Assessment of a Serum Microrna Risk Score for Colorectal Cancer among Participants of Screening Colonoscopy at Various Stages of Colorectal Carcinogenesis
Abstract
:1. Introduction
2. Materials and Methods
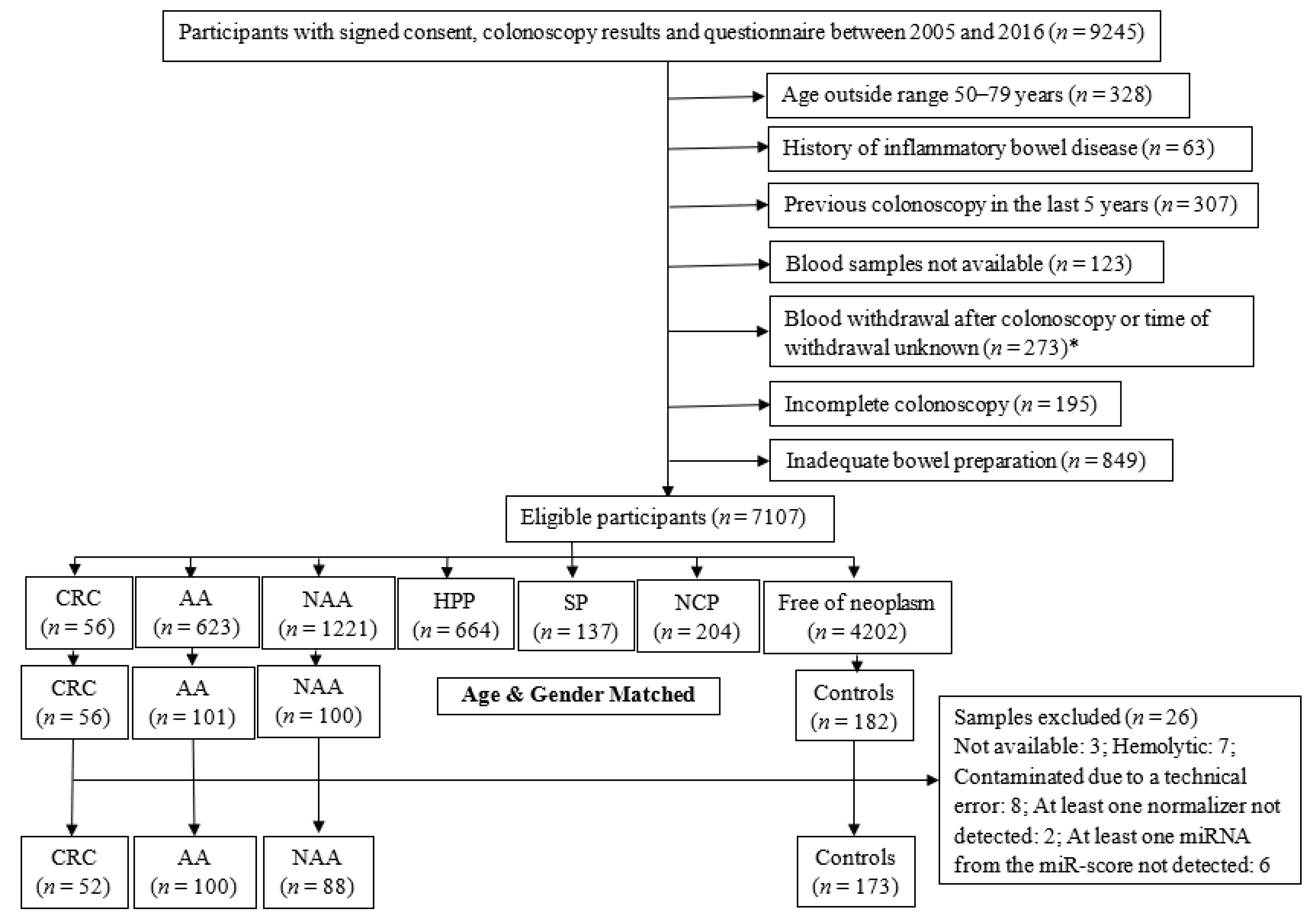
2.1. Study Design and Population
2.2. MiRNA Profiling by Quantitative Real-Time PCR (qPCR)
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Study Population
3.2. qPCR Quality Controls
3.3. Comparison of miR-Score Distributions between Groups with Various Findings at Screening Colonoscopy
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AA | advanced colorectal adenoma |
| AUC | area under the receiver operating characteristic curve |
| BliTz | Begleitende Evaluierung innovativer Testverfahren zur Darmkrebs-Früherkennung |
| cDNA | complementary DNA |
| CI | confidence interval |
| Cq | quantification cycle |
| CRC | colorectal cancer |
| HPP | hyperplastic polyp |
| HLS | healthy lifestyle score |
| miRNA | microRNA |
| miR-score | microRNA risk score |
| n | number |
| NAA | non-advanced colorectal adenoma |
| NCP | non-classified polyp |
| OR | odds ratio |
| PRS | polygenic risk score |
| qPCR | quantitative real-time polymerase chain reaction |
| Ref. | reference category |
| SD | standard deviation |
| SP | serrated poly |
| TNM | Tumour Nodes Metastasis classification |
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Nishihara, R.; Wu, K.; Lochhead, P.; Morikawa, T.; Liao, X.; Qian, Z.R.; Inamura, K.; Kim, S.A.; Kuchiba, A.; Yamauchi, M.; et al. Long-term colorectal-cancer incidence and mortality after lower endoscopy. N. Engl. J. Med. 2013, 369, 1095–1105. [Google Scholar] [CrossRef] [Green Version]
- Shaukat, A.; Mongin, S.J.; Geisser, M.S.; Lederle, F.A.; Bond, J.H.; Mandel, J.S.; Church, T.R. Long-term mortality after screening for colorectal cancer. N. Engl. J. Med. 2013, 369, 1106–1114. [Google Scholar] [CrossRef] [PubMed]
- Brenner, H.; Stock, C.; Hoffmeister, M. Effect of screening sigmoidoscopy and screening colonoscopy on colorectal cancer incidence and mortality: Systematic review and meta-analysis of randomised controlled trials and observational studies. BMJ 2014, 348, g2467. [Google Scholar] [CrossRef] [Green Version]
- Hassan, C.; Rossi, P.G.; Camilloni, L.; Rex, D.K.; Jimenez-Cendales, B.; Ferroni, E.; Borgia, P.; Zullo, A.; Guasticchi, G. Meta-analysis: Adherence to colorectal cancer screening and the detection rate for advanced neoplasia, according to the type of screening test. Aliment. Pharmacol. Ther. 2012, 36, 929–940. [Google Scholar] [CrossRef] [PubMed]
