Clinical Trials Using Mesenchymal Stem Cells for Spinal Cord Injury: Challenges in Generating Evidence
Abstract
1. Introduction
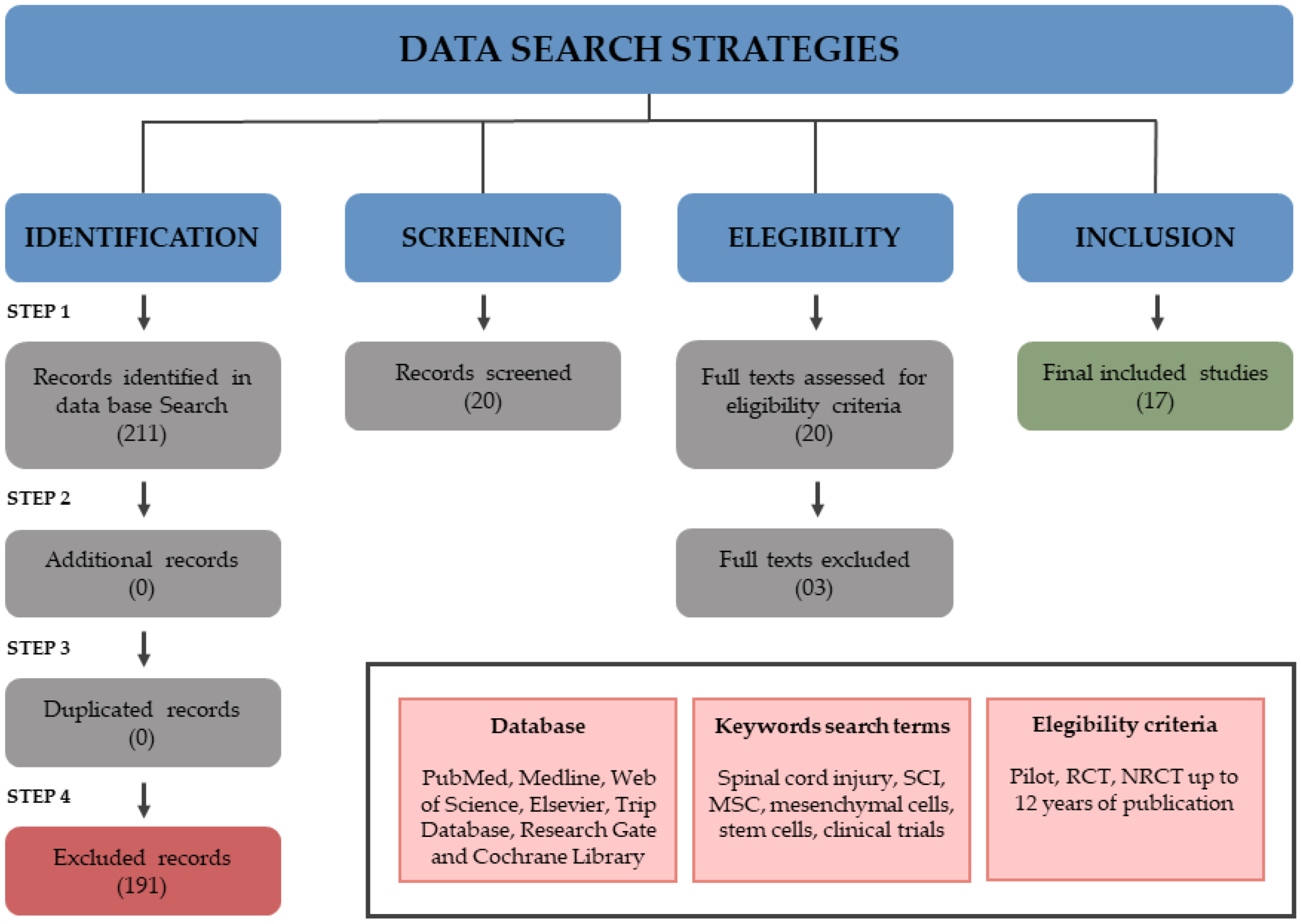
2. Materials and Methods
2.1. Study Design and Data Search Strategies
2.2. Selection Criteria
2.3. Data Extraction
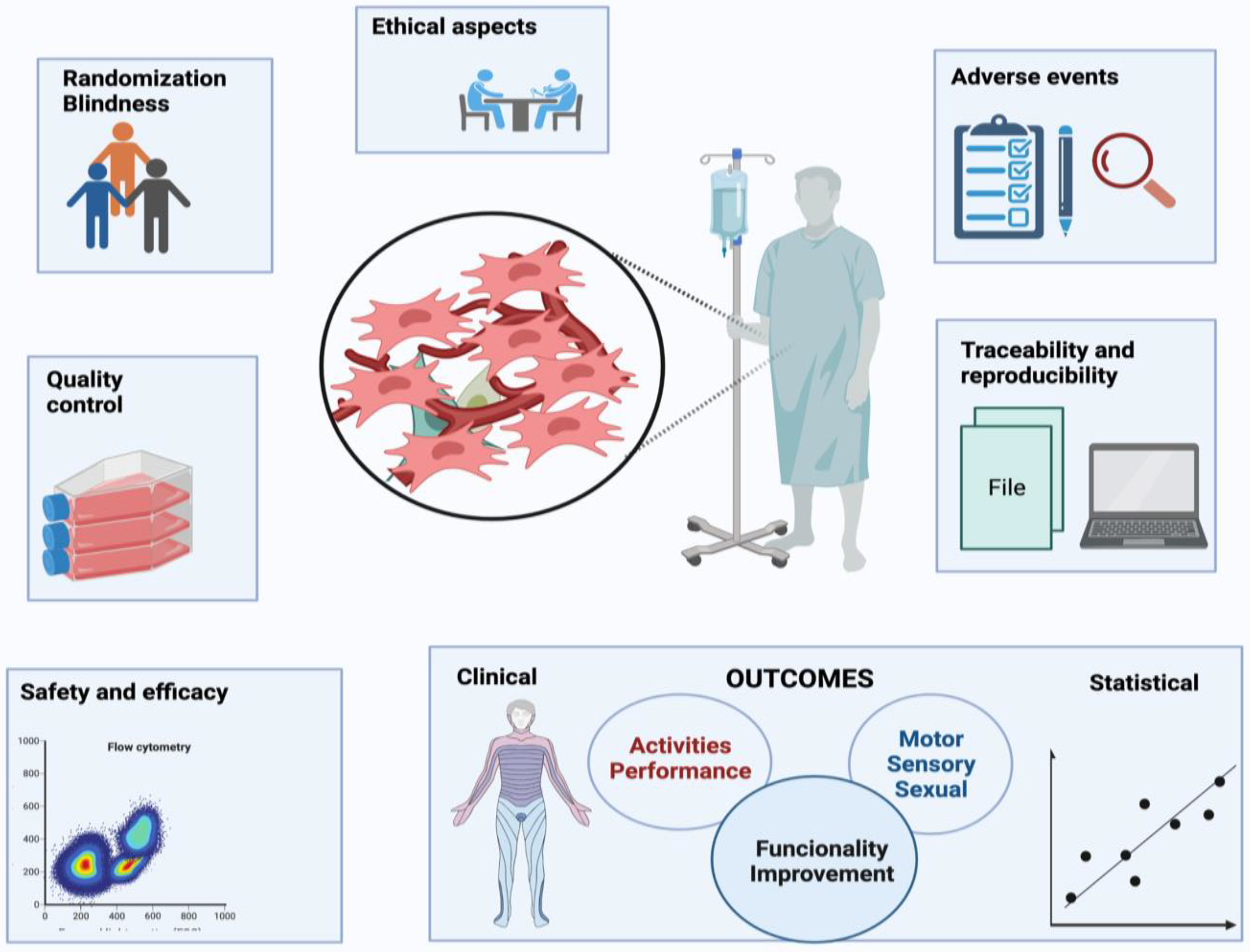
3. Results and Discussion
3.1. Clinical Trials’ Main Variables
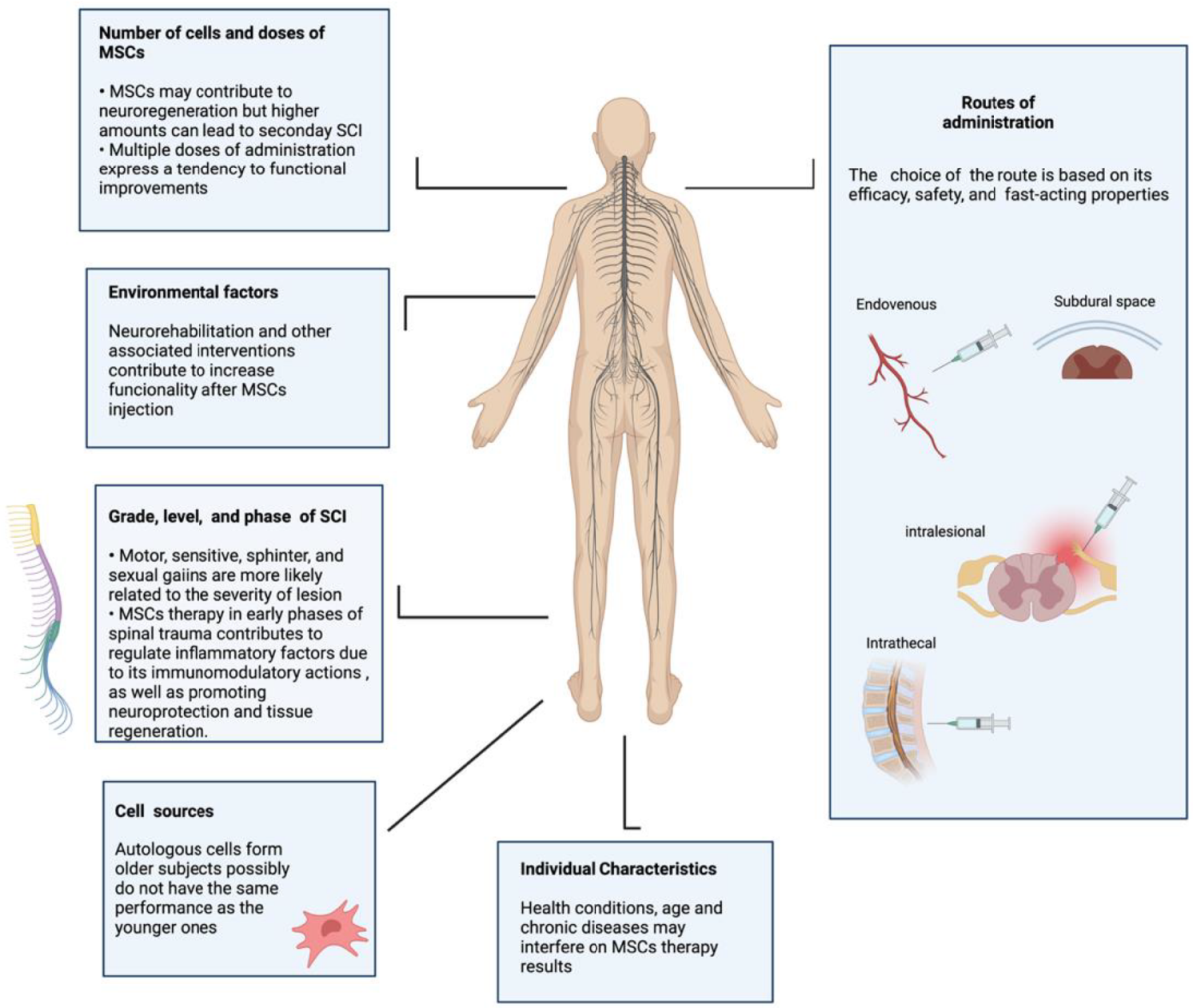
