Periodontal Bone-Ligament-Cementum Regeneration via Scaffolds and Stem Cells
Abstract
1. Introduction
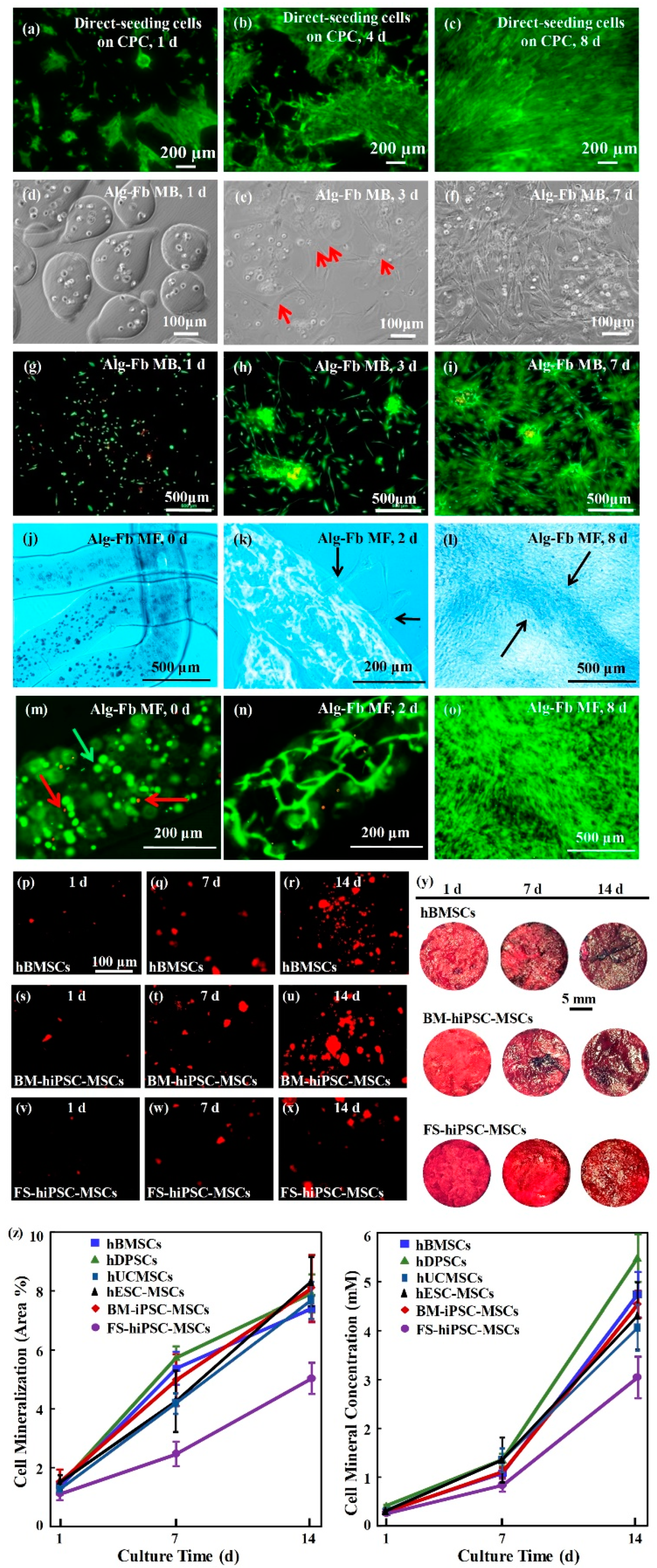
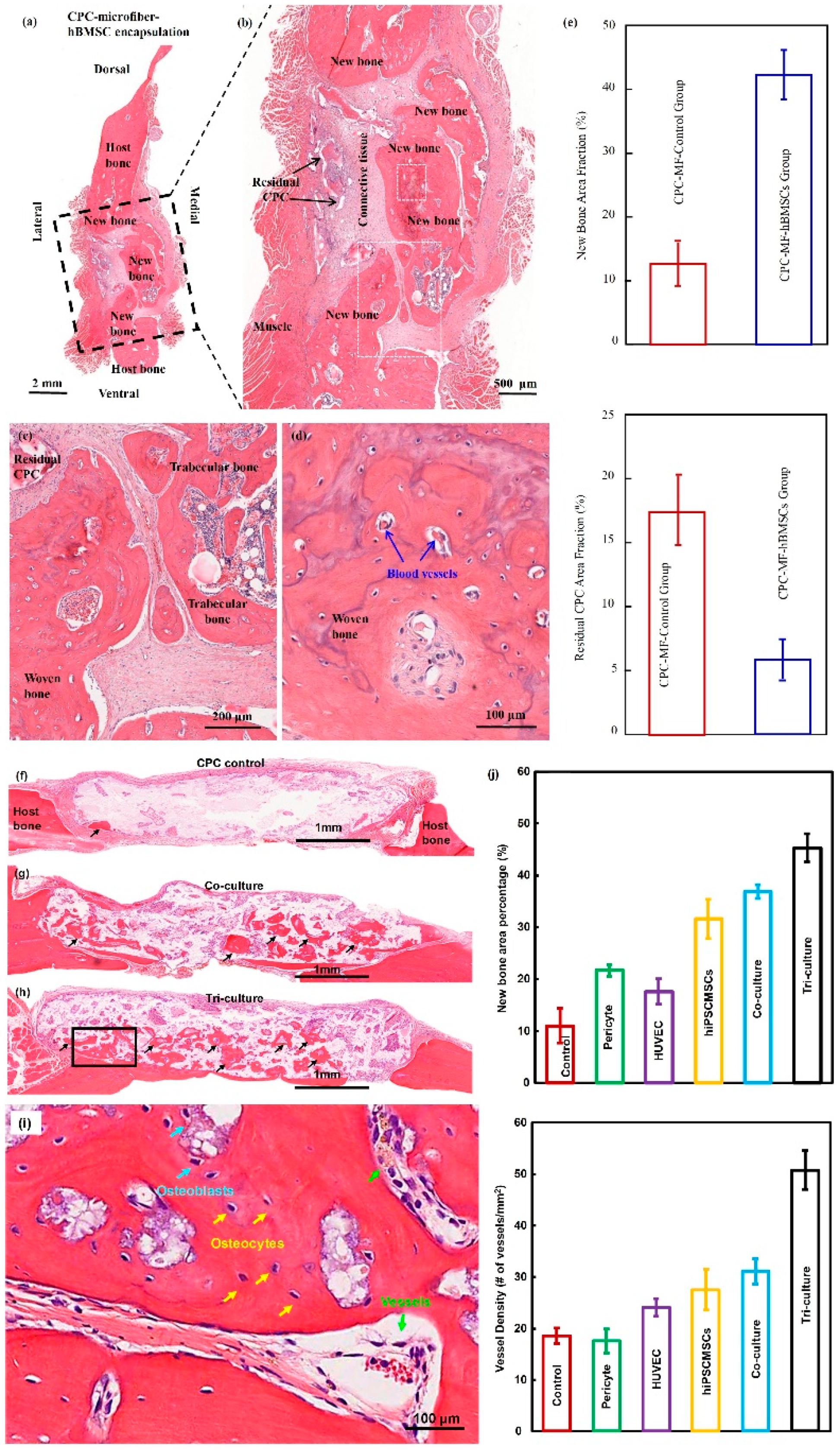
2. Bone Regeneration
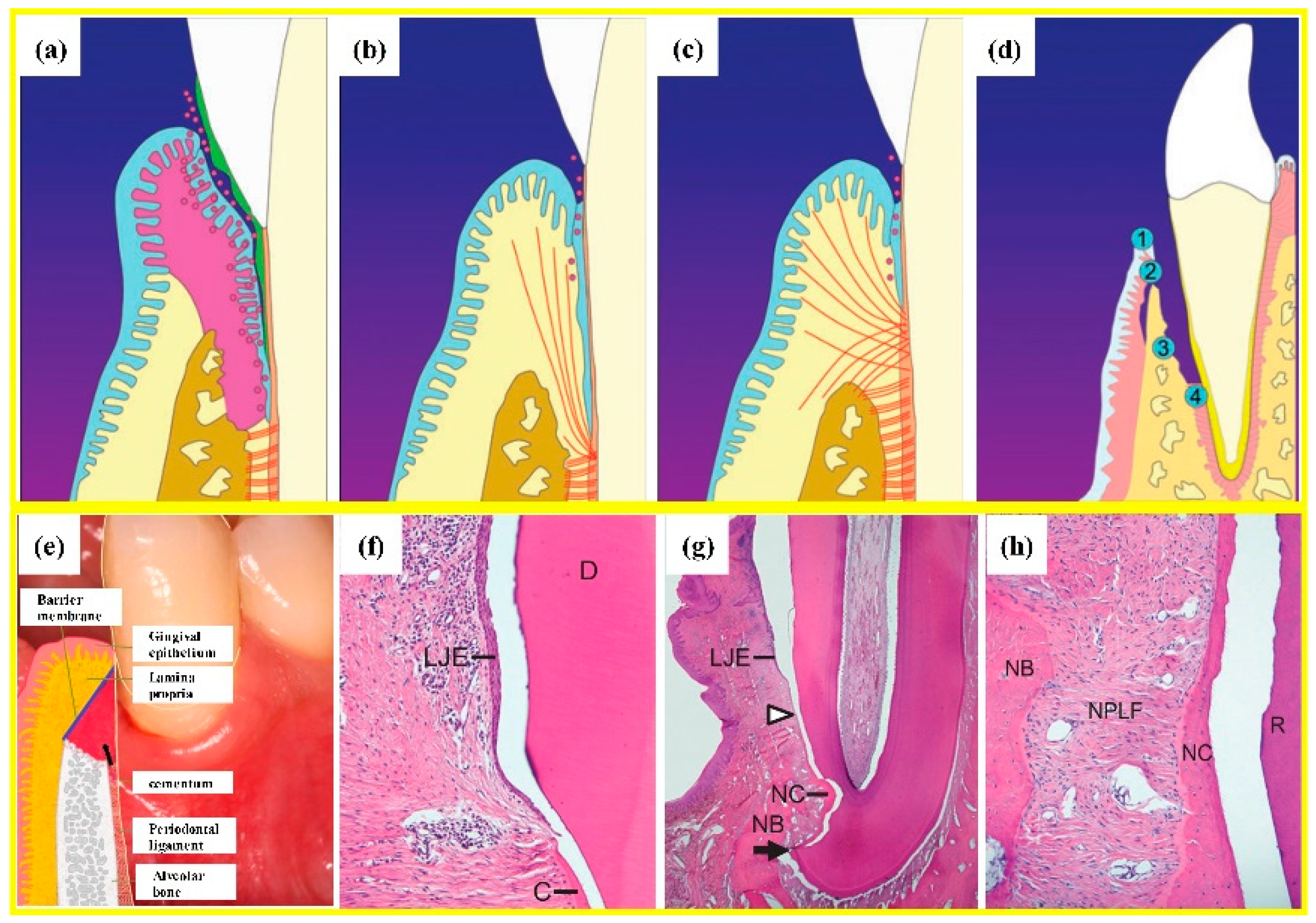
3. PDL Regeneration
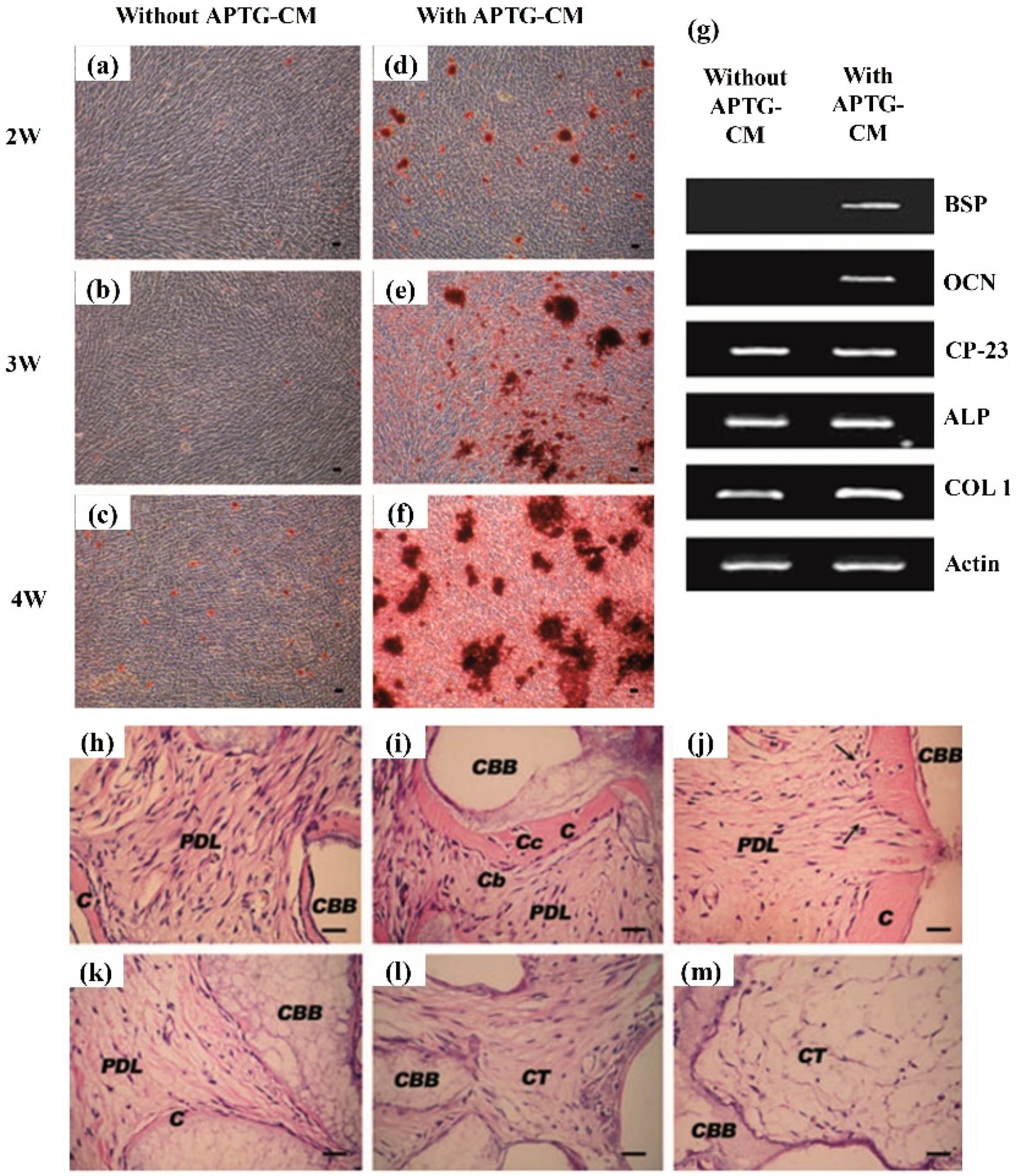
4. Cementum Regeneration
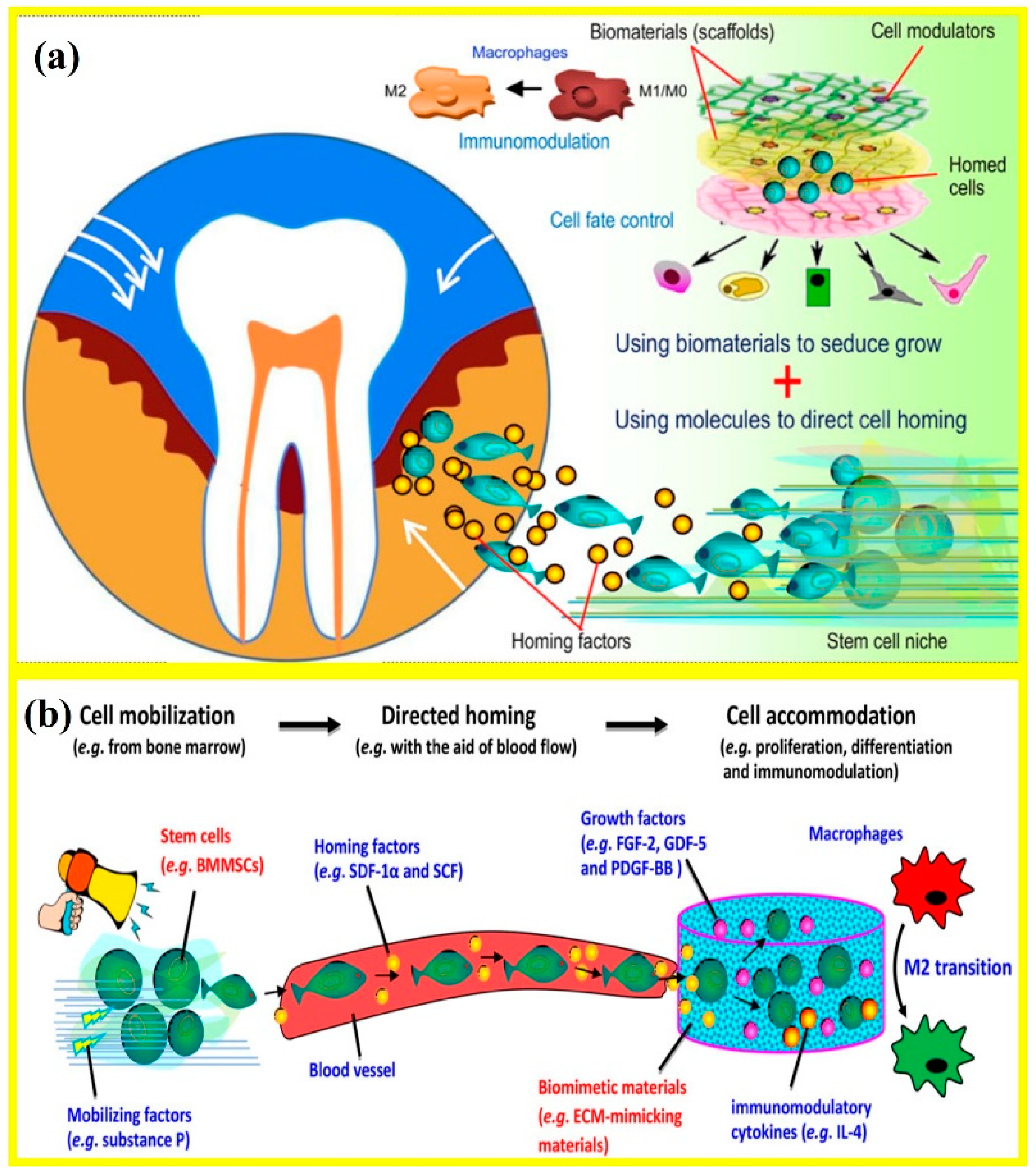
5. Endogenous Cell-Homing and Host-Mobilized Stem Cells
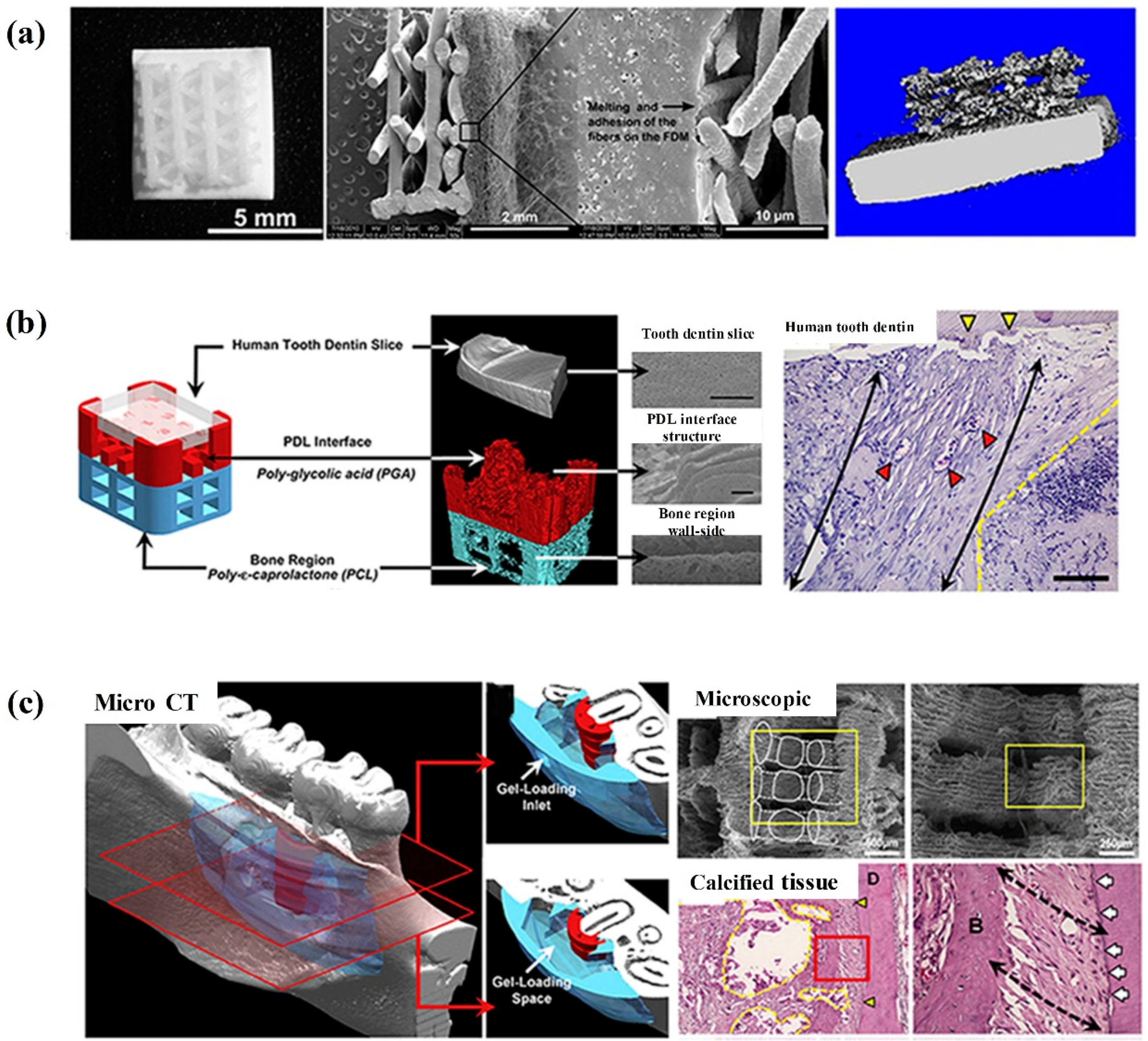
6. 3D-Bioprinting and the Generation of the Oriented PDL Fibers
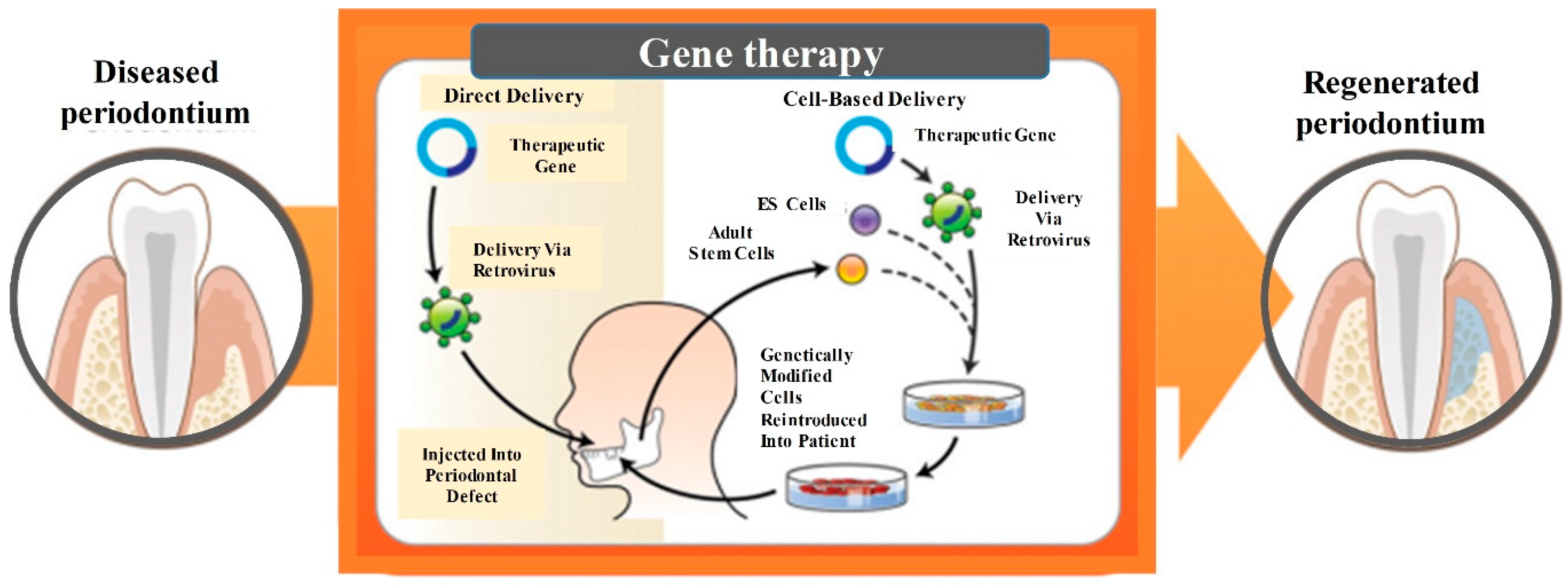
7. Gene Therapy-Based Approaches for Periodontal Regeneration
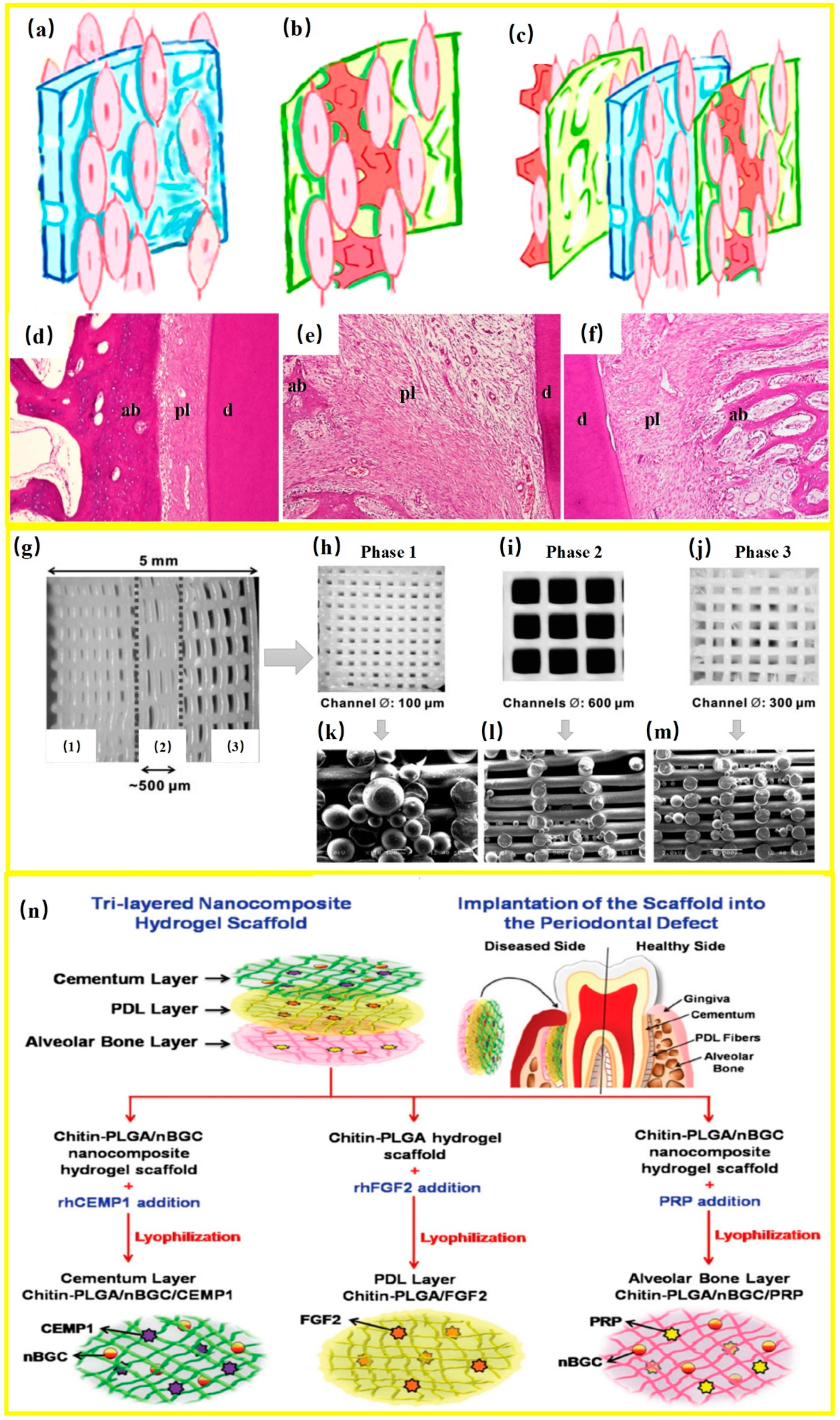
8. Regenerating Bone-PDL-Cementum Complex via Layered Materials and Cells
9. Conclusions
Funding
Conflicts of Interest
References
- Hernández-Monjaraz, B.; Santiago-Osorio, E.; Monroy-García, A.; Ledesma-Martínez, E.; Mendoza-Núñez, V.M. Mesenchymal stem cells of dental origin for inducing tissue regeneration in periodontitis: A mini-review. Int. J. Mol. Sci. 2018, 19, 944. [Google Scholar] [CrossRef] [PubMed]
- Carasol, M.; Llodra, J.C.; Fernández-Meseguer, A.; Bravo, M.; García-Margallo, M.T.; Calvo-Bonacho, E.; Sanz, M.; Herrera, D. Periodontal conditions among employed adults in spain. J. Clin. Periodontol. 2016, 43, 548–556. [Google Scholar] [CrossRef] [PubMed]
- Schaudinn, C.; Gorur, A.; Keller, D.; Sedghizadeh, P.P.; Costerton, J.W. Periodontitis: An archetypical biofilm disease. J. Am. Dent. Assoc. 2009, 140, 978–986. [Google Scholar] [CrossRef] [PubMed]
- Han, M.A. Oral health status and behavior among cancer survivors in korea using nationwide survey. Int. J. Environ. Res. Public Health 2018, 15, 14. [Google Scholar] [CrossRef] [PubMed]
- Beukers, N.G.; Gj, V.D.H.; van Wijk, A.J.; Loos, B.G. Periodontitis is an independent risk indicator for atherosclerotic cardiovascular diseases among 60 174 participants in a large dental school in the netherlands. J. Epidemiol. Community Health 2017, 71, 37–42. [Google Scholar] [CrossRef]
- Tonetti, M.S.; Van Dyke, T.E.; Beck, J.; Bouchard, P.; Cutler, C.W.; D’Aiuto, F.; Dietrich, T.; Eke, P.; Graziani, F.; Gunsolley, J. Periodontitis and atherosclerotic cardiovascular disease. J. Periodontol. 2013, 84, S24–S29. [Google Scholar] [CrossRef] [PubMed]
- Meurman, J.H.; Sanz, M.; Janket, S.-J. Oral health, atherosclerosis, and cardiovascular disease. Crit. Rev. Oral Biol. Med. 2004, 15, 403–413. [Google Scholar] [CrossRef]
- Isola, G.; Cicciù, M.; Fiorillo, L.; Matarese, G. Association between odontoma and impacted teeth. J. Craniofac. Surg. 2017, 28, 755–758. [Google Scholar] [CrossRef]
- Ferlazzo, N.; Currò, M.; Zinellu, A.; Caccamo, D.; Isola, G.; Ventura, V.; Carru, C.; Matarese, G.; Ientile, R. Influence of mthfr genetic background on p16 and mgmt methylation in oral squamous cell cancer. Int. J. Mol. Sci. 2017, 18, 724. [Google Scholar] [CrossRef]
- Sculean, A.; Chapple, I.L.; Giannobile, W.V. Wound models for periodontal and bone regeneration: The role of biologic research. Periodontology 2015, 68, 7–20. [Google Scholar] [CrossRef]
- Sowmya, S.; Mony, U.; Jayachandran, P.; Reshma, S.; Kumar, R.A.; Arzate, H.; Nair, S.V.; Jayakumar, R. Tri-layered nanocomposite hydrogel scaffold for the concurrent regeneration of cementum, periodontal ligament, and alveolar bone. Adv. Healthc. Mater. 2017, 6, 1601252. [Google Scholar] [CrossRef] [PubMed]
- Maske, B.S.; Rathod, S.; Wanikar, I. Critical issues in periodontal regeneration. SRM J. Res. Dent. Sci. 2018, 9, 119–124. [Google Scholar]
- Xu, X.-Y.; Li, X.; Wang, J.; He, X.-T.; Sun, H.-H.; Chen, F.-M. Concise review: Periodontal tissue regeneration using stem cells: Strategies and translational considerations. Stem Cells Transl. Med. 2018, 8, 392–403. [Google Scholar] [CrossRef] [PubMed]
