The Translocator Protein (TSPO) in Mitochondrial Bioenergetics and Immune Processes
Abstract
1. Introduction
2. TSPO in Mitochondrial Processes
2.1. TSPO in Mitochondrial Bioenergetics
2.2. TSPO and Redox Mechanisms
2.3. In Vivo Evidence for TSPO in Mitochondrial Processes
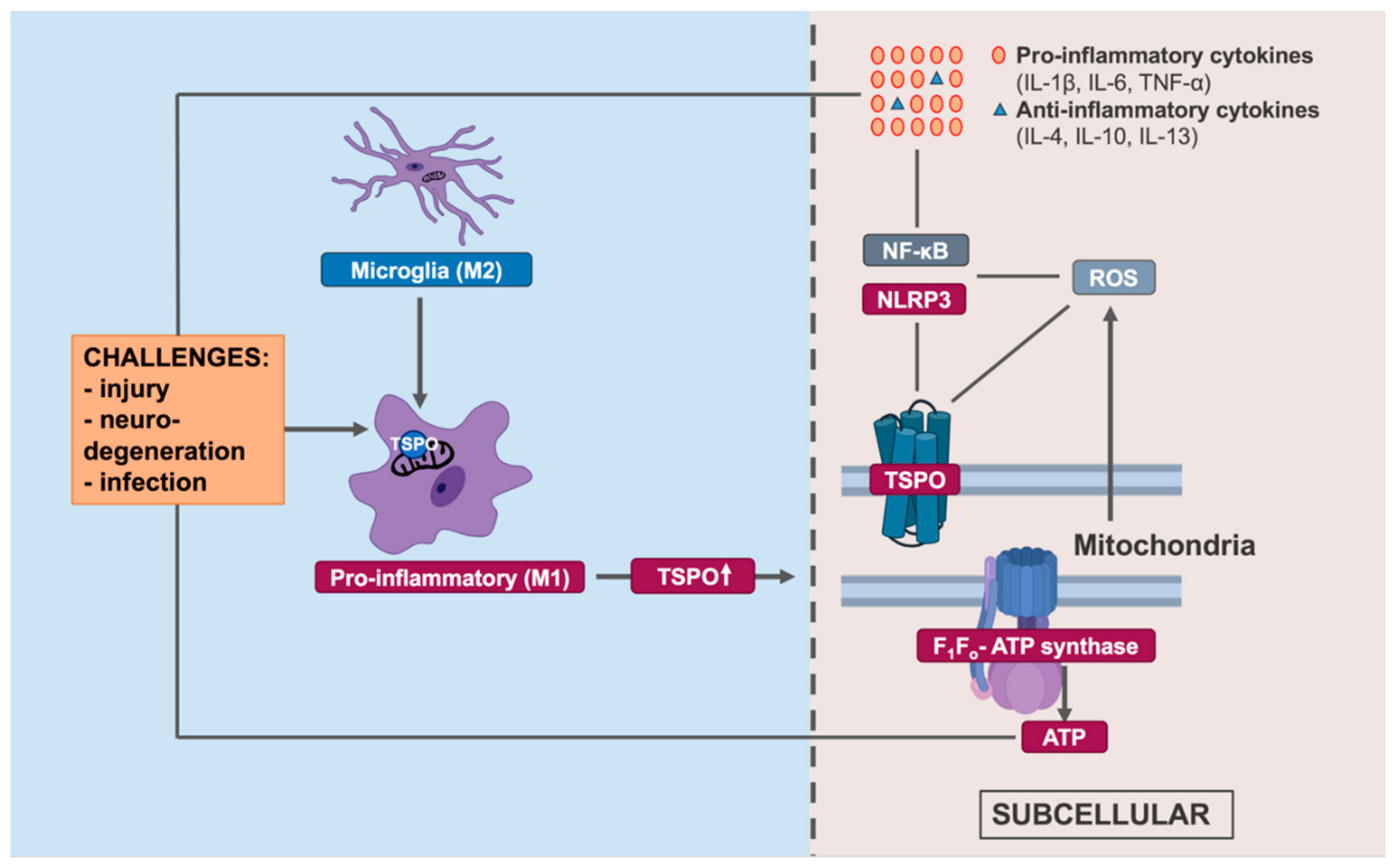
3. TSPO in the Innate Immune Response
3.1. Microglial TSPO Expression and Modulation by TSPO Ligands
3.2. Molecular Pathways of TSPO Immunomodulation
3.3. In Vivo Immunomodulation of TSPO Ligands
4. Future Directions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Banati, R.B. Visualising microglial activation in vivo. Glia 2002, 40, 206–217. [Google Scholar] [CrossRef] [PubMed]
- Kreutzberg, G.W. Microglia: A sensor for pathological events in the cns. Trends Neurosci. 1996, 19, 312–318. [Google Scholar] [CrossRef]
- Ley, K. M1 means kill; m2 means heal. J. Immunol. (Baltimore, Md.: 1950) 2017, 199, 2191–2193. [Google Scholar] [CrossRef] [PubMed]
- Akhmetzyanova, E.; Kletenkov, K.; Mukhamedshina, Y.; Rizvanov, A. Different approaches to modulation of microglia phenotypes after spinal cord injury. Front. Syst. Neurosci. 2019, 13, 37. [Google Scholar] [CrossRef] [PubMed]
- Graeber, M.B.; Li, W.; Rodriguez, M.L. Role of microglia in cns inflammation. FEBS Lett. 2011, 585, 3798–3805. [Google Scholar] [CrossRef] [PubMed]
- Graeber, M.B.; Streit, W.J. Microglia: Biology and pathology. Acta Neuropathol. 2010, 119, 89–105. [Google Scholar] [CrossRef]
- Block, M.L.; Zecca, L.; Hong, J.S. Microglia-mediated neurotoxicity: Uncovering the molecular mechanisms. Nat. Rev. Neurosci. 2007, 8, 57–69. [Google Scholar] [CrossRef]
- Banati, R.B.; Cagnin, A.; Myers, R.; Gunn, R.N.; Turkheimer, F.E.; Brooks, D.J.; Jones, T. Microglial activation in neurodegenerative diseases: A pet study using [11c](r)-pk11195. NeuroImage 2000, 11. [Google Scholar]
- Banati, R.B.; Newcombe, J.; Gunn, R.N.; Cagnin, A.; Turkheimer, F.; Heppner, F.; Price, G.; Wegner, F.; Giovannoni, G.; Miller, D.H.; et al. The peripheral benzodiazepine binding site in the brain in multiple sclerosis. Quantitative in vivo imaging of microglia as a measure of disease activity. Brain 2000, 123, 2321–2337. [Google Scholar] [CrossRef]
- Banati, R.B.; Egensperger, R.; Maassen, A.; Hager, G.; Kreutzberg, G.W.; Graeber, M.B. Mitochondria in activated microglia in vitro. J. Neurocytol. 2004, 33, 535–541. [Google Scholar] [CrossRef]
- Weinberg, S.E.; Sena, L.A.; Chandel, N.S. Mitochondria in the regulation of innate and adaptive immunity. Immunity 2015, 42, 406–417. [Google Scholar] [CrossRef] [PubMed]
- Aldana, B.I. Microglia-specific metabolic changes in neurodegeneration. J. Mol. Biol. 2019, 431, 1830–1842. [Google Scholar] [CrossRef] [PubMed]
- Orihuela, R.; McPherson, C.A.; Harry, G.J. Microglial m1/m2 polarization and metabolic states. Br. J. Pharm. 2016, 173, 649–665. [Google Scholar] [CrossRef] [PubMed]
- Nair, S.; Sobotka, K.S.; Joshi, P.; Gressens, P.; Fleiss, B.; Thornton, C.; Mallard, C.; Hagberg, H. Lipopolysaccharide-induced alteration of mitochondrial morphology induces a metabolic shift in microglia modulating the inflammatory response in vitro and in vivo. Glia 2019, 67, 1047–1061. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.; Castillo, E.; Frias, E.S.; Swanson, R.A. Bioenergetic regulation of microglia. Glia 2018, 66, 1200–1212. [Google Scholar] [CrossRef]
- Angajala, A.; Lim, S.; Phillips, J.B.; Kim, J.H.; Yates, C.; You, Z.; Tan, M. Diverse roles of mitochondria in immune responses: Novel insights into immuno-metabolism. Front. Immunol. 2018, 9. [Google Scholar] [CrossRef]
- Gatliff, J.; Campanella, M. Tspo is a redox regulator of cell mitophagy. Biochem. Soc. Trans. 2015, 43, 543–552. [Google Scholar] [CrossRef]
- Banati, R.B.; Rothe, G.; Valet, G.; Kreutzberg, G.W. Respiratory burst activity in brain macrophages: A flow cytometric study on cultured rat microglia. Neuropathol. Appl. Neurobiol. 1991, 17, 223–230. [Google Scholar] [CrossRef]
- Banati, R.B.; Gehrmann, J.; Schubert, P.; Kreutzberg, G.W. Cytotoxicity of microglia. Glia 1993, 7, 111–118. [Google Scholar] [CrossRef]
- Lee, J.W.; Kim, L.E.; Shim, H.J.; Kim, E.K.; Hwang, W.C.; Min, D.S.; Yu, S.W. A translocator protein 18 kda ligand, ro5-4864, inhibits atp-induced nlrp3 inflammasome activation. Biochem. Biophys. Res. Commun. 2016, 474, 587–593. [Google Scholar] [CrossRef]
- Anholt, R.R.; Pedersen, P.L.; De Souza, E.B.; Snyder, S.H. The peripheral-type benzodiazepine receptor. Localization to the mitochondrial outer membrane. J. Biol. Chem. 1986, 261, 576–583. [Google Scholar] [PubMed]
- Yasin, N.; Veenman, L.; Singh, S.; Azrad, M.; Bode, J.; Vainshtein, A.; Caballero, B.; Marek, I.; Gavish, M. Classical and novel tspo ligands for the mitochondrial tspo can modulate nuclear gene expression: Implications for mitochondrial retrograde signaling. Int. J. Mol. Sci. 2017, 18. [Google Scholar] [CrossRef] [PubMed]