3.2. The Importance of Grade, Level, and Severity of a Lesion
3.3. Spinal Cord Injury Phases
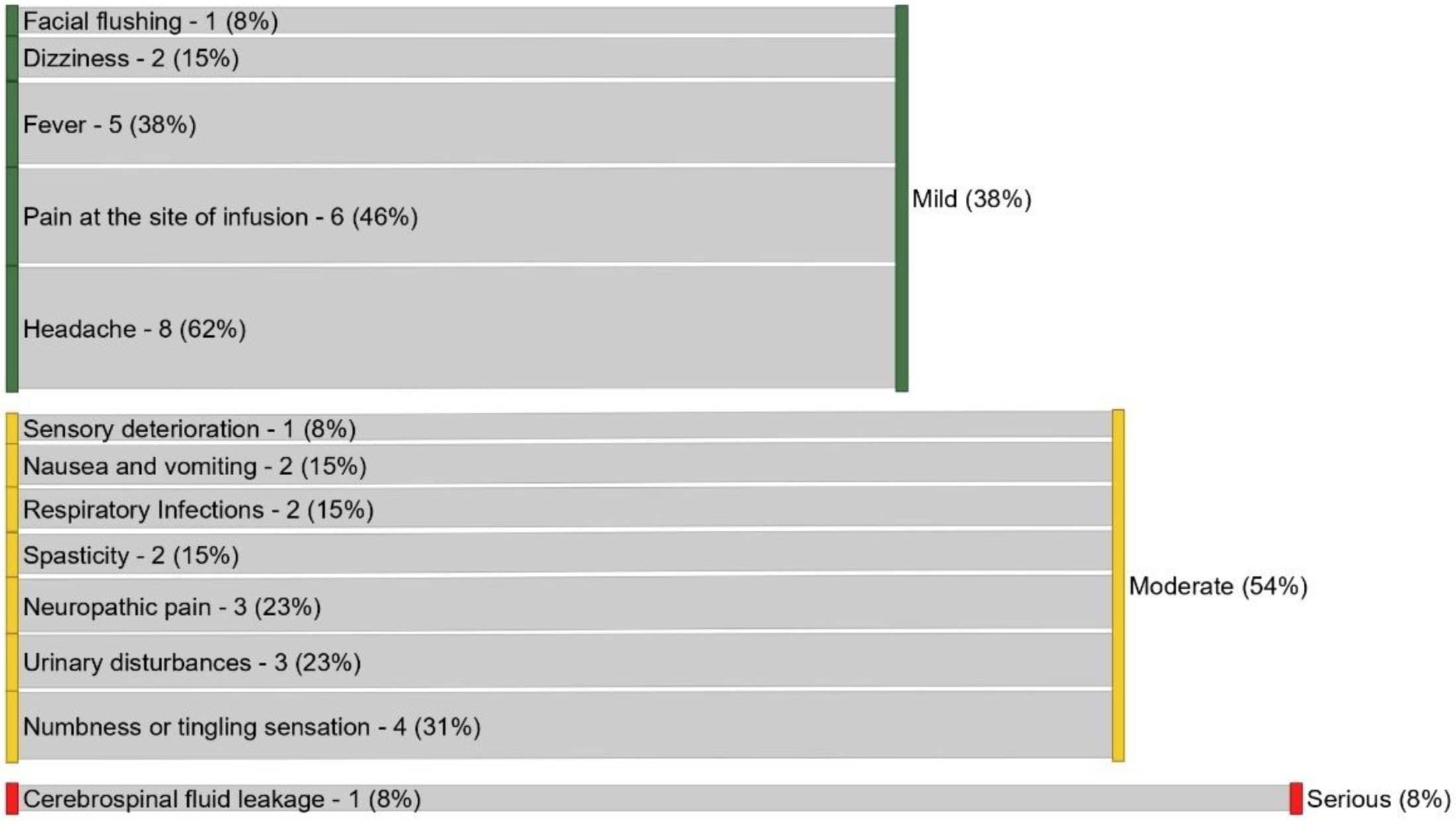
3.4. Adverse Events (AE)
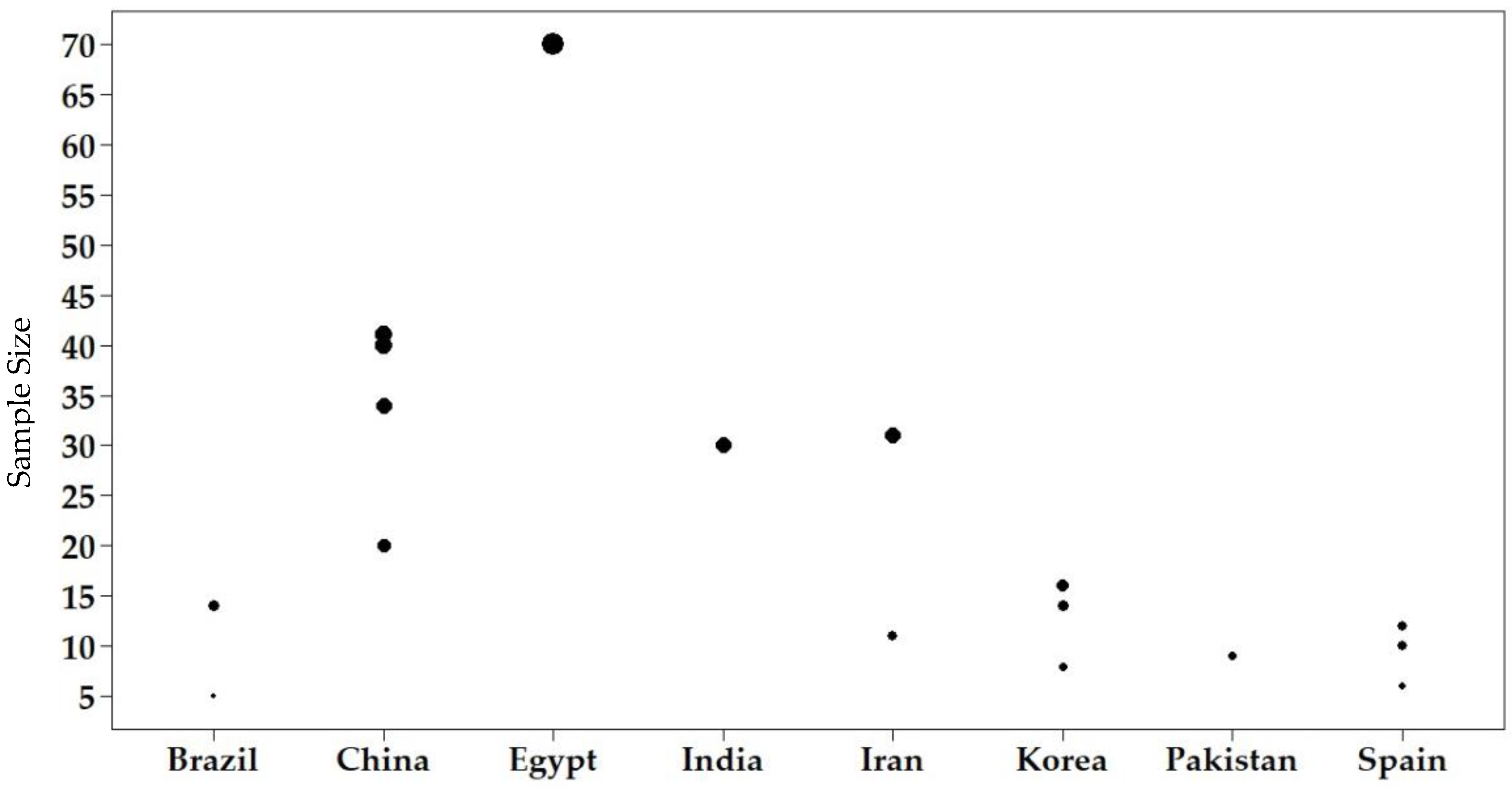
3.5. Sample Size
3.6. Cell Sources
3.7. Routes of Administration
3.8. Therapeutic Scheme
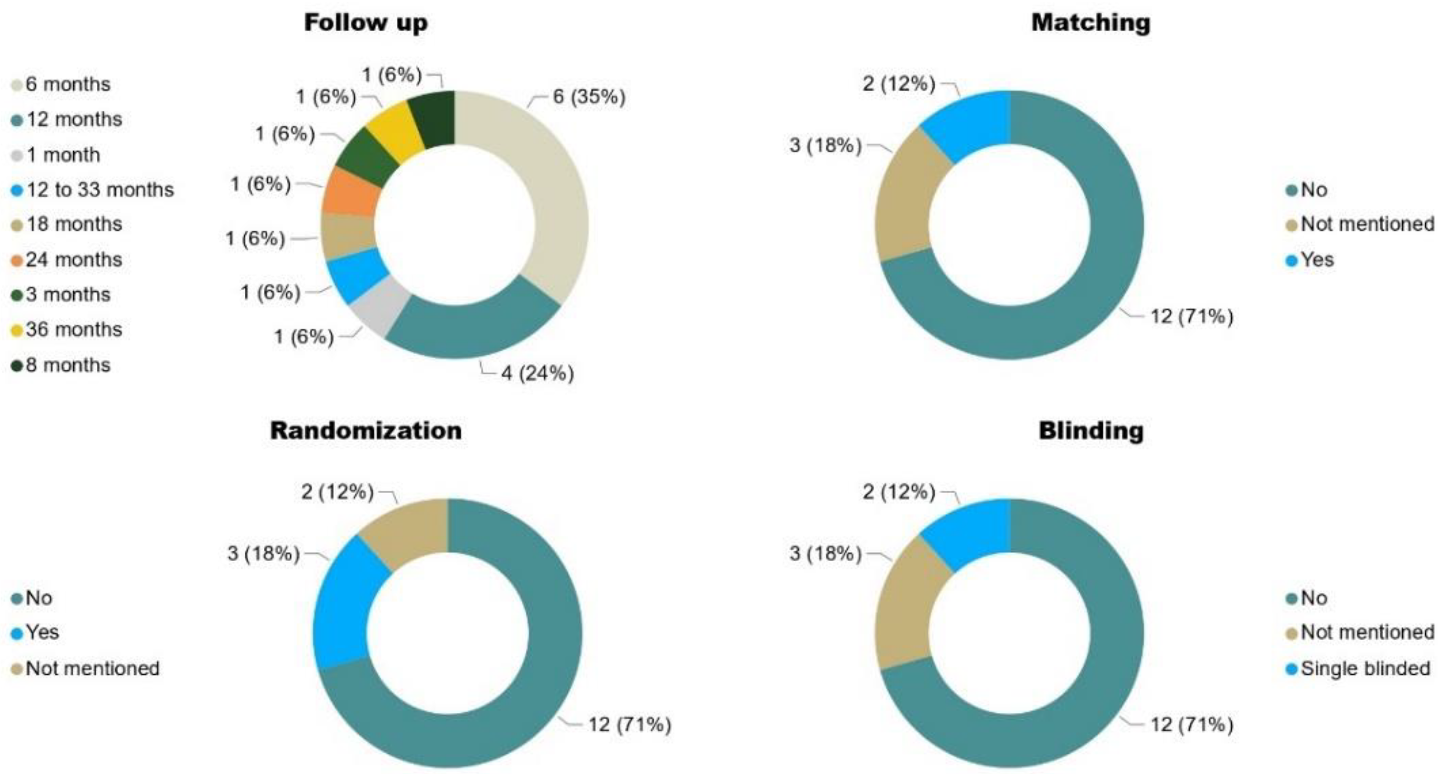
3.9. Follow-up
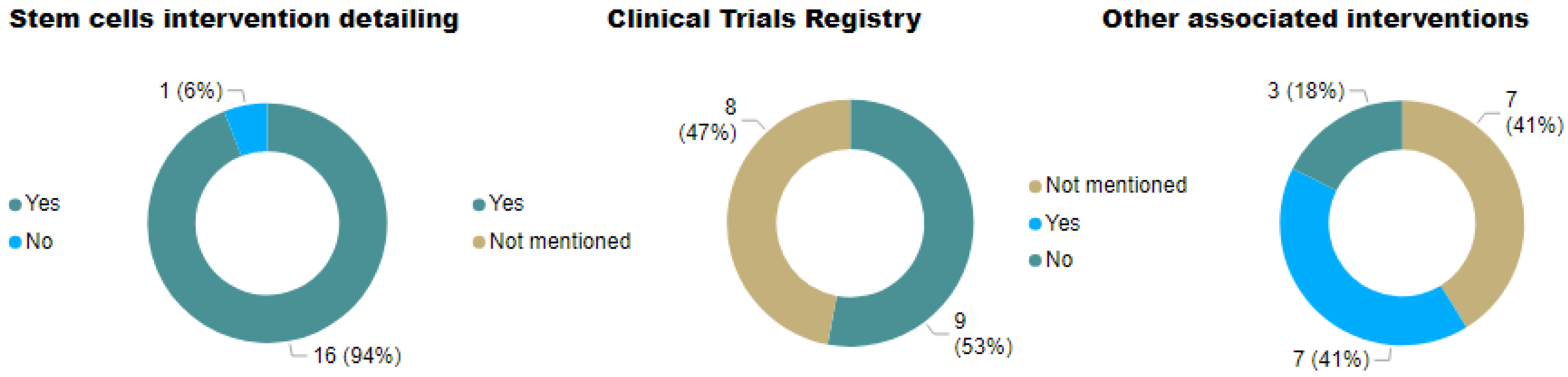
3.10. Associated Interventions
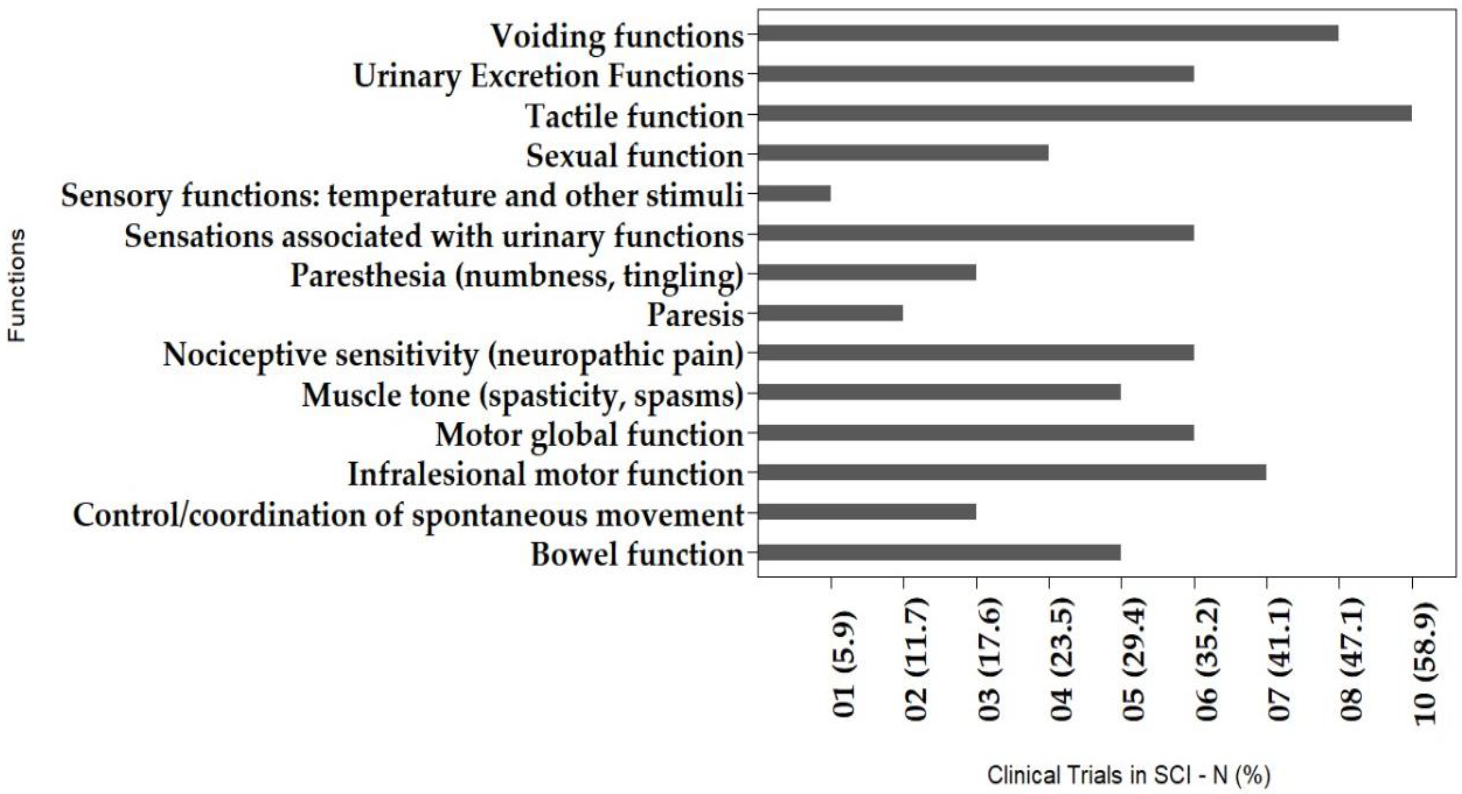
