Mechanistic Paradigms of Natural Plant Metabolites as Remedial Candidates for Systemic Lupus Erythromatosus
Abstract
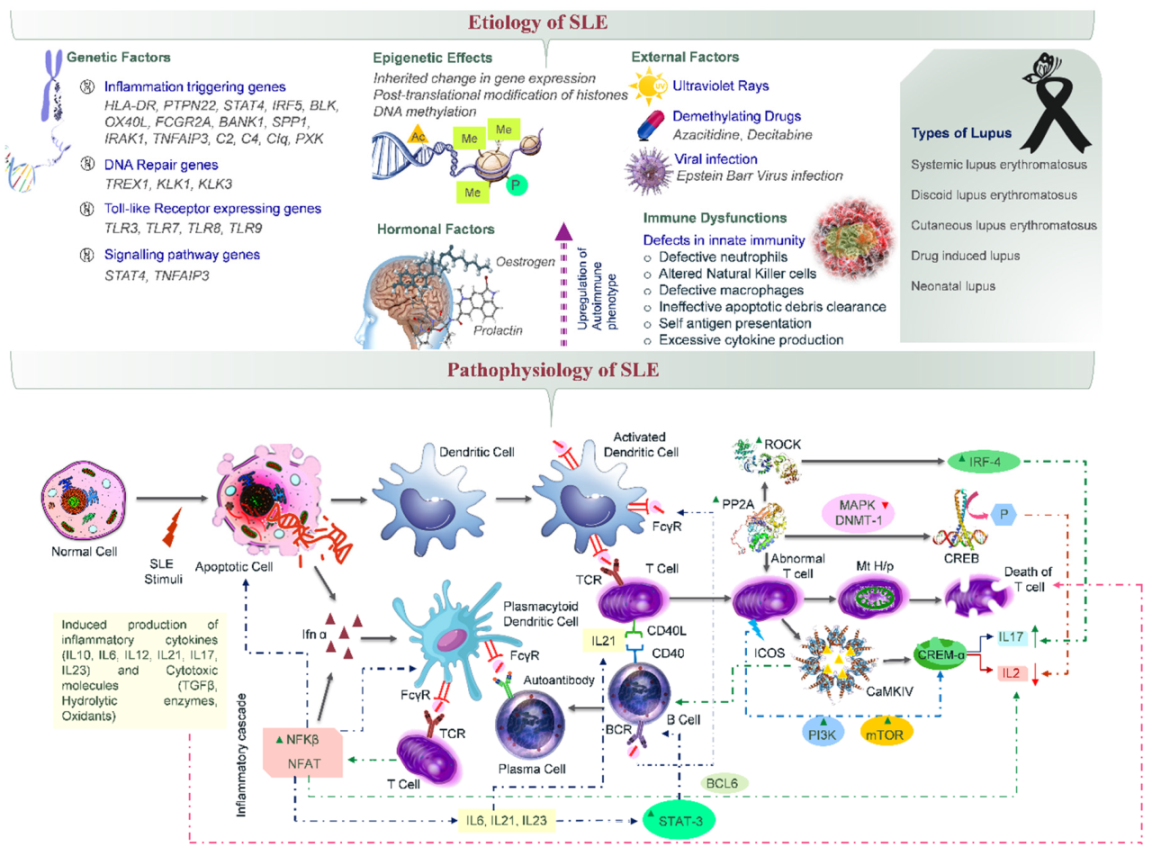
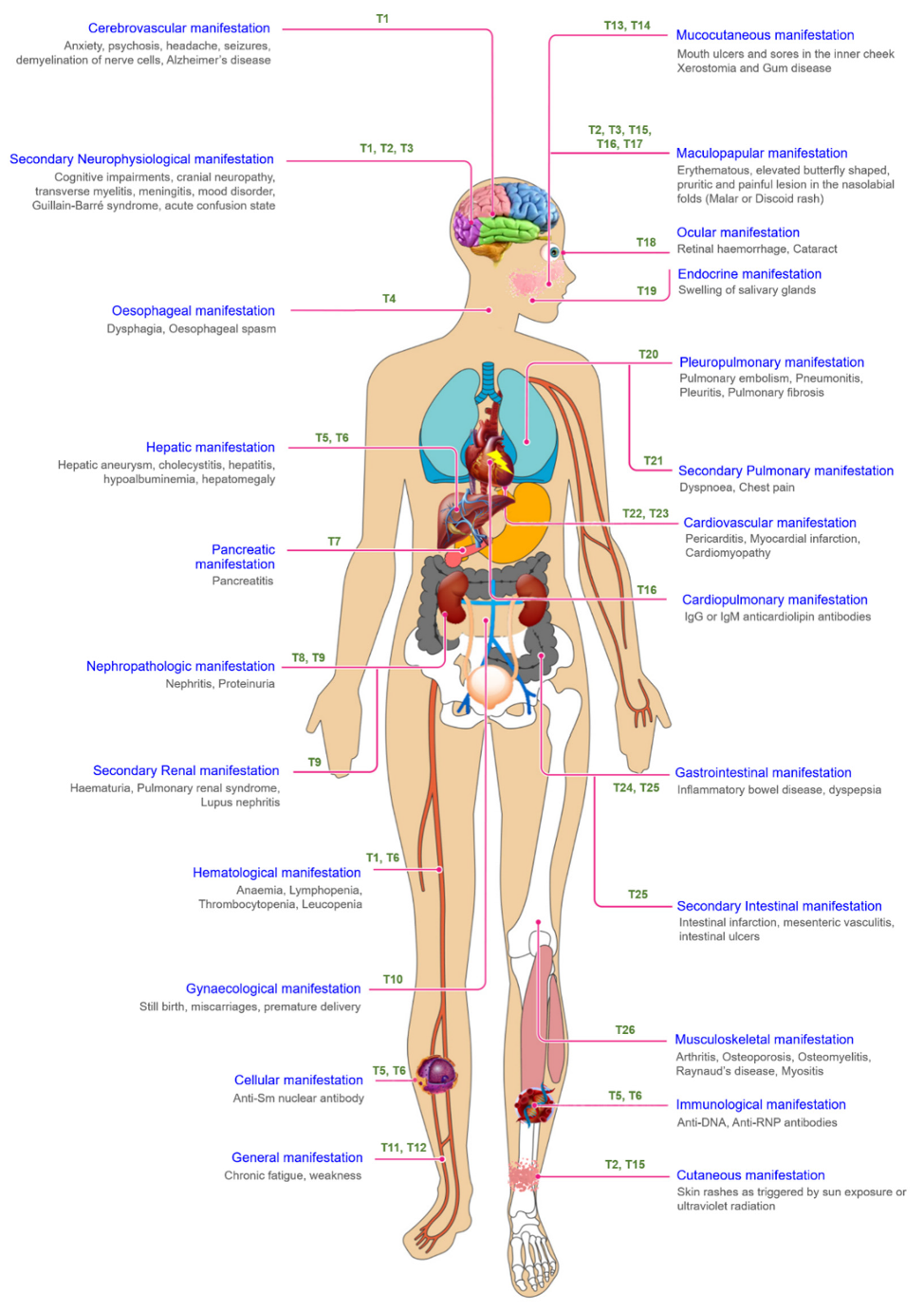
1. Introduction
2. Chemotherapeutic Modalities for Treating SLE
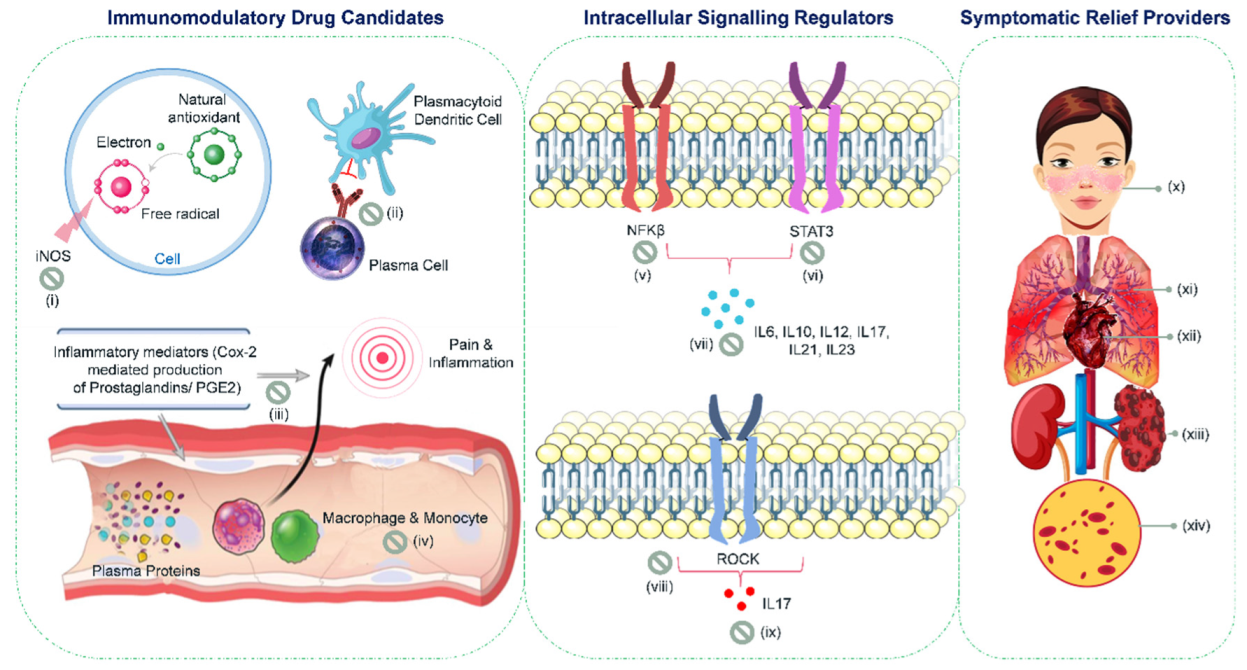
3. Plant-Derived Natural Compounds for Treating SLE
4. Natural Sources of Immunoregulatory Drug Candidates
5. Phytoconstituents as Intracellular Signaling Regulators
6. Holistic Herbs as Symptomatic Relief Providers
7. Propitious Drug Candidates
8. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sarzi-Puttini, P.; Atzeni, F.; Iaccarino, L.; Doria, A. Environment and systemic lupus erythematosus: An overview. Autoimmunity 2005, 38, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Bootsma, H.; Spronk, P.; de Boer, G.; Limburg, P.; Kallenberg, C.; Derksen, R.H.; Wolters-Dicke, J.; Gmelig-Meyling, F.; Kater, L.; Hermans, J. Prevention of relapses in Systemic Lupus Erythematosus. Lancet 1995, 345, 1595–1599. [Google Scholar] [CrossRef]
- Adu, D.; Cross, J.; Jayne, D.R. Treatment of Systemic Lupus Erythematosus with Mycophenolate Mofetil. Lupus 2001, 10, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, R. Why can’t we find a new treatment for SLE? Autoimmunity 2009, 32, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Mok, C.C.; Lau, C.S. Pathogenesis of systemic lupus erythematosus. J. Clin. Pathol. 2003, 56, 481–490. [Google Scholar] [CrossRef] [PubMed]
- Webber, D.; Cao, J.; Dominguez, D.; Gladman, D.D.; Levy, D.M.; Ng, L.; Paterson, A.D.; Touma, Z.; Urowitz, M.B.; Wither, J.E.; et al. Association of systemic lupus erythematosus (SLE) genetic susceptibility loci with lupus nephritis in childhood-onset and adult-onset SLE. Rheumatology 2020, 59, 90–98. [Google Scholar] [CrossRef]
- Munroe, M.E.; James, J.A. Genetics of lupus nephritis: Clinical implications. Semin. Nephrol. 2015, 35, 396–409. [Google Scholar] [CrossRef]
- Bertsias, G.K.; Ioannidis, J.P.A.; Aringer, M.; Bollen, E.; Bombardieri, S.; Bruce, I.N.; Cervera, R.; Dalakas, M.; Doria, A.; Hanly, J.G.; et al. EULAR Recommendations for the Management of Systemic Lupus Erythematosus with Neuropsychiatric Manifestations: Report of a Task Force of the EULAR Standing Committee for Clinical Affairs. Ann. Rheum. Dis. 2010, 69, 2074–2082. [Google Scholar] [CrossRef]