- Chaudhari, A.; Borse, H.; Mali, A.; Agrawal, P.; Landge, N.; Khadtare, Y. Guide the tissues for periodontal regeneration (gtr): A review. Int. J. Curr. Res. 2017, 9, 59269–59278. [Google Scholar]
- Sheikh, Z.; Hamdan, N.; Ikeda, Y.; Grynpas, M.; Ganss, B.; Glogauer, M. Natural graft tissues and synthetic biomaterials for periodontal and alveolar bone reconstructive applications: A review. Biomater. Res. 2017, 21, 9. [Google Scholar] [CrossRef] [PubMed]
- Pihlstrom, B.L.; Michalowicz, B.S.; Johnson, N.W. Periodontal diseases. Lancet 2005, 366, 1809–1820. [Google Scholar] [CrossRef]
- Anushi, M.; Suresh, K. Periodontal bone regeneration in intrabony defects using osteoconductive bone graft versus combination of osteoconductive and osteostimulative bone graft: A comparative study. Dent. Res. J. 2015, 12, 25–30. [Google Scholar]
- Zhou, M.; Geng, Y.-M.; Li, S.-Y.; Yang, X.-B.; Che, Y.-J.; Pathak, J.L.; Wu, G. Nanocrystalline hydroxyapatite-based scaffold adsorbs and gives sustained release of osteoinductive growth factor and facilitates bone regeneration in mice ectopic model. J. Nanomater. 2019, 2019, 10. [Google Scholar] [CrossRef]
- Chen, M.; Xu, Y.; Zhang, T.; Ma, Y.; Liu, J.; Yuan, B.; Chen, X.; Zhou, P.; Zhao, X.; Pang, F. Mesenchymal stem cell sheets: A new cell-based strategy for bone repair and regeneration. Biotechnol. Lett. 2019, 41, 305–318. [Google Scholar] [CrossRef]
- Ivanovski, S.; Vaquette, C.; Gronthos, S.; Hutmacher, D.; Bartold, P. Multiphasic scaffolds for periodontal tissue engineering. J. Dent. Res. 2014, 93, 1212–1221. [Google Scholar] [CrossRef]
- Park, C.H.; Kim, K.H.; Lee, Y.M.; Seol, Y.J. Advanced engineering strategies for periodontal complex regeneration. Materials 2016, 9, 57. [Google Scholar] [CrossRef] [PubMed]
- Sakkas, A.; Wilde, F.; Heufelder, M.; Winter, K.; Schramm, A. Autogenous bone grafts in oral implantology—Is it still a “gold standard”? A consecutive review of 279 patients with 456 clinical procedures. Int. J. Implant Dent. 2017, 3, 23. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, M.A.; Aichelmann-Reidy, M.E.; Branch-Mays, G.L. Regeneration of periodontal tissue: Bone replacement grafts. Dent. Clin. 2010, 54, 55–71. [Google Scholar] [CrossRef] [PubMed]
- Keith, J.D., Jr.; Petrungaro, P.; Leonetti, J.A.; Elwell, C.W., Jr.; Zeren, K.J.; Caputo, C.; Nikitakis, N.G.; Schöpf, C.; Warner, M.M. Clinical and histologic evaluation of a mineralized block allograft: Results from the developmental period (2001–2004). Int. J. Periodont. Restor. Dent. 2006, 26, 320–327. [Google Scholar]
- Piattelli, A.; Scarano, A.; Fau-Corigliano, M.; Corigliano, M.; Fau-Piattelli, M.; Piattelli, M. Comparison of bone regeneration with the use of mineralized and demineralized freeze-dried bone allografts: A histological and histochemical study in man. Biomaterials 1996, 17, 1127–1131. [Google Scholar] [CrossRef]
- Liu, X.; Li, Q.; Wang, F.; Wang, Z. Maxillary sinus floor augmentation and dental implant placement using dentin matrix protein-1 gene-modified bone marrow stromal cells mixed with deproteinized boving bone: A comparative study in beagles. Arch. Oral Biol. 2016, 64, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Xu, H.H.; Takagi, S.; Chow, L.C. In-situ hardening hydroxyapatite-based scaffold for bone repair. J. Mater. Sci. Mater. Med. 2006, 17, 437–445. [Google Scholar] [CrossRef] [PubMed]
- Belal, M.; Al-Noamany, F.; El-Tonsy, M.; El-Guindy, H.; Ishikawa, I. Treatment of human class ii furcation defects using connective tissue grafts, bioabsorbable membrane, and resorbable hydroxylapatite: A comparative study. J. Int. Acad. Periodontol. 2005, 7, 114–128. [Google Scholar] [PubMed]
