Photochemotherapy Induces Interferon Type III Expression via STING Pathway
Abstract
1. Introduction
1.1. Stimulator of Interferon Genes (STING) Pathway and Cancer
1.2. Interferon Signaling
1.3. Cutaneous T Cell Lymphoma (CTCL) as a Research Model
1.4. Treatment Modalities in CTCL
2. Materials and Methods
2.1. Cell Lines Used and Experimental Conditions
2.2. Small Interfering RNA (siRNA) Transfection
2.3. Photochemotherapy (8–MOP + UVA Treatment)
2.4. DNA-Damaging Agents
2.5. Viability Assessment
2.6. Real-Time PCR Analysis of Gene Expression
2.7. Micronuclei Detection
2.8. RNA-Seq Library Preparation and Sequencing
2.9. RNA-Seq Data Analysis
2.10. Statistical Analysis
3. Results
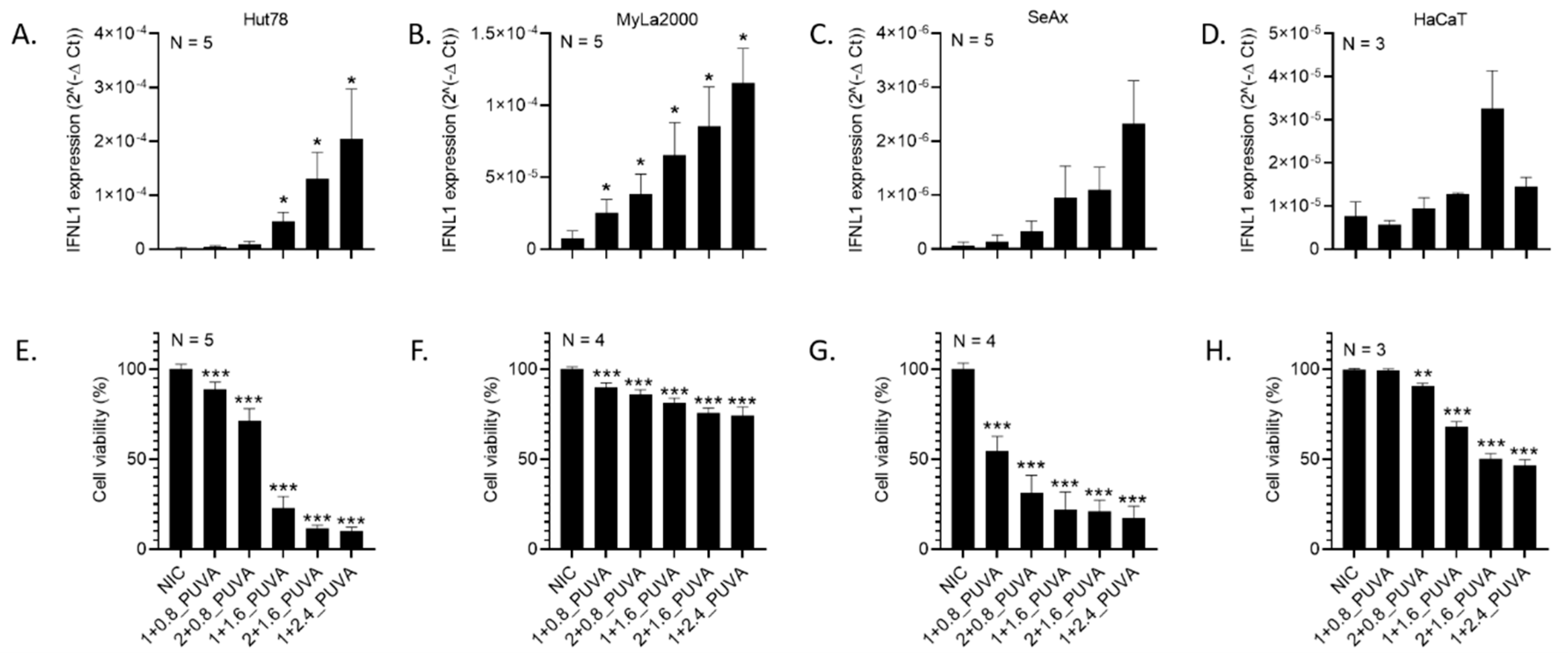
3.1. Photochemotherapy Induces Interferon Expression in CTCL Cells
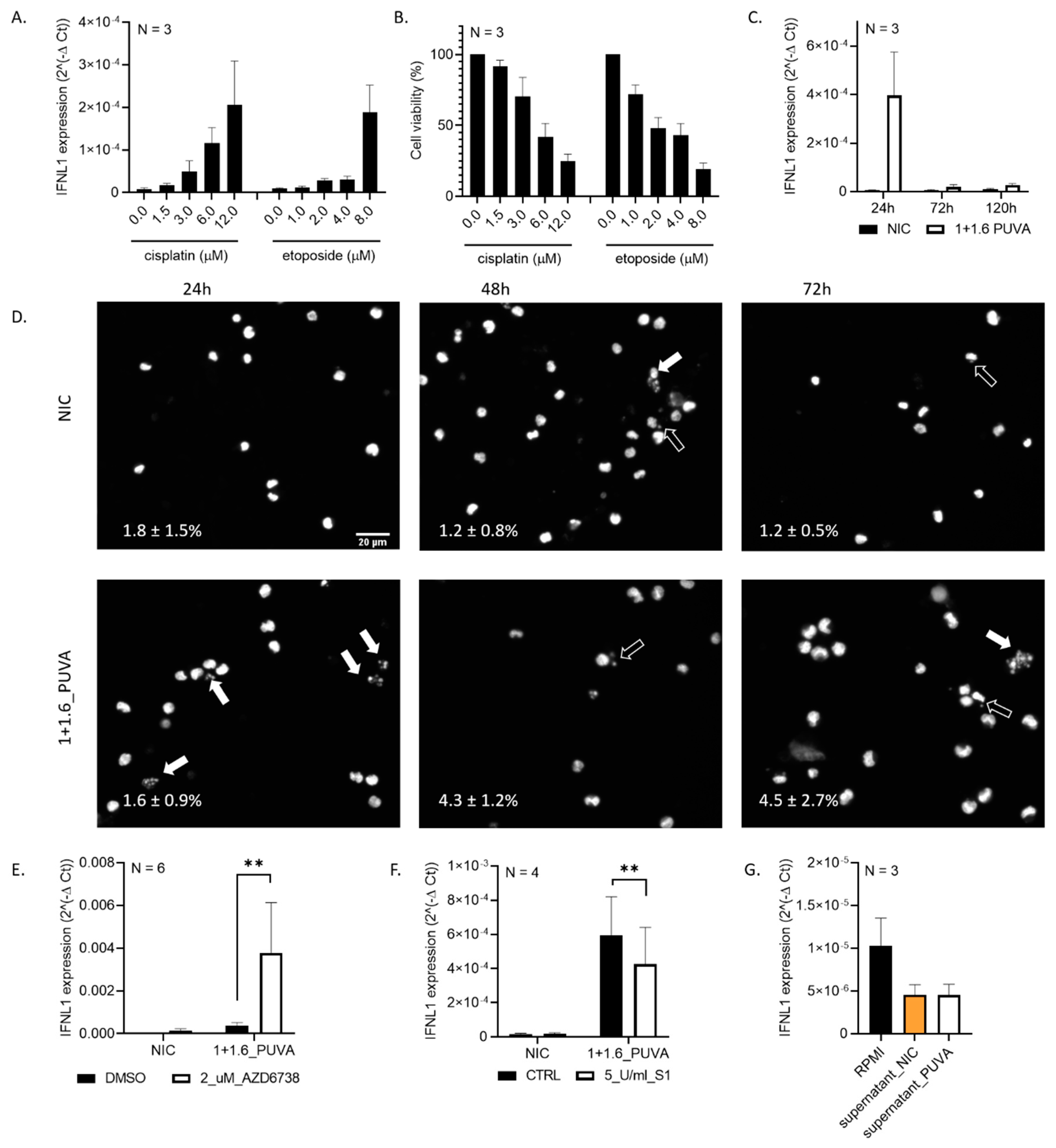
3.2. Expression of IFNL1 Is Related to DNA Damage
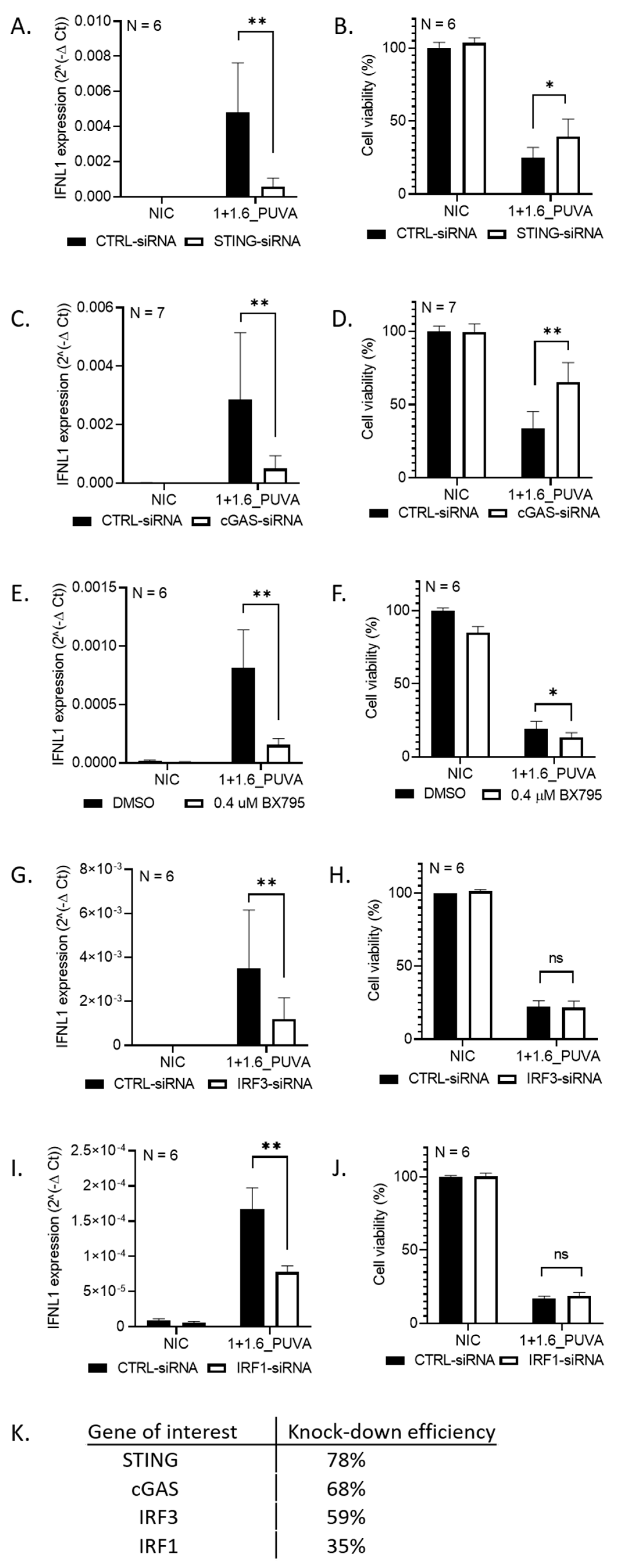
3.3. IFNL1 Activation Following DNA Damage Is STING-Dependent
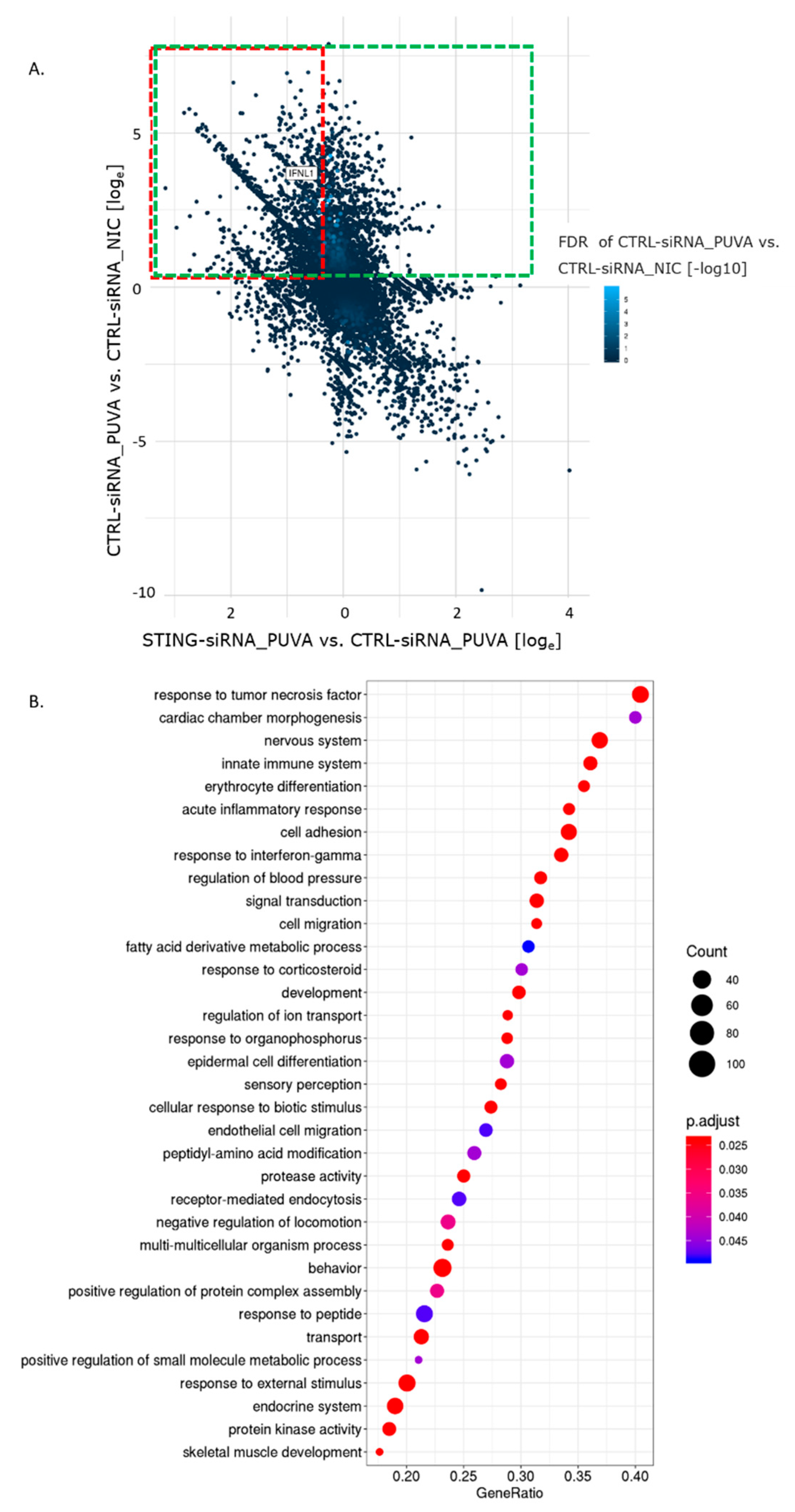
3.4. 8–MOP + UVA Treatment Elicits Changes in the Gene Expression Profile Partly Dependent on the STING Pathway
3.5. Pathways Deregulated by 8–MOP + UVA Treatment
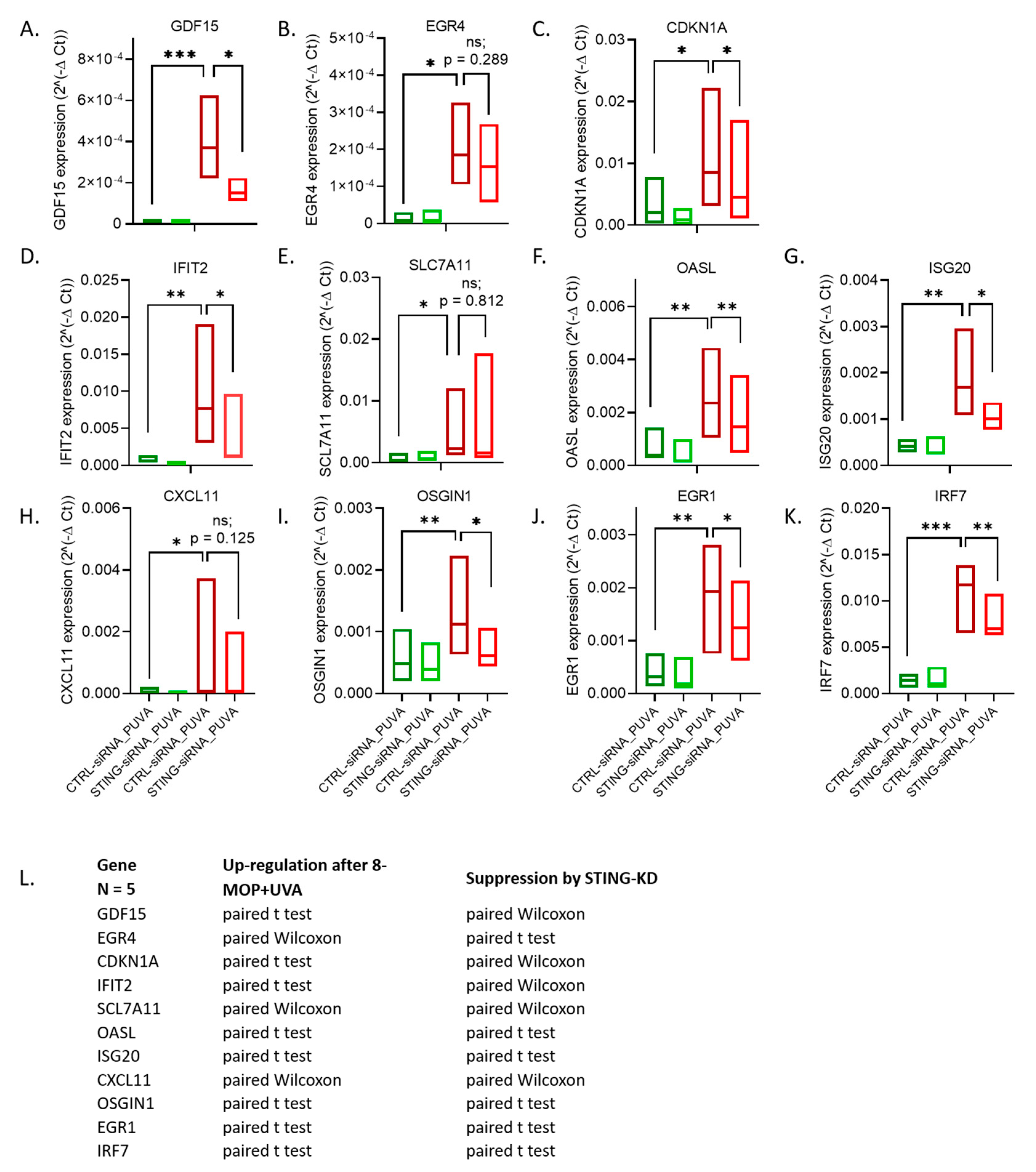
3.6. Hit Verification by RT-qPCR
4. Discussion
4.1. STING Pathway Activation in CTCL Cells
4.2. Immunomodulatory Effect of Photochemotherapy
