Hyperleukocytosis and Leukostasis in Acute Myeloid Leukemia: Can a Better Understanding of the Underlying Molecular Pathophysiology Lead to Novel Treatments?
Abstract
1. Introduction
2. The Bone Marrow Niche under Physiologic Conditions and Its Role in the Transformation to AML
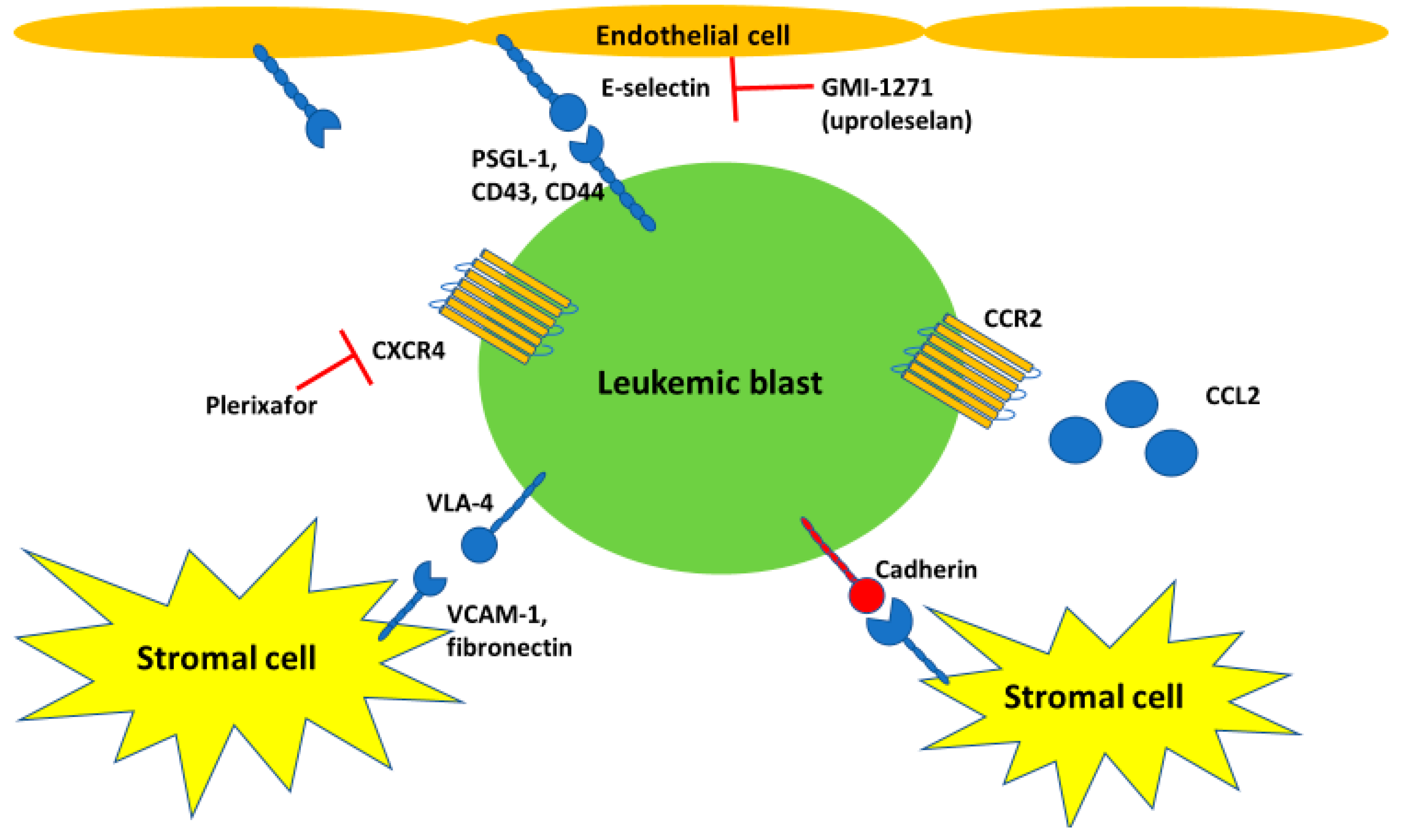
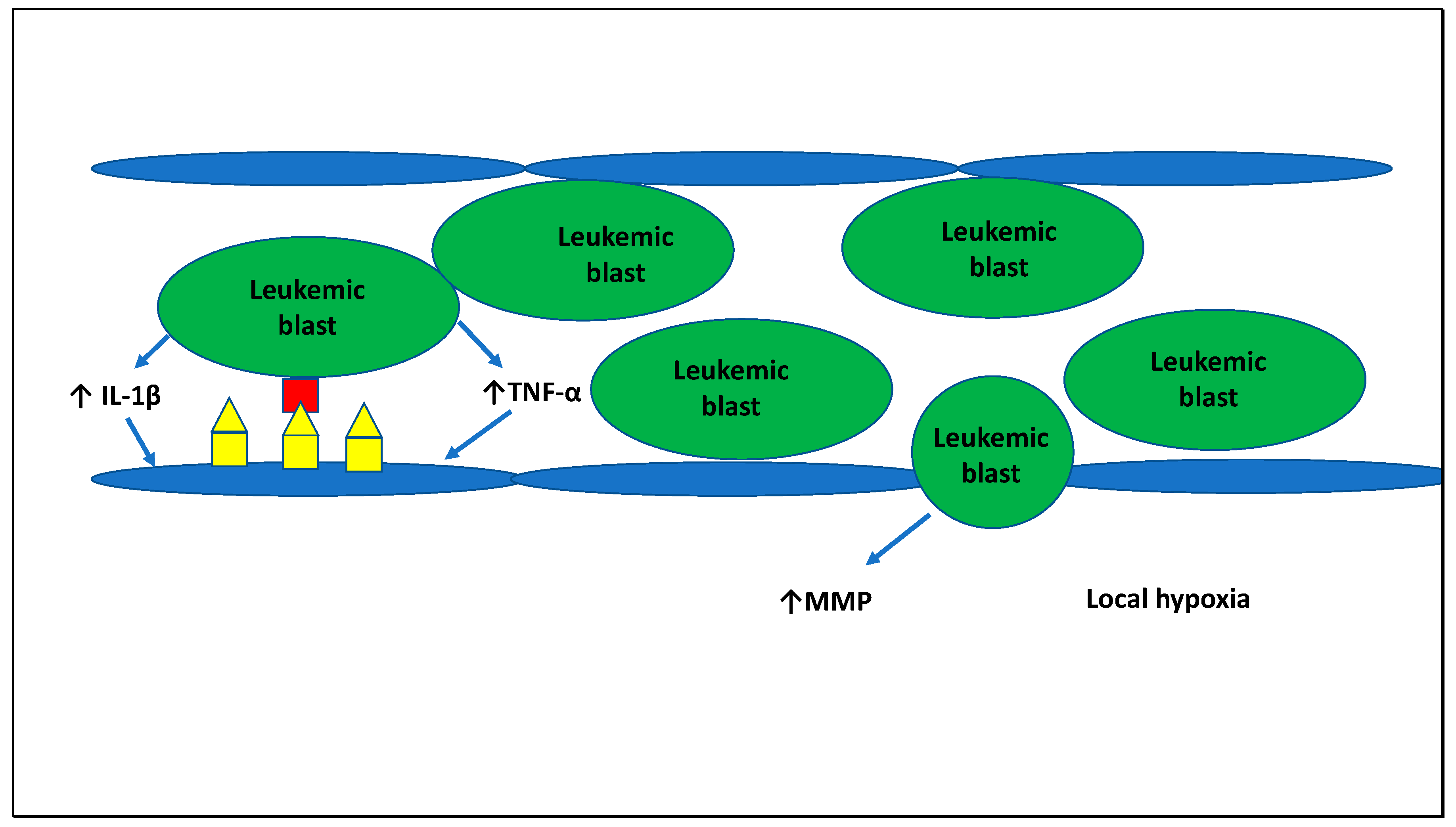
3. Interaction between Leukemic Cells and Endothelial Cells and Molecular Processes Underlying Leukostasis
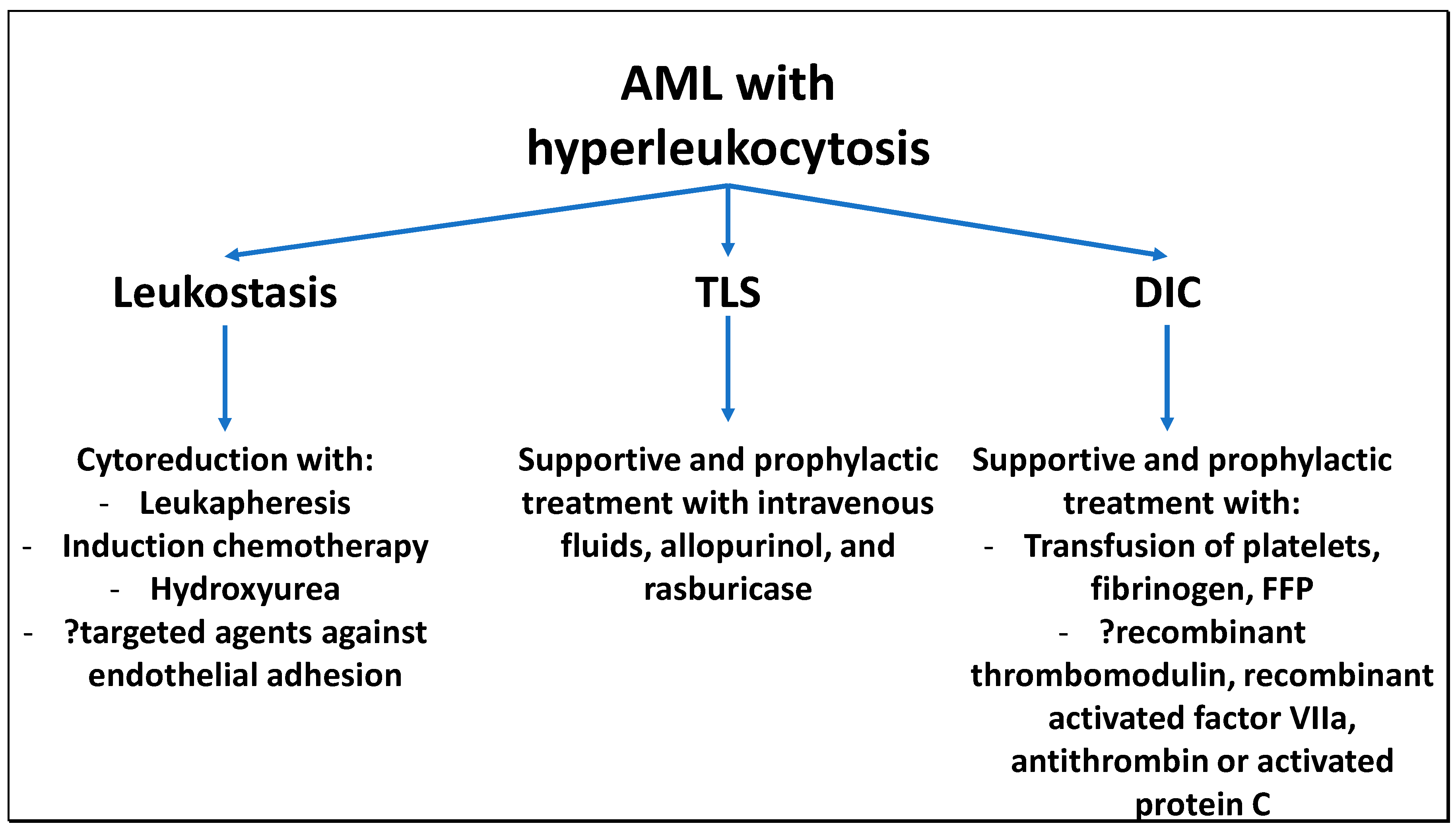
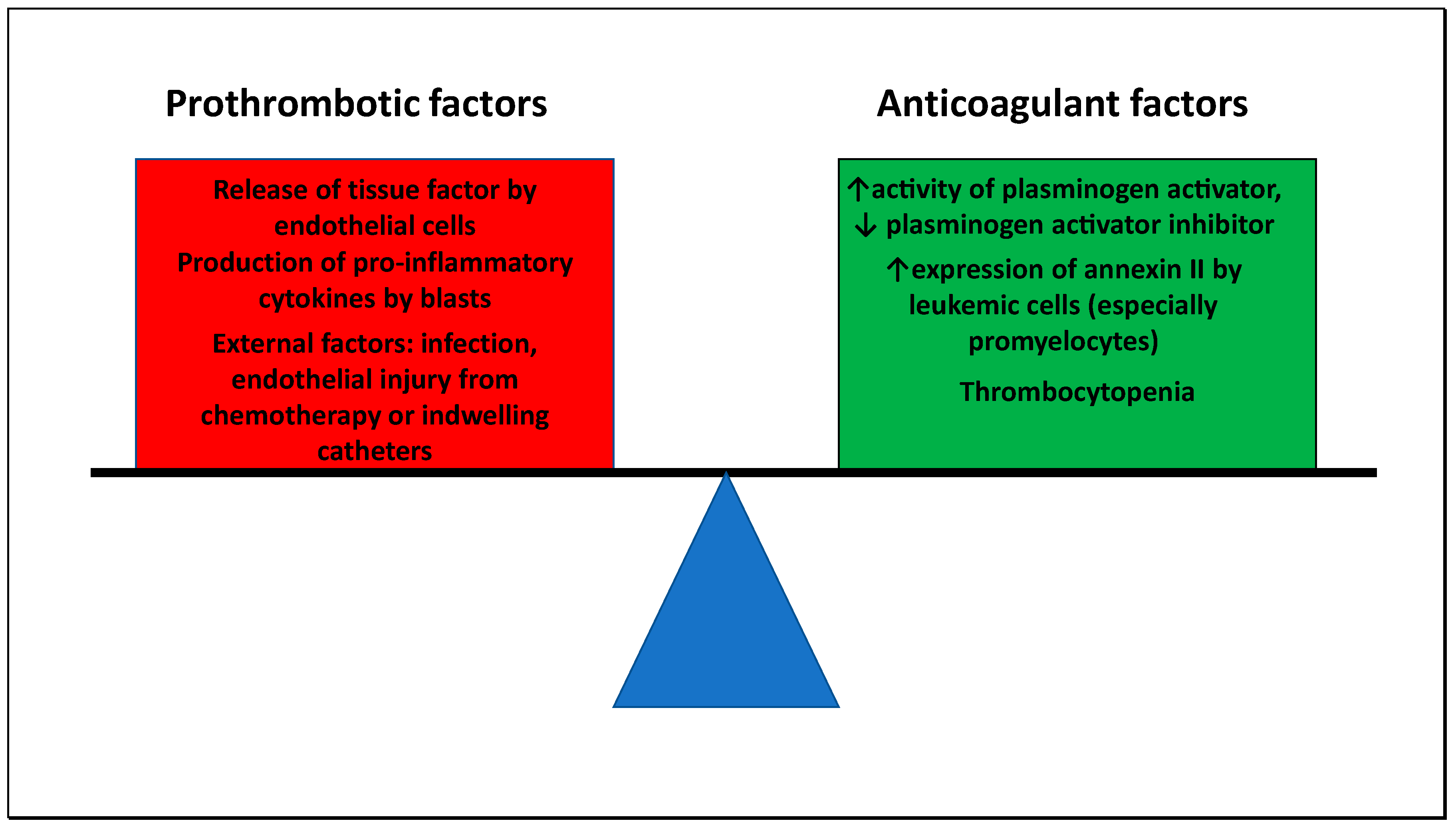
4. Coagulopathy
5. Tumor Lysis Syndrome
6. Current and Novel Molecularly Targeted Therapies for Hyperleukocytosis and Leukostasis
7. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Döhner, H.; Weisdorf, D.J.; Bloomfield, C.D. Acute Myeloid Leukemia. N. Engl. J. Med. 2015, 373, 1136–1152. [Google Scholar] [CrossRef] [PubMed]
- Short, N.J.; Rytting, M.E.; Cortes, J.E. Acute myeloid leukaemia. Lancet 2018, 392, 593–606. [Google Scholar] [CrossRef]
- Dutcher, J.P.; Schiffer, C.A.; Wiernik, P.H. Hyperleukocytosis in adult acute nonlymphocytic leukemia: Impact on remission rate and duration, and survival. J. Clin. Oncol. 1987, 5, 1364–1372. [Google Scholar] [CrossRef]
- Burnett, A.K.; Russell, N.H.; Hills, R.K.; Kell, J.; Cavenagh, J.; Kjeldsen, L.; McMullin, M.F.; Cahalin, P.; Dennis, M.; Friis, L.; et al. A randomized comparison of daunorubicin 90 mg/m2 vs. 60 mg/m2 in AML induction: Results from the UK NCRI AML17 trial in 1206 patients. Blood 2015, 125, 3878–3885. [Google Scholar] [CrossRef] [PubMed]
- Pastore, F.; Pastore, A.; Wittmann, G.; Hiddemann, W.; Spiekermann, K. The role of therapeutic leukapheresis in hyperleukocytotic AML. PLoS ONE 2014, 9, e95062. [Google Scholar] [CrossRef] [PubMed]
- Inaba, H.; Fan, Y.; Pounds, S.; Geiger, T.L.; Rubnitz, J.E.; Ribeiro, R.C.; Pui, C.-H.; Razzouk, B.I. Clinical and biologic features and treatment outcome of children with newly diagnosed acute myeloid leukemia and hyperleukocytosis. Cancer 2008, 113, 522–529. [Google Scholar] [CrossRef] [PubMed]
- Byrd, J.C.; Mrózek, K.; Dodge, R.K.; Carroll, A.J.; Edwards, C.G.; Arthur, D.C.; Pettenati, M.J.; Patil, S.R.; Rao, K.W.; Watson, M.S.; et al. Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: Results from Cancer and Leukemia Group B (CALGB 8461): Presented in part at the 43rd annual meeting of the American Society of Hematology, Orlando, FL, December 10, 2001, and published in abstract form.59. Blood 2002, 100, 4325–4336. [Google Scholar] [CrossRef]
- Feng, S.; Zhou, L.; Zhang, X.; Tang, B.; Zhu, X.; Liu, H.; Sun, Z.; Zheng, C. Impact Of ELN Risk Stratification, Induction Chemotherapy Regimens And Hematopoietic Stem Cell Transplantation On Outcomes In Hyperleukocytic Acute Myeloid Leukemia With Initial White Blood Cell Count More Than 100 × 10(9)/L. Cancer Manag. Res. 2019, 11, 9495–9503. [Google Scholar] [CrossRef]
- Röllig, C.; Ehninger, G. How I treat hyperleukocytosis in acute myeloid leukemia. Blood 2015, 125, 3246–3252. [Google Scholar] [CrossRef]
- Ventura, G.J.; Hester, J.P.; Smith, T.L.; Keating, M.J. Acute myeloblastic leukemia with hyperleukocytosis: Risk factors for early mortality in induction. Am. J. Hematol. 1988, 27, 34–37. [Google Scholar] [CrossRef]
- Shallis, R.M.; Stahl, M.; Wei, W.; Montesinos, P.; Lengline, E.; Neukirchen, J.; Bhatt, V.R.; Sekeres, M.A.; Fathi, A.T.; Konig, H.; et al. Patterns of care and clinical outcomes of patients with newly diagnosed acute myeloid leukemia presenting with hyperleukocytosis who do not receive intensive chemotherapy. Leuk. Lymphoma 2020, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Bewersdorf, J.P.; Giri, S.; Tallman, M.S.; Zeidan, A.M.; Stahl, M. Leukapheresis for the management of hyperleukocytosis in acute myeloid leukemia-A systematic review and meta-analysis. Transfusion 2020. [Google Scholar] [CrossRef] [PubMed]
- Stahl, M.; Shallis, R.M.; Wei, W.; Montesinos, P.; Lengline, E.; Neukirchen, J.; Bhatt, V.R.; Sekeres, M.A.; Fathi, A.T.; Konig, H.; et al. Management of hyperleukocytosis and impact of leukapheresis among patients with acute myeloid leukemia (AML) on short- and long-term clinical outcomes: A large, retrospective, multicenter, international study. Leukemia 2020, 04. [Google Scholar] [CrossRef] [PubMed]
- Oberoi, S.; Lehrnbecher, T.; Phillips, B.; Hitzler, J.; Ethier, M.-C.; Beyene, J.; Sung, L. Leukapheresis and low-dose chemotherapy do not reduce early mortality in acute myeloid leukemia hyperleukocytosis: A systematic review and meta-analysis. Leuk. Res. 2014, 38, 460–468. [Google Scholar] [CrossRef]
- Thiede, C.; Steudel, C.; Mohr, B.; Schaich, M.; Schäkel, U.; Platzbecker, U.; Wermke, M.; Bornhäuser, M.; Ritter, M.; Neubauer, A.; et al. Analysis of FLT3-activating mutations in 979 patients with acute myelogenous leukemia: Association with FAB subtypes and identification of subgroups with poor prognosis. Blood 2002, 99, 4326–4335. [Google Scholar] [CrossRef] [PubMed]