- Zhang, Y.; Xu, H.H.K. Effects of synergistic reinforcement and absorbable fiber strength on hydroxyapatite bone cement. J. Biomed. Mater. Res. Part A 2005, 75A, 832–840. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, C.; Kinoshita, A.; Oda, S.; Mizutani, K.; Shirakata, Y.; Ishikawa, I. Injectable calcium phosphate bone cement provides favorable space and a scaffold for periodontal regeneration in dogs. J. Periodontol. 2006, 77, 940–946. [Google Scholar] [CrossRef]
- Chu, K.; Oshida, Y.; Hancock, E.; Kowolik, M.; Barco, T.; Zunt, S. Hydroxyapatite/pmma composites as bone cements. BioMed. Mater. Eng. 2004, 14, 87–105. [Google Scholar] [PubMed]
- Fu, Q.; Saiz, E.; Rahaman, M.N.; Tomsia, A.P. Tissue engineering: Toward strong and tough glass and ceramic scaffolds for bone repair. Adv. Funct. Mater 2013, 23, 5460. [Google Scholar] [CrossRef]
- Tsai, H.-C.; Li, Y.-C.; Young, T.-H.; Chen, M.-H. Novel microinjector for carrying bone substitutes for bone regeneration in periodontal diseases. J. Formos. Med. Assoc. 2016, 115, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Simon, C.G., Jr.; Khatri, C.A.; Wight, S.A.; Wang, F.W. Preliminary report on the biocompatibility of a moldable, resorbable, composite bone graft consisting of calcium phosphate cement and poly (lactide-co-glycolide) microspheres. J. Orthopaed. Res. 2002, 20, 473–482. [Google Scholar] [CrossRef]
- Brown, W.E.; Chow, L.C. Combinations of Sparingly Soluble Calcium Phosphates in Slurries and Pastes as Mineralizers and Cements. U.S. Patent 4,612,053, 16 September 1986. [Google Scholar]
- Takagi, S.; Chow, L.C.; Hirayama, S.; Eichmiller, F.C. Properties of elastomeric calcium phosphate cement–chitosan composites. Dent. Mater. 2003, 19, 797–804. [Google Scholar] [CrossRef]
- Xu, H.H.; Wang, P.; Wang, L.; Bao, C.; Chen, Q.; Weir, M.D.; Chow, L.C.; Zhao, L.; Zhou, X.; Reynolds, M.A. Calcium phosphate cements for bone engineering and their biological properties. Bone Res. 2017, 5, 17056. [Google Scholar] [CrossRef]
- Villalona, G.A.; Udelsman, B.; Duncan, D.R.; McGillicuddy, E.; Sawh-Martinez, R.F.; Hibino, N.; Painter, C.; Mirensky, T.; Erickson, B.; Shinoka, T. Cell-seeding techniques in vascular tissue engineering. Tissue Eng. Part B Rev. 2010, 16, 341–350. [Google Scholar] [CrossRef]
- Wang, P.; Song, Y.; Weir, M.D.; Sun, J.; Zhao, L.; Simon, C.G.; Xu, H.H.K. A self-setting ipsmsc-alginate-calcium phosphate paste for bone tissue engineering. Dent. Mater. 2016, 32, 252–263. [Google Scholar] [CrossRef]
- Grosfeld, E.-C.; Hoekstra, J.W.M.; Herber, R.-P.; Ulrich, D.J.; Jansen, J.A.; van den Beucken, J.J. Long-term biological performance of injectable and degradable calcium phosphate cement. Biomed. Mater. 2016, 12, 015009. [Google Scholar] [CrossRef]
- Song, Y.; Zhang, C.; Wang, P.; Wang, L.; Bao, C.; Weir, M.D.; Reynolds, M.A.; Ren, K.; Zhao, L.; Xu, H.H. Engineering bone regeneration with novel cell-laden hydrogel microfiber-injectable calcium phosphate scaffold. Mater. Sci. Eng. C 2017, 75, 895–905. [Google Scholar] [CrossRef]
- Zhao, L.; Weir, M.D.; Xu, H.H. An injectable calcium phosphate-alginate hydrogel-umbilical cord mesenchymal stem cell paste for bone tissue engineering. Biomaterials 2010, 31, 6502–6510. [Google Scholar] [CrossRef] [PubMed]
- Mitsiadis, T.A.; Feki, A.; Papaccio, G.; Catón, J. Dental pulp stem cells, niches, and notch signaling in tooth injury. Adv. Dent. Res. 2011, 23, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Liu, X.; Zhao, L.; Weir, M.D.; Sun, J.; Chen, W.; Man, Y.; Xu, H.H.K. Bone tissue engineering via human induced pluripotent, umbilical cord and bone marrow mesenchymal stem cells in rat cranium. Acta Biomater. 2015, 18, 236–248. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Zhang, C.; Li, C.; Weir, M.D.; Wang, P.; Reynolds, M.A.; Zhao, L.; Xu, H.H. Injectable calcium phosphate with hydrogel fibers encapsulating induced pluripotent, dental pulp and bone marrow stem cells for bone repair. Mater. Sci. Eng. C 2016, 69, 1125–1136. [Google Scholar] [CrossRef] [PubMed]