5. Summary and Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bracci, L.; Schiavoni, G.; Sistigu, A.; Belardelli, F. Immune-based mechanisms of cytotoxic chemotherapy: Implications for the design of novel and rationale-based combined treatments against cancer. Cell Death Differ. 2014, 21, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Mitchison, T.J.; Pineda, J.; Shi, J.; Florian, S. Is inflammatory micronucleation the key to a successful anti-mitotic cancer drug? Open Biol. 2017, 7. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.J.; Fletcher, R.; Yu, J.; Zhang, L. Immunogenic effects of chemotherapy-induced tumor cell death. Genes Dis. 2018, 5, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Vatner, R.E.; Janssen, E.M. STING, DCs and the link between innate and adaptive tumor immunity. Mol. Immunol. 2019, 110, 13–23. [Google Scholar] [CrossRef]
- Yum, S.; Li, M.; Chen, Z.J. Old dogs, new trick: Classic cancer therapies activate cGAS. Cell Res. 2020, 30, 639–648. [Google Scholar] [CrossRef]
- Donnelly, R.P.; Kotenko, S.V. Interferon-lambda: A new addition to an old family. J. Interferon Cytokine Res. 2010, 30, 555–564. [Google Scholar] [CrossRef]
- Snell, L.M.; McGaha, T.L.; Brooks, D.G. Type I Interferon in Chronic Virus Infection and Cancer. Trends Immunol. 2017, 38, 542–557. [Google Scholar] [CrossRef]