- Shallis, R.M.; Stahl, M.; Bewersdorf, J.P.; Hendrickson, J.E.; Zeidan, A.M. Leukocytapheresis for patients with acute myeloid leukemia presenting with hyperleukocytosis and leukostasis: A contemporary appraisal of outcomes and benefits. Expert Rev. Hematol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Schoch, C.; Schnittger, S.; Klaus, M.; Kern, W.; Hiddemann, W.; Haferlach, T. AML with 11q23/MLL abnormalities as defined by the WHO classification: Incidence, partner chromosomes, FAB subtype, age distribution, and prognostic impact in an unselected series of 1897 cytogenetically analyzed AML cases. Blood 2003, 102, 2395–2402. [Google Scholar] [CrossRef]
- Spertini, C.; Baïsse, B.; Bellone, M.; Gikic, M.; Smirnova, T.; Spertini, O. Acute Myeloid and Lymphoblastic Leukemia Cell Interactions with Endothelial Selectins: Critical Role of PSGL-1, CD44 and CD43. Cancers 2019, 11, 1253. [Google Scholar] [CrossRef]
- Stucki, A.; Rivier, A.-S.; Gikic, M.; Monai, N.; Schapira, M.; Spertini, O. Endothelial cell activation by myeloblasts: Molecular mechanisms of leukostasis and leukemic cell dissemination. Blood 2001, 97, 2121–2129. [Google Scholar] [CrossRef]
- Winkler, I.G.; Barbier, V.; Nowlan, B.; Jacobsen, R.N.; Forristal, C.E.; Patton, J.T.; Magnani, J.L.; Lévesque, J.P. Vascular niche E-selectin regulates hematopoietic stem cell dormancy, self renewal and chemoresistance. Nat. Med. 2012, 18, 1651–1657. [Google Scholar] [CrossRef]
- Barbier, V.; Erbani, J.; Fiveash, C.; Davies, J.M.; Tay, J.; Tallack, M.R.; Lowe, J.; Magnani, J.L.; Pattabiraman, D.R.; Perkins, A.C.; et al. Endothelial E-selectin inhibition improves acute myeloid leukaemia therapy by disrupting vascular niche-mediated chemoresistance. Nat. Commun. 2020, 11, 2042. [Google Scholar] [CrossRef] [PubMed]
- Calvi, L.M.; Link, D.C. The hematopoietic stem cell niche in homeostasis and disease. Blood 2015, 126, 2443–2451. [Google Scholar] [CrossRef] [PubMed]
- Boulais, P.E.; Frenette, P.S. Making sense of hematopoietic stem cell niches. Blood 2015, 125, 2621–2629. [Google Scholar] [CrossRef] [PubMed]
- Méndez-Ferrer, S.; Bonnet, D.; Steensma, D.P.; Hasserjian, R.P.; Ghobrial, I.M.; Gribben, J.G.; Andreeff , M.; Krause, D.S. Bone marrow niches in haematological malignancies. Nat. Rev. Cancer 2020, 20, 285–298. [Google Scholar] [CrossRef] [PubMed]
- Ding, L.; Morrison, S.J. Haematopoietic stem cells and early lymphoid progenitors occupy distinct bone marrow niches. Nature 2013, 495, 231–235. [Google Scholar] [CrossRef]
- Pinho, S.; Marchand, T.; Yang, E.; Wei, Q.; Nerlov, C.; Frenette, P.S. Lineage-Biased Hematopoietic Stem Cells Are Regulated by Distinct Niches. Dev. Cell 2018, 44, 634–641. [Google Scholar] [CrossRef] [PubMed]
- Crane, G.M.; Jeffery, E.; Morrison, S.J. Adult haematopoietic stem cell niches. Nat. Rev. Immunol. 2017, 17, 573–590. [Google Scholar] [CrossRef]
- Kokkaliaris, K.D.; Scadden, D.T. Cell interactions in the bone marrow microenvironment affecting myeloid malignancies. Blood Adv. 2020, 4, 3795–3803. [Google Scholar] [CrossRef]
- Mende, N.; Jolly, A.; Percin, G.I.; Günther, M.; Rostovskaya, M.; Krishnan, S.M.; Oostendorp, R.A.J.; Dahl, A.; Anastassiadis, K.; Höfer, T.; et al. Prospective isolation of nonhematopoietic cells of the niche and their differential molecular interactions with HSCs. Blood 2019, 134, 1214–1226. [Google Scholar] [CrossRef]
- von der Heide, E.K.; Neumann, M.; Vosberg, S.; James, A.R.; Schroeder, M.P.; Ortiz-Tanchez, J.; Isaakidis, K.; Schlee, C.; Luther, M.; Jöhrens, K.; et al. Molecular alterations in bone marrow mesenchymal stromal cells derived from acute myeloid leukemia patients. Leukemia 2017, 31, 1069–1078. [Google Scholar] [CrossRef]
- Desbourdes, L.; Javary, J.; Charbonnier, T.; Ishac, N.; Bourgeais, J.; Iltis, A.; Chomel, J.C.; Turhan, A.; Guilloton, F.; Tarte, K.; et al. Alteration Analysis of Bone Marrow Mesenchymal Stromal Cells from De Novo Acute Myeloid Leukemia Patients at Diagnosis. Stem Cells Dev. 2017, 26, 709–722. [Google Scholar] [CrossRef]
- Azadniv, M.; Myers, J.R.; McMurray, H.R.; Guo, N.; Rock, P.; Coppage, M.L.; Ashton, J.; Becker, M.W.; Calvi, L.M.; Liesveld, J.L. Bone marrow mesenchymal stromal cells from acute myelogenous leukemia patients demonstrate adipogenic differentiation propensity with implications for leukemia cell support. Leukemia 2020, 34, 391–403. [Google Scholar] [CrossRef] [PubMed]
- Blau, O.; Baldus, C.D.; Hofmann, W.K.; Thiel, G.; Nolte, F.; Burmeister, T.; Türkmen, S.; Benlasfer, O.; Schümann, E.; Sindram, A.; et al. Mesenchymal stromal cells of myelodysplastic syndrome and acute myeloid leukemia patients have distinct genetic abnormalities compared with leukemic blasts. Blood 2011, 118, 5583–5592. [Google Scholar] [CrossRef] [PubMed]
- Raaijmakers, M.H.; Mukherjee, S.; Guo, S.; Zhang, S.; Kobayashi, T.; Schoonmaker, J.A.; Ebert, B.L.; Al-Shahrour, F.; Hasserjian, R.P.; Scadden, E.O.; et al. Bone progenitor dysfunction induces myelodysplasia and secondary leukaemia. Nature 2010, 464, 852–857. [Google Scholar] [CrossRef] [PubMed]