- Braestrup, C.; Squires, R.F. Specific benzodiazepine receptors in rat brain characterized by high-affinity (3h)diazepam binding. Proc. Natl. Acad. Sci. United. States. Am. 1977, 74, 3805–3809. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.K.; Guilarte, T.R. Translocator protein 18 kda (tspo): Molecular sensor of brain injury and repair. Pharm. Thera. 2008, 118, 1–17. [Google Scholar] [CrossRef]
- Gehlert, D.R.; Stephenson, D.T.; Schober, D.A.; Rash, K.; Clemens, J.A. Increased expression of peripheral benzodiazepine receptors in the facial nucleus following motor neuron axotomy. Neurochem. Int. 1997, 31, 705–713. [Google Scholar] [CrossRef]
- Banati, R.B.; Myers, R.; Kreutzberg, G.W. Pk (’peripheral benzodiazepine’)—Binding sites in the cns indicate early and discrete brain lesions: Microautoradiographic detection of [3h]pk 11195 binding to activated microglia. J. Neurocytol. 1997, 26, 77–82. [Google Scholar] [CrossRef]
- Ghadery, C.; Best, L.A.; Pavese, N.; Tai, Y.F.; Strafella, A.P. Pet evaluation of microglial activation in non-neurodegenerative brain diseases. Curr. Neurol. Neurosci. Rep. 2019, 19. [Google Scholar] [CrossRef]
- Best, L.; Ghadery, C.; Pavese, N.; Tai, Y.F.; Strafella, A.P. New and old tspo pet radioligands for imaging brain microglial activation in neurodegenerative disease. Curr. Neurol. Neurosci. Rep. 2019, 19. [Google Scholar] [CrossRef]
- Cumming, P.; Burgher, B.; Patkar, O.; Breakspear, M.; Vasdev, N.; Thomas, P.; Liu, G.J.; Banati, R. Sifting through the surfeit of neuroinflammation tracers. J. Cereb. Blood. Flow. Metab. 2018, 38, 204–224. [Google Scholar] [CrossRef]
- Mirzaei, N.; Tang, S.P.; Ashworth, S.; Coello, C.; Plisson, C.; Passchier, J.; Selvaraj, V.; Tyacke, R.J.; Nutt, D.J.; Sastre, M. In vivo imaging of microglial activation by positron emission tomography with [(11)c]pbr28 in the 5xfad model of alzheimer's disease. Glia 2016, 64, 993–1006. [Google Scholar]
- Ji, B.; Maeda, J.; Sawada, M.; Ono, M.; Okauchi, T.; Inaji, M.; Zhang, M.R.; Suzuki, K.; Ando, K.; Staufenbiel, M.; et al. Imaging of peripheral benzodiazepine receptor expression as biomarkers of detrimental versus beneficial glial responses in mouse models of alzheimer's and other cns pathologies. J. Neurosci. 2008, 28, 12255–12267. [Google Scholar] [CrossRef] [PubMed]
- Dupont, A.C.; Largeau, B.; Ribeiro, M.J.S.; Guilloteau, D.; Tronel, C.; Arlicot, N. Translocator protein-18 kda (tspo) positron emission tomography (pet) imaging and its clinical impact in neurodegenerative diseases. Int. J. Mol. 2017, 18. [Google Scholar] [CrossRef] [PubMed]
- Cagnin, A.; Brooks, D.J.; Kennedy, A.M.; Gunn, R.N.; Myers, R.; Turkheimer, F.E.; Jones, T.; Banati, R.B. In-vivo measurement of activated microglia in dementia. Lancet 2001, 358, 461–467. [Google Scholar] [CrossRef]
- Notter, T.; Coughlin, J.M.; Gschwind, T.; Weber-Stadlbauer, U.; Wang, Y.; Kassiou, M.; Vernon, A.C.; Benke, D.; Pomper, M.G.; Sawa, A.; et al. Translational evaluation of translocator protein as a marker of neuroinflammation in schizophrenia. Mol. Psychiatry 2018, 23, 323–334. [Google Scholar] [CrossRef]
- Barichello, T.; Simões, L.R.; Collodel, A.; Giridharan, V.V.; Dal-Pizzol, F.; Macedo, D.; Quevedo, J. The translocator protein (18 kda) and its role in neuropsychiatric disorders. Neurosci. Biobehav. Rev. 2017, 83, 183–199. [Google Scholar] [CrossRef]
- Guilarte, T.R. Tspo in diverse cns pathologies and psychiatric disease: A critical review and a way forward. Pharm. Thera. 2019, 194, 44–58. [Google Scholar] [CrossRef]
- Roncaroli, F.; Su, Z.; Herholz, K.; Gerhard, A.; Turkheimer, F.E. Tspo expression in brain tumours: Is tspo a target for brain tumour imaging? Clin. Transl. Imaging 2016, 4, 145–156. [Google Scholar] [CrossRef]
- Fan, J.; Campioli, E.; Midzak, A.; Culty, M.; Papadopoulos, V. Conditional steroidogenic cell-targeted deletion of tspo unveils a crucial role in viability and hormone-dependent steroid formation. Proc. Natl. Acad. Sci. USA 2015, 112, 7261–7266. [Google Scholar] [CrossRef]
- Costa, B.; Pozzo, E.D.; Martini, C. Translocator protein and steroidogenesis. Biochem. J. 2018, 475, 901–904. [Google Scholar] [CrossRef]
- Papadopoulos, V.; Baraldi, M.; Guilarte, T.R.; Knudsen, T.B.; Lacapere, J.J.; Lindemann, P.; Norenberg, M.D.; Nutt, D.; Weizman, A.; Zhang, M.R.; et al. Translocator protein (18kda): New nomenclature for the peripheral-type benzodiazepine receptor based on its structure and molecular function. Trends. Pharm. Sci. 2006, 27, 402–409. [Google Scholar] [CrossRef]
- Banati, R.B.; Middleton, R.J.; Chan, R.; Hatty, C.R.; Kam, W.W.; Quin, C.; Graeber, M.B.; Parmar, A.; Zahra, D.; Callaghan, P.; et al. Positron emission tomography and functional characterization of a complete pbr/tspo knockout. Nat. Commun. 2014, 5, 5452. [Google Scholar] [CrossRef] [PubMed]
- Middleton, R.J.; Liu, G.J.; Banati, R.B. Guwiyang wurra—’Fire mouse’: A global gene knockout model for tspo/pbr drug development, loss-of-function and mechanisms of compensation studies. Biochem. Soc. Trans. 2015, 43, 553–558. [Google Scholar] [CrossRef] [PubMed]
