Activation of Mammary Epithelial and Stromal Fibroblasts upon Exposure to Escherichia coli Metabolites
Abstract
1. Introduction
2. Materials and Methods
2.1. Cells and Cell Culture
2.2. Fibroblast-Conditioned Medium
2.3. Bacteria-Conditioned Medium
2.4. Purification of RNA and qRT-PCR
2.5. NF-kB RT-PCR Array
2.6. Preparation of Cellular Lysates and Immunoblotting
2.7. Quantification of Protein Levels
2.8. Proliferation, Migration, and Invasion Assays
2.9. Enzyme-Linked Immunosorbent Assay (ELISA)
2.10. Human Cytokine Antibody Array
2.11. Spheroid Formation Assay
2.12. Statistical Analysis
3. Results
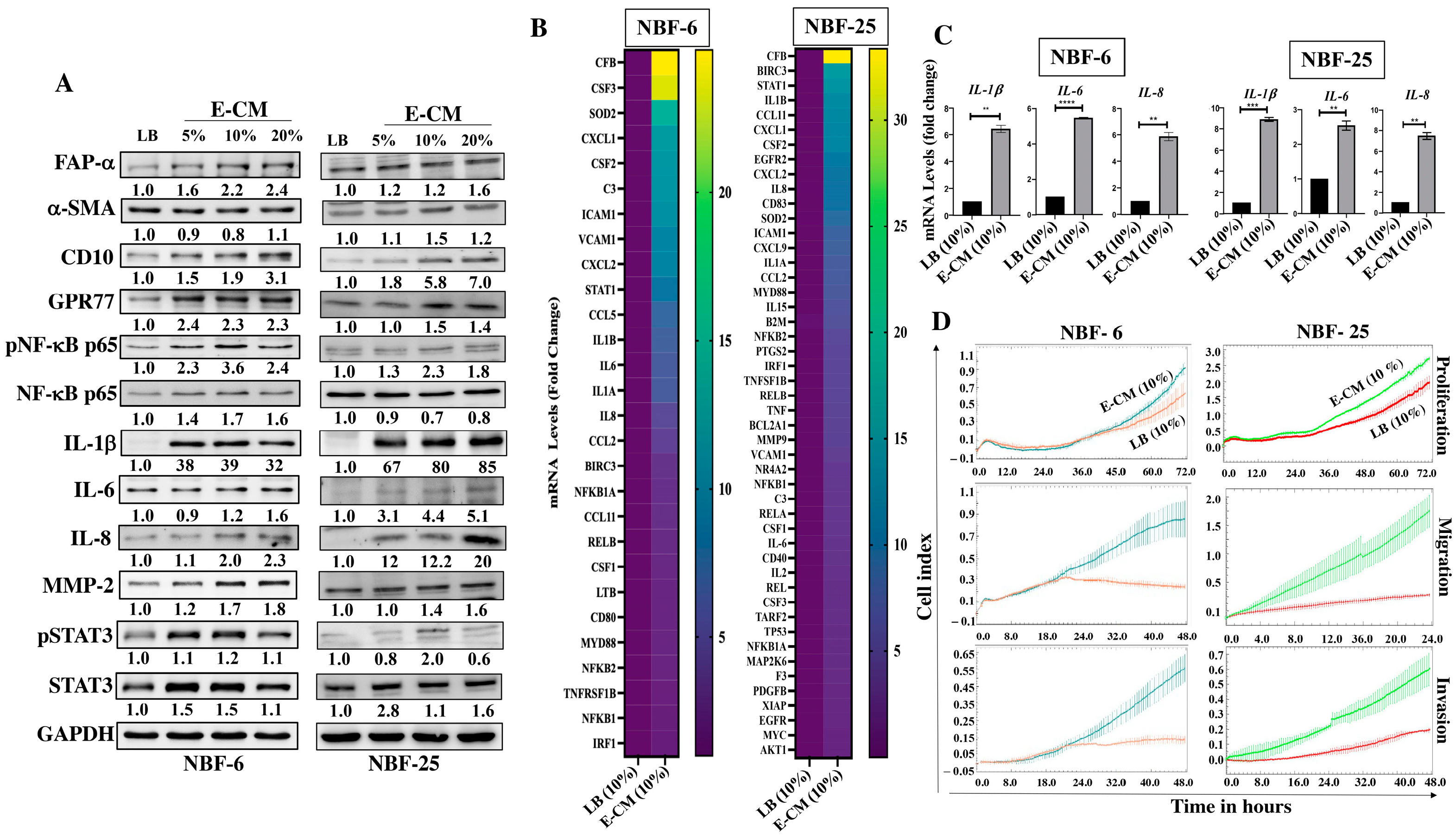
3.1. E. coli Metabolites Activate Breast Stromal Fibroblasts
3.2. E. coli-Metabolite-Activated Normal Breast Fibroblasts Secrete High Levels of Several Pro-Carcinogenic Cytokines
3.3. E. coli-Metabolites-Activated Normal Breast Fibroblasts Induce EMT and Stemness in Normal Breast Epithelial Cells in a Paracrine Manner
3.4. E. coli-Secreted Metabolites Induce EMT and Stemness in Normal Breast Epithelial Cells
3.5. Recombinant Human IL-1β Induces EMT and Stemness in Normal and Neoplastic Breast Epithelial Cells
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Barbazan, J.; Matic Vignjevic, D. Cancer associated fibroblasts: Is the force the path to the dark side? Curr. Opin. Cell Biol. 2019, 56, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Tan, Z.; Kan, C.; Sun, M.; Yang, F.; Wong, M.; Wang, S.; Zheng, H. Mapping Breast Cancer Microenvironment Through Single-Cell Omics. Front. Immunol. 2022, 13, 868813. [Google Scholar] [CrossRef] [PubMed]
- Hu, D.; Li, Z.; Zheng, B.; Lin, X.; Pan, Y.; Gong, P.; Zhuo, W.; Hu, Y.; Chen, C.; Chen, L.; et al. Cancer-associated fibroblasts in breast cancer: Challenges and opportunities. Cancer Commun. 2022, 42, 401–434. [Google Scholar] [CrossRef]
- Sahai, E.; Astsaturov, I.; Cukierman, E.; DeNardo, D.G.; Egeblad, M.; Evans, R.M.; Fearon, D.; Greten, F.R.; Hingorani, S.R.; Hunter, T.; et al. A framework for advancing our understanding of cancer-associated fibroblasts. Nat. Rev. Cancer 2020, 20, 174–186. [Google Scholar] [CrossRef]
- Toumazi, D.; Daccache, S.E.; Constantinou, C. An unexpected link: The role of mammary and gut microbiota on breast cancer development and management. Oncol. Rep. 2021, 45, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Urbaniak, C.; Gloor, G.B.; Brackstone, M.; Scott, L.; Tangney, M.; Reid, G. The Microbiota of Breast Tissue and Its Association with Breast Cancer. Appl. Environ. Microbiol. 2016, 82, 5039–5048. [Google Scholar] [CrossRef]
