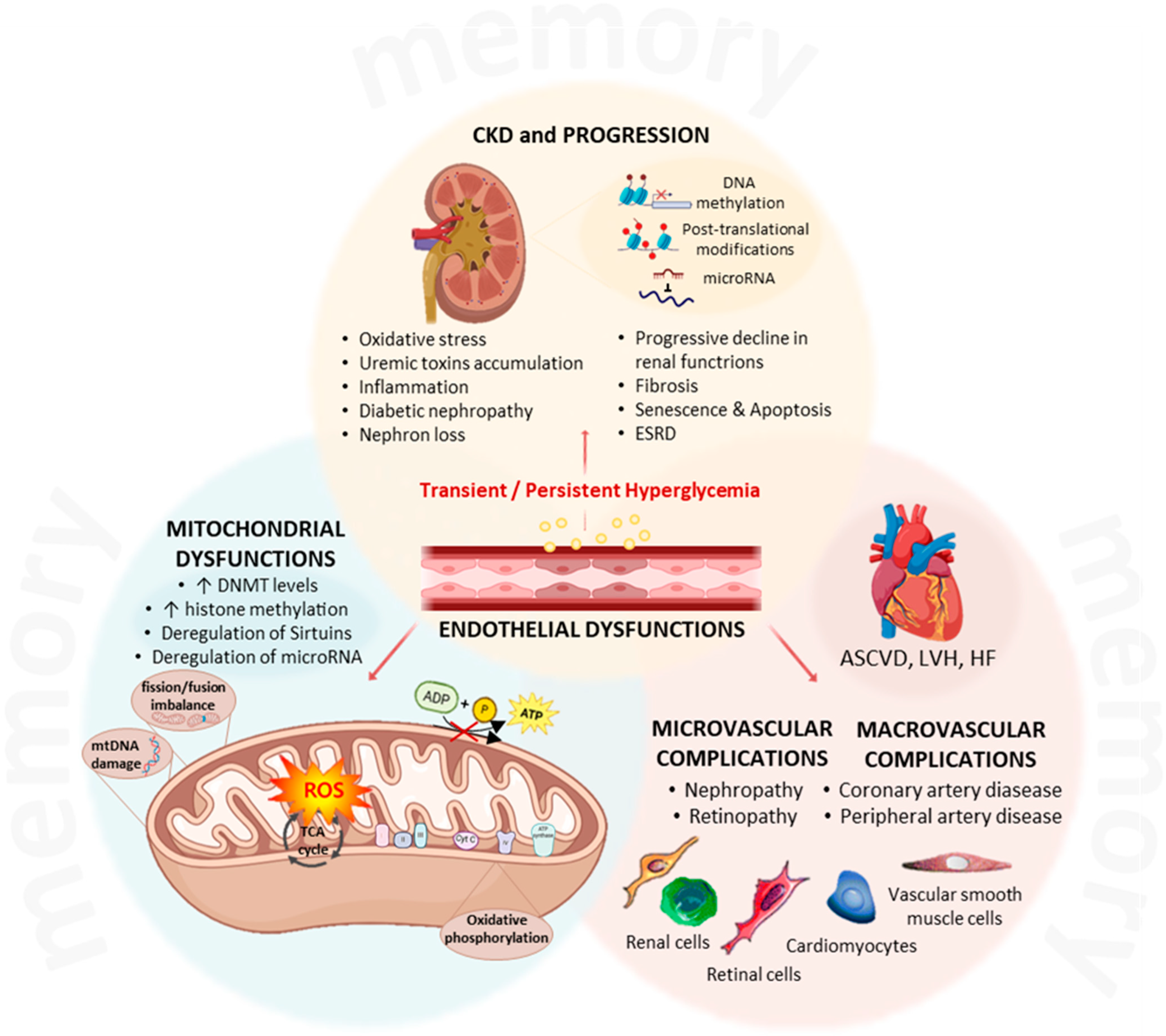
2. The Metabolic Memory
2.1. Clinical Evidence from Landmark Trials
2.2. Oxidative Stress and Mitochondrial Dysfunction
2.3. Impact of Glucose Fluctuations
2.4. Therapeutic Implications
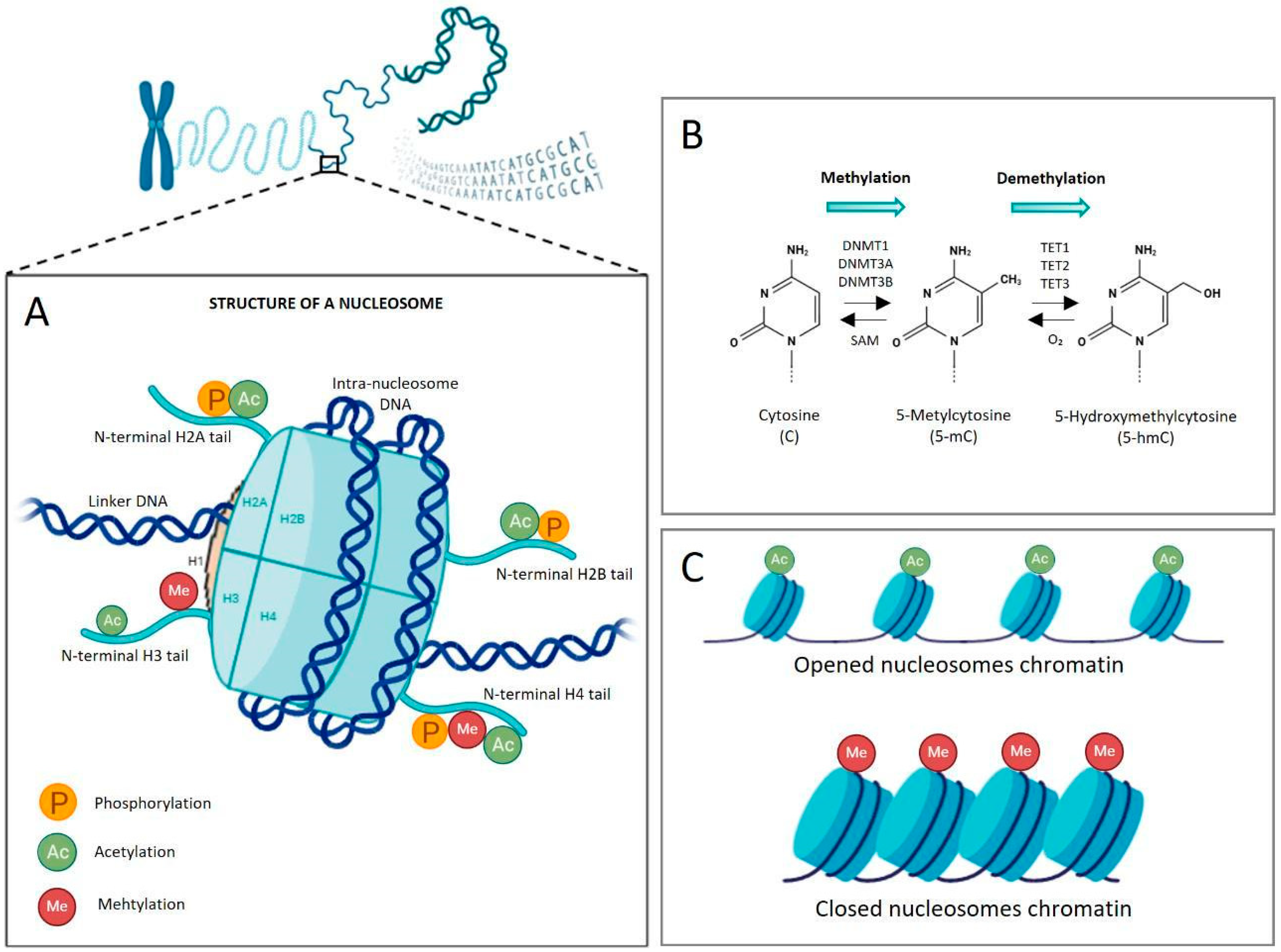
3. Epigenetic Regulation of the Gene Expression
3.1. Chromatin Structure and DNA Methylation
3.2. Histone Post-Translational Modifications
3.3. Polycomb Repressive Complexes and Chromatin Remodeling
3.4. Histone Acetylation and Deacetylation
- Class I (HDAC1, 2, 3, 8);
- Class II (HDAC4, 5, 6, 7, 9, 10);
- Class III or Sirtuins (SIRT1-7);
- Class IV (HDAC11).
3.5. Interplay Between Epigenetic Mechanisms
3.6. Non-Coding RNAs and microRNA-Mediated Regulation
3.7. Epigenetics and Disease Implications
4. The Role of the Epigenetic Memory in Hyperglycemia-Related CKD Progression
4.1. Histone Modifications and the Activation of Pro-Inflammatory Signaling
4.2. DNA Methylation Status Connected to Renal Disease Progression
4.3. The Role of Sirtuins in the Hyperglycemia-Induced Epigenetic Memory
4.4. MicroRNAs and the Epigenetic Memory
5. Epigenetic Players as Therapeutic Targets and Biomarkers for CKD Patients’ Stratification
5.1. Epigenetic Biomarkers in CKD and Diabetes
- (1)
- In a first study, patients exhibited elevated levels of the active chromatin mark H3K9ac in monocytes, correlated with baseline hyperglycemia and the upregulation of genes linked to inflammation and vascular complications. H3K9ac thus emerged as a potential biomarker for metabolic memory [162].
- (2)
- In a second study, DNA methylation profiling at two time points revealed 12 persistently differentially methylated loci, notably TXNIP, which was hypomethylated in patients with more complications [163]. Other validations confirmed a strong inverse correlation between TXNIP methylation and glycemic control, suggesting that TXNIP hypomethylation reflects chronic hyperglycemia and may predict renal and vascular damage [164].
- (3)
5.2. Histone Deacetylase Inhibitors and miRNA-Based Therapies
- Inhibition of overexpressed miRNAs (via antisense oligonucleotides, gene knockouts, or “sponges”);
- Restoration of protective miRNAs (via double-stranded mimics or expression vectors).