- Kode, A.; Manavalan, J.S.; Mosialou, I.; Bhagat, G.; Rathinam, C.V.; Luo, N.; Khiabanian, H.; Lee, A.; Murty, V.V.; Friedman, R.; et al. Leukaemogenesis induced by an activating β-catenin mutation in osteoblasts. Nature 2014, 506, 240–244. [Google Scholar] [CrossRef]
- Dong, L.; Yu, W.M.; Zheng, H.; Loh, M.L.; Bunting, S.T.; Pauly, M.; Huang, G.; Zhou, M.; Broxmeyer, H.E.; Scadden, D.T.; et al. Leukaemogenic effects of Ptpn11 activating mutations in the stem cell microenvironment. Nature 2016, 539, 304–308. [Google Scholar] [CrossRef] [PubMed]
- Genovese, G.; Kahler, A.K.; Handsaker, R.E.; Lindberg, J.; Rose, S.A.; Bakhoum, S.F.; Chambert, K.; Mick, E.; Neale, B.M.; Fromer, M.; et al. Clonal hematopoiesis and blood-cancer risk inferred from blood DNA sequence. N. Engl. J. Med. 2014, 371, 2477–2487. [Google Scholar] [CrossRef]
- Wang, L.; Zhang, H.; Rodriguez, S.; Cao, L.; Parish, J.; Mumaw, C.; Zollman, A.; Kamoka, M.M.; Mu, J.; Chen, D.Z.; et al. Notch-dependent repression of miR-155 in the bone marrow niche regulates hematopoiesis in an NF-κB-dependent manner. Cell Stem Cell 2014, 15, 51–65. [Google Scholar] [CrossRef]
- Abelson, S.; Collord, G.; Ng, S.W.K.; Weissbrod, O.; Mendelson Cohen, N.; Niemeyer, E.; Barda, N.; Zuzarte, P.C.; Heisler, L.; Sundaravadanam, Y.; et al. Prediction of acute myeloid leukaemia risk in healthy individuals. Nature 2018, 559, 400–404. [Google Scholar] [CrossRef]
- Walter, M.J.; Shen, D.; Ding, L.; Shao, J.; Koboldt, D.C.; Chen, K.; Larson, D.E.; McLellan, M.D.; Dooling, D.; Abbott, R.; et al. Clonal architecture of secondary acute myeloid leukemia. N. Engl. J. Med. 2012, 366, 1090–1098. [Google Scholar] [CrossRef]
- Cooper, J.N.; Young, N.S. Clonality in context: Hematopoietic clones in their marrow environment. Blood 2017, 130, 2363–2372. [Google Scholar] [CrossRef]
- Windisch, R.; Pirschtat, N.; Kellner, C.; Chen-Wichmann, L.; Lausen, J.; Humpe, A.; Krause, D.S.; Wichmann, C. Oncogenic Deregulation of Cell Adhesion Molecules in Leukemia. Cancers 2019, 11, 311. [Google Scholar] [CrossRef] [PubMed]
- Gruszka, A.M.; Valli, D.; Restelli, C.; Alcalay, M. Adhesion Deregulation in Acute Myeloid Leukaemia. Cells 2019, 8, 66. [Google Scholar] [CrossRef] [PubMed]
- Craddock, C.F.; Nakamoto, B.; Andrews, R.G.; Priestley, G.V.; Papayannopoulou, T. Antibodies to VLA4 integrin mobilize long-term repopulating cells and augment cytokine-induced mobilization in primates and mice. Blood 1997, 90, 4779–4788. [Google Scholar] [CrossRef] [PubMed]
- Jin, L.; Hope, K.J.; Zhai, Q.; Smadja-Joffe, F.; Dick, J.E. Targeting of CD44 eradicates human acute myeloid leukemic stem cells. Nat. Med. 2006, 12, 1167–1174. [Google Scholar] [CrossRef] [PubMed]
- Nervi, B.; Ramirez, P.; Rettig, M.P.; Uy, G.L.; Holt, M.S.; Ritchey, J.K.; Prior, J.L.; Piwnica-Worms, D.; Bridger, G.; Ley, T.J.; et al. Chemosensitization of acute myeloid leukemia (AML) following mobilization by the CXCR4 antagonist AMD3100. Blood 2009, 113, 6206–6214. [Google Scholar] [CrossRef] [PubMed]
- Rettig, M.P.; Ansstas, G.; DiPersio, J.F. Mobilization of hematopoietic stem and progenitor cells using inhibitors of CXCR4 and VLA-4. Leukemia 2012, 26, 34–53. [Google Scholar] [CrossRef] [PubMed]
- Matsunaga, T.; Takemoto, N.; Sato, T.; Takimoto, R.; Tanaka, I.; Fujimi, A.; Akiyama, T.; Kuroda, H.; Kawano, Y.; Kobune, M.; et al. Interaction between leukemic-cell VLA-4 and stromal fibronectin is a decisive factor for minimal residual disease of acute myelogenous leukemia. Nat. Med. 2003, 9, 1158–1165. [Google Scholar] [CrossRef]
- Hsieh, Y.T.; Gang, E.J.; Geng, H.; Park, E.; Huantes, S.; Chudziak, D.; Dauber, K.; Schaefer, P.; Scharman, C.; Shimada, H.; et al. Integrin alpha4 blockade sensitizes drug resistant pre-B acute lymphoblastic leukemia to chemotherapy. Blood 2013, 121, 1814–1818. [Google Scholar] [CrossRef] [PubMed]
- Matsunaga, T.; Fukai, F.; Miura, S.; Nakane, Y.; Owaki, T.; Kodama, H.; Tanaka, M.; Nagaya, T.; Takimoto, R.; Takayama, T.; et al. Combination therapy of an anticancer drug with the FNIII14 peptide of fibronectin effectively overcomes cell adhesion-mediated drug resistance of acute myelogenous leukemia. Leukemia 2008, 22, 353–360. [Google Scholar] [CrossRef]
- Yi, H.; Zeng, D.; Shen, Z.; Liao, J.; Wang, X.; Liu, Y.; Zhang, X.; Kong, P. Integrin alphavbeta3 enhances β-catenin signaling in acute myeloid leukemia harboring Fms-like tyrosine kinase-3 internal tandem duplication mutations: Implications for microenvironment influence on sorafenib sensitivity. Oncotarget 2016, 7, 40387–40397. [Google Scholar] [CrossRef]
- Macanas-Pirard, P.; Quezada, T.; Navarrete, L.; Broekhuizen, R.; Leisewitz, A.; Nervi, B.; Ramírez, P.A. The CCL2/CCR2 Axis Affects Transmigration and Proliferation but Not Resistance to Chemotherapy of Acute Myeloid Leukemia Cells. PLoS ONE 2017, 12, e0168888. [Google Scholar] [CrossRef] [PubMed]
