The Role of FNDC5/Irisin in Cardiovascular Disease
Abstract
1. Introduction
1.1. The Structure of FNDC5/Irisin
1.2. Signaling Pathways Related to FNDC5/Irisin in Heart and Cardiovascular Diseases
1.3. Function and Effect of FNDC5/Irisin on Cells
1.3.1. The Effect of Physical Exertion on the Secretion of Irisin
1.3.2. Impact of FNDC5/Irisin on Adipose Cells
1.3.3. Impact of FNDC5/Irisin on Osteoclasts and Osteoblasts
1.3.4. Impact of FNDC5/Irisin on Endothelial Cells, VSCMs and Angiogenesis
1.3.5. Impact of FNDC5/Irisin on Cardiomyocytes
2. Significance of FNDC5/Irisin in Cardiovascular Disease
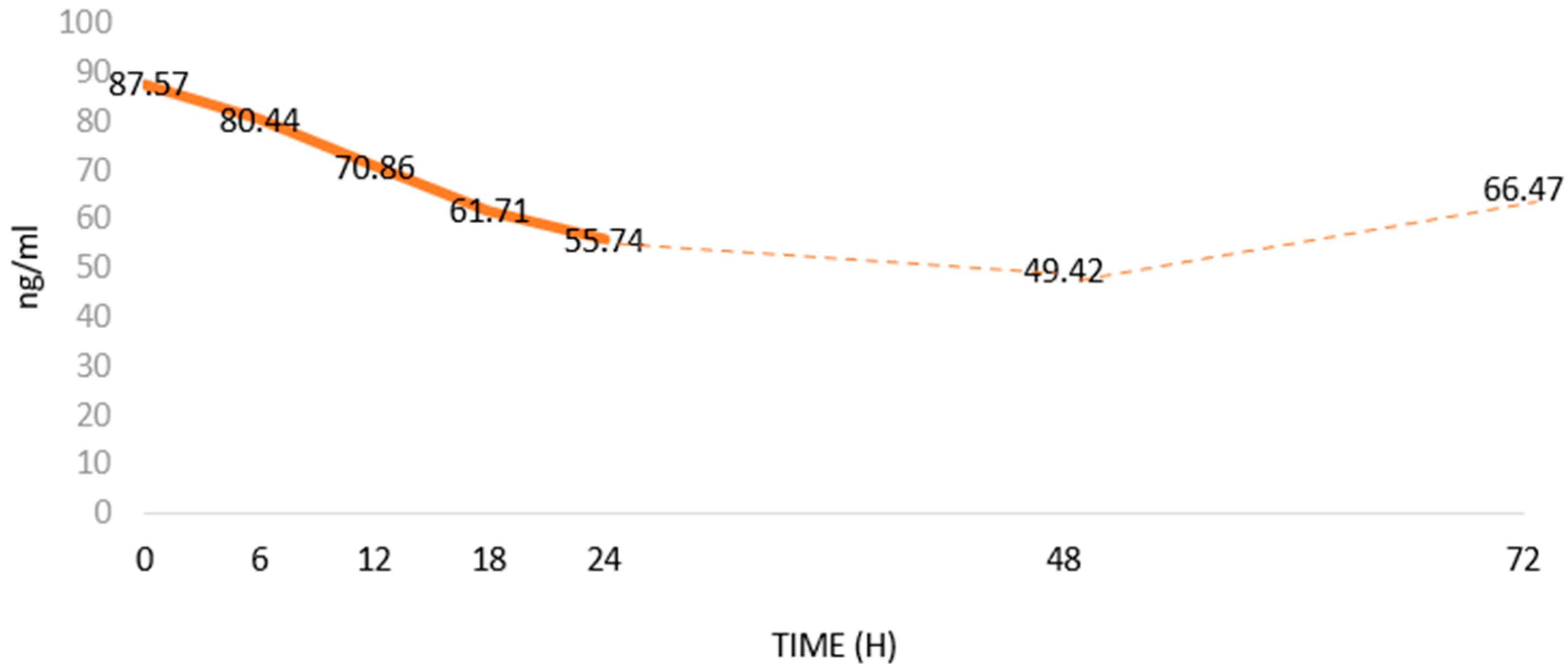
2.1. Significance of FNDC5/Irisin in Myocardial Infarction
2.2. Significance of FNDC5/Irisin in Atherosclerosis, Coronary Artery Disease and Hypertension
2.3. Protective Effect of FNDC5/Irisin on the Cardiovascular System
2.4. Potential Therapeutic Use of FNDC5/Irisin in Cardiovascular Disease
3. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Zhu, D.; Wang, H.; Zhang, J.; Zhang, X.; Xin, C.; Zhang, F.; Lee, Y.; Zhang, L.; Lian, K.; Yan, W.; et al. Irisin Improves Endothelial Function in Type 2 Diabetes through Reducing Oxidative/Nitrative Stresses. J. Mol. Cell Cardiol. 2015, 87, 138–147. [Google Scholar] [CrossRef] [PubMed]
- Huh, J.Y.; Panagiotou, G.; Mougios, V.; Brinkoetter, M.; Vamvini, M.T.; Schneider, B.E.; Mantzoros, C.S. FNDC5 and Irisin in Humans: I. Predictors of Circulating Concentrations in Serum and Plasma and II. MRNA Expression and Circulating Concentrations in Response to Weight Loss and Exercise. Metabolism 2012, 61, 1725–1738. [Google Scholar] [CrossRef] [PubMed]
- Kuloglu, T.; Aydin, S.; Eren, M.N.; Yilmaz, M.; Sahin, I.; Kalayci, M.; Sarman, E.; Kaya, N.; Yilmaz, O.F.; Turk, A.; et al. Irisin: A Potentially Candidate Marker for Myocardial Infarction. Peptides 2014, 55, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.J.; Wong, M.D.S.; Toy, W.C.; Tan, C.S.H.; Liu, S.; Ng, X.W.; Tavintharan, S.; Sum, C.F.; Lim, S.C. Lower Circulating Irisin Is Associated with Type 2 Diabetes Mellitus. J. Diabetes Complicat. 2013, 27, 365–369. [Google Scholar] [CrossRef] [PubMed]
- Roca-Rivada, A.; Castelao, C.; Senin, L.L.; Landrove, M.O.; Baltar, J.; Crujeiras, A.B.; Seoane, L.M.; Casanueva, F.F.; Pardo, M. FNDC5/Irisin Is Not Only a Myokine but Also an Adipokine. PLoS ONE 2013, 8, e60563. [Google Scholar] [CrossRef] [PubMed]
- Us Altay, D.; Keha, E.E.; Ozer Yaman, S.; Ince, I.; Alver, A.; Erdogan, B.; Canpolat, S.; Cobanoglu, U.; Mentese, A. Investigation of the Expression of Irisin and Some Cachectic Factors in Mice with Experimentally Induced Gastric Cancer. QJM Int. J. Med. 2016, 109, 785–790. [Google Scholar] [CrossRef]
- Esawy, M.M.; Abdel-Samd, K.M. The Diagnostic and Prognostic Roles of Serum Irisin in Bladder Cancer. Curr. Probl. Cancer 2020, 44, 100529. [Google Scholar] [CrossRef]
- Nowinska, K.; Jablonska, K.; Pawelczyk, K.; Piotrowska, A.; Partynska, A.; Gomulkiewicz, A.; Ciesielska, U.; Katnik, E.; Grzegrzolka, J.; Glatzel-Plucinska, N.; et al. Expression of Irisin/FNDC5 in Cancer Cells and Stromal Fibroblasts of Non-Small Cell Lung Cancer. Cancers 2019, 11, 1538. [Google Scholar] [CrossRef]
- Pinkowska, A.; Nowinska, K.; Ciesielska, U.; Podhorska-Okolow, M. Irisin Association with Ki-67, MCM3 and MT-I/II in Squamous Cell Carcinomas of the Larynx. Biomolecules 2022, 12, 52. [Google Scholar] [CrossRef]
- Cebulski, K.; Nowińska, K.; Jablońska, K.; Romanowicz, H.; Smolarz, B.; Dzięgiel, P.; Podhorska-Okołów, M. Expression of Irisin/FNDC5 in Breast Cancer. Int. J. Mol. Sci. 2022, 23, 3530. [Google Scholar] [CrossRef]
- Cebulski, K.; Piotrowska, A.; Kmiecik, A.; Haczkiewicz-Leśniak, K.; Ciesielska, U.; Grzegrzółka, J.; Jabłońska, K.; Romanowicz, H.; Smolarz, B.; Dzięgiel, P.; et al. The Role of Irisin/FNDC5 Expression and Its Serum Level in Breast Cancer. Int. J. Mol. Sci. 2023, 24, 8628. [Google Scholar] [CrossRef] [PubMed]