- Zhou, Z.; Hamming, O.J.; Ank, N.; Paludan, S.R.; Nielsen, A.L.; Hartmann, R. Type III interferon (IFN) induces a type I IFN-like response in a restricted subset of cells through signaling pathways involving both the Jak-STAT pathway and the mitogen-activated protein kinases. J. Virol. 2007, 81, 7749–7758. [Google Scholar] [CrossRef]
- Hervas-Stubbs, S.; Perez-Gracia, J.L.; Rouzaut, A.; Sanmamed, M.F.; Le Bon, A.; Melero, I. Direct effects of type I interferons on cells of the immune system. Clin. Cancer Res. 2011, 17, 2619–2627. [Google Scholar] [CrossRef]
- Chen, J.; Markelc, B.; Kaeppler, J.; Ogundipe, V.M.L.; Cao, Y.; McKenna, W.G.; Muschel, R.J. STING-Dependent Interferon-lambda1 Induction in HT29 Cells, a Human Colorectal Cancer Cell Line, After Gamma-Radiation. Int. J. Radiat. Oncol. Biol. Phys. 2018, 101, 97–106. [Google Scholar] [CrossRef]
- Harding, S.M.; Benci, J.L.; Irianto, J.; Discher, D.E.; Minn, A.J.; Greenberg, R.A. Mitotic progression following DNA damage enables pattern recognition within micronuclei. Nature 2017, 548, 466–470. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.J.; Hess, S.; Richardson, S.K.; Newton, S.; Showe, L.C.; Benoit, B.M.; Ubriani, R.; Vittorio, C.C.; Junkins-Hopkins, J.M.; Wysocka, M.; et al. Immunopathogenesis and therapy of cutaneous T cell lymphoma. J. Clin. Investig. 2005, 115, 798–812. [Google Scholar] [CrossRef] [PubMed]