- Casanova-Acebes, M.; Pitaval, C.; Weiss, L.A.; Nombela-Arrieta, C.; Chèvre, R.; Noelia, A.; Kunisaki, Y.; Zhang, D.; van Rooijen, N.; Silberstein, L.E.; et al. Rhythmic modulation of the hematopoietic niche through neutrophil clearance. Cell 2013, 153, 1025–1035. [Google Scholar] [CrossRef]
- Christopher, M.J.; Liu, F.; Hilton, M.J.; Long, F.; Link, D.C. Suppression of CXCL12 production by bone marrow osteoblasts is a common and critical pathway for cytokine-induced mobilization. Blood 2009, 114, 1331–1339. [Google Scholar] [CrossRef] [PubMed]
- Saia, M.; Termanini, A.; Rizzi, N.; Mazza, M.; Barbieri, E.; Valli, D.; Ciana, P.; Gruszka, A.M.; Alcalay, M. AML1/ETO accelerates cell migration and impairs cell-to-cell adhesion and homing of hematopoietic stem/progenitor cells. Sci. Rep. 2016, 6, 34957. [Google Scholar] [CrossRef] [PubMed]
- Tien, F.-M.; Hou, H.-A.; Tsai, C.-H.; Tang, J.-L.; Chen, C.-Y.; Kuo, Y.-Y.; Li, C.-C.; Lin, C.-T.; Yao, M.; Huang, S.-Y.; et al. Hyperleukocytosis is associated with distinct genetic alterations and is an independent poor-risk factor in de novo acute myeloid leukemia patients. Eur. J. Haematol. 2018, 101, 86–94. [Google Scholar] [CrossRef]
- Rose, D.; Haferlach, T.; Schnittger, S.; Perglerová, K.; Kern, W.; Haferlach, C. Subtype-specific patterns of molecular mutations in acute myeloid leukemia. Leukemia 2017, 31, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Cuttner, J.; Conjalka, M.S.; Reilly, M.; Goldberg, J.; Reisman, A.; Meyer, R.J.; Holland, J.F. Association of monocytic leukemia in patients with extreme leukocytosis. Am. J. Med. 1980, 69, 555–558. [Google Scholar] [CrossRef]
- Kaneko, Y.; Maseki, N.; Takasaki, N.; Sakurai, M.; Hayashi, Y.; Nakazawa, S.; Mori, T.; Sakurai, M.; Takeda, T.; Shikano, T.; et al. Clinical and hematologic characteristics in acute leukemia with 11q23 translocations. Blood 1986, 67, 484–491. [Google Scholar] [CrossRef]
- Nourshargh, S.; Alon, R. Leukocyte Migration into Inflamed Tissues. Immunity 2014, 41, 694–707. [Google Scholar] [CrossRef]
- Ley, K.; Laudanna, C.; Cybulsky, M.I.; Nourshargh, S. Getting to the site of inflammation: The leukocyte adhesion cascade updated. Nat. Rev. Immunol. 2007, 7, 678–689. [Google Scholar] [CrossRef] [PubMed]
- Porcu, P.; Cripe, L.D.; Ng, E.W.; Bhatia, S.; Danielson, C.M.; Orazi, A.; McCarthy, L.J. Hyperleukocytic Leukemias and Leukostasis: A Review of Pathophysiology, Clinical Presentation and Management. Leuk. Lymphoma 2000, 39, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Soares, F.A.; Landell, G.A.; Cardoso, M.C. Pulmonary leukostasis without hyperleukocytosis: A clinicopathologic study of 16 cases. Am. J. Hematol. 1992, 40, 28–32. [Google Scholar] [CrossRef]
- Lichtman, M.A. Rheology of leukocytes, leukocyte suspensions, and blood in leukemia. Possible relationship to clinical manifestations. J. Clin. Invest. 1973, 52, 350–358. [Google Scholar] [CrossRef]
- Ali, A.M.; Mirrakhimov, A.E.; Abboud, C.N.; Cashen, A.F. Leukostasis in adult acute hyperleukocytic leukemia: A clinician’s digest. Hematol. Oncol. 2016, 34, 69–78. [Google Scholar] [CrossRef]
- Novotny, J.R.; MÜller-Beißenhirtz, H.; Herget-Rosenthal, S.; Kribben, A.; Dührsen, U. Grading of symptoms in hyperleukocytic leukaemia: A clinical model for the role of different blast types and promyelocytes in the development of leukostasis syndrome. Eur. J. Haematol. 2005, 74, 501–510. [Google Scholar] [CrossRef]
- Watarai, M.; Miwa, H.; Shikami, M.; Sugamura, K.; Wakabayashi, M.; Satoh, A.; Tsuboi, K.; Imamura, A.; Mihara, H.; Katoh, Y.; et al. Expression of endothelial cell-associated molecules in AML cells. Leukemia 2002, 16, 112–119. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cavenagh, J.D.; Gordon-Smith, E.C.; Gibson, F.M.; Gordon, M.Y. Acute myeloid leukaemia blast cells bind to human endothelium in vitro utilizing E-selectin and vascular cell adhesion molecule-1 (VCAM-1). Br. J. Haematol. 1993, 85, 285–291. [Google Scholar] [CrossRef]
- van Buchem, M.A.; Hogendoorn, P.C.; Bruijn, J.A.; Kluin, P.M. Endothelial activation antigens in pulmonary leukostasis in leukemia. Acta Haematol. 1993, 90, 29–33. [Google Scholar] [CrossRef]
- van Buchem, M.A.; Levelt, C.N.; Hogendoorn, P.C.; Colly, L.P.; Kluin, P.M.; Willemze, R.; Daha, M.R. Involvement of the complement system in the pathogenesis of pulmonary leukostasis in experimental myelocytic leukemia. Leukemia 1993, 7, 1608–1614. [Google Scholar]
- Cunningham, B.A.; Hemperly, J.J.; Murray, B.A.; Prediger, E.A.; Brackenbury, R.; Edelman, G.M. Neural cell adhesion molecule: Structure, immunoglobulin-like domains, cell surface modulation, and alternative RNA splicing. Science 1987, 236, 799–806. [Google Scholar] [CrossRef]
- Novotny, J.R.; Nuckel, H.; Duhrsen, U. Correlation between expression of CD56/NCAM and severe leukostasis in hyperleukocytic acute myelomonocytic leukaemia. Eur. J. Haematol. 2006, 76, 299–308. [Google Scholar] [CrossRef] [PubMed]