- Schweikle, M.Z.T.; Lund, R.; Tiainen, H. Injectable synthetic hydrogel for bone regeneration: Physicochemical characterisation of a high and a low ph gelling system. Mater. Sci. Eng. C 2018, 90, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Acar, A.H.; Alan, H.; Ozgur, C.; Vardi, N.; Asutay, F.; Guler, C. Is more cortical bone decortication effective on guided bone augmentation? J. Craniofac. Surg. 2016, 27, 1879–1883. [Google Scholar] [CrossRef] [PubMed]
- Du, B.; Liu, W.; Deng, Y.; Li, S.; Liu, X.; Gao, Y.; Zhou, L. Angiogenesis and bone regeneration of porous nano-hydroxyapatite/coralline blocks coated with rhvegf165 in critical-size alveolar bone defects in vivo. Int. J. Nanomed. 2015, 10, 2555–2565. [Google Scholar]
- Zhang, C.; Hu, K.; Liu, X.; Reynolds, M.A.; Bao, C.; Wang, P.; Zhao, L.; Xu, H.H. Novel hipsc-based tri-culture for pre-vascularization of calcium phosphate scaffold to enhance bone and vessel formation. Mater. Sci. Eng. C 2017, 79, 296–304. [Google Scholar] [CrossRef]
- Besinis, A.; De Peralta, T.; Tredwin, C.J.; Handy, R.D. Review of nanomaterials in dentistry: Interactions with the oral microenvironment, clinical applications, hazards, and benefits. ACS Nano 2015, 9, 2255–2289. [Google Scholar] [CrossRef]
- Batool, F.; Strub, M.; Petit, C.; Bugueno, I.; Bornert, F.; Clauss, F.; Huck, O.; Kuchler-Bopp, S.; Benkirane-Jessel, N. Periodontal tissues, maxillary jaw bone, and tooth regeneration approaches: From animal models analyses to clinical applications. Nanomaterials 2018, 8, 337. [Google Scholar] [CrossRef]
- Mitsiadis, T.A.; Woloszyk, A.; Jiménez-Rojo, L. Nanodentistry: Combining nanostructured materials and stem cells for dental tissue regeneration. Nanomedicine 2012, 7, 1743–1753. [Google Scholar] [CrossRef] [PubMed]
- Polini, A.; Bai, H.; Tomsia, A.P. Dental applications of nanostructured bioactive glass and its composites. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2013, 5, 399–410. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.H.; Weir, M.D.; Zhao, L.; Moreau, J.L.; Arola, D.D.; Simon, C.G. Nano-Apatitic Composite Scaffolds for Stem Cell Delivery and Bone Tissue Engineering. In Emerging Nanotechnologies in Dentistry; William Andrew Publishing: Park Ridge, NJ, USA, 2012; pp. 189–207. [Google Scholar]
- Li, G.; Zhou, T.; Lin, S.; Shi, S.; Lin, Y. Nanomaterials for craniofacial and dental tissue engineering. J. Dent. Res. 2017, 96, 725–732. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Li, Y.; Ma, S.; Gao, Y.; Zuo, Y.; Hu, J. Enhancement of bone formation by bmp-7 transduced mscs on biomimetic nano-hydroxyapatite/polyamide composite scaffolds in repair of mandibular defects. J. Biomed. Mater. Res. Part A 2010, 95, 973–981. [Google Scholar] [CrossRef] [PubMed]
- Xia, Y.; Chen, H.; Zhang, F.; Bao, C.; Weir, M.D.; Reynolds, M.A.; Ma, J.; Gu, N.; Xu, H.H. Gold nanoparticles in injectable calcium phosphate cement enhance osteogenic differentiation of human dental pulp stem cells. Nanomed. Nanotechnol. Biol. Med. 2018, 14, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Zhang, Q.; Zhang, Y.; Cen, L.; Wang, J. Pdl regeneration via cell homing in delayed replantation of avulsed teeth. J. Transl. Med. 2015, 13, 357. [Google Scholar] [CrossRef]
- Bartold, P.M.; Shi, S.; Gronthos, S. Stem cells and periodontal regeneration. Periodontology 2000 2006, 40, 164–172. [Google Scholar] [CrossRef] [PubMed]
- Catón, J.; Bostanci, N.; Remboutsika, E.; De Bari, C.; Mitsiadis, T.A. Future dentistry: Cell therapy meets tooth and periodontal repair and regeneration. J. Cell. Mol. Med. 2011, 15, 1054–1065. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Zong, W.; Xu, X.; Chen, J. Improved biphasic calcium phosphate combined with periodontal ligament stem cells may serve as a promising method for periodontal regeneration. Am. J. Transl. Res. 2018, 10, 4030. [Google Scholar]