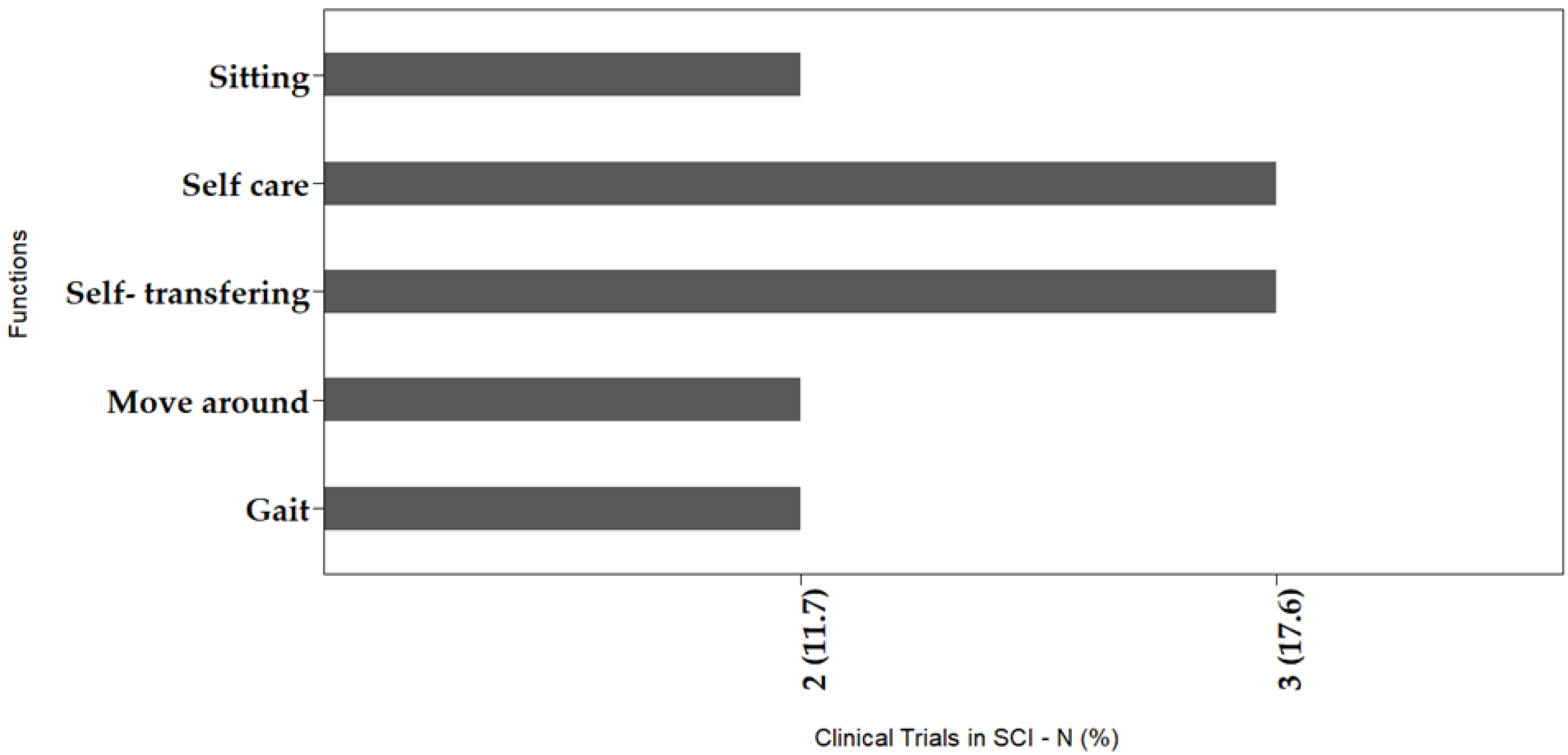
3.11. Outcomes
3.12. Methods for Evaluating Gains in Motor/Sensory Impairments and Human Functioning
3.13. Quality in Clinical Trials
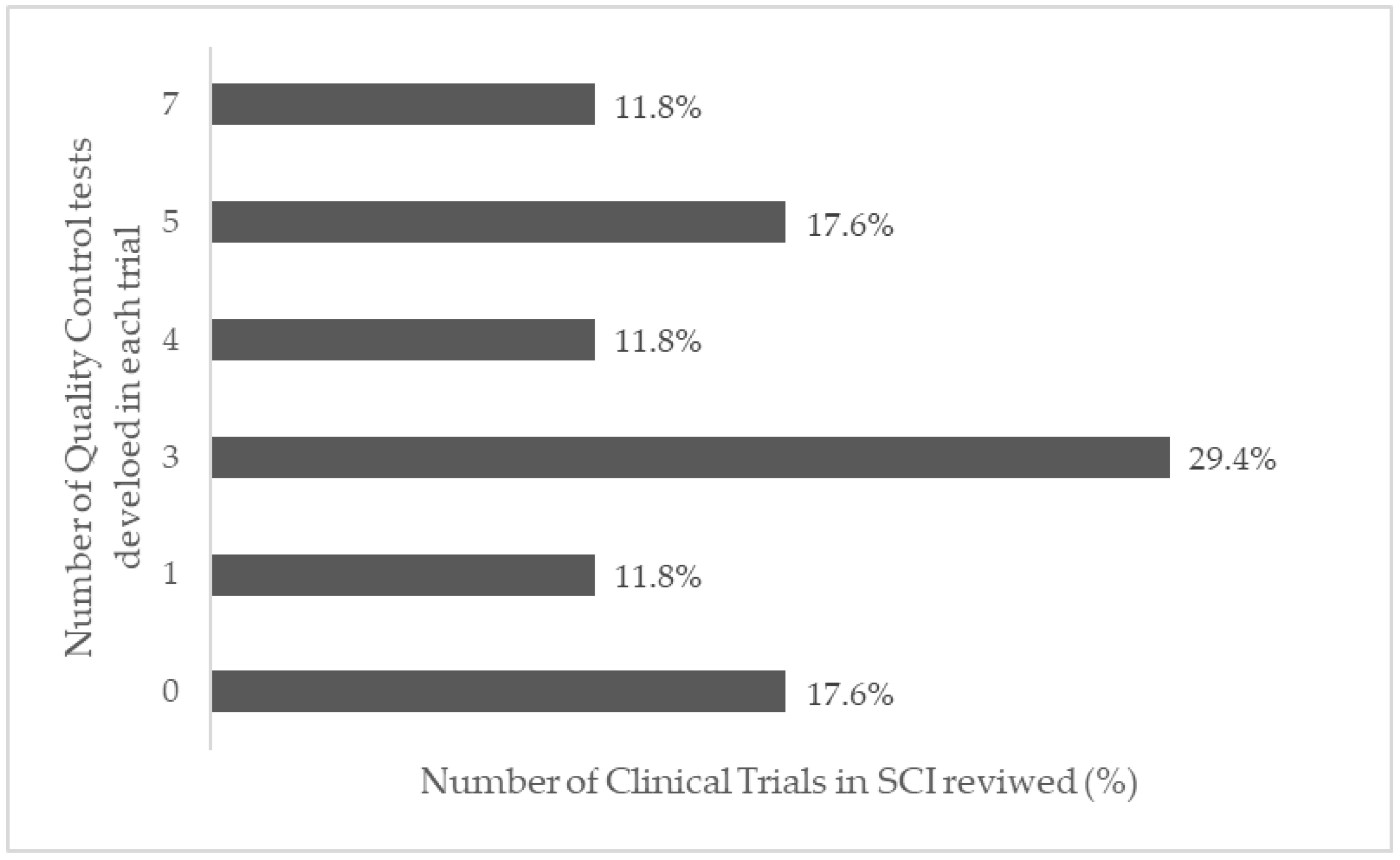
3.14. Quality Control in Stem Cell Manufacturing
3.15. Ethical Aspects
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Thompson, C.; Mutch, J.; Parent, S.; Mac-Thiong, J.-M. The changing demographics of traumatic spinal cord injury: An 11-year study of 831 patients. J. Spinal Cord Med. 2015, 38, 214–223. [Google Scholar] [CrossRef] [PubMed]
- DeVivo, M.J. Epidemiology of traumatic spinal cord injury: Trends and future implications. Spinal Cord 2012, 50, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Brasil. Diretrizes de Atenção à Pessoa com Lesão Medular; Ministério da Saúde Secretaria de Atenção à Saúde Departamento de Ações Programáticas Estratégicas: Brasilia, Brazil, 2015.