- Fu, A.; Yao, B.; Dong, T.; Chen, Y.; Yao, J.; Liu, Y.; Li, H.; Bai, H.; Liu, X.; Zhang, Y.; et al. Tumor-resident intracellular microbiota promotes metastatic colonization in breast cancer. Cell 2022, 185, 1356–1372.e26. [Google Scholar] [CrossRef]
- Nejman, D.; Livyatan, I.; Fuks, G.; Gavert, N.; Zwang, Y.; Geller, L.T.; Rotter-Maskowitz, A.; Weiser, R.; Mallel, G.; Gigi, E.; et al. The human tumor microbiome is composed of tumor type-specific intracellular bacteria. Science 2020, 368, 973–980. [Google Scholar] [CrossRef]
- Cullin, N.; Azevedo Antunes, C.; Straussman, R.; Stein-Thoeringer, C.K.; Elinav, E. Microbiome and cancer. Cancer Cell 2021, 39, 1317–1341. [Google Scholar] [CrossRef]
- Peters, B.A.; Kelly, L.; Wang, T.; Loudig, O.; Rohan, T.E. The Breast Microbiome in Breast Cancer Risk and Progression: A Narrative Review. Cancer Epidemiol. Biomark. Prev. 2024, 33, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Hieken, T.J.; Chen, J.; Hoskin, T.L.; Walther-Antonio, M.; Johnson, S.; Ramaker, S.; Xiao, J.; Radisky, D.C.; Knutson, K.L.; Kalari, K.R.; et al. The Microbiome of Aseptically Collected Human Breast Tissue in Benign and Malignant Disease. Sci. Rep. 2016, 6, 30751. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, S.; Wei, Z.; Tan, F.; Peck, K.N.; Shih, N.; Feldman, M.; Rebbeck, T.R.; Alwine, J.C.; Robertson, E.S. Distinct microbiological signatures associated with triple negative breast cancer. Sci. Rep. 2015, 5, 15162. [Google Scholar] [CrossRef] [PubMed]
- Hawsawi, N.M.; Ghebeh, H.; Hendrayani, S.F.; Tulbah, A.; Al-Eid, M.; Al-Tweigeri, T.; Ajarim, D.; Alaiya, A.; Dermime, S.; Aboussekhra, A. Breast carcinoma-associated fibroblasts and their counterparts display neoplastic-specific changes. Cancer Res. 2008, 68, 2717–2725. [Google Scholar] [CrossRef] [PubMed]
- Al-Mohanna, M.A.; Al-Khalaf, H.H.; Al-Yousef, N.; Aboussekhra, A. The p16INK4a tumor suppressor controls p21WAF1 induction in response to ultraviolet light. Nucleic Acids Res. 2007, 35, 223–233. [Google Scholar] [CrossRef]
- Su, S.; Chen, J.; Yao, H.; Liu, J.; Yu, S.; Lao, L.; Wang, M.; Luo, M.; Xing, Y.; Chen, F.; et al. CD10(+)GPR77(+) Cancer-Associated Fibroblasts Promote Cancer Formation and Chemoresistance by Sustaining Cancer Stemness. Cell 2018, 172, 841–856.e16. [Google Scholar] [CrossRef]
