Current Knowledge on Genomic Profiling of Upper Tract Urothelial Carcinoma
Abstract
:1. Introduction
2. Genomics of Upper Tract Urothelial Carcinoma
3. Genomics of Lynch Syndrome-Associated Upper Urinary Tract Urothelial Carcinomas
4. Genomics of Aristolochic Acid-Associated Upper Urinary Tract Urothelial Carcinoma
5. Differences between Bladder Cancer and Upper Urinary Tract Urothelial Carcinomas
6. Molecular Subtypes
7. Variant Histology
8. Implications for Prognosis Predication after Radical Nephroureterectomy or Kidney-Sparing Surgery
9. Implications for Systemic Therapy
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer Statistics, 2018: Cancer Statistics, 2018. CA A Cancer J. Clin. 2018, 68, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Rouprêt, M.; Babjuk, M.; Burger, M.; Capoun, O.; Cohen, D.; Compérat, E.M.; Cowan, N.C.; Dominguez-Escrig, J.L.; Gontero, P.; Hugh Mostafid, A.; et al. European Association of Urology Guidelines on Upper Urinary Tract Urothelial Carcinoma: 2020 Update. Eur. Urol. 2021, 79, 62–79. [Google Scholar] [CrossRef]
- Mori, K.; Janisch, F.; Parizi, M.K.; Mostafaei, H.; Lysenko, I.; Kimura, S.; Enikeev, D.V.; Egawa, S.; Shariat, S.F. Prognostic Value of Variant Histology in Upper Tract Urothelial Carcinoma Treated with Nephroureterectomy: A Systematic Review and Meta-Analysis. J. Urol. 2020, 203, 1075–1084. [Google Scholar] [CrossRef]
- Rink, M.; Robinson, B.D.; Green, D.A.; Cha, E.K.; Hansen, J.; Comploj, E.; Margulis, V.; Raman, J.D.; Ng, C.K.; Remzi, M.; et al. Impact of Histological Variants on Clinical Outcomes of Patients with Upper Urinary Tract Urothelial Carcinoma. J. Urol. 2012, 188, 398–404. [Google Scholar] [CrossRef] [PubMed]
- Roupret, M.; Azzouzi, A.-R.; Cussenot, O. Microsatellite Instability and Transitional Cell Carcinoma of the Upper Urinary Tract. BJU Int. 2005, 96, 489–492. [Google Scholar] [CrossRef]
- Catto, J.W.F.; Azzouzi, A.-R.; Rehman, I.; Feeley, K.M.; Cross, S.S.; Amira, N.; Fromont, G.; Sibony, M.; Cussenot, O.; Meuth, M.; et al. Promoter Hypermethylation Is Associated With Tumor Location, Stage, and Subsequent Progression in Transitional Cell Carcinoma. JCO 2005, 23, 2903–2910. [Google Scholar] [CrossRef] [PubMed]
- Sfakianos, J.P.; Cha, E.K.; Iyer, G.; Scott, S.N.; Zabor, E.C.; Shah, R.H.; Ren, Q.; Bagrodia, A.; Kim, P.H.; Hakimi, A.A.; et al. Genomic Characterization of Upper Tract Urothelial Carcinoma. Eur. Urol. 2015, 68, 970–977. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hassler, M.R.; Bray, F.; Catto, J.W.F.; Grollman, A.P.; Hartmann, A.; Margulis, V.; Matin, S.F.; Roupret, M.; Sfakianos, J.P.; Shariat, S.F.; et al. Molecular Characterization of Upper Tract Urothelial Carcinoma in the Era of Next-Generation Sequencing: A Systematic Review of the Current Literature. Eur. Urol. 2020, 78, 209–220. [Google Scholar] [CrossRef]
- Hoang, M.L.; Chen, C.-H.; Sidorenko, V.S.; He, J.; Dickman, K.G.; Yun, B.H.; Moriya, M.; Niknafs, N.; Douville, C.; Karchin, R.; et al. Mutational Signature of Aristolochic Acid Exposure as Revealed by Whole-Exome Sequencing. Sci. Transl. Med. 2013, 5, 197ra102. [Google Scholar] [CrossRef] [Green Version]
- Castells, X.; Karanović, S.; Ardin, M.; Tomić, K.; Xylinas, E.; Durand, G.; Villar, S.; Forey, N.; Le Calvez-Kelm, F.; Voegele, C.; et al. Low-Coverage Exome Sequencing Screen in Formalin-Fixed Paraffin-Embedded Tumors Reveals Evidence of Exposure to Carcinogenic Aristolochic Acid. Cancer Epidemiol. Biomark. Prev. 2015, 24, 1873–1881. [Google Scholar] [CrossRef] [Green Version]
- Bagrodia, A.; Cha, E.K.; Sfakianos, J.P.; Zabor, E.C.; Bochner, B.H.; Al-Ahmadie, H.A.; Solit, D.B.; Coleman, J.A. Genomic Biomarkers for the Prediction of Stage and Prognosis of Upper Tract Urothelial Carcinoma. J. Urol. 2016, 195, 1684–1689. [Google Scholar] [CrossRef] [Green Version]
- Moss, T.J.; Qi, Y.; Xi, L.; Peng, B.; Kim, T.-B.; Ezzedine, N.E.; Mosqueda, M.E.; Guo, C.C.; Czerniak, B.A.; Ittmann, M.; et al. Comprehensive Genomic Characterization of Upper Tract Urothelial Carcinoma. Eur. Urol. 2017, 72, 641–649. [Google Scholar] [CrossRef] [PubMed]