- Bombardier, C.H.; Azuero, C.B.; Fann, J.R.; Kautz, D.D.; Richards, J.S.; Sabharwal, S. Management of Mental Health Disorders, Substance Use Disorders, and Suicide in Adults with Spinal Cord Injury: Clinical Practice Guideline for Healthcare Providers. Top. Spinal Cord Inj. Rehabil. 2021, 27, 152–224. [Google Scholar] [PubMed]
- Janahú, L.T.A.; Neves, L.M.T.; Silva, M.C.; Oliveira, I.S. Trauma raquimedular: Perfil epidemiológico dos pacientes atendidos no Pronto Socorro Municipal Mário Pinotti nos anos de 2003 à 2005. Fisioter. Ser 2009, 4, 246–249. [Google Scholar]
- Yamazaki, K.; Kawabori, M.; Seki, T.; Houkin, K. Clinical Trials of Stem Cell Treatment for Spinal Cord Injury. Int. J. Mol. Sci. 2020, 21, 3994. [Google Scholar] [CrossRef] [PubMed]
- Cristante, A.F.; Barros, T.; Marcon, R.M.; Letaif, O.B.; Rocha, I.; Filho, T.E.P.D.B.; Da Rocha, I.D. Therapeutic approaches for spinal cord injury. Clinics 2012, 67, 1219–1224. [Google Scholar] [CrossRef]
- Zhang, Y.; Al Mamun, A.; Yuan, Y.; Lu, Q.; Xiong, J.; Yang, S.; Wu, C.; Wu, Y.; Wang, J. Acute spinal cord injury: Pathophysiology and pharmacological intervention (Review). Mol. Med. Rep. 2021, 23, 417. [Google Scholar] [CrossRef]
- Alexander, J.K.; Popovich, P.G. Neuroinflammation in spinal cord injury: Therapeutic targets for neuroprotection and regeneration. Prog. Brain Res. 2009, 175, 125–137. [Google Scholar] [CrossRef]
- Crowe, M.J.; Bresnahan, J.C.; Shuman, S.L.; Masters, J.N.; Beattie, M.S. Apoptosis and delayed degeneration after spinal cord injury in rats and monkeys. Nat. Med. 1997, 3, 73–76. [Google Scholar] [CrossRef]
- Shuman, S.L.; Bresnahan, J.C.; Beattie, M.S. Apoptosis of Microglia and Oligodendrocytes After Spinal Cord Contusion in Rats; Wiley-Liss, Inc.: Hoboken, NJ, USA, 1997; Volume 50. [Google Scholar]
- Barnabé-Heider, F.; Frisén, J. Stem Cells for Spinal Cord Repair. Cell Stem Cell 2008, 3, 16–24. [Google Scholar] [CrossRef]
- Jiang, P.-C.; Xiong, W.-P.; Wang, G.; Ma, C.; Yao, W.-Q.; Kendell, S.F.; Mehling, B.M.; Yuan, X.-H.; Wu, D.-C. A clinical trial report of autologous bone marrow-derived mesenchymal stem cell transplantation in patients with spinal cord injury. Exp. Ther. Med. 2013, 6, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Mabon, P.; Weaver, L.C.; Dekaban, G.A. Inhibition of Monocyte/Macrophage Migration to a Spinal Cord Injury Site by an Antibody to the Integrin αD: A Potential New Anti-inflammatory Treatment. Exp. Neurol. 2000, 166, 52–64. [Google Scholar] [CrossRef] [PubMed]
- Jones, L.L.; Margolis, R.U.; Tuszynski, M.H. The chondroitin sulfate proteoglycans neurocan, brevican, phosphacan, and versican are differentially regulated following spinal cord injury. Exp. Neurol. 2003, 182, 399–411. [Google Scholar] [CrossRef]
- Khorasanizadeh, M.; Yousefifard, M.; Eskian, M.; Lu, Y.; Chalangari, M.; Harrop, J.S.; Jazayeri, S.B.; Seyedpour, S.; Khodaei, B.; Hosseini, M.; et al. Neurological recovery following traumatic spinal cord injury: A systematic review and meta-analysis. J. Neurosurg. Spine 2019, 30, 683–699. [Google Scholar] [CrossRef] [PubMed]
- Ter Wengel, P.V.; De Witt Hamer, P.C.; Pauptit, J.C.; van der Gaag, N.A.; Oner, F.C.; Vandertop, W.P. Early Surgical Decompression Improves Neurological Outcome after Complete Traumatic Cervical Spinal Cord Injury: A Meta-Analysis. J. Neurotrauma 2019, 36, 835–844. [Google Scholar] [CrossRef]
- Ter Wengel, P.V.; Martin, E.; De Witt Hamer, P.C.; Feller, R.E.; van Oortmerssen, J.A.E.; van der Gaag, N.A.; Oner, F.C.; Vandertop, W.P. Impact of Early (<24 h) Surgical Decompression on Neurological Recovery in Thoracic Spinal Cord Injury: A Meta-Analysis. J. Neurotrauma 2019, 36, 2609–2617. [Google Scholar] [CrossRef]
- Alishahi, M.; Anbiyaiee, A.; Farzaneh, M.; Khoshnam, S.E. Human Mesenchymal Stem Cells for Spinal Cord Injury. Curr. Stem Cell Res. Ther. 2020, 15, 340–348. [Google Scholar] [CrossRef]
- Liau, L.L.; Looi, Q.H.; Chia, W.C.; Subramaniam, T.; Ng, M.H.; Law, J.X. Treatment of spinal cord injury with mesenchymal stem cells. Cell Biosci. 2020, 10, 112. [Google Scholar] [CrossRef]
- Ma, Y.; Zhu, Y.; Zhang, B.; Wu, Y.; Liu, X.; Zhu, Q. The Impact of Urgent (<8 Hours) Decompression on Neurologic Recovery in Traumatic Spinal Cord Injury: A Meta-Analysis. World Neurosurg. 2020, 140, e185–e194. [Google Scholar] [CrossRef]
- Naji, A.; Eitoku, M.; Favier, B.; Deschaseaux, F.; Rouas-Freiss, N.; Suganuma, N. Biological functions of mesenchymal stem cells and clinical implications. Cell Mol. Life Sci. 2019, 76, 3323–3348. [Google Scholar] [CrossRef]
- Cloutier, F.; Siegenthaler, M.M.; Nistor, G.; Keirstead, H.S. Transplantation of human embryonic stem cell-derived oligodendrocyte progenitors into rat spinal cord injuries does not cause harm. Regen. Med. 2006, 1, 469–479. [Google Scholar] [CrossRef] [PubMed]
- Hiemstra, L.E.; Terblanche, L.; Adriaanse, B. Rehabilitation outcomes following autologous human stem cell transplantation in a chronic complete C4 tetraplegic—The first 12 months: A case report. S. Afr. J. Occup. Ther. 2015, 45, 29–42. [Google Scholar] [CrossRef]
- Saporta, S.; Kim, J.-J.; Willing, A.E.; Fu, E.S.; Davis, C.D.; Sanberg, P.R. Human Umbilical Cord Blood Stem Cells Infusion in Spinal Cord Injury: Engraftment and Beneficial Influence on Behavior. J. Hematotherapy 2003, 12, 271–278. [Google Scholar] [CrossRef]
- Carlson, K.-S.; Singh, P.; Feaster, M.M.; Ramnarain, A.; Pavlides, C.; Chen, Z.-L.; Yu, W.-M.; Feltri, M.L.; Strickland, S. Mesenchymal stem cells facilitate axon sorting, myelination, and functional recovery in paralyzed mice deficient in Schwann cell-derived laminin. Glia 2010, 59, 267–277. [Google Scholar] [CrossRef] [PubMed]
- Penha, E.M.; Aguiar, P.H.; Barrouin-Melo, S.M.; Lima, R.S.; Silveira, A.C.; Otelo, A.R.; Pinheiro, C.M.; Ribeiro-dos-Santos, R.; Soares, M.B.P. Clinical Neurofunctional Rehabilitation of a Cat with Spinal Cord Injury after Hemilaminectomy and Autologous Stem Cell Transplantation. Int. J. Stem Cells 2012, 5, 146–150. [Google Scholar] [CrossRef]
- Penha, E.M.; Meira, C.S.; Guimarães, E.T.; Mendonça, M.V.P.; Gravely, F.A.; Pinheiro, C.M.B.; Pinheiro, T.M.B.; Barrouin-Melo, S.M.; Ribeiro-Dos-Santos, R.; Soares, M.B.P. Use of Autologous Mesenchymal Stem Cells Derived from Bone Marrow for the Treatment of Naturally Injured Spinal Cord in Dogs. Stem Cells Int. 2014, 2014, 437521. [Google Scholar] [CrossRef]
- Silva, T.G.F.S.L.; Oliveira, F.M.; Fracaro, L.; Silva, C.; Rebelatto, C.K.L.; Pimpão, C.T.; Brofman, P.R.S.; Junior, J.A.V. Sensory, motor and cystometric evaluation of dogs with chronic spinal cord injury submitted to mesenchymal stem cell transplantation. Pesqui. Vet. Bras. 2018, 38, 1955–1965. [Google Scholar] [CrossRef]
- Kim, M.; Kim, K.H.; Song, S.U.; Yi, T.G.; Yoon, S.H.; Park, S.R.; Choi, B.H. Transplantation of human bone marrow-derived clonal mesenchymal stem cells reduces fibrotic scar formation in a rat spinal cord injury model. J. Tissue Eng. Regen. Med. 2017, 12, e1034–e1045. [Google Scholar] [CrossRef]
- Hofstetter, C.P.; Schwarz, E.J.; Hess, D.; Widenfalk, J.; El Manira, A.; Prockop, D.J.; Olson, L. Marrow stromal cells form guiding strands in the injured spinal cord and promote recovery. Proc. Natl. Acad. Sci. USA 2002, 99, 2199–2204. [Google Scholar] [CrossRef]
- Rodríguez Sánchez, D.N.; de Lima Resende, L.A.; Boff Araujo Pinto, G.; Bovolato, A.L.C.; Possebon, F.S.; Deffune, E.; Amorim, R.M. Canine Adipose-Derived Mesenchymal Stromal Cells Enhance Neuroregeneration in a Rat Model of Sciatic Nerve Crush Injury. Cell Transplant. 2019, 28, 47–54. [Google Scholar] [CrossRef]
- Yang, L.; Li, Z.; Zhao, W.; Liu, W.; Zhou, Y.; Jia, J. Transplantation of placenta-derived mesenchymal stem cell-induced neural stem cells to treat spinal cord injury. Neural Regen. Res. 2014, 9, 2197–2204. [Google Scholar] [CrossRef] [PubMed]
- Krupa, P.; Vackova, I.; Ruzicka, J.; Zaviskova, K.; Dubisova, J.; Koci, Z.; Turnovcova, K.; Urdzikova, L.M.; Kubinova, S.; Rehak, S.; et al. The Effect of Human Mesenchymal Stem Cells Derived from Wharton’s Jelly in Spinal Cord Injury Treatment Is Dose-Dependent and Can Be Facilitated by Repeated Application. Int. J. Mol. Sci. 2018, 19, 1503. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Rong, P.; Ma, X.; Nie, W.; Chen, C.; Yang, C.; Zhang, J.; Dong, Q.; Wang, W. Paracrine effect of mesenchymal stem cell as a novel therapeutic strategy for diabetic nephropathy. Life Sci. 2018, 215, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Fiore, E.J.; Domínguez, L.M.; Bayo, J.; García, M.G.; Mazzolini, G.D. Taking advantage of the potential of mesenchymal stromal cells in liver regeneration: Cells and extracellular vesicles as therapeutic strategies. World J. Gastroenterol. 2018, 24, 2427–2440. [Google Scholar] [CrossRef]
- Zheng, G.; Huang, R.; Qiu, G.; Ge, M.; Wang, J.; Shu, Q.; Xu, J. Mesenchymal stromal cell-derived extracellular vesicles: Regenerative and immunomodulatory effects and potential applications in sepsis. Cell Tissue Res. 2018, 374, 1–15. [Google Scholar] [CrossRef]
