Hyaluronic Acid Injection Laryngoplasty for Unilateral Vocal Fold Paralysis—A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Search Strategy
2.4. Data Extraction and Study Items
2.5. Assessment of Reporting Quality and Risk of Bias
2.6. Data Synthesis and Meta-Analysis
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.3. Pre-Injection and Post-Injection Glottal Function Evaluations
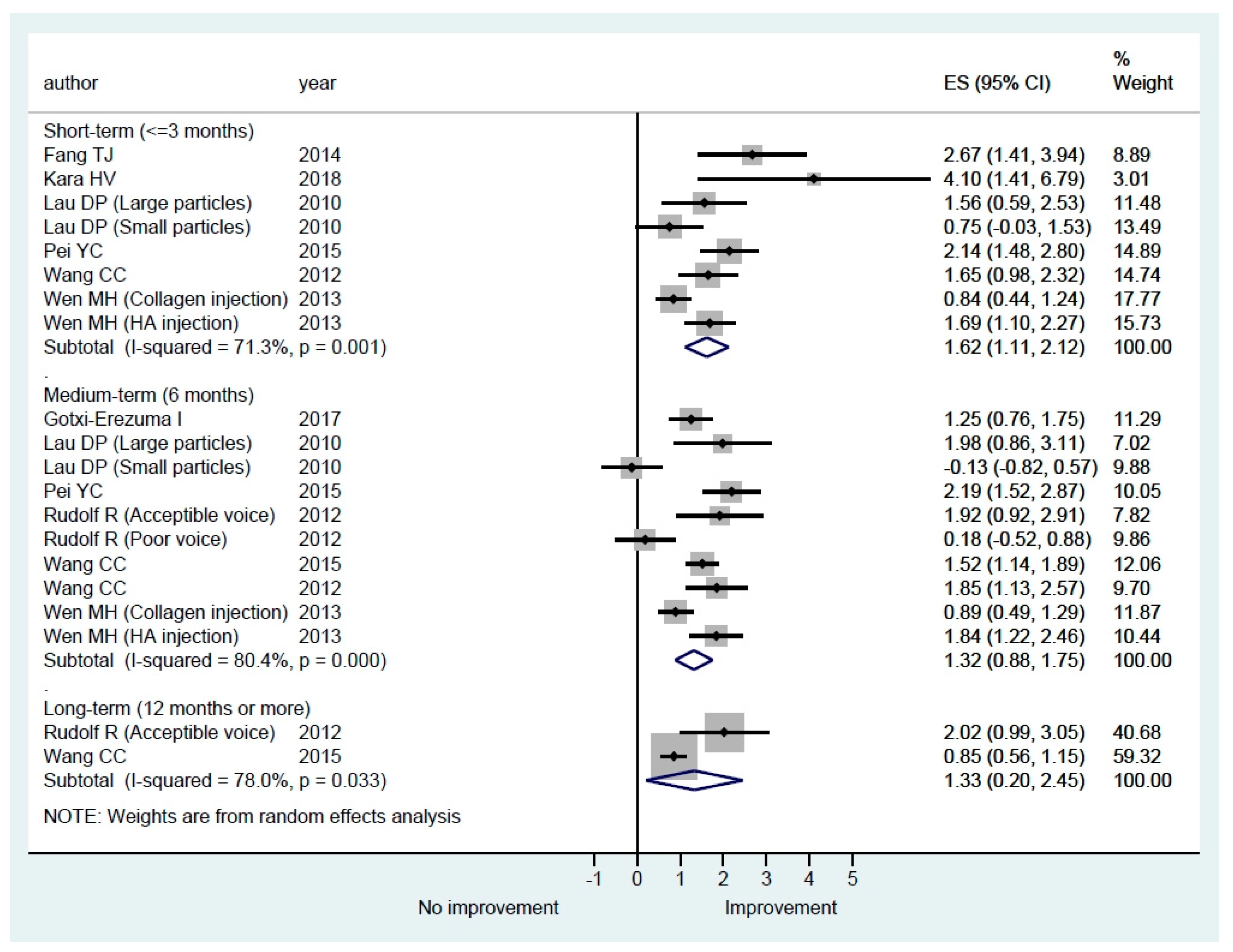
3.3.1. Quality of Life Questionnaires
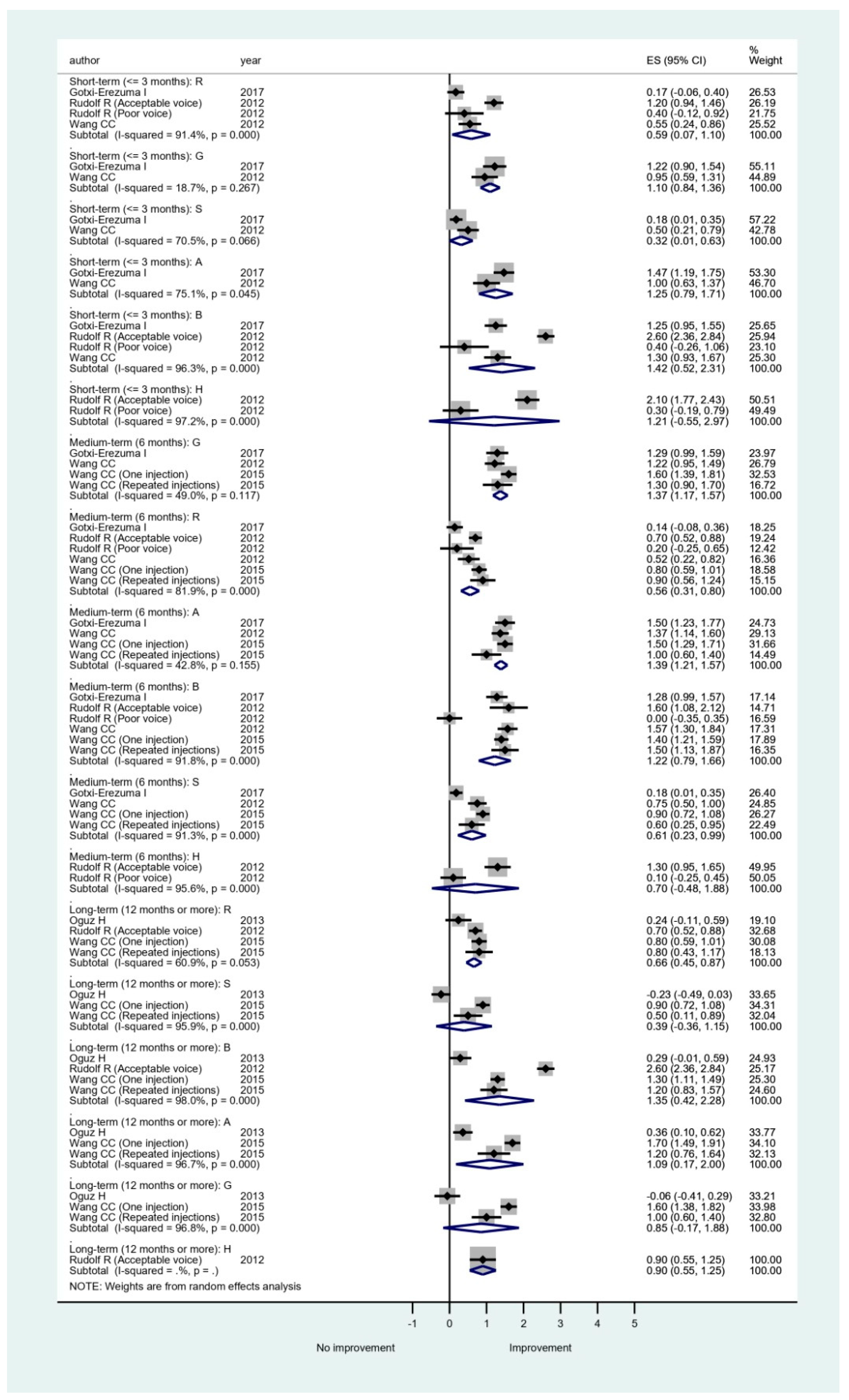
3.3.2. Perceptual Evaluation Grading Systems
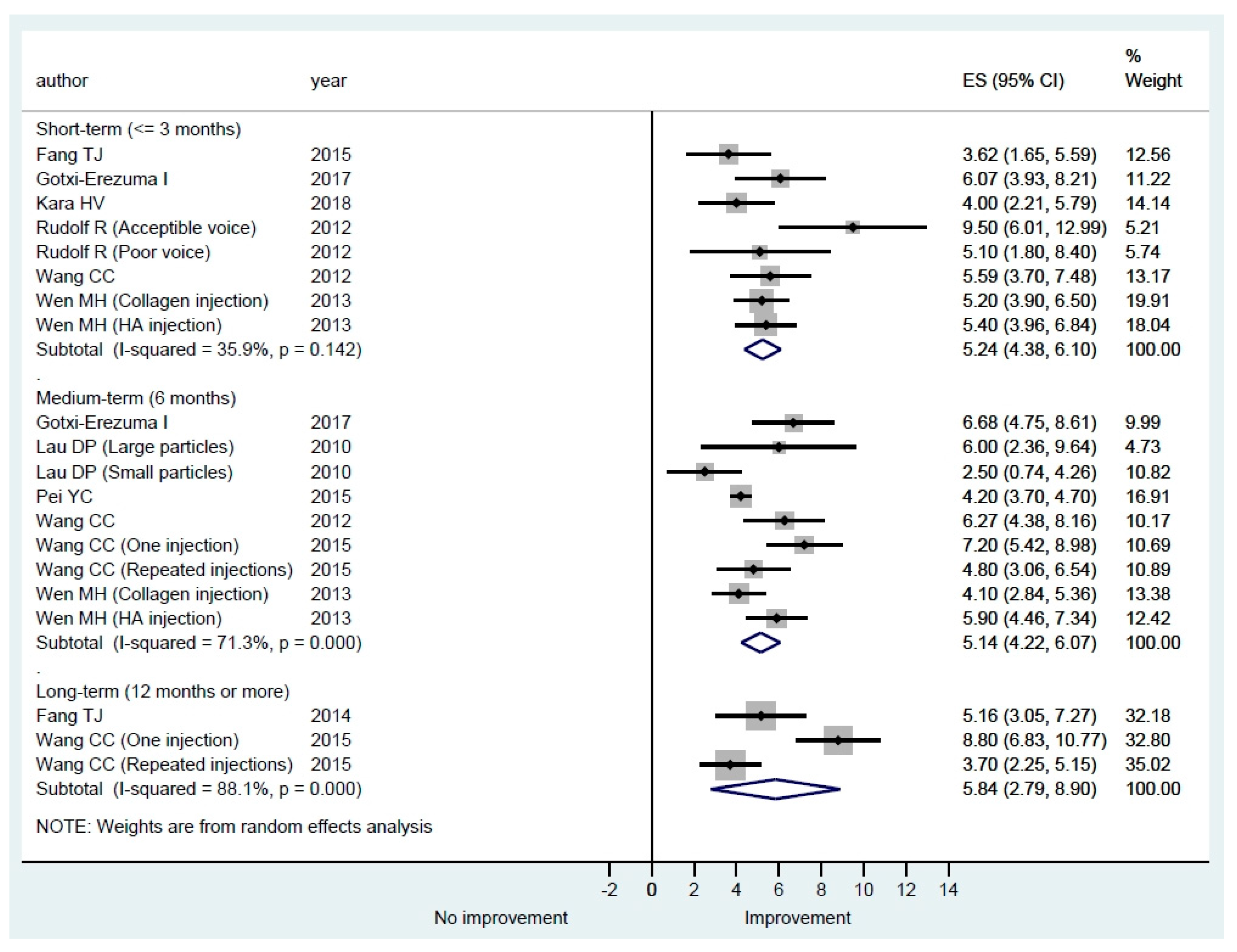
3.3.3. Voice Laboratory Recording
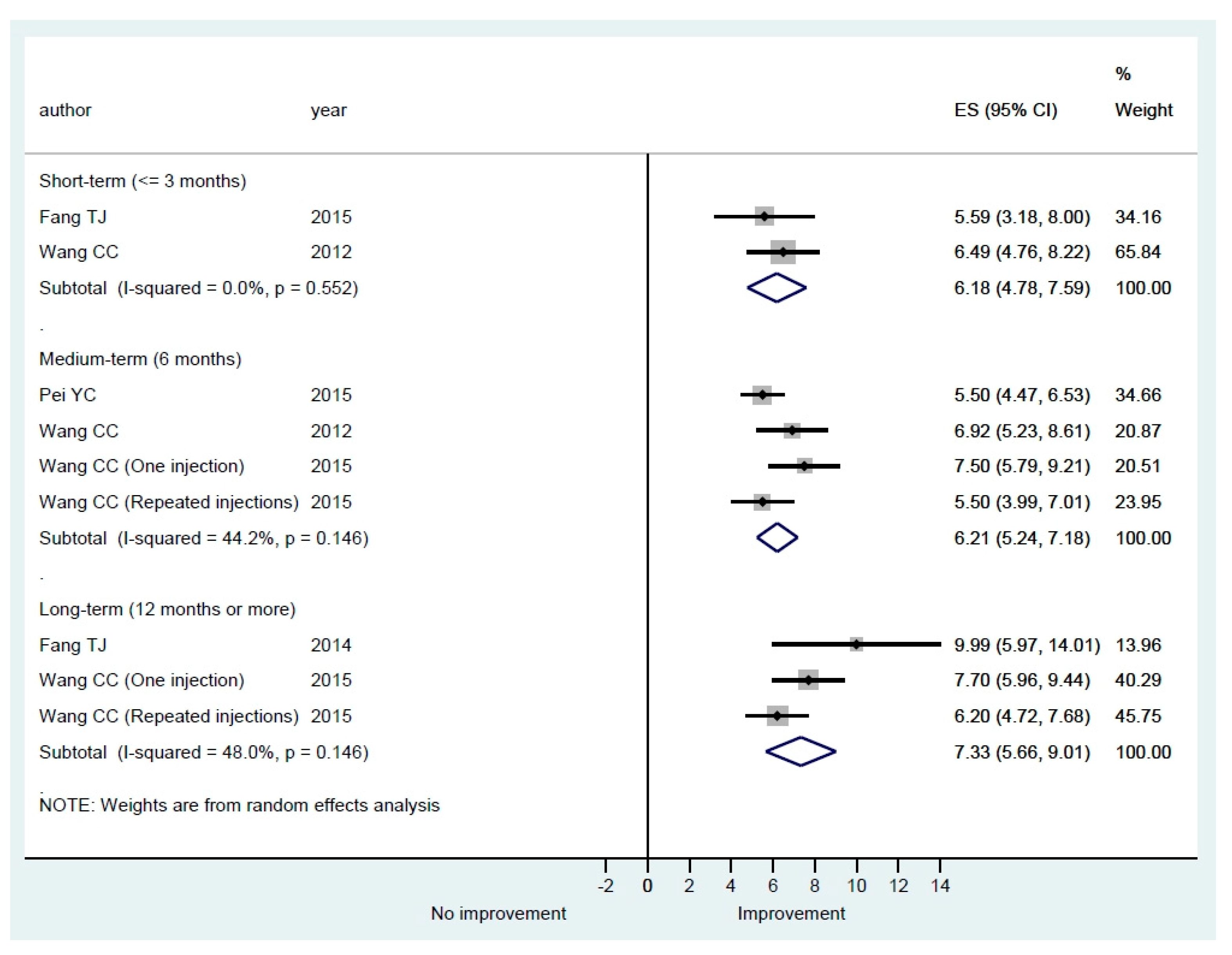
3.3.4. Image or Video Analysis
3.3.5. Additional Evaluations
4. Discussion
4.1. Safety and Complications of HA IL
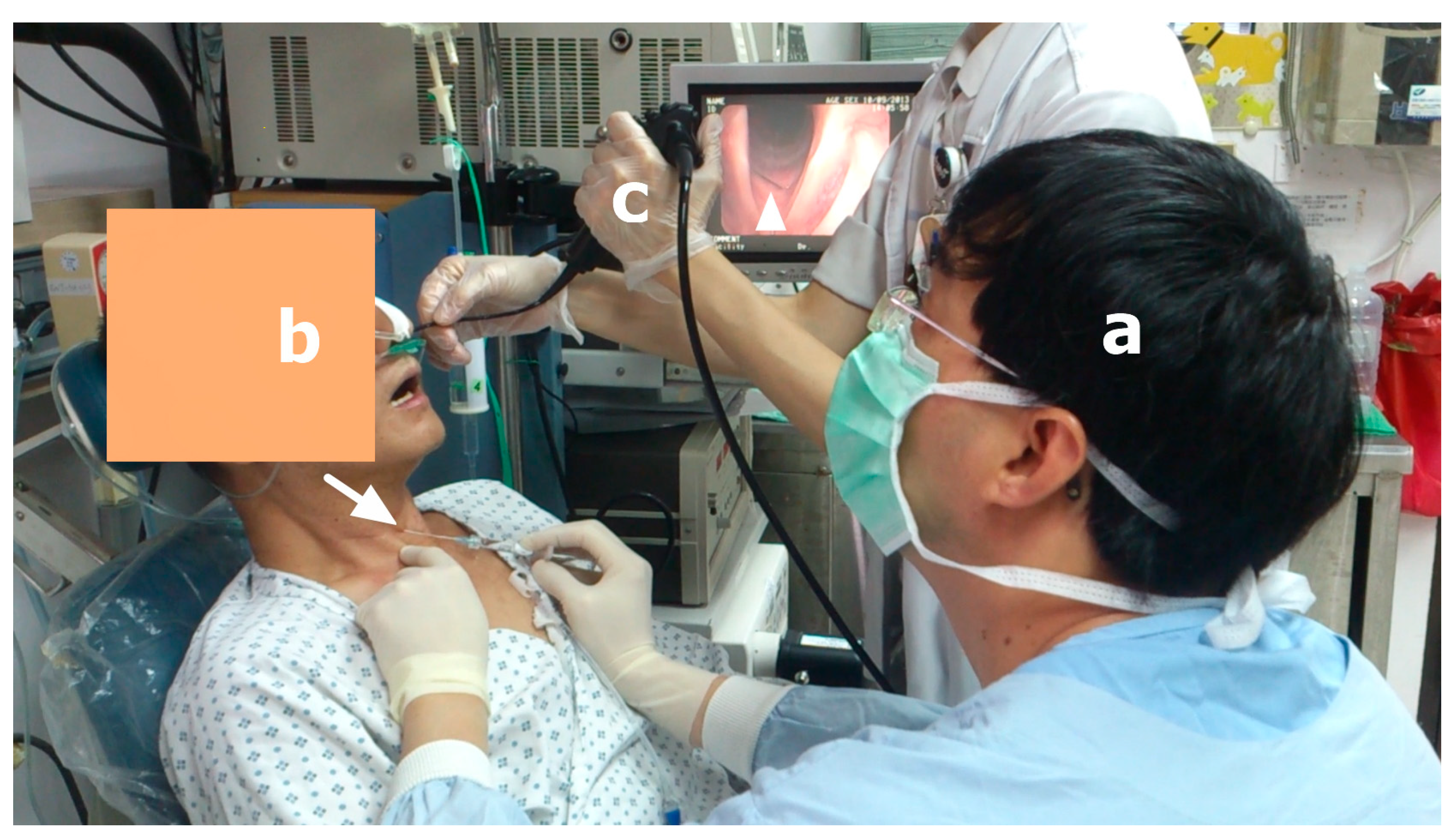
4.2. Techniques of HA IL
4.3. Different HA, Volume, and Needle
4.4. Treatment Outcomes
4.5. Study Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Marie, J.P.; Hansen, K.; Brami, P.; Marronnier, A.; Bon-Mardion, N. Nonselective Reinnervation as a Primary or Salvage Treatment of Unilateral Vocal Fold Palsy. Laryngoscope 2020, 130, 1756–1763. [Google Scholar] [CrossRef] [PubMed]
- Vila, P.M.; Bhatt, N.K.; Paniello, R.C. Early-injection laryngoplasty may lower risk of thyroplasty: A systematic review and meta-analysis. Laryngoscope 2018, 128, 935–940. [Google Scholar] [CrossRef] [PubMed]
- Brunings, W. Uber eine neue behandlungsmethode der rekurrenslahmung. Verh. Ver Laryngol. 1911, 18, 93–151. [Google Scholar]
- Sulica, L.; Rosen, C.A.; Postma, G.N.; Postma, G.N.; Simpson, B.; Amin, M.; Courey, M.; Merati, A. Current practice in injection augmentation of the vocal folds: Indications, treatment principles, techniques, and complications. Laryngoscope 2010, 120, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Kwon, T.K.; Buckmire, R. Injection laryngoplasty for management of unilateral vocal fold paralysis. Curr. Opin. Otolaryngol. Head Neck Surg. 2004, 12, 538–542. [Google Scholar] [CrossRef]