- Chung, C.G.; Poligone, B. Cutaneous T cell Lymphoma: An Update on Pathogenesis and Systemic Therapy. Curr. Hematol. Malig. Rep. 2015, 10, 468–476. [Google Scholar] [CrossRef] [PubMed]
- Geskin, L. ECP versus PUVA for the treatment of cutaneous T-cell lymphoma. Skin Therapy Lett. 2007, 12, 1–4. [Google Scholar] [PubMed]
- Scarisbrick, J. Extracorporeal photopheresis: What is it and when should it be used? Clin. Exp. Dermatol. 2009, 34, 757–760. [Google Scholar] [CrossRef] [PubMed]
- Spaccarelli, N.; Rook, A.H. The Use of Interferons in the Treatment of Cutaneous T-Cell Lymphoma. Dermatol. Clin. 2015, 33, 731–745. [Google Scholar] [CrossRef] [PubMed]
- Kaltoft, K.; Bisballe, S.; Dyrberg, T.; Boel, E.; Rasmussen, P.B.; Thestrup-Pedersen, K. Establishment of two continuous T-cell strains from a single plaque of a patient with mycosis fungoides. In Vitro Cell. Dev. Biol. 1992, 28A, 161–167. [Google Scholar] [CrossRef]
- Gootenberg, J.E.; Ruscetti, F.W.; Mier, J.W.; Gazdar, A.; Gallo, R.C. Human cutaneous T cell lymphoma and leukemia cell lines produce and respond to T cell growth factor. J. Exp. Med. 1981, 154, 1403–1418. [Google Scholar] [CrossRef]
- Kaltoft, K.; Bisballe, S.; Rasmussen, H.F.; Thestrup-Pedersen, K.; Thomsen, K.; Sterry, W. A continuous T-cell line from a patient with Sezary syndrome. Arch. Dermatol. Res. 1987, 279, 293–298. [Google Scholar] [CrossRef]