- Pinkowska, A.; Podhorska-Okołów, M.; Dzięgiel, P.; Nowińska, K. The Role of Irisin in Cancer Disease. Cells 2021, 10, 1479. [Google Scholar] [CrossRef] [PubMed]
- Nowińska, K.; Jabłońska, K.; Ciesielska, U.; Piotrowska, A.; Haczkiewicz-Leśniak, K.; Pawełczyk, K.; Podhorska-Okołów, M.; Dzięgiel, P. Association of Irisin/FNDC5 with ERRα and PGC-1α Expression in NSCLC. Int. J. Mol. Sci. 2022, 23, 14204. [Google Scholar] [CrossRef] [PubMed]
- Polyzos, S.A.; Anastasilakis, A.D.; Efstathiadou, Z.A.; Makras, P.; Perakakis, N.; Kountouras, J.; Mantzoros, C.S. Irisin in Metabolic Diseases. Endocrine 2018, 59, 260–274. [Google Scholar] [CrossRef] [PubMed]
- Aydin, S. Three New Players in Energy Regulation: Preptin, Adropin and Irisin. Peptides 2014, 56, 94–110. [Google Scholar] [CrossRef] [PubMed]
- Ivanov, I.P.; Firth, A.E.; Michel, A.M.; Atkins, J.F.; Baranov, P.V. Identification of Evolutionarily Conserved Non-AUG-Initiated N-Terminal Extensions in Human Coding Sequences. Nucleic Acids Res. 2011, 39, 4220–4234. [Google Scholar] [CrossRef]
- Raschke, S.; Elsen, M.; Gassenhuber, H.; Sommerfeld, M.; Schwahn, U.; Brockmann, B.; Jung, R.; Wisløff, U.; Tjønna, A.E.; Raastad, T.; et al. Evidence against a Beneficial Effect of Irisin in Humans. PLoS ONE 2013, 8, e73680. [Google Scholar] [CrossRef] [PubMed]
- Boström, P.; Wu, J.; Jedrychowski, M.P.; Korde, A.; Ye, L.; Lo, J.C.; Rasbach, K.A.; Boström, E.A.; Choi, J.H.; Long, J.Z.; et al. A PGC1-α-Dependent Myokine That Drives Brown-Fat-like Development of White Fat and Thermogenesis. Nature 2012, 481, 463–468. [Google Scholar] [CrossRef]
- Wrann, C.D.; White, J.P.; Salogiannnis, J.; Laznik-Bogoslavski, D.; Wu, J.; Ma, D.; Lin, J.D.; Greenberg, M.E.; Spiegelman, B.M. Exercise Induces Hippocampal BDNF through a PGC-1α/FNDC5 Pathway. Cell Metab. 2013, 18, 649–659. [Google Scholar] [CrossRef]
- Kim, H.K.; Jeong, Y.J.; Song, I.S.; Noh, Y.H.; Seo, K.W.; Kim, M.; Han, J. Glucocorticoid Receptor Positively Regulates Transcription of FNDC5 in the Liver. Sci. Rep. 2017, 7, 43296. [Google Scholar] [CrossRef]
- Jaenisch, R.; Bird, A. Epigenetic Regulation of Gene Expression: How the Genome Integrates Intrinsic and Environmental Signals. Nat. Genet. 2003, 33, 245–254. [Google Scholar] [CrossRef]
- Rabiee, F.; Forouzanfar, M.; Ghazvini Zadegan, F.; Tanhaei, S.; Ghaedi, K.; Motovali Bashi, M.; Baharvand, H.; Nasr-Esfahani, M.H. Induced Expression of Fndc5 Significantly Increased Cardiomyocyte Differentiation Rate of Mouse Embryonic Stem Cells. Gene 2014, 551, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Nazem, S.; Rabiee, F.; Ghaedi, K.; Babashah, S.; Sadeghizadeh, M.; Nasr-Esfahani, M.H. Fndc5 Knockdown Induced Suppression of Mitochondrial Integrity and Significantly Decreased Cardiac Differentiation of Mouse Embryonic Stem Cells. J. Cell Biochem. 2018, 119, 4528–4539. [Google Scholar] [CrossRef]
- Ghazvini Zadegan, F.; Ghaedi, K.; Kalantar, S.M.; Peymani, M.; Hashemi, M.S.; Baharvand, H.; Nasr-Esfahani, M.H. Cardiac Differentiation of Mouse Embryonic Stem Cells Is Influenced by a PPAR γ/PGC-1α-FNDC5 Pathway during the Stage of Cardiac Precursor Cell Formation. Eur. J. Cell Biol. 2015, 94, 257–266. [Google Scholar] [CrossRef]
- UniProt: The Universal Protein Knowledgebase in 2021. Nucleic Acids Res. 2021, 49, D480–D489. [CrossRef]
- Young, M.F.; Valaris, S.; Wrann, C.D. A Role for FNDC5/Irisin in the Beneficial Effects of Exercise on the Brain and in Neurodegenerative Diseases. Prog. Cardiovasc. Dis. 2019, 62, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Yu, Q.; Kou, W.; Xu, X.; Zhou, S.; Luan, P.; Xu, X.; Li, H.; Zhuang, J.; Wang, J.; Zhao, Y.; et al. FNDC5/Irisin Inhibits Pathological Cardiac Hypertrophy. Clin. Sci. 2019, 133, 611–627. [Google Scholar] [CrossRef] [PubMed]
- Schumacher, M.A.; Chinnam, N.; Ohashi, T.; Shah, R.S.; Erickson, H.P. The Structure of Irisin Reveals a Novel Intersubunit β-Sheet Fibronectin Type III (FNIII) Dimer: Implications for Receptor Activation. J. Biol. Chem. 2013, 288, 33738–33744. [Google Scholar] [CrossRef]