- Du, J.; Shan, Z.; Ma, P.; Wang, S.; Fan, Z. Allogeneic bone marrow mesenchymal stem cell transplantation for periodontal regeneration. J. Dent. Res. 2014, 93, 183–188. [Google Scholar] [CrossRef]
- Mohammed, E.; Khalil, E.; Sabry, D. Effect of adipose-derived stem cells and their exo as adjunctive therapy to nonsurgical periodontal treatment: A histologic and histomorphometric study in rats. Biomolecules 2018, 8, 167. [Google Scholar] [CrossRef] [PubMed]
- Duan, X.; Tu, Q.; Zhang, J.; Ye, J.; Sommer, C.; Mostoslavsky, G.; Kaplan, D.; Yang, P.; Chen, J. Application of induced pluripotent stem (ips) cells in periodontal tissue regeneration. J. Cell. Physiol. 2011, 226, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Bosshardt, D.D.; Sculean, A. Does periodontal tissue regeneration really work? Periodontol. 2000 2009, 51, 208–219. [Google Scholar] [CrossRef] [PubMed]
- Siaili, M.; Chatzopoulou, D.; Gillam, D.G. An overview of periodontal regenerative procedures for the general dental practitioner. Saudi Dent. J. 2018, 30, 26–37. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.K. Gtr membranes: The barriers for periodontal regeneration. DHR Int. J. Med. Sci. 2013, 4, 31–38. [Google Scholar]
- Bottino, M.C.; Thomas, V.; Schmidt, G.; Vohra, Y.K.; Chu, T.-M.G.; Kowolik, M.J.; Janowski, G.M. Recent advances in the development of gtr/gbr membranes for periodontal regeneration—A materials perspective. Dent. Mater. 2012, 28, 703–721. [Google Scholar] [CrossRef] [PubMed]
- Cash, A. 20 Years of Guided Bone Regeneration in Implant Dentistry, 2nd ed.; Oxford University Press: Oxford, UK, 2019. [Google Scholar]
- Pretzl, B.; Kim, T.-S.; Holle, R.; Eickholz, P. Long-term results of guided tissue regeneration therapy with non-resorbable and bioabsorbable barriers. Iv. A case series of infrabony defects after 10 years. J. Periodontol. 2008, 79, 1491–1499. [Google Scholar] [CrossRef] [PubMed]
- Corinaldesi, G.; Lizio, G.; Badiali, G.; Morselli-Labate, A.M.; Marchetti, C. Treatment of intrabony defects after impacted mandibular third molar removal with bioabsorbable and non-resorbable membranes. J. Periodontol. 2011, 82, 1404–1413. [Google Scholar] [CrossRef]
- Moshaverinia, A.; Chen, C.; Xu, X.; Akiyama, K.; Ansari, S.; Zadeh, H.H.; Shi, S. Bone regeneration potential of stem cells derived from periodontal ligament or gingival tissue sources encapsulated in rgd-modified alginate scaffold. Tissue Eng. Part A 2013, 20, 611–621. [Google Scholar] [CrossRef] [PubMed]
- Bollati, D.; Morra, M.; Cassinelli, C.; Cascardo, G. Implantable Devices Having Antibacterial Properties and Multifunctional Surfaces. U.S. Patent 9,999,706, 19 June 2018. [Google Scholar]
- Nyamsuren, E.; Bayarchimeg, B.; Urjinlkham, J.; Oyun-enkh, P.; Kh, O.; Batsuuri, M.; Lu, S.-l. Efficacy of natural biopolymer chitosan membrane for guided tissue regeneration. Innovation 2018, 12, 16–20. [Google Scholar]
- Cui, J.; Liang, J.; Wen, Y.; Sun, X.; Li, T.; Zhang, G.; Sun, K.; Xu, X. In vitro and in vivo evaluation of chitosan/β-glycerol phosphate composite membrane for guided bone regeneration. J. Biomed. Mater. Res. Part A 2014, 102, 2911–2917. [Google Scholar] [CrossRef] [PubMed]
- Xue, Y.; Hong, X.; Gao, J.; Shen, R.; Ye, Z. Preparation and biological characterization of the mixture of poly (lactic-co-glycolic acid)/chitosan/ag nanoparticles for periodontal tissue engineering. Int. J. Nanomed. 2019, 14, 483. [Google Scholar] [CrossRef] [PubMed]
- Lausch, A.J.; Chong, L.C.; Uludag, H.; Sone, E.D. Multiphasic collagen scaffolds for engineered tissue interfaces. Adv. Funct. Mater. 2018, 28, 1804730. [Google Scholar] [CrossRef]
