Evaluation of Blood Tumor Mutation Burden for the Efficacy of Second-Line Atezolizumab Treatment in Non-Small Cell Lung Cancer: BUDDY Trial
Abstract
1. Introduction
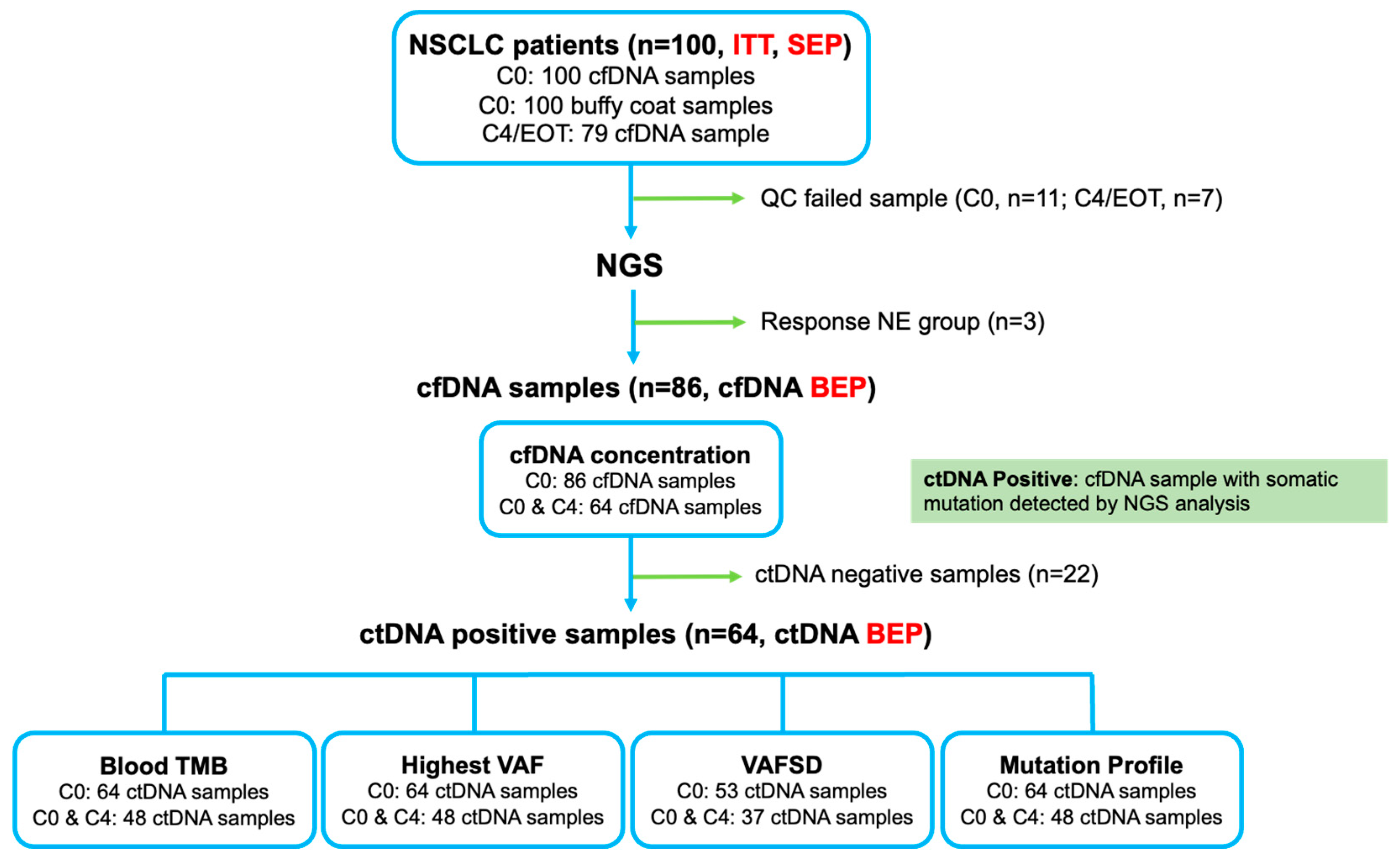
2. Materials and Methods
2.1. Study Design, Patients, and Procedures
2.2. Blood Sample Collection and Processing
2.3. Preparation and Quantification of cfDNA
2.4. Targeted NGS and Analysis of bTMB and Other Biomarkers
2.5. Variant Calling and Filtering for Analysis of the bTMB and Other Candidate Biomarkers
2.6. Outcomes and Statistical Analyses
3. Results
3.1. Patient Characteristics and Efficacy of Atezolizumab
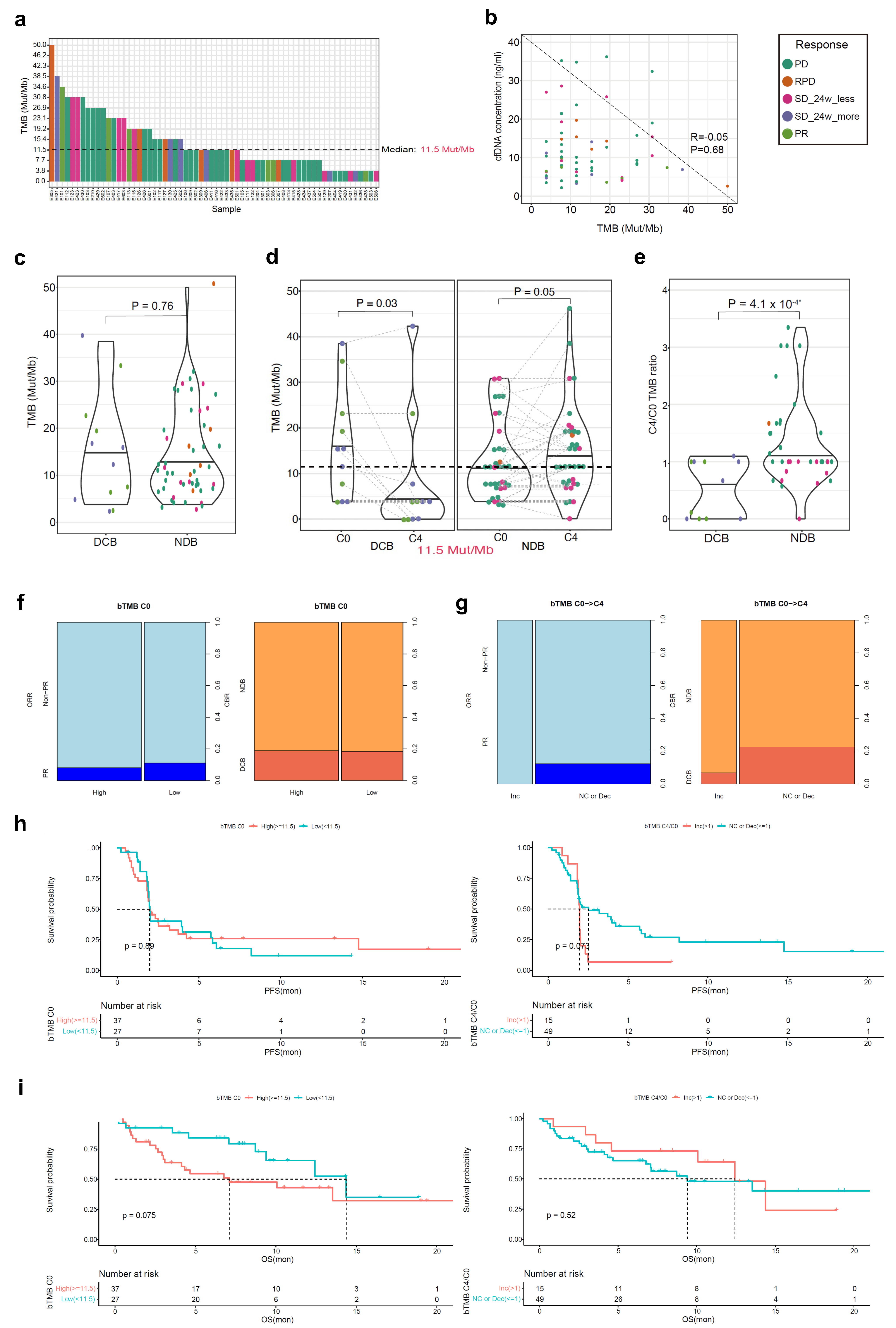
3.2. bTMB as a Biomarker for Atezolizumab Response
3.3. cfDNA Concentration as a Biomarker for Atezolizumab Response
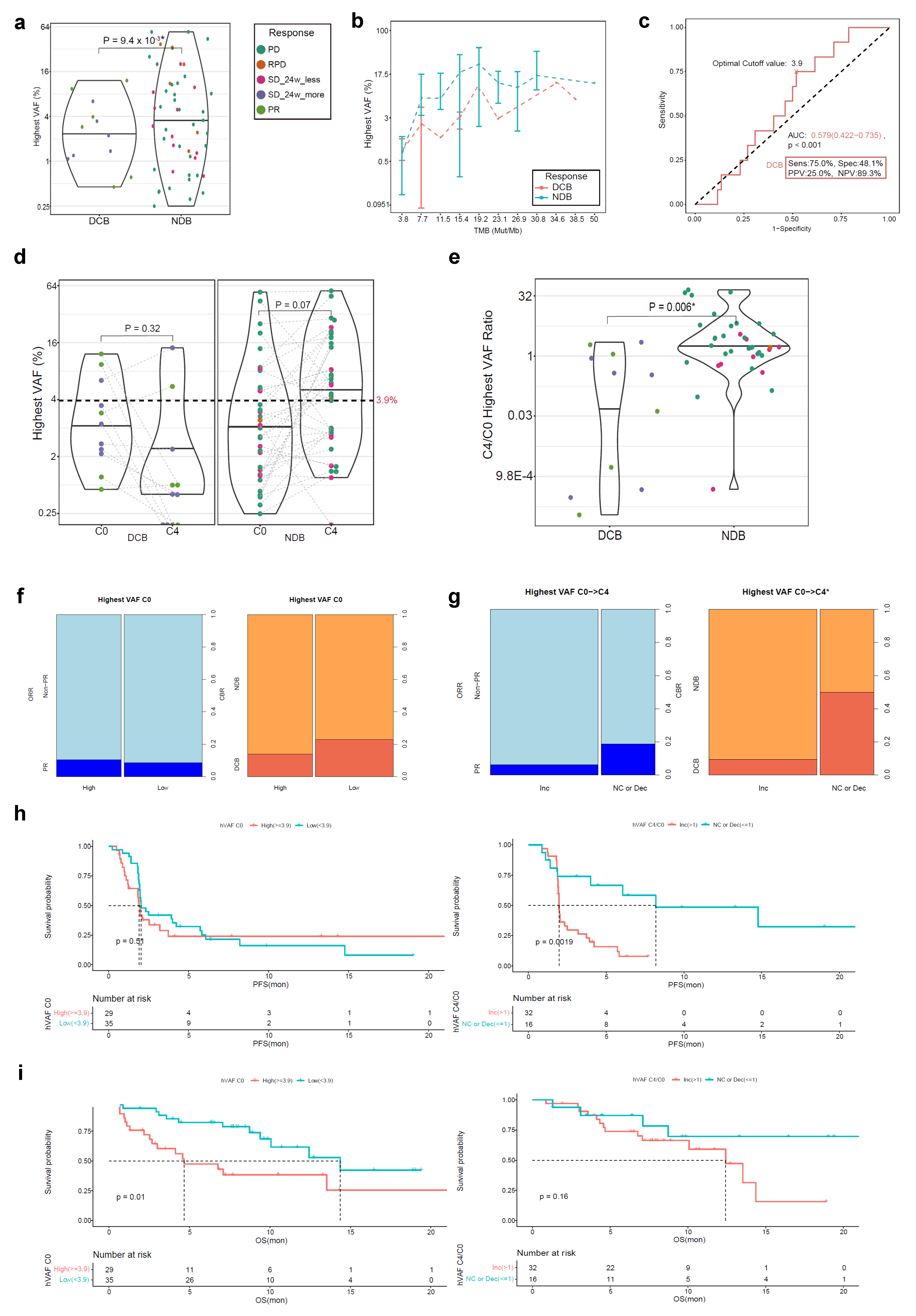
3.4. ctDNA hVAF as a Biomarker for Atezolizumab Response
3.5. VAFSD in ctDNA as a Biomarker for Atezolizumab Response
3.6. Mutation Profiling
3.7. Subgroup Analysis for PFS and OS in the cfDNA BEP
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Inclusion and Exclusion Criteria
Appendix A.1. Inclusion Criteria
- (1)
- Provision of informed consent prior to any study-specific procedures