5.3. Integrating Machine Learning and Multi-Omics
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| 5-aza | 5-Aza-2′-deoxycytidine |
| 5-mC | 5-Methylcytosine |
| ADP | Adenine Diphosphate |
| AGE | Advanced Glycation End Products |
| AI | Artificial Intelligence |
| AMPK | AMP-Activated Protein Kinase |
| AKI | Acute Kidney Injury |
| Akt | Protein Kinase B |
| AR-42 | Histone Deacetylase Inhibitor AR-42/HDAC-42 |
| ARE | Antioxidant Response Element |
| AUH | AU RNA Binding Methylglutaconyl-CoA Hydratase |
| BD1 | Bromodomain1 |
| BD2 | Bromodomain2 |
| BET | Bromodomain and Extra-Terminal Domain |
| BETi | Bromodomain and Extra-Terminal Domain Inhibitor |
| BRD | Bromodomain Containing Protein |
| -CH3 | Methyl group |
| CaMK2a | Calcium/Calmodulin-Dependent Protein Kinase II alpha |
| CBP | CREB-Binding Protein |
| CBX | Polycomb Group Protein Chromobox |
| CCL-2 | C-C Motif Chemokine Ligand 2 |
| CDKN1A | Cyclin Dependent Kinase Inhibitor 1A |
| CH3CO- | Acetyl group |
| CKD | Chronic Kidney Disease |
| COX6A1 | Cytochrome C Oxidase Subunit 6A1 |
| CpG | Cytosine-phosphate-Guanine |
| DAPK3 | Death-Associated Protein Kinase 3 |
| DCCT | Diabetes Control and Complications Trial |
| DGCR8 | DiGeorge Syndrome Critical Region Gene 8 |
| DKD | Diabetic Kidney Disease |
| DMNT | DNA Methyltransferases |
| DNMTi | DNA Methyltransferase Inhibitor |
| DRP1 | Dynamin-Related Protein 1 |
| ECM | Extracellular Matrix |
| EDIC | Epidemiology of Diabetes Interventions and Complications Study |
| ELK1 | ETS Transcription Factor ELK1 |
| EGF | Epidermal Growth Factor |
| eGFR | Estimated Glomerular Filtration Rate |
| EMT | Epithelial-to-Mesenchymal Transition |
| EndMT | Endothelial-to-Mesenchymal Transition |
| eNOS | Endothelial Nitric Oxide Synthase |
| ERK | Extracellular signal-regulated kinase |
| ESRD | End-Stage Renal Disease |
| EWAS | Epigenetic-Wide Association Study |
| EZH2 | Enhancer of Zeste Homolog 2 |
| FDA | Food and Drug Administration |
| GBD | Global Burden Disease, Injuries, and Risk Factors |
| GFR | Glomerular Filtration Rate |
| GPX | Glutathione Peroxidase |
| GRK5 | G Protein-coupled Receptor Kinase 5 |
| H1 | Histone H1 |
| H2A | Histone H2A |
| H2B | Histone H2B |
| H3 | Histone H3 |
| H4 | Histone H4 |
| HATs | Histone Acetyltransferases |
| HbA1c | Glycated Haemoglobin |
| HDAC | Histone Deacetylase |
| HDACi | Histone Deacetylase Inhibitor |
| HDM | Histone Demethylase |
| HIC-1 | Hypermethylated in Cancer 1 |
| HMT | Histone Methyltransferase |
| HO-1 | Heme Oxygenase-1 |
| IRS2 | Insulin Receptor Substrate 2 |
| JNK | Janus Kinase |
| JMJD3 | Lysine demethylase 6B |
| JunD | Transcription Factor JunD |
| JQ-1 | Bromodomain 4 Inhibitor |
| KDIGO | Kidney Disease Improving Global Outcomes Guidelines |
| KDM | Lysine Demethylase |
| KDOQI | Kidney Disease Outcomes Quality Initiative Guidelines |
| KMT | Lysine Methyltransferase |
| LCAT | Lecithin Cholesterol Acyltransferase |
| LKB1 | Liver Kinase B1 |
| MAPK | Mitogen-Activated Protein Kinase |
| Mdivi-1 | Mitochondrial Division Inhibitor-1 |
| MeCP2 | Methyl-CpG-Binding Protein |
| MESA | Multi-Ethnic Study of Atherosclerosis |
| MFN2 | Mitofusin-2 |
| miRNA | MicroRNA |
| mtDNA | Mitochondrial DNA |
| mtROS | Mitochondrial Reactive Oxygen Species |
| mTOR | Mechanistic Target of Rapamycin |
| mTORC | Mechanistic Target of Rapamycin Complex |
| NAD+ | Nicotinamide Adenine Dinucleotide |
| NOX | Nicotinamide Adenine Dinucleotide Phosphate Oxidase |
| NF-κB | Nuclear Factor Kappa-Light-Chain-Enhancer of Activated B Cell |
| NRF2 | Nuclear Factor Erythroid 2-Related Factor 2 |
| Pai-1 | Plasminogen Activator Inhibitor 1 |
| PARP | Poly (ADP-ribose) Polymerase |
| p21 | Cyclin-Dependent Kinase Inhibitor 1 |
| p53 | Transformation-Related Protein 53 |
| p65 | NF-Kappa-B Transcription Factor P65 |
| PINK-1 | PTEN-Induced Kinase 1 |
| PMPCB | Peptidase, Mitochondrial Processing Subunit Beta |
| PRC2 | Polycomb Repressive Complex 2 |
| PTEN | Phosphatase and TENsin Homolog |
| PTM | Post-Translational Modification |
| RAGE | Glycation End Products Receptor |
| RISC | RNA-Induced Silencing Complex |
| ROS | Reactive Oxygen Species |
| RPTOR | Regulatory Associated Protein of mTOR Complex 1 |
| SAHA | Suberoylanilide Hydroxamic Acid |
| SAM | S-Adenosyl-l-Methionine |
| SGI-1027 | DNA Methyltransferase Inhibitor II |
| SIRT | Silent Mating Type Information Regulation 2 Homolog |
| SLC1A5 | Solute Carrier Family 1 (neutral amino acid transporter), Member 5 |
| SLC27A3 | Solute Carrier Family 27 Member 3 |
| SMAD | Small Mother Against Decapentaplegic |
| SOD | Superoxide Dismutase |
| Sp-1 | Specificity Protein 1 |
| Suv39H1 | Suppressor of Variegation 3-9 Homolog 1 |
| TAMM41 | TAM41 Mitochondrial Translocator Assembly and Maintenance Homolog |
| TET | Ten-Eleven Translocation |
| TGF-α | Transforming Growth Factor-alpha |
| TGF-β | Transforming Growth Factor-beta |
| Th1 | T helper 1 |
| TSA | Trichostatin A |
| TSFM | Ts Translation Elongation Factor, Mitochondrial |
| TXNIP | Thioredoxin-Interacting Protein |
| UKPDS | United Kingdom Prospective Diabetes Study |
| VCAM-1 | Vascular Cell Adhesion Molecule 1 |
| VPA | Valproic Acid |
References
- Inker, L.A.; Astor, B.C.; Fox, C.H.; Isakova, T.; Lash, J.P.; Peralta, C.A.; Kurella Tamura, M.; Feldman, H.I. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am. J. Kidney Dis. 2014, 63, 713–735. [Google Scholar] [CrossRef]
- Rysz, J.; Franczyk, B.; Rysz-Gorzynska, M.; Gluba-Brzozka, A. Are Alterations in DNA Methylation Related to CKD Development? Int. J. Mol. Sci. 2022, 23, 7108. [Google Scholar] [CrossRef]
- Gilg, J.; Rao, A.; Fogarty, D. UK Renal Registry 16th annual report: Chapter 1 UK renal replacement therapy incidence in 2012: National and centre-specific analyses. Nephron. Clin. Pract. 2014, 125, 1–28. [Google Scholar] [CrossRef]
- GBD Chronic Kidney Disease Collaboration, Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2020, 395, 709–733. [CrossRef]
- Ho, H.J.; Shirakawa, H. Oxidative Stress and Mitochondrial Dysfunction in Chronic Kidney Disease. Cells 2022, 12, 88. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Coresh, J. Conceptual model of CKD: Applications and implications. Am. J. Kidney Dis. 2009, 53, S4–S16. [Google Scholar] [CrossRef] [PubMed]
- Rout, P.; Jialal, I. Diabetic Nephropathy; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Tervaert, T.W.; Mooyaart, A.L.; Amann, K.; Cohen, A.H.; Cook, H.T.; Drachenberg, C.B.; Ferrario, F.; Fogo, A.B.; Haas, M.; de Heer, E.; et al. Pathologic classification of diabetic nephropathy. J. Am. Soc. Nephrol. 2010, 21, 556–563. [Google Scholar] [CrossRef]
- Liebisch, M.; Wolf, G. Role of Epigenetic Changes in the Pathophysiology of Diabetic Kidney Disease. Glomerular Dis. 2024, 4, 211–226. [Google Scholar] [CrossRef] [PubMed]
- Amorim, R.G.; Guedes, G.D.S.; Vasconcelos, S.M.L.; Santos, J.C.F. Kidney Disease in Diabetes Mellitus: Cross-Linking between Hyperglycemia, Redox Imbalance and Inflammation. Arq. Bras. Cardiol. 2019, 112, 577–587, Erratum in Arq. Bras. Cardiol. 2019, 113, 182. [Google Scholar] [CrossRef]
- Reidy, K.; Kang, H.M.; Hostetter, T.; Susztak, K. Molecular mechanisms of diabetic kidney disease. J. Clin. Investig. 2014, 124, 2333–2340. [Google Scholar] [CrossRef] [PubMed]
- Turkmen, K. Inflammation, oxidative stress, apoptosis, and autophagy in diabetes mellitus and diabetic kidney disease: The Four Horsemen of the Apocalypse. Int. Urol. Nephrol. 2017, 49, 837–844. [Google Scholar] [CrossRef]
- Kato, M.; Natarajan, R. Epigenetics and epigenomics in diabetic kidney disease and metabolic memory. Nat. Rev. Nephrol. 2019, 15, 327–345. [Google Scholar] [CrossRef] [PubMed]
- Kuo, F.C.; Chao, C.T.; Lin, S.H. The Dynamics and Plasticity of Epigenetics in Diabetic Kidney Disease: Therapeutic Applications Vis-a-Vis. Int. J. Mol. Sci. 2022, 23, 843. [Google Scholar] [CrossRef] [PubMed]