- Hertegård, S.; Hallén, L.; Laurent, C.; Lindström, E.; Olofsson, K.; Testad, P.; Dahlqvist, A. Cross-linked hyaluronan used as augmentation substance for treatment of glottal insufficiency: Safety aspects and vocal fold function. Laryngoscope 2002, 112, 2211–2219. [Google Scholar] [CrossRef]
- Chhetri, D.K.; Mendelsohn, A.H. Hyaluronic acid for the treatment of vocal fold scars. Curr. Opin. Otolaryngol. Head Neck Surg. 2010, 18, 498–502. [Google Scholar] [CrossRef]
- Borzacchiello, A.; Mayol, L.; Gärskog, O.; Dahlqvist, A.; Ambrosio, L. Evaluation of Injection Augmentation Treatment of Hyaluronic Acid Based Materials on Rabbit Vocal Folds Viscoelasticity. J. Mater. Sci. Mater. Med. 2005, 16, 553–557. [Google Scholar] [CrossRef]
- Manna, F.; Dentini, M.; Desideri, P.; De Pità, O.; Mortilla, E.; Maras, B. Comparative chemical evaluation of two commercially available derivatives of hyaluronic acid (hylaform from rooster combs and restylane from streptococcus) used for soft tissue augmentation. J. Eur. Acad. Dermatol. Venereol. 1999, 13, 183–192. [Google Scholar] [CrossRef]
- Lacapere, J.; Delaville, G. Study on Hyaluronic Acid and Variations of Its Molecular Size. Pathol. Biol. 1960, 8, 29–36. [Google Scholar] [PubMed]
- Booth, A.; Clarke, M.; Dooley, G.; Ghersi, D.; Moher, D.; Petticrew, M.; Stewart, L. The nuts and bolts of PROSPERO: An international prospective register of systematic reviews. Syst. Rev. 2012, 1, 2. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzla, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematicreviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Becker, B.J. Synthesizing standardized mean-change measures. Br. J. Math. Stat. Psychol. 1988, 41, 257–278. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials revisited. Contemp. Clin. Trials 2015, 45, 139–145. [Google Scholar] [CrossRef]
- Ng, M.L.; Wong, B.Y.H. Voice performance in tonal language speakers with glottal insufficiency due to unilateral vocal fold paralysis after injection laryngoplasty: A multidimensional study of Cantonese patients. Hong Kong Med. J. 2018, 24 (Suppl. 2), 42–44. [Google Scholar] [PubMed]
- Pei, Y.C.; Chuang, H.F.; Chang, C.F.; Chang, T.L.; Chiang, H.C.; Fang, T.J. Voice Range Change After Injection Laryngoplasty for Unilateral Vocal Fold Paralysis. J. Voice 2018, 32, 625–632. [Google Scholar] [CrossRef]