- Tu, L.N.; Morohaku, K.; Manna, P.R.; Pelton, S.H.; Butler, W.R.; Stocco, D.M.; Selvaraj, V. Peripheral benzodiazepine receptor/translocator protein global knock-out mice are viable with no effects on steroid hormone biosynthesis. J. Biol. Chem. 2014, 289, 27444–27454. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Zhai, K.; Xue, Y.; Yang, J.; Yang, Q.; Fu, Y.; Hu, Y.; Liu, F.; Wang, W.; Cui, L.; et al. Global deletion of tspo does not affect the viability and gene expression profile. PLoS ONE 2016, 11, e0167307. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.J.; Middleton, R.J.; Hatty, C.R.; Kam, W.W.; Chan, R.; Pham, T.; Harrison-Brown, M.; Dodson, E.; Veale, K.; Banati, R.B. The 18 kda translocator protein, microglia and neuroinflammation. Brain. Pathol. 2014, 24, 631–653. [Google Scholar] [CrossRef]
- Beurdeley-Thomas, A.; Miccoli, L.; Oudard, S.; Dutrillaux, B.; Poupon, M.F. The peripheral benzodiazepine receptors: A review. J. Neurooncol. 2000, 46, 45–56. [Google Scholar] [CrossRef]
- Gavish, M.; Bachman, I.; Shoukrun, R.; Katz, Y.; Veenman, L.; Weisinger, G.; Weizman, A. Enigma of the peripheral benzodiazepine receptor. Pharm. Rev. 1999, 51, 629–650. [Google Scholar]
- Anholt, R.R.H. Mitochondrial benzodiazepine receptors as potential modulators of intermediary metabolism. Trends. Pharm. Sci. 1986, 7, 506–511. [Google Scholar] [CrossRef]
- Hirsch, J.D.; Beyer, C.F.; Malkowitz, L.; Beer, B.; Blume, A.J. Mitochondrial benzodiazepine receptors mediate inhibition of mitochondrial respiratory control. Mol. Pharm. 1989, 35, 157–163. [Google Scholar]
- Larcher, J.C.; Vayssiere, J.L.; Le Marquer, F.J.; Cordeau, L.R.; Keane, P.E.; Bachy, A.; Gross, F.; Croizat, B.P. Effects of peripheral benzodiazepines upon the o2 consumption of neuroblastoma cells. Eur. J. Pharm. 1989, 161, 197–202. [Google Scholar] [CrossRef]
- Shiraishi, T.; Black, K.L.; Ikezaki, K.; Becker, D.P. Peripheral benzodiazepine induces morphological changes and proliferation of mitochondria in glioma cells. J. Neurosci. Res. 1991, 30, 463–474. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Papadopoulos, V. Peripheral-type benzodiazepine receptor function in cholesterol transport. Identification of a putative cholesterol recognition/interaction amino acid sequence and consensus pattern. Endocrinology 1998, 139, 4991–4997. [Google Scholar] [CrossRef] [PubMed]
- Jaipuria, G.; Leonov, A.; Giller, K.; Vasa, S.K.; Jaremko, Ł.; Jaremko, M.; Linser, R.; Becker, S.; Zweckstetter, M. Cholesterol-mediated allosteric regulation of the mitochondrial translocator protein structure. Nat. Commun. 2017, 8, 14893. [Google Scholar] [CrossRef]
- Da Pozzo, E.; Giacomelli, C.; Costa, B.; Cavallini, C.; Taliani, S.; Barresi, E.; Da Settimo, F.; Martini, C. Tspo piga ligands promote neurosteroidogenesis and human astrocyte well-being. Int. J. Mol. Sci. 2016, 17, 1028. [Google Scholar] [CrossRef] [PubMed]
- Morohaku, K.; Pelton, S.H.; Daugherty, D.J.; Butler, W.R.; Deng, W.; Selvaraj, V. Translocator protein/peripheral benzodiazepine receptor is not required for steroid hormone biosynthesis. Endocrinology 2014, 155, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.J.; Middleton, R.J.; Kam, W.W.; Chin, D.Y.; Hatty, C.R.; Chan, R.H.; Banati, R.B. Functional gains in energy and cell metabolism after tspo gene insertion. Cell. Cycle. 2017, 16, 436–447. [Google Scholar] [CrossRef]
- Milenkovic, V.M.; Slim, D.; Bader, S.; Koch, V.; Heinl, E.S.; Alvarez-Carbonell, D.; Nothdurfter, C.; Rupprecht, R.; Wetzel, C.H. Crispr-cas9 mediated tspo gene knockout alters respiration and cellular metabolism in human primary microglia cells. Int. J. Mol. 2019, 20. [Google Scholar] [CrossRef]
- Bader, S.; Wolf, L.; Milenkovic, V.M.; Gruber, M.; Nothdurfter, C.; Rupprecht, R.; Wetzel, C.H. Differential effects of tspo ligands on mitochondrial function in mouse microglia cells. Psychoneuroendocrinology 2019, 106, 65–76. [Google Scholar] [CrossRef]
- Fu, Y.; Wang, D.; Wang, H.; Cai, M.; Li, C.; Zhang, X.; Chen, H.; Hu, Y.; Zhang, X.; Ying, M.; et al. Tspo deficiency induces mitochondrial dysfunction, leading to hypoxia, angiogenesis and a growth-promoting metabolic shift towards glycolysis in glioblastoma. Neuro. Oncol. 2019. [Google Scholar] [CrossRef]
- Krestinina, O.V.; Grachev, D.E.; Odinokova, I.V.; Reiser, G.; Evtodienko, Y.V.; Azarashvili, T.S. Effect of peripheral benzodiazepine receptor (pbr/tspo) ligands on opening of ca2+-induced pore and phosphorylation of 3.5-kda polypeptide in rat brain mitochondria. Biochem. (Mosc. ) 2009, 74, 421–429. [Google Scholar] [CrossRef]
- Seneviratne, M.S.; Faccenda, D.; De Biase, V.; Campanella, M. Pk11195 inhibits mitophagy targeting the f1fo-atpsynthase in bcl-2 knock-down cells. Curr. Mol. Med. 2012, 12, 476–482. [Google Scholar] [PubMed]
- Jayakumar, A.R.; Panickar, K.S.; Norenberg, M.D. Effects on free radical generation by ligands of the peripheral benzodiazepine receptor in cultured neural cells. J. Neurochem. 2002, 83, 1226–1234. [Google Scholar] [CrossRef] [PubMed]