- Nassar, A.H.; Umeton, R.; Kim, J.; Lundgren, K.; Harshman, L.; Van Allen, E.M.; Preston, M.; Dong, F.; Bellmunt, J.; Mouw, K.W.; et al. Mutational Analysis of 472 Urothelial Carcinoma Across Grades and Anatomic Sites. Clin. Cancer Res. 2019, 25, 2458–2470. [Google Scholar] [CrossRef]
- Lee, J.Y.; Kim, K.; Sung, H.H.; Jeon, H.G.; Jeong, B.C.; Seo, S.I.; Jeon, S.S.; Lee, H.M.; Choi, H.-Y.; Kwon, G.-Y.; et al. Molecular Characterization of Urothelial Carcinoma of the Bladder and Upper Urinary Tract. Transl. Oncol. 2018, 11, 37–42. [Google Scholar] [CrossRef]
- Donahu, T.F.; Bagrodia, A.; Audenet, F.; Donoghue, M.T.A.; Cha, E.K.; Sfakianos, J.P.; Sperling, D.; Al-Ahmadie, H.; Clendenning, M.; Rosty, C.; et al. Genomic Characterization of Upper-Tract Urothelial Carcinoma in Patients With Lynch Syndrome. JCO Precis. Oncol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Robinson, B.D.; Vlachostergios, P.J.; Bhinder, B.; Liu, W.; Li, K.; Moss, T.J.; Bareja, R.; Park, K.; Tavassoli, P.; Cyrta, J.; et al. Upper Tract Urothelial Carcinoma Has a Luminal-Papillary T-Cell Depleted Contexture and Activated FGFR3 Signaling. Nat. Commun. 2019, 10, 2977. [Google Scholar] [CrossRef] [Green Version]
- Audenet, F.; Isharwal, S.; Cha, E.K.; Donoghue, M.T.A.; Drill, E.N.; Ostrovnaya, I.; Pietzak, E.J.; Sfakianos, J.P.; Bagrodia, A.; Murugan, P.; et al. Clonal Relatedness and Mutational Differences between Upper Tract and Bladder Urothelial Carcinoma. Clin. Cancer Res. 2019, 25, 967–976. [Google Scholar] [CrossRef] [Green Version]
- Bagrodia, A.; Audenet, F.; Pietzak, E.J.; Kim, K.; Murray, K.S.; Cha, E.K.; Sfakianos, J.P.; Iyer, G.; Singla, N.; Arcila, M.; et al. Genomic Profile of Urothelial Carcinoma of the Upper Tract from Ureteroscopic Biopsy: Feasibility and Validation Using Matched Radical Nephroureterectomy Specimens. Eur. Urol. Focus 2019, 5, 365–368. [Google Scholar] [CrossRef] [PubMed]
- Necchi, A.; Madison, R.; Pal, S.K.; Ross, J.S.; Agarwal, N.; Sonpavde, G.; Joshi, M.; Yin, M.; Miller, V.A.; Grivas, P.; et al. Comprehensive Genomic Profiling of Upper-Tract and Bladder Urothelial Carcinoma. Eur. Urol. Focus 2020, S2405456920302145. [Google Scholar] [CrossRef]
- Van Oers, J.M.M.; Zwarthoff, E.C.; Rehman, I.; Azzouzi, A.-R.; Cussenot, O.; Meuth, M.; Hamdy, F.C.; Catto, J.W.F. FGFR3 Mutations Indicate Better Survival in Invasive Upper Urinary Tract and Bladder Tumours. Eur. Urol. 2009, 55, 650–657. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, S.; Mayer, E.; Patel, A. Expression of P53 in Upper Urinary Tract Urothelial Carcinoma. Nat. Rev. Urol. 2011, 8, 516–522. [Google Scholar] [CrossRef] [PubMed]
- Rey, A.; Lara, P.C.; Redondo, E.; Valdés, E.; Apolinario, R. Overexpression of P53 in Transitional Cell Carcinoma of the Renal Pelvis and Ureter. Relation to Tumor Proliferation and Survival. Cancer 1997, 79, 2178–2185. [Google Scholar] [CrossRef]
- Lee, Y.-C.; Wu, W.-J.; Li, W.-M.; Lin, H.-H.; Huang, C.-N.; Chai, C.-Y.; Chang, L.-L.; Lin, H.-L.; Ke, H.-L. Prognostic Value of P53 Protein Overexpression in Upper Tract Urothelial Carcinomas in Taiwan. Anticancer Res. 2013, 33, 1091–1098. [Google Scholar]
- Furihata, M.; Yamasaki, I.; Ohtsuki, Y.; Sonobe, H.; Morioka, M.; Yamamoto, A.; Terao, N.; Kuwahara, M.; Fujisaki, N. P53 and Human Papillomavirus DNA in Renal Pelvic and Ureteral Carcinoma Including Dysplastic Lesions. Int. J. Cancer 1995, 64, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Subiela, J.D.; Territo, A.; Mercadé, A.; Balañà, J.; Aumatell, J.; Calderon, J.; Gallioli, A.; González-Padilla, D.A.; Gaya, J.M.; Palou, J.; et al. Diagnostic Accuracy of Ureteroscopic Biopsy in Predicting Stage and Grade at Final Pathology in Upper Tract Urothelial Carcinoma: Systematic Review and Meta-Analysis. Eur. J. Surg. Oncol. 2020, 46, 1989–1997. [Google Scholar] [CrossRef] [PubMed]
- Koornstra, J.J.; Mourits, M.J.; Sijmons, R.H.; Leliveld, A.M.; Hollema, H.; Kleibeuker, J.H. Management of Extracolonic Tumours in Patients with Lynch Syndrome. Lancet Oncol. 2009, 10, 400–408. [Google Scholar] [CrossRef]
- Watson, P.; Lynch, H.T. The Tumor Spectrum in HNPCC. Anticancer Res. 1994, 14, 1635–1639. [Google Scholar] [PubMed]
- Watson, P.; Riley, B. The Tumor Spectrum in the Lynch Syndrome. Fam. Cancer 2005, 4, 245–248. [Google Scholar] [CrossRef]
