1. Introduction
Acute myeloid leukemia (AML) is a heterogeneous group of clonal hematopoietic neoplasms characterized by the accumulation of myeloid blasts in the bone marrow and peripheral blood. This accumulation results from a blockade of differentiation combined with enhanced proliferative capacity of myeloid precursor cells, ultimately impairing normal hematopoiesis [
1].
Despite recent advances in hematologic malignancy management, including the development of targeted and immune therapies and improved supportive care, AML outcomes remain poor. The 5-year relative survival is approximately 24%, with an incidence of 4.3 new cases per 100,000 individuals per year in the US [
2]. Several factors contribute to this unfavorable prognosis, including its higher incidence in older adults, poor chemotherapy response, high relapse rates, and limited options for relapsed disease. AML also imposes a significant clinical and financial burden due to its heterogeneity in age and genetic profile, prolonged hospitalizations, and infection-related complications. Standard first-line treatment consists of intensive chemotherapy aimed at achieving remission, followed by additional chemotherapy, radiation therapy, or stem cell transplantation [
3]. However, significant unmet clinical needs remain, such as the urgency for more effective and less toxic treatments, strategies to prevent relapse, and better support to improve patients’ quality of life [
4].
Given the urgency to identify novel therapeutic strategies, particular attention has been directed toward the diacylglycerol kinase (DGK) family, especially the DGKα and DGKζ isoforms. DGKs comprise a group of ten different cytosolic or nuclear enzymes that catalyze the phosphorylation of the lipid second messenger diacylglycerol (DAG), generating phosphatidic acid (PA). Both DAG and PA are primarily localized to cellular membranes where these lipids facilitate the activation of several proteins, such as protein kinase C, RAS activators, the mammalian target of rapamycin, and various tyrosine kinases. Through these interactions, DAG and PA act as dynamic second messengers regulating proliferation, survival, motility, and metabolic activity [
5,
6,
7]. Dysregulation of DAG/PA lipid signaling has been implicated in several human disorders, including cancer [
8,
9]. Among the ten DGK-encoding genes, DGKA and DGKZ, which code for DGKα and DGKζ proteins, respectively, are the most extensively investigated owing to their central involvement in regulating immune responses, cancer immunotolerance, and tumorigenesis [
10,
11].
Several lines of evidence point to a relevant role for DGKs in AML. Indeed, analyses of cancer databases, including The Cancer Genome Atlas, have revealed DGKα, DGKγ, DGKδ, DGKε, and DGKζ overexpression in AML, although without a clear correlation to specific subtypes. High expression of DGKα is associated with poor overall survival, whereas elevated DGKγ appears to be linked to a more favorable prognosis. Interestingly, the Beat-AML dataset showed that bone marrow cells express all DGK isoforms at very high levels, which often exceeded those observed in tumor samples, suggesting that DGKs expression may increase during hematopoietic differentiation [
12]. Moreover, overexpression of DGKα in human bone marrow AML samples compared to normal samples, has been associated with poor clinical outcomes, suggesting a possible oncogenic role [
12,
13]. Among DGK isoforms, α and especially ζ exhibit frequent alterations in leukemic cell lines where they play distinct functional roles. For instance, in Kasumi-1 and KG-1α AML cell lines, treatment with the DGKα-specific inhibitor ritanserin resulted in significant inhibition of the phospholipase D–PA–sphingosine kinase 1 axis, suppression of the JAK–STAT and MAPK pathways, and downregulation of PARP, caspase-3, MCL1, and Bcl-xL. Ritanserin exerted cytotoxic effects on both cell lines, with half maximal inhibitory concentration (IC
50) values of 51 μM and 38 μM, respectively, after 24 h, and 30 μM and 26 μM after 72 h. Similarly, treatment of bone marrow mononuclear cells from primary AML samples with 40 μM ritanserin induced apoptosis in up to 70% of cells, whereas apoptosis in normal hematopoietic stem cell samples remained below 30%.
Collectively, these findings suggest that ritanserin reduces AML cell viability through a complex mechanism involving DGKα inhibition, signaling pathway downregulation, and caspase-dependent apoptosis. Congruently, in xenograft mouse models injected with Kasumi-1, ritanserin administration led to a significant reduction in tumor burden and improved survival [
13]. Conversely, in HEL and HL-60 cells, the DGKα-specific inhibitors CU-3 and AMB639752 did not significantly affect viability, whereas the ritanserin-related inhibitors R59022 and R59949 induced marked cytotoxicity after 24 h, with IC
50 values of 32 μM and 72 μM, respectively, in HL-60 cells, and 49 μM and 80 μM, respectively, in HEL cells [
12]. In K562 cells, DGKα translocates into the nucleus during both the G
1 and G
2 phases of the cell cycle, and its presence is required for efficient cell cycle progression. Inhibition or silencing of DGKα in these cells reduced proliferation and altered nuclear morphology, supporting a direct role for this isoform in mitotic regulation [
14].
RAS-mutation in AML cells alters lipid metabolism and promotes DGKζ overexpression, suggesting an additional role for this isoform [
15]. Consistently, knockdown of DGKZ via RNA interference in HL-60 cells induced significant apoptosis and G
2/M phase arrest, accompanied by MAPK pathway downregulation, suppression of the anti-apoptotic protein survivin, and activation of caspase-3 and caspase-9 [
16].
Given the persistent clinical challenges and biological heterogeneity of AML, this study aimed to expand upon the fragmented data present in the literature on the roles of DGKα and DGKζ in leukemic cell biology. To this end, two complementary approaches were employed: (i) the use of newly developed isoform-specific inhibitors; and (ii) transient siRNA-mediated silencing across a panel of four well-established, yet biologically distinct, cell line models relevant to AML research. This combined strategy enabled a comprehensive assessment of their effects on cell viability, apoptosis/necrosis, and global proteomic profiles, thus providing mechanistic insights extending beyond those reported so far.
To reflect AML heterogeneity, four distinct models were selected. HL-60 cells, derived from acute promyelocytic leukaemia [
16], were chosen due to their strong differentiation potential along the myeloid lineage [
17,
18,
19,
20,
21]. HEL cells, established from a case of erythroleukemia, were included for their erythroid characteristics and presence of relevant driver mutations, making them suitable for modeling pure erythroid leukaemia [
22]. THP-1 cells, obtained from acute monocytic leukaemia, harbor the typical t (9;11) translocation and reproduce chemoresistant and invasive phenotypes [
23]. Upon stimulation they can differentiate into macrophage-like cells [
24], providing a model to investigate DGK functions in monocyte-to-macrophage transition. Finally, K562 cells, although originally derived from chronic myeloid leukemia (CML), were included because of their frequent use in AML research owing to their conserved myeloid properties and ability to differentiate towards erythroid or megakaryocytic lineages under specific treatments [
25,
26,
27].
In the rapidly growing field of DGKα inhibitors, ritanserin was selected as a reference compound. Ritanserin is a synthetic compound initially developed as a selective antagonist of serotonin 5-HT
2A and 5-HT
2C receptors, with an inhibition constant (Ki) of 0.45 nM and 0.71 nM, respectively [
28]. Although never approved for clinical use, it has been tested in clinical trials at doses ranging from 1 to 30 mg, and its favorable oral bioavailability and tolerability in early trials have maintained its relevance in research [
29,
30]. Besides its serotonergic activity, ritanserin has been identified as a potent and selective inhibitor of DGKα [
31,
32].