- Stoebner, P.E.; Carayon, P.; Casellas, P.; Portier, M.; Lavabre-Bertrand, T.; Cuq, P.; Cano, J.P.; Meynadier, J.; Meunier, L. Transient protection by peripheral benzodiazepine receptors during the early events of ultraviolet light-induced apoptosis. Cell. Death Differ. 2001, 8, 747–753. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lejri, I.; Grimm, A.; Halle, F.; Abarghaz, M.; Klein, C.; Maitre, M.; Schmitt, M.; Bourguignon, J.J.; Mensah-Nyagan, A.G.; Bihel, F.; et al. Tspo ligands boost mitochondrial function and pregnenolone synthesis. J. Alzheimer’s Dis. Jad. 2019. [Google Scholar] [CrossRef]
- Grimm, A.; Lejri, I.; Halle, F.; Schmitt, M.; Gotz, J.; Bihel, F.; Eckert, A. Mitochondria modulatory effects of new tspo ligands in a cellular model of tauopathies. J. Neuroendocr. 2019, e12796. [Google Scholar] [CrossRef]
- Kupa, L.V.K.; Drewes, C.C.; Barioni, E.D.; Neves, C.L.; Sampaio, S.C.; Farsky, S.H.P. Role of translocator 18 kda ligands in the activation of leukotriene b4 activated g-protein coupled receptor and toll like receptor-4 pathways in neutrophils. Front. Pharm. 2017, 8, 766. [Google Scholar] [CrossRef]
- Baez, E.; Guio-Vega, G.P.; Echeverria, V.; Sandoval-Rueda, D.A.; Barreto, G.E. 4′-chlorodiazepam protects mitochondria in t98g astrocyte cell line from glucose deprivation. Neurotox. Res. 2017, 32, 163–171. [Google Scholar] [CrossRef]
- Gatliff, J.; East, D.; Crosby, J.; Abeti, R.; Harvey, R.; Craigen, W.; Parker, P.; Campanella, M. Tspo interacts with vdac1 and triggers a ros-mediated inhibition of mitochondrial quality control. Autophagy 2014, 10, 2279–2296. [Google Scholar] [CrossRef]
- Sliter, D.A.; Martinez, J.; Hao, L.; Chen, X.; Sun, N.; Fischer, T.D.; Burman, J.L.; Li, Y.; Zhang, Z.; Narendra, D.P.; et al. Parkin and pink1 mitigate sting-induced inflammation. Nature 2018, 561, 258–262. [Google Scholar] [CrossRef]
- Guilarte, T.R.; Loth, M.K.; Guariglia, S.R. Tspo finds nox2 in microglia for redox homeostasis. Trends. Pharm. Sci. 2016, 37, 334–343. [Google Scholar] [CrossRef]
- Zeineh, N.; Nagler, R.; Gabay, M.; Weizman, A.; Gavish, M. Effects of cigarette smoke on tspo-related mitochondrial processes. Cells 2019, 8. [Google Scholar] [CrossRef] [PubMed]
- Zeno, S.; Zaaroor, M.; Leschiner, S.; Veenman, L.; Gavish, M. Cocl(2) induces apoptosis via the 18 kda translocator protein in u118mg human glioblastoma cells. Biochemistry 2009, 48, 4652–4661. [Google Scholar] [CrossRef] [PubMed]
- Shargorodsky, L.; Veenman, L.; Caballero, B.; Pe'er, Y.; Leschiner, S.; Bode, J.; Gavish, M. The nitric oxide donor sodium nitroprusside requires the 18 kda translocator protein to induce cell death. Apoptosis 2012, 17, 647–665. [Google Scholar] [CrossRef] [PubMed]
- Lin, R.; Angelin, A.; Da Settimo, F.; Martini, C.; Taliani, S.; Zhu, S.; Wallace, D.C. Genetic analysis of dtspo, an outer mitochondrial membrane protein, reveals its functions in apoptosis, longevity, and ab42-induced neurodegeneration. Aging Cell 2014, 13, 507–518. [Google Scholar] [CrossRef]
- Lin, R.; Rittenhouse, D.; Sweeney, K.; Potluri, P.; Wallace, D.C. Tspo, a mitochondrial outer membrane protein, controls ethanol-related behaviors in drosophila. PloS Genet. 2015, 11, e1005366. [Google Scholar] [CrossRef]
- Xiao, J.; Liang, D.; Zhang, H.; Liu, Y.; Li, F.; Chen, Y.H. 4′-chlorodiazepam, a translocator protein (18 kda) antagonist, improves cardiac functional recovery during postischemia reperfusion in rats. Exp. Biol. Med. (Maywood.) 2010, 235, 478–486. [Google Scholar] [CrossRef]
- Musman, J.; Paradis, S.; Panel, M.; Pons, S.; Barau, C.; Caccia, C.; Leoni, V.; Ghaleh, B.; Morin, D. A tspo ligand prevents mitochondrial sterol accumulation and dysfunction during myocardial ischemia-reperfusion in hypercholesterolemic rats. Biochem. Pharm. 2017, 142, 87–95. [Google Scholar] [CrossRef]
- Soustiel, J.F.; Vlodavsky, E.; Milman, F.; Gavish, M.; Zaaroor, M. Improvement of cerebral metabolism mediated by ro5-4864 is associated with relief of intracranial pressure and mitochondrial protective effect in experimental brain injury. Pharm. Res. 2011, 28, 2945–2953. [Google Scholar] [CrossRef]
- Chen, Y.; Veenman, L.; Singh, S.; Ouyang, F.; Liang, J.; Huang, W.; Marek, I.; Zeng, J.; Gavish, M. 2-cl-mgv-1 ameliorates apoptosis in the thalamus and hippocampus and cognitive deficits after cortical infarct in rats. Stroke 2017, 48, 3366–3374. [Google Scholar] [CrossRef]
- Cheng, Q.; Sun, G.J.; Liu, S.B.; Yang, Q.; Li, X.M.; Li, X.B.; Liu, G.; Zhao, J.N.; Zhao, M.G. A novel translocator protein 18 kda ligand, zbd-2, exerts neuroprotective effects against acute spinal cord injury. Clin. Exp. Pharm. Physiol. 2016, 43, 930–938. [Google Scholar] [CrossRef]
- Boche, D.; Perry, V.H.; Nicoll, J.A.R. Review: Activation patterns of microglia and their identification in the human brain. Neuropathol. Appl. Neurobiol. 2013, 39, 3–18. [Google Scholar] [CrossRef] [PubMed]