- (2)
- Willingness and ability to comply with the protocol for the duration of the study, including undergoing treatment and scheduled visits and examinations, including follow-up
- (3)
- Age ≥ 18 years
- (4)
- Histologically or cytologically confirmed, locally advanced or metastatic (i.e., stage IIIB-IV not suitable for definitive concurrent chemoradiation therapy or relapsed) non-small cell lung carcinoma (NSCLC)
- (5)
- Confirmed disease progression during or after platinum-based chemotherapy
- (i)
- A patient is allowed to receive one or more additional cytotoxic chemotherapy
- (ii)
- A patient with epidermal growth factor receptor (EGFR) mutation or anaplastic lymphoma kinase (ALK) rearrangement should have confirmed disease progression even after the administration of approved oncogene-directed therapy prior to atezolizumab
- (6)
- At least one measurable lesion defined using the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1
- (7)
- Eastern Cooperative Oncology Group performance status (ECOG PS) score of 0–2
- (8)
- Life expectancy ≥12 weeks
- (9)
- The normal function of the main organs:
- (i)
- WBC: >2500/mm3 (Neutrophil count: >1000/mm3)
- (ii)
- Hemoglobin: >8.0 g/dL
- (iii)
- Total bilirubin: ≤2.5 × ULN
- (iv)
- A patient with known Gilbert syndrome with serum bilirubin ≤3 × ULN can be registered
- (v)
- AST, ALT, and ALP ≤2.5 × UNL, exceptions for:
- (vi)
- A patient with liver metastasis: AST and ALT ≤ 5 × ULN
- (vii)
- A patient with liver or bone metastasis: ALP ≤ 5 × ULN
Appendix A.2. Exclusion Criteria
- (1)
- Active central nervous system (CNS) metastasis
- ▪
- Patients with a history of pretreated, asymptomatic CNS metastasis or patients with asymptomatic brain metastasis could be registered.
- (2)
- Presence of an active double cancer other than NSCLC within five years prior to enrollment, except malignant disease with negligible risk of metastasis or death and treated with curative intent such as adequately treated carcinoma in situ of the cervix, basal or squamous cell skin cancer, localized prostate cancer or ductal carcinoma in situ treated with curative intent.
- ▪
- If there were a history of a malignant disease other than NSCLC, the patient could be registered if the diagnosis of the malignant disease exceeded five years based on the enrollment and treatment was completed
- (3)
- Pregnant and lactating women
- ▪
- A woman of childbearing age: Very effective contraception should be used during the administration of atezolizumab and for at least five months after the last administration.
- (4)
- Significant cardiovascular diseases such as New York Heart Association (NYHA) class II or higher or myocardial infarction within three months prior to enrollment
- (5)
- A patient with an active autoimmune disorder or a history of a chronic or recurrent autoimmune disorder
- ▪
- A patient with a history of autoimmune-mediated hypothyroidism when administering stable doses of thyroid hormone replacement may have been eligible for registration in this study
- ▪
- Patients with type 1 diabetes controlled by a stable insulin dose could be registered
- (6)
- Uncontrolled idiopathic pulmonary fibrosis or drug-induced pneumonitis
- (7)
- Administration of systemic corticosteroids or other systemic immunosuppressive drugs (prednisone, dexamethasone, cyclophosphamide, azathioprine, methotrexate, thalidomide, and anti-TNF agents) within two weeks prior to enrollment
- ▪
- Inhaled corticosteroids, megestrol acetate, and premedication up to three days were acceptable.