To evaluate the effects of DGKζ inhibition on AML cell viability, two selective inhibitors were used: DGKζ-IN-4 and BAY 2965501. DGKζ-IN-4, a heteroaryl carboxamide compound, has been reported as a potent and selective inhibitor of DGKζ with an IC
50 of 0.4 nM while also increasing IL-2 release by T cells by 10-fold in the nanomolar range (Watanabe et al. Patent WO2022114164). BAY 2965501, another DGKζ-selective inhibitor, showed in vitro activity by increasing natural killer (NK)- and T-cell-mediated tumor cell killing and enhancing IL-2-induced NK cell activation. In syngeneic murine tumor models, oral administration of BAY 2965501 improved T cell efficacy, reactivated exhausted T cells, and reduced tumor growth [
33,
34]. Currently, BAY 2965501 is undergoing a first-in-human Phase I clinical trial to evaluate its safety, tolerability, pharmacokinetics, pharmacodynamics, best dosage and preliminary efficacy in patients with advanced solid tumors (Clinical trial ID NCT05614102
https://www.clinicaltrials.gov/study/NCT05614102, accessed on 20 September 2025).
2. Materials and Methods
2.1. Cell Lines and Culture Conditions
The HL-60 cell line was derived in 1976 from the peripheral blood of a 36-year-old woman diagnosed with acute promyelocytic leukemia [
17]. HL-60 cells exhibit multipotentiality and can differentiate along various myeloid lineages: upon treatment with phorbol esters (DAG analogues), they differentiate into macrophage-like cells in a process counteracted by DGKγ [
18,
19], while exposure to vitamin D
3 induces monocytic differentiation [
20] and dimethyl sulfoxide (DMSO) promotes granulocyte differentiation in a DGKα-dependent manner [
21].
The HEL cell line originated in 1980 from the peripheral blood of a 30-year-old man who experienced a relapse of erythroleukemia following treatment for Hodgkin lymphoma. HEL cells are positive for KIT, harbor TP53 mutations, and express high level of glycophorin A, making them a model for pure erythroid leukemia [
22].
The THP-1 cell line was obtained from the peripheral blood of a 1-year-old male patient with acute monocytic leukemia. THP-1 cells serve as a model of this AML subtype, as they harbor the typical t (9;11) (p21.3;q23.3) translocation, which generates the AF9-MLL fusion protein that promotes expression of genes involved in epithelial–mesenchymal transition and confers chemoresistant and invasive phenotypes [
23]. Upon stimulation with phorbol esters, THP-1 cells cease proliferation, become adherent, and differentiate into macrophage-like cells [
24].
The K562 cell line was derived from the pleural effusion of a 53-year-old woman in the terminal blast crisis phase of CML. Although K562 cells presents the Philadelphia chromosome containing the BCR-ABL1 fusion gene, they are widely utilized in AML research due to their myeloid characteristics and their ability to differentiate toward erythroid or megakaryocytic lineages under specific treatments [
25,
26,
27].
These four cell lines were employed in this study as in vitro models of AML, cell line identity was verified through a Cell Line Authentication Test conducted by Eurofins Genomics (Ebersberg, Germany) or by the internal university service. The resulting markers matched 100% with those reported in the ATCC database. Notably, an additional K562 clone, described in
Supplementary Figure S8 and kindly provided by Prof. L. Manzoli (Bologna, Italy), is reported as K562-related, differing from K526 by a single marker. Cells were cultured in RPMI-1640 medium (ThermoFisher Scientific, Waltham, MA, USA) supplemented with 10% heat-inactivated fetal bovine serum (FBS) and 1% penicillin-streptomycin, following the handling protocols provided by ATCC (Manassas, VA, USA). Additionally, healthy donor blood samples were provided by the UPO biobank under approved Ethical Committee authorization (Comitato Etico Interaziendale A.O.U. Maggiore della Carità 865/CE-CE206/2022 date 24 October 2022) and with informed consent for research use. Peripheral blood mononuclear cells were isolated by density gradient centrifugation using Ficoll-Paque PLUS (GE 14 Healthcare, Chicago, IL, USA), washed, and resuspended at a concentration of 2 × 10
6 cells/mL in RPMI-1640 medium containing 10% heat-inactivated FBS. Peripheral blood lymphocytes (PBLs) were selected by the treatment with 1 μg/mL anti-CD3 (clone OKT3) and anti-CD28 (clone CD28.2) human antibodies for 72 h. Activated T cells were then cultured in complete medium supplemented with 100 IU/mL recombinant human IL-2 (rhIL-2, PeproTech, Cranbury, NJ, USA) at a density of 0.5 × 10
6 cells/mL.
2.2. Cell Viability Assays
The alamarBlue assay was performed to assess cell viability in presence of chemical inhibitors. A total of 50,000 cells per well were seeded in a 96-wells plate in a volume of 100 μL of complete medium together with 10 μL of 10× concentrated inhibitor solution and then incubated for either 24 or 72 h. Each experimental condition was performed in technical quadruplicates, using cells treated with equal amounts of DMSO vehicle as control and medium alone as background. After incubation, alamarBlue was added to each well at a final concentration of 0.15 mg/mL. The fluorescence of the samples was measured 24 h later using a Spark 10 M Multimode Plate Reader (Tecan, Switzerland) with excitation and emission wavelengths of 535 nm and 590 nm, respectively. For dose–response curve fitting, fluorescence values were normalized according to the following formula:
Data are the results of at least five independent experiments analyzed with GraphPad Prism 10 as [inhibitor] vs. normalized response curve (variable slope, after manual outlier removal).
To determine the type of cell death, apoptotic and necrotic cells were detected by flow cytometry using the Apoptosis Detection Kit Annexin V-FITC (Invitrogen, Carlsbad, CA, USA). For each sample, 500,000 cells, pretreated for 24 h, were stained according to manufacturer’s instructions, using 7-aminoactinomycin D (7AAD) instead of propidium iodide. Samples were analyzed on a BD FACS Symphony A5 flow cytometer (Franklin Lakes, NJ, USA) using BD FACSDiva 9.1 software. Data were gated based on FSC-A vs. FSC-H to exclude cell doublets and FSC-A vs. SSC-A to exclude debris. Different populations were identified as: live (Annexin V− and 7AAD−), necrotic (Annexin− and 7AAD+), early apoptotic (Annexin V+ and 7AAD−) and late apoptotic (Annexin+ and 7AAD+). Data are shown as mean ± SD of at least three independent experiments analyzed by GraphPad Prism 10 (control vs. [inhibitor]).
To assess cell viability, trypan blue exclusion assays were performed on transfected HL-60, HEL, THP-1, and K562 cells. Trypan blue reagent was added to samples (1:1 v/v), and the number of live/dead cells was automatically recorded by the Automatic counter TC20 (Invitrogen). Each experiment was performed in triplicate. Results are reported as both the total number of live and dead cells from a representative experiment and as the percentage of cell viability averaged from three biological replicates. All data were graphed and analyzed using GraphPad Prism 8 through one-way ANOVA and unpaired t-test.
2.3. Silencing
To achieve DGKA and DGKZ silencing, HL-60, HEL, THP-1, and K562 cells were electroporated with 80 nM of siRNA using Neon™ 100 µL Kit (MPK10025, Invitrogen) with Neon™ electroporator (ThermoFisher Scientific, Waltham, MA, USA) under the conditions reported in
Table 1. All siRNAs used are listed in the
Supplementary Table S2.
After siRNA transfection, cells were resuspended in RPMI-1640 medium with 10% heat inactivated FBS without streptomycin and penicillin and incubated for 72 h at 37 °C in 5% CO2. Following incubation, silencing efficiency was evaluated for each experiment by RT-PCR and Western blot, after which cells were used for viability assays.