- Pozzo, E.D.; Tremolanti, C.; Costa, B.; Giacomelli, C.; Milenkovic, V.M.; Bader, S.; Wetzel, C.H.; Rupprecht, R.; Taliani, S.; Settimo, F.D.; et al. Microglial pro-inflammatory and anti-inflammatory phenotypes are modulated by translocator protein activation. Int. J. Mol. Sci. 2019, 20, 4467. [Google Scholar] [CrossRef] [PubMed]
- Beckers, L.; Ory, D.; Geric, I.; Declercq, L.; Koole, M.; Kassiou, M.; Bormans, G.; Baes, M. Increased expression of translocator protein (tspo) marks pro-inflammatory microglia but does not predict neurodegeneration. Mol. Imaging. Biol. 2018, 20, 94–102. [Google Scholar] [CrossRef] [PubMed]
- Pannell, M.; Economopoulos, V.; Wilson, T.C.; Kersemans, V.; Isenegger, P.G.; Larkin, J.R.; Smart, S.; Gilchrist, S.; Gouverneur, V.; Sibson, N.R. Imaging of translocator protein upregulation is selective for pro-inflammatory polarized astrocytes and microglia. Glia 2019. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.B.; Khoo, C.; Ryu, J.K.; van Breemen, E.; Kim, S.U.; McLarnon, J.G. Inhibition of lipopolysaccharide-induced cyclooxygenase-2, tumor necrosis factor-alpha and [ca2+]i responses in human microglia by the peripheral benzodiazepine receptor ligand pk11195. J. Neurochem. 2002, 83, 546–555. [Google Scholar] [CrossRef]
- Wilms, H.; Claasen, J.; Rohl, C.; Sievers, J.; Deuschl, G.; Lucius, R. Involvement of benzodiazepine receptors in neuroinflammatory and neurodegenerative diseases: Evidence from activated microglial cells in vitro. Neurobiol. Dis. 2003, 14, 417–424. [Google Scholar] [CrossRef]
- Lee, J.W.; Nam, H.; Yu, S.W. Systematic analysis of translocator protein 18 kda (tspo) ligands on toll-like receptors-mediated pro-inflammatory responses in microglia and astrocytes. Exp. Neurobiol. 2016, 25, 262–268. [Google Scholar] [CrossRef]
- Zhao, Y.Y.; Yu, J.Z.; Li, Q.Y.; Ma, C.G.; Lu, C.Z.; Xiao, B.G. Tspo-specific ligand vinpocetine exerts a neuroprotective effect by suppressing microglial inflammation. Neuron. Glia. Biol. 2011, 7, 187–197. [Google Scholar] [CrossRef]
- Azrad, M.; Zeineh, N.; Weizman, A.; Veenman, L.; Gavish, M. The tspo ligands 2-cl-mgv-1, mgv-1, and pk11195 differentially suppress the inflammatory response of bv-2 microglial cell to lps. Int. J. Mol. Sci. 2019, 20. [Google Scholar] [CrossRef]
- Monga, S.; Nagler, R.; Amara, R.; Weizman, A.; Gavish, M. Inhibitory effects of the two novel tspo ligands 2-cl-mgv-1 and mgv-1 on lps-induced microglial activation. Cells 2019, 8. [Google Scholar] [CrossRef]
- Choi, J.; Ifuku, M.; Noda, M.; Guilarte, T.R. Translocator protein (18 kda)/peripheral benzodiazepine receptor specific ligands induce microglia functions consistent with an activated state. Glia 2011, 59, 219–230. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Wang, X.; Zhao, L.; Ma, W.; Rodriguez, I.R.; Fariss, R.N.; Wong, W.T. Macroglia-microglia interactions via tspo signaling regulates microglial activation in the mouse retina. J. Neurosci. 2014, 34, 3793–3806. [Google Scholar] [CrossRef] [PubMed]
- Bonsack, F.t.; Alleyne, C.H., Jr.; Sukumari-Ramesh, S. Augmented expression of tspo after intracerebral hemorrhage: A role in inflammation? J. Neuroinflammation 2016, 13, 151. [Google Scholar] [CrossRef]
- Narayan, N.; Mandhair, H.; Smyth, E.; Dakin, S.G.; Kiriakidis, S.; Wells, L.; Owen, D.; Sabokbar, A.; Taylor, P. The macrophage marker translocator protein (tspo) is down-regulated on pro-inflammatory ’m1’ human macrophages. PLoS ONE 2017, 12, e0185767. [Google Scholar] [CrossRef] [PubMed]
- Owen, D.R.; Narayan, N.; Wells, L.; Healy, L.; Smyth, E.; Rabiner, E.A.; Galloway, D.; Williams, J.B.; Lehr, J.; Mandhair, H.; et al. Pro-inflammatory activation of primary microglia and macrophages increases 18 kda translocator protein expression in rodents but not humans. J. Cereb. Blood. Flow. Metab. 2017, 37, 2679–2690. [Google Scholar] [CrossRef] [PubMed]
- Batarseh, A.; Li, J.; Papadopoulos, V. Protein kinase c epsilon regulation of translocator protein (18 kda) tspo gene expression is mediated through a mapk pathway targeting stat3 and c-jun transcription factors. Biochemistry 2010, 49, 4766–4778. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Zamel, R.; Bai, X.H.; Liu, M. Pkc activation induces inflammatory response and cell death in human bronchial epithelial cells. PLoS ONE 2013, 8, e64182. [Google Scholar] [CrossRef] [PubMed]
- Kaminska, B. Mapk signalling pathways as molecular targets for anti-inflammatory therapy--from molecular mechanisms to therapeutic benefits. Biochim. Biophys. Acta 2005, 1754, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Gatliff, J.; Campanella, M. Tspo: Kaleidoscopic 18-kda amid biochemical pharmacology, control and targeting of mitochondria. Biochem. J. 2016, 473, 107–121. [Google Scholar] [CrossRef]
- Horiguchi, Y.; Ohta, N.; Yamamoto, S.; Koide, M.; Fujino, Y. Midazolam suppresses the lipopolysaccharide-stimulated immune responses of human macrophages via translocator protein signaling. Int. Immunopharmacol. 2019, 66, 373–382. [Google Scholar] [CrossRef]