- Rouprêt, M.; Yates, D.R.; Comperat, E.; Cussenot, O. Upper Urinary Tract Urothelial Cell Carcinomas and Other Urological Malignancies Involved in the Hereditary Nonpolyposis Colorectal Cancer (Lynch Syndrome) Tumor Spectrum. Eur. Urol. 2008, 54, 1226–1236. [Google Scholar] [CrossRef]
- Watson, P.; Vasen, H.F.A.; Mecklin, J.-P.; Bernstein, I.; Aarnio, M.; Järvinen, H.J.; Myrhøj, T.; Sunde, L.; Wijnen, J.T.; Lynch, H.T. The Risk of Extra-Colonic, Extra-Endometrial Cancer in the Lynch Syndrome. Int. J. Cancer 2008, 123, 444–449. [Google Scholar] [CrossRef] [Green Version]
- Audenet, F.; Colin, P.; Yates, D.R.; Ouzzane, A.; Pignot, G.; Long, J.-A.; Soulie, M.; Phé, V.; Bensadoun, H.; Guy, L.; et al. A Proportion of Hereditary Upper Urinary Tract Urothelial Carcinomas Are Misclassified as Sporadic According to a Multi-Institutional Database Analysis: Proposal of Patient-Specific Risk Identification Tool. Bju Int. 2012, 110, E583–E589. [Google Scholar] [CrossRef] [PubMed]
- Michl, J.; Ingrouille, M.J.; Simmonds, M.S.J.; Heinrich, M. Naturally Occurring Aristolochic Acid Analogues and Their Toxicities. Nat. Prod. Rep. 2014, 31, 676–693. [Google Scholar] [CrossRef] [PubMed]
- Rebhan, K.; Ertl, I.E.; Shariat, S.F.; Grollman, A.P.; Rosenquist, T. Aristolochic Acid and Its Effect on Different Cancers in Uro-Oncology. Curr. Opin. Urol. 2020, 30, 689–695. [Google Scholar] [CrossRef]
- Tate, J.G.; Bamford, S.; Jubb, H.C.; Sondka, Z.; Beare, D.M.; Bindal, N.; Boutselakis, H.; Cole, C.G.; Creatore, C.; Dawson, E.; et al. COSMIC: The Catalogue Of Somatic Mutations In Cancer. Nucleic Acids Res. 2019, 47, D941–D947. [Google Scholar] [CrossRef] [Green Version]
- Springer, S.U.; Chen, C.-H.; Rodriguez Pena, M.D.C.; Li, L.; Douville, C.; Wang, Y.; Cohen, J.D.; Taheri, D.; Silliman, N.; Schaefer, J.; et al. Non-Invasive Detection of Urothelial Cancer through the Analysis of Driver Gene Mutations and Aneuploidy. Elife 2018, 7. [Google Scholar] [CrossRef]
- Lu, H.; Liang, Y.; Guan, B.; Shi, Y.; Gong, Y.; Li, J.; Kong, W.; Liu, J.; Fang, D.; Liu, L.; et al. Aristolochic Acid Mutational Signature Defines the Low-Risk Subtype in Upper Tract Urothelial Carcinoma. Theranostics 2020, 10, 4323–4333. [Google Scholar] [CrossRef]
- Cukuranovic, R.; Ignjatovic, I.; Visnjic, M.; Velickovic, L.J.; Petrovic, B.; Potic, M.; Stefanovic, V. Characteristics of Upper Urothelial Carcinoma in an Area of Balkan Endemic Nephropathy in South Serbia. A Fifty-Year Retrospective Study. Tumori 2010, 96, 674–679. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-H.; Dickman, K.G.; Huang, C.-Y.; Moriya, M.; Shun, C.-T.; Tai, H.-C.; Huang, K.-H.; Wang, S.-M.; Lee, Y.-J.; Grollman, A.P.; et al. Aristolochic Acid-Induced Upper Tract Urothelial Carcinoma in Taiwan: Clinical Characteristics and Outcomes. Int. J. Cancer 2013, 133, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Zhong, W.; Zhang, L.; Ma, J.; Shao, S.; Lin, R.; Li, X.; Xiong, G.; Fang, D.; Zhou, L. Impact of Aristolochic Acid Exposure on Oncologic Outcomes of Upper Tract Urothelial Carcinoma after Radical Nephroureterectomy. Onco Targets 2017, 10, 5775–5782. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, H.-Y.; Yang, C.-C.; Wu, C.-Y.; Wang, L.-J.; Lu, K.-L. Aristolochic Acid and Immunotherapy for Urothelial Carcinoma: Directions for Unmet Needs. Int. J. Mol. Sci. 2019, 20, 3162. [Google Scholar] [CrossRef] [Green Version]
- Green, D.A.; Rink, M.; Xylinas, E.; Matin, S.F.; Stenzl, A.; Roupret, M.; Karakiewicz, P.I.; Scherr, D.S.; Shariat, S.F. Urothelial Carcinoma of the Bladder and the Upper Tract: Disparate Twins. J. Urol. 2013, 189, 1214–1221. [Google Scholar] [CrossRef] [PubMed]
- Szarvas, T.; Módos, O.; Horváth, A.; Nyirády, P. Why Are Upper Tract Urothelial Carcinoma Two Different Diseases? Transl. Urol. 2016, 5, 636–647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanford, T.; Porten, S.; Meng, M.V. Molecular Analysis of Upper Tract and Bladder Urothelial Carcinoma: Results from a Microarray Comparison. PLoS ONE 2015, 10, e0137141. [Google Scholar] [CrossRef]