- Reikvam, H.; Hatfield, K.J.; Oyan, A.M.; Kalland, K.H.; Kittang, A.O.; Bruserud, O. Primary human acute myelogenous leukemia cells release matrix metalloproteases and their inhibitors: Release profile and pharmacological modulation. Eur. J. Haematol. 2010, 84, 239–251. [Google Scholar] [CrossRef]
- Stefanidakis, M.; Karjalainen, K.; Jaalouk, D.E.; Gahmberg, C.G.; O’Brien, S.; Pasqualini, R.; Arap, W.; Koivunen, E. Role of leukemia cell invadosome in extramedullary infiltration. Blood 2009, 114, 3008–3017. [Google Scholar] [CrossRef] [PubMed]
- Hatfield, K.J.; Bedringsaas, S.L.; Ryningen, A.; Gjertsen, B.T.; Bruserud, O. Hypoxia increases HIF-1α expression and constitutive cytokine release by primary human acute myeloid leukaemia cells. Eur. Cytokine Netw. 2010, 21, 154–164. [Google Scholar] [CrossRef] [PubMed]
- Libourel, E.J.; Klerk, C.P.W.; van Norden, Y.; de Maat, M.P.M.; Kruip, M.J.; Sonneveld, P.; Löwenberg, B.; Leebeek, F.W.G. Disseminated intravascular coagulation at diagnosis is a strong predictor for thrombosis in acute myeloid leukemia. Blood 2016, 128, 1854–1861. [Google Scholar] [CrossRef]
- Uchiumi, H.; Matsushima, T.; Yamane, A.; Doki, N.; Irisawa, H.; Saitoh, T.; Sakura, T.; Jimbo, T.; Handa, H.; Tsukamoto, N.; et al. Prevalence and clinical characteristics of acute myeloid leukemia associated with disseminated intravascular coagulation. Int. J. Hematol. 2007, 86, 137–142. [Google Scholar] [CrossRef]
- Yanada, M.; Matsushita, T.; Suzuki, M.; Kiyoi, H.; Yamamoto, K.; Kinoshita, T.; Kojima, T.; Saito, H.; Naoe, T. Disseminated intravascular coagulation in acute leukemia: Clinical and laboratory features at presentation. Eur. J. Haematol. 2006, 77, 282–287. [Google Scholar] [CrossRef]
- Lad, D.; Jain, A.; Varma, S. Complications and management of coagulation disorders in leukemia patients. Blood Lymphat. Cancer 2017, 7, 61–72. [Google Scholar] [CrossRef]
- Menell, J.S.; Cesarman, G.M.; Jacovina, A.T.; McLaughlin, M.A.; Lev, E.A.; Hajjar, K.A. Annexin II and bleeding in acute promyelocytic leukemia. N. Engl. J. Med. 1999, 340, 994–1004. [Google Scholar] [CrossRef]
- Dicke, C.; Amirkhosravi, A.; Spath, B.; Jiménez-Alcázar, M.; Fuchs, T.; Davila, M.; Francis, J.L.; Bokemeyer, C.; Langer, F. Tissue factor-dependent and -independent pathways of systemic coagulation activation in acute myeloid leukemia: A single-center cohort study. Exp. Hematol. Oncol. 2015, 4, 22. [Google Scholar] [CrossRef] [PubMed]
- Taylor, F.B., Jr.; Toh, C.H.; Hoots, W.K.; Wada, H.; Levi, M. Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb. Haemost. 2001, 86, 1327–1330. [Google Scholar] [CrossRef]
- Van de Louw, A. Effect of leukapheresis on blood coagulation in patients with hyperleukocytic acute myeloid leukemia. Transfus. Apher. Sci. 2017, 56, 214–219. [Google Scholar] [CrossRef]
- Nawroth, P.P.; Handley, D.A.; Esmon, C.T.; Stern, D.M. Interleukin 1 induces endothelial cell procoagulant while suppressing cell-surface anticoagulant activity. Proc. Natl. Acad. Sci. USA 1986, 83, 3460–3464. [Google Scholar] [CrossRef] [PubMed]
- Saito, H.; Maruyama, I.; Shimazaki, S.; Yamamoto, Y.; Aikawa, N.; Ohno, R.; Hirayama, A.; Matsuda, T.; Asakura, H.; Nakashima, M.; et al. Efficacy and safety of recombinant human soluble thrombomodulin (ART-123) in disseminated intravascular coagulation: Results of a phase III, randomized, double-blind clinical trial. J. Thromb. Haemost. 2007, 5, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, H.; Takahashi, N.; Katsuoka, Y.; Inomata, M.; Ito, T.; Meguro, K.; Kameoka, Y.; Tsumanuma, R.; Murai, K.; Noji, H.; et al. Evaluation of the safety and efficacy of recombinant soluble thrombomodulin for patients with disseminated intravascular coagulation associated with acute leukemia: Multicenter prospective study by the Tohoku Hematology Forum. Int. J. Hematol. 2017, 105, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Ookura, M.; Hosono, N.; Tasaki, T.; Oiwa, K.; Fujita, K.; Ito, K.; Lee, S.; Matsuda, Y.; Morita, M.; Tai, K.; et al. Successful treatment of disseminated intravascular coagulation by recombinant human soluble thrombomodulin in patients with acute myeloid leukemia. Medicine 2018, 97, e12981. [Google Scholar] [CrossRef]
- Martí-Carvajal, A.J.; Anand, V.; Solà, I. Treatment for disseminated intravascular coagulation in patients with acute and chronic leukemia. Cochrane Database Syst. Rev. 2015, 2015, CD008562. [Google Scholar] [CrossRef]
- Coiffier, B.; Altman, A.; Pui, C.-H.; Younes, A.; Cairo, M.S. Guidelines for the Management of Pediatric and Adult Tumor Lysis Syndrome: An Evidence-Based Review. J. Clin. Oncol. 2008, 26, 2767–2778. [Google Scholar] [CrossRef]
- Cairo, M.S.; Bishop, M. Tumour lysis syndrome: New therapeutic strategies and classification. Br. J. Haematol. 2004, 127, 3–11. [Google Scholar] [CrossRef]