- Belot, A.; Rice, G.I.; Omarjee, S.O.; Rouchon, Q.; Smith, E.M.; Moreews, M.; Tusseau, M.; Frachette, C.; Bournhonesque, R.; Thielens, N.; et al. Contribution of rare and predicted pathogenic gene variants to childhood-onset lupus: A large, genetic panel analysis of British and French cohorts. Lancet Rheumatol. 2020, 2, e99–e109. [Google Scholar] [CrossRef]
- Ballestar, E.; Esteller, M.; Richardson, B.C. The epigenetic face of Systemic Lupus Erythematosus. J. Immunol. 2006, 176, 7143–7147. [Google Scholar] [CrossRef]
- Grimaldi, C.M. Sex and Systemic Lupus Erythematosus: The role of the sex hormones Estrogen and Prolactin on the regulation of autoreactive B cells. Curr. Opin. Rheumatol. 2006, 18, 456–461. [Google Scholar] [CrossRef] [PubMed]
- Pan, L.; Lu, M.P.; Wang, J.H.; Xu, M.; Yang, S.R. Immunological pathogenesis and treatment of systemic lupus erythematosus. World. J. Pediatr. 2020, 16, 19–30. [Google Scholar] [CrossRef]
- Sherer, Y.; Gorstein, A.; Fritzler, M.J.; Shoenfeld, Y. Autoantibody explosion in systemic lupus erythematosus: More than 100 different antibodies found in SLE patients. Semin. Arthritis Rheum. 2004, 34, 501–537. [Google Scholar] [CrossRef] [PubMed]
- Lourenco, E.V.; Cava, A.L. Cytokines in systemic lupus erythematosus. Curr. Mol. Med. 2009, 9, 242–254. [Google Scholar] [CrossRef] [PubMed]
- Nam, S.; Xie, J.; Perkins, A.; Ma, Y.; Yang, F.; Wu, J.; Jove, R. Novel synthetic derivatives of the natural product berbamine inhibit Jak2/Stat3 signaling and induce apoptosis of human melanoma cells. Mol. Oncol. 2012, 6, 484–493. [Google Scholar] [CrossRef]
- Crispín, J.C. Dysregulation of the serine/threonine phosphatase PP2A contributes to autoimmunity. Arthritis Res. Ther. 2012, 14, 1–28. [Google Scholar] [CrossRef][Green Version]
- Metry, A.M.; Al Salmi, I.; Al Balushi, F.; Yousef, M.A.; Al Ismaili, F.; Hola, A.; Hannawi, S. Systemic Lupus Erythematosus: Symptoms and Signs at Initial Presentations. Antiinflamm. Antiallergy Agents Med. Chem. 2019, 18, 142–150. [Google Scholar] [CrossRef]
- Crispín, J.C.; Kyttaris, V.C.; Terhorst, C.; Tsokos, G.C. T Cells as Therapeutic Targets in SLE. Nat. Rev. Rheumatol. 2010, 6, 317–325. [Google Scholar] [CrossRef]
- Shi, X.; Qian, T.; Li, M.; Chen, F.; Chen, Y.; Hao, F. Aberrant low expression of A20 in tumor necrosis factor-α-stimulated SLE monocytes mediates sustained NF-κB inflammatory response. Immunol. Invest. 2015, 44, 497–508. [Google Scholar]
- Xu, W.D.; Pan, H.F.; Ye, D.Q.; Xu, Y. Targeting IRF4 in autoimmune diseases. Autoimmun. Rev. 2012, 11, 918–924. [Google Scholar] [CrossRef]