2.4. Quantitative Real-Time PCR
Transfected cells were lysed in 200 µL of nuclease-free water supplemented with 2% thioglycerol. Total RNA was extracted from lysates by Kingfisher automated nucleic acid extractor (Thermo Fisher Scientific, Waltham, MA, USA with the MVP_2WASH_200_FLEX protocol and the MagMAXTM Viral/Pathogen Nucleic Acid Isolation Kit (Thermo Fisher) and then quantified using NanoDrop (Thermo Fisher). Subsequently, equal amounts of RNA were retrotranscribed into cDNA using the High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher) following the manufacturer’s instructions. The relative expression of DGK isoforms (DGKA Assay ID Hs00176278_m1, DGKZ Assay ID Hs05025727_m1) was assessed by quantitative real-time PCR (qRT-PCR) using TaqMan technology. Glucuronidase beta (GUSB Assay ID Hs00939627_m1) served as the internal reference gene. qRT-PCR was performed in a 384-well plate according to the TaqMan™ Fast Advanced Master Mix kit (Thermo Fisher), using 4 µL of mix and 1 µL of cDNA and run on a Bio-Rad CFX384TM (Bio-Rad, Hercules, CA, USA) real-time PCR system. The amplification protocol consisted of an initial denaturation at 95 °C for 20 s, followed by 50 cycles of denaturation at 95 °C for 3 s and annealing/extension at 60 °C for 30 s. The qPCR reactions were performed in technical triplicates. Data were analyzed with Bio-Rad CFX Maestro 4.1.2433.1219 software, using GUSB as reference and normalizing DGKA and DGKZ expression to the corresponding siRNA control.
2.5. Western Blotting
Cells were lysed in buffer containing HEPES 25 mM, NaCl 150 mM, EDTA 5 mM EGTA 1 mM NP40 1%, and glycerol 10%, supplemented with sodium orthovanadate (1 mM, Thermo Fisher) and protease inhibitor cocktail (0.0089 mg/mL, Sigma Aldrich, St. Louis, MO, USA). Samples were incubated for 15 min at 4 °C, under gentle, constant shaking, and then centrifuged at 12,000× g for 15 min at 4 °C. The concentrations of proteins in lysates were quantified by Qubit Protein BR Assay Kit (A50669, Thermo Fisher Scientific, Waltham, MA, USA) according to the manufacturer’s instructions. Equal amounts of proteins were separated on SDS–PAGE gels and subsequently transferred onto polyvinylidene fluoride (PVDF) membranes. Membranes were then blocked with 3% (w/v) BSA for 1 h at room temperature and incubated overnight at 4 °C with the appropriate primary antibodies under gentle agitation. The following day, membranes were washed 3 times in TBS-T buffer and then incubated for 1 h at room temperature with HRP-conjugated rabbit or mouse secondary antibodies (1:5000) under gentle agitation. After three additional washes with TBS-T, the membranes were developed using the Western Chemiluminescence Substrate (PerkinElmer, Shelton, CT, USA) and visualized with the ChemiDoc™ Imaging System (Bio-Rad, Hercules, CA, USA). Band intensities were quantified by densitometry using Bio-Rad Image Lab 6.1 software, normalized to β-actin, and further normalized to the respective siRNA controls. Finally, results were analyzed and graphed using GraphPad Prism 8 with one-way ANOVA and unpaired t-test.
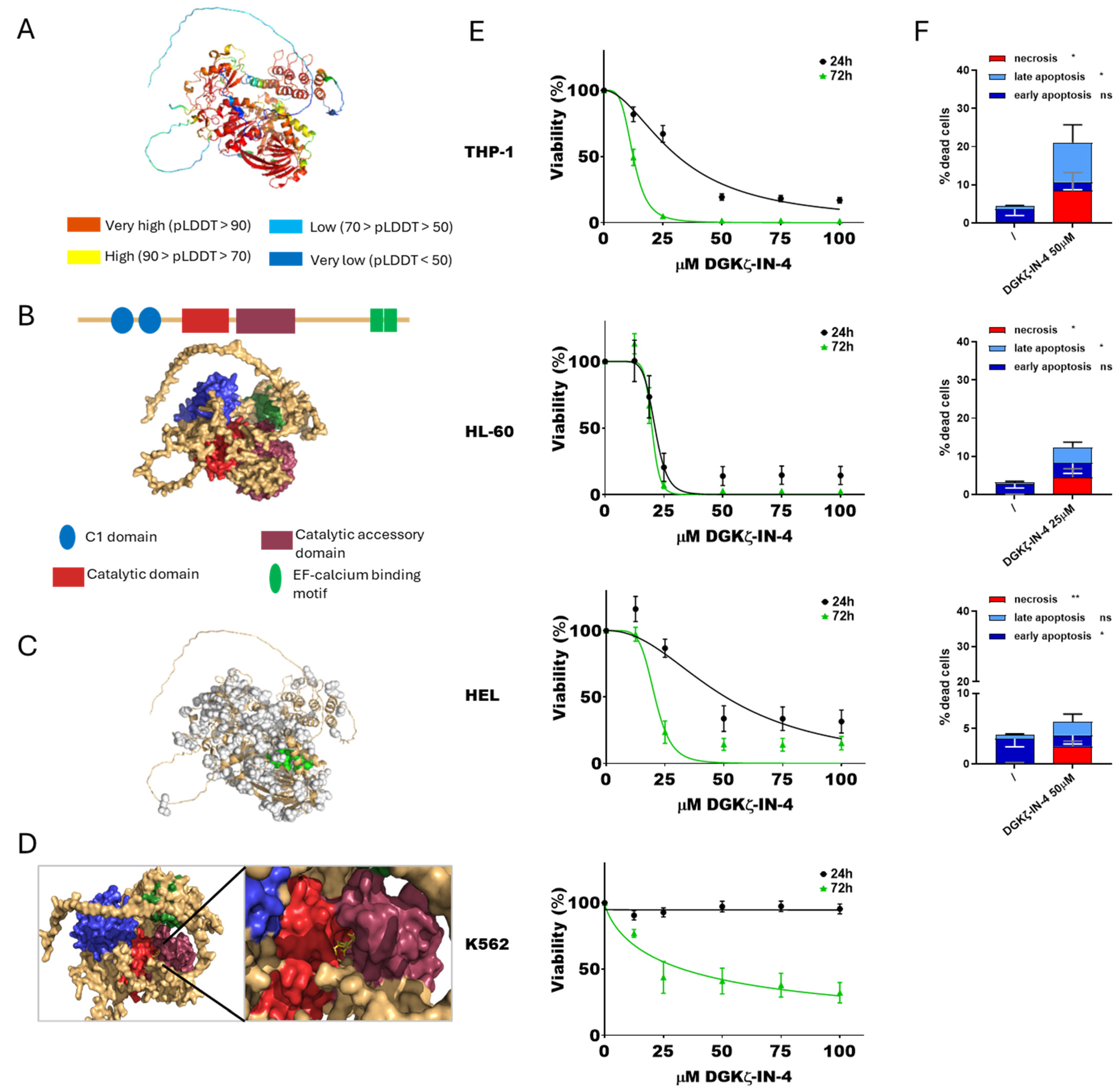
2.6. Simulations
All computational analyses were performed on a Tesla workstation equipped with two Intel Xeon X5650 2.67 GHz processors and running Ubuntu 20.04 (
http://www.ubuntu.com). Preliminary information on the full-length human DGKα (735 amino acids, UniProt ID: P23743) and DGKζ (928 amino acids, UniProt ID: Q13574) sequences was obtained from the UniProt database (
https://www.uniprot.org/) [
35]. Since the complete resolved structures are not yet available, predicted models generated by AlphaFold [
36,
37] (AF-P23743-F1-v4 and AF-Q13574-F1-v4) were analyzed. The predicted protein structures were visualized using PyMOL (version 3.1.4.1), with structural domains annotated according to the Simple Modular Architecture Research Tool (SMART, version 9.0
https://smart.embl.de/, accessed on 5 March 2024) [
38].