- Robertson, A.G.; Kim, J.; Al-Ahmadie, H.; Bellmunt, J.; Guo, G.; Cherniack, A.D.; Hinoue, T.; Laird, P.W.; Hoadley, K.A.; Akbani, R.; et al. Comprehensive Molecular Characterization of Muscle-Invasive Bladder Cancer. Cell 2017, 171, 540–556.e25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McConkey, D.J.; Choi, W.; Shen, Y.; Lee, I.-L.; Porten, S.; Matin, S.F.; Kamat, A.M.; Corn, P.; Millikan, R.E.; Dinney, C.; et al. A Prognostic Gene Expression Signature in the Molecular Classification of Chemotherapy-Naïve Urothelial Cancer Is Predictive of Clinical Outcomes from Neoadjuvant Chemotherapy: A Phase 2 Trial of Dose-Dense Methotrexate, Vinblastine, Doxorubicin, and Cisplatin with Bevacizumab in Urothelial Cancer. Eur. Urol. 2016, 69, 855–862. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Black, P.C.; Brown, G.A.; Dinney, C.P.N. The Impact of Variant Histology on the Outcome of Bladder Cancer Treated with Curative Intent. Urol. Oncol. Semin. Orig. Investig. 2009, 27, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Xylinas, E.; Rink, M.; Robinson, B.D.; Lotan, Y.; Babjuk, M.; Brisuda, A.; Green, D.A.; Kluth, L.A.; Pycha, A.; Fradet, Y.; et al. Impact of Histological Variants on Oncological Outcomes of Patients with Urothelial Carcinoma of the Bladder Treated with Radical Cystectomy. Eur. J. Cancer 2013, 49, 1889–1897. [Google Scholar] [CrossRef]
- Vetterlein, M.W.; Seisen, T.; Leow, J.J.; Preston, M.A.; Sun, M.; Friedlander, D.F.; Meyer, C.P.; Chun, F.K.-H.; Lipsitz, S.R.; Menon, M.; et al. Effect of Nonurothelial Histologic Variants on the Outcomes of Radical Cystectomy for Nonmetastatic Muscle-Invasive Urinary Bladder Cancer. Clin. Genitourin Cancer 2017. [Google Scholar] [CrossRef]
- Sfakianos, J.P.; Gul, Z.; Shariat, S.F.; Matin, S.F.; Daneshmand, S.; Plimack, E.; Lerner, S.; Roupret, M.; Pal, S. Genetic Differences Between Bladder and Upper Urinary Tract Carcinoma: Implications for Therapy. Eur. Urol. Oncol. 2020, S2588931120302157. [Google Scholar] [CrossRef]
- Arriola, A.G.P.; Farahani, S.J.; Bhargava, H.K.; Guzzo, T.J.; Brooks, J.S.J.; Lal, P. PD-L1 Expression Reveals Significant Association With Squamous Differentiation in Upper Tract Urothelial Carcinoma. Am. J. Clin. Pathol. 2019, 151, 561–573. [Google Scholar] [CrossRef] [PubMed]
- Guo, C.C.; Tamboli, P.; Czerniak, B. Micropapillary Variant of Urothelial Carcinoma in the Upper Urinary Tract. Arch. Pathol. Lab. Med. 2009, 133, 5. [Google Scholar] [CrossRef]
- Masson-Lecomte, A.; Colin, P.; Bozzini, G.; Nison, L.; de La Taille, A.; Comperat, E.; Zerbib, M.; Rozet, F.; Cathelineau, X.; Valeri, A.; et al. Impact of Micropapillary Histological Variant on Survival after Radical Nephroureterectomy for Upper Tract Urothelial Carcinoma. World J. Urol. 2014, 32, 531–537. [Google Scholar] [CrossRef]
- Isharwal, S.; Huang, H.; Nanjangud, G.; Audenet, F.; Chen, Y.-B.; Gopalan, A.; Fine, S.W.; Tickoo, S.K.; Lee, B.H.; Iyer, G.; et al. Intratumoral Heterogeneity of ERBB2 Amplification and HER2 Expression in Micropapillary Urothelial Carcinoma. Hum. Pathol. 2018, 77, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Keck, B.; Giedl, J.; Kunath, F.; Goebell, P.J.; Engehausen, D.G.; Hartmann, A.; Wullich, B. Clinical Course of Plasmacytoid Urothelial Carcinoma of the Upper Urinary Tract: A Case Report. Urol. Int. 2012, 89, 120–122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jibril, A.; Stevens, A.C. Plasmacytoid Urothelial Carcinoma of Ureter with Retroperitoneal Metastasis: A Case Report. Am. J. Case Rep. 2018, 19, 158–162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fox, M.D.; Xiao, L.; Zhang, M.; Kamat, A.M.; Siefker-Radtke, A.; Zhang, L.; Dinney, C.P.; Czerniak, B.; Guo, C.C. Plasmacytoid Urothelial Carcinoma of the Urinary Bladder: A Clinicopathologic and Immunohistochemical Analysis of 49 Cases. Am. J. Clin. Pathol. 2017, 147, 500–506. [Google Scholar] [CrossRef]
- Lopez-Beltran, A.; Henriques, V.; Montironi, R.; Cimadamore, A.; Raspollini, M.R.; Cheng, L. Variants and New Entities of Bladder Cancer. Histopathology 2019, 74, 77–96. [Google Scholar] [CrossRef] [Green Version]
- Lau, S.K. Nested Variant of Urothelial Carcinoma of the Renal Pelvis. Pathol. Res. Pract. 2009, 205, 508–512. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Liu, H.; Wang, P. Primary Sarcomatoid Urothelial Carcinoma of the Ureter: A Case Report and Review of the Literature. World J. Surg. Oncol. 2018, 16, 77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thiel, D.D.; Igel, T.C.; Wu, K.J. Sarcomatoid Carcinoma of Transitional Cell Origin Confined to Renal Pelvis. Urology 2006, 67, 622.e9–622.e11. [Google Scholar] [CrossRef]