- Kim, H.; Wrann, C.D.; Jedrychowski, M.; Vidoni, S.; Kitase, Y.; Nagano, K.; Zhou, C.; Chou, J.; Parkman, V.J.A.; Novick, S.J.; et al. Irisin Mediates Effects on Bone and Fat via AV Integrin Receptors. Cell 2018, 175, 1756–1768.e17. [Google Scholar] [CrossRef]
- Rabiee, F.; Lachinani, L.; Ghaedi, S.; Nasr-Esfahani, M.H.; Megraw, T.L.; Ghaedi, K. New Insights into the Cellular Activities of Fndc5/Irisin and Its Signaling Pathways. Cell Biosci. 2020, 10, 51. [Google Scholar] [CrossRef]
- Lu, L.; Shao, Y.; Xiong, X.; Ma, J.; Zhai, M.; Lu, G. Biomedicine & Pharmacotherapy Irisin Improves Diabetic Cardiomyopathy-Induced Cardiac Remodeling by Regulating GSDMD-Mediated Pyroptosis through MITOL/STING Signaling. Biomed. Pharmacother. 2024, 171, 116007. [Google Scholar] [CrossRef]
- Rech, L.; Rainer, P.P. The Innate Immune CGAS-STING-Pathway in Cardiovascular Diseases—A Mini Review. Front. Cardiovasc. Med. 2021, 8, 715903. [Google Scholar] [CrossRef]
- Lin, C.; Guo, Y.; Xia, Y.; Li, C.; Xu, X.; Qi, T.; Zhang, F.; Fan, M.; Hu, G.; Zhao, H.; et al. FNDC5/Irisin Attenuates Diabetic Cardiomyopathy in a Type 2 Diabetes Mouse Model by Activation of Integrin αV/Β5-AKT Signaling and Reduction of Oxidative/Nitrosative Stress. J. Mol. Cell Cardiol. 2021, 160, 27–41. [Google Scholar] [CrossRef]
- Deng, J.; Zhang, N.; Chen, F.; Yang, C.; Ning, H.; Xiao, C.; Sun, K.; Liu, Y.; Yang, M.; Hu, T.; et al. Irisin Ameliorates High Glucose-Induced Cardiomyocytes Injury via AMPK/MTOR Signal Pathway. Cell Biol. Int. 2020, 44, 2315–2325. [Google Scholar] [CrossRef]
- Zhu, D.; Zhang, X.; Wang, F.; Ye, Q.; Yang, C.; Liu, D. Irisin Rescues Diabetic Cardiac Microvascular Injury via ERK1/2/Nrf2/HO-1 Mediated Inhibition of Oxidative Stress. Diabetes Res. Clin. Pract. 2022, 183, 109170. [Google Scholar] [CrossRef]
- Demirel, S.; Sahinturk, S.; Isbil, N.; Ozyener, F. Irisin Relaxes Rat Thoracic Aorta: MEK1/2 Signaling Pathway, KV Channels, SKCa Channels, and BKCa Channels Are Involved in Irisin-Induced Vasodilation. Can. J. Physiol. Pharmacol. 2022, 100, 379–385. [Google Scholar] [CrossRef]
- Wu, Y.; Luo, J.; Song, X.; Gu, W.; Wang, S.; Hao, S.; Dong, Z.; Ning, Z. Irisin Attenuates Angiotensin II-Induced Atrial Fibrillation and Atrial Fibrosis via LOXL2 and TGFβ1/Smad2/3 Signaling Pathways. Iran. J. Basic Med. Sci. 2023, 26, 717–724. [Google Scholar] [CrossRef]
- Pang, Q.; Wang, P.; Pan, Y.; Dong, X.; Zhou, T.; Song, X.; Zhang, A. Irisin Protects against Vascular Calcification by Activating Autophagy and Inhibiting NLRP3-Mediated Vascular Smooth Muscle Cell Pyroptosis in Chronic Kidney Disease. Cell Death Dis. 2022, 13, 283. [Google Scholar] [CrossRef]
- Wang, P.W.; Pang, Q.; Zhou, T.; Song, X.Y.; Pan, Y.J.; Jia, L.P.; Zhang, A.H. Irisin Alleviates Vascular Calcification by Inhibiting VSMC Osteoblastic Transformation and Mitochondria Dysfunction via AMPK/Drp1 Signaling Pathway in Chronic Kidney Disease. Atherosclerosis 2022, 346, 36–45. [Google Scholar] [CrossRef] [PubMed]
- Ouchi, N.; Ohashi, K.; Shibata, R.; Murohara, T. Protective Roles of Adipocytokines and Myokines in Cardiovascular Disease. Circ. J. 2016, 80, 2073–2080. [Google Scholar] [CrossRef] [PubMed]
- Lightfoot, A.P.; Cooper, R.G. The Role of Myokines in Muscle Health and Disease. Curr. Opin. Rheumatol. 2016, 28, 661–666. [Google Scholar] [CrossRef] [PubMed]
- Fox, J.; Rioux, B.V.; Goulet, E.D.B.; Johanssen, N.M.; Swift, D.L.; Bouchard, D.R.; Loewen, H.; Sénéchal, M. Effect of an Acute Exercise Bout on Immediate Post-Exercise Irisin Concentration in Adults: A Meta-Analysis. Scand. J. Med. Sci. Sports 2018, 28, 16–28. [Google Scholar] [CrossRef] [PubMed]
- Maak, S.; Norheim, F.; Drevon, C.A.; Erickson, H.P. Progress and Challenges in the Biology of FNDC5 and Irisin. Endocr. Rev. 2021, 42, 436–456. [Google Scholar] [CrossRef] [PubMed]
- Kraemer, R.R.; Shockett, P.E.; Webb, N.D.; Shah, U.; Castracane, V.D. A Transient Elevated Irisin Blood Concentration in Response to Prolonged, Moderate Aerobic Exercise in Young Men and Women. Med. Sci. Sports Exerc. 2014, 46, 404. [Google Scholar] [CrossRef]