- Giacco, F.; Brownlee, M. Oxidative stress and diabetic complications. Circ. Res. 2010, 107, 1058–1070. [Google Scholar] [CrossRef] [PubMed]
- Yapislar, H.; Gurler, E.B. Management of Microcomplications of Diabetes Mellitus: Challenges, Current Trends, and Future Perspectives in Treatment. Biomedicines 2024, 12, 1958. [Google Scholar] [CrossRef]
- Thomas, M.C.; Brownlee, M.; Susztak, K.; Sharma, K.; Jandeleit-Dahm, K.A.; Zoungas, S.; Rossing, P.; Groop, P.H.; Cooper, M.E. Diabetic kidney disease. Nat. Rev. Dis. Primers 2015, 1, 15018. [Google Scholar] [CrossRef]
- Pal, R.; Bhadada, S.K. AGEs accumulation with vascular complications, glycemic control and metabolic syndrome: A narrative review. Bone 2023, 176, 116884. [Google Scholar] [CrossRef]
- Ng, Z.X.; Kuppusamy, U.R.; Iqbal, T.; Chua, K.H. Receptor for advanced glycation end-product (RAGE) gene polymorphism 2245G/A is associated with pro-inflammatory, oxidative-glycation markers and sRAGE in diabetic retinopathy. Gene 2013, 521, 227–233. [Google Scholar] [CrossRef]
- de Souza Ferreira, C.; Pennacchi, P.C.; Araujo, T.H.; Taniwaki, N.N.; de Araujo Paula, F.B.; da Silveira Duarte, S.M.; Rodrigues, M.R. Aminoguanidine treatment increased NOX2 response in diabetic rats: Improved phagocytosis and killing of Candida albicans by neutrophils. Eur. J. Pharmacol. 2016, 772, 83–91. [Google Scholar] [CrossRef]
- Sugahara, M.; Pak, W.L.W.; Tanaka, T.; Tang, S.C.W.; Nangaku, M. Update on diagnosis, pathophysiology, and management of diabetic kidney disease. Nephrology 2021, 26, 491–500. [Google Scholar] [CrossRef]
- Ceriello, A. Hypothesis: The “metabolic memory”, the new challenge of diabetes. Diabetes Res. Clin. Pract. 2009, 86, S2–S6. [Google Scholar] [CrossRef]
- El-Osta, A.; Brasacchio, D.; Yao, D.; Pocai, A.; Jones, P.L.; Roeder, R.G.; Cooper, M.E.; Brownlee, M. Transient high glucose causes persistent epigenetic changes and altered gene expression during subsequent normoglycemia. J. Exp. Med. 2008, 205, 2409–2417. [Google Scholar] [CrossRef]
- Luna, P.; Guarner, V.; Farias, J.M.; Hernandez-Pacheco, G.; Martinez, M. Importance of Metabolic Memory in the Development of Vascular Complications in Diabetic Patients. J. Cardiothorac. Vasc. Anesth. 2016, 30, 1369–1378. [Google Scholar] [CrossRef] [PubMed]
- Testa, R.; Bonfigli, A.R.; Prattichizzo, F.; La Sala, L.; De Nigris, V.; Ceriello, A. The “Metabolic Memory” Theory and the Early Treatment of Hyperglycemia in Prevention of Diabetic Complications. Nutrients 2017, 9, 437. [Google Scholar] [CrossRef] [PubMed]
- Dong, H.; Sun, Y.; Nie, L.; Cui, A.; Zhao, P.; Leung, W.K.; Wang, Q. Metabolic memory: Mechanisms and diseases. Signal Transduct. Target. Ther. 2024, 9, 38. [Google Scholar] [CrossRef]
- Roy, S.; Sala, R.; Cagliero, E.; Lorenzi, M. Overexpression of fibronectin induced by diabetes or high glucose: Phenomenon with a memory. Proc. Natl. Acad. Sci. USA 1990, 87, 404–408. [Google Scholar] [CrossRef]
- Lachin, J.M.; Bebu, I.; Nathan, D.M. DCCT/EDIC Research Group, The Beneficial Effects of Earlier Versus Later Implementation of Intensive Therapy in Type 1 Diabetes. Diabetes Care 2021, 44, 2225–2230. [Google Scholar] [CrossRef]
- Wilson-Verdugo, M.; Bustos-Garcia, B.; Adame-Guerrero, O.; Hersch-Gonzalez, J.; Cano-Dominguez, N.; Soto-Nava, M.; Acosta, C.A.; Tusie-Luna, T.; Avila-Rios, S.; Noriega, L.G.; et al. Reversal of high-glucose-induced transcriptional and epigenetic memories through NRF2 pathway activation. Life Sci. Alliance 2024, 7, e202302382. [Google Scholar] [CrossRef] [PubMed]
- Nishikawa, T.; Edelstein, D.; Du, X.L.; Yamagishi, S.; Matsumura, T.; Kaneda, Y.; Yorek, M.A.; Beebe, D.; Oates, P.J.; Hammes, H.P.; et al. Normalizing mitochondrial superoxide production blocks three pathways of hyperglycaemic damage. Nature 2000, 404, 787–790. [Google Scholar] [CrossRef]
- Ihnat, M.A.; Thorpe, J.E.; Kamat, C.D.; Szabó, C.; Green, D.E.; Warnke, L.A.; Lacza, Z.; Cselenyák, A.; Ross, K.; Shakir, S.; et al. Reactive oxygen species mediate a cellular ‘memory’ of high glucose stress signalling. Diabetologia 2007, 50, 1523–1531. [Google Scholar] [CrossRef]
- Brownlee, M. The pathobiology of diabetic complications: A unifying mechanism. Diabetes 2005, 54, 1615–1625. [Google Scholar] [CrossRef]
- Araki, E.; Nishikawa, T. Oxidative stress: A cause and therapeutic target of diabetic complications. J. Diabetes Investig. 2010, 1, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Caja, S.; Enríquez, J.A. Mitochondria in endothelial cells: Sensors and integrators of environmental cues. Redox Biol. 2017, 12, 821–827. [Google Scholar] [CrossRef]
- Cannito, S.; Giardino, I.; d’Apolito, M.; Pettoello-Mantovani, M.; Scaltrito, F.; Mangieri, D.; Piscazzi, A. The Multifaceted Role of Mitochondria in Angiogenesis. Int. J. Mol. Sci. 2025, 26, 7960. [Google Scholar] [CrossRef]
- Zorov, D.B.; Juhaszova, M.; Sollott, S.J. Mitochondrial ROS-induced ROS release: An update and review. Biochim. Biophys. Acta 2006, 1757, 509–517. [Google Scholar] [CrossRef]
- Kowluru, R.A.; Alka, K. Mitochondrial Quality Control and Metabolic Memory Phenomenon Associated with Continued Progression of Diabetic Retinopathy. Int. J. Mol. Sci. 2023, 24, 8076. [Google Scholar] [CrossRef]
- Hombrebueno, J.R.; Cairns, L.; Dutton, L.R.; Lyons, T.J.; Brazil, D.P.; Moynagh, P.; Curtis, T.M.; Xu, H. Uncoupled turnover disrupts mitochondrial quality control in diabetic retinopathy. JCI Insight 2019, 4, e129760. [Google Scholar] [CrossRef]
- Kowluru, R.A.; Mohammad, G.; Kumar, J. Impaired Removal of the Damaged Mitochondria in the Metabolic Memory Phenomenon Associated with Continued Progression of Diabetic Retinopathy. Mol. Neurobiol. 2024, 61, 188–199. [Google Scholar] [CrossRef]
- Ho, P.T.B.; Clark, I.M.; Le, L.T.T. MicroRNA-Based Diagnosis and Therapy. Int. J. Mol. Sci. 2022, 23, 7167. [Google Scholar] [CrossRef] [PubMed]
- Wenceslau, C.F.; McCarthy, C.G.; Szasz, T.; Spitler, K.; Goulopoulou, S.; Webb, R.C. Working Group on DAMPs in Cardiovascular Disease. Mitochondrial damage-associated molecular patterns and vascular function. Eur. Heart J. 2014, 35, 1172–1177. [Google Scholar] [CrossRef] [PubMed]
- Giardino, I.; d’Apolito, M.; Brownlee, M.; Maffione, A.B.; Colia, A.L.; Sacco, M.; Ferrara, P.; Pettoello-Mantovani, M. Vascular toxicity of urea, a new “old player” in the pathogenesis of chronic renal failure induced cardiovascular diseases. Turk. Pediatri Ars. 2017, 52, 187–193. [Google Scholar] [CrossRef]
- Vercellino, I.; Sazanov, L.A. The assembly, regulation and function of the mitochondrial respiratory chain. Nat. Rev. Mol. Cell Biol. 2022, 23, 141–161. [Google Scholar] [CrossRef] [PubMed]
- Dai, W.; Lu, H.; Chen, Y.; Yang, D.; Sun, L.; He, L. The Loss of Mitochondrial Quality Control in Diabetic Kidney Disease. Front. Cell Dev. Biol. 2021, 9, 706832. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Qi, F.; Guo, F.; Shao, M.; Song, Y.; Ren, G.; Linlin, Z.; Qin, G.; Zhao, Y. An update on chronic complications of diabetes mellitus: From molecular mechanisms to therapeutic strategies with a focus on metabolic memory. Mol. Med. 2024, 30, 71. [Google Scholar] [CrossRef]
- Mohammad, H.P.; Barbash, O.; Creasy, C.L. Targeting epigenetic modifications in cancer therapy: Erasing the roadmap to cancer. Nat. Med. 2019, 25, 403–418. [Google Scholar] [CrossRef] [PubMed]
- Schisano, B.; Tripathi, G.; McGee, K.; McTernan, P.G.; Ceriello, A. Glucose oscillations, more than constant high glucose, induce p53 activation and a metabolic memory in human endothelial cells. Diabetologia 2011, 54, 1219–1226. [Google Scholar] [CrossRef]
- Brownlee, M.; Hirsch, I.B. Glycemic variability: A hemoglobin A1c-independent risk factor for diabetic complications. JAMA 2006, 295, 1707–1708. [Google Scholar] [CrossRef]
- Tonna, S.; El-Osta, A.; Cooper, M.E.; Tikellis, C. Metabolic memory and diabetic nephropathy: Potential role for epigenetic mechanisms. Nat. Rev. Nephrol. 2010, 6, 332–341. [Google Scholar] [CrossRef]