- Lu, W.; Wang, Y.; Li, Y.; Cao, Y.; Han, H.; Zhou, F. Sarcomatoid Urothelial Carcinoma with Chondrosarcomatous Differentiation of the Ureter: A Case Report and Review of the Literature. Oncol. Lett. 2017, 13, 1331–1337. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; MacLennan, G.T.; Zhang, S.; Montironi, R.; Lopez-Beltran, A.; Tan, P.-H.; Foster, S.; Baldridge, L.A.; Cheng, L. Sarcomatoid Carcinoma of the Upper Urinary Tract: Clinical Outcome and Molecular Characterization. Hum. Pathol. 2009, 40, 211–217. [Google Scholar] [CrossRef]
- Hensley, P.J.; Bhalodi, A.A.; Gupta, S. Primary Upper Urinary Tract Small Cell Carcinoma: A Case Series and Literature Review. J. Endourol. Case Rep. 2017, 3, 165–168. [Google Scholar] [CrossRef] [Green Version]
- Acosta, A.M.; Kajdacsy-Balla, A. Primary Neuroendocrine Tumors of the Ureter: A Short Review. Arch. Pathol. Lab. Med. 2016, 140, 714–717. [Google Scholar] [CrossRef] [Green Version]
- Ouzzane, A.; Ghoneim, T.P.; Udo, K.; Verhasselt-Crinquette, M.; Puech, P.; Betrouni, N.; Rouprêt, M.; Villers, A.; Leroy, X.; Colin, P. Small Cell Carcinoma of the Upper Urinary Tract (UUT-SCC): Report of a Rare Entity and Systematic Review of the Literature. Cancer Treat. Rev. 2011, 37, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Al-Ahmadie, H.; Iyer, G. Updates on the Genetics and Molecular Subtypes of Urothelial Carcinoma and Select Variants. Surg. Pathol. Clin. 2018, 11, 713–723. [Google Scholar] [CrossRef] [PubMed]
- Sood, A.; Williamson, S.R.; Leavitt, D.A. Neuroendocrine Tumor of the Ureter: A Zebra Among Horses. J. Endourol. Case Rep. 2016, 2, 204–208. [Google Scholar] [CrossRef] [Green Version]
- Moschini, M.; D’Andrea, D.; Korn, S.; Irmak, Y.; Soria, F.; Compérat, E.; Shariat, S.F. Characteristics and Clinical Significance of Histological Variants of Bladder Cancer. Nat. Rev. Urol. 2017, 14, 651–668. [Google Scholar] [CrossRef]
- Ku, J.H.; Byun, S.-S.; Jeong, H.; Kwak, C.; Kim, H.H.; Lee, S.E. The Role of P53 on Survival of Upper Urinary Tract Urothelial Carcinoma: A Systematic Review and Meta-Analysis. Clin. Genitourin. Cancer 2013, 11, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Liang, P.-I.; Li, W.-M.; Wang, Y.-H.; Wu, T.-F.; Wu, W.-R.; Liao, A.C.; Shen, K.-H.; Wei, Y.-C.; Hsing, C.-H.; Shiue, Y.-L.; et al. HuR Cytoplasmic Expression Is Associated with Increased Cyclin A Expression and Poor Outcome with Upper Urinary Tract Urothelial Carcinoma. BMC Cancer 2012, 12, 611. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Y.; Zhang, J.-X.; Wang, S.-F.; Zhang, Y.; He, H.-Y. Expression of the Epigenetic H3K27me3 Modifier Genes KDM6A and EZH2 in Patients with Upper Tract Urothelial Carcinoma. Oncol. Lett. 2020, 20, 349. [Google Scholar] [CrossRef]
- Singla, N.; Krabbe, L.-M.; Aydin, A.M.; Panwar, V.; Woldu, S.L.; Freifeld, Y.; Wood, C.G.; Karam, J.A.; Weizer, A.Z.; Raman, J.D.; et al. Multi-Institutional Evaluation of the Prognostic Significance of EZH2 Expression in High-Grade Upper Tract Urothelial Carcinoma. Urol. Oncol. 2018, 36, 343.e1–343.e8. [Google Scholar] [CrossRef]
- Miyakawa, J.; Morikawa, T.; Miyama, Y.; Nakagawa, T.; Kawai, T.; Homma, Y.; Fukayama, M. Loss of Stromal Antigen 2 (STAG2) Expression in Upper Urinary Tract Carcinoma: Differential Prognostic Effect According to the Ki-67 Proliferating Index. Ann. Surg. Oncol. 2017, 24, 4059–4066. [Google Scholar] [CrossRef]
- Kaag, M.G.; O’Malley, R.L.; O’Malley, P.; Godoy, G.; Chen, M.; Smaldone, M.C.; Hrebinko, R.L.; Raman, J.D.; Bochner, B.; Dalbagni, G.; et al. Changes in Renal Function Following Nephroureterectomy May Affect the Use of Perioperative Chemotherapy. Eur. Urol. 2010, 58, 581–587. [Google Scholar] [CrossRef] [Green Version]
- Xylinas, E.; Rink, M.; Margulis, V.; Clozel, T.; Lee, R.K.; Comploj, E.; Novara, G.; Raman, J.D.; Lotan, Y.; Weizer, A.; et al. Impact of Renal Function on Eligibility for Chemotherapy and Survival in Patients Who Have Undergone Radical Nephro-Ureterectomy. BJU Int. 2013, 112, 453–461. [Google Scholar] [CrossRef] [Green Version]