- Kara, H.V.; Karaaltin, A.B.; Ersen, E.; Alaskarov, E.; Kilic, B.; Turna, A. Minimally invasive injection laryngoplasty in the management of unilateral vocal cord paralysis after video-assisted mediastinal lymph adenectomy. Wideochirurgia Inne Tech. Maloinwazyjne 2018, 13, 388–393. [Google Scholar] [CrossRef]
- Gotxi-Erezuma, I.; Ortega-Galán, M.; Laso-Elguezabal, A.; Puga, G.P.; Bullido-Alonso, C.; García-Gutiérrez, S.; Anton-Ladislao, A.; Moreno-Alonso, E. Electromyography-guided Hyaluronic Acid Injection Laryngoplasty in Early Stage of Unilateral Vocal Fold Paralysis. Acta Otorrinolaringol. Esp. 2017, 68, 274–283. [Google Scholar] [CrossRef]
- Fang, T.J.; Hsin, L.J.; Chung, H.F.; Chiang, H.C.; Li, H.Y.; Wong, A.M.K.; Pei, C.P. Office-Based Intracordal Hyaluronate Injections Improve Quality of Life in Thoracic-Surgery-Related Unilateral Vocal Fold Paralysis. Medicine 2015, 94, e1787. [Google Scholar] [CrossRef]
- Pei, Y.C.; Fang, T.J.; Hsin, L.J.; Li, H.Y.; Wong, A.M.K. Early hyaluronate injection improves quality of life but not neural recovery in unilateral vocal fold paralysis: An open-label randomized controlled study. Restor. Neurol. Neurosci. 2015, 33, 121–130. [Google Scholar] [CrossRef]
- Wang, C.C.; Chang, M.H.; Jiang, R.S.; Lai, H.C.; De Virgilio, A.; Wang, C.P.; Wu, S.H.; Liu, S.A.; Liang, K.L. Laryngeal electromyography-guided hyaluronic acid vocal fold injection for unilateral vocal fold paralysis- a prospective long term follow up outcome report. JAMA Otolaryngol. Head Neck Surg. 2015, 141, 264–271. [Google Scholar] [CrossRef]
- Fang, T.J.; Pei, Y.C.; Li, H.Y.; Wong, A.M.K.; Chiang, H.C. Glottal Gap as an Early Predictor for Permanent Laryngoplasty in Unilateral Vocal Fold Paralysis. Laryngoscope 2014, 124, 2125–2130. [Google Scholar] [CrossRef] [PubMed]
- Wen, M.H.; Cheng, P.W.; Liao, L.J.; Chou, S.W.; Wang, C.T. Treatment Outcomes of Injection Laryngoplasty Using Cross-Linked Porcine Collagen and Hyaluronic Acid. Otolaryngol. Head Neck Surg. 2013, 149, 900–906. [Google Scholar] [CrossRef]