- Kushwaha, K.; Garg, S.S.; Gupta, J. Targeting epigenetic regulators for treating diabetic nephropathy. Biochimie 2022, 202, 146–158. [Google Scholar] [CrossRef]
- Siebel, A.L.; Fernandez, A.Z.; El-Osta, A. Glycemic memory associated epigenetic changes. Biochem. Pharmacol. 2010, 80, 1853–1859. [Google Scholar] [CrossRef]
- Reddy, M.A.; Zhang, E.; Natarajan, R. Epigenetic mechanisms in diabetic complications and metabolic memory. Diabetologia 2015, 58, 443–455. [Google Scholar] [CrossRef] [PubMed]
- Tanemoto, F.; Nangaku, M.; Mimura, I. Epigenetic memory contributing to the pathogenesis of AKI-to-CKD transition. Front. Mol. Biosci. 2022, 9, 1003227. [Google Scholar] [CrossRef] [PubMed]
- Esteller, M. Epigenetics in cancer. N. Engl. J. Med. 2008, 358, 1148–1159. [Google Scholar] [CrossRef]
- Li, E.; Bestor, T.H.; Jaenisch, R. Targeted mutation of the DNA methyltransferase gene results in embryonic lethality. Cell 1992, 69, 915–926. [Google Scholar] [CrossRef]
- Egger, G.; Liang, G.; Aparicio, A.; Jones, P.A. Epigenetics in human disease and prospects for epigenetic therapy. Nature 2004, 429, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Robertson, K.D. DNA methylation and chromatin—Unraveling the tangled web. Oncogene 2002, 21, 5361–5379. [Google Scholar] [CrossRef]
- Okano, M.; Bell, D.W.; Haber, D.A.; Li, E. DNA methyltransferases Dnmt3a and Dnmt3b are essential for de novo methylation and mammalian development. Cell 1999, 99, 247–257. [Google Scholar] [CrossRef]
- Dabrowski, M.J.; Wojtas, B. Global DNA Methylation Patterns in Human Gliomas and Their Interplay with Other Epigenetic Modifications. Int. J. Mol. Sci. 2019, 20, 3478. [Google Scholar] [CrossRef]
- Toth, D.M.; Szeri, F.; Ashaber, M.; Muazu, M.; Szekvolgyi, L.; Aranyi, T. Tissue-specific roles of de novo DNA methyltransferases. Epigenetics Chromatin 2025, 18, 5. [Google Scholar] [CrossRef]
- Yang, L.; Yu, S.J.; Hong, Q.; Yang, Y.; Shao, Z.M. Reduced Expression of TET1, TET2, TET3 and TDG mRNAs Are Associated with Poor Prognosis of Patients with Early Breast Cancer. PLoS ONE 2015, 10, e0133896. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, Y.; Wang, C.; Wang, X. TET (Ten-eleven translocation) family proteins: Structure, biological functions and applications. Signal Transduct. Target. Ther. 2023, 8, 297. [Google Scholar] [CrossRef] [PubMed]
- Sufiyan, S.; Salam, H.; Ilyas, S.; Amin, W.; Arshad, F.; Fatima, K.; Naeem, S.; Laghari, A.A.; Enam, S.A.; Mughal, N. Prognostic implications of DNA methylation machinery (DNMTs and TETs) expression in gliomas: Correlations with tumor grading and patient survival. J. Neurooncol. 2025, 173, 667–682. [Google Scholar] [CrossRef] [PubMed]
- Kouzarides, T. Chromatin modifications and their function. Cell 2007, 128, 693–705. [Google Scholar] [CrossRef] [PubMed]
- Hermann, J.; Schurgers, L.; Jankowski, V. Identification and characterization of post-translational modifications: Clinical implications. Mol. Aspects Med. 2022, 86, 101066. [Google Scholar] [CrossRef] [PubMed]
- Ji, Y.; Liu, S.; Zhang, Y.; Min, Y.; Wei, L.; Guan, C.; Yu, H.; Zhang, Z. Lysine crotonylation in disease: Mechanisms, biological functions and therapeutic targets. Epigenetics Chromatin 2025, 18, 13. [Google Scholar] [CrossRef]
- Raju, C.; Sankaranarayanan, K. Insights on post-translational modifications in fatty liver and fibrosis progression. Biochim. Biophys. Acta Mol. Basis Dis. 2025, 1871, 167659. [Google Scholar] [CrossRef]
- Shiio, Y.; Eisenman, R.N. Histone sumoylation is associated with transcriptional repression. Proc. Natl. Acad. Sci. USA 2003, 100, 13225–13230. [Google Scholar] [CrossRef]
- Tahiliani, M.; Mei, P.; Fang, R.; Leonor, T.; Rutenberg, M.; Shimizu, F.; Li, J.; Rao, A.; Shi, Y. The histone H3K4 demethylase SMCX links REST target genes to X-linked mental retardation. Nature 2007, 447, 601–605. [Google Scholar] [CrossRef]
- Kaniskan, H.U.; Martini, M.L.; Jin, J. Inhibitors of Protein Methyltransferases and Demethylases. Chem. Rev. 2018, 118, 989–1068. [Google Scholar] [CrossRef]
- Bu, C.; Xie, Y.; Weng, J.; Sun, Y.; Wu, H.; Chen, Y.; Ye, Y.; Zhou, E.; Yang, Z.; Wang, J. Inhibition of JMJD3 attenuates acute liver injury by suppressing inflammation and oxidative stress in LPS/D-Gal-induced mice. Chem. Biol. Interact. 2025, 418, 111576. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Li, Y.; Zhang, N.; Hu, J.; Yin, L.; Pan, Z.; Li, Y.; Du, X.; Zhang, W.; Li, F. Quantitative DNA hypomethylation of ligand Jagged1 and receptor Notch1 signifies occurrence and progression of breast carcinoma. Am. J. Cancer Res. 2015, 5, 1621–1634. [Google Scholar]
- Tycko, B. Epigenetic gene silencing in cancer. J. Clin. Investig. 2000, 105, 401–407. [Google Scholar] [CrossRef]
- Urli, T.; Greenberg, M.V.C. Epigenetic relay: Polycomb-directed DNA methylation in mammalian development. PLoS Genet. 2025, 21, e1011854. [Google Scholar] [CrossRef] [PubMed]
- Wiles, E.T.; Selker, E.U. H3K27 methylation: A promiscuous repressive chromatin mark. Curr. Opin. Genet. Dev. 2017, 43, 31–37. [Google Scholar] [CrossRef]
- Sharma, S.; Hampton, J.T.; Kutateladze, T.G.; Liu, W.R. Epigenetic reader chromodomain as a potential therapeutic target. RSC Chem. Biol. 2025, 6, 833–844. [Google Scholar] [CrossRef]
- Angrand, P.O. Structure and Function of the Polycomb Repressive Complexes PRC1 and PRC2. Int. J. Mol. Sci. 2022, 23, 5971. [Google Scholar] [CrossRef] [PubMed]
- Seto, E.; Yoshida, M. Erasers of histone acetylation: The histone deacetylase enzymes. Cold Spring Harb. Perspect. Biol. 2014, 6, a018713. [Google Scholar] [CrossRef] [PubMed]
- Cedar, H.; Bergman, Y. Linking DNA methylation and histone modification: Patterns and paradigms. Nat. Rev. Genet. 2009, 10, 295–304. [Google Scholar] [CrossRef]
- Esteve, P.O.; Chin, H.G.; Benner, J.; Feehery, G.R.; Samaranayake, M.; Horwitz, G.A.; Jacobsen, S.E.; Pradhan, S. Regulation of DNMT1 stability through SET7-mediated lysine methylation in mammalian cells. Proc. Natl. Acad. Sci. USA 2009, 106, 5076–5081. [Google Scholar] [CrossRef]
- Feng, Q.; Zhang, Y. The MeCP1 complex represses transcription through preferential binding, remodeling, and deacetylating methylated nucleosomes. Genes. Dev. 2001, 15, 827–832. [Google Scholar]
- Tan, J.Z.; Yan, Y.; Wang, X.X.; Jiang, Y.; Xu, H.E. EZH2: Biology, disease, and structure-based drug discovery. Acta Pharmacol. Sin. 2014, 35, 161–174. [Google Scholar] [CrossRef]
- Wahid, F.; Shehzad, A.; Khan, T.; Kim, Y.Y. MicroRNAs: Synthesis, mechanism, function, and recent clinical trials. Biochim. Biophys. Acta 2010, 1803, 1231–1243. [Google Scholar] [CrossRef]
- Nzobokela, J.; Muchaili, L.; Mwambungu, A.; Masenga Sepiso, K.; Kirabo, A. Pathophysiology and emerging biomarkers of cardiovascular-renal-hepato-metabolic syndrome. Front. Cardiovasc. Med. 2025, 12, 1661563. [Google Scholar] [CrossRef]
- Zou, C. Advances in the study of miRNAs in chronic kidney disease with cardiovascular complications. Front. Physiol. 2023, 14, 1283597. [Google Scholar] [CrossRef]
- Mahjoob, G.; Ahmadi, Y.; Fatima Rajani, H.; Khanbabaei, N.; Abolhasani, S. Circulating microRNAs as predictive biomarkers of coronary artery diseases in type 2 diabetes patients. J. Clin. Lab. Anal. 2022, 36, e24380. [Google Scholar] [CrossRef] [PubMed]
- Macgregor-Das, A.M.; Das, S. A microRNA’s journey to the center of the mitochondria. Am. J. Physiol. Heart Circ. Physiol. 2018, 315, H206–H215. [Google Scholar] [CrossRef]
- Tang, J.; Yan, H.; Zhuang, S. Histone deacetylases as targets for treatment of multiple diseases. Clin. Sci. 2013, 124, 651–662. [Google Scholar] [CrossRef] [PubMed]
- Ibanez-Cabellos, J.S.; Pallardo, F.V.; Garcia-Gimenez, J.L.; Seco-Cervera, M. Oxidative Stress and Epigenetics: miRNA Involvement in Rare Autoimmune Diseases. Antioxidants 2023, 12, 800. [Google Scholar] [CrossRef]