- Boukamp, P.; Petrussevska, R.T.; Breitkreutz, D.; Hornung, J.; Markham, A.; Fusenig, N.E. Normal keratinization in a spontaneously immortalized aneuploid human keratinocyte cell line. J. Cell Biol. 1988, 106, 761–771. [Google Scholar] [CrossRef]
- FastQC: A Quality Control Tool for High Throughput Sequence Data. Available online: http://www.bioinformatics.babraham.ac.uk/projects/fastqc (accessed on 9 November 2020).
- Wang, L.; Wang, S.; Li, W. RSeQC: Quality control of RNA-seq experiments. Bioinformatics 2012, 28, 2184–2185. [Google Scholar] [CrossRef] [PubMed]
- FastQ Screen Allows You to Screen a Library of Sequences in FastQ Format against a Set of Sequence Databases So You Can See If the Composition of the Library Matches with What You Expect. Available online: https://www.bioinformatics.babraham.ac.uk/projects/fastq_screen/ (accessed on 9 November 2020).
- Bolger, A.M.; Lohse, M.; Usadel, B. Trimmomatic: A flexible trimmer for Illumina sequence data. Bioinformatics 2014, 30, 2114–2120. [Google Scholar] [CrossRef] [PubMed]
- Dobin, A.; Davis, C.A.; Schlesinger, F.; Drenkow, J.; Zaleski, C.; Jha, S.; Batut, P.; Chaisson, M.; Gingeras, T.R. STAR: Ultrafast universal RNA-seq aligner. Bioinformatics 2012, 29, 15–21. [Google Scholar] [CrossRef] [PubMed]
- A Set of Command Line Tools (in Java) for Manipulating High-throughput Sequencing (HTS) Data and Formats Such as SAM/BAM/CRAM and VCF. Available online: http://broadinstitute.github.io/picard/ (accessed on 9 November 2020).