- Gorelik, G.; Richardson, B. Key role of ERK pathway signaling in lupus. Autoimmunity 2010, 43, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Patavino, T.; Brady, D.M. Natural medicine and nutritional therapy as an alternative treatment in systemic lupus erythematosus. Altern. Med. Rev. 2001, 6, 460–472. [Google Scholar] [PubMed]
- Abrantes, V.E.F.; Rocha, B.A.M.D.; Nóbrega, R.B.D.; Silva-Filho, J.C.; Teixeira, C.S.; Cavada, B.S.; Gadelha, C.A.D.A.; Ferreira, S.H.; Figueiredo, J.G.; Santi-Gadelha, T.; et al. Molecular modeling of Lectin-like protein from Acacia farnesiana reveals a possible anti-inflammatory mechanism in carrageenan-induced inflammation. Biomed. Res. Int. 2013, 2013, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Bukoye, O.; Musbau, A. Immune modulation potentials of aqueous extract of Andrographis paniculata leaves in male rat. Researcher 2011, 3, 48–57. [Google Scholar]
- Chung, J.W.; Choi, R.J.; Seo, E.K.; Nam, J.W.; Dong, M.S.; Shin, E.M.; Guo, L.Y.; Kim, Y.S. Anti-inflammatory effects of (Z)-Ligustilide through suppression of mitogen-activated protein kinases and Nuclear factor-κB activation pathways. Arch. Pharm. Res. 2012, 35, 723–732. [Google Scholar] [CrossRef]
- Kaur, A.; Singh, J.; Kamboj, S.S.; Sexana, A.K.; Pandita, R.M.; Shamnugavel, M. Isolation of an N-acetyl-D-glucosamine specific lectin from the rhizomes of Arundo donax with antiproliferative activity. Phytochemistry 2005, 66, 1933–1940. [Google Scholar] [CrossRef]
- Zesiorani, N.F.; Anwar, E. Transfersome gel formulation of an ethanol extract of apples (Malus domestica Mill) containing antioxidants and in vitro penetration testing using Franz diffusion cells. Int. J. App. Pharm. 2017, 9, 32–37. [Google Scholar] [CrossRef][Green Version]
- Mahapatra, S.K.; Chakraborty, S.P.; Roy, S. Immunomodulatory role of Ocimum gratissimum and ascorbic acid against nicotine-induced murine peritoneal macrophages in vitro. Oxid. Med. Cell Longev. 2011, 2011, 1–11. [Google Scholar] [CrossRef][Green Version]
- He, D.Y.; Dai, S.M. Anti-inflammatory and immunomodulatory effects of Paeonia lactiflora Pall, a traditional Chinese herbal medicine. Front. Pharmacol. 2011, 2, 1–5. [Google Scholar] [CrossRef]
- Zeng, S.; Wang, D.; Cao, Y.; An, N.; Zeng, F.; Han, C.; Song, Y.; Deng, X. Immunopotentiation of Caffeoyl Glycoside from Picrorhiza scrophulariiflora on activation and cytokines secretion of immunocyte in vitro. Int. Immunopharmacol. 2008, 8, 1707–1712. [Google Scholar] [CrossRef]