- Oguz, H.; Demirci, M.; Arslan, N.; Arslan, E. Long-term voice results of injection with hyaluronic acid-dextranomere in unilateral vocal fold paralysis. Acta Oto-Laryngol. 2013, 133, 513–517. [Google Scholar] [CrossRef]
- Rudolf, R.; Sibylle, B. Laryngoplasty with Hyaluronic Acid in Patients with Unilateral Vocal Fold Paralysis. J. Voice 2012, 26, 785–791. [Google Scholar] [CrossRef]
- Wang, C.C.; Chang, M.H.; Wang, C.P.; Liu, S.A.; Liang, K.L.; Wu, S.H.; Jiang, R.S.; Huang, H.T.; Lai, H.C. Laryngeal Electromyography-Guided Hyaluronic Acid Vocal Fold Injection for Unilateral Vocal Fold Paralysis-Preliminary Results. J. Voice 2012, 26, 506–514. [Google Scholar] [CrossRef] [PubMed]
- Lau, D.P.; Lee, G.A.; Wong, S.M.; Lim, V.P.; Chan, Y.H.; Tan, N.G.; Rammage, L.A.; Morrison, M.D. Injection Laryngoplasty With Hyaluronic Acid for Unilateral Vocal Cord Paralysis. Randomized Controlled Trial Comparing Two Different Particle Sizes. J. Voice 2010, 24, 113–118. [Google Scholar] [CrossRef]
- Friedman, A.D.; Burns, J.A.; Heaton, J.T.; Zeitels, S.M. Early Versus Late Injection Medialization for Unilateral Vocal Cord Paralysis. Laryngoscope 2010, 120, 2042–2046. [Google Scholar] [CrossRef]
- Jacobson, B.H.; Johnson, A.; Grywalsky, C.; Silbergleit, A.; Jacobson, G.; Benninger, M.S.; Newman, C.W. The Voice Handicap Index (VHI): Development and validation. Am. Speech Lang. Pathol. 1997, 6, 66–70. [Google Scholar] [CrossRef]
- Rosen, C.A.; Lee, A.S.; Osborne, J.; Zullo, T.; Murry, T. Development and Validation of the Voice Handicap index-10. Laryngoscope 2004, 114, 1549–1556. [Google Scholar] [CrossRef]
- Gliklich, R.E.; Glovsky, R.M.; Montgomery, W.W. Validation of a voice outcome survey for unilateral vocal cord paralysis. Otolaryngol. Head Neck Surg. 1999, 120, 153–158. [Google Scholar] [PubMed]
- Hirano, M. Clinical Examination of Voice; Springer: New York, NY, USA, 1981; pp. 81–84. [Google Scholar]
- Ptok, M.; Schwemmle, C.; Iven, C.; Jessen, M.; Nawka, T. Zur auditiven Bewertung der Stimmqualitat [On the auditory evaluation of voice quality]. HNO 2006, 54, 793–802. [Google Scholar] [CrossRef]
- Wang, C.C.; Huang, H.T. Voice Acoustic Analysis of Normal Taiwanese Adults. Chin. Med. J. 2004, 67, 179–184. [Google Scholar]