- Huh, J.Y.; Mougios, V.; Kabasakalis, A.; Fatouros, I.; Siopi, A.; Douroudos, I.I.; Filippaios, A.; Panagiotou, G.; Park, K.H.; Mantzoros, C.S. Exercise-Induced Irisin Secretion Is Independent of Age or Fitness Level and Increased Irisin May Directly Modulate Muscle Metabolism through AMPK Activation. J. Clin. Endocrinol. Metab. 2014, 99, E2154–E2161. [Google Scholar] [CrossRef]
- Jóźków, P.; Koźlenia, D.; Zawadzka, K.; Konefał, M.; Chmura, P.; Młynarska, K.; Kosowski, M.; Mędraś, M.; Chmura, J.; Ponikowski, P.; et al. Effects of Running a Marathon on Irisin Concentration in Men Aged over 50. J. Physiol. Sci. 2019, 69, 79–84. [Google Scholar] [CrossRef]
- Joro, R.; Korkmaz, A.; Lakka, T.A.; Uusitalo, A.L.T.; Atalay, M. Plasma Irisin and Its Associations with Oxidative Stress in Athletes Suffering from Overtraining Syndrome. Physiol. Int. 2021, 107, 513–526. [Google Scholar] [CrossRef]
- Lawson, E.A.; Ackerman, K.E.; Slattery, M.; Marengi, D.A.; Clarke, H.; Misra, M. Oxytocin Secretion Is Related to Measures of Energy Homeostasis in Young Amenorrheic Athletes. J. Clin. Endocrinol. Metab. 2014, 99, 881–885. [Google Scholar] [CrossRef]
- Pearson, N.; Sherar, L.B. Sedentary Behaviour and Health. Oxford University Press In Oxford Textbook of Children’s Sport and Excercise Medicine, 4th ed.; Oxford University Press: Oxford, UK, 2023; Volume 51, pp. 255–266. [Google Scholar] [CrossRef]
- Lecker, S.H.; Zavin, A.; Cao, P.; Arena, R.; Allsup, K.; Daniels, K.M.; Joseph, J.; Schulze, P.C.; Forman, D.E. Expression of the Irisin Precursor Fndc5 in Skeletal Muscle Correlates with Aerobic Exercise Performance in Patients with Heart Failure. Circ. Heart Fail. 2012, 5, 812–818. [Google Scholar] [CrossRef]
- Rana, K.S.; Arif, M.; Hill, E.J.; Aldred, S.; Nagel, D.A.; Nevill, A.; Randeva, H.S.; Bailey, C.J.; Bellary, S.; Brown, J.E. Plasma Irisin Levels Predict Telomere Length in Healthy Adults. Age 2014, 36, 995–1001. [Google Scholar] [CrossRef]
- Weischer, M.; Bojesen, S.E.; Cawthon, R.M.; Freiberg, J.J.; Tybjærg-Hansen, A.; Nordestgaard, B.G. Short Telomere Length, Myocardial Infarction, Ischemic Heart Disease, and Early Death. Arterioscler. Thromb. Vasc. Biol. 2012, 32, 822–829. [Google Scholar] [CrossRef]
- Emanuele, E.; Minoretti, P.; Pareja-Galeano, H.; Sanchis-Gomar, F.; Garatachea, N.; Lucia, A. Serum Irisin Levels, Precocious Myocardial Infarction, and Healthy Exceptional Longevity. Am. J. Med. 2014, 127, 888–890. [Google Scholar] [CrossRef]
- Lo, K.A.; Sun, L. Turning WAT into BAT: A Review on Regulators Controlling the Browning of White Adipocytes. Biosci. Rep. 2013, 33, 711–719. [Google Scholar] [CrossRef]
- Pinckard, K.M.; Stanford, K.I. The Heartwarming Effect of Brown Adipose Tissue. Mol Pharmacol. 2022, 102, 460–471. [Google Scholar] [CrossRef]
- Brown, N.K.; Zhou, Z.; Zhang, J.; Zeng, R.; Wu, J.; Eitzman, D.T.; Chen, Y.E.; Chang, L. Perivascular Adipose Tissue in Vascular Function and Disease: A Review of Current Research and Animal Models. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 1621–1630. [Google Scholar] [CrossRef] [PubMed]
- Jeremic, N.; Chaturvedi, P.; Tyagi, S.C. Browning of White Fat: Novel Insight into Factors, Mechanisms, and Therapeutics. J. Cell Physiol. 2017, 232, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Greenhill, C. Irisin Receptor in Osteocytes Identified. Nat. Rev. Endocrinol. 2019, 15, 63. [Google Scholar] [CrossRef] [PubMed]
- Colaianni, G.; Cuscito, C.; Mongelli, T.; Oranger, A.; Mori, G.; Brunetti, G.; Colucci, S.; Cinti, S.; Grano, M. Irisin Enhances Osteoblast Differentiation in Vitro. Int. J. Endocrinol. 2014, 2014, 902186. [Google Scholar] [CrossRef]
- Wahab, F.; Drummer, C.; Mätz-Rensing, K.; Fuchs, E.; Behr, R. Irisin Is Expressed by Undifferentiated Spermatogonia and Modulates Gene Expression in Organotypic Primate Testis Cultures. Mol. Cell Endocrinol. 2020, 504, 110670. [Google Scholar] [CrossRef] [PubMed]