Potential ligand-binding pockets were then identified using FPocketWeb [
39] (
https://durrantlab.pitt.edu/fpocketweb/, accessed on 5 March 2024), focusing on putative pockets located near the catalytic sites of each isoform for further analysis. Molecular docking analyses were then performed using AutoDock Vina—Smina version 15 October 2019. based on AutoDock Vina 1.1.2. [
40,
41]. The docking procedure employed the PDB structure of each protein, the selected binding pocket as the target site, and a known inhibitor—provided as a SMILES strings—as ligands. The top-ranked docking poses corresponding to the inhibitor and the respective binding pocket were finally reassembled in PyMOL for structural visualization. In details, the ritanserin–pocket 56 complex was analyzed for DGKα, while the BAY 2965501 and DGKζ-IN-4 ligands were docked within pocket 65 of DGKζ.
2.7. Proteomics
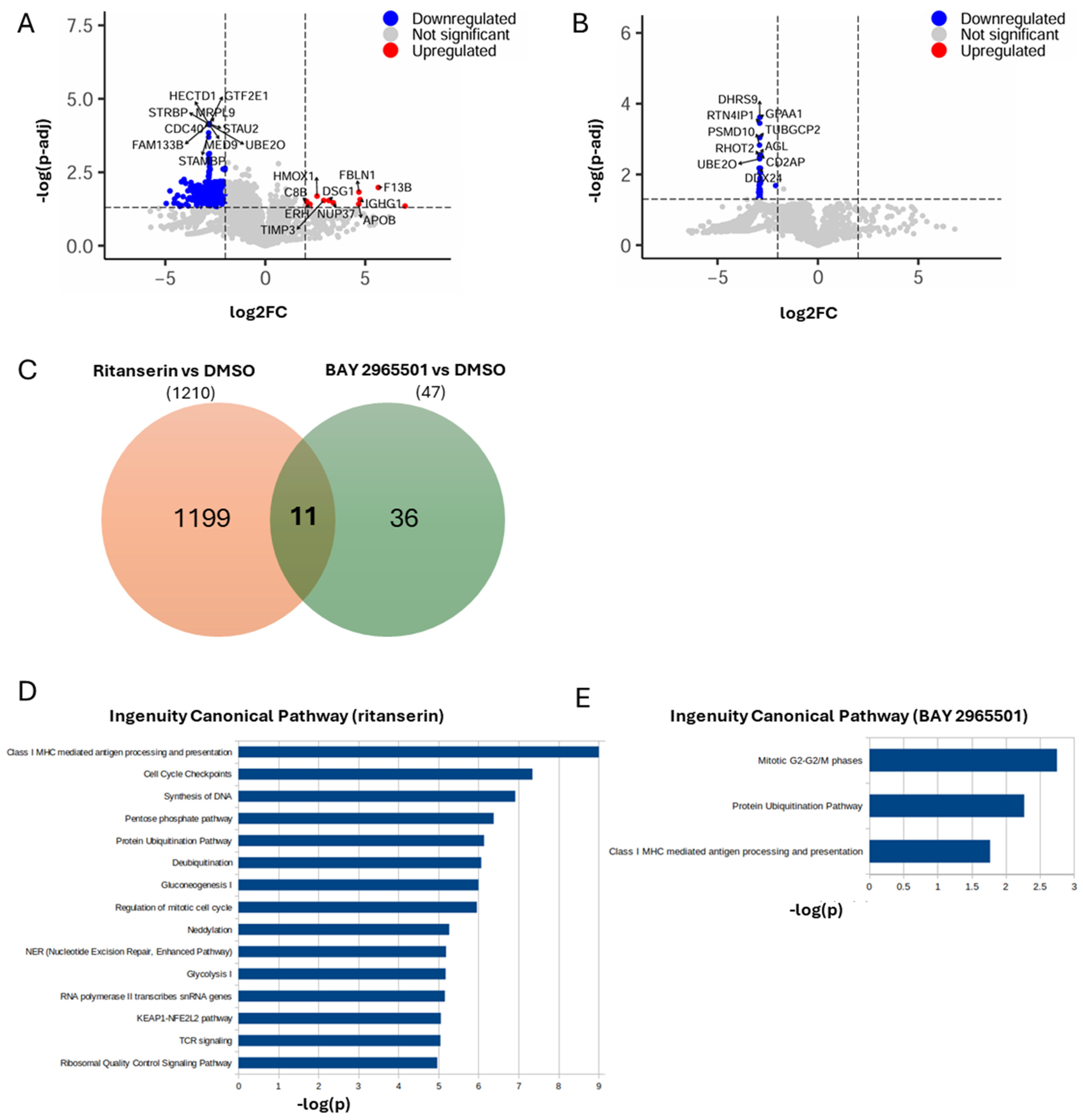
Cells were lysed in RIPA buffer and sonicated. Proteins were precipitated with cold acetone, pelleted, and resuspended. Reduction was carried out in 25 µL of 100 mM NH4HCO3 with 2.5 µL of 200 mM DTT (Merck, St. Louis, MO, USA) at 60 °C for 45 min, followed by alkylation with 10 µL of 200 mM iodoacetamide (Merck, St. Louis, MO, USA) for 1 h at room temperature in the dark. Excess iodoacetamide was quenched by adding 200 mM DTT. Proteins were then digested with trypsin, dried by SpeedVac, and desalted. Peptides were analyzed on an Ultimate 3000 RSLCnano system coupled to an Orbitrap Exploris 480 equipped with FAIMS (all from Thermo Fisher Scientific). Samples were loaded onto a reversed-phase C18 column (15 cm × 75 µm i.d., Thermo Fisher Scientific) and eluted at 500 nL min−1 using a 6–95% solvent B gradient over 41 min, followed by 1 min of re-equilibration at 6% B. Data were acquired in positive mode with a spray voltage of 2500 V and FAIMS in standard resolution at a compensation voltage of −45 V. Data-independent acquisition (DIA) was performed with a precursor m/z range of 400–900, using 8 m/z isolation windows with 1 m/z overlap, HCD collision energy of 27%, Orbitrap resolution of 30,000, RF Lens 50%, normalized AGC target 1000, maximum injection time 25 ms, and 1 microscan. DIA data were processed with DIA-NN (v1.8.1) in library-free mode, applying deep-learning prediction for spectra, retention times, and ion mobility. Searches assumed Trypsin/P specificity, precursor charges 1–4, peptide lengths of 7–30 amino acids, and precursor m/z values of 400–900, allowing up to two missed cleavages. Carbamidomethylation of Cys was set as a fixed modification; Met oxidation was set as a variable modification (maximum two per peptide). The false discovery rate was maintained at 1%.
Normalized data from two independent proteomic experiments were obtained, each comparing a treatment condition to DMSO: (1) ritanserin vs. DMSO and (2) BAY 2965501 vs. DMSO. For each condition, three biological replicates were analyzed.
Protein abundance differences were calculated separately for each treatment relative to DMSO using a
t-test, generating log
2 fold change (log
2FC) and adjusted
p-values (
p-adj). All proteins identified by UniProt ID were annotated with the corresponding gene symbol using QIAGEN Ingenuity Pathway Analysis (IPA; QIAGEN Inc.,
https://digitalinsights.qiagen.com/IPA, accessed on 5 June 2025). Proteins lacking a gene symbol were annotated as NA [
42].
Data were filtered to include only proteins with |log2FC| > 2 and p-adj < 0.05, and retaining those annotated with a gene symbol. This resulted in 1210 differentially abundant proteins for the ritanserin vs. DMSO condition and 47 for BAY 2965501 vs. DMSO.