- Sun, X.G.; Fu, X.Q.; Cai, H.B.; Liu, Q.; Li, C.H.; Liu, Y.W.; Lv, Z.P. Proteomic analysis of protective effects of polysaccharides from Salvia miltiorrhiza against immunological liver injury in mice. Phytother. Res. 2011, 25, 1087–1094. [Google Scholar] [CrossRef] [PubMed]
- Sheng, Y.; Li, L.; Holmgren, K.; Pero, R.W. DNA repair enhancement of aqueous extracts of Uncaria tomentosa in a human volunteer study. Phytomedicine 2001, 8, 275–282. [Google Scholar] [CrossRef] [PubMed]
- Reis, S.R.I.; Valente, L.M.; Sampaio, A.L.; Siani, A.C.; Gandini, M.; Azeredo, E.L.; Kubelka, C.F. Immunomodulating and antiviral activities of Uncaria tomentosa on human monocytes infected with Dengue Virus-2. Int. Immunopharmacol. 2008, 8, 468–476. [Google Scholar] [CrossRef]
- Chandrashekara, P.M.; Venkatesh, Y.P. Immunostimulatory properties of fructans derived from raw garlic (Allium Sativum, L.). Bioact. Carbohydr. Diet. Fibre 2016, 8, 65–70. [Google Scholar] [CrossRef]
- Amirghofran, Z. Herbal medicines for immunosuppression. Iran. J. Allergy Asthma Immunol. 2012, 11, 111–119. [Google Scholar]
- Ishida, M.; Nishi, K.; Kunihiro, N.; Onda, H.; Nishimoto, S.; Sugahara, T. Immunostimulatory effect of aqueous extract of Coriandrum sativum L. seed on macrophages. Sci. Food Agric. 2017, 97, 4727–4736. [Google Scholar] [CrossRef]
- Chauhan, P.S.; Gupta, K.K.; Bani, S. The immunosuppressive effects of Agyrolobium roseum and Pinitol in experimental animals. Int. Immunopharmacol. 2011, 11, 286–291. [Google Scholar] [CrossRef]
- Rahayu, R.P.; Prasetyo, R.A.; Purwanto, D.A.; Kresnoadi, U.; Iskandar, R.P.; Rubianto, M. The immunomodulatory effect of green tea (Camellia sinensis) leaves extract on immunocompromised Wistar rats infected by Candida albicans. Vet. World 2018, 11, 765–770. [Google Scholar]
- Wan, Y.G.; Che, X.Y.; Sun, W.; Huang, Y.R.; Meng, X.J.; Chen, H.L.; Shi, X.M.; Tu, Y.; Wu, W.; Liu, Y.L. Low-dose of multi-glycoside of Tripterygium wilfordii Hook. f., a natural regulator of TGF-β1/Smad signaling activity improves adriamycin-induced glomerulosclerosis in vivo. J. Ethnopharmacol. 2014, 151, 1079–1089. [Google Scholar] [CrossRef]
- Zhao, W.M.; Yang, Y.F.; Liu, Q.F.; Zhou, Y.; Tian, J.; Zhou, R. Periplocoside E, an effective compound from Periploca sepium Bge, inhibited T cell activation in vitro and in vivo. J. Pharmacol. Exp. Ther. 2006, 316, 662–669. [Google Scholar] [CrossRef]