- Thomas, M.C. Epigenetic Mechanisms in Diabetic Kidney Disease. Curr. Diab Rep. 2016, 16, 31. [Google Scholar] [CrossRef] [PubMed]
- Marumo, T.; Yagi, S.; Kawarazaki, W.; Nishimoto, M.; Ayuzawa, N.; Watanabe, A.; Ueda, K.; Hirahashi, J.; Hishikawa, K.; Sakurai, H.; et al. Diabetes Induces Aberrant DNA Methylation in the Proximal Tubules of the Kidney. J. Am. Soc. Nephrol. 2015, 26, 2388–2397. [Google Scholar] [CrossRef]
- Mimura, I.; Chen, Z.; Natarajan, R. Epigenetic alterations and memory: Key players in the development/progression of chronic kidney disease promoted by acute kidney injury and diabetes. Kidney Int. 2025, 107, 434–456. [Google Scholar] [CrossRef]
- Dwivedi, R.S.; Herman, J.G.; McCaffrey, T.A.; Raj, D.S. Beyond genetics: Epigenetic code in chronic kidney disease. Kidney Int. 2013, 79, 23–32. [Google Scholar] [CrossRef]
- Wing, M.R.; Ramezani, A.; Gill, H.S.; Devaney, J.M.; Raj, D.S. Epigenetics of progression of chronic kidney disease: Fact or fantasy? Semin. Nephrol. 2014, 33, 363–374. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Shen, F.; Liu, F.; Zhuang, S. Histone Modifications in Acute Kidney Injury. Kidney Dis. 2022, 8, 466–477. [Google Scholar] [CrossRef] [PubMed]
- Villeneuve, L.M.; Reddy, M.A.; Lanting, L.L.; Wang, M.; Meng, L.; Natarajan, R. Epigenetic histone H3 lysine 9 methylation in metabolic memory and inflammatory phenotype of vascular smooth muscle cells in diabetes. Proc. Natl. Acad. Sci. USA 2008, 105, 9047–9052. [Google Scholar] [CrossRef]
- De Marinis, Y.; Cai, M.; Bompada, P.; Atac, D.; Kotova, O.; Johansson, M.E.; Garcia-Vaz, E.; Gomez, M.F.; Laakso, M.; Groop, L. Epigenetic regulation of the thioredoxin-interacting protein (TXNIP) gene by hyperglycemia in kidney. Kidney Int. 2016, 89, 342–353. [Google Scholar] [CrossRef]
- Yuan, H.; Reddy, M.A.; Sun, G.; Lanting, L.; Wang, M.; Kato, M.; Natarajan, R. Involvement of p300/CBP and epigenetic histone acetylation in TGF-β1-mediated gene transcription in mesangial cells. Am. J. Physiol. Ren. Physiol. 2013, 304, F601–F613. [Google Scholar] [CrossRef] [PubMed]
- Mishra, M.; Kowluru, R.A. The Role of DNA Methylation in the Metabolic Memory Phenomenon Associated With the Continued Progression of Diabetic Retinopathy. Investig. Ophthalmol. Vis. Sci. 2016, 57, 5748–5757. [Google Scholar] [CrossRef]
- Liao, Y.; Gou, L.; Chen, L.; Zhong, X.; Zhang, D.; Zhu, H.; Lu, X.; Zeng, T.; Deng, X.; Li, Y. NADPH oxidase 4 and endothelial nitric oxide synthase contribute to endothelial dysfunction mediated by histone methylations in metabolic memory. Free Radic. Biol. Med. 2018, 115, 383–394. [Google Scholar] [CrossRef]
- Brasacchio, D.; Okabe, J.; Tikellis, C.; Balcerczyk, A.; George, P.; Baker, E.K.; Calkin, A.C.; Brownlee, M.; Cooper, M.E.; El-Osta, A. Hyperglycemia induces a dynamic cooperativity of histone methylase and demethylase enzymes associated with gene-activating epigenetic marks that coexist on the lysine tail. Diabetes 2009, 58, 1229–1236. [Google Scholar] [CrossRef]
- Zeng, S.; Wu, X.; Chen, X.; Xu, H.; Zhang, T.; Xu, Y. Hypermethylated in cancer 1 (HIC1) mediates high glucose induced ROS accumulation in renal tubular epithelial cells by epigenetically repressing SIRT1 transcription. Biochim. Biophys. Acta Gene Regul. Mech. 2018, 1861, 917–927. [Google Scholar] [CrossRef]
- Rossi, M.N.; Ciolfi, A.; Matteo, V.; Pedace, L.; Nardini, C.; Loricchio, E.; Caiello, I.; Bellomo, F.; Taranta, A.; De Leo, E.; et al. Genome-wide DNA methylation analysis identifies kidney epigenetic dysregulation in a cystinosis mouse model. Front. Cell Dev. Biol. 2025, 13, 1638123. [Google Scholar] [CrossRef]
- Stenvinkel, P.; Ekstrom, T.J. Does the uremic milieu affect the epigenotype? J. Ren. Nutr. 2009, 19, 82–85. [Google Scholar] [CrossRef]
- Kato, S.; Lindholm, B.; Stenvinkel, P.; Ekstrom, T.J.; Luttropp, K.; Yuzawa, Y.; Yasuda, Y.; Tsuruta, Y.; Maruyama, S. DNA hypermethylation and inflammatory markers in incident Japanese dialysis patients. Nephron Extra 2012, 2, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Wielscher, M.; Mandaviya, P.R.; Kuehnel, B.; Joehanes, R.; Mustafa, R.; Robinson, O.; Zhang, Y.; Bodinier, B.; Walton, E.; Mishra, P.P.; et al. DNA methylation signature of chronic low-grade inflammation and its role in cardio-respiratory diseases. Nat. Commun. 2022, 13, 2408. [Google Scholar] [CrossRef]
- Vujcic, S.; Kotur-Stevuljevic, J.; Vujcic, Z.; Stojanovic, S.; Beljic Zivkovic, T.; Vuksanovic, M.; Marjanovic Petkovic, M.; Perovic Blagojevic, I.; Koprivica-Uzelac, B.; Ilic-Mijailovic, S.; et al. Global DNA Methylation in Poorly Controlled Type 2 Diabetes Mellitus: Association with Redox and Inflammatory Biomarkers. Int. J. Mol. Sci. 2025, 26, 6716. [Google Scholar] [CrossRef]
- Gluck, C.; Qiu, C.; Han, S.Y.; Palmer, M.; Park, J.; Ko, Y.A.; Guan, Y.; Sheng, X.; Hanson, R.L.; Huang, J.; et al. Kidney cytosine methylation changes improve renal function decline estimation in patients with diabetic kidney disease. Nat. Commun. 2019, 10, 2461. [Google Scholar] [CrossRef] [PubMed]
- Ingrosso, D.; Perna, A.F. DNA Methylation Dysfunction in Chronic Kidney Disease. Genes 2020, 11, 811. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.Z.; Xu, W.W.; Zhu, D.Y.; Zhang, N.; Wang, Y.L.; Ding, M.; Xie, X.M.; Sun, L.L.; Wang, X.X. Specific expression network analysis of diabetic nephropathy kidney tissue revealed key methylated sites. J. Cell Physiol. 2018, 233, 7139–7147. [Google Scholar] [CrossRef]
- Swan, E.J.; Maxwell, A.P.; McKnight, A.J. Distinct methylation patterns in genes that affect mitochondrial function are associated with kidney disease in blood-derived DNA from individuals with Type 1 diabetes. Diabet. Med. 2015, 32, 1110–1115. [Google Scholar] [CrossRef]
- Imai, S.; Guarente, L. NAD+ and sirtuins in aging and disease. Trends Cell Biol. 2014, 24, 464–471. [Google Scholar] [CrossRef]
- Zheng, Z.; Chen, H.; Li, J.; Li, T.; Zheng, B.; Zheng, Y.; Jin, H.; He, Y.; Gu, Q.; Xu, X. Sirtuin 1-mediated cellular metabolic memory of high glucose via the LKB1/AMPK/ROS pathway and therapeutic effects of metformin. Diabetes 2012, 61, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Gao, Y.; Yi, W.; Qiao, Y.; Hu, H.; Wang, Y.; Hu, Y.; Wu, S.; Sun, H.; Zhang, T. Inhibition of miRNA-155 Alleviates High Glucose-Induced Podocyte Inflammation by Targeting SIRT1 in Diabetic Mice. J. Diabetes Res. 2021, 2021, 5597394. [Google Scholar] [CrossRef]
- Orimo, M.; Minamino, T.; Miyauchi, H.; Tateno, K.; Okada, S.; Moriya, J.; Komuro, I. Protective role of SIRT1 in diabetic vascular dysfunction. Arterioscler. Thromb. Vasc. Biol. 2009, 29, 889–894. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Kim, Y.R.; Vikram, A.; Kumar, S.; Kassan, M.; Gabani, M.; Lee, S.K.; Jacobs, J.S.; Irani, K. P66Shc-Induced MicroRNA-34a Causes Diabetic Endothelial Dysfunction by Downregulating Sirtuin1. Arter. Thromb. Vasc. Biol. 2017, 36, 2394–2403. [Google Scholar] [CrossRef]
- Huang, K.; Huang, J.; Xie, X.; Wang, S.; Chen, C.; Shen, X.; Liu, P.; Huang, H. Sirt1 resists advanced glycation end products-induced expressions of fibronectin and TGF-beta1 by activating the Nrf2/ARE pathway in glomerular mesangial cells. Free Radic. Biol. Med. 2013, 65, 528–540. [Google Scholar] [CrossRef]
- Koyama, T.; Kume, S.; Koya, D.; Araki, S.; Isshiki, K.; Chin-Kanasaki, M.; Sugimoto, T.; Haneda, M.; Sugaya, T.; Kashiwagi, A.; et al. SIRT3 attenuates palmitate-induced ROS production and inflammation in proximal tubular cells. Free Radic. Biol. Med. 2011, 51, 1258–1267. [Google Scholar] [CrossRef]
- Juszczak, F.; Arnould, T.; Decleves, A.E. The Role of Mitochondrial Sirtuins (SIRT3, SIRT4 and SIRT5) in Renal Cell Metabolism: Implication for Kidney Diseases. Int. J. Mol. Sci. 2024, 25, 6936. [Google Scholar] [CrossRef]
- Dikalova, A.E.; Itani, H.A.; Nazarewicz, R.R.; McMaster, W.G.; Flynn, C.R.; Uzhachenko, R.; Fessel, J.P.; Gamboa, J.L.; Harrison, D.G.; Dikalov, S.I. Sirt3 Impairment and SOD2 Hyperacetylation in Vascular Oxidative Stress and Hypertension. Circ. Res. 2017, 121, 564–574. [Google Scholar] [CrossRef]