Volcano plots were generated for each treatment using the EnhancedVolcano package in R (
https://bioconductor.org/packages/EnhancedVolcano, accessed on 12 June 2025), showing upregulated proteins in red and down-regulated proteins in blue, with labels for the ten most significantly modulated proteins. A Venn diagram was created to depict the overlap of differentially abundant proteins shared between the two treatments. These proteins, along with their gene symbols and log
2FC values, were then used as input for IPA Core Analysis. The following filters were applied: human species and reference tissues/cells (hematopoietic progenitor cells, macrophages, monocytes, peripheral blood monocytes, and THP1 leukemic cells) [
42]. The resulting Ingenuity Canonical Pathways were downloaded using standard filters and further refined to consider only those with a |Z-score| > 1. For ritanserin vs. DMSO, the top 15 most significant pathways were represented in a bar plot, while for BAY 2965501 vs. DMSO, only three significant pathways were identified and plotted.
4. Discussion
AML remains a major therapeutic challenge, highlighting the need for novel, effective treatments and the identification of new molecular targets. DGKα and DGKζ play critical roles in regulating a number of tumorigenic processes as well as in modulating the immune response to tumors [
50,
51,
52,
53,
54]. Inhibition of these isoforms has been shown to induce antitumor effects in AML cell models, including reduced cell viability, cell cycle arrest, induction of apoptosis, and promotion of differentiation [
12,
13,
14,
16]. In this study, four representative cell line models relevant to AML research (i.e., HL-60, HEL, THP-1 and K562) were selected to determine the relevance of DGKα and DGKζ in AML cell viability using both isoform-specific chemical inhibitors and siRNA-mediated gene silencing.
R59949, R59022, and ritanserin constitute a family of structurally related DGKα specific inhibitors that bind within a pocket formed by the C1 and catalytic domains [
32,
55]. These inhibitors have been shown to decrease AML cell viability both in vitro and in vivo [
12,
13]. Here, a binding mode for ritanserin within the DGKα catalytic domain was proposed based on molecular simulations, and cytotoxicity experiments were extended to additional AML cell models. Consistent with previous studies, ritanserin reduced cell viability across all selected AML models tested, with THP-1 being the most sensitive (IC
50 ≈ 37 μM), followed by HL-60 (IC
50 ≈ 38 μM) and HEL (IC
50 ≈ 49 μM), while K562 cells were more resistant (IC
50 ≈ 70 μM). Additionally, the effects of ritanserin increased with prolonged exposure, showing clear dose- and time-dependent toxicity characterized by a significant increase in apoptosis without evidence of necrosis. Notably, untransformed but IL-2 stimulated proliferating PBLs exhibited complete cell death at a ritanserin concentration of 50 μM, consistent with the known role of DGKα downstream of IL-2 signaling [
56]. These observations suggest that ritanserin cytotoxicity is not restricted to AML cells and that, at concentrations required to induce AML cell death, it may exert broader toxic effects in proliferating cells [
57].
The mechanisms underlying ritanserin-induced cell death in AML are only partially understood. Previous studies have shown that ritanserin downregulates key signaling molecules, including sphingosine kinase 1, JAK–STAT, MAPK, PARP, caspase-3, MCL1, and Bcl-xL in Kasumi-1 and KG-1α (AML) cell lines [
13]. In this study, proteomic profiling of THP-1 cells treated with ritanserin at near-IC
50 concentrations confirmed a global downregulation of proteins, such as PARP, caspase-3, MAPK, JAK, and STAT, consistent with previous findings [
13]. Functional enrichment analysis revealed that ritanserin treatment led to suppression of pathways involved in MHC I-mediated antigen processing and presentation, cell metabolism, cell cycle progression, DNA synthesis, and nucleotide excision repair. These alterations are in line with the molecular signatures of growth-arrested and apoptotic cells.
Since ritanserin is also known as a potent serotonin receptors antagonist, AML cells were treated with increasing amounts of altanserin, risperidone, and metoclopramide, three selective and strong serotonin/dopamine receptors antagonists. These compounds produced negligible effects on AML cell viability, with the greatest reduction (11%) observed following treatment with 100 μM metoclopramide. Therefore, ritanserin-induced cytotoxicity is unlikely to be mediated through serotonergic signaling, supporting a specific effect on DGKα inhibition.
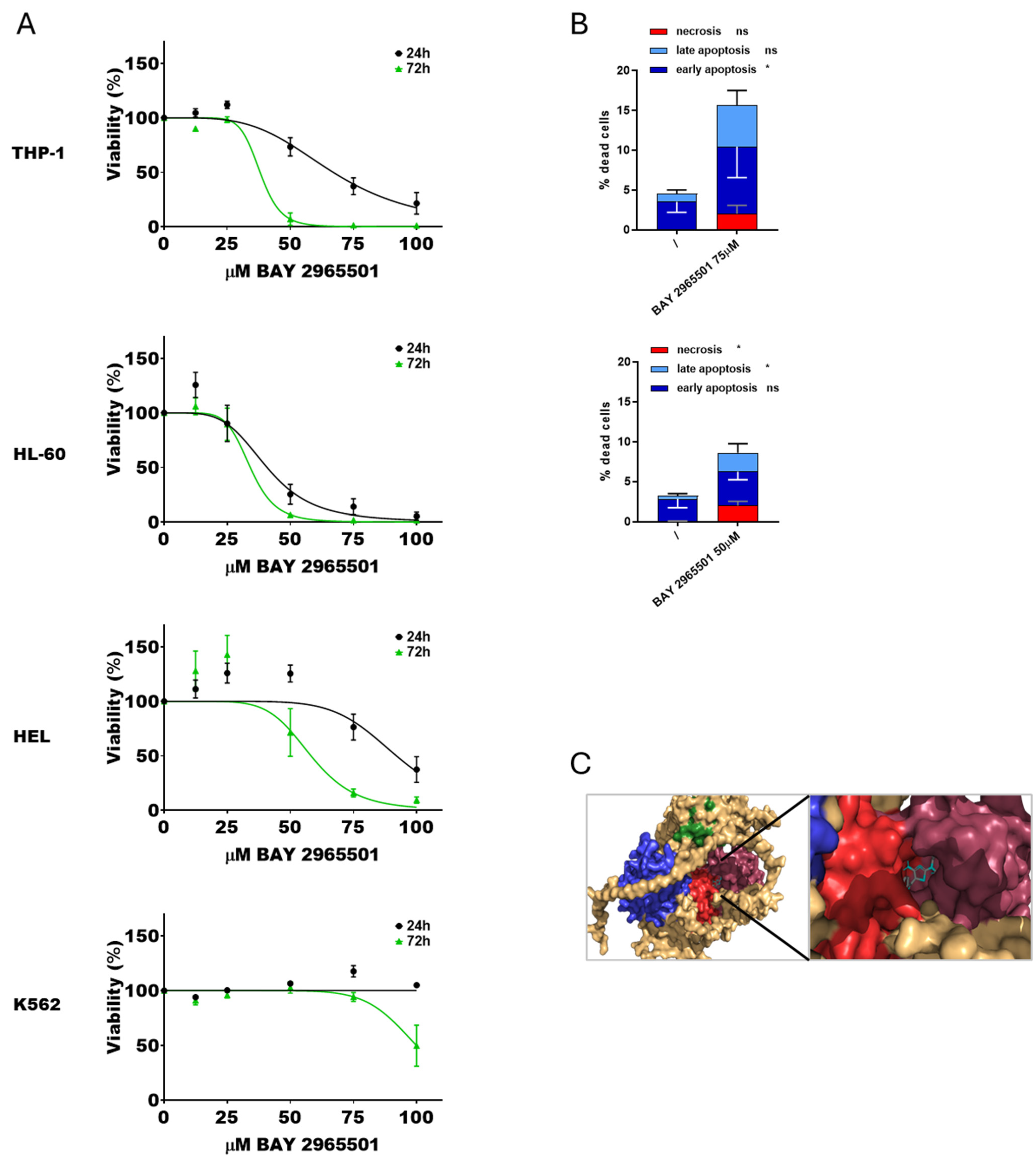
To specifically target DGKζ activity, newly developed isoform-specific inhibitors recently reported in patents were employed. DGKζ-IN-4 is a selective inhibitor of DGKζ active in the nanomolar range and proposed as a potential therapeutic agent for cancer associated with immune cell activation or resistant to anti-PD-1 antibody/anti-PD-L1 antibody therapy (Watanabe et al. Patent WO2022114164). Similarly to ritanserin, DGKζ-IN-4 reduced cell viability in some of the selected AML models, with HL-60 being the most sensitive (IC50 = 21 μM), followed by THP-1 (IC50 = 31 μM) and HEL (IC50 = 51 μM), while K562 showed no detectable cytotoxic effects across the tested concentration range at 24 h and mild sensitivity after prolonged exposure (IC50 = 33 μM at 72 h). These results are the first available data on a DGKζ inhibitor in AML cell lines and support its potential application in this tumor type. However, PBLs from healthy donors were also sensitive to this drug with an IC50 of 29 μM after 24 h of exposure, indicating potential general toxicity. Apoptosis and necrosis assays revealed that DGKζ-IN-4 treatment induced a statistically significant increase in both apoptotic and, unexpectedly, necrotic cell death.