- Young, P.E.; Womeldorph, C.M. Colonoscopy for colorectal cancer screening. J. Cancer 2013, 4, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Kim, H.S.; Park, H.J. Adverse events related to colonoscopy: Global trends and future challenges. World J. Gastroenterol. 2019, 25, 190–204. [Google Scholar] [CrossRef]
- Niedermaier, T.; Tikk, K.; Gies, A.; Bieck, S.; Brenner, H. Sensitivity of fecal immunochemical test for colorectal cancer detection differs according to stage and location. Clin. Gastroenterol. Hepatol. 2020, 18, 2920–2928. [Google Scholar] [CrossRef]
- Niedermaier, T.; Balavarca, Y.; Brenner, H. Stage-Specific Sensitivity of Fecal Immunochemical Tests for Detecting Colorectal Cancer: Systematic Review and Meta-Analysis. Am. J. Gastroenterol. 2020, 115, 56–69. [Google Scholar] [CrossRef] [Green Version]
- Thomas, M.; Sakoda, L.C.; Hoffmeister, M.; Rosenthal, E.A.; Lee, J.K.; van Duijnhoven, F.J.; Platz, E.A.; Wu, A.H.; Dampier, C.H.; de la Chapelle, A.; et al. Genome-wide Modeling of Polygenic Risk Score in Colorectal Cancer Risk. Am. J. Hum. Genet. 2020, 107, 432–444. [Google Scholar] [CrossRef]
- Ibáñez-Sanz, G.; Díez-Villanueva, A.; Alonso, M.H.; Moranta, F.R.; Pérez-Gómez, B.; Bustamante, M.; Martin, V.; Llorca, J.; Amiano, P.; Ardanaz, E.; et al. Risk Model for Colorectal Cancer in Spanish Population Using Environmental and Genetic Factors: Results from the MCC-Spain study. Sci. Rep. 2017, 7, 43263. [Google Scholar] [CrossRef] [PubMed]
- Gafni, A.; Dite, G.S.; Spaeth Tuff, E.; Allman, R.; Hopper, J.L. Ability of known colorectal cancer susceptibility SNPs to predict colorectal cancer risk: A cohort study within the UK Biobank. PLoS ONE 2021, 16, e0251469. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, J.; Hayder, H.; Zayed, Y.; Peng, C. Overview of MicroRNA Biogenesis, Mechanisms of Actions, and Circulation. Front. Endocrinol. 2018, 9, 402. [Google Scholar] [CrossRef] [Green Version]
- Strubberg, A.M.; Madison, B.B. MicroRNAs in the etiology of colorectal cancer: Pathways and clinical implications. Dis. Model. Mech. 2017, 10, 197–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schetter, A.J.; Okayama, H.; Harris, C.C. The role of microRNAs in colorectal cancer. Cancer J. 2012, 18, 244–252. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mitchell, P.S.; Parkin, R.K.; Kroh, E.M.; Fritz, B.R.; Wyman, S.K.; Pogosova-Agadjanyan, E.L.; Peterson, A.; Noteboom, J.; O’Briant, K.C.; Allen, A.; et al. Circulating microRNAs as stable blood-based markers for cancer detection. Proc. Natl. Acad. Sci. USA 2008, 105, 10513–10518. [Google Scholar] [CrossRef] [Green Version]
- Raut, J.R.; Schöttker, B.; Holleczek, B.; Guo, F.; Bhardwaj, M.; Miah, K.; Schrotz-King, P.; Brenner, H. A microRNA panel compared to environmental and polygenic scores for colorectal cancer risk prediction. Nat. Commun. 2021, 12, 4811. [Google Scholar] [CrossRef]