- Jiang, H.; Li, H. Prognostic values of tumoral MMP2 and MMP9 overexpression in breast cancer: A systematic review and meta-analysis. BMC Cancer 2021, 21, 149. [Google Scholar] [CrossRef]
- Marotta, L.L.; Almendro, V.; Marusyk, A.; Shipitsin, M.; Schemme, J.; Walker, S.R.; Bloushtain-Qimron, N.; Kim, J.J.; Choudhury, S.A.; Maruyama, R.; et al. The JAK2/STAT3 signaling pathway is required for growth of CD44(+)CD24(-) stem cell-like breast cancer cells in human tumors. J. Clin. Investig. 2011, 121, 2723–2735. [Google Scholar] [CrossRef]
- Hieken, T.J.; Chen, J.; Chen, B.; Johnson, S.; Hoskin, T.L.; Degnim, A.C.; Walther-Antonio, M.R.; Chia, N. The breast tissue microbiome, stroma, immune cells and breast cancer. Neoplasia 2022, 27, 100786. [Google Scholar] [CrossRef]
- Chen, J.; Douglass, J.; Prasath, V.; Neace, M.; Atrchian, S.; Manjili, M.H.; Shokouhi, S.; Habibi, M. The microbiome and breast cancer: A review. Breast Cancer Res. Treat. 2019, 178, 493–496. [Google Scholar] [CrossRef]
- Urbaniak, C.; Cummins, J.; Brackstone, M.; Macklaim, J.M.; Gloor, G.B.; Baban, C.K.; Scott, L.; O’Hanlon, D.M.; Burton, J.P.; Francis, K.P.; et al. Microbiota of human breast tissue. Appl. Environ. Microbiol. 2014, 80, 3007–3014. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wang, C.; Huang, T.; Yu, X.; Tian, B. The role of cancer-associated fibroblasts in breast cancer metastasis. Front. Oncol. 2023, 13, 1194835. [Google Scholar] [CrossRef] [PubMed]
- Krzysiek-Maczka, G.; Targosz, A.; Szczyrk, U.; Strzalka, M.; Sliwowski, Z.; Brzozowski, T.; Czyz, J.; Ptak-Belowska, A. Role of Helicobacter pylori infection in cancer-associated fibroblast-induced epithelial-mesenchymal transition in vitro. Helicobacter 2018, 23, e12538. [Google Scholar] [CrossRef] [PubMed]
- Shen, J.; Zhai, J.; You, Q.; Zhang, G.; He, M.; Yao, X.; Shen, L. Cancer-associated fibroblasts-derived VCAM1 induced by H. pylori infection facilitates tumor invasion in gastric cancer. Oncogene 2020, 39, 2961–2974. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Zhou, Q.; Wu, X.; Xu, S.; Hu, X.; Tao, X.; Li, B.; Peng, J.; Li, D.; Shen, L.; et al. VCAM-1 secreted from cancer-associated fibroblasts enhances the growth and invasion of lung cancer cells through AKT and MAPK signaling. Cancer Lett. 2020, 473, 62–73. [Google Scholar] [CrossRef]