As this inhibitor is still poorly characterized, a second molecule, BAY 2965501, was also evaluated. This compound is known to inhibit DGKζ in vitro with an IC
50 of 76 nM, as judged by ADP-Glo assays [
58], and is reported to be highly selective for DGKζ. It is currently undergoing a phase I clinical trial in patients with advanced non-small cell lung cancer, gastric and esophagogastric junction adenocarcinoma, clear cell renal cell carcinoma, and melanoma [
33,
34] (Clinical trial ID NCT05614102
https://www.clinicaltrials.gov/study/NCT05614102, accessed on 20 September 2025). BAY 2965501 reduced cell viability in a subset of AML models with HL-60 being the most sensitive (IC
50 of ≈41 μM), followed by THP-1 (IC
50 of ≈67 μM), whereas HEL and K562 cells were resistant to this drug, with minimal cytotoxic effects. PBLs from healthy donor showed IC
50 values of 77.1 ± 4.8 μM at 24 h and 35.2 ± 0.7 μM at 72 h (
Figure 2), indicating that this inhibitor also affects untransformed cells at concentrations required to induce AML cytotoxicity. Apoptosis and necrosis assays confirmed that BAY 2965501 treatment induced a statistically significant increase in both apoptotic and necrotic cell death across sensitive AML cell lines, similarly to what observed with DGKζ-IN-4. Interestingly, molecular docking and dynamics simulations indicated that, despite their distinct chemical structures, DGKζ-IN-4 and BAY 2965501 may bind to the same catalytic domain pocket of DGKζ (
Figure 2 and
Figure 3). In future, these data could be complemented by the establishment of cell lines resistant to DGK inhibitors to study the potential resistance mechanisms.
To investigate the pathways modulated by BAY 2965501, THP-1 cells were treated with concentrations near to the estimated IC
50, and the effects on the cellular proteome were analyzed. A limited number of proteins (47) were downregulated, comprising small G-protein regulators and proteins involved in protein trafficking and turnover (
Figure 4B). These changes mainly affected three biological pathways: (i) the mitotic G
2-G
2/M phases; (ii) the protein ubiquitination pathway; and (iii) class I MHC mediated antigen processing and presentation. Even though most of the regulated proteins differed between ritanserin and BAY 2965501 treatments, these three pathways were among the most significantly modulated by both inhibitors, indicating that DGKα and DGKζ inhibition influences similar biological functions through different pathways.
The sensitivity to DGK inhibitors varied considerably among AML cell lines, highlighting the need to identify predictive biomarkers that could guide patient selection. Correlation analyses between IC