- Liao, Y.; Smyth, G.K.; Shi, W. The R package Rsubread is easier, faster, cheaper and better for alignment and quantification of RNA sequencing reads. Nucleic Acids Res. 2019, 47, e47. [Google Scholar] [CrossRef]
- Robinson, M.D.; McCarthy, D.J.; Smyth, G.K. edgeR: A Bioconductor package for differential expression analysis of digital gene expression data. Bioinformatics 2009, 26, 139–140. [Google Scholar] [CrossRef]
- Yu, G.; Wang, L.G.; Han, Y.; He, Q.Y. clusterProfiler: An R package for comparing biological themes among gene clusters. OMICS 2012, 16, 284–287. [Google Scholar] [CrossRef]
- Yu, G.; Wang, L.-G.; Yan, G.-R.; He, Q.-Y. DOSE: An R/Bioconductor package for disease ontology semantic and enrichment analysis. Bioinformatics 2014, 31, 608–609. [Google Scholar] [CrossRef]
- Almine, J.F.; O′Hare, C.A.; Dunphy, G.; Haga, I.R.; Naik, R.J.; Atrih, A.; Connolly, D.J.; Taylor, J.; Kelsall, I.R.; Bowie, A.G.; et al. IFI16 and cGAS cooperate in the activation of STING during DNA sensing in human keratinocytes. Nat. Commun. 2017, 8, 14392. [Google Scholar] [CrossRef]
- Derheimer, F.A.; Hicks, J.K.; Paulsen, M.T.; Canman, C.E.; Ljungman, M. Psoralen-induced DNA interstrand cross-links block transcription and induce p53 in an ataxia-telangiectasia and rad3-related-dependent manner. Mol. Pharmacol. 2009, 75, 599–607. [Google Scholar] [CrossRef]
- Wu, Q.; Vasquez, K.M. Human MLH1 protein participates in genomic damage checkpoint signaling in response to DNA interstrand crosslinks, while MSH2 functions in DNA repair. PLoS Genet. 2008, 4, e1000189. [Google Scholar] [CrossRef]
- Biskup, E.; Naym, D.G.; Gniadecki, R. Small-molecule inhibitors of Ataxia Telangiectasia and Rad3 related kinase (ATR) sensitize lymphoma cells to UVA radiation. J. Dermatol. Sci. 2016, 84, 239–247. [Google Scholar] [CrossRef] [PubMed]
- Erdal, E.; Haider, S.; Rehwinkel, J.; Harris, A.L.; McHugh, P.J. A prosurvival DNA damage-induced cytoplasmic interferon response is mediated by end resection factors and is limited by Trex1. Genes Dev. 2017, 31, 353–369. [Google Scholar] [CrossRef] [PubMed]
- Hartlova, A.; Erttmann, S.F.; Raffi, F.A.; Schmalz, A.M.; Resch, U.; Anugula, S.; Lienenklaus, S.; Nilsson, L.M.; Kroger, A.; Nilsson, J.A.; et al. DNA damage primes the type I interferon system via the cytosolic DNA sensor STING to promote anti-microbial innate immunity. Immunity 2015, 42, 332–343. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.J.; Le Bert, N.; Chitre, A.A.; Koo, C.X.; Nga, X.H.; Ho, S.S.; Khatoo, M.; Tan, N.Y.; Ishii, K.J.; Gasser, S. Genome-derived cytosolic DNA mediates type I interferon-dependent rejection of B cell lymphoma cells. Cell Rep. 2015, 11, 460–473. [Google Scholar] [CrossRef]
- Dickey, J.S.; Baird, B.J.; Redon, C.E.; Avdoshina, V.; Palchik, G.; Wu, J.; Kondratyev, A.; Bonner, W.M.; Martin, O.A. Susceptibility to bystander DNA damage is influenced by replication and transcriptional activity. Nucleic Acids Res. 2012, 40, 10274–10286. [Google Scholar] [CrossRef]
- Salton, S.R.; Ferri, G.L.; Hahm, S.; Snyder, S.E.; Wilson, A.J.; Possenti, R.; Levi, A. VGF: A novel role for this neuronal and neuroendocrine polypeptide in the regulation of energy balance. Front. Neuroendocrinol. 2000, 21, 199–219. [Google Scholar] [CrossRef]
- Honda, K.; Yanai, H.; Negishi, H.; Asagiri, M.; Sato, M.; Mizutani, T.; Shimada, N.; Ohba, Y.; Takaoka, A.; Yoshida, N.; et al. IRF-7 is the master regulator of type-I interferon-dependent immune responses. Nature 2005, 434, 772–777. [Google Scholar] [CrossRef]
- Emmerson, P.J.; Duffin, K.L.; Chintharlapalli, S.; Wu, X. GDF15 and Growth Control. Front. Physiol. 2018, 9, 1712. [Google Scholar] [CrossRef]
- Mookerjee-Basu, J.; Hooper, R.; Gross, S.; Schultz, B.; Go, C.K.; Samakai, E.; Ladner, J.; Nicolas, E.; Tian, Y.; Zhou, B.; et al. Suppression of Ca(2+) signals by EGR4 controls Th1 differentiation and anti-cancer immunity in vivo. EMBO Rep. 2020, 21, e48904. [Google Scholar] [CrossRef]