- Fabbri, A.; Travaglione, S.; Rosadi, F.; Ballan, G.; Maroccia, Z.; Giambenedetti, M.; Guidotti, M.; Odum, N.; Krejsgaard, T.; Fiorentini, C. The Escherichia coli protein toxin cytotoxic necrotizing factor 1 induces epithelial mesenchymal transition. Cell. Microbiol. 2020, 22, e13138. [Google Scholar] [CrossRef]
- Li, Y.; Wang, L.; Pappan, L.; Galliher-Beckley, A.; Shi, J. IL-1beta promotes stemness and invasiveness of colon cancer cells through Zeb1 activation. Mol. Cancer 2012, 11, 87. [Google Scholar] [CrossRef]




| Primers | Sequence | |
|---|---|---|
| IL-6 | Forward | 5′-AGACAG CCA CTC ACC TCT TCA G-3′ |
| Reverse | 5′-TTC TGC CAG TGC CTC TTT GCT G-3′ | |
| IL-8 | Forward | 5′-GAT CCA CAA GTC CTT GTT CCA-3′ |
| Reverse | 5′-GCT TCC ACA TGT CCT CAC AA-3′ | |
| GAPDH | Forward | 5′-GAGTCCACTGGCGTCTTC-3′ |
| Reverse | 5′-GGGGTGCTAAGCAGTTGGT-3′ | |
| IL-1β | Forward | 5′-GCTGGAATTTGAGTCTGCCC-3′ |
| Reverse | 5′-TCCACATTCAGCACAGGACT-3′ | |
| Gene | NBF-6 | NBF-25 |
|---|---|---|
| CFB | 24.8 | 33.4 |
| BIRC3 | 3.3 | 15.8 |
| STAT1 | 8.2 | 14.3 |
| IL1b | 6.5 | 9.8 |
| CCL11 | 3.0 | 12.7 |
| CXCL1 | 12.1 | 12.3 |
| CSF2 | 11.8 | 12.2 |
| CXCL2 | 9.6 | 10 |
| IL8 | 4.7 | 9.8 |
| ICAM1 | 10.9 | 7.9 |
| IL1A | 6.1 | 7.3 |
| CCL2 | 4.1 | 7.2 |
| MYD88 | 2.5 | 6.9 |
| NFKB2 | 2.4 | 5.2 |
| IRF1 | 2 | 4.9 |
| TNFSF1B | 2.2 | 4.9 |
| RELB | 2.8 | 4.9 |
| VCAM1 | 9.6 | 4.2 |
| NFKB1 | 2.1 | 3.6 |
| C3 | 11.6 | 3.5 |
| CSF1 | 2.6 | 3.4 |
| IL6 | 6.1 | 3.3 |
| CSF3 | 23.3 | 2.8 |
| NFKB1A | 3.1 | 2.7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alshehri, J.H.; Al-Nasrallah, H.K.; Al-Ansari, M.M.; Aboussekhra, A. Activation of Mammary Epithelial and Stromal Fibroblasts upon Exposure to Escherichia coli Metabolites. Cells 2024, 13, 1723. https://doi.org/10.3390/cells13201723
Alshehri JH, Al-Nasrallah HK, Al-Ansari MM, Aboussekhra A. Activation of Mammary Epithelial and Stromal Fibroblasts upon Exposure to Escherichia coli Metabolites. Cells. 2024; 13(20):1723. https://doi.org/10.3390/cells13201723
Chicago/Turabian StyleAlshehri, Jamilah H., Huda K. Al-Nasrallah, Mysoon M. Al-Ansari, and Abdelilah Aboussekhra. 2024. "Activation of Mammary Epithelial and Stromal Fibroblasts upon Exposure to Escherichia coli Metabolites" Cells 13, no. 20: 1723. https://doi.org/10.3390/cells13201723
APA StyleAlshehri, J. H., Al-Nasrallah, H. K., Al-Ansari, M. M., & Aboussekhra, A. (2024). Activation of Mammary Epithelial and Stromal Fibroblasts upon Exposure to Escherichia coli Metabolites. Cells, 13(20), 1723. https://doi.org/10.3390/cells13201723