- Wu, F.; Song, H.; Zhang, Y.; Zhang, Y.; Mu, Q.; Jiang, M.; Wang, F.; Zhang, W.; Li, L.; Li, H.; et al. Irisin Induces Angiogenesis in Human Umbilical Vein Endothelial Cells in Vitro and in Zebrafish Embryos in Vivo via Activation of the ERK Signaling Pathway. PLoS ONE 2015, 10, e134662. [Google Scholar] [CrossRef] [PubMed]
- Albrecht-Schgoer, K.; Schgoer, W.; Holfeld, J.; Theurl, M.; Wiedemann, D.; Steger, C.; Gupta, R.; Semsroth, S.; Fischer-Colbrie, R.; Beer, A.G.E.; et al. The Angiogenic Factor Secretoneurin Induces Coronary Angiogenesis in a Model of Myocardial Infarction by Stimulation of Vascular Endothelial Growth Factor Signaling in Endothelial Cells. Circulation 2012, 126, 2491–2501. [Google Scholar] [CrossRef] [PubMed]
- Altaweel, R.; Shatarat, A.; Badran, D.; Abu Tarboush, N.M. The Effects of Irisin on the Rat Thoracic Aorta: A Histological Study. Folia Morphol. 2022, 81, 923–930. [Google Scholar] [CrossRef]
- Zhang, Y.; Song, H.; Zhang, Y.; Wu, F.; Mu, Q.; Jiang, M.; Wang, F.; Zhang, W.; Li, L.; Shao, L.; et al. Irisin Inhibits Atherosclerosis by Promoting Endothelial Proliferation Through MicroRNA126-5p. J. Am. Heart Assoc. 2016, 5. [Google Scholar] [CrossRef] [PubMed]
- Chi, C.; Fu, H.; Li, Y.H.; Zhang, G.Y.; Zeng, F.Y.; Ji, Q.X.; Shen, Q.R.; Wang, X.J.; Li, Z.C.; Zhou, C.C.; et al. Exerkine Fibronectin Type-III Domain-Containing Protein 5/Irisin-Enriched Extracellular Vesicles Delay Vascular Ageing by Increasing SIRT6 Stability. Eur. Heart J. 2022, 43, 4579–4595. [Google Scholar] [CrossRef] [PubMed]
- Mancinelli, R.; Checcaglini, F.; Coscia, F.; Gigliotti, P.; Fulle, S.; Fanò-Illic, G. Biological Aspects of Selected Myokines in Skeletal Muscle: Focus on Aging. Int. J. Mol. Sci. 2021, 22, 8520. [Google Scholar] [CrossRef] [PubMed]
- Gélinas, R.; Mailleux, F.; Dontaine, J.; Bultot, L.; Demeulder, B.; Ginion, A.; Daskalopoulos, E.P.; Esfahani, H.; Dubois-Deruy, E.; Lauzier, B.; et al. AMPK Activation Counteracts Cardiac Hypertrophy by Reducing O-GlcNAcylation. Nat. Commun. 2018, 9, 374. [Google Scholar] [CrossRef] [PubMed]
- Coelho-Filho, O.R.; Shah, R.V.; Mitchell, R.; Neilan, T.G.; Moreno, H., Jr.; Simonson, B.; Kwong, R.; Rosenzweig, A.; Das, S.; Jerosch-Herold, M. Quantification of Cardiomyocyte Hypertrophy by Cardiac Magnetic Resonance: Implications on Early Cardiac Remodeling. Circulation 2013, 128, 1225–1233. [Google Scholar] [CrossRef] [PubMed]
- Yue, R.; Lv, M.; Lan, M.; Zheng, Z.; Tan, X.; Zhao, X.; Zhang, Y.; Pu, J.; Xu, L.; Hu, H. Irisin Protects Cardiomyocytes against Hypoxia/Reoxygenation Injury via Attenuating AMPK Mediated Endoplasmic Reticulum Stress. Sci. Rep. 2022, 12, 7415. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wei, C.; Wang, H.; Tang, S.; Jia, Z.; Wang, L.; Xu, D.; Wu, Y. Protective Effect of Qiliqiangxin Capsule on Energy Metabolism and Myocardial Mitochondria in Pressure Overload Heart Failure Rats. Evid. Based Complement. Altern. Med. 2013, 2013, 378298. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.; Zhu, Q.; Wu, Z.; Ding, J.; Qin, S.; Liu, H.; Miao, P. Protective Effects of Irisin on Hypoxia-Reoxygenation Injury in Hyperglycemia-Treated Cardiomyocytes: Role of AMPK Pathway and Mitochondrial Protection. J. Cell Physiol. 2020, 235, 1165–1174. [Google Scholar] [CrossRef] [PubMed]
- Moscoso, I.; Cebro-Márquez, M.; Rodríguez-Mañero, M.; González-Juanatey, J.R.; Lage, R. FNDC5/Irisin Counteracts Lipotoxic-Induced Apoptosis in Hypoxic H9c2 Cells. J. Mol. Endocrinol. 2019, 63, 151–159. [Google Scholar] [CrossRef]
- Xie, C.; Zhang, Y.; Tran, T.D.N.; Wang, H.; Li, S.; George, E.V.; Zhuang, H.; Zhang, P.; Kandel, A.; Lai, Y.; et al. Irisin Controls Growth, Intracellular Ca2+ Signals, and Mitochondrial Thermogenesis in Cardiomyoblasts. PLoS ONE 2015, 10, e136816. [Google Scholar] [CrossRef] [PubMed]