- (8)
- Hypersensitivity to atezolizumab and its component
References
- Herbst, R.S.; Baas, P.; Kim, D.W.; Felip, E.; Pérez-Gracia, J.L.; Han, J.Y.; Molina, J.; Kim, J.H.; Arvis, C.D.; Ahn, M.J.; et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): A randomised controlled trial. Lancet 2016, 387, 1540–1550. [Google Scholar] [CrossRef] [PubMed]
- Reck, M.; Rodríguez-Abreu, D.; Robinson, A.G.; Hui, R.; Csőszi, T.; Fülöp, A.; Gottfried, M.; Peled, N.; Tafreshi, A.; Cuffe, S.; et al. Updated Analysis of KEYNOTE-024: Pembrolizumab Versus Platinum-Based Chemotherapy for Advanced Non-Small-Cell Lung Cancer with PD-L1 Tumor Proportion Score of 50% or Greater. J. Clin. Oncol. 2019, 37, 537–546. [Google Scholar] [CrossRef] [PubMed]
- Herbst, R.S.; Giaccone, G.; de Marinis, F.; Reinmuth, N.; Vergnenegre, A.; Barrios, C.H.; Morise, M.; Felip, E.; Andric, Z.; Geater, S.; et al. Atezolizumab for First-Line Treatment of PD-L1-Selected Patients with NSCLC. N. Engl. J. Med. 2020, 383, 1328–1339. [Google Scholar] [CrossRef]
- Mazieres, J.; Rittmeyer, A.; Gadgeel, S.; Hida, T.; Gandara, D.R.; Cortinovis, D.L.; Barlesi, F.; Yu, W.; Matheny, C.; Ballinger, M.; et al. Atezolizumab Versus Docetaxel in Pretreated Patients with NSCLC: Final Results from the Randomized Phase 2 POPLAR and Phase 3 OAK Clinical Trials. J. Thorac. Oncol. 2021, 16, 140–150. [Google Scholar] [CrossRef]
- Juarez-Garcia, A.; Sharma, R.; Hunger, M.; Kayaniyil, S.; Penrod, J.R.; Chouaïd, C. Real-world effectiveness of immunotherapies in pre-treated, advanced non-small cell lung cancer Patients: A systematic literature review. Lung Cancer 2022, 166, 205–220. [Google Scholar] [CrossRef]
- Mok, T.S.K.; Wu, Y.L.; Kudaba, I.; Kowalski, D.M.; Cho, B.C.; Turna, H.Z.; Castro, G., Jr.; Srimuninnimit, V.; Laktionov, K.K.; Bondarenko, I.; et al. Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): A randomised, open-label, controlled, phase 3 trial. Lancet 2019, 393, 1819–1830. [Google Scholar] [CrossRef]
- Tray, N.; Weber, J.S.; Adams, S. Predictive Biomarkers for Checkpoint Immunotherapy: Current Status and Challenges for Clinical Application. Cancer Immunol. Res. 2018, 6, 1122–1128. [Google Scholar] [CrossRef]
- Kim, H.; Kwon, H.J.; Kim, E.S.; Kwon, S.; Suh, K.J.; Kim, S.H.; Kim, Y.J.; Lee, J.S.; Chung, J.H. Comparison of the Predictive Power of a Combination versus Individual Biomarker Testing in Non-Small Cell Lung Cancer Patients Treated with Immune Checkpoint Inhibitors. Cancer Res. Treat. 2022, 54, 424–433. [Google Scholar] [CrossRef]
- Yarchoan, M.; Albacker, L.A.; Hopkins, A.C.; Montesion, M.; Murugesan, K.; Vithayathil, T.T.; Zaidi, N.; Azad, N.S.; Laheru, D.A.; Frampton, G.M.; et al. PD-L1 expression and tumor mutational burden are independent biomarkers in most cancers. JCI Insight 2019, 4, e126908. [Google Scholar] [CrossRef] [PubMed]
- Gandara, D.R.; Paul, S.M.; Kowanetz, M.; Schleifman, E.; Zou, W.; Li, Y.; Rittmeyer, A.; Fehrenbacher, L.; Otto, G.; Malboeuf, C.; et al. Blood-based tumor mutational burden as a predictor of clinical benefit in non-small-cell lung cancer patients treated with atezolizumab. Nat. Med. 2018, 24, 1441–1448. [Google Scholar] [CrossRef]