- Wang, C.C.; Huang, H.T. Voice Aerodynamic Analysis of Normal Taiwanese Adults. J. Formos. Med. Assoc. 2005, 104, 868–872. [Google Scholar]
- Xue, S.A.; Fucci, D. Effects of Race and Sex on Acoustic Features of Voice Analysis. Percept. Mot. Skills 2000, 91 Pt 1, 951–958. [Google Scholar] [CrossRef]
- Speyer, R.; Bogaardt, H.C.; Passos, V.L.; Roodenburg, N.P.; Zumach, A.; Heijnen, M.A.; Baijens, L.W.; Fleskens, S.J.; Brunings, J.W. Maximum Phonation Time: Variability and Reliability. J. Voice 2010, 24, 281–284. [Google Scholar] [CrossRef]
- Omori, K.; Kacker, A.; Slavit, D.H.; Blaugrund, S.M. Quantitative videostroboscopic measurement of glottal gap and vocal function: An analysis of thyroplasty type I. Ann. Otol. Rhinol. Laryngol. 1996, 105, 280–285. [Google Scholar] [CrossRef] [PubMed]
- Siu, J.; Tam, S.; Fung, K.A. Comparison of Outcomes in Interventions for Unilateral Vocal FoldParalysis: A Systematic Review. Laryngoscope 2016, 126, 1616–1624. [Google Scholar] [CrossRef]
- Hallén, L.; Dahlqvist, A.; Laurent, C. (DiHA): A promising substance in treating vocal cord insufficiency. Laryngoscope 1998, 108, 393–397. [Google Scholar] [CrossRef]
- Lakhani, R.; Fishman, J.M.; Bleach, N.; Costello, D.; Birchall, M. Alternative Injectable Materials for Vocal Fold Medialisation in Unilateral Vocal Fold Paralysis. Cochrane Database Syst. Rev. 2012, 17, CD009239. [Google Scholar] [CrossRef]
- Lendvay, T.S.; Sorensen, M.; Cowan, C.A.; Joyner, B.D.; Mitchell, M.M.; Grady, R.W. The evolution of vesicoureteral reflux management in the era of dextranomer/hyaluronic acid copolymer: A pediatric health information system database study. J. Urol. 2006, 176, 1864–1867. [Google Scholar] [CrossRef]
- Hamdan, A.L.; Khalifee, E. Adverse Reaction to Restylane: A Review of 63 Cases of Injection Laryngoplasty. Ear Nose Throat J. 2019, 98, 212–216. [Google Scholar] [CrossRef]
- Dominguez, L.M.; Tibbetts, K.M.; Simpson, C.B. Inflammatory reaction to hyaluronic acid: A newly described complication in vocal fold augmentation. Laryngoscope 2017, 127, 445–449. [Google Scholar] [CrossRef]