- Dutto, I.; Tillhon, M.; Cazzalini, O.; Stivala, L.A.; Prosperi, E. Biology of the cell cycle inhibitor p21(CDKN1A): Molecular mechanisms and relevance in chemical toxicology. Arch. Toxicol. 2015, 89, 155–178. [Google Scholar] [CrossRef]
- Reich, N.C. A death-promoting role for ISG54/IFIT2. J. Interferon Cytokine Res. 2013, 33, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Linher-Melville, K.; Singh, G. The complex roles of STAT3 and STAT5 in maintaining redox balance: Lessons from STAT-mediated xCT expression in cancer cells. Mol. Cell Endocrinol. 2017, 451, 40–52. [Google Scholar] [CrossRef] [PubMed]
- Leisching, G.; Wiid, I.; Baker, B. The Association of OASL and Type I Interferons in the Pathogenesis and Survival of Intracellular Replicating Bacterial Species. Front. Cell Infect. Microbiol. 2017, 7, 196. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Z.; Wang, L.; Pan, J. Interferon-stimulated gene 20-kDa protein (ISG20) in infection and disease: Review and outlook. Intractable Rare Dis. Res. 2017, 6, 35–40. [Google Scholar] [CrossRef]
- Tokunaga, R.; Zhang, W.; Naseem, M.; Puccini, A.; Berger, M.D.; Soni, S.; McSkane, M.; Baba, H.; Lenz, H.J. CXCL9, CXCL10, CXCL11/CXCR3 axis for immune activation—A target for novel cancer therapy. Cancer Treat. Rev. 2018, 63, 40–47. [Google Scholar] [CrossRef]
- Yao, H.; Li, P.; Venters, B.J.; Zheng, S.; Thompson, P.R.; Pugh, B.F.; Wang, Y. Histone Arg modifications and p53 regulate the expression of OKL38, a mediator of apoptosis. J. Biol. Chem. 2008, 283, 20060–20068. [Google Scholar] [CrossRef]
- Dai, L.; Cao, Y.; Chen, Y.; Kaleeba, J.A.; Zabaleta, J.; Qin, Z. Genomic analysis of xCT-mediated regulatory network: Identification of novel targets against AIDS-associated lymphoma. Oncotarget 2015, 6, 12710–12722. [Google Scholar] [CrossRef]
- Baron, V.; Adamson, E.D.; Calogero, A.; Ragona, G.; Mercola, D. The transcription factor Egr1 is a direct regulator of multiple tumor suppressors including TGFbeta1, PTEN, p53, and fibronectin. Cancer Gene Ther. 2006, 13, 115–124. [Google Scholar] [CrossRef]
- Sistigu, A.; Yamazaki, T.; Vacchelli, E.; Chaba, K.; Enot, D.P.; Adam, J.; Vitale, I.; Goubar, A.; Baracco, E.E.; Remedios, C.; et al. Cancer cell-autonomous contribution of type I interferon signaling to the efficacy of chemotherapy. Nat. Med. 2014, 20, 1301–1309. [Google Scholar] [CrossRef]
- Corrales, L.; Glickman, L.H.; McWhirter, S.M.; Kanne, D.B.; Sivick, K.E.; Katibah, G.E.; Woo, S.R.; Lemmens, E.; Banda, T.; Leong, J.J.; et al. Direct Activation of STING in the Tumor Microenvironment Leads to Potent and Systemic Tumor Regression and Immunity. Cell Rep. 2015, 11, 1018–1030. [Google Scholar] [CrossRef]
- Tatsuno, K.; Yamazaki, T.; Hanlon, D.; Han, P.; Robinson, E.; Sobolev, O.; Yurter, A.; Rivera-Molina, F.; Arshad, N.; Edelson, R.L.; et al. Extracorporeal photochemotherapy induces bona fide immunogenic cell death. Cell Death Dis. 2019, 10, 578. [Google Scholar] [CrossRef] [PubMed]
- Hodge, J.W.; Garnett, C.T.; Farsaci, B.; Palena, C.; Tsang, K.Y.; Ferrone, S.; Gameiro, S.R. Chemotherapy-induced immunogenic modulation of tumor cells enhances killing by cytotoxic T lymphocytes and is distinct from immunogenic cell death. Int. J. Cancer 2013, 133, 624–636. [Google Scholar] [CrossRef]
- Edelson, R.L. Cutaneous T cell lymphoma: The helping hand of dendritic cells. Ann. N. Y. Acad. Sci. 2001, 941, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Vieyra-Garcia, P.A.; Wolf, P. From Early Immunomodulatory Triggers to Immunosuppressive Outcome: Therapeutic Implications of the Complex Interplay Between the Wavebands of Sunlight and the Skin. Front. Med. 2018, 5, 232. [Google Scholar] [CrossRef] [PubMed]
- Lasfar, A.; Abushahba, W.; Balan, M.; Cohen-Solal, K.A. Interferon lambda: A new sword in cancer immunotherapy. Clin. Dev. Immunol. 2011, 2011, 349575. [Google Scholar] [CrossRef] [PubMed]
- Reislander, T.; Lombardi, E.P.; Groelly, F.J.; Miar, A.; Porru, M.; Di Vito, S.; Wright, B.; Lockstone, H.; Biroccio, A.; Harris, A.; et al. BRCA2 abrogation triggers innate immune responses potentiated by treatment with PARP inhibitors. Nat. Commun. 2019, 10, 3143. [Google Scholar] [CrossRef]