- Hundt, S.; Haug, U.; Brenner, H. Comparative evaluation of immunochemical fecal occult blood tests for colorectal adenoma detection. Ann. Intern. Med. 2009, 150, 162–169. [Google Scholar] [CrossRef]
- Blondal, T.; Jensby Nielsen, S.; Baker, A.; Andreasen, D.; Mouritzen, P.; Wrang Teilum, M.; Dahlsveen, I.K. Assessing sample and miRNA profile quality in serum and plasma or other biofluids. Methods 2013, 59, S1–S6. [Google Scholar] [CrossRef]
- Kirschner, M.B.; Edelman, J.J.; Kao, S.C.; Vallely, M.P.; van Zandwijk, N.; Reid, G. The Impact of Hemolysis on Cell-Free microRNA Biomarkers. Front. Genet. 2013, 4, 94. [Google Scholar] [CrossRef] [Green Version]
- Pritchard, C.C.; Kroh, E.; Wood, B.; Arroyo, J.D.; Dougherty, K.J.; Miyaji, M.M.; Tait, J.F.; Tewari, M. Blood cell origin of circulating microRNAs: A cautionary note for cancer biomarker studies. Cancer Prev. Res. 2012, 5, 492–497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shah, J.S.; Soon, P.S.; Marsh, D.J. Comparison of Methodologies to Detect Low Levels of Hemolysis in Serum for Accurate Assessment of Serum microRNAs. PLoS ONE 2016, 11, e0153200. [Google Scholar] [CrossRef] [PubMed]
- Ramakers, C.; Ruijter, J.M.; Deprez, R.H.; Moorman, A.F. Assumption-free analysis of quantitative real-time polymerase chain reaction (PCR) data. Neurosci. Lett. 2003, 339, 62–66. [Google Scholar] [CrossRef]
- Andersen, C.L.; Jensen, J.L.; Orntoft, T.F. Normalization of real-time quantitative reverse transcription-PCR data: A model-based variance estimation approach to identify genes suited for normalization, applied to bladder and colon cancer data sets. Cancer Res. 2004, 64, 5245–5250. [Google Scholar] [CrossRef] [Green Version]
- Schmittgen, T.D.; Lee, E.J.; Jiang, J.; Sarkar, A.; Yang, L.; Elton, T.S.; Chen, C. Real-time PCR quantification of precursor and mature microRNA. Methods 2008, 44, 31–38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pritchard, C.C.; Cheng, H.H.; Tewari, M. MicroRNA profiling: Approaches and considerations. Nat. Rev. Genet. 2012, 13, 358–369. [Google Scholar] [CrossRef] [PubMed]
- Jensen, S.G.; Lamy, P.; Rasmussen, M.H.; Ostenfeld, M.S.; Dyrskjøt, L.; Ørntoft, T.F.; Andersen, C.L. Evaluation of two commercial global miRNA expression profiling platforms for detection of less abundant miRNAs. BMC Genom. 2011, 12, 435. [Google Scholar] [CrossRef] [Green Version]
- Marabita, F.; de Candia, P.; Torri, A.; Tegnér, J.; Abrignani, S.; Rossi, R.L. Normalization of circulating microRNA expression data obtained by quantitative real-time RT-PCR. Brief. Bioinform. 2015, 17, 204–212. [Google Scholar] [CrossRef] [Green Version]