- Zhou, T.; Liu, X.; Sui, B.; Liu, C.; Mo, X.; Sun, J. Development of fish collagen/bioactive glass/chitosan composite nanofibers as a gtr/gbr membrane for inducing periodontal tissue regeneration. Biomed. Mater. 2017, 12, 055004. [Google Scholar] [CrossRef] [PubMed]
- Foster, B.L.; Nagatomo, K.J.; Nociti, F.H., Jr.; Fong, H.; Dunn, D.; Tran, A.B.; Wang, W.; Narisawa, S.; Millán, J.L.; Somerman, M.J. Central role of pyrophosphate in acellular cementum formation. PLoS ONE 2012, 7, e38393. [Google Scholar] [CrossRef] [PubMed]
- Matalová, E.; Lungová, V.; Sharpe, P. Development of Tooth and Associated Structures. In Stem Cell Biology and Tissue Engineering in Dental Sciences; Academic Press: Cambridge, MA, USA, 2015; pp. 335–346. [Google Scholar]
- Foster, B.L.; Popowics, T.E.; Fong, H.K.; Somerman, M.J. Advances in defining regulators of cementum development and periodontal regeneration. Curr. Top. Dev. Biol. 2007, 78, 47–126. [Google Scholar]
- Arzate, H.; Zeichner-David, M.; Mercado-Celis, G. Cementum proteins: Role in cementogenesis, biomineralization, periodontium formation and regeneration. Periodontology 2000 2015, 67, 211–233. [Google Scholar] [CrossRef]
- Hoz, L.; Romo, E.; Zeichner-David, M.; Sanz, M.; Nuñez, J.; Gaitán, L.; Mercado, G.; Arzate, H. Cementum protein 1 (cemp1) induces differentiation by human periodontal ligament cells under three-dimensional culture conditions. Cell Biol. Int. 2012, 36, 129–136. [Google Scholar] [CrossRef]
- Bosshardt, D.D.; Schroeder, H.E. Cementogenesis reviewed: A comparison between human premolars and rodent molars. Anat. Rec. 1996, 245, 267–292. [Google Scholar] [CrossRef]
- Bar-Kana, I.; Savion, N.; Narayanan, A.; Pitaru, S. Cementum attachment protein manifestation is restricted to the mineralized tissue forming cells of the periodontium. Eur. J. Oral Sci. 1998, 106, 357–364. [Google Scholar] [CrossRef]
- Zhu, W.; Liang, M. Periodontal ligament stem cells: Current status, concerns, and future prospects. Stem Cells Int. 2015, 2015, 972313. [Google Scholar] [CrossRef] [PubMed]
- Lemaitre, M.; Monsarrat, P.; Blasco-Baque, V.; Loubières, P.; Burcelin, R.; Casteilla, L.; Planat-Bénard, V.; Kémoun, P. Periodontal tissue regeneration using syngeneic adipose-derived stromal cells in a mouse model. Stem Cells Transl. Med. 2017, 6, 656–665. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.; Chen, G.; Li, J.; Zou, Q.; Xie, D.; Chen, Y.; Wang, H.; Zheng, X.; Long, J.; Tang, W. Tooth root regeneration using dental follicle cell sheets in combination with a dentin matrix-based scaffold. Biomaterials 2012, 33, 2449–2461. [Google Scholar] [CrossRef] [PubMed]
- Crossman, J.; Elyasi, M.; Elbialy, T.; Flores, C.M. Cementum regeneration using stem cells in the dog model: A systematic review. Arch. Oral Biol. 2018, 91, 78–90. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.H.; Zhang, X.J.; Dang, N.N.; Ma, Z.F.; Xu, L.; Wu, J.J.; Sun, Y.J.; Duan, Y.Z.; Lin, Z.; Jin, Y. Apical tooth germ cell-conditioned medium enhances the differentiation of periodontal ligament stem cells into cementum/periodontal ligament-like tissues. J. Periodont. Res. 2009, 44, 199–210. [Google Scholar] [CrossRef] [PubMed]
- Owaki, T.; Shimizu, T.; Yamato, M.; Okano, T. Cell sheet engineering for regenerative medicine: Current challenges and strategies. Biotechnol. J. 2014, 9, 904–914. [Google Scholar] [CrossRef] [PubMed]
- Pedroni, A.C.F.; Sarra, G.; de Oliveira, N.K.; Moreira, M.S.; Deboni, M.C.Z.; Marques, M.M. Cell sheets of human dental pulp stem cells for future application in bone replacement. Clin. Oral Investig. 2018, 23, 2713–2721. [Google Scholar] [CrossRef] [PubMed]
- Yorukoglu, A.C.; Kiter, A.; Akkaya, S.; Satiroglu-Tufan, N.L.; Tufan, A.C. A concise review on the use of mesenchymal stem cells in cell sheet-based tissue engineering with special emphasis on bone tissue regeneration. Stem Cells Int. 2017, 2017, 13. [Google Scholar] [CrossRef]