| IFNA1 | IFNA2 | IFNB1 | IFNG | IFNL1 | |
|---|---|---|---|---|---|
| Hut78 | n.d. | n.d. | n.d. | (traces) | +++ |
| MyLa2000 | n.d. | n.d. | + | +++ | +++ |
| SeAx | n.d. | n.d. | +++ | ++ | +++ |
| HaCaT | + | n.d. | +++ | n.d. | + |
| Gene Candidate | Biological Role |
|---|---|
| GDF15 | Growth/differentiation factor 15 (GDF15), belongs to the transforming growth factor β (TGF–β) superfamily; stress-induced, released in response to chemical or mechanical tissue injury [41] |
| EGR4 | early growth response–4 (EGR4); zinc-finger transcription factor; a key regulator of T-cell differentiation and function; upregulated upon T-cell receptor (TCR) engagement, serves as a critical “brake” on T-cell activation [42] |
| CDKN1A | cyclin-dependent kinase inhibitor 1 (CDKN1A) regulates cell cycle progression by inhibiting cyclin dependent kinase 1 (CDK1) and CDK2 in e.g., response to genotoxic stress; facilitates cell entry into quiescence and senescence; acts to limit proliferation of stem cells; involved in the regulation of transcription, apoptosis, DNA repair, as well as cell motility [43] |
| IFIT2 | IFN-induced gene with tetratricopeptide repeats 2 (IFIT2) syn. ISG54; one of cellular binding partners of STING; expressed in response to viral infections upon type I or III IFN; expression promotes apoptosis via a mitochondrial pathway [44] |
| SLC7A11 | Solute Carrier Family 7 Member 11 (SLC7A11), syn. xCT; a subunit of an amino acid antiporter system, contributing to redox balance; its promoter contains sites recognized by STAT3 and STAT5 [45] |
| OASL | Oligoadenylate Synthetase-Like (OASL); IFN-induced; during infection with RNA viruses: binds to retinoic acid-inducible gene I (RIG–I) sensor sensitizing its activation and enhances antiviral signaling; during infection with DNA viruses: deactivates cGAS inhibiting IFN production [46] |
| ISG20 | interferon-stimulated exonuclease gene 20 (ISG20); RNA exonuclease, induced by exposure to both type I (IFNA and IFNB) and type II (IFNG) IFNs; plays a role in mediating interferon’s antiviral activities [47] |
| CXCL11 | C-X-C motif chemokine 11 (CXCL11) is a chemokine induced by IFNG and IFNB, and weakly by IFNA. One of three ligands of CXCR3, a receptor expressed i.a. on naïve T cells and upregulated by antigen presenting dendritic cells, resulting in Th1 polarization. CXCL11/CXCR3 interaction plays a role in immune cell activation, differentiation and migration, as well as in tumor suppression [48] |
| OSGIN1 | Oxidative Stress Induced Growth Inhibitor 1 (OSGIN1) syn. OKL38 is a tumor suppressor, induced by DNA Damage in a p53-dependent Manner and regulated by histone Arg modifications [49]. It has been reported to be negatively regulated by xCT/SCL7A11 [50] |
| EGR1 | early growth response–1 (EGR1) zinc-finger transcription factor; directly induces transcription of, i.e., TGFβ1, phosphatase and tensin homolog (PTEN), p53, fibronectin [51] |
| IRF7 | Interferon regulatory factor 7 (IRF7); transcription factor essential for the induction of IFN–a/b genes [40] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Biskup, E.; Larsen, B.D.; Rib, L.; Folkersen, L.; Niazi, O.; Kamstrup, M.R.; Sørensen, C.S. Photochemotherapy Induces Interferon Type III Expression via STING Pathway. Cells 2020, 9, 2452. https://doi.org/10.3390/cells9112452
Biskup E, Larsen BD, Rib L, Folkersen L, Niazi O, Kamstrup MR, Sørensen CS. Photochemotherapy Induces Interferon Type III Expression via STING Pathway. Cells. 2020; 9(11):2452. https://doi.org/10.3390/cells9112452
Chicago/Turabian StyleBiskup, Edyta, Brian Daniel Larsen, Leonor Rib, Lasse Folkersen, Omid Niazi, Maria R. Kamstrup, and Claus Storgaard Sørensen. 2020. "Photochemotherapy Induces Interferon Type III Expression via STING Pathway" Cells 9, no. 11: 2452. https://doi.org/10.3390/cells9112452
APA StyleBiskup, E., Larsen, B. D., Rib, L., Folkersen, L., Niazi, O., Kamstrup, M. R., & Sørensen, C. S. (2020). Photochemotherapy Induces Interferon Type III Expression via STING Pathway. Cells, 9(11), 2452. https://doi.org/10.3390/cells9112452