- Hirayama, K.; Ishii, H.; Kikuchi, R.; Suzuki, S.; Aoki, T.; Harada, K.; Sumi, T.; Negishi, Y.; Shibata, Y.; Tatami, Y.; et al. Clinical Impact of Circulating Irisin on Classified Coronary Plaque Characteristics. J. Appl. Lab. Med. 2018, 3, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Park, K.H.; Zaichenko, L.; Brinkoetter, M.; Thakkar, B.; Sahin-Efe, A.; Joung, K.E.; Tsoukas, M.A.; Geladari, E.V.; Huh, J.Y.; Dincer, F.; et al. Circulating Irisin in Relation to Insulin Resistance and the Metabolic Syndrome. J. Clin. Endocrinol. Metab. 2013, 98, 4899–4907. [Google Scholar] [CrossRef] [PubMed]
- Aronis, K.N.; Moreno, M.; Polyzos, S.A.; Moreno-Navarrete, J.M.; Ricart, W.; Delgado, E.; De La Hera, J.; Sahin-Efe, A.; Chamberland, J.P.; Berman, R.; et al. Circulating Irisin Levels and Coronary Heart Disease: Association with Future Acute Coronary Syndrome and Major Adverse Cardiovascular Events. Int. J. Obes. 2015, 39, 156–161. [Google Scholar] [CrossRef]
- Anderson, J.L.; Morrow, D.A. Acute Myocardial Infarction. N. Engl. J. Med. 2017, 376, 2053–2064. [Google Scholar] [CrossRef]
- Vafaie, M. State-of-the-Art Diagnosis of Myocardial Infarction. Diagnosis 2016, 3, 137–142. [Google Scholar] [CrossRef]
- Aydin, S.; Aydin, S.; Kobat, M.A.; Kalayci, M.; Eren, M.N.; Yilmaz, M.; Kuloglu, T.; Gul, E.; Secen, O.; Alatas, O.D.; et al. Decreased Saliva/Serum Irisin Concentrations in the Acute Myocardial Infarction Promising for Being a New Candidate Biomarker for Diagnosis of This Pathology. Peptides 2014, 56, 141–145. [Google Scholar] [CrossRef]
- Anastasilakis, A.D.; Koulaxis, D.; Kefala, N.; Polyzos, S.A.; Upadhyay, J.; Pagkalidou, E.; Economou, F.; Anastasilakis, C.D.; Mantzoros, C.S. Circulating Irisin Levels Are Lower in Patients with Either Stable Coronary Artery Disease (CAD) or Myocardial Infarction (MI) versus Healthy Controls, Whereas Follistatin and Activin A Levels Are Higher and Can Discriminate MI from CAD with Similar to CK. Metabolism 2017, 73, 1–8. [Google Scholar] [CrossRef]
- Aydin, S.; Aydin, S. Irisin Concentrations as a Myocardial Biomarker. Biomark. Cardiovasc. Dis. 2015, 1–16. [Google Scholar] [CrossRef]
- Matsuo, Y.; Gleitsmann, K.; Mangner, N.; Werner, S.; Fischer, T.; Bowen, T.S.; Kricke, A.; Matsumoto, Y.; Kurabayashi, M.; Schuler, G.; et al. Fibronectin Type III Domain Containing 5 Expression in Skeletal Muscle in Chronic Heart Failure—Relevance of Inflammatory Cytokines. J. Cachexia Sarcopenia Muscle 2015, 6, 62–72. [Google Scholar] [CrossRef]
- Peacock, W.F.; Cannon, C.M.; Singer, A.J.; Hiestand, B.C. Considerations for Initial Therapy in the Treatment of Acute Heart Failure. Crit. Care 2015, 19, 1–11. [Google Scholar] [CrossRef]
- Bashar, S.M.; Samir El-Sherbeiny, S.M.; Boraie, M.Z. Correlation between the Blood Level of Irisin and the Severity of Acute Myocardial Infarction in Exercise-Trained Rats. J. Basic. Clin. Physiol. Pharmacol. 2019, 30, 59–71. [Google Scholar] [CrossRef]
- Seo, D.Y.; Bae, J.H.; Kim, T.N.; Kwak, H.B.; Kha, P.T.; Han, J. Exercise-Induced Circulating Irisin Level Is Correlated with Improved Cardiac Function in Rats. Int. J. Environ. Res. Public. Health 2020, 17, 3863. [Google Scholar] [CrossRef]
- Liao, Q.; Qu, S.; Tang, L.X.; Li, L.P.; He, D.F.; Zeng, C.Y.; Wang, W.E. Irisin Exerts a Therapeutic Effect against Myocardial Infarction via Promoting Angiogenesis. Acta Pharmacol. Sin. 2019, 40, 1314–1321. [Google Scholar] [CrossRef]
- Sundarrajan, L.; Yeung, C.; Hahn, L.; Weber, L.P.; Unniappan, S. Irisin Regulates Cardiac Physiology in Zebrafish. PLoS ONE 2017, 12, e181461. [Google Scholar] [CrossRef]
- Ho, M.Y.; Wen, M.S.; Yeh, J.K.; Hsieh, I.C.; Chen, C.C.; Hsieh, M.J.; Tsai, M.L.; Yang, C.H.; Wu, V.C.C.; Hung, K.C.; et al. Excessive Irisin Increases Oxidative Stress and Apoptosis in Murine Heart. Biochem. Biophys. Res. Commun. 2018, 503, 2493–2498. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, I.C.; Ho, M.Y.; Wen, M.S.; Chen, C.C.; Hsieh, M.J.; Lin, C.P.; Yeh, J.K.; Tsai, M.L.; Yang, C.H.; Wu, V.C.C.; et al. Serum Irisin Levels Are Associated with Adverse Cardiovascular Outcomes in Patients with Acute Myocardial Infarction. Int. J. Cardiol. 2018, 261, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Aydin, S.; Azboy, D.; Temizturk, Z.; Kuloglu, T.; Aydin, S.; Yardim, M.; Kalkan, A.K.; Eren, M.N. The Effect of Iloprost and Sildenafil, Alone and in Combination, on Myocardial Ischaemia and Nitric Oxide and Irisin Levels. Cardiovasc. J. Afr. 2017, 28, 389–396. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; He, Z.; Li, Q.; Lv, M.; Cai, Y.; Ke, W.; Niu, X.; Zhang, Z. Adipokines in Atherosclerosis: Unraveling Complex Roles. Front. Cardiovasc. Med. 2023, 10, 1235953. [Google Scholar] [CrossRef] [PubMed]