- Volk, G.F.; Hagen, R.; Pototschnig, C.; Friedrich, G.; Nawka, T.; Arens, C.; Mueller, A.; Foerster, G.; Finkensieper, M.; Lang-Roth, R.; et al. Laryngeal electromyography: A proposal for guidelines of the European Laryngological Society. Eur. Arch. Otorhinolaryngol. 2012, 269, 2227–2245. [Google Scholar] [CrossRef]
- Wang, C.C.; Chang, M.H. A proposal to extend application of laryngeal electromyography (LEMG)-guided vocal fold injection to treatment of unilateral vocal fold paralysis to enhance clinical popularity of LEMG: Response to the paper by G.F. Volk et al. Eur. Arch. Otorhinolaryngol. 2013, 270, 1563–1565. [Google Scholar] [CrossRef]
- Wang, C.C.; Chang, M.H.; De Virgilio, A.; Jiang, R.S.; Lai, H.C.; Wang, C.P.; Wu, S.H.; Liu, S.A. Laryngeal electromyography and prognosis of unilateral vocal fold paralysis—A long-term prospective study. Laryngoscope 2015, 125, 898–903. [Google Scholar] [CrossRef]
- Caton, T.; Thibeault, S.L.; Klemuk, S.; Smith, M.E. Viscoelasticity of hyaluronan and nonhyaluronan based vocal fold injectables: Implications for mucosal versus muscle use. Laryngoscope 2007, 117, 516–521. [Google Scholar] [CrossRef]
- Friedman, P.M.; Mafong, E.A.; Kauvar, A.N.; Geronemus, R.G. Safety data of injectable nonanimal stabilized hyaluronic acid gel for soft tissue augmentation. Dermatol. Surg. 2002, 28, 491–494. [Google Scholar]
- Woodson, G.E. Spontaneous laryngeal reinnervation after recurrent laryngeal or vagus nerve injury. Ann. Otol. Rhinol. Laryngol. 2007, 116, 57–65. [Google Scholar] [CrossRef]
- Yung, K.C.; Likhterov, I.; Courey, M.S. Effect of temporary vocal fold injection medialization on the rate of permanent medialization laryngoplasty in unilateral vocal fold paralysis patients. Laryngoscope 2011, 121, 2191–2194. [Google Scholar] [CrossRef]


| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
|
|
|
|
|
|
|
|
| Number + References | Year | Nation | 1st Author | Retrospective or Prospective | Patient Number | Anesthesia Type | Injection Guidance | Injection Approach | Skin Injection Route | Vocal Fold Injection | HA Name | Injected Volume | Gauge of Needle | Men F-U (Months) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 [15] | 2018 | Hong kong | Ng ML | NA | 30 | Local | Flexible L-S | Trans-cutaneous | NA | NA | Restylane | NA | NA | 3 |