- Weiss, A.R.R.; Dahlke, M.H. Immunomodulation by Mesenchymal Stem Cells (MSCs): Mechanisms of Action of Living, Apoptotic, and Dead MSCs. Front. Immunol. 2019, 10, 1191. [Google Scholar] [CrossRef]
- Zhou, Y.; Xu, H.; Xu, W.; Wang, B.; Wu, H.; Tao, Y.; Zhang, B.; Wang, M.; Mao, F.; Yan, Y.; et al. Exosomes released by human umbilical cord mesenchymal stem cells protect against cisplatin-induced renal oxidative stress and apoptosis in vivo and in vitro. Stem Cell Res. Ther. 2013, 4, 34. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, X.; Cao, W.; Shi, Y. Plasticity of mesenchymal stem cells in immunomodulation: Pathological and therapeutic implications. Nat. Immunol. 2014, 15, 1009–1016. [Google Scholar] [CrossRef]
- Yu, B.; Kim, H.W.; Gong, M.; Wang, J.; Millard, R.W.; Wang, Y.; Ashraf, M.; Xu, M. Exosomes secreted from GATA-4 overexpressing mesenchymal stem cells serve as a reservoir of anti-apoptotic microRNAs for cardioprotection. Int. J. Cardiol. 2014, 182, 349–360. [Google Scholar] [CrossRef]
- Caplan, A.I.; Dennis, J.E. Mesenchymal stem cells as trophic mediators. J. Cell. Biochem. 2006, 98, 1076–1084. [Google Scholar] [CrossRef]
- Dasari, V.R.; Veeravalli, K.K.; Dinh, D.H. Mesenchymal stem cells in the treatment of spinal cord injuries: A review. World J. Stem Cells 2014, 6, 120–133. [Google Scholar] [CrossRef] [PubMed]
- Hur, J.W.; Cho, T.-H.; Park, D.-H.; Lee, J.-B.; Park, J.-Y.; Chung, Y.-G. Intrathecal transplantation of autologous adipose-derived mesenchymal stem cells for treating spinal cord injury: A human trial. J. Spinal Cord Med. 2016, 39, 655–664. [Google Scholar] [CrossRef] [PubMed]
- Takami, T.; Shimokawa, N.; Parthiban, J.; Zileli, M.; Ali, S. Pharmacologic and Regenerative Cell Therapy for Spinal Cord Injury: WFNS Spine Committee Recommendations. Neurospine 2020, 17, 785–796. [Google Scholar] [CrossRef] [PubMed]
- Maynard, F.M.; Bracken, M.B.; Creasey, G.; Ditunno, J.F.D., Jr.; Donovan, W.H.; Ducker, T.B.; Garber, S.L.; Marino, R.; Stover, S.L.; Tator, C.H.; et al. International Standards for Neurological and Functional Classification of Spinal Cord Injury. Spinal Cord 1997, 35, 266–274. [Google Scholar] [CrossRef]
- Aimetti, A.A.; Kirshblum, S.; Curt, A.; Mobley, J.; Grossman, R.G.; Guest, J.D. Natural history of neurological improvement following complete (AIS A) thoracic spinal cord injury across three registries to guide acute clinical trial design and interpretation. Spinal Cord 2019, 57, 753–762. [Google Scholar] [CrossRef]
- Mendonça, M.V.P.; Larocca, T.F.; Souza, B.S.D.F.; Villarreal, C.F.; Silva, L.F.M.; Matos, A.C.; Novaes, M.A.; Bahia, C.M.P.; Martinez, A.C.D.O.M.; Kaneto, C.M.; et al. Safety and neurological assessments after autologous transplantation of bone marrow mesenchymal stem cells in subjects with chronic spinal cord injury. Stem Cell Res. Ther. 2014, 5, 126. [Google Scholar] [CrossRef]
- Coumans, J.V.; Tai-Sen Lin, T.; Ning Dai, H. Axonal Regeneration and Functional Recovery after Complete Spinal Cord Transection in Rats by Delayed Treatment with Transplants and Neurotrophins. J. Neurosci. 2001, 21, 9334–9344. [Google Scholar] [CrossRef]
- Nakamura, M.; Houghtling, R.A.; MacArthur, L.; Bayer, B.M.; Bregman, B.S. Differences in cytokine gene expression profile between acute and secondary injury in adult rat spinal cord. Exp. Neurol. 2003, 184, 313–325. [Google Scholar] [CrossRef]
- El-Kheir, W.A.; Gabr, H.; Awad, M.R.; Ghannam, O.; Barakat, Y.; Farghali, H.A.M.A.; El Maadawi, Z.M.; Ewes, I.; Sabaawy, H.E. Autologous Bone Marrow-Derived Cell Therapy Combined with Physical Therapy Induces Functional Improvement in Chronic Spinal Cord Injury Patients. Cell Transplant. 2014, 23, 729–745. [Google Scholar] [CrossRef]
- Zhang, H.; Wang, L.; Wen, S.; Xiang, Q.; Xiang, X.; Xu, C.; Wan, Y.; Wang, J.; Li, B.; Wan, Y.; et al. Magnetic resonance imaging tracking and assessing repair function of the bone marrow mesenchymal stem cells transplantation in a rat model of spinal cord injury. Oncotarget 2017, 8, 58985–58999. [Google Scholar] [CrossRef][Green Version]
- Silvestro, S.; Bramanti, P.; Trubiani, O.; Mazzon, E. Stem Cells Therapy for Spinal Cord Injury: An Overview of Clinical Trials. Int. J. Mol. Sci. 2020, 21, 659. [Google Scholar] [CrossRef] [PubMed]
- Ciavarella, C.; Pasquinelli, G. The Dual Nature of Mesenchymal Stem Cells (MSCs): Yin and Yang of the Inflammatory Process. 2020. Available online: https://www.intechopen.com/chapters/65091 (accessed on 12 December 2021).
- Mason, C.; Dunnill, P. Assessing the value of autologous and allogeneic cells for regenerative medicine. Regen. Med. 2009, 4, 835–853. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Pang, M.; Du, C.; Liu, Z.Y.; Chen, Z.H.; Wang, N.X.; Zhang, L.M.; Chen, Y.Y.; Mo, J.; Dong, J.W.; et al. Repeated subarachnoid administrations of allogeneic human umbilical cord mesenchymal stem cells for spinal cord injury: A phase 1/2 pilot study. Cytotherapy 2021, 23, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Bydon, M.; Dietz, A.B.; Goncalves, S.; Moinuddin, F.M.; Alvi, M.A.; Goyal, A.; Yolcu, Y.; Hunt, C.L.; Garlanger, K.L.; Del Fabro, A.S.; et al. CELLTOP Clinical Trial: First Report from a Phase 1 Trial of Autologous Adipose Tissue–Derived Mesenchymal Stem Cells in the Treatment of Paralysis Due to Traumatic Spinal Cord Injury. Mayo Clin. Proc. 2019, 95, 406–414. [Google Scholar] [CrossRef] [PubMed]
- Pal, R.; Venkataramana, N.K.; Bansal, A.; Balaraju, S.; Jan, M.; Chandra, R.; Dixit, A.; Rauthan, A.; Murgod, U.; Totey, S. Ex vivo-expanded autologous bone marrow-derived mesenchymal stromal cells in human spinal cord injury/paraplegia: A pilot clinical study. Cytotherapy 2009, 11, 897–911. [Google Scholar] [CrossRef]
- Satti, H.S.; Waheed, A.; Ahmed, P.; Ahmed, K.; Akram, Z.; Aziz, T.; Satti, T.M.; Shahbaz, N.; Khan, M.A.; Malik, S.A. Autologous mesenchymal stromal cell transplantation for spinal cord injury: A Phase I pilot study. Cytotherapy 2016, 18, 518–522. [Google Scholar] [CrossRef]
- Vaquero, J.; Zurita, M.; Rico, M.A.; Bonilla, C.; Aguayo, C.; Montilla, J.; Bustamante, S.; Carballido, J.; Marin, E.; Martinez, F.; et al. An approach to personalized cell therapy in chronic complete paraplegia: The Puerta de Hierro phase I/II clinical trial. Cytotherapy 2016, 18, 1025–1036. [Google Scholar] [CrossRef]
- Vaquero, J.; Zurita, M.; Rico, M.A.; Bonilla, C.; Aguayo, C.; Fernández, C.; Tapiador, N.; Sevilla, M.; Morejón, C.; Montilla, J.; et al. Repeated subarachnoid administrations of autologous mesenchymal stromal cells supported in autologous plasma improve quality of life in patients suffering incomplete spinal cord injury. Cytotherapy 2017, 19, 349–359. [Google Scholar] [CrossRef]
- Vaquero, J.; Zurita, M.; Rico, M.A.; Aguayo, C.; Fernandez, C.; Rodriguez-Boto, G.; Marin, E.; Tapiador, N.; Sevilla, M.; Carballido, J.; et al. Cell therapy with autologous mesenchymal stromal cells in post-traumatic syringomyelia. Cytotherapy 2018, 20, 796–805. [Google Scholar] [CrossRef]
- Karamouzian, S.; Nematollahi-Mahani, S.N.; Nakhaee, N.; Eskandary, H. Clinical safety and primary efficacy of bone marrow mesenchymal cell transplantation in subacute spinal cord injured patients. Clin. Neurol. Neurosurg. 2012, 114, 935–939. [Google Scholar] [CrossRef]
- Oraee-Yazdani, S.; Akhlaghpasand, M.; Golmohammadi, M.; Hafizi, M.; Zomorrod, M.S.; Kabir, N.M.; Oraee-Yazdani, M.; Ashrafi, F.; Zali, A.; Soleimani, M. Combining cell therapy with human autologous Schwann cell and bone marrow-derived mesenchymal stem cell in patients with subacute complete spinal cord injury: Safety considerations and possible outcomes. Stem Cell Res. Ther. 2021, 12, 445. [Google Scholar] [CrossRef] [PubMed]
- Karp, J.M.; Leng Teo, G.S. Mesenchymal Stem Cell Homing: The Devil Is in the Details. Cell Stem Cell 2009, 4, 206–216. [Google Scholar] [CrossRef] [PubMed]
- Syková, E.; Jendelova, P.; Urdzikova, L.M.; Lesný, P.; Hejčl, A. Bone Marrow Stem Cells and Polymer Hydrogels—Two Strategies for Spinal Cord Injury Repair. Cell. Mol. Neurobiol. 2006, 26, 1111–1127. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.K.; Choi, K.H.; Yoo, J.Y.; Kim, D.Y.; Kim, S.J.; Jeon, S.R. A Phase III Clinical Trial Showing Limited Efficacy of Autologous Mesenchymal Stem Cell Therapy for Spinal Cord Injury. Neurosurgery 2015, 78, 436–447. [Google Scholar] [CrossRef] [PubMed]
- Amariglio, N.; Hirshberg, A.; Scheithauer, B.W.; Cohen, Y.; Loewenthal, R.; Trakhtenbrot, L.; Paz, N.; Koren-Michowitz, M.; Waldman, D.; Leider-Trejo, L.; et al. Donor-Derived Brain Tumor Following Neural Stem Cell Transplantation in an Ataxia Telangiectasia Patient. PLoS Med. 2009, 6, e1000029. [Google Scholar] [CrossRef]
- Brazil, Agência Nacional de Vigilância Sanitária. Manual Para Notificação de Eventos Adversos E Monitoramento de Segurança em Ensaios Clínicos; Coordenação de Pesquisa Clínica em Medicamentos e Produtos Biológicos—COPEC: Brasilia, Brasil, 2016.