- Icli, A.; Cure, E.; Cure, M.C.; Uslu, A.U.; Balta, S.; Arslan, S.; Sakiz, D.; Kucuk, A. Novel Myokine: Irisin May Be an Independent Predictor for Subclinic Atherosclerosis in Behçet’s Disease. J. Investig. Med. 2016, 64, 875–881. [Google Scholar] [CrossRef] [PubMed]
- Deng, X.; Huang, W.; Peng, J.; Zhu, T.T.; Sun, X.L.; Zhou, X.Y.; Yang, H.; Xiong, J.F.; He, H.Q.; Xu, Y.H.; et al. Irisin Alleviates Advanced Glycation End Products-Induced Inflammation and Endothelial Dysfunction via Inhibiting ROS-NLRP3 Inflammasome Signaling. Inflammation 2018, 41, 260–275. [Google Scholar] [CrossRef]
- Guo, W.; Zhang, B.; Wang, X. Lower Irisin Levels in Coronary Artery Disease: A Meta-Analysis. Minerva Endocrinol. 2020, 45, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Kurdiova, T.; Balaz, M.; Vician, M.; Maderova, D.; Vlcek, M.; Valkovic, L.; Srbecky, M.; Imrich, R.; Kyselovicova, O.; Belan, V.; et al. Effects of Obesity, Diabetes and Exercise on Fndc5 Gene Expression and Irisin Release in Human Skeletal Muscle and Adipose Tissue: In Vivo and in Vitro Studies. J. Physiol. 2014, 592, 1091–1107. [Google Scholar] [CrossRef]
- Chen, K.; Zhou, M.; Wang, X.; Li, S.; Yang, D. The Role of Myokines and Adipokines in Hypertension and Hypertension-Related Complications. Hypertens. Res. 2019, 42, 1544–1551. [Google Scholar] [CrossRef] [PubMed]
- Fu, J.; Han, Y.; Wang, J.; Liu, Y.; Zheng, S.; Zhou, L.; Jose, P.A.; Zeng, C. Irisin Lowers Blood Pressure by Improvement of Endothelial Dysfunction via AMPK-Akt-ENOS-NO Pathway in the Spontaneously Hypertensive Rat. J. Am. Heart Assoc. 2016, 5, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Huo, C.-J.; Yu, X.-J.; Sun, Y.-J.; Li, H.-B.; Su, Q.; Bai, J.; Li, Y.; Liu, K.-L.; Qi, J.; Zhou, S.-W.; et al. Irisin Lowers Blood Pressure by Activating the Nrf2 Signaling Pathway in the Hypothalamic Paraventricular Nucleus of Spontaneously Hypertensive Rats. Toxicol. Appl. Pharmacol. 2020, 394, 114953. [Google Scholar] [CrossRef]
- Maciorkowska, M.; Musiałowska, D.; Małyszko, J. Adropin and Irisin in Arterial Hypertension, Diabetes Mellitus and Chronic Kidney Disease. Adv. Clin. Exp. Med. 2019, 28, 1571–1575. [Google Scholar] [CrossRef]
- Ellefsen, S.; Vikmoen, O.; Slettaløkken, G.; Whist, J.E.; Nygaard, H.; Hollan, I.; Rauk, I.; Vegge, G.; Strand, T.A.; Raastad, T.; et al. Irisin and FNDC5: Effects of 12-Week Strength Training, and Relations to Muscle Phenotype and Body Mass Composition in Untrained Women. Eur. J. Appl. Physiol. 2014, 114, 1875–1888. [Google Scholar] [CrossRef]
- Qin, S.; Tian, Z.; Boidin, M.; Buckley, B.J.R.; Thijssen, D.H.J.; Lip, G.Y.H. Irisin Is an Effector Molecule in Exercise Rehabilitation Following Myocardial Infarction (Review). Front. Physiol. 2022, 13, 1–15. [Google Scholar] [CrossRef]
- Xin, T.; Lu, C. Irisin Activates Opa1-Induced Mitophagy to Protect Cardiomyocytes against Apoptosis Following Myocardial Infarction. Aging 2020, 12, 4474–4488. [Google Scholar] [CrossRef]
- Bacmeister, L.; Schwarzl, M.; Warnke, S.; Stoffers, B.; Blankenberg, S.; Westermann, D.; Lindner, D. Inflammation and Fibrosis in Murine Models of Heart Failure; Springer: Berlin/Heidelberg, Germany, 2019; Volume 114, ISBN 0123456789. [Google Scholar]
- Basalay, M.V.; Davidson, S.M.; Gourine, A.V.; Yellon, D.M. Neural Mechanisms in Remote Ischaemic Conditioning in the Heart and Brain: Mechanistic and Translational Aspects. Basic. Res. Cardiol. 2018, 113, 1–15. [Google Scholar] [CrossRef]
- Hockings, C.; Alsop, A.E.; Fennell, S.C.; Lee, E.F.; Fairlie, W.D.; Dewson, G.; Kluck, R.M. Mcl-1 and Bcl-x L Sequestration of Bak Confers Differential Resistance to BH3-Only Proteins. Cell Death Differ. 2018, 25, 719–732. [Google Scholar] [CrossRef] [PubMed]