- Wang, H.; Zhou, F.; Qiao, M.; Li, X.; Zhao, C.; Cheng, L.; Chen, X.; Zhou, C. The Role of Circulating Tumor DNA in Advanced Non-Small Cell Lung Cancer Patients Treated with Immune Checkpoint Inhibitors: A Systematic Review and Meta-Analysis. Front. Oncol. 2021, 11, 671874. [Google Scholar] [CrossRef] [PubMed]
- Nabet, B.Y.; Esfahani, M.S.; Moding, E.J.; Hamilton, E.G.; Chabon, J.J.; Rizvi, H.; Steen, C.B.; Chaudhuri, A.A.; Liu, C.L.; Hui, A.B.; et al. Noninvasive Early Identification of Therapeutic Benefit from Immune Checkpoint Inhibition. Cell 2020, 183, 363–376.e313. [Google Scholar] [CrossRef] [PubMed]
- Park, C.K.; Oh, H.J.; Kim, M.S.; Koh, B.G.; Cho, H.J.; Kim, Y.C.; Yang, H.J.; Lee, J.Y.; Chun, S.M.; Oh, I.J. Comprehensive analysis of blood-based biomarkers for predicting immunotherapy benefits in patients with advanced non-small cell lung cancer. Transl. Lung Cancer Res. 2021, 10, 2103–2117. [Google Scholar] [CrossRef] [PubMed]
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef]
- Qin, A.; Street, L.; Cease, K.; Viglianti, B.L.; Warren, E.H.; Zhao, L.; Ramnath, N. Clinical Determinants of Durable Clinical Benefit of Pembrolizumab in Veterans with Advanced Non-Small-Cell Lung Cancer. Clin. Lung Cancer 2017, 18, 559–564. [Google Scholar] [CrossRef]
- Proctor, M.J.; McMillan, D.C.; Morrison, D.S.; Fletcher, C.D.; Horgan, P.G.; Clarke, S.J. A derived neutrophil to lymphocyte ratio predicts survival in patients with cancer. Br. J. Cancer 2012, 107, 695–699. [Google Scholar] [CrossRef]
- Team, R.C. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021; Available online: https://www.R-project.org/ (accessed on 1 November 2021).
- Bratman, S.V.; Yang, S.Y.C.; Iafolla, M.A.J.; Liu, Z.; Hansen, A.R.; Bedard, P.L.; Lheureux, S.; Spreafico, A.; Razak, A.A.; Shchegrova, S.; et al. Personalized circulating tumor DNA analysis as a predictive biomarker in solid tumor patients treated with pembrolizumab. Nat. Cancer 2020, 1, 873–881. [Google Scholar] [CrossRef]
- Ba, H.; Liu, L.; Peng, Q.; Chen, J.; Zhu, Y.D. The relationship between blood-based tumor mutation burden level and efficacy of PD-1/PD-L1 inhibitors in advanced non-small cell lung cancer: A systematic review and meta-analysis. BMC Cancer 2021, 21, 1220. [Google Scholar] [CrossRef]
- Van Campenhout, C.; Meléndez, B.; Remmelink, M.; Salmon, I.; D’Haene, N. Blood tumor mutational burden: Are we ready for clinical implementation? J. Thorac. Dis. 2019, 11, S1906–S1908. [Google Scholar] [CrossRef]
- Peters, S.; Dziadziuszko, R.; Morabito, A.; Felip, E.; Gadgeel, S.M.; Cheema, P.; Cobo, M.; Andric, Z.; Barrios, C.H.; Yamaguchi, M.; et al. Atezolizumab versus chemotherapy in advanced or metastatic NSCLC with high blood-based tumor mutational burden: Primary analysis of BFAST cohort C randomized phase 3 trial. Nat. Med. 2022, 28, 1831–1839. [Google Scholar] [CrossRef]
- Cheng, M.L.; Pectasides, E.; Hanna, G.J.; Parsons, H.A.; Choudhury, A.D.; Oxnard, G.R. Circulating tumor DNA in advanced solid tumors: Clinical relevance and future directions. CA Cancer J. Clin. 2021, 71, 176–190. [Google Scholar] [CrossRef] [PubMed]