50 values and DGKs expression at both mRNA and protein levels revealed no significant direct associations, indicating that DGK isoforms abundance is not the main determinant of inhibitor sensitivity and cannot be used for patient-tailored therapy. In previous reports [
12], DGK isoforms overexpression was not associated with specific AML subtypes, although it may be associated with the occurrence of specific mutations, such as those leading to aberrant Ras pathway activation [
15]. These findings underscore the need for further studies to clarify the role of DGKs in a heterogeneous disease like AML.
In agreement with earlier studies [
12,
13,
14], DGK inhibitors effectively decreased AML cell viability in the high micromolar range. However, it will be necessary to extend this study to patient samples which could provide important insights into the roles of these enzymes in malignant cells compared to untransformed controls. Indeed, IL-2 stimulated proliferating PBLs also showed reduced viability, suggesting that the concentrations required to trigger AML cytotoxicity may also affect untransformed cells, limiting their potential therapeutic use. Both DGKα and DGKζ inhibitors are known to enhance immune responses [
50,
52], thus achieving a dual effect: direct tumor growth suppression and stimulation of immunosurveillance [
10,
11]. Considering the complexity and immunological activity of the tumor microenvironment, this dual action may lead to improved therapeutic efficacy at lower doses in vivo. Whether isoform-specific inhibition is advantageous in this setting or whether dual DGKα/ζ inhibition might be more beneficial remains to be determined [
12,
51]. Moreover, these molecules could be explored in combination with existing chemotherapeutic regimens or as adjuvants to improve the efficacy and persistence of CAR-T cells therapies, which are already approved for acute lymphoblastic leukemia and currently under clinical investigation in AML [
59]. In addition the development of an efficient delivery system to enhance compound uptake in tumor cells could improve their efficacy.
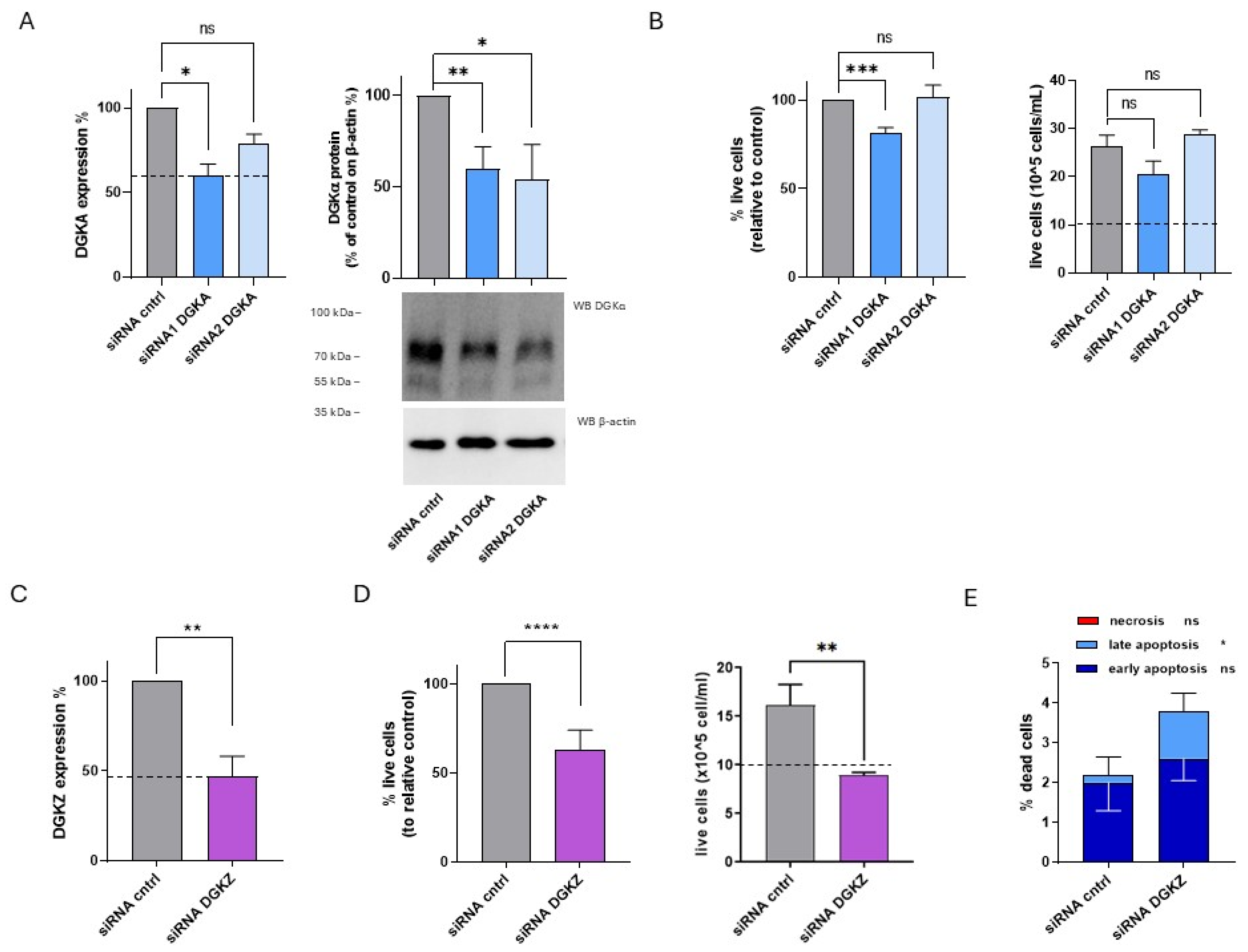
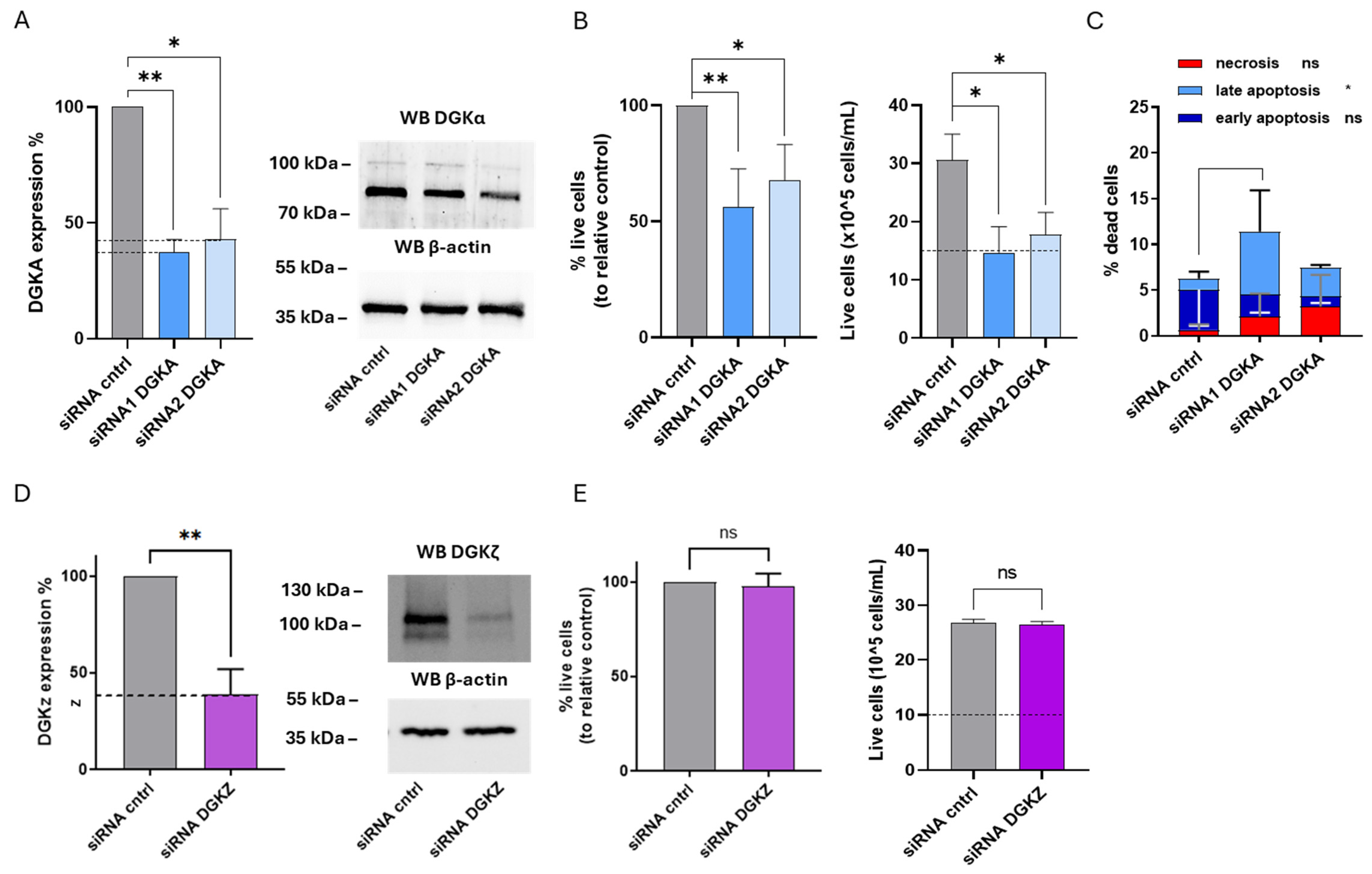
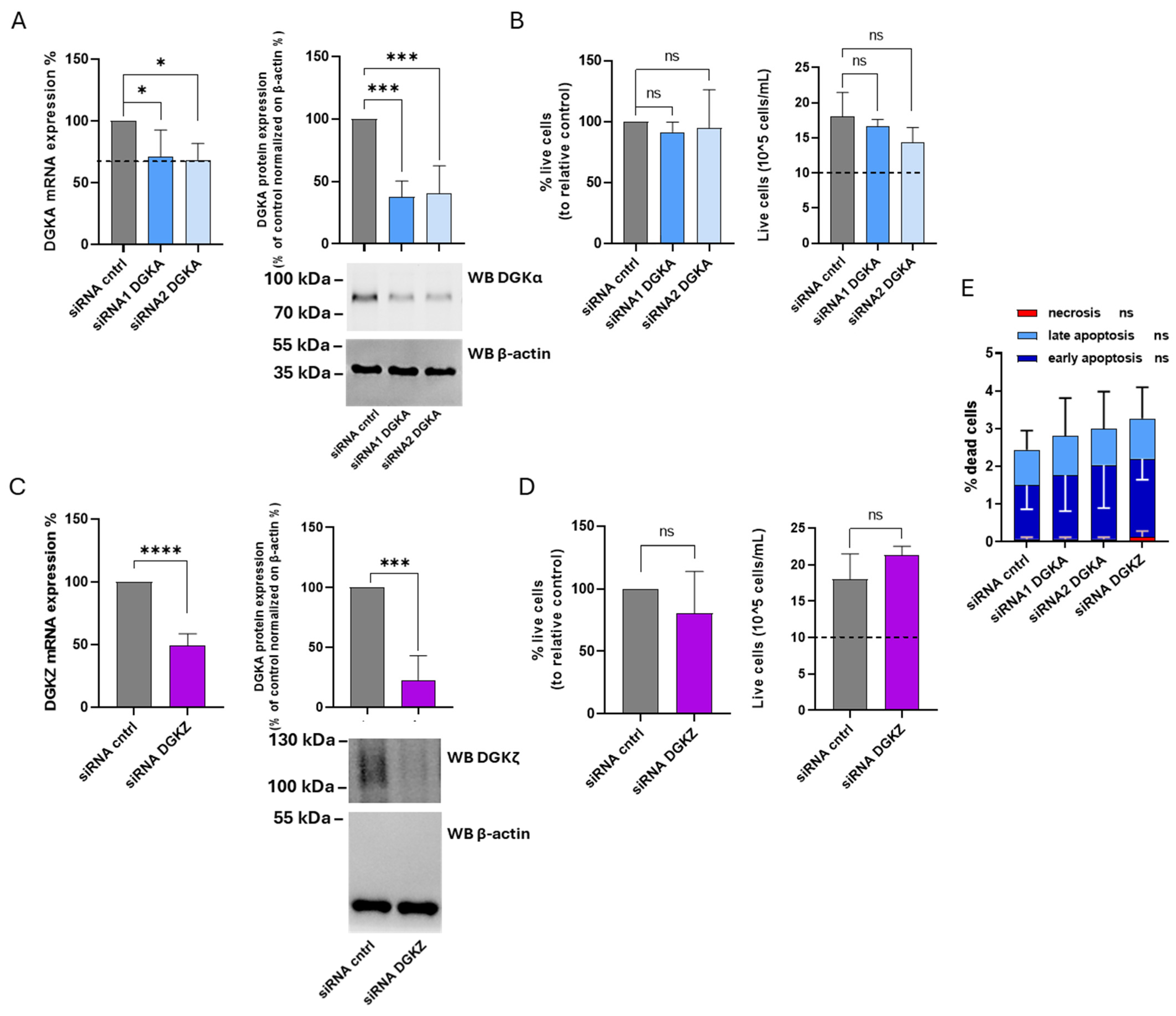
When specifically addressing the role of DGKα and DGKζ through transient silencing, their relevance proved to be strongly cell line-dependent. DGKζ played a unique and crucial role in HL-60 cell viability as its knockdown led to a profound reduction in proliferation and an increase in late apoptosis, in line with data from Li et al. [
16]. In the same model, DGKA silencing induced only a modest reduction in viability with one of the siRNA tested, suggesting that DGKα is less relevant for viability in this cell line.