- Gandhi, M.; Shree, R. Immuno-modulatory effect of Turmeric (Curcuma longa) and Aloe vera on cultured Polymorphonuclear cells (PMN) and adherent mononuclear cells. Webmedcentral 2016, 7, 2–7. [Google Scholar]
- Lim, S.L.; Goh, Y.M.; Noordin, M.M.; Rahman, H.S.; Othman, H.H.; Bakar, N.A.A.; Mohamed, S. Morinda citrifolia edible leaf extract enhanced immune response against lung cancer. Food Funct. 2016, 7, 741–751. [Google Scholar] [CrossRef] [PubMed]
- Klippel, J.H. Systemic lupus erythematosus: Treatment-related complications superimposed on chronic disease. JAMA 1990, 263, 1812–1815. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.J.; Sweet, D.E.; Reger, S.I.; Thompson, R.C. Fat-cell changes as a mechanism of avascular necrosis of the femoral head in cortisone-treated rabbits. J. Bone Joint. Surg. Am. 1977, 59, 729–735. [Google Scholar] [CrossRef]
- Richards, R.N. Side effects of short-term oral corticosteroids. J. Cutan. Med. Surg. 2008, 12, 77–81. [Google Scholar] [CrossRef]
- Ficat, R.P. Idiopathic bone necrosis of the femoral head. Early diagnosis and treatment. J. Bone Joint. Surg. Am. 1985, 67, 3–9. [Google Scholar] [CrossRef]
- Simkin, P.A.; Downey, D.J. Hypothesis: Retrograde embolization of marrow fat may cause osteonecrosis. J. Rheumatol. 1987, 14, 870–872. [Google Scholar]
- Cojocaru, M.; Cojocaru, I.M.; Silosi, I.; Vrabie, C.D. Manifestations of systemic lupus erythematosus. Maedica 2011, 6, 330–336. [Google Scholar]
- Sostres, C.; Gargallo, C.J.; Arroyo, M.T.; Lanas, A. Adverse effects of non-steroidal anti-inflammatory drugs (NSAIDs, aspirin and coxibs) on upper gastrointestinal tract. Best Pract. Res. Clin. Gastroenterol. 2010, 24, 121–132. [Google Scholar] [CrossRef]
- Crofford, L.J.; Lipsky, P.E.; Brooks, P.; Abramson, S.B.; Simon, L.S.; Leo, B.A. Van De Putte. Basic Biology and Clinical Application of Specific Cyclooxygenase-2 Inhibitors. Arthritis Rheum. 2000, 43, 4–13. [Google Scholar] [CrossRef]
- Østensen, M.; Villiger, P.M. Nonsteroidal anti-inflammatory drugs in systemic lupus erythematosus. Lupus 2001, 10, 135–139. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Irastorza, G.; Khamashta, M.A. Hydroxychloroquine: The cornerstone of lupus therapy. Lupus 2008, 17, 271–273. [Google Scholar] [CrossRef] [PubMed]
- Lafyatis, R.; York, M.; Marshak-Rothstein, A. Antimalarial agents: Closing the gate on toll-like receptors? Arthr. Rheum. 2006, 54, 3068–3070. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, A.; Bonsmann, G.; Anders, H.J.; Herzer, P.; Tenbrock, K.; Schneider, M. The diagnosis and treatment of systemic lupus erythematosus. Dtsch. Arztebl. Int. 2015, 112, 423–432. [Google Scholar]