- Riccio, B.; Mato, A.; Olson, E.M.; Berns, J.S.; Luger, S. Spontaneous tumor lysis syndrome in acute myeloid leukemia: Two cases and a review of the literature. Cancer Biol. Ther. 2006, 5, 1614–1617. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Montesinos, P.; Lorenzo, I.; Martín, G.; Sanz, J.; Pérez-Sirvent, M.L.; Martínez, D.; Ortí, G.; Algarra, L.; Martínez, J.; Moscardó, F.; et al. Tumor lysis syndrome in patients with acute myeloid leukemia: Identification of risk factors and development of a predictive model. Haematologica 2008, 93, 67–74. [Google Scholar] [CrossRef]
- Annemans, L.; Moeremans, K.; Lamotte, M.; Garcia Conde, J.; van den Berg, H.; Myint, H.; Pieters, R.; Uyttebroeck, A. Incidence, Medical Resource Utilisation and Costs of Hyperuricemia and Tumour Lysis Syndrome in Patients with Acute Leukaemia and Non-Hodgkin’s Lymphoma in Four European Countries. Leuk. Lymphoma 2003, 44, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Nan, X.; Qin, Q.; Gentille, C.; Ensor, J.; Leveque, C.; Pingali, S.R.; Phan, A.T.; Rice, L.; Iyer, S. Leukapheresis reduces 4-week mortality in acute myeloid leukemia patients with hyperleukocytosis-a retrospective study from a tertiary center. Leuk. Lymphoma 2017, 58, 2110–2117. [Google Scholar] [CrossRef]
- Mato, A.R.; Riccio, B.E.; Qin, L.; Heitjan, D.F.; Carroll, M.; Loren, A.; Porter, D.L.; Perl, A.; Stadtmauer, E.; Tsai, D.; et al. A predictive model for the detection of tumor lysis syndrome during AML induction therapy. Leuk. Lymphoma 2006, 47, 877–883. [Google Scholar] [CrossRef]
- Cortes, J.; Moore, J.O.; Maziarz, R.T.; Wetzler, M.; Craig, M.; Matous, J.; Luger, S.; Dey, B.R.; Schiller, G.J.; Pham, D.; et al. Control of Plasma Uric Acid in Adults at Risk for Tumor Lysis Syndrome: Efficacy and Safety of Rasburicase Alone and Rasburicase Followed by Allopurinol Compared With Allopurinol Alone—Results of a Multicenter Phase III Study. J. Clin. Oncol. 2010, 28, 4207–4213. [Google Scholar] [CrossRef] [PubMed]
- Dohner, H.; Estey, E.; Grimwade, D.; Amadori, S.; Appelbaum, F.R.; Buchner, T.; Dombret, H.; Ebert, B.L.; Fenaux, P.; Larson, R.A.; et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 2017, 129, 424–447. [Google Scholar] [CrossRef]
- Bewersdorf, J.P.; Stahl, M.; Zeidan, A.M. Are we witnessing the start of a therapeutic revolution in acute myeloid leukemia? Leuk. Lymphoma 2019, 60, 1354–1369. [Google Scholar] [CrossRef]
- Tallman, M.S.; Wang, E.S.; Altman, J.K.; Appelbaum, F.R.; Bhatt, V.R.; Bixby, D.; Coutre, S.E.; De Lima, M.; Fathi, A.T.; Fiorella, M.; et al. Acute Myeloid Leukemia, Version 3.2019, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Canc. Netw. 2019, 17, 721–749. [Google Scholar] [CrossRef] [PubMed]
- Wei, A.H.; Montesinos, P.; Ivanov, V.; DiNardo, C.D.; Novak, J.; Laribi, K.; Kim, I.; Stevens, D.; Fiedler, W.; Pagoni, M.; et al. Venetoclax plus LDAC for patients with untreated AML ineligible for intensive chemotherapy: Phase 3 randomized placebo-controlled trial. Blood 2020. [Google Scholar] [CrossRef]
- DiNardo, C.D.; Jonas, B.A.; Pullarkat, V.; Thirman, M.J.; Garcia, J.S.; Wei, A.H.; Konopleva, M.; Döhner, H.; Letai, A.; Fenaux, P.; et al. Azacitidine and Venetoclax in Previously Untreated Acute Myeloid Leukemia. N. Engl. J. Med. 2020, 383, 617–629. [Google Scholar] [CrossRef] [PubMed]
- DiNardo, C.D.; Stein, E.M.; de Botton, S.; Roboz, G.J.; Altman, J.K.; Mims, A.S.; Swords, R.; Collins, R.H.; Mannis, G.N.; Pollyea, D.A.; et al. Durable Remissions with Ivosidenib in IDH1-Mutated Relapsed or Refractory AML. N. Engl. J. Med. 2018, 378, 2386–2398. [Google Scholar] [CrossRef] [PubMed]
- Perl, A.E.; Martinelli, G.; Cortes, J.E.; Neubauer, A.; Berman, E.; Paolini, S.; Montesinos, P.; Baer, M.R.; Larson, R.A.; Ustun, C.; et al. Gilteritinib or Chemotherapy for Relapsed or Refractory FLT3-Mutated AML. N. Engl. J. Med. 2019, 381, 1728–1740. [Google Scholar] [CrossRef]
- Stone, R.M.; Mandrekar, S.J.; Sanford, B.L.; Laumann, K.; Geyer, S.; Bloomfield, C.D.; Thiede, C.; Prior, T.W.; Dohner, K.; Marcucci, G.; et al. Midostaurin plus Chemotherapy for Acute Myeloid Leukemia with a FLT3 Mutation. N. Engl. J. Med. 2017, 377, 454–464. [Google Scholar] [CrossRef]
- Stein, E.M.; DiNardo, C.D.; Pollyea, D.A.; Fathi, A.T.; Roboz, G.J.; Altman, J.K.; Stone, R.M.; DeAngelo, D.J.; Levine, R.L.; Flinn, I.W.; et al. Enasidenib in mutant IDH2 relapsed or refractory acute myeloid leukemia. Blood 2017, 130, 722–731. [Google Scholar] [CrossRef] [PubMed]
- Castaigne, S.; Pautas, C.; Terre, C.; Raffoux, E.; Bordessoule, D.; Bastie, J.N.; Legrand, O.; Thomas, X.; Turlure, P.; Reman, O.; et al. Effect of gemtuzumab ozogamicin on survival of adult patients with de-novo acute myeloid leukaemia (ALFA-0701): A randomised, open-label, phase 3 study. Lancet 2012, 379, 1508–1516. [Google Scholar] [CrossRef]