In HEL cells, the opposite pattern was observed: DGKA silencing resulted in a significant reduction in cell proliferation and a reduction in viability. In contrast, DGKZ silencing, despite achieving substantial mRNA and protein downregulation, did not affect cell proliferation and viability.
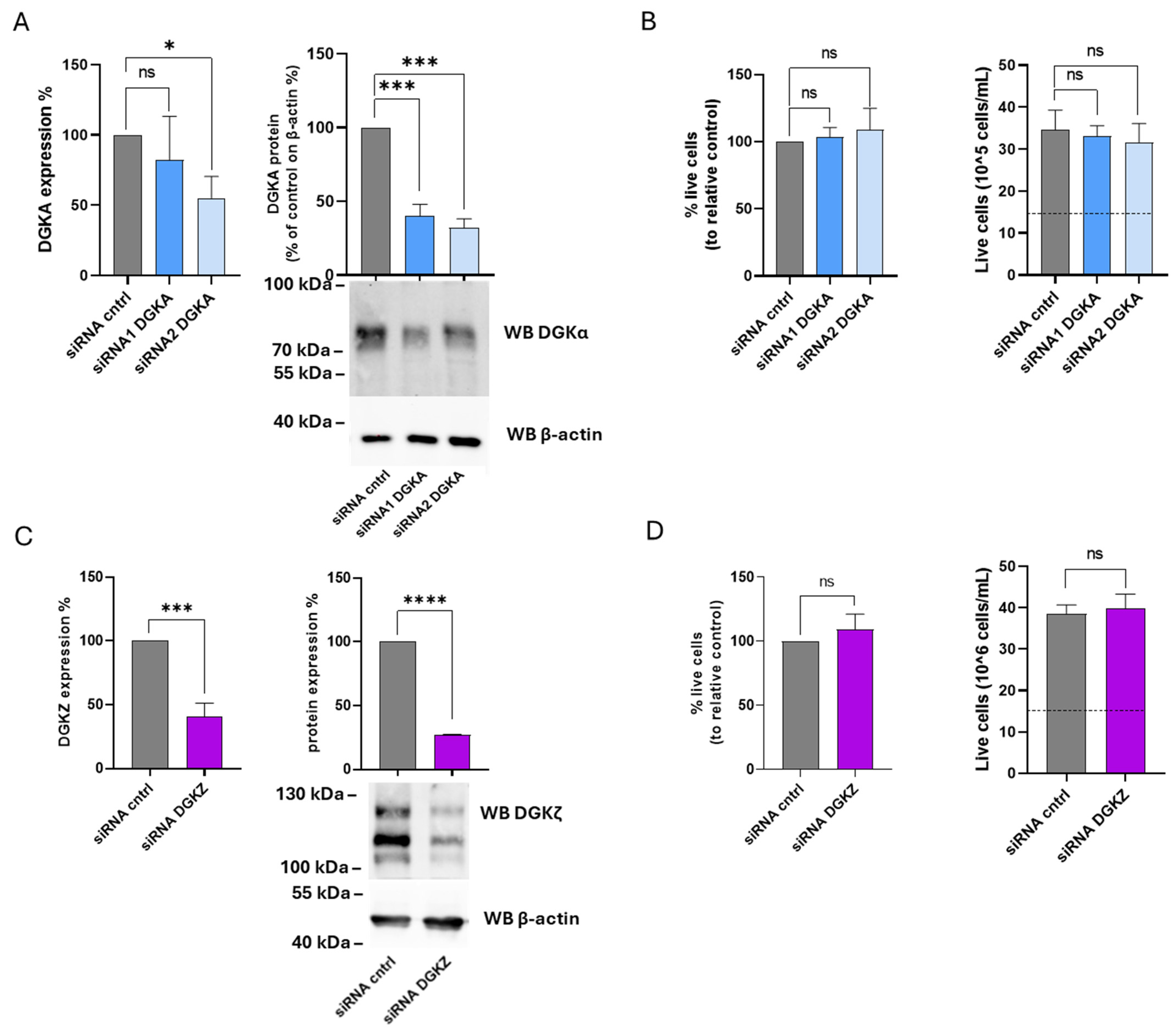
In THP-1 cells, silencing of DGKA and DGKZ did not lead to significant changes in cell viability or proliferation. Similarly, K562 cells appeared to be quite resistant to both the effect of DGK inhibitors and DGKα and DGKζ gene silencing, showing no significant reduction in viability and proliferation. This latter finding is partially in disagreement with the results reported by Poli et al. [
14] who, in addition to observing decreased proliferation following DGKα inhibitor treatment in the micromolar range, also reported reduced viability upon DGKα silencing. When the same K562 subclone used in that study was tested, a modest but significant decrease in viability was observed upon DGKζ silencing, whereas DGKA silencing again produced no detectable effect (
Supplementary Figure S8). The discrepancy may be attributed to differences in silencing efficiency, as DGKA mRNA levels in our experiments were reduced by only 50%. Indeed, using transient siRNA mediated silencing by electroporation allowed us to overcome long-term cell line adaptation to DGK depletion, which represents a limitation of our work due to the residual target expression observed across all experiments. In addition, the greater cytotoxicity observed with small-molecule inhibitors compared with siRNA knockdown may partly reflect off-target effects.
Overall, our findings indicate that AML cell viability depends variably on DGKα or DGKζ expression. While some AML lines, such as HEL (
Figure 6) and previously described Kasumi-1 and KG-1α [
13], rely primarily on DGKα, others, such as HL-60 (
Figure 5 and [
16]) and the K562 subclone (
Supplementary Figure S8) are DGKζ-dependent. Intriguingly, certain cell lines may not rely on either isoform, suggesting functional redundancy. To test this hypothesis and eventually determine the extent of this redundancy, further studies targeting additional DGK isoforms and employing combined inhibition or silencing approaches will be necessary. Furthermore, additional research on patient-derived AML blasts will be crucial to ascertain whether isoform dependency is associated with specific AML subtypes, molecular alterations, or stages of myeloid differentiation. Such studies should enable patient stratification and design optimization of future clinical trials.