- Carter, J.V.; Galbraith, N.J.; Yang, D.; Burton, J.F.; Walker, S.P.; Galandiuk, S. Blood-based microRNAs as biomarkers for the diagnosis of colorectal cancer: A systematic review and meta-analysis. Br. J. Cancer 2017, 116, 762–774. [Google Scholar] [CrossRef] [PubMed]
- Marcuello, M.; Duran-Sanchon, S.; Moreno, L.; Lozano, J.J.; Bujanda, L.; Castells, A.; Gironella, M. Analysis of A 6-Mirna Signature in Serum from Colorectal Cancer Screening Participants as Non-Invasive Biomarkers for Advanced Adenoma and Colorectal Cancer Detection. Cancers 2019, 11, 1542. [Google Scholar] [CrossRef] [Green Version]
- Rodriguez-Montes, J.A.; Menendez Sanchez, P. Role of micro-RNA in colorectal cancer screening. Cir. Esp. 2014, 92, 654–658. [Google Scholar] [CrossRef] [PubMed]
- Toiyama, Y.; Okugawa, Y.; Fleshman, J.; Richard Boland, C.; Goel, A. MicroRNAs as potential liquid biopsy biomarkers in colorectal cancer: A systematic review. Biochim. Biophys. Acta (BBA)—Rev. Cancer 2018, 1870, 274–282. [Google Scholar] [CrossRef] [PubMed]
- Zanutto, S.; Ciniselli, C.M.; Belfiore, A.; Lecchi, M.; Masci, E.; Delconte, G.; Primignani, M.; Tosetti, G.; Fante, M.D.; Fazzini, L.; et al. Plasma miRNA-based signatures in CRC screening programs. Int. J. Cancer 2020, 146, 1164–1173. [Google Scholar] [CrossRef] [Green Version]
- Sun, Y.; Liu, Y.; Cogdell, D.; Calin, G.A.; Sun, B.; Kopetz, S.; Hamilton, S.R.; Zhang, W. Examining plasma microRNA markers for colorectal cancer at different stages. Oncotarget 2016, 7, 11434–11449. [Google Scholar] [CrossRef] [Green Version]
- Erben, V.; Carr, P.R.; Guo, F.; Weigl, K.; Hoffmeister, M.; Brenner, H. Individual and Joint Associations of Genetic Risk and Healthy Lifestyle Score with Colorectal Neoplasms Among Participants of Screening Colonoscopy. Cancer Prev. Res. 2021, 14, 649–658. [Google Scholar] [CrossRef] [PubMed]
- Wikberg, M.L.; Myte, R.; Palmqvist, R.; van Guelpen, B.; Ljuslinder, I. Plasma miRNA can detect colorectal cancer, but how early? Cancer Med. 2018, 7, 1697–1705. [Google Scholar] [CrossRef]
- Keller, A.; Fehlmann, T.; Backes, C.; Kern, F.; Gislefoss, R.; Langseth, H.; Rounge, T.B.; Ludwig, N.; Meese, E. Competitive learning suggests circulating miRNA profiles for cancers decades prior to diagnosis. RNA Biol. 2020, 17, 1416–1426. [Google Scholar] [CrossRef] [PubMed]
- Petrovic, N.; Ergun, S.; Isenovic, E.R. Levels of MicroRNA Heterogeneity in Cancer Biology. Mol. Diagn. Ther. 2017, 21, 511–523. [Google Scholar] [CrossRef]
| Characteristics | CRC Cases (n = 52) | AA Cases (n = 100) | NAA Cases (n = 88) | Controls (n = 173) |
|---|---|---|---|---|
| Age (Years) | ||||
| Mean (SD) | 66.3 (6.1) | 65.4 (6.6) | 65.2 (6.1) | 65.7 (6.7) |