- Ho, M.Y.; Wang, C.Y. Role of Irisin in Myocardial Infarction, Heart Failure, and Cardiac Hypertrophy. Cells 2021, 10, 2103. [Google Scholar] [CrossRef]
- Wang, H.; Zhao, Y.T.; Zhang, S.; Dubielecka, P.M.; Du, J.; Yano, N.; Chin, Y.E.; Zhuang, S.; Qin, G.; Zhao, T.C. Irisin Plays a Pivotal Role to Protect the Heart against Ischemia and Reperfusion Injury. J. Cell Physiol. 2017, 232, 3775–3785. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Chen, K.; Han, Y.; Zhu, H.; Zhou, X.; Tan, T.; Zeng, J.; Zhang, J.; Liu, Y.; Li, Y.; et al. Irisin Protects Heart against Ischemia-Reperfusion Injury through a SOD2-Dependent Mitochondria Mechanism. J. Cardiovasc. Pharmacol. 2018, 72, 259–269. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.T.; Wang, H.; Zhang, S.; Du, J.; Zhuang, S.; Zhao, T.C. Irisin Ameliorates Hypoxia/Reoxygenation-Induced Injury through Modulation of Histone Deacetylase 4. PLoS ONE 2016, 11, e166182. [Google Scholar] [CrossRef] [PubMed]
- Li, R.L.; Wu, S.S.; Wu, Y.; Wang, X.X.; Chen, H.Y.; Xin, J.J.; Li, H.; Lan, J.; Xue, K.Y.; Li, X.; et al. Irisin Alleviates Pressure Overload-Induced Cardiac Hypertrophy by Inducing Protective Autophagy via MTOR-Independent Activation of the AMPK-ULK1 Pathway. J. Mol. Cell Cardiol. 2018, 121, 242–255. [Google Scholar] [CrossRef]
- Zhang, X.; Hu, C.; Kong, C.Y.; Song, P.; Wu, H.M.; Xu, S.C.; Yuan, Y.P.; Deng, W.; Ma, Z.G.; Tang, Q.Z. FNDC5 Alleviates Oxidative Stress and Cardiomyocyte Apoptosis in Doxorubicin-Induced Cardiotoxicity via Activating AKT. Cell Death Differ. 2020, 27, 540–555. [Google Scholar] [CrossRef]
- Ouyang, H.; Li, Q.; Zhong, J.; Xia, F.; Zheng, S.; Lu, J.; Deng, Y.; Hu, Y. Combination of Melatonin and Irisin Ameliorates Lipopolysaccharide-Induced Cardiac Dysfunction through Suppressing the Mst1–JNK Pathways. J. Cell Physiol. 2020, 235, 6647–6659. [Google Scholar] [CrossRef]
- Li, R.; Wang, X.; Wu, S.; Wu, Y.; Chen, H.; Xin, J.; Li, H.; Lan, J.; Xue, K.; Li, X.; et al. Irisin Ameliorates Angiotensin II-Induced Cardiomyocyte Apoptosis through Autophagy. J. Cell Physiol. 2019, 234, 17578–17588. [Google Scholar] [CrossRef]
- Zhao, Y.T.; Wang, J.; Yano, N.; Zhang, L.X.; Wang, H.; Zhang, S.; Qin, G.; Dubielecka, P.M.; Zhuang, S.; Liu, P.Y.; et al. Irisin Promotes Cardiac Progenitor Cell-Induced Myocardial Repair and Functional Improvement in Infarcted Heart. J. Cell Physiol. 2019, 234, 1671–1681. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Boerm, M.; McCarty, M.; Bucana, C.; Fidler, I.J.; Zhuang, Y.; Su, B. Mekk3 Is Essential for Early Embryonic Cardiovascular Development. Nat. Genet. 2000, 24, 309–313. [Google Scholar] [CrossRef] [PubMed]




| Marker | Marker Detectability | Time of Onset of the Increase (Diagnostic Window) | Time of Maximum Concentration | Time to Normalization |
|---|---|---|---|---|
| h-FABP | Very early | 0.5–1 h | 4–10 h | 24 h |
| GP-BB | Very early | 1–4 h | 6–12 h | 24–48 h |
| Myoglobin | Very early | 2–3 h | 6–8 h | 20–24 h |
| CK-MB | Early | 3.5 h | 12–16 h | 48–96 h |
| CK-MB mass | Early | 4–5 h | 12–16 h | 48–96 h |
| cTnT | Late | 4–6 h | 12–24 h | 7 days |
| cTnI | Late | 4–6 h | 12–24 h | 10 days |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grzeszczuk, M.; Dzięgiel, P.; Nowińska, K. The Role of FNDC5/Irisin in Cardiovascular Disease. Cells 2024, 13, 277. https://doi.org/10.3390/cells13030277
Grzeszczuk M, Dzięgiel P, Nowińska K. The Role of FNDC5/Irisin in Cardiovascular Disease. Cells. 2024; 13(3):277. https://doi.org/10.3390/cells13030277
Chicago/Turabian StyleGrzeszczuk, Maciej, Piotr Dzięgiel, and Katarzyna Nowińska. 2024. "The Role of FNDC5/Irisin in Cardiovascular Disease" Cells 13, no. 3: 277. https://doi.org/10.3390/cells13030277
APA StyleGrzeszczuk, M., Dzięgiel, P., & Nowińska, K. (2024). The Role of FNDC5/Irisin in Cardiovascular Disease. Cells, 13(3), 277. https://doi.org/10.3390/cells13030277