- Vallerskog, T.; Gunnarsson, I.; Widhe, M.; Risselada, A.; Klareskog, L.; van Vollenhoven, R.; Trollmo, C. Treatment with rituximab affects both the cellular and the humoral arm of the immune system in patients with SLE. Clin. Immunol. 2007, 122, 62–74. [Google Scholar] [CrossRef] [PubMed]
- Pers, J.O.; Daridon, C.; Devauchelle, V.; Jousse, S.; Saraux, A.; Jamin, C.; Youinou, P. BAFF overexpression is associated with autoantibody production in autoimmune diseases. Ann. N. Y. Acad. Sci. 2005, 1050, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Dasgupta, A.; Hammett-Stabler, C.A. Herbal Supplements: Efficacy, Toxicity, Interactions with Western Drugs and Effects on Clinical Laboratory Tests, 1st ed.; John Wiley & Son: Hoboken, NJ, USA, 2011; pp. 135–154. [Google Scholar]
- Ziaei, A.; Hoppstädter, J.; Kiemer, A.K.; Ramezani, M.; Amirghofran, Z.; Diesel, B. Inhibitory effects of teuclatriol, a sesquiterpene from salvia mirzayanii, on nuclear factor-κB activation and expression of inflammatory mediators. J. Ethnopharmacol. 2015, 160, 94–100. [Google Scholar] [CrossRef]
- Upadhyay, R.K. Nutraceutical, pharmaceutical and therapeutic uses of Allium cepa: A review. Int. J. Green Pharm. 2016, 10, S46–S64. [Google Scholar]
- Kala, C.; Ali, S.S.; Khan, N.A. Immunostimulatory potential of n-butanolic fraction of hydroalcoholic extract of Costus speciosus koen. Rhizome. Int. J. Pharm. Sci. Res. 2015, 6, 2886–2892. [Google Scholar]
- Thangam, R.; Sathuvan, M.; Poongodi, A.; Suresh, V.; Pazhanichamy, K.; Sivasubramanian, S.; Kannan, S. Activation of intrinsic apoptotic signaling pathway in cancer cells by Cymbopogon citratus polysaccharide fractions. Carbohydr. Polym. 2014, 107, 138–150. [Google Scholar] [CrossRef]
- Yin, Y.; Gong, F.Y.; Wu, X.X.; Sun, Y.; Li, Y.H.; Chen, T.; Xu, Q. Anti-inflammatory and immunosuppressive effect of flavones isolated from Artemisia vestita. J. Ethnopharmacol. 2008, 120, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Sani, T.A.; Mohammadpour, E.; Mohammadi, A.; Memariani, T.; Yazdi, M.V.; Rezaee, R.; Shahsavand, S. Cytotoxic and apoptogenic properties of Dracocephalum kotschyi aerial part different fractions on calu-6 and mehr-80 lung cancer cell lines. Farmacia 2017, 65, 189–199. [Google Scholar]