- Jiang, T.; Chen, J.; Xu, X.; Cheng, Y.; Chen, G.; Pan, Y.; Fang, Y.; Wang, Q.; Huang, Y.; Yao, W.; et al. On-treatment blood TMB as predictors for camrelizumab plus chemotherapy in advanced lung squamous cell carcinoma: Biomarker analysis of a phase III trial. Mol. Cancer 2022, 21, 4. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Duan, J.; Wang, G.; Zhao, J.; Xu, J.; Han, J.; Zhao, Z.; Zhao, J.; Zhu, B.; Zhuo, M.; et al. Allele Frequency-Adjusted Blood-Based Tumor Mutational Burden as a Predictor of Overall Survival for Patients with NSCLC Treated with PD-(L)1 Inhibitors. J. Thorac. Oncol. 2020, 15, 556–567. [Google Scholar] [CrossRef]
- Kim, E.S.; Velcheti, V.; Mekhail, T.; Yun, C.; Shagan, S.M.; Hu, S.; Chae, Y.K.; Leal, T.A.; Dowell, J.E.; Tsai, M.L.; et al. Blood-based tumor mutational burden as a biomarker for atezolizumab in non-small cell lung cancer: The phase 2 B-F1RST trial. Nat. Med. 2022, 28, 939–945. [Google Scholar] [CrossRef]
- Zhang, Q.; Luo, J.; Wu, S.; Si, H.; Gao, C.; Xu, W.; Abdullah, S.E.; Higgs, B.W.; Dennis, P.A.; van der Heijden, M.S.; et al. Prognostic and Predictive Impact of Circulating Tumor DNA in Patients with Advanced Cancers Treated with Immune Checkpoint Blockade. Cancer Discov. 2020, 10, 1842–1853. [Google Scholar] [CrossRef] [PubMed]
- Nicos, M.; Krawczyk, P.; Crosetto, N.; Milanowski, J. The Role of Intratumor Heterogeneity in the Response of Metastatic Non-Small Cell Lung Cancer to Immune Checkpoint Inhibitors. Front. Oncol. 2020, 10, 569202. [Google Scholar] [CrossRef]
- Vitale, I.; Shema, E.; Loi, S.; Galluzzi, L. Intratumoral heterogeneity in cancer progression and response to immunotherapy. Nat. Med. 2021, 27, 212–224. [Google Scholar] [CrossRef]
- Zhang, J.; Fujimoto, J.; Zhang, J.; Wedge, D.C.; Song, X.; Zhang, J.; Seth, S.; Chow, C.W.; Cao, Y.; Gumbs, C.; et al. Intratumor heterogeneity in localized lung adenocarcinomas delineated by multiregion sequencing. Science 2014, 346, 256–259. [Google Scholar] [CrossRef]
- Fang, W.; Jin, H.; Zhou, H.; Hong, S.; Ma, Y.; Zhang, Y.; Su, X.; Chen, L.; Yang, Y.; Xu, S.; et al. Intratumoral heterogeneity as a predictive biomarker in anti-PD-(L)1 therapies for non-small cell lung cancer. Mol. Cancer 2021, 20, 37. [Google Scholar] [CrossRef]
- Liu, Z.; Xie, Z.; Zhao, S.; Ye, D.; Cai, X.; Cheng, B.; Li, C.; Xiong, S.; Li, J.; Liang, H.; et al. Presence of allele frequency heterogeneity defined by ctDNA profiling predicts unfavorable overall survival of NSCLC. Transl. Lung Cancer Res. 2019, 8, 1045–1050. [Google Scholar] [CrossRef]
- Zhou, J.; Bao, M.; Gao, G.; Cai, Y.; Wu, L.; Lei, L.; Zhao, J.; Ji, X.; Huang, Y.; Su, C. Increased blood-based intratumor heterogeneity (bITH) is associated with unfavorable outcomes of immune checkpoint inhibitors plus chemotherapy in non-small cell lung cancer. BMC Med. 2022, 20, 256. [Google Scholar] [CrossRef] [PubMed]



| Characteristics | No. of Patients, n = 100 |
|---|---|
| Age, years | 65.0 (42–82) |
| Sex: Male/Female | 84/16 |
| ECOG PS score: 0/1/2 | 7/92/1 |
| Smoking: Never/Ex/Current smoker | 21/66/13 |
| Pack-years | 40.0 (1–100) |
| Histology | |
| Squamous cell carcinoma | 39 |
| Adenocarcinoma | 52 |
| NSCLC, NOS | 7 |
| Others 1 | 2 |
| Clinical stage (TNM 8th) | |
| IIIB/IIIC | 5/3 |
| IVA/IVB | 51/39 |
| Recurrence | 2 |
| EGFR mutation, tested | 80 (100.0) |
| Positive | 11 (13.8) |