| 2 [16] | 2018 | Taiwan | Pei YC | Prospective | 68 | Local | Flexible L-S | Trans-cutaeous | CT | Sub-mucosa | Restylane | 1cc | NA | 1 |
| 3 [17] | 2018 | Turkey | Kara HV | Retrospective | 5 | General | Direct L-S | Trans-oral | nil | Trans-mucosa | NA | 1cc | 25 | 3 days |
| 4 [18] | 2017 | Spain | Gotxi-Erezuma I | NA | 28 | Local | LEMG | Trans-cutaneous | CT | NA | Perlane | 2cc | 23 | 6 |
| 5 [19] | 2015 | Taiwan | Fang TJ | Retrospective | 34 | Local | Flexible L-S | Trans-cutaeous | CT | Sub-mucosa | Restylane | 1cc | NA | 1 |
| 6 [20] | 2015 | Taiwan | Pei YC | NA | 29 | Local | Flexible L-S | Trans-cutaeous | CT | Sub-mucosa | Restylane | NA | 23 or 25 | 6 |
| 7 [21] | 2015 | Taiwan | Wang CC | Prospective | 60 | Spared | LEMG | Trans-cutaeous | CT | Sub-mucosa | Perlane | 1cc | 26 | 17.4 |
| 8 [22] | 2014 | Taiwan | Fang TJ | Prospective | 20 | Local | Flexible L-S | Trans-cutaeous | CT | Sub-mucosa | Restylane | NA | NA | 15 |
| 9 [23] | 2013 | Taiwan | Wen MH | NA | 60 | Local | NA | Both | TH | Trans-mucosa | Perlane (27) + collagen (33) | 0.5 to 1cc | NA | 15 |
| 10 [24] | 2013 | Turkey | Oguz H | Retrospective | 17 | General | Direct L-S | NA | nil | NA | Hyaluronan dextranomere | NA | NA | 14 |
| 11 [25] | 2012 | Germany | Rudolf R | Prospective | 19 | General | NA | NA | NA | NA | Restylane | 0.9 cc | NA | 12.6 |
| 12 [26] | 2012 | Taiwan | Wang CC | Prospective | 20 | Spared | LEMG | Trans-cutaeous | CT | Sub-mucosa | Perlane | 1cc | 26 | 6 |
| 13 [27] | 2010 | Singapore | Lau DP | Prospective | 17 | Local | Flexible L-S | Trans-cutaeous | CT or TH | Sub-mucosa | Restylane (8) + Perlane (9) | NA | 21 or 27 | 6 |
| 14 [28] | 2010 | USA | Friedman AD | Retrospective | 35 | Local | NA | Trans-oral | nil | Trans-mucosa | NA | NA | NA | 15 |
| Number + References | 1st Author | QoL | Perceptual | Voice Laboratory | Image or Video | Additional Evaluations |
|---|---|---|---|---|---|---|
| 1 [15] | Ng ML | VHI | GRBAS | Pitch, | nil | Tone production |
| 2 [16] | Pei YC | nil | nil | MPT, F0, Jitter, shimmer, H/N, S/Z, VRP | NGGA | Q-LEMG |