| Median (Interquartile Range) | 67 (62–71) | 65 (60–71) | 65 (61–70) | 66 (60–71) |
| Sex (%) | ||||
| Male | 33 (63.5) | 65 (65.0) | 55 (62.5) | 109 (63.0) |
| Female | 19 (36.5) | 35 (35.0) | 33 (37.5) | 64 (37.0) |
| TNM stage—counts (%) | ||||
| Stage I | 17 (32.7) | - | - | - |
| Stage II | 6 (11.5) | - | - | - |
| Stage III | 22 (42.3) | - | - | - |
| Stage IV | 7 (13.5) | - | - | - |
| miR-Score | Comparison CRC–AA | Comparison AA–NAA | Comparison NAA–No Neoplasm | ||||
|---|---|---|---|---|---|---|---|
| CRC (n = 52) | AA (n = 100) | NAA (n = 88) | No neoplasm (n = 173) | ||||
| Mean (SD) | −0.8 (0.7) | −0.6 (0.7) | −0.8 (0.7) | −0.6 (0.7) | |||
| Median (Range) | −0.8 (−2.6–0.7) | −0.5 (−2.4–1.2) | −0.8 (−2.6–0.9) | −0.6 (−3.3–3.0) | |||
| p-Value a | 0.014 | 0.027 | 0.127 | ||||
| miR-Score Category b | OR (95% CI) c | OR (95% CI) c | OR (95% CI) c | ||||
| Low | 24 (46.2) | Ref | 28 (28.0) | Ref | 32 (36.4) | Ref | 58 (33.5) |
| Medium | 15 (28.8) | 0.54 (0.23−1.22) | 32 (32.0) | 1.05 (0.52−2.12) | 35 (39.8) | 1.07 (0.58−1.98) | 57 (32.9) |
| High | 13 (25.0) | 0.37 (0.16−0.86) | 40 (40.0) | 2.22 (1.06−4.64) | 21 (23.9) | 0.63 (0.32−1.24) | 58 (33.5) |
| OR per SD Increase | 0.66 (0.47−0.94) | 1.35 (1.00−1.82) | 0.79 (0.61−1.04) | ||||
| AUC | 0.38 (0.28−0.47) | 0.59 (0.51−0.68) | 0.44 (0.37−0.52) | ||||
| Brier Score | 0.269 | 0.280 | 0.257 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raut, J.R.; Bhardwaj, M.; Niedermaier, T.; Miah, K.; Schrotz-King, P.; Brenner, H. Assessment of a Serum Microrna Risk Score for Colorectal Cancer among Participants of Screening Colonoscopy at Various Stages of Colorectal Carcinogenesis. Cells 2022, 11, 2462. https://doi.org/10.3390/cells11152462
Raut JR, Bhardwaj M, Niedermaier T, Miah K, Schrotz-King P, Brenner H. Assessment of a Serum Microrna Risk Score for Colorectal Cancer among Participants of Screening Colonoscopy at Various Stages of Colorectal Carcinogenesis. Cells. 2022; 11(15):2462. https://doi.org/10.3390/cells11152462
Chicago/Turabian StyleRaut, Janhavi R., Megha Bhardwaj, Tobias Niedermaier, Kaya Miah, Petra Schrotz-King, and Hermann Brenner. 2022. "Assessment of a Serum Microrna Risk Score for Colorectal Cancer among Participants of Screening Colonoscopy at Various Stages of Colorectal Carcinogenesis" Cells 11, no. 15: 2462. https://doi.org/10.3390/cells11152462
APA StyleRaut, J. R., Bhardwaj, M., Niedermaier, T., Miah, K., Schrotz-King, P., & Brenner, H. (2022). Assessment of a Serum Microrna Risk Score for Colorectal Cancer among Participants of Screening Colonoscopy at Various Stages of Colorectal Carcinogenesis. Cells, 11(15), 2462. https://doi.org/10.3390/cells11152462