- Cortes, J.E.; Heidel, F.H.; Hellmann, A.; Fiedler, W.; Smith, B.D.; Robak, T.; Montesinos, P.; Pollyea, D.A.; DesJardins, P.; Ottmann, O.; et al. Randomized comparison of low dose cytarabine with or without glasdegib in patients with newly diagnosed acute myeloid leukemia or high-risk myelodysplastic syndrome. Leukemia 2019, 33, 379–389. [Google Scholar] [CrossRef]
- Lancet, J.E.; Uy, G.L.; Cortes, J.E.; Newell, L.F.; Lin, T.L.; Ritchie, E.K.; Stuart, R.K.; Strickland, S.A.; Hogge, D.; Solomon, S.R.; et al. CPX-351 (cytarabine and daunorubicin) Liposome for Injection Versus Conventional Cytarabine Plus Daunorubicin in Older Patients With Newly Diagnosed Secondary Acute Myeloid Leukemia. J. Clin. Oncol. 2018, 36, 2684–2692. [Google Scholar] [CrossRef]
- Wei, A.H.; Döhner, H.; Pocock, C.; Montesinos, P.; Afanasyev, B.; Dombret, H.; Ravandi, F.; Sayar, H.; Jang, J.H.; Porkka, K.; et al. The QUAZAR AML-001 Maintenance Trial: Results of a Phase III International, Randomized, Double-Blind, Placebo-Controlled Study of CC-486 (Oral Formulation of Azacitidine) in Patients with Acute Myeloid Leukemia (AML) in First Remission. Blood 2019, 134. [Google Scholar] [CrossRef]
- DiNardo, C.D.; Watts, J.M.; Stein, E.M.; de Botton, S.; Fathi, A.T.; Prince, G.T.; Stein, A.S.; Foran, J.M.; Stone, R.M.; Patel, P.A.; et al. Ivosidenib (AG-120) Induced Durable Remissions and Transfusion Independence in Patients with IDH1-Mutant Relapsed or Refractory Myelodysplastic Syndrome: Results from a Phase 1 Dose Escalation and Expansion Study. Blood 2018, 132, 1812. [Google Scholar] [CrossRef]
- Erbani, J.; Tay, J.; Barbier, V.; Levesque, J.P.; Winkler, I.G. Acute Myeloid Leukemia Chemo-Resistance Is Mediated by E-selectin Receptor CD162 in Bone Marrow Niches. Front. Cell Dev. Biol. 2020, 8, 668. [Google Scholar] [CrossRef] [PubMed]
- Winkler, I.G.; Barbier, V.; Tay, J.; Levesque, J.-P.; Magnani, J.L.; Fiveash, C.E.; Erbani, J.D. Blocking Vascular Niche E-Selectin Dampens AML Stem Cell Regeneration/Survival Potential In Vivo By Inhibiting MAPK/ERK and PI3K/AKT Signalling Pathways. Blood 2019, 134, 2657. [Google Scholar] [CrossRef]
- Devata, S.; Sood, S.L.; Hemmer, M.V.; Flanner, H.; Kramer, W.; Nietubicz, C.; Hawley, A.; Angelini, D.E.; Myers, D.D.; Blackburn, S.; et al. First in Human Phase 1 Single Dose Escalation Studies of the E-Selectin Antagonist GMI-1271 Show a Favorable Safety, Pharmacokinetic, and Biomarker Profile. Blood 2015, 126, 1004. [Google Scholar] [CrossRef]
- DeAngelo, D.J.; Jonas, B.A.; Liesveld, J.L.; Bixby, D.L.; Advani, A.S.; Marlton, P.; O’Dwyer, M.E.; Fogler, W.E.; Wolfgang, C.D.; Magnani, J.L.; et al. Uproleselan (GMI-1271), an E-Selectin Antagonist, Improves the Efficacy and Safety of Chemotherapy in Relapsed/Refractory (R/R) and Newly Diagnosed Older Patients with Acute Myeloid Leukemia: Final, Correlative, and Subgroup Analyses. Blood 2018, 132, 331. [Google Scholar] [CrossRef]
- Zeidan, A.M.; Podoltsev, N.A.; Wang, X.; Zhang, C.; Bewersdorf, J.P.; Shallis, R.M.; Huntington, S.F.; Neparidze, N.; Giri, S.; Gore, S.D.; et al. Patterns of care and clinical outcomes with cytarabine-anthracycline induction chemotherapy for AML patients in the United States. Blood Adv. 2020, 4, 1615–1623. [Google Scholar] [CrossRef]
- Martínez-Cuadrón, D.; Boluda, B.; Martínez, P.; Bergua, J.; Rodríguez-Veiga, R.; Esteve, J.; Vives, S.; Serrano, J.; Vidriales, B.; Salamero, O.; et al. A phase I-II study of plerixafor in combination with fludarabine, idarubicin, cytarabine, and G-CSF (PLERIFLAG regimen) for the treatment of patients with the first early-relapsed or refractory acute myeloid leukemia. Ann. Hematol. 2018, 97, 763–772. [Google Scholar] [CrossRef]
- Uy, G.L.; Rettig, M.P.; Stone, R.M.; Konopleva, M.Y.; Andreeff, M.; McFarland, K.; Shannon, W.; Fletcher, T.R.; Reineck, T.; Eades, W.; et al. A phase 1/2 study of chemosensitization with plerixafor plus G-CSF in relapsed or refractory acute myeloid leukemia. Blood Cancer J. 2017, 7, e542. [Google Scholar] [CrossRef]
- Roboz, G.J.; Ritchie, E.K.; Dault, Y.; Lam, L.; Marshall, D.C.; Cruz, N.M.; Hsu, H.C.; Hassane, D.C.; Christos, P.J.; Ippoliti, C.; et al. Phase I trial of plerixafor combined with decitabine in newly diagnosed older patients with acute myeloid leukemia. Haematologica 2018, 103, 1308–1316. [Google Scholar] [CrossRef]
- Layani-Bazar, A.; Skornick, I.; Berrebi, A.; Pauker, M.H.; Noy, E.; Silberman, A.; Albeck, M.; Longo, D.L.; Kalechman, Y.; Sredni, B. Redox modulation of adjacent thiols in VLA-4 by AS101 converts myeloid leukemia cells from a drug-resistant to drug-sensitive state. Cancer Res. 2014, 74, 3092–3103. [Google Scholar] [CrossRef]
- Villatoro, A.; Konieczny, J.; Cuminetti, V.; Arranz, L. Leukemia Stem Cell Release From the Stem Cell Niche to Treat Acute Myeloid Leukemia. Front. Cell Dev. Biol. 2020, 8, 607. [Google Scholar] [CrossRef]
- Stefanski, M.; Jamis-Dow, C.; Bayerl, M.; Desai, R.J.; Claxton, D.F.; Van de Louw, A. Chest radiographic and CT findings in hyperleukocytic acute myeloid leukemia: A retrospective cohort study of 73 patients. Medicine 2016, 95, e5285. [Google Scholar] [CrossRef] [PubMed]