- Zavala, F.; Taupin, V.; Descamps-Latscha, B. In vivo treatment with benzodiazepines inhibits murine phagocyte oxidative metabolism and production of interleukin 1, tumor necrosis factor and interleukin-6. J. Pharm. Exp. 1990, 255, 442–450. [Google Scholar]
- Ryu, J.K.; Choi, H.B.; McLarnon, J.G. Peripheral benzodiazepine receptor ligand pk11195 reduces microglial activation and neuronal death in quinolinic acid-injected rat striatum. Neurobiol. Dis. 2005, 20, 550–561. [Google Scholar] [CrossRef] [PubMed]
- Leaver, K.R.; Reynolds, A.; Bodard, S.; Guilloteau, D.; Chalon, S.; Kassiou, M. Effects of translocator protein (18 kda) ligands on microglial activation and neuronal death in the quinolinic-acid-injected rat striatum. ACS Chem. Neurosci. 2012, 3, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Ma, B.; Liu, X.; Huang, X.; Ji, Y.; Jin, T.; Ma, K. Translocator protein agonist ro5-4864 alleviates neuropathic pain and promotes remyelination in the sciatic nerve. Mol. Pain. 2018, 14, 1744806917748019. [Google Scholar] [CrossRef] [PubMed]
- Mills, C.; Makwana, M.; Wallace, A.; Benn, S.; Schmidt, H.; Tegeder, I.; Costigan, M.; Brown, R.H., Jr.; Raivich, G.; Woolf, C.J. Ro5-4864 promotes neonatal motor neuron survival and nerve regeneration in adult rats. Eur. J. Neurosci. 2008, 27, 937–946. [Google Scholar] [CrossRef] [PubMed]
- Girard, C.; Liu, S.; Cadepond, F.; Adams, D.; Lacroix, C.; Verleye, M.; Gillardin, J.M.; Baulieu, E.E.; Schumacher, M.; Schweizer-Groyer, G. Etifoxine improves peripheral nerve regeneration and functional recovery. Proc. Natl. Acad. Sci. USA 2008, 105, 20505–20510. [Google Scholar] [CrossRef] [PubMed]
- Simon-O'Brien, E.; Gauthier, D.; Riban, V.; Verleye, M. Etifoxine improves sensorimotor deficits and reduces glial activation, neuronal degeneration, and neuroinflammation in a rat model of traumatic brain injury. J. Neuroinflammation 2016, 13, 203. [Google Scholar] [CrossRef]
- Barron, A.M.; Garcia-Segura, L.M.; Caruso, D.; Jayaraman, A.; Lee, J.W.; Melcangi, R.C.; Pike, C.J. Ligand for translocator protein reverses pathology in a mouse model of alzheimer's disease. J. Neurosci. 2013, 33, 8891–8897. [Google Scholar] [CrossRef]
- Scholz, R.; Caramoy, A.; Bhuckory, M.B.; Rashid, K.; Chen, M.; Xu, H.; Grimm, C.; Langmann, T. Targeting translocator protein (18 kda) (tspo) dampens pro-inflammatory microglia reactivity in the retina and protects from degeneration. J. Neuroinflammation 2015, 12, 201. [Google Scholar] [CrossRef]
- Leva, G.; Klein, C.; Benyounes, J.; Halle, F.; Bihel, F.; Collongues, N.; De Seze, J.; Mensah-Nyagan, A.G.; Patte-Mensah, C. The translocator protein ligand xbd173 improves clinical symptoms and neuropathological markers in the sjl/j mouse model of multiple sclerosis. Biochim. Biophys. Acta Mol. Basis. Dis. 2017, 1863, 3016–3027. [Google Scholar] [CrossRef]
- Gong, J.; Szego, E.M.; Leonov, A.; Benito, E.; Becker, S.; Fischer, A.; Zweckstetter, M.; Outeiro, T.; Schneider, A. Translocator protein ligand protects against neurodegeneration in the mptp mouse model of parkinsonism. J. Neurosci. 2019, 39, 3752–3769. [Google Scholar] [CrossRef] [PubMed]
- Snell, C.R.; Snell, P.H. Benzodiazepines modulate the a2 adenosine binding sites on 108cc15 neuroblastoma x glioma hybrid cells. Br. J. Pharm. 1984, 83, 791–798. [Google Scholar] [CrossRef] [PubMed]
- File, S.E.; Pellow, S. Ro5-4864, a ligand for benzodiazepine micromolar and peripheral binding sites: Antagonism and enhancement of behavioural effects. Psychopharmacol. (Berl.) 1983, 80, 166–170. [Google Scholar] [CrossRef] [PubMed]
- Hatty, C.R.; Le Brun, A.P.; Lake, V.; Clifton, L.A.; Liu, G.J.; James, M.; Banati, R.B. Investigating the interactions of the 18kda translocator protein and its ligand pk11195 in planar lipid bilayers. Biochim. Biophys. Acta 2014, 1838, 1019–1030. [Google Scholar] [CrossRef] [PubMed]
- Hatty, C.R.; Banati, R.B. Protein-ligand and membrane-ligand interactions in pharmacology: The case of the translocator protein (tspo). Pharmacol. Res. 2015, 100, 58–63. [Google Scholar] [CrossRef]
- Costa, B.; Cavallini, C.; Da Pozzo, E.; Taliani, S.; Da Settimo, F.; Martini, C. The anxiolytic etifoxine binds to tspo ro5-4864 binding site with long residence time showing a high neurosteroidogenic activity. ACS Chem. Neurosci. 2017, 8, 1448–1454. [Google Scholar] [CrossRef]
- Yang, L.; Zhang, S.; Ling, X.; Shao, P.; Jia, N.; Bai, M. Multilayer photodynamic therapy for highly effective and safe cancer treatment. Acta Biomater. 2017, 54, 271–280. [Google Scholar] [CrossRef]
- Sun, X.; Guo, S.; Wang, W.; Cao, Z.; Dan, J.; Cheng, J.; Cao, W.; Tian, F.; Cao, W.; Tian, Y. Potential involvement of the 18 kda translocator protein and reactive oxygen species in apoptosis of thp-1 macrophages induced by sonodynamic therapy. PLoS ONE 2018, 13, e0196541. [Google Scholar] [CrossRef]
- Klee, K.; Storti, F.; Barben, M.; Samardzija, M.; Langmann, T.; Dunaief, J.; Grimm, C. Systemic knockout of tspo in mice does not affect retinal morphology, function and susceptibility to degeneration. Exp. Eye. Res. 2019, 188. [Google Scholar] [CrossRef]