- Dikalova, S.; Dikalova, A. Mitochondrial deacetylase Sirt3 in vascular dysfunction and hypertension. Curr. Opin. Nephrol. Hypertens. 2024, 31, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Pacher, P.; Szabo, C. Role of poly(ADP-ribose) polymerase-1 activation in the pathogenesis of diabetic complications: Endothelial dysfunction, as a common underlying theme. Antioxid. Redox Signal 2008, 7, 1568–1580. [Google Scholar]
- Kanasaki, K.; Shi, S.; Kanasaki, M.; He, J.; Nagai, T.; Nakamura, Y.; Ishigaki, Y.; Kitada, M.; Srivastava, S.P.; Koya, D. Linagliptin-mediated DPP-4 inhibition ameliorates kidney fibrosis in streptozotocin-induced diabetic mice by inhibiting endothelial-to-mesenchymal transition in a therapeutic regimen. Diabetes 2014, 63, 2120–2131. [Google Scholar] [CrossRef]
- Wang, X.; Lin, B.; Nie, L.; Li, P. microRNA-20b contributes to high glucose-induced podocyte apoptosis by targeting SIRT7. Mol. Med. Rep. 2017, 16, 5667–5674. [Google Scholar] [CrossRef] [PubMed]
- Jin, Q.; Ma, F.; Liu, T.; Yang, L.; Mao, H.; Wang, Y.; Peng, L.; Li, P.; Zhan, Y. Sirtuins in kidney diseases: Potential mechanism and therapeutic targets. Cell Commun. Signal 2024, 22, 114. [Google Scholar]
- Zhang, Y.; Zhang, C.; Zhang, H.; Zeng, W.; Li, S.; Chen, C.; Song, X.; Sun, J.; Sun, Z.; Cui, C.; et al. ZIPK mediates endothelial cell contraction through myosin light chain phosphorylation and is required for ischemic-reperfusion injury. FASEB J. 2019, 33, 9062–9074. [Google Scholar] [CrossRef]
- Li, X.; Liu, J.; Lu, L.; Huang, T.; Hou, W.; Wang, F.; Yu, L.; Wu, F.; Qi, J.; Chen, X.; et al. Sirt7 associates with ELK1 to participate in hyperglycemia memory and diabetic nephropathy via modulation of DAPK3 expression and endothelial inflammation. Transl. Res. 2022, 247, 99–116. [Google Scholar] [CrossRef]
- Wegner, M.; Neddermann, D.; Piorunska-Stolzmann, M.; Jagodzinski, P.P. Role of epigenetic mechanisms in the development of chronic complications of diabetes. Diabetes Res. Clin. Pract. 2014, 105, 164–175. [Google Scholar] [CrossRef]
- Yang, Y.; Wang, Y.; Fan, X.; Xu, X.; Wang, H.; Wang, X.; Shi, T.; Tang, J.; Guan, Y.; Li, S.; et al. Role of DNA methylation transferase in urinary system diseases: From basic to clinical perspectives (Review). Int. J. Mol. Med. 2025, 55, 19. [Google Scholar] [CrossRef] [PubMed]
- Yao, Y.; Song, Q.; Hu, C.; Da, X.; Yu, Y.; He, Z.; Xu, C.; Chen, Q.; Wang, Q.K. Endothelial cell metabolic memory causes cardiovascular dysfunction in diabetes. Cardiovasc. Res. 2022, 118, 196–211. [Google Scholar] [PubMed]
- Pedruzzi, L.M.; Cardozo, L.F.; Daleprane, J.B.; Stockler-Pinto, M.B.; Monteiro, E.B.; Leite, M., Jr.; Vaziri, N.D.; Mafra, D. Systemic inflammation and oxidative stress in hemodialysis patients are associated with down-regulation of Nrf2. J. Nephrol. 2015, 28, 495–501. [Google Scholar] [CrossRef]
- Bondi, C.D.; Hartman, H.L.; Tan, R.J. NRF2 in kidney physiology and disease. Physiol. Rep. 2024, 12, e15961. [Google Scholar] [CrossRef]
- McClelland, A.D.; Kantharidis, P. microRNA in the development of diabetic complications. Clin. Sci. 2014, 126, 95–110. [Google Scholar] [CrossRef] [PubMed]
- Prattichizzo, F.; Giuliani, A.; De Nigris, V.; Pujadas, G.; Ceka, A.; La Sala, L.; Genovese, S.; Testa, R.; Procopio, A.D.; Olivieri, F.; et al. Extracellular microRNAs and endothelial hyperglycaemic memory: A therapeutic opportunity? Diabetes Obes. Metab. 2016, 18, 855–867. [Google Scholar] [CrossRef] [PubMed]
- Jin, J.; Wang, X.; Zhi, X.; Meng, D. Epigenetic regulation in diabetic vascular complications. J. Mol. Endocrinol. 2019, 63, R103–R115. [Google Scholar] [CrossRef]
- Zhong, X.; Liao, Y.; Chen, L.; Liu, G.; Feng, Y.; Zeng, T.; Zhang, J. The MicroRNAs in the Pathogenesis of Metabolic Memory. Endocrinology 2015, 156, 3157–3168. [Google Scholar] [CrossRef]
- Bera, A.; Das, F.; Ghosh-Choudhury, N.; Mariappan, M.M.; Kasinath, B.S.; Ghosh Choudhury, G. Reciprocal regulation of miR-214 and PTEN by high glucose regulates renal glomerular mesangial and proximal tubular epithelial cell hypertrophy and matrix expansion. Am. J. Physiol. Cell Physiol. 2017, 313, C430–C447. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhao, S.; Wu, D.; Liu, X.; Shi, M.; Wang, Y.; Zhang, F.; Ding, J.; Xiao, Y.; Guo, B. MicroRNA-22 Promotes Renal Tubulointerstitial Fibrosis by Targeting PTEN and Suppressing Autophagy in Diabetic Nephropathy. J. Diabetes Res. 2018, 2018, 4728645. [Google Scholar] [CrossRef]
- Wang, J.Y.; Gao, Y.B.; Zhang, N.; Zou, D.W.; Wang, P.; Zhu, Z.Y.; Li, J.Y.; Zhou, S.N.; Wang, S.C.; Wang, Y.Y.; et al. miR-21 overexpression enhances TGF-β1-induced epithelial-to-mesenchymal transition by target smad7 and aggravates renal damage in diabetic nephropathy. Mol. Cell Endocrinol. 2014, 392, 163–172. [Google Scholar] [CrossRef]
- Kato, M.; Zhang, J.; Wang, M.; Lanting, L.; Yuan, H.; Rossi, J.J.; Natarajan, R. MicroRNA-192 in diabetic kidney glomeruli and its function in TGF-beta-induced collagen expression via inhibition of E-box repressors. Proc. Natl. Acad. Sci. USA 2007, 104, 3432–3437. [Google Scholar] [CrossRef] [PubMed]
- Barutta, F.; Bellini, S.; Mastrocola, R.; Bruno, G.; Gruden, G. MicroRNA and Microvascular Complications of Diabetes. Int. J. Endocrinol. 2018, 2018, 6890501. [Google Scholar] [CrossRef]
- da Cunha, R.S.D.; Azevedo, C.A.B.; Miniskiskosky, G.; Gregório, P.C.; Stinghen, A.E.M. MicroRNAs and vascular damage in chronic kidney disease: Advances and clinical implications. J. Bras. Nefrol. 2025, 47, e20240223. [Google Scholar] [CrossRef] [PubMed]
- Satake, E.; Pezzolesi, M.G.; Md Dom, Z.I.; Smiles, A.M.; Niewczas, M.A.; Krolewski, A.S. Circulating miRNA Profiles Associated With Hyperglycemia in Patients With Type 1 Diabetes. Diabetes 2018, 67, 1013–1023. [Google Scholar] [CrossRef] [PubMed]
- Ding, M.; Shi, R.; Du, Y.; Chang, P.; Gao, T.; De, D.; Chen, Y.; Li, M.; Li, J.; Li, K.; et al. O-GlcNAcylation-mediated endothelial metabolic memory contributes to cardiac damage via small extracellular vesicles. Cell Metab. 2025, 37, 1344–1363 e6. [Google Scholar] [CrossRef]
- Intine, R.V.; Sarras, M.P., Jr. Metabolic memory and chronic diabetes complications: Potential role for epigenetic mechanisms. Curr. Diab Rep. 2013, 12, 551–559. [Google Scholar] [CrossRef] [PubMed]
- Yang, A.Y.; Kim, H.; Li, W.; Kong, A.N. Natural compound-derived epigenetic regulators targeting epigenetic readers, writers and erasers. Curr. Top. Med. Chem. 2017, 16, 697–713. [Google Scholar] [CrossRef]
- Biswas, S.; Rao, C.M. Epigenetic tools (The Writers, The Readers and The Erasers) and their implications in cancer therapy. Eur. J. Pharmacol. 2018, 837, 8–24. [Google Scholar] [CrossRef]
- Contieri, B.; Duarte, B.K.L.; Lazarini, M. Updates on DNA methylation modifiers in acute myeloid leukemia. Ann. Hematol. 2020, 99, 693–701. [Google Scholar] [CrossRef]
- Pinto, V.; Bergantim, R.; Caires, H.R.; Seca, H.; Guimaraes, J.E.; Vasconcelos, M.H. Multiple Myeloma: Available Therapies and Causes of Drug Resistance. Cancers 2020, 12, 407. [Google Scholar] [CrossRef]
- Damiani, E.; Duran, M.N.; Mohan, N.; Rajendran, P.; Dashwood, R.H. Targeting Epigenetic ‘Readers’ with Natural Compounds for Cancer Interception. J. Cancer Prev. 2020, 25, 189–203. [Google Scholar] [CrossRef]
- Arce, C.; Perez-Plasencia, C.; Gonzalez-Fierro, A.; de la Cruz-Hernandez, E.; Revilla-Vazquez, A.; Chavez-Blanco, A.; Trejo-Becerril, C.; Perez-Cardenas, E.; Taja-Chayeb, L.; Bargallo, E.; et al. A proof-of-principle study of epigenetic therapy added to neoadjuvant doxorubicin cyclophosphamide for locally advanced breast cancer. PLoS ONE 2006, 1, e98. [Google Scholar] [CrossRef]