- Azoulay, É.; Canet, E.; Raffoux, E.; Lengliné, E.; Lemiale, V.; Vincent, F.; de Labarthe, A.; Seguin, A.; Boissel, N.; Dombret, H.; et al. Dexamethasone in patients with acute lung injury from acute monocytic leukaemia. Eur. Respir. J. 2012, 39, 648–653. [Google Scholar] [CrossRef] [PubMed]
- Jaramillo, A.C.; Bergman, A.M.; Comijn, E.M.; Jansen, G.; Kaspers, G.J.L.; Cloos, J.; Peters, G.J. Effect of dexamethasone on the antileukemic effect of cytarabine: Role of deoxycytidine kinase. Nucleosides Nucleotides Nucleic Acids 2020, 1–12. [Google Scholar] [CrossRef]
- Bower, H.; Andersson, T.M.L.; Björkholm, M.; Dickman, P.W.; Lambert, P.C.; Derolf, Å.R. Continued improvement in survival of acute myeloid leukemia patients: An application of the loss in expectation of life. Blood Cancer J. 2016, 6, e390. [Google Scholar] [CrossRef] [PubMed]
| Risk Factor | Patient Population (References) | Risk Factor Associated with Hyperleukocytosis |
|---|---|---|
| FAB subtypes M4 and M5 | Single center retrospective studies of AML patients with hyperleukocytosis [5,6,8,58] | 45–73% of AML patients with hyperleukocytosis with FAB M4/5 [5,6,8,58] |
| MLL gene rearrangements |
| |
| Presence of selected mutations (e.g., FLT3) |
|
| Author [Reference] | Trial Design | Patient Population | Proportion of and Outcomes among Patients with HL |
|---|---|---|---|
| DiNardo et al. [110] | Phase I trial; single arm ivosidenib monotherapy | 258 patients with IDH1 mutations; 179 with R/R-AML | 3.5% of patients with WBC ≥ 30,000/µL; outcomes not reported separately; 36.8% with leukocytosis while receiving ivosidenib |
| Stein et al. [105] | Phase I/II trial; single arm enasidenib monotherapy | 239 patients with IDH2-mutated R/R-AML or MDS-RAEB | Median WBC 2600/µL (R: 0.2–88); proportion and outcomes of patients with HL not reported; 17% of patients with worsening non-infectious leukocytosis |
| Lancet et al. [108] | Phase III randomized trial of CPX-351 vs. standard 7 + 3 | 309 patients 60–75 years with newly diagnosed secondary AML or AML-MRC | 14.4% of patients with WBC ≥ 20,000/µL; OS significantly inferior compared to WBC ≤ 20,000/µL (HR 0.67 (95% CI: 0.45 to 0.98); p = 0.04) |
| Stone et al. [104] | Phase III randomized trial of midostaurin vs. placebo in addition to standard 7 + 3 | 717 patients 18 to 59 years of age with FLT3-mutated newly diagnosed AML | Median WBC 34,900/µL (R: 0.600–421,800); no impact of higher WBC on OS but adverse impact on EFS (HR: 1.018 [95% CI: 1.001–1.035]; p = 0.04) |
| Perl et al. [103] | Phase III randomized trial of midostaurin vs. salvage chemotherapy | 317 patients with FLT3-mutated R/R-AML | No information on WBC or outcomes reported |
| DiNardo et al. | Phase III randomized trial of azacitidine + venetoclax vs. azacitidine + placebo | 431 newly diagnosed AML patients ≥75 years or ineligible for intensive chemotherapy | WBC ≥ 25,000/µL excluded (cytoreduction with hydroxyurea or leukapheresis permitted) |
| Wei et al. [100] | Phase III randomized trial of low-dose cytarabine + venetoclax vs. low-dose cytarabine + placebo | 210 newly diagnosed AML patients ≥75 years or ineligible for intensive chemotherapy | WBC ≥ 25,000/µL excluded (cytoreduction with hydroxyurea or leukapheresis permitted) |
| Castaigne et al. [106] | Phase III randomized trial of gemtuzumab ozogamicin + standard 7 + 3 vs. standard 7 + 3 alone | 210 newly diagnosed AML patients 50–70 years | Median WBC 5900/µL (IQR: 2.100–29,100); proportion and outcomes of patients with HL not reported |
| Cortes et al. [107] | Phase II randomized trial of glasdegib + low-dose cytarabine vs. low-dose cytarabine alone | 132 newly diagnosed AML and high-risk MDS patients ineligible for intensive chemotherapy | WBC ≥ 30,000/µL excluded (cytoreduction with hydroxyurea or leukapheresis permitted) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bewersdorf, J.P.; Zeidan, A.M. Hyperleukocytosis and Leukostasis in Acute Myeloid Leukemia: Can a Better Understanding of the Underlying Molecular Pathophysiology Lead to Novel Treatments? Cells 2020, 9, 2310. https://doi.org/10.3390/cells9102310
Bewersdorf JP, Zeidan AM. Hyperleukocytosis and Leukostasis in Acute Myeloid Leukemia: Can a Better Understanding of the Underlying Molecular Pathophysiology Lead to Novel Treatments? Cells. 2020; 9(10):2310. https://doi.org/10.3390/cells9102310
Chicago/Turabian StyleBewersdorf, Jan Philipp, and Amer M. Zeidan. 2020. "Hyperleukocytosis and Leukostasis in Acute Myeloid Leukemia: Can a Better Understanding of the Underlying Molecular Pathophysiology Lead to Novel Treatments?" Cells 9, no. 10: 2310. https://doi.org/10.3390/cells9102310
APA StyleBewersdorf, J. P., & Zeidan, A. M. (2020). Hyperleukocytosis and Leukostasis in Acute Myeloid Leukemia: Can a Better Understanding of the Underlying Molecular Pathophysiology Lead to Novel Treatments? Cells, 9(10), 2310. https://doi.org/10.3390/cells9102310