| 3 [17] | Kara HV | VHI-10 | nil | MPT | nil | nil |
| 4 [18] | Gotxi-Erezuma I | VHI | GRBAS | MPT | unknown | LEMG |
| 5 [19] | Fang TJ | VOS; SF-36 | nil | MPT, S/Z, F0, Jitter, shimmer, H/N | NGGA | Q-LEMG |
| 6 [20] | Pei YC | VOS; SF-36 | nil | MPT, S/Z, F0, Jitter, shimmer, H/N | NGGA | Compare conservation management, Q-LEMG; |
| 7 [21] | Wang CC | VHI | GRBAS | MPT, PQ, MAFR | NGGA | LEMG |
| 8 [22] | Fang TJ | VOS; SF-36 | nil | MPT, S/Z, Jitter, shimmer | NGGA | Compare conservation management, Q-LEMG; |
| 9 [23] | Wen MH | VHI-10 | nil | MPT | nil | Compare HA and collagen injection |
| 10 [24] | Oguz H | nil | GRBAS | F0, jitter, shimmer, HN | nil | nil |
| 11 [25] | Rudolf R | VHI | RBH scale | MPT, intensity, F0, jitter, shimmer, VRP | nil | Compare acceptable voice + bad voice group |
| 12 [26] | Wang CC | VHI | GRBAS | MPT, PQ, MAFR | NGGA | Choking scale |
| 13 [27] | Lau DP | VHI | nil | MPT, MAFR, Jitter, shimmer, N/H, pitch range, intensity range | Glottic closed phase, Golttic open fraction | Compare large + small particle HA |
| 14 [28] | Friedman | nil | nil | nil | nil | Compare early injection + late injection group |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, C.-C.; Wu, S.-H.; Tu, Y.-K.; Lin, W.-J.; Liu, S.-A. Hyaluronic Acid Injection Laryngoplasty for Unilateral Vocal Fold Paralysis—A Systematic Review and Meta-Analysis. Cells 2020, 9, 2417. https://doi.org/10.3390/cells9112417
Wang C-C, Wu S-H, Tu Y-K, Lin W-J, Liu S-A. Hyaluronic Acid Injection Laryngoplasty for Unilateral Vocal Fold Paralysis—A Systematic Review and Meta-Analysis. Cells. 2020; 9(11):2417. https://doi.org/10.3390/cells9112417
Chicago/Turabian StyleWang, Chen-Chi, Shang-Heng Wu, Yu-Kang Tu, Wen-Jiun Lin, and Shih-An Liu. 2020. "Hyaluronic Acid Injection Laryngoplasty for Unilateral Vocal Fold Paralysis—A Systematic Review and Meta-Analysis" Cells 9, no. 11: 2417. https://doi.org/10.3390/cells9112417
APA StyleWang, C.-C., Wu, S.-H., Tu, Y.-K., Lin, W.-J., & Liu, S.-A. (2020). Hyaluronic Acid Injection Laryngoplasty for Unilateral Vocal Fold Paralysis—A Systematic Review and Meta-Analysis. Cells, 9(11), 2417. https://doi.org/10.3390/cells9112417