- Candelaria, M.; Gallardo-Rincon, D.; Arce, C.; Cetina, L.; Aguilar-Ponce, J.L.; Arrieta, O.; Gonzalez-Fierro, A.; Chavez-Blanco, A.; de la Cruz-Hernandez, E.; Camargo, M.F.; et al. A phase II study of epigenetic therapy with hydralazine and magnesium valproate to overcome chemotherapy resistance in refractory solid tumors. Ann. Oncol. 2007, 18, 1529–1538. [Google Scholar] [CrossRef]
- Coronel, J.; Cetina, L.; Pacheco, I.; Trejo-Becerril, C.; Gonzalez-Fierro, A.; de la Cruz-Hernandez, E.; Perez-Cardenas, E.; Taja-Chayeb, L.; Arias-Bofill, D.; Candelaria, M.; et al. A double-blind, placebo-controlled, randomized phase III trial of chemotherapy plus epigenetic therapy with hydralazine valproate for advanced cervical cancer. Preliminary results. Med. Oncol. 2011, 28 (Suppl. 1), S540–S546. [Google Scholar] [CrossRef]
- Candelaria, M.; Herrera, A.; Labardini, J.; Gonzalez-Fierro, A.; Trejo-Becerril, C.; Taja-Chayeb, L.; Perez-Cardenas, E.; de la Cruz-Hernandez, E.; Arias-Bofill, D.; Vidal, S.; et al. Hydralazine and magnesium valproate as epigenetic treatment for myelodysplastic syndrome. Preliminary results of a phase-II trial. Ann. Hematol. 2011, 90, 379–387. [Google Scholar] [CrossRef]
- Heerboth, S.; Lapinska, K.; Snyder, N.; Leary, M.; Rollinson, S.; Sarkar, S. Use of epigenetic drugs in disease: An overview. Genet. Epigenetics 2014, 6, 9–19. [Google Scholar] [CrossRef]
- Farsetti, A.; Illi, B.; Gaetano, C. How epigenetics impacts on human diseases. Eur. J. Intern. Med. 2023, 114, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Han, Z.; Ji, X.; Luo, Y. Epigenetic Regulation of Oxidative Stress in Ischemic Stroke. Aging Dis. 2016, 7, 295–306. [Google Scholar] [CrossRef] [PubMed]
- Guzik, T.J.; Touyz, R.M. Oxidative Stress, Inflammation, and Vascular Aging in Hypertension. Hypertension 2017, 70, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Marchant, V.; Trionfetti, F.; Tejedor-Santamaria, L.; Rayego-Mateos, S.; Rotili, D.; Bontempi, G.; Domenici, A.; Mene, P.; Mai, A.; Martin-Cleary, C.; et al. BET Protein Inhibitor JQ1 Ameliorates Experimental Peritoneal Damage by Inhibition of Inflammation and Oxidative Stress. Antioxidants 2023, 12, 2055. [Google Scholar] [CrossRef]
- Fraile-Martinez, O.; De Leon-Oliva, D.; Boaru, D.L.; De Castro-Martinez, P.; Garcia-Montero, C.; Barrena-Blazquez, S.; Garcia-Garcia, J.; Garcia-Honduvilla, N.; Alvarez-Mon, M.; Lopez-Gonzalez, L.; et al. Connecting epigenetics and inflammation in vascular senescence: State of the art, biomarkers and senotherapeutics. Front. Genet. 2024, 15, 1345459. [Google Scholar] [CrossRef]
- Chen, Z.; Malek, V.; Natarajan, R. Update: The role of epigenetics in the metabolic memory of diabetic complications. Am. J. Physiol. Renal Physiol. 2024, 327, F327–F339. [Google Scholar] [CrossRef]
- Miao, F.; Chen, Z.; Genuth, S.; Paterson, A.; Zhang, L.; Wu, X.; Li, S.M.; Cleary, P.; Riggs, A.; Harlan, D.M.; et al. Evaluating the role of epigenetic histone modifications in the metabolic memory of type 1 diabetes. Diabetes 2014, 63, 1748–1762. [Google Scholar] [CrossRef]
- Chen, Z.; Miao, F.; Paterson, A.D.; Lachin, J.M.; Zhang, L.; Schones, D.E.; Wu, X.; Wang, J.; Tompkins, J.D.; Genuth, S.; et al. Epigenomic profiling reveals an association between persistence of DNA methylation and metabolic memory in the DCCT/EDIC type 1 diabetes cohort. Proc. Natl. Acad. Sci. USA 2016, 113, E3002–E3011. [Google Scholar] [CrossRef]
- Soriano-Tarraga, C.; Jimenez-Conde, J.; Giralt-Steinhauer, E.; Mola-Caminal, M.; Vivanco-Hidalgo, R.M.; Ois, A.; Rodriguez-Campello, A.; Cuadrado-Godia, E.; Sayols-Baixeras, S.; Elosua, R.; et al. Epigenome-wide association study identifies TXNIP gene associated with type 2 diabetes mellitus and sustained hyperglycemia. Hum. Mol. Genet. 2016, 25, 609–619. [Google Scholar] [CrossRef]
- Cooper, M.E.; El-Osta, A.; Allen, T.J.; Watson, A.M.D.; Thomas, M.C.; Jandeleit-Dahm, K.A.M. Metabolic Karma-The Atherogenic Legacy of Diabetes: The 2017 Edwin Bierman Award Lecture. Diabetes 2018, 67, 785–790. [Google Scholar] [CrossRef]
- Chen, Z.; Natarajan, R. Epigenetic modifications in metabolic memory: What are the memories, and can we erase them? Am. J. Physiol. Cell Physiol. 2022, 323, C570–C582. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Zhao, S.; Yuan, Q.; Zhu, L.; Li, F.; Wang, H.; Kong, D.; Hao, J. TXNIP, a novel key factor to cause Schwann cell dysfunction in diabetic peripheral neuropathy, under the regulation of PI3K/Akt pathway inhibition-induced DNMT1 and DNMT3a overexpression. Cell Death Dis. 2021, 12, 642. [Google Scholar] [CrossRef]
- Singh, L.P. Thioredoxin Interacting Protein (TXNIP) and Pathogenesis of Diabetic Retinopathy. J. Clin. Exp. Ophthalmol. 2013, 4, 4172. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Calzon, S.; Maguolo, A.; Eichelmann, F.; Edsfeldt, A.; Perfilyev, A.; Maziarz, M.; Lindstrom, A.; Sun, J.; Briviba, M.; Schulze, M.B.; et al. Epigenetic biomarkers predict macrovascular events in individuals with type 2 diabetes. Cell Rep. Med. 2025, 6, 102290. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Guan, Y.; Sheng, X.; Gluck, C.; Seasock, M.J.; Hakimi, A.A.; Qiu, C.; Pullman, J.; Verma, A.; Li, H.; et al. Functional methylome analysis of human diabetic kidney disease. JCI Insight 2019, 4, e128886. [Google Scholar] [CrossRef]
- Smyth, L.J.; Patterson, C.C.; Swan, E.J.; Maxwell, A.P.; McKnight, A.J. DNA Methylation Associated with Diabetic Kidney Disease in Blood-Derived DNA. Front. Cell Dev. Biol. 2020, 8, 561907. [Google Scholar] [CrossRef]
- Smyth, L.J.; Dahlstrom, E.H.; Syreeni, A.; Kerr, K.; Kilner, J.; Doyle, R.; Brennan, E.; Nair, V.; Fermin, D.; Nelson, R.G.; et al. Epigenome-wide meta-analysis identifies DNA methylation biomarkers associated with diabetic kidney disease. Nat. Commun. 2022, 13, 7891. [Google Scholar] [CrossRef]
- Marchiori, M.; Maguolo, A.; Perfilyev, A.; Maziarz, M.; Martinell, M.; Gomez, M.F.; Ahlqvist, E.; Garcia-Calzon, S.; Ling, C. Blood-Based Epigenetic Biomarkers Associated with Incident Chronic Kidney Disease in Individuals with Type 2 Diabetes. Diabetes 2025, 74, 439–450. [Google Scholar] [CrossRef]
- Akhouri, V.; Majumder, S.; Gaikwad, A.B. Targeting DNA methylation in diabetic kidney disease: A new perspective. Life Sci. 2023, 335, 122256. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Chen, H.; Ren, S.; Xia, M.; Zhu, J.; Liu, Y.; Zhang, L.; Tang, L.; Sun, L.; Liu, H.; et al. Aberrant DNA methylation of mTOR pathway genes promotes inflammatory activation of immune cells in diabetic kidney disease. Kidney Int. 2019, 96, 409–420. [Google Scholar] [CrossRef] [PubMed]
- Al-Dabet, M.M.; Shahzad, K.; Elwakiel, A.; Sulaj, A.; Kopf, S.; Bock, F.; Gadi, I.; Zimmermann, S.; Rana, R.; Krishnan, S.; et al. Reversal of the renal hyperglycemic memory in diabetic kidney disease by targeting sustained tubular p21 expression. Nat. Commun. 2020, 13, 5062. [Google Scholar] [CrossRef]
- Feng, S.; Peden, E.K.; Guo, Q.; Lee, T.H.; Li, Q.; Yuan, Y.; Chen, C.; Huang, F.; Cheng, J. Downregulation of the endothelial histone demethylase JMJD3 is associated with neointimal hyperplasia of arteriovenous fistulas in kidney failure. J. Biol. Chem. 2022, 298, 101816. [Google Scholar] [CrossRef]
- Sanchez-Ceinos, J.; Hussain, S.; Khan, A.W.; Zhang, L.; Almahmeed, W.; Pernow, J.; Cosentino, F. Repressive H3K27me3 drives hyperglycemia-induced oxidative and inflammatory transcriptional programs in human endothelium. Cardiovasc. Diabetol. 2024, 23, 122. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Yu, C.; Zhuang, S. Histone Methyltransferase EZH2: A Potential Therapeutic Target for Kidney Diseases. Front. Physiol. 2021, 12, 640700. [Google Scholar] [CrossRef]
- Siddiqi, F.S.; Majumder, S.; Thai, K.; Abdalla, M.; Hu, P.; Advani, S.L.; White, K.E.; Bowskill, B.B.; Guarna, G.; Dos Santos, C.C.; et al. The Histone Methyltransferase Enzyme Enhancer of Zeste Homolog 2 Protects against Podocyte Oxidative Stress and Renal Injury in Diabetes. J. Am. Soc. Nephrol. 2015, 27, 2021–2034. [Google Scholar] [CrossRef]