- Iwata, T.; Yamato, M.; Tsuchioka, H.; Takagi, R.; Mukobata, S.; Washio, K.; Okano, T.; Ishikawa, I. Periodontal regeneration with multi-layered periodontal ligament-derived cell sheets in a canine model. Biomaterials 2009, 30, 2716–2723. [Google Scholar] [CrossRef]
- Iwata, T.; Washio, K.; Yoshida, T.; Ishikawa, I.; Ando, T.; Yamato, M.; Okano, T. Cell sheet engineering and its application for periodontal regeneration. J. Tissue Eng. Regen. Med. 2015, 9, 343–356. [Google Scholar] [CrossRef]
- Mao, L.; Liu, J.; Zhao, J.; Chang, J.; Xia, L.; Jiang, L.; Wang, X.; Lin, K.; Fang, B. Effect of micro-nano-hybrid structured hydroxyapatite bioceramics on osteogenic and cementogenic differentiation of human periodontal ligament stem cell via wnt signaling pathway. Int. J. Nanomed. 2015, 10, 7031. [Google Scholar] [CrossRef] [PubMed]
- Yin, Y.; Li, X.; He, X.; Wu, R.; Sun, H.; Chen, F. Leveraging stem cell homing for therapeutic regeneration. J. Dent. Res. 2017, 96, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Lane, S.W.; Williams, D.A.; Watt, F.M. Modulating the stem cell niche for tissue regeneration. Nat. Biotechnol. 2014, 32, 795. [Google Scholar] [CrossRef] [PubMed]
- Andreas, K.; Sittinger, M.; Ringe, J. Toward in situ tissue engineering: Chemokine-guided stem cell recruitment. Trends Biotechnol. 2014, 32, 483–492. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Lei, L.; Wang, S.; Nie, H. Understanding cell homing-based tissue regeneration from the perspective of materials. J. Mater. Chem. B 2015, 3, 7319–7333. [Google Scholar] [CrossRef]
- Liu, H.; Li, M.; Du, L.; Yang, P.; Ge, S. Local administration of stromal cell-derived factor-1 promotes stem cell recruitment and bone regeneration in a rat periodontal bone defect model. Mater. Sci. Eng. C 2015, 53, 83–94. [Google Scholar] [CrossRef] [PubMed]
- Tian, B.M.; He, X.T.; Xu, X.Y.; Li, X.; Wu, R.X.; Chen, F.M. Advanced biotechnologies toward engineering a cell home for stem cell accommodation. Adv. Mater. Technol. 2017, 2, 1700022. [Google Scholar] [CrossRef]
- Wu, R.-X.; Xu, X.-Y.; Wang, J.; He, X.-T.; Sun, H.-H.; Chen, F.-M. Biomaterials for endogenous regenerative medicine: Coaxing stem cell homing and beyond. Appl. Mater. Today 2018, 11, 144–165. [Google Scholar] [CrossRef]
- Carter, S.-S.D.; Costa, P.F.; Vaquette, C.; Ivanovski, S.; Hutmacher, D.W.; Malda, J. Additive biomanufacturing: An advanced approach for periodontal tissue regeneration. Ann. Biomed. Eng. 2017, 45, 12–22. [Google Scholar] [CrossRef]
- Obregon, F.; Vaquette, C.; Ivanovski, S.; Hutmacher, D.; Bertassoni, L. Three-dimensional bioprinting for regenerative dentistry and craniofacial tissue engineering. J. Dent. Res. 2015, 94, 143S–152S. [Google Scholar] [CrossRef]
- Sun, J.; Lee, Y. 3d Printing of Composition-Controlled Copolymers. Google Patent 15/702,779, 29 March 2018. [Google Scholar]
- Vaquette, C.; Fan, W.; Xiao, Y.; Hamlet, S.; Hutmacher, D.W.; Ivanovski, S. A biphasic scaffold design combined with cell sheet technology for simultaneous regeneration of alveolar bone/periodontal ligament complex. Biomaterials 2012, 33, 5560–5573. [Google Scholar] [CrossRef] [PubMed]
- Park, C.H.; Rios, H.F.; Jin, Q.; Bland, M.E.; Flanagan, C.L.; Hollister, S.J.; Giannobile, W.V. Biomimetic hybrid scaffolds for engineering human tooth-ligament interfaces. Biomaterials 2010, 31, 5945–5952. [Google Scholar] [CrossRef] [PubMed]
- Park, C.H.; Rios, H.F.; Jin, Q.; Sugai, J.V.; Padial-Molina, M.; Taut, A.D.; Flanagan, C.L.; Hollister, S.J.; Giannobile, W.V. Tissue engineering bone-ligament complexes using fiber-guiding scaffolds. Biomaterials 2012, 33, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Park, C.H.; Rios, H.F.; Taut, A.D.; Padial-Molina, M.; Flanagan, C.L.; Pilipchuk, S.P.; Hollister, S.J.; Giannobile, W.V. Image-based, fiber guiding scaffolds: A platform for regenerating tissue interfaces. Tissue Eng. Part C Methods 2013, 20, 533–542. [Google Scholar] [CrossRef] [PubMed]