- Svahn, A.J.; Becker, T.S.; Graeber, M.B. Emergent properties of microglia. Brain Pathol. 2014, 24, 665–670. [Google Scholar] [CrossRef]
- Notter, T.; Coughlin, J.M.; Sawa, A.; Meyer, U. Reconceptualization of translocator protein as a biomarker of neuroinflammation in psychiatry. Mol. Psychiatry 2018, 23, 36–47. [Google Scholar] [CrossRef] [PubMed]
- Betlazar, C.; Harrison-Brown, M.; Middleton, R.J.; Banati, R.; Liu, G.J. Cellular sources and regional variations in the expression of the neuroinflammatory marker translocator protein (tspo) in the normal brain. Int. J. Mol. 2018, 19. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Kim, N.; Park, S.; Jeon, Y.; Lee, J.; Yoo, S.J.; Lee, J.W.; Moon, C.; Yu, S.W.; Kim, E.K. Tanycytic tspo inhibition induces lipophagy to regulate lipid metabolism and improve energy balance. Autophagy 2019, 1–21. [Google Scholar] [CrossRef] [PubMed]
| Model | Treatment/Ligands (Concentration) | Outcome | Reference |
|---|---|---|---|
| In vitro | |||
| Mouse GL261 glioma cells | TSPO KO | ↑ mitochondrial fragmentation, fission proteins, ROS, glycolysis ↓ Complex I activity, MMP, global ATP production, basal and maximal mitochondrial respiratory capacity | Fu et al. (2019) |
| Human C20 microglia | TSPO KO | ↓ MMP, basal and maximal respiration, ATP-related oxygen consumption | Milenkovic et al. (2019) |
| Mouse primary microglia | TSPO KO | ↓ mitochondrial ATP production, basal oxygen consumption rate | Banati et al. (2014) |
| Mouse BV2 microglia | TSPO KD and scramble control cells LPS + Ro5-4864 (100 nM), PK11195 (100 nM), XBD173 (1 or 10 μM) | TSPO KD ↓ MMP, proliferation ↑ non-mitochondrial respiration, proton leak Control cells, Ro5-4864 and PK11195 ↑ basal respiration, ATP-related oxygen consumption ↓ spare respiratory capacity TSPO KD, control cells, Ro5-4864, PK11195 ↑ MMP TSPO KD, Ro5-4864 ↑ maximal respiration and proton leak TSPO KD, PK11195, XBD173 ↑ coupling efficiency | Bader et al. (2019) |
| Human U118MG cells | TSPO KD or Sodium nitroprusside + PK11195 (25 μM) | ↑ metabolic activity ↓ cell death, MMP collapse | Shargorodsky et al. (2012) |
| Human U118MG cells | TSPO KD or CoCl2 + PK11195 (25 μM) | ↓ apoptosis, MMP collapse, ROS | Zeno et al. (2009) |
| Mouse embryonic fibroblasts, canine mammary gland epithelia | TSPO KD or overexpression | TSPO KD ↑ ATP production, GSH, LC3B-II ↓ ROS TSPO overexpression ↑ ROS ↓ GSH | Gatliff et al. (2014) |
| HeLa cells | Bcl-2 KD + PK11195 (100 μM) | ↓ mitophagy, F1Fo-ATPsynthase | Seneviratne et al. (2012) |
| Mouse peritoneal macrophages | PK11195, Ro5-4864 (1 μM) | PK11195 ↓ basal ROS Ro5-4864 ↑ basal ROS | Kupa et al. (2017) |
| Mouse BV2 microglia | PK11195, Ro5-4864, PPIX (10 nM) | ↑ ROS | Jayakumar et al. (2002) |
| Rat C6 and Human T98G cells | PK11195, Ro5-4864 (10 nM) | ↑ number of mitochondria, dividing mitochondria | Shirashi et al. (1991) |
| Mouse C1300 neuroblastoma cells | PK11195, Ro5-4864 (1 fm – 1 μM) | ↓ oxygen consumption | Larcher et al. (1989) |
| Rat isolated liver, kidney, adrenal mitochondria | PK11195, Ro5-4864 (1 μM) | ↓ mitochondrial respiratory control ratio | Hirsch et al. (1988) |
| Human T98G cells | Glucose deprivation + Ro5-4864 (10 nM-10 μm) | ↑ cell viability, MMP preservation ↓ ROS | Baez et al. (2017) |
| Human SH-SY5Y neuroblastoma cells | Mutant Tau cells + imidazoquinazolinones compounds 2a and 2b (10 nM) | ↑ ATP levels, MMP | Grimm et al. (2019) |
| Human SH-SY5Y neuroblastoma cells | APP overexpression + imidazoquinazolinones compounds 2a and 2b (10 nM) | ↑ mitochondrial respiration ↓ ROS, oxidative injury, cell death, Aβ levels | Lejri et al. (2019) |
| Human Jurkat cells | TSPO transfection | ↑ mitochondrial ATP production, cell proliferation | Liu et al. (2017) |
| Human Jurkat cells | TSPO transfection + UV exposure | ↓ superoxide, caspase 3 activity, MMP ↑ apoptosis resistance | Stoebner et al. (2001) |
| In vivo | |||
| Drosophila Aβ-42 induced neurodegeneration | TSPO KO | ↓ radiation-induced apoptosis, mitochondrial respiration, OXPHOS enzyme activity ↑ H2O2 resistance | Lin et al. (2014) |
| Drosophila model of alcohol dependence | Conditional TSPO KO in neurons | ↑ ROS (males only) ↓ caspase 3/7 activity | Lin et al. (2015) |
| Rat hypercholesterolemic rats | Myocardial ischemia-reperfusion + Ro5-4864 (10 mg/kg) | ↑ calcium retention, respiratory control ratio | Musman et al. (2017) |
| Rat cortical trauma injury | Ro5-4864, (5 mg/kg, repeat) | ↓ mitochondrial ultrastructural damage, metabolic damage ↑ neurological recovery | Soustiel et al. (2011) |
| Rat postischemia reperfusion, heart tissue | Ro5-4864 (16 μmol/L, 32 μmol/L, 64 μmol/L | ↓ ROS, NADPH oxidase ↑ functional recovery, complex I and III activity | Xiao et al. (2010) |
| Rat cortical infarction | 2-CI-MGV (7.5 mg/kg, repeat) | ↑ MMP, cognitive impairments, neuronal survival ↓ cytochrome c, Iba1+ microglia | Chen et al. (2017) |
| Mouse spinal cord injury | ZBD-2 (10 mg/kg, repeat) | ↓ serum MDA, iNOS ↑ SOD, neuronal survival | Cheng et al. (2016) |