- Sekine, S.; Youle, R.J. PINK1 import regulation; a fine system to convey mitochondrial stress to the cytosol. BMC Biol. 2018, 16, 2. [Google Scholar] [CrossRef]
- Mu, J.; Zhang, D.; Tian, Y.; Xie, Z.; Zou, M.H. BRD4 inhibition by JQ1 prevents high-fat diet-induced diabetic cardiomyopathy by activating PINK1/Parkin-mediated mitophagy in vivo. J. Mol. Cell Cardiol. 2021, 149, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Ray, K.K.; Nicholls, S.J.; Buhr, K.A.; Ginsberg, H.N.; Johansson, J.O.; Kalantar-Zadeh, K.; Kulikowski, E.; Toth, P.P.; Wong, N.; Sweeney, M.; et al. Effect of Apabetalone Added to Standard Therapy on Major Adverse Cardiovascular Events in Patients With Recent Acute Coronary Syndrome and Type 2 Diabetes: A Randomized Clinical Trial. JAMA 2020, 323, 1565–1573. [Google Scholar] [CrossRef]
- Brandts, J.; Ray, K.K. Apabetalone—BET protein inhibition in cardiovascular disease and Type 2 diabetes. Future Cardiol. 2020, 16, 385–395. [Google Scholar] [CrossRef]
- Sasaki, K.; Masaki, T. Epigenetic histone modifications in kidney disease and epigenetic memory. Clin. Exp. Nephrol. 2025, 29, 1129–1138. [Google Scholar] [CrossRef]
- Liu, M.; Qiao, Z.; Zhang, Y.; Zhan, P.; Yi, F. Histone Deacetylases Take Center Stage on Regulation of Podocyte Function. Kidney Dis. 2020, 6, 236–246, Erratum in Kidney Dis. 2020, 6, 382–383. [Google Scholar] [CrossRef]
- Khan, S.; Jena, G.; Tikoo, K.; Kumar, V. Valproate attenuates the proteinuria, podocyte and renal injury by facilitating autophagy and inactivation of NF-kappaB/iNOS signaling in diabetic rat. Biochimie 2015, 110, 1–16. [Google Scholar] [CrossRef]
- Yoshikawa, M.; Hishikawa, K.; Marumo, T.; Fujita, T. Inhibition of histone deacetylase activity szouuppresses epithelial-to-mesenchymal transition induced by TGF-beta1 in human renal epithelial cells. J. Am. Soc. Nephrol. 2007, 18, 58–65. [Google Scholar] [CrossRef]
- Huang, K.; Gao, X.; Wei, W. The crosstalk between Sirt1 and Keap1/Nrf2/ARE anti-oxidative pathway forms a positive feedback loop to inhibit FN and TGF-beta1 expressions in rat glomerular mesangial cells. Exp. Cell Res. 2017, 361, 63–72. [Google Scholar] [CrossRef]
- Martinez-Arroyo, O.; Flores-Chova, A.; Mendez-Debaets, M.; Garcia-Ferran, L.; Escriva, L.; Forner, M.J.; Redon, J.; Cortes, R.; Ortega, A. Inhibiting miR-200a-3p Increases Sirtuin 1 and Mitigates Kidney Injury in a Tubular Cell Model of Diabetes and Hypertension-Related Renal Damage. Biomolecules 2025, 15, 995. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.Y.; Zhong, X.; Huang, X.R.; Meng, X.M.; You, Y.; Chung, A.C.; Lan, H.Y. MicroRNA-29b inhibits diabetic nephropathy in db/db mice. Mol. Ther. 2014, 22, 842–853. [Google Scholar] [CrossRef] [PubMed]
- Gondaliya, P.; Dasare, A.; Srivastava, A.; Kalia, K. miR29b regulates aberrant methylation in In-Vitro diabetic nephropathy model of renal proximal tubular cells. PLoS ONE 2018, 13, e0208044, Erratum in PLoS ONE, 2019, 14, e0211591. [Google Scholar] [CrossRef]
- Putta, S.; Lanting, L.; Sun, G.; Lawson, G.; Kato, M.; Natarajan, R. Inhibiting microRNA-192 ameliorates renal fibrosis in diabetic nephropathy. J. Am. Soc. Nephrol. 2012, 23, 458–469. [Google Scholar] [CrossRef]
- Dhas, Y.; Arshad, N.; Biswas, N.; Jones, L.D.; Ashili, S. MicroRNA-21 Silencing in Diabetic Nephropathy: Insights on Therapeutic Strategies. Biomedicines 2023, 11, 2583. [Google Scholar] [CrossRef]
- de Gonzalo-Calvo, D.; van der Meer, R.W.; Rijzewijk, L.J.; Smit, J.W.; Revuelta-Lopez, E.; Nasarre, L.; Escola-Gil, J.C.; Lamb, H.J.; Llorente-Cortes, V. Serum microRNA-1 and microRNA-133a levels reflect myocardial steatosis in uncomplicated type 2 diabetes. Sci. Rep. 2017, 7, 47. [Google Scholar] [CrossRef]
- Napoli, C.; Benincasa, G.; Schiano, C.; Salvatore, M. Differential epigenetic factors in the prediction of cardiovascular risk in diabetic patients. Eur. Heart J. Cardiovasc. Pharmacother. 2020, 6, 239–247. [Google Scholar] [CrossRef]
- Al-Kafaji, G.; Al-Muhtaresh, H.A. Expression of microRNA377 and microRNA192 and their potential as blood-based biomarkers for early detection of type 2 diabetic nephropathy. Mol. Med. Rep. 2018, 18, 1171–1180. [Google Scholar]
- De, A.; Sarkar, A.; Banerjee, T.; Bhowmik, R.; Sar, S.; Shaharyar, M.A.; Karmakar, S.; Ghosh, N. MicroRNA: Unveiling novel mechanistic and theranostic pathways in diabetic cardiomyopathy. Front. Pharmacol. 2025, 16, 1613844. [Google Scholar] [CrossRef] [PubMed]
- Yousri, N.A.; Albagha, O.M.E.; Hunt, S.C. Integrated epigenome, whole genome sequence and metabolome analyses identify novel multi-omics pathways in type 2 diabetes: A Middle Eastern study. BMC Med. 2023, 21, 347. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Mei, S.; Ma, X.; Wuyun, Q.; Cai, Z.; Chen, C.; Ding, H.; Yan, J. Multi-omics insights into the pathogenesis of diabetic cardiomyopathy: Epigenetic and metabolic profiles. Epigenomics 2025, 17, 33–48. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Su, Q.; Lu, Y.; Zhao, M.; Niu, B. Application of machine learning approaches for protein-protein interactions prediction. Med. Chem. 2017, 13, 506–514. [Google Scholar] [CrossRef]
| Class | Enzymes | Common Name/Characteristics | Mechanism |
|---|---|---|---|
| I | HDAC1, HDAC2, HDAC3, HDAC8 | “Classical” HDACs | Traditional deacetylation mechanism |
| II | HDAC4, HDAC5, HDAC6, HDAC7, HDAC9, HDAC10 | “Classical” HDACs | Traditional deacetylation mechanism |
| III | SIRT 1–7 | Sirtuins | NAD+-dependent mechanism |
| IV | HDAC11 | “Classical” HDACs | Shares only weak homology with Class I and II |
| Drug Name | Target | Indication | Year |
|---|---|---|---|
| Azacitidine (Vidaza®) | DNMTi | Myelodysplastic syndromes, Chronic myelomonocytic leukemia, Acute myeloid leukemia | 2004 2004 2007 |
| Decitabine (Dacogen®) Decitabine-Cedazuridine (Inqovi®) | DNMTi | Myelodysplastic syndromes, Intermediate/high-risk myelodysplastic syndromes | 2006 2020 |
| Valproic Acid (Depakin®) | Class I/II HDAC | Epilepsy, bipolar disorder, migraine | 2010 |
| Vorinostat (Zolinza®) | Class I/II HDAC | Cutaneous T-cell lymphoma | 2006 |
| Romidepsin (Istodax®) | HDAC6 | Cutaneous T-cell lymphoma, Peripheral T-cell lymphoma (withdrawn 2021) | 2009 2011 |
| Belinostat (Beleodaq®) | Non-selective HDACi | Relapsed or refractory peripheral T-cell lymphoma | 2014 |
| Panobinostat (Farydak®) | Non-selective HDACi | Relapsed multiple myeloma (discontinued 2021) | 2015 |
| Tazemetostat (Tazverik®) | EZH2i | Metastatic or locally advanced epithelioid sarcoma, Relapsed or refractory follicular lymphoma | 2020 2020 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cannito, S.; Giardino, I.; D’Apolito, M.; Ranaldi, A.; Scaltrito, F.; Pettoello-Mantovani, M.; Piscazzi, A. From Metabolic to Epigenetic Memory: The Impact of Hyperglycemia-Induced Epigenetic Signature on Kidney Disease Progression and Complications. Genes 2025, 16, 1442. https://doi.org/10.3390/genes16121442
Cannito S, Giardino I, D’Apolito M, Ranaldi A, Scaltrito F, Pettoello-Mantovani M, Piscazzi A. From Metabolic to Epigenetic Memory: The Impact of Hyperglycemia-Induced Epigenetic Signature on Kidney Disease Progression and Complications. Genes. 2025; 16(12):1442. https://doi.org/10.3390/genes16121442
Chicago/Turabian StyleCannito, Sara, Ida Giardino, Maria D’Apolito, Alessandra Ranaldi, Francesca Scaltrito, Massimo Pettoello-Mantovani, and Annamaria Piscazzi. 2025. "From Metabolic to Epigenetic Memory: The Impact of Hyperglycemia-Induced Epigenetic Signature on Kidney Disease Progression and Complications" Genes 16, no. 12: 1442. https://doi.org/10.3390/genes16121442
APA StyleCannito, S., Giardino, I., D’Apolito, M., Ranaldi, A., Scaltrito, F., Pettoello-Mantovani, M., & Piscazzi, A. (2025). From Metabolic to Epigenetic Memory: The Impact of Hyperglycemia-Induced Epigenetic Signature on Kidney Disease Progression and Complications. Genes, 16(12), 1442. https://doi.org/10.3390/genes16121442