- Marodin, G.; Goldim, J.R. Confusões e ambigüidades na classificação de eventos adversos em pesquisa clínica. Rev. Esc. Enferm. USP. 2009, 43, 690–696. [Google Scholar] [CrossRef][Green Version]
- Park, J.H.; Kim, D.Y.; Sung, I.Y.; Choi, G.H.; Jeon, M.H.; Kim, K.K.; Jeon, S.R. Long-term Results of Spinal Cord Injury Therapy Using Mesenchymal Stem Cells Derived from Bone Marrow in Humans. Neurosurgery 2011, 70, 1238–1247. [Google Scholar] [CrossRef]
- Failli, V.; Kleitman, N.; Lammertse, D.P.; Hsieh, J.T.C.; Steeves, J.D.; Fawcett, J.W.; Tuszynski, M.H.; Curt, A.; Fehlings, M.G.; Guest, J.D.; et al. Experimental Treatments for Spinal Cord Injury: What you Should Know. Top. Spinal Cord Inj. Rehabil. 2021, 27, 50–74. [Google Scholar] [CrossRef]
- Park, H.C.; Shim, Y.S.; Ha, Y.; Yoon, S.H.; Park, S.R.; Choi, B.H.; Park, H.S. Treatment of Complete Spinal Cord Injury Patients by Autologous Bone Marrow Cell Transplantation and Administration of Granulocyte-Macrophage Colony Stimulating Factor. Tissue Eng. 2005, 11, 913–922. [Google Scholar] [CrossRef]
- Krebs, H.I.; Hogan, N.; Aisen, M.L.; Volpe, B. Robot-Aided Neurorehabilitation. IEEE Trans. Rehabil. Eng. 1998, 6, 75–87. [Google Scholar] [CrossRef]
- Bass, A.; Aubertin-Leheudre, M.; Vincent, C.; Karelis, A.D.; Morin, S.N.; McKerral, M.; Duclos, C.; Gagnon, D.H. Effects of an Overground Walking Program with a Robotic Exoskeleton in Long-Term Manual Wheelchair Users with a Chronic Spinal Cord Injury: Protocol for a Self-Controlled Interventional Study (Preprint). JMIR Res. Protoc. 2020, 9, e19251. [Google Scholar] [CrossRef] [PubMed]
- Ra, J.C.; Shin, I.S.; Kim, S.H.; Kang, S.K.; Kang, B.C.; Lee, H.Y.; Kim, Y.J.; Jo, J.Y.; Yoon, E.J.; Choi, H.J.; et al. Safety of Intravenous Infusion of Human Adipose Tissue-Derived Mesenchymal Stem Cells in Animals and Humans. Stem Cells Dev. 2011, 20, 1297–1308. [Google Scholar] [CrossRef] [PubMed]
- Dai, G.; Liu, X.; Zhang, Z.; Yang, Z.; Dai, Y.; Xu, R. Transplantation of autologous bone marrow mesenchymal stem cells in the treatment of complete and chronic cervical spinal cord injury. Brain Res. 2013, 1533, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.; Liu, X.; Hua, R.; Dai, G.; Wang, X.; Gao, J.; An, Y. Clinical observation of umbilical cord mesenchymal stem cell transplantation in treatment for sequelae of thoracolumbar spinal cord injury. J. Transl. Med. 2014, 12, 253. [Google Scholar] [CrossRef] [PubMed]
- Larocca, T.F.; Macêdo, C.T.; Souza, B.S.D.F.; Andrade-Souza, Y.M.; Villarreal, C.F.; Matos, A.C.; Silva, D.; da Silva, K.N.; Souza, C.L.E.M.D.; Paixão, D.D.S.; et al. Image-guided percutaneous intralesional administration of mesenchymal stromal cells in subjects with chronic complete spinal cord injury: A pilot study. Cytotherapy 2017, 19, 1189–1196. [Google Scholar] [CrossRef]
- Wang, Y.-J.; Li, J.-J.; Zhou, H.-J.; Liu, G.-L.; Zheng, Y.; Wei, B.; Zhang, Y.; Hao, C.-X.; Kang, H.-Q.; Yuan, Y.; et al. Surface electromyography as a measure of trunk muscle activity in patients with spinal cord injury: A meta-analytic review. J. Spinal Cord Med. 2015, 39, 15–23. [Google Scholar] [CrossRef]
- Ervilha, U.F.; Duarte, M.; Amadio, A.C. Estudo Sobre Procedimentos de Normalização do Sinal Eletromiográfico Durante o Movimento Humano. Rev. Bras. Fisiot. 1998, 3, 15–20. [Google Scholar]
- Yoon, S.H.; Shim, Y.S.; Park, Y.H.; Chung, J.K.; Nam, J.H.; Kim, M.O.; Park, H.C.; Park, S.R.; Min, B.-H.; Kim, E.Y.; et al. Complete Spinal Cord Injury Treatment Using Autologous Bone Marrow Cell Transplantation and Bone Marrow Stimulation with Granulocyte Macrophage-Colony Stimulating Factor: Phase I/II Clinical Trial. Stem Cells 2007, 25, 2066–2073. [Google Scholar] [CrossRef]
- Berwanger, O.; Guimarães, H.P.; Avezum, A.; Leopoldo, S. Os dez mandamentos do ensaio clínico randomizado—Princípios para avaliação crítica da literatura médica. Rev. Bras. Hipertens. 2006, 13, 55–70. [Google Scholar]
- Yusuf, S.; Collins, R.; Peto, R. Why do we need some large, simple randomized trials? Stat. Med. 1984, 3, 409–420. [Google Scholar] [CrossRef]
- International Society for Stem Cell Research (ISSCR). Guidelines for Stem Cell Research and Clinical Translation; International Society for Stem Cell Research: Skokie, IL, USA, 2016. [Google Scholar]
- CHMP & CPWP. Guideline on Human Cell-Based Medicinal Products; European Medicines Agency: Amsterdam, The Netherlands, 2006. [Google Scholar]
- Food and Drug Administration Center-FDA. Guidance for Industry Guidance for Human Somatic Cell Therapy and Gene Therapy; Food and Drug Administration: Rockville, MD, USA, 1998.
- Diário Oficial da União-DOU. Resolução Anvisa Rdc n. 508, de 27 de Maio de 2021; Imprensa Nacional: Brasilia, Brazil, 2021.
- Dominici, M.; Le Blanc, K.; Mueller, I.; Slaper-Cortenbach, I.; Marini, F.C.; Krause, D.S.; Deans, R.J.; Keating, A.; Prockop, D.J.; Horwitz, E.M. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 2006, 8, 315–317. [Google Scholar] [CrossRef] [PubMed]

| Cell Therapy Approach | Cell Source | Routes of Administration | SCI Level/ASIA Grade | SCI Phase | Interventions Associated | Tools for Evaluating Functioning and Motor/Sensory Improvements | Clinically Significant Outcomes | Statistically Significant Outcomes | References |
|---|---|---|---|---|---|---|---|---|---|
| 1 × 106 cells/kg | Autologous BM | Intrathecal | Cervical and Thoracic AIS A | Sub-acute, Chronic | No | ASIA, BI, SSEP, MEP, NCV, MRI | Improvement in bladder function, supportive walking and sitting | No | Pal et al., 2009 |
| 4 × 108 | Autologous AD | Intravenous | Cervical and thoracolumbar AIS A, B | Chronic | No | ASIA, SCIM, VAS, MRI, MEP, SEP | improvement in Self-care | SEP in 3 subjects and ASIA A to C in 1 subject | Ra et al., 2011 |
| 7 × 105 to 1.2 × 106 | Autologous BM | Intrathecal | Thoracic AIS A | Acute and Sub acute | Rehabilitation | ASIA | 5 Subjects changed from AIS A to C | No | Karamouzian et al., 2012 |
| 25 μL–8 × 105 cells/μL | Autologous BM | Intralesional | Cervical AIS A | Chronic | No | ASIA, RUV, EMG, PSSEP, MRI | Improvement in ASIA score, residual urine volume | ASIA score, residual urine volume | Dai et al., 2013 |
| 1 × 108 cells in 5 mL | Autologous BM | Intralesional | Cervical and thoraco lumbar AIS A-, B, and C | Acute, Sub acute and Chronic | No | ASIA, BI, ASHWORT | Benefits in AIS grading and score, bowel, and urinary function, reduction of pain, erectile dysfunction and hypertonia | Not mentioned | Jiang et al., 2013 |
| 2 × 106 cells/kg 1–8 monthly injections | Autologous-BM | Intrathecal | Cervical and thoracic AIS A and B | Chronic | Rehabilitation | ASIA, SSEP MRI, FIM | Improvement of neurological and functional measures | Motor and sensory improvement | El-Kheir et al., 2014 |
| 2 doses (50 µL to 4 × 105 cells/μL) | Allogenic UC | Intralesional | Thoraco Lumbar AIS A | Chronic | Neurological rehabilitation | ASIA, BI, MMS, MTS | Significant and stable improvement in movement, self-care ability, and muscular tension; residue urine volume | Strength of waist, abdomen, and lower limbs increased, excessive muscle tension decreased, and self-care ability | Cheng et al., 2014 |
| 5 × 106 cells/cm3 | Autologous BM | Intralesional | Thoraco Lumbar AIS A | Chronic | Rehabilitation | ASIS, SSEP, MRI, VAS, USD | Improvement in urologic function, lower limb sensitivity and motor function, reduction in pain | ASIA sensitivity and motor scores | Mendonça et al., 2014 |
| 2 × 107 cells | Autologous BM | Intralesional | Thoraco Lumbar AIS A | Chronic | No | ASIA, SSEP, MRI, SCIM, FIM, USD | Improvement in sexual dysfunction, urinary bladder-filling sensation and sphincter control. | Bowel regularity | Larocca et al., 2016 |
| 2 or 3 injections (1.2 × 106/kg) | Autologous BM | Intrathecal | Thoracic AIS A | Sub-acute, Chronic | No | ASIA, MRI | Not mentioned | Not mentioned | Satti et al., 2016 |
| 3–7 injections; 100 × 106 to 230 × 106 cells. additional dose (30 × 106 cells) after 3 months | Autologous BM | Intrathecal | Thoracic AIS A | Chronic | Not mentioned | ASIA, FIM, IANR-SCIFRS, BI, Ashworth, Geffner, VAS, MRI, USD | Improvement in sensitivity and sphincter (urinary and bowel) control, infralesional motor activity, decreases in spasms and spasticity, improvement in sexual function | Sphincter control, reduction of neuropathic pain and spasticity | Vaquero, 2016 |