| Model | Treatment/Ligands (Concentration) | Outcome | Reference |
|---|---|---|---|
| In vitro | |||
| Human C20 microglia | TSPO KD or IL-1β/IL-1β+IFN-γ + PK11195, Ro5-4864, Etifoxine, XBD173 (all 100 nM) | IL-1β/IL-1β+IFN-γ ↑ TSPO mRNA Etifoxine, XBD173 ↓ IL-8 Ro5-4864, PK11195, Etifoxine, XBD173 ↑ IL-4 ↓ ROS TSPO KD ↑ IL-8 ↓ IL-4 | Da Pozzo et al. (2019) |
| Mouse RAW 264.7 macrophages | TSPO KD or Hemin activation + Ro5-4864 (5 and 10 μM) | Ro5-4864 ↓ TNF-α, IL-6 TSPO KD ↑ IL-6, TNF-α | Bonsack et al. (2016) |
| Mouse BV2 microglia | LPS + TSPO KD | ↑ ROS, TNF-α, proliferation rate | Wang et al. (2014) |
| Mouse BV2 microglia | LPS + TSPO KD/overexpression, PK11195, Ro5-4864 (0.1 or 10 μM) | LPS + TSPO overexpression/ligands ↑ M2 related genes ↓ NF-κB activity, IL-6, TNF-α LPS +TSPO KD ↑ IL-6, TNF-α, NO | Bae et al. (2014) |
| Mouse primary microglia and bone-marrow derived macrophages | LPS/IL-4 polarisation | LPS ↑ TSPO expression | Pannell et al. (2019) |
| Human monocyte-derived macrophages and microglia | LPS/IL-4/IL-13 | LPS ↓ TSPO mRNA, TSPO radioligand binding | Owen et al. (2017) |
| Mouse primary microglia | LPS/IL-4 polarisation | LPS ↑ TSPO mRNA | Beckers et al. (2018) |
| Human monocyte-derived macrophages | LPS/IFN-γ stimulation | ↓ TSPO mRNA | Narayan et al. (2017) |
| Mouse BV2 microglia | LPS + 2-MGV-1, MGV-1, PK11195 (25 μM) | ↓ COX2, iNOS, NO | Azrad et al. (2019) |
| Mouse BV2 microglia | LPS + 2-MGV-1, MGV-1 (25 μM) | ↓ IL-6, IL-1β, TNF-α, IFN-γ, ROS, NF-κB p65 activity | Monga et al. (2019) |
| Human THP-1 monocytes/macrophages, mouse primary bone marrow-derived macrophages | LPS + ATP + Ro5-4864 (50 μM) | ↓ NLRP3 inflammasome activation/assembly, caspase-1, IL-1β, IL-18, ROS, MMP depolarization | Lee et al. (2016b) |
| Mouse BV2 microglia | LPS or oxygen-glucose deprivation + Vinpocetine (20 and 50 μM) | ↓ microglial activation and proliferation, NO, IL-6, IL-1β, TNF-α, NF-κB, AP-1 | Zhao et al. (2011) |
| Human THP-1 macrophages | LPS + Midazolam (15 μM) | ↓ IL-6, NO, NF-κB, MAPK | Horiguchi et al. (2019) |
| Rat primary microglia | LPS + PK11195 (100 μM) | ↓ NO | Wilms et al. (2003) |
| Human primary microglia | LPS + PK11195 (1 μM or 50 μM) | ↓ COX2, TNF-α, calcium influx, microglial activation | Choi et al. (2002) |
| Rat primary microglia | PK11195, Ro5-4864 (1nm-100 nM) | ↑ phagocytosis, cell proliferation, ROS, NADPH oxidase, IL-1β, microglial activation | Choi et al. (2011) |
| Mouse primary microglia | TLR ligand activation + PK11195, Etifoxine (50 μM) | ↓ TNF-α, IL-6, CCL2 | Lee et al. (2016) |
| In vivo | |||
| Mouse 3xTg-AD Alzheimer’s Disease | Ro5-4864 (3 mg/kg, repeat) | ↓ Aβ plaques, Iba1+ microglia ↑ behaviour and cognition | Barron et al. (2013) |
| Mouse primary peritoneal macrophages | LPS + Ro5-4864 (1 mg/kg) | ↓ IL-1β, TNF-α, IL-6, oxidative metabolism | Zavala et al. (1990) |
| Rat excitotoxic Huntington’s Disease | Quinolinic acid + PK11195 (5 nM) | ↓ Iba1+ microglia, IL-1β, IL-6, TNF-α, iNOS, 4-HNE, 8-OHdG ↑ neuronal survival | Ryu et al. (2005) |
| Rat excitotoxic neurodegeneration | Quinolinic acid + DPA-713, DPA-714 and propargyl-DPA (5 nM) | ↓ OX-42+ microglia ↑ neuronal survival | Leaver et al. (2012) |
| Mouse MPTP Parkinson’s Disease | XBD173 (50 mg/kg, repeat) | ↑ neuronal survival, dopamine, motor function, IL-10 ↓ Iba1+ microglia, COX2, CXCL10 | Gong et al. (2019) |
| Mouse EAE model | XBD173 (10, 20, 30 mg/kg, repeat) | ↓ IL-6, TNF-α and IL-17, clinical EAE score ↑ MBP expression, motor function | Leva et al. (2017) |
| Mouse retinal degeneration | XBD173 (10 mg/kg, repeat) | ↓ Iba1+ microglia, IL-6, CCL2, retinal degeneration | Scholz et al. (2015) |
| Rat traumatic brain injury | Etifoxine (50 mg/kg, repeat) | ↑ behaviour and sensorimotor function ↓ CD68+ microglia, neuronal degeneration, IL-1α, IL-1β, IL-6, TNF-α, CCL2 | Simon O’Brien et al. (2016) |
| Rat sciatic nerve crush injury | Etifoxine (50 mg/kg, repeat) | ↑ myelination, neuronal survival, sensory and motor function ↓ macrophage activation (OX-42+), IL-6, TNF-α, IL-1β | Girard et al. (2008) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Betlazar, C.; Middleton, R.J.; Banati, R.; Liu, G.-J. The Translocator Protein (TSPO) in Mitochondrial Bioenergetics and Immune Processes. Cells 2020, 9, 512. https://doi.org/10.3390/cells9020512
Betlazar C, Middleton RJ, Banati R, Liu G-J. The Translocator Protein (TSPO) in Mitochondrial Bioenergetics and Immune Processes. Cells. 2020; 9(2):512. https://doi.org/10.3390/cells9020512
Chicago/Turabian StyleBetlazar, Calina, Ryan J. Middleton, Richard Banati, and Guo-Jun Liu. 2020. "The Translocator Protein (TSPO) in Mitochondrial Bioenergetics and Immune Processes" Cells 9, no. 2: 512. https://doi.org/10.3390/cells9020512
APA StyleBetlazar, C., Middleton, R. J., Banati, R., & Liu, G.-J. (2020). The Translocator Protein (TSPO) in Mitochondrial Bioenergetics and Immune Processes. Cells, 9(2), 512. https://doi.org/10.3390/cells9020512