- Faham, N.; Javidnia, K.; Bahmani, M.; Amirghofran, Z. Calycopterin, an immunoinhibitory compound from the extract of Dracocephalum kotschyi. Phytother. Res. 2008, 22, 1154–1158. [Google Scholar] [CrossRef] [PubMed]
- Haija, A.J.; Schulz, S.W. The role and effect of complementary and alternative medicine in Systemic Lupus Erythematosus. Rheum. Dis. Clin. North. Am. 2011, 37, 47–62. [Google Scholar] [CrossRef]
- Jiao, B.; Gao, J. Intensive research on the prospective use of complementary and alternative medicine to treat systemic lupus erythematosus. Drug Discov. Ther. 2013, 7, 167–171. [Google Scholar] [CrossRef]
- Moore, A.D.; Petri, M.A.; Manzi, S.; Isenberg, D.A.; Gordon, C.; Senécal, J.L.; Sutcliffe, N. The use of alternative medical therapies in patients with systemic lupus erythematosus. Arthr. Rheum. 2000, 43, 1410–1418. [Google Scholar] [CrossRef]
- Yarnell, E.; Abascal, K. Lupus Erythematosus and Herbal Medicine. Altern. Complement. Ther. 2008, 14, 1–10. [Google Scholar] [CrossRef]
- Alvarez-Nemegyei, J.; Bautista-Botello, A. Complementary or Alternative therapy use and health status in Systemic Lupus Erythematosus. Lupus 2009, 18, 159–163. [Google Scholar] [CrossRef]
- Greco, C.M.; Nakajima, C.; Manzi, S. Updated Review of Complementary and Alternative Medicine Treatments for Systemic Lupus Erythematosus. Curr. Rheumatol. Rep. 2013, 15, 1–9. [Google Scholar] [CrossRef]
- Prasanna, V.K.; Venkatesh, Y.P. Characterization of onion lectin (Allium cepa agglutinin) as an immunomodulatory protein inducing Th1-type immune response in vitro. Int. Immunopharmacol. 2015, 26, 304–313. [Google Scholar] [CrossRef]
| Molecular Target | Probable Utility | Therapeutic Benefits | Source Plant | Active Metabolites # | Reference (s) |
|---|---|---|---|---|---|
| iNOS and COX | Decreasing the nitrite and PGE2 levels by inhibition of the iNOS and COX expression | Anti-inflammatory | Acacia farnesiana | Lectin, Lupeol, α-Amyrin, β-Amyrin | [23] |
| Andrographis paniculata | Andrographolide | [24] | |||
| Angelica glauca | Angelic acid, β-Phellandrene, Ligustilide, Limonene | [25] | |||
| Arundo donax | N-acetyl-D-glucosamine lectin | [26] | |||
| Malus domestica | Isophytol, Farnesene, Cadinol | [27] | |||
| Ocimum gratissimum | Eugenol | [28] | |||
| Paeonia lactiflora | Gallic acid, Kaempferol | [29] | |||
| Picrorhiza scrophulariiflora | Caffeoyl glycosides, Phenylethanoid glycoside, Plantamajoside, Scrocaffeside A | [30] | |||