- Necchi, A.; Anichini, A.; Raggi, D.; Briganti, A.; Massa, S.; Lucianò, R.; Colecchia, M.; Giannatempo, P.; Mortarini, R.; Bianchi, M.; et al. Pembrolizumab as Neoadjuvant Therapy Before Radical Cystectomy in Patients With Muscle-Invasive Urothelial Bladder Carcinoma (PURE-01): An Open-Label, Single-Arm, Phase II Study. J. Clin. Oncol. 2018, 36, 3353–3360. [Google Scholar] [CrossRef] [Green Version]
- Balar, A.V.; Castellano, D.; O’Donnell, P.H.; Grivas, P.; Vuky, J.; Powles, T.; Plimack, E.R.; Hahn, N.M.; de Wit, R.; Pang, L.; et al. First-Line Pembrolizumab in Cisplatin-Ineligible Patients with Locally Advanced and Unresectable or Metastatic Urothelial Cancer (KEYNOTE-052): A Multicentre, Single-Arm, Phase 2 Study. Lancet Oncol. 2017, 18, 1483–1492. [Google Scholar] [CrossRef]
- Balar, A.V.; Galsky, M.D.; Rosenberg, J.E.; Powles, T.; Petrylak, D.P.; Bellmunt, J.; Loriot, Y.; Necchi, A.; Hoffman-Censits, J.; Perez-Gracia, J.L.; et al. Atezolizumab as First-Line Treatment in Cisplatin-Ineligible Patients with Locally Advanced and Metastatic Urothelial Carcinoma: A Single-Arm, Multicentre, Phase 2 Trial. Lancet 2017, 389, 67–76. [Google Scholar] [CrossRef] [Green Version]
- Galsky, M.D.; Arija, J.Á.A.; Bamias, A.; Davis, I.D.; De Santis, M.; Kikuchi, E.; Garcia-Del-Muro, X.; De Giorgi, U.; Mencinger, M.; Izumi, K.; et al. Atezolizumab with or without Chemotherapy in Metastatic Urothelial Cancer (IMvigor130): A Multicentre, Randomised, Placebo-Controlled Phase 3 Trial. Lancet 2020, 395, 1547–1557. [Google Scholar] [CrossRef]
- Patel, M.R.; Ellerton, J.; Infante, J.R.; Agrawal, M.; Gordon, M.; Aljumaily, R.; Britten, C.D.; Dirix, L.; Lee, K.-W.; Taylor, M.; et al. Avelumab in Metastatic Urothelial Carcinoma after Platinum Failure (JAVELIN Solid Tumor): Pooled Results from Two Expansion Cohorts of an Open-Label, Phase 1 Trial. Lancet Oncol. 2018, 19, 51–64. [Google Scholar] [CrossRef]
- Powles, T.; Durán, I.; van der Heijden, M.S.; Loriot, Y.; Vogelzang, N.J.; De Giorgi, U.; Oudard, S.; Retz, M.M.; Castellano, D.; Bamias, A.; et al. Atezolizumab versus Chemotherapy in Patients with Platinum-Treated Locally Advanced or Metastatic Urothelial Carcinoma (IMvigor211): A Multicentre, Open-Label, Phase 3 Randomised Controlled Trial. Lancet 2018, 391, 748–757. [Google Scholar] [CrossRef]
- Bellmunt, J.; de Wit, R.; Vaughn, D.J.; Fradet, Y.; Lee, J.-L.; Fong, L.; Vogelzang, N.J.; Climent, M.A.; Petrylak, D.P.; Choueiri, T.K.; et al. Pembrolizumab as Second-Line Therapy for Advanced Urothelial Carcinoma. N. Engl. J. Med. 2017, 376, 1015–1026. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosenberg, J.E.; Hoffman-Censits, J.; Powles, T.; van der Heijden, M.S.; Balar, A.V.; Necchi, A.; Dawson, N.; O’Donnell, P.H.; Balmanoukian, A.; Loriot, Y.; et al. Atezolizumab in Patients with Locally Advanced and Metastatic Urothelial Carcinoma Who Have Progressed Following Treatment with Platinum-Based Chemotherapy: A Single-Arm, Multicentre, Phase 2 Trial. Lancet 2016, 387, 1909–1920. [Google Scholar] [CrossRef] [Green Version]
- Califano, G.; Ouzaid, I.; Verze, P.; Hermieu, J.-F.; Mirone, V.; Xylinas, E. Immune Checkpoint Inhibition in Upper Tract Urothelial Carcinoma. World J. Urol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Groenendijk, F.H.; de Jong, J.; Fransen van de Putte, E.E.; Michaut, M.; Schlicker, A.; Peters, D.; Velds, A.; Nieuwland, M.; van den Heuvel, M.M.; Kerkhoven, R.M.; et al. ERBB2 Mutations Characterize a Subgroup of Muscle-Invasive Bladder Cancers with Excellent Response to Neoadjuvant Chemotherapy. Eur. Urol. 2016, 69, 384–388. [Google Scholar] [CrossRef]
- Kujtan, L.; Hussain, A.; Subramanian, J.; Masood, A. The Evolving Genomic Landscape in Urothelial Cancer. Curr. Opin. Oncol. 2018, 1. [Google Scholar] [CrossRef]
- Morrison, K.; Challita-Eid, P.M.; Raitano, A.; An, Z.; Yang, P.; Abad, J.D.; Liu, W.; Lortie, D.R.; Snyder, J.T.; Capo, L.; et al. Development of ASG-15ME, a Novel Antibody-Drug Conjugate Targeting SLITRK6, a New Urothelial Cancer Biomarker. Mol. Cancer 2016, 15, 1301–1310. [Google Scholar] [CrossRef] [Green Version]


| Author | Year | Method | n. UTUC | n. Bladder Cancer | Characteristics of UTUC Patients |
|---|---|---|---|---|---|