| Wild type | 69 (86.3) |
| ALK fusion, tested: FISH/IHC/both | 74 (100.0): 35/36/3 |
| Positive | 1 (1.4) |
| Negative | 73 (98.6) |
| ROS1 fusion, tested: FISH/PCR/IHC | 35 (100.0): 6/28/1 |
| Positive | 0 (0.0) |
| Negative | 35 (100.0) |
| PD-L1 TPS, tested: 22C3/SP263/SP142 | 95: 67/84/15 |
| 22C3: 0%/1–49%/≥50% | 24 (35.8)/17 (25.4)/26 (38.8) |
| SP263: 0%/1–49%/≥50% | 27 (32.1)/28 (33.4)/29 (34.5) |
| SP142 (TC): 0%/1–4%/5–49%/≥50% | 11 (73.3)/2 (13.4)/1 (6.7)/1 (6.7) |
| SP142 (IC): 0%/1–4%/5–9%/≥10% | 12 (80.0)/3 (20.0)/0 (0.0)/0 (0.0) |
| Prior chemotherapy (last) | 100 |
| Numbers: 1/2/3/4 | 67/22/7/4 |
| Aim: Palliative/CCRT 2 | 93/7 |
| Regimen | |
| Platinum doublet | 93 |
| Cytotoxic monotherapy | 3 |
| Tyrosine kinase inhibitor | 3 |
| Others 3 | 1 |
| Treatment duration, months | 5.3 (0.7–36.3) |
| Best response: CR/PR/SD/PD/Unknown | 0/31/44/24/1 |
| Reason for cessation of treatment | |
| Completion | 8 |
| Progression | 90 |
| Patient refusal | 1 |
| Investigator’s judgment | 1 |
| Variables | No. of Patients, n = 100 |
|---|---|
| Atezolizumab cycles | 3 (1–32) |
| Reason for cessation of treatment | |
| Progression | 64 |
| Adverse events | 9 |
| Withdrawal of consent | 6 |
| Others | 21 |
| Best response | |
| CR | 0 |
| PR | 10 |
| SD: ≥24weeks/<24 weeks | 15/18 |
| PD 1 | 54 |
| NE | 3 |
| Objective response rate, % | 10 |
| Durable clinical benefit, % | 25 |
| Progression | |
| Confirmed progression | 76 |
| No progression | 20 |
| Unknown | 4 |
| Follow-up duration, months, median (95% CI) | 12.3 (10.0–14.6) |
| PFS, months, median (95% CI) | 2.1 (1.6–3.0) |
| DoR, months, median (95% CI) | NR |
| OS, months, median (95% CI) | 13.1 (10.1–16.2) |
| Alive | 42 |
| Death | 39 |
| Lost to follow-up | 13 |
| Withdrawal of consent | 6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, C.-K.; Jun, H.R.; Oh, H.-J.; Lee, J.-Y.; Cho, H.-J.; Kim, Y.-C.; Lee, J.E.; Yoon, S.H.; Choi, C.M.; Lee, J.C.; et al. Evaluation of Blood Tumor Mutation Burden for the Efficacy of Second-Line Atezolizumab Treatment in Non-Small Cell Lung Cancer: BUDDY Trial. Cells 2023, 12, 1246. https://doi.org/10.3390/cells12091246
Park C-K, Jun HR, Oh H-J, Lee J-Y, Cho H-J, Kim Y-C, Lee JE, Yoon SH, Choi CM, Lee JC, et al. Evaluation of Blood Tumor Mutation Burden for the Efficacy of Second-Line Atezolizumab Treatment in Non-Small Cell Lung Cancer: BUDDY Trial. Cells. 2023; 12(9):1246. https://doi.org/10.3390/cells12091246
Chicago/Turabian StylePark, Cheol-Kyu, Ha Ra Jun, Hyung-Joo Oh, Ji-Young Lee, Hyun-Ju Cho, Young-Chul Kim, Jeong Eun Lee, Seong Hoon Yoon, Chang Min Choi, Jae Cheol Lee, and et al. 2023. "Evaluation of Blood Tumor Mutation Burden for the Efficacy of Second-Line Atezolizumab Treatment in Non-Small Cell Lung Cancer: BUDDY Trial" Cells 12, no. 9: 1246. https://doi.org/10.3390/cells12091246
APA StylePark, C.-K., Jun, H. R., Oh, H.-J., Lee, J.-Y., Cho, H.-J., Kim, Y.-C., Lee, J. E., Yoon, S. H., Choi, C. M., Lee, J. C., Lee, S. Y., Lee, S. Y., Chun, S.-M., & Oh, I.-J. (2023). Evaluation of Blood Tumor Mutation Burden for the Efficacy of Second-Line Atezolizumab Treatment in Non-Small Cell Lung Cancer: BUDDY Trial. Cells, 12(9), 1246. https://doi.org/10.3390/cells12091246