| Salvia miltiorrhiza | Salvianolic acid, Dihydrotanshinone, Tanshinone | [31] | |||
| Uncaria tomentosa | Mitraphylline | [32,33] | |||
| NFκB | Inhibits T cell activation through the modulation of NFκB transcription factor; reducing the level of pro-inflammatory cytokines | Immunomodulator, Signaling Regulator | Allium sativum | Allicin, Alliin, γ-Glutamyl-S-allyl-L-cysteines | [34] |
| Bupleurum falcatum | 3-O-Feruloyl 5-O-Caffeoylquinic acid, Saikosaponin | [35] | |||
| Clerodendron trichotomum | Lupeol, Friedelin, Betulinic acid, Taraxerol | [35] | |||
| Coriandrum sativum | Linalool, Terpinene, Pinene, Limonene, p-Cymene | [36] | |||
| Th1/Th2 proinflammatory cytokines | Suppress inflammation, inhibit proliferation and pro-inflammatory cytokines, downregulation of Th1/Th2 cytokines expression | Immunomodulator | Argyrolobium roseum | Pinitol | [37] |
| Camellia sinensis | Theophylline, Epigallocatechin gallate | [38] | |||
| Tripterygium wilfordii | Triptolide | [35,39,40] | |||
| STAT3 and ROCK | Downregulating the expression of STAT3 and ROCK | Signaling regulator | Berberis aristata | Berbamine | [15] |
| Curcuma longa | Curcumin | [35,41] | |||
| RAF1 and mTOR | Downregulating the expression of V-raf-leukemia viral oncogene 1 (RAF1), and mechanistic target of rapamycin (mTOR) mRNA | Signaling regulator | Morinda citrifolia | Alizarin, Asperuloside, Chrysophanol, Digoxin | [42] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Balkrishna, A.; Thakur, P.; Singh, S.; Chandra Dev, S.N.; Varshney, A. Mechanistic Paradigms of Natural Plant Metabolites as Remedial Candidates for Systemic Lupus Erythromatosus. Cells 2020, 9, 1049. https://doi.org/10.3390/cells9041049
Balkrishna A, Thakur P, Singh S, Chandra Dev SN, Varshney A. Mechanistic Paradigms of Natural Plant Metabolites as Remedial Candidates for Systemic Lupus Erythromatosus. Cells. 2020; 9(4):1049. https://doi.org/10.3390/cells9041049
Chicago/Turabian StyleBalkrishna, Acharya, Pallavi Thakur, Shivam Singh, Swami Narsingh Chandra Dev, and Anurag Varshney. 2020. "Mechanistic Paradigms of Natural Plant Metabolites as Remedial Candidates for Systemic Lupus Erythromatosus" Cells 9, no. 4: 1049. https://doi.org/10.3390/cells9041049
APA StyleBalkrishna, A., Thakur, P., Singh, S., Chandra Dev, S. N., & Varshney, A. (2020). Mechanistic Paradigms of Natural Plant Metabolites as Remedial Candidates for Systemic Lupus Erythromatosus. Cells, 9(4), 1049. https://doi.org/10.3390/cells9041049