| 4 doses 3 × 107 cells day 1, 4, 7 and 10 months (120 × 106 total) | Autologous BM | Intrathecal | Cervical and thoraco Lumbar AIS B, C or D | Chronic | Not mentioned | ASIA, FIM, IANR-SCIFRS, BI, Ashworth, Geffner, VAS, MRI, USD | Sensitivity and motor improvement, reduction of pain | Sensitivity and motor improvement | Vaquero et al., 2017 |
| 3 doses 100 × 106 (1, 4 e 7 months) | Autologous BM | Intrathecal | Cervical, thoracic and lumbar AIS A, B, C and D | Chronic | Not mentioned | ASIA, FIM, IANR- SCIFRS, BI, Ashworth, Geffner, VAS, MRI, USD | Improvement in sensitivity, in neurogenic bowel and bladder dysfunction, spasms and spasticity, neuropathic pain, and voluntary muscle contraction | Pin prick score assessment, improvements in the syrinx size | Vaquero et al., 2018 |
| (9 × 107 céls) | Autologous AD | Intrathecal | Cervical and thoraco Lumbar AIS A, B, D | Sub-acute, Chronic | Not mentioned | ASIA, MRI, EMG, SSEP, MEP | Improvement in ASIA motor score, Voluntary anal contraction improvement | Not mentioned | Hur et al., 2016 |
| 2 doses: 1.6 × 107 + 3.2 × 107 | Autologous BM | Intralesional/subdural | Cervical AIS B | Chronic | Rehabilitation | MEP, SEP, MRI | Improvement in motor grade of the upper extremities and ADL; Increases in spinal cord diameter; disappearance of the cavity; SEP and MEP improvements | Not mentioned | Oh et al., 2016 |
| 5 × 107 | Autologous BM and SC | Intrathecal | Cervical, thoracic and lumbar AIS A | Subacute | Rehabilitation | ASIA, SCIM-III, EMG, NCV, MRI, UDS | Recovery of trunk movement and equilibrium in standing/sitting positions, reduction in the severity of constipation, sensation of the filling bladder, voiding. | Score Sensory (pinprick and light touch); SCIM III total score respiration and sphincter management, mobility, and self-care; | Oraee-Yazdani 2021 |
| 5 × 107/kg | Allogenic UC | Subarachnoid | Cervical, thoracic, thoracolumbar ASIA A-D | Chronic | ASIA, IANR-SCIFRS, MRI Penn scale, Geffner, Neurogenic Bowel Dysfunction score, RUV | Improvements of pinprick, light touch, motor and sphincter scores. Decrease in muscle spasticity | Improvements in muscle spasm, autonomic system, bladder and bowel functions, RUV and MRI | Yang et al., 2020 |
| References | Fever | Numbness or Tingling | Facial Flushing | Headache | Neuropathic Pain | Spasticity | Pain at the Site | Dizziness | Cerebrospinal Fluid Leakage | Respiratory Infections | Nausea and Vomiting | Sensory Deterioration | Urinary Disturbances |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pal et al., 2009 |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Ra et al., 2011 |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Karamouzian et al., 2012 |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Dai et al., 2013 |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Jiang et al., 2013 |  |  |  |  |  |  |  |  |  |  |  |  |  |
| El-Kheir et al., 2014 |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Cheng et al., 2014 |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Mendonça et al., 2014 |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Larocca et al., 2017 |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Satti et al., 2016 |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Vaquero et al., 2016 |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Vaquero et al., 2017 |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Vaquero et al., 2018 |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Hur et al., 2016 |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Oh et al., 2016 |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Oraee-Yazdani et al., 2021 |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Yang et al., 2021 |  |  |  |  |  |  |  |  |  |  |  |  |  |
 AE present;
AE present;  AE absent.
AE absent.| References | Clinical Trial Phase | Description of Study Design | Criteria of Eligibility Well Defined | Cell Therapy Intervention Detailing | Other Associated Interventions | Group Control | Sample Size | Randomization | Allocation Sequence Method | Blinding | Matching | Description of Detailed Clinical Features | Clinical Trials.Gov Registry |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| El-Kheir et al., 2014 | Phase 1/Phase 2 | Yes | Yes | Yes | Yes | Yes | 70 | Yes | Not mentioned | Single blinded | Not mentioned | Yes | Yes |
| Pal et al., 2009 | Pilot clinical study | Yes | Yes | Yes | Not mentioned | No | 30 | Not mentioned | Not mentioned | Not mentioned | Not mentioned | No | Yes |
| Ra et al., 2011 | Phase 1 | Yes | Yes | Yes | Not mentioned | No | 8 | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Yes | Yes |
| Oh et al., 2016 | Phase 3 | Yes | Yes | Yes | Yes | No | 16 | No | No | No | No | Yes | Not mentioned |
| Hur et al., 2016 | Pilot clinical study | Yes | Yes | Yes | No | No | 14 | No | No | No | No | Yes | Not mentioned |
| Karamouzian et al., 2012 | Phase 1/Phase 2 | Yes | Yes | Yes | Yes | Yes | 31 | No | No | No | No | Yes | Not mentioned |
| Dai et al., 2013 | Not mentioned | Yes | Yes | Yes | Yes | Yes | 40 | Yes | No | Single blinded | Yes | Yes | Not mentioned |
| Cheng et al., 2014 | Phase 2 | Yes | Yes | Yes | No | Yes | 34 | Yes | Not mentioned | Not mentioned | Yes | Yes | Yes |
| Jiang et al., 2013 | Not mentioned | Yes | Yes | Yes | No | No | 20 | No | No | No | No | Yes | Not mentioned |
| Mendonça et al., 2014 | Phase 1 | Yes | Yes | Yes | Yes | No | 14 | No | No | No | No | Yes | Yes |
| Larocca et al., 2016 | Phase 1 | Yes | Yes | Yes | Not mentioned | No | 5 | No | No | No | No | Yes | Yes |
| Satti et al., 2016 | Phase 1 | Yes | Yes | Yes | Yes | Yes | 9 | No | No | No | No | Yes | Yes |
| Vaquero et al., 2016 | Phase 1/Phase 2 | Yes | Yes | Yes | Not mentioned | No | 12 | No | No | No | No | Yes | Yes |
| Vaquero et al., 2017 | Phase 2 | Yes | Yes | No | Not mentioned | No | 10 | No | No | No | No | Yes | Yes |
| Vaquero et al., 2018 | Phase 2 | Yes | Yes | Yes | Not mentioned | No | 6 | No | No | No | No | Yes | Not mentioned |
| Oraee-Yazdani et al., 2021 | Phase 1/Phase 2 | Yes | Yes | Yes | Yes | No | 11 | No | No | No | No | Yes | Not mentioned |
| Yang et al., 2021 | Phase 1/Phase 2 | Yes | Yes | Yes | Not mentioned | No | 41 | No | No mentioned | No | No | Yes | Not mentioned |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Araújo, L.T.; Macêdo, C.T.; Damasceno, P.K.F.; das Neves, Í.G.C.; de Lima, C.S.; Santos, G.C.; de Santana, T.A.; Sampaio, G.L.d.A.; Silva, D.N.; Villarreal, C.F.; et al. Clinical Trials Using Mesenchymal Stem Cells for Spinal Cord Injury: Challenges in Generating Evidence. Cells 2022, 11, 1019. https://doi.org/10.3390/cells11061019
de Araújo LT, Macêdo CT, Damasceno PKF, das Neves ÍGC, de Lima CS, Santos GC, de Santana TA, Sampaio GLdA, Silva DN, Villarreal CF, et al. Clinical Trials Using Mesenchymal Stem Cells for Spinal Cord Injury: Challenges in Generating Evidence. Cells. 2022; 11(6):1019. https://doi.org/10.3390/cells11061019
Chicago/Turabian Stylede Araújo, Lila Teixeira, Carolina Thé Macêdo, Patrícia Kauanna Fonseca Damasceno, Ítalo Gabriel Costa das Neves, Carla Souza de Lima, Girlaine Café Santos, Thaís Alves de Santana, Gabriela Louise de Almeida Sampaio, Daniela Nascimento Silva, Cristiane Flora Villarreal, and et al. 2022. "Clinical Trials Using Mesenchymal Stem Cells for Spinal Cord Injury: Challenges in Generating Evidence" Cells 11, no. 6: 1019. https://doi.org/10.3390/cells11061019
APA Stylede Araújo, L. T., Macêdo, C. T., Damasceno, P. K. F., das Neves, Í. G. C., de Lima, C. S., Santos, G. C., de Santana, T. A., Sampaio, G. L. d. A., Silva, D. N., Villarreal, C. F., Chaguri, A. C. d. C., da Silva, C. G., Mota, A. C. d. A., Badaró, R., Ribeiro dos Santos, R., & Soares, M. B. P. (2022). Clinical Trials Using Mesenchymal Stem Cells for Spinal Cord Injury: Challenges in Generating Evidence. Cells, 11(6), 1019. https://doi.org/10.3390/cells11061019