- Mitsiadis, T.A.; Smith, M.M. How do genes make teeth to order through development? J. Exp. Zool. Part B Mol. Dev. Evol. 2006, 306B, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Lahann, J. Vapor-based polymer coatings for potential biomedical applications. Polym. Int. 2006, 55, 1361–1370. [Google Scholar] [CrossRef]
- Rios, H.F.; Lin, Z.; Oh, B.; Park, C.H.; Giannobile, W.V. Cell-and gene-based therapeutic strategies for periodontal regenerative medicine. J. Periodontol. 2011, 82, 1223–1237. [Google Scholar] [CrossRef]
- Vhora, I.; Lalani, R.; Bhatt, P.; Patil, S.; Patel, H.; Patel, V.; Misra, A. Colloidally stable small unilamellar stearyl amine lipoplexes for effective bmp-9 gene delivery to stem cells for osteogenic differentiation. AAPS PharmSciTech 2018, 19, 3550–3560. [Google Scholar] [CrossRef]
- Tsuchiya, S.; Chiba, M.; Kishimoto, K.; Nakamura, H.; Mitani, H. Gene transfer into periodontal tissue by in vivo electroporation. J. Dent. Res. 2002, 81, A452. [Google Scholar]
- Jin, Q.; Anusaksathien, O.; Webb, S.A.; Printz, M.A.; Giannobile, W.V. Engineering of tooth-supporting structures by delivery of pdgf gene therapy vectors. Mol. Ther. 2004, 9, 519–526. [Google Scholar] [CrossRef]
- Mah, T.F.; Pitts, B.; Pellock, B.; Walker, G.C.; Stewart, P.S.; O’Toole, G.A. A genetic basis for pseudomonas aeruginosa biofilm antibiotic resistance. Nature 2003, 426, 306–310. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Honma, K.; Evans, R.T.; Hruby, D.E.; Genco, R.J. Oral immunization with recombinant streptococcus gordonii expressing porphyromonas gingivalis fima domains. Infect. Immun. 2001, 69, 2928–2934. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Lin, J.D.; Fong, J.I.; Ryder, M.I.; Ho, S.P. The adaptive nature of the bone-periodontal ligament-cementum complex in a ligature-induced periodontitis rat model. BioMed Res. Int. 2013, 2013, 876316. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.; Wang, J.; Zhang, Y.; Liu, H.; Dong, F. Mineralization induction of gingival fibroblasts and construction of a sandwich tissue-engineered complex for repairing periodontal defects. Med. Sci. Monit. 2018, 24, 1112–1123. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.H.; Hajibandeh, J.; Suzuki, T.; Fan, A.; Shang, P.; Mao, J.J. Three-dimensional printed multiphase scaffolds for regeneration of periodontium complex. Tissue Eng. Part A 2014, 20, 1342–1351. [Google Scholar] [CrossRef] [PubMed]
- Wu, R.-X.; Yin, Y.; He, X.-T.; Li, X.; Chen, F.-M. Engineering a cell home for stem cell homing and accommodation. Adv. Biosyst. 2017, 1, 1700004. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, J.; Ruan, J.; Weir, M.D.; Ren, K.; Schneider, A.; Wang, P.; Oates, T.W.; Chang, X.; Xu, H.H.K. Periodontal Bone-Ligament-Cementum Regeneration via Scaffolds and Stem Cells. Cells 2019, 8, 537. https://doi.org/10.3390/cells8060537
Liu J, Ruan J, Weir MD, Ren K, Schneider A, Wang P, Oates TW, Chang X, Xu HHK. Periodontal Bone-Ligament-Cementum Regeneration via Scaffolds and Stem Cells. Cells. 2019; 8(6):537. https://doi.org/10.3390/cells8060537
Chicago/Turabian StyleLiu, Jin, Jianping Ruan, Michael D. Weir, Ke Ren, Abraham Schneider, Ping Wang, Thomas W. Oates, Xiaofeng Chang, and Hockin H. K. Xu. 2019. "Periodontal Bone-Ligament-Cementum Regeneration via Scaffolds and Stem Cells" Cells 8, no. 6: 537. https://doi.org/10.3390/cells8060537
APA StyleLiu, J., Ruan, J., Weir, M. D., Ren, K., Schneider, A., Wang, P., Oates, T. W., Chang, X., & Xu, H. H. K. (2019). Periodontal Bone-Ligament-Cementum Regeneration via Scaffolds and Stem Cells. Cells, 8(6), 537. https://doi.org/10.3390/cells8060537