| Hoang [9] | 2013 | whole exome sequencing | 19 | 0 | Patients with documented exposure to AA Pathological data not available |
| Sfakianos [7] | 2015 | NGS array (300 genes) | 83 | 102 (all HG) | All UTUC patients treated with RNU Female patients 33.7%; median age 68 (63–75) years Tumor grade: 71.1% HG-UTUC No predominant variant histologies were included Tumor stage: 20.5% pN+; 57% Pt ≥ 2 |
| Castells [10] | 2015 | low-coverage whole-exome sequencing | 17 | 0 | Urothelial tumors from 15 patients with aristolochic acid nephropathy Pathological data not available |
| Bagrodia [11] | 2016 | NGS array (300 genes) | 82 | 0 | All patients treated with RNU Female patients 34.1%; median age 68 (38–68) years Tumor grade: 72% HG-UTUC Tumor stage: 20.7% pN+; 46.3% pT ≥ 2 Tumor site: renal pelvis (52.4%), pelvis and ureter (31.7%), ureter (15.9%) 8.5% received NAC |
| Moss [12] | 2017 | whole exome sequencing | 31 | 0 | Patients treated with endoscopic biopsy or surgical resection Female patients 32%, median age 74 (68–80) years Tumor grade: 55% HG-UTUC No variant histology was present Tumor stage: 32% pT ≥ 2 Tumor site: ureter (32.2%), renal pelvis (67.8%) |
| Nassar [13] | 2018 | targeted exome sequencing (237 genes) | 65 | 407 (31% HG and 49% MIBC) | Female patients 29.2%; median age 68 (45–88) years in HG-UTUC Tumor grade: 84.6% HG-UTUC Variant differentiation: 18.5% Tumor stage: 78.5% pT ≥ 2, 23.1% pN+, 12.3% were metastatic 16.9% received prior chemotherapy treatment |
| Lee [14] | 2018 | NGS with Ampliseq (50 genes) | 31 | 61 | All UTUC patients treated with RNU, LND was performed in only 48.4% of UTUC patients Female patients 29%, median age 65 (50–79) years Tumor grade: 67.7% HG-UTUC Tumor stage: 96.8% pT ≥ 2, 29% pN+ 3.2% received NAC |
| Donahu [15] | 2018 | MSK-IMPACT assay (341 genes) | 17 | 0 | Patients with Lynch syndrome Female patients 47%; median age 61 (53–66) years Tumor grade: 71% HG-UTUC Tumor stage: 45% pT ≥ 2 Tumor site: renal pelvis (53%), ureter (47%) |
| Robinson [16] | 2019 | whole-exome sequencing and RNA sequencing | 37 | 0 | Tumor grade: all HG-UTUC 84.3% of the UTUC tumors clustered with the luminal subtype |
| Audenet [17] | 2019 | NGS platform | 195 | 454 (94% HG) | Female patients 38%; median age 67.1 (58.1–74.5) years Tumor grade: 85% HG-UTUC Variant differentiation: 12% Tumor stage: 42% pT ≥ 2; 14% were metastatic Tumor site: renal pelvis (79%), ureter (21%) |
| Bagrodia [18] | 2019 | hybridization-based exon capture assay (410 genes) | 36 (biopsy) 130 (RNU) | 0 | Tumor grade: 34% HG-UTUC in the biopsy cohort, 17% in the RNU group |
| Necchi [19] | 2020 | hybrid capture-based comprehensive genomic profiling | 479 | 1984 | Female patients 38%, median age 68 (61–75) years Source of the analyzed tumor: 61% primary tumor, 18% visceral metastasis, 8.4% lymph node metastasis, 12.5% unknown All primary tumor samples were of high grade Tumor site: renal pelvis (66%), ureter (34%) |
| Score | TP53/MDM2 Status | FGFR3 Status |
|---|---|---|
| 0 | normal | altered |
| 1 2 | Normal altered | Normal normal |
| Oncologic Characteristic | Mutational Landscape |
|---|---|
| Low-grade tumor | ↑ FGFR3 mutations, ↓ TP53/MDM2 mutations |
| High-grade tumor | ↑ mutations genes p53 signaling (TP53, ATM, ATR) ↓ FGFR3 mutations |
| Higher stage | ↓ alterations RTK/RAS pathway ↓ activating alterations of FGFR3 and HRAS ↑ TP53/MDM2 alterations ↑ TP53, ATM, ATR mutations |
| Metastatic disease | ↑ TP53 and MDM2 mutations < FGFR3 mutations than in primary tissue |
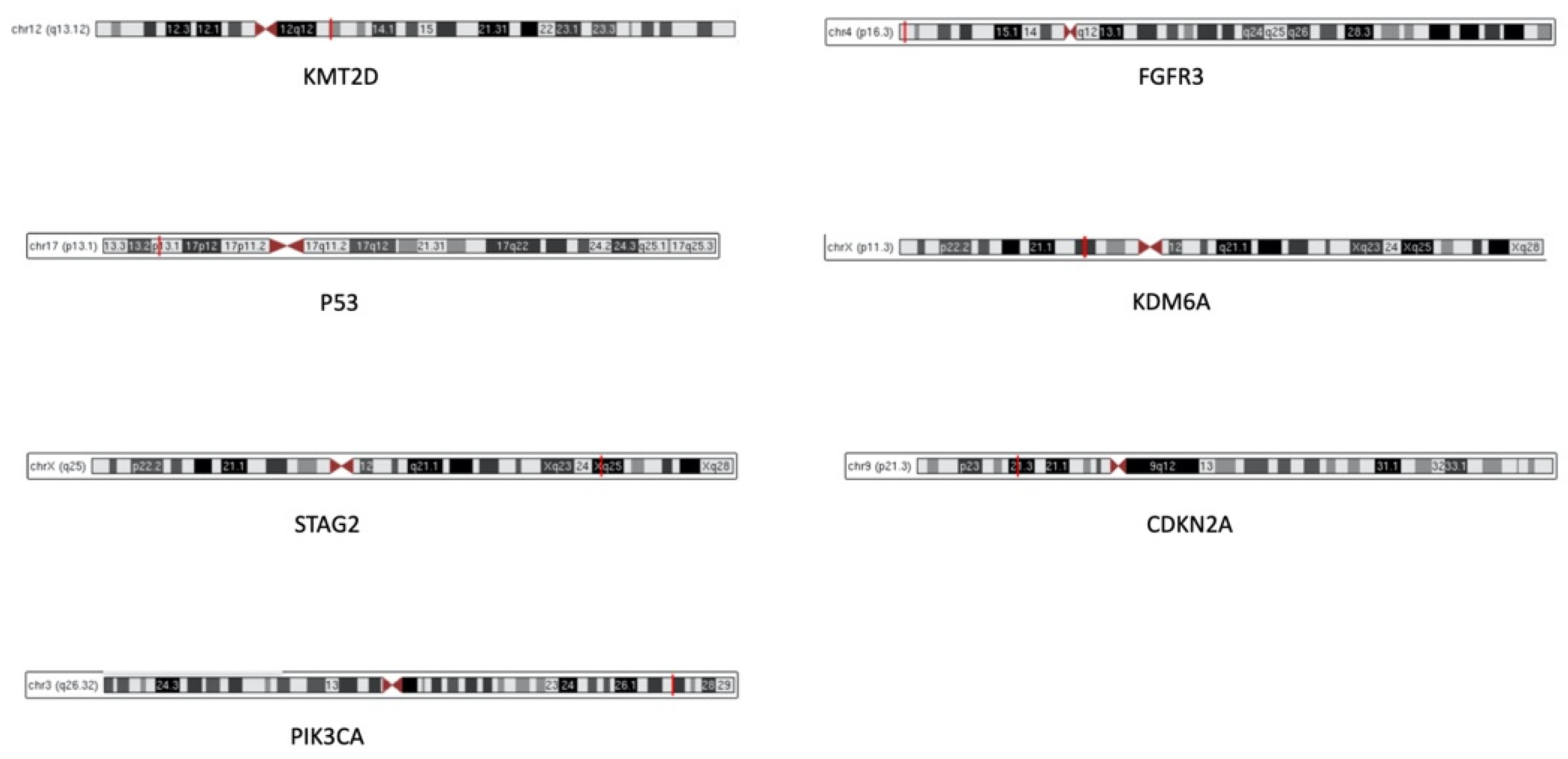
| Biomarker | Description | Function | Cytogenetic Location |
|---|---|---|---|
| FGFR3 | Fibroblast Growth Factor Receptor 3 | Transmembrane tyrosine kinase protein, member of the fibroblast growth factor receptor family. Involved in MAP kinase signaling pathway and AKT1 signaling pathway | 4p16.3 |
| KMTD2 | Histone-lysine N-methyltransferase 2D | Histone methyltransferase that methylates ASCOM protein complex, transcriptional regulator of the beta-globin and estrogen receptor genes | 12q13.12 |
| TP53 | Tumor Protein P53 | Tumor suppressor; induces growth arrest or apoptosis depending on the physiological circumstances and cell type | 17p13.1 |
| KDM6A | Lysine demethylase 6A | Histone demethylase that specifically demethylates “Lys-27” of histone H3, thereby playing a central role in histone code | Xp11.3 |
| STAG2 | Stromal antigen 2 | Chromatin binding, component of cohesin complex required for the cohesion of sister chromatids after DNA replication | Xq25 |
| CDKN2A | Cyclin Dependent Kinase Inhibitor 2A | Regulate 2 cell cycle regulatory pathways: the p53 pathway and the RB1 pathway | 9p21.3 |
| PIK3CA | Phosphatidylinositol-4,5-Bisphosphate 3-Kinase Catalytic Subunit Alpha | Lipid kinases responsible for coordinating a diverse range of cell functions including proliferation and survival. Involved in AKT and mTOR pathways | 3q26.32 |
| Urothelial Carcinoma Histology | Frequency |
|---|---|
| Pure Variant histology - Squamous - Glandular - Sarcomatoid - Micropapillary - Small cell (neuroendocrine) - Plasmacytoid - Multiple | 75.8% 24.2% 9.9% 4% 2.4% 1.9% 1.9% 0.2% 3.9% |
| Author | Year | Drug | Setting | Patients | Results |
|---|---|---|---|---|---|
| Galsky [79] IMvigor130 NCT02807636 | 2020 | Atezolizumab plus platinum-based CHT (group A), atezolizumab monotherapy (group B) or placebo plus platinum-based CHT (group C) | Locally advanced or metastatic UC | Group A
| Addition of atezolizumab to platinum-based CHT as first-line treatment prolonged PFS in patients with metastatic UC Median follow up 11.8 (6.1–17.2) months |
| Powles [81] IMvigor211 NCT02302807 | 2018 | Atezolizumab (anti- PD-L1) versus CHT (vinflunine, paclitaxel, docetaxel) | Platinum-treated locally advanced or metastatic UC | #ATZ group:
| OS did not differ significantly between groups; OS seems to be better with CHT in renal pelvis group [HR 1.32 (0.50–3.48)] Safety profile for atezolizumab was favorable compared with CHT Median follow up 17.3 (0–24.5) months |
| Patel [80] JAVELIN Solid Tumor NCT01772004 | 2018 | Avelumab (anti-PD-L1 IgG1 antibody) | Metastatic UC after platinum failure |
| Objective response: - 11% in UTUC - 18% in LTUC Median follow up 9.9 (4.3–12.1) months |
| Balar [78] IMvigor210 NCT02108652 | 2017 | Atezolizumab (anti- PD-L1) | First-line in locally advanced or metastatic UC, cisplatin ineligible patients |
| Objective response: - 39% in UTUC - 17% in LTUC Most frequent responses in luminal II subtype and in higher tumor mutation load Median follow up 17.2 (0.2–23.5) months |
| Balar [77] KEYNOTE-052 NCT02335424 | 2017 | Pembrolizumab (anti-PD-1 antibody) | First-line in locally advanced or unresectable or metastatic UC, cisplatin ineligible patients |
| Tumor response: - 22% in UTUC - 28% in LTUC PD-L1-expression cut-off 10% associated with a higher response Median follow up 5 (3.0–8.6) months |
| Bellmunt [82] KEYNOTE-045 | 2017 | Pembrolizumab (anti-PD-1 antibody) versus CHT (paclitaxel, docetaxel, vinflunine) | Advanced UC that recurred or progressed after platinum-based CHT | PMZ group:
| Longer OS and lower rate of treatment-related adverse events in PMZ group |
| Rosenberg [83] NCT02108652 | 2016 | Atezolizumab (anti- PD-L1) | Locally advanced and metastatic UC that progressed after platinum-based CHT |
| Objective response *: - 17% in bladder - 7% in renal pelvis - 9% in ureter Significantly higher response in the luminal II subtype and in in higher tumor mutation load |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Lorenzis, E.; Albo, G.; Longo, F.; Bebi, C.; Boeri, L.; Montanari, E. Current Knowledge on Genomic Profiling of Upper Tract Urothelial Carcinoma. Genes 2021, 12, 333. https://doi.org/10.3390/genes12030333
De Lorenzis E, Albo G, Longo F, Bebi C, Boeri L, Montanari E. Current Knowledge on Genomic Profiling of Upper Tract Urothelial Carcinoma. Genes. 2021; 12(3):333. https://doi.org/10.3390/genes12030333
Chicago/Turabian StyleDe Lorenzis, Elisa, Giancarlo Albo, Fabrizio Longo, Carolina Bebi, Luca Boeri, and Emanuele Montanari. 2021. "Current Knowledge on Genomic Profiling of Upper Tract Urothelial Carcinoma" Genes 12, no. 3: 333. https://doi.org/10.3390/genes12030333
APA StyleDe Lorenzis, E., Albo, G., Longo, F., Bebi, C., Boeri, L., & Montanari, E. (2021). Current Knowledge on Genomic Profiling of Upper Tract Urothelial Carcinoma. Genes, 12(3), 333. https://doi.org/10.3390/genes12030333






