T Cell Interactions in Mycobacterial Granulomas: Non-Specific T Cells Regulate Mycobacteria-Specific T Cells in Granulomatous Lesions
Abstract
:1. Introduction
2. Materials and Methods
2.1. Mice
2.2. Infections
2.3. Testing Transgenic T Cells for Reactivity to PCC-BCG Antigens
2.4. Cell Isolation and Flow Cytometry
2.5. Adoptive Transfer and Immunization
2.6. Immunofluorescence
2.7. Histopathology
2.8. Multiplex Cytokine Assay
3. Results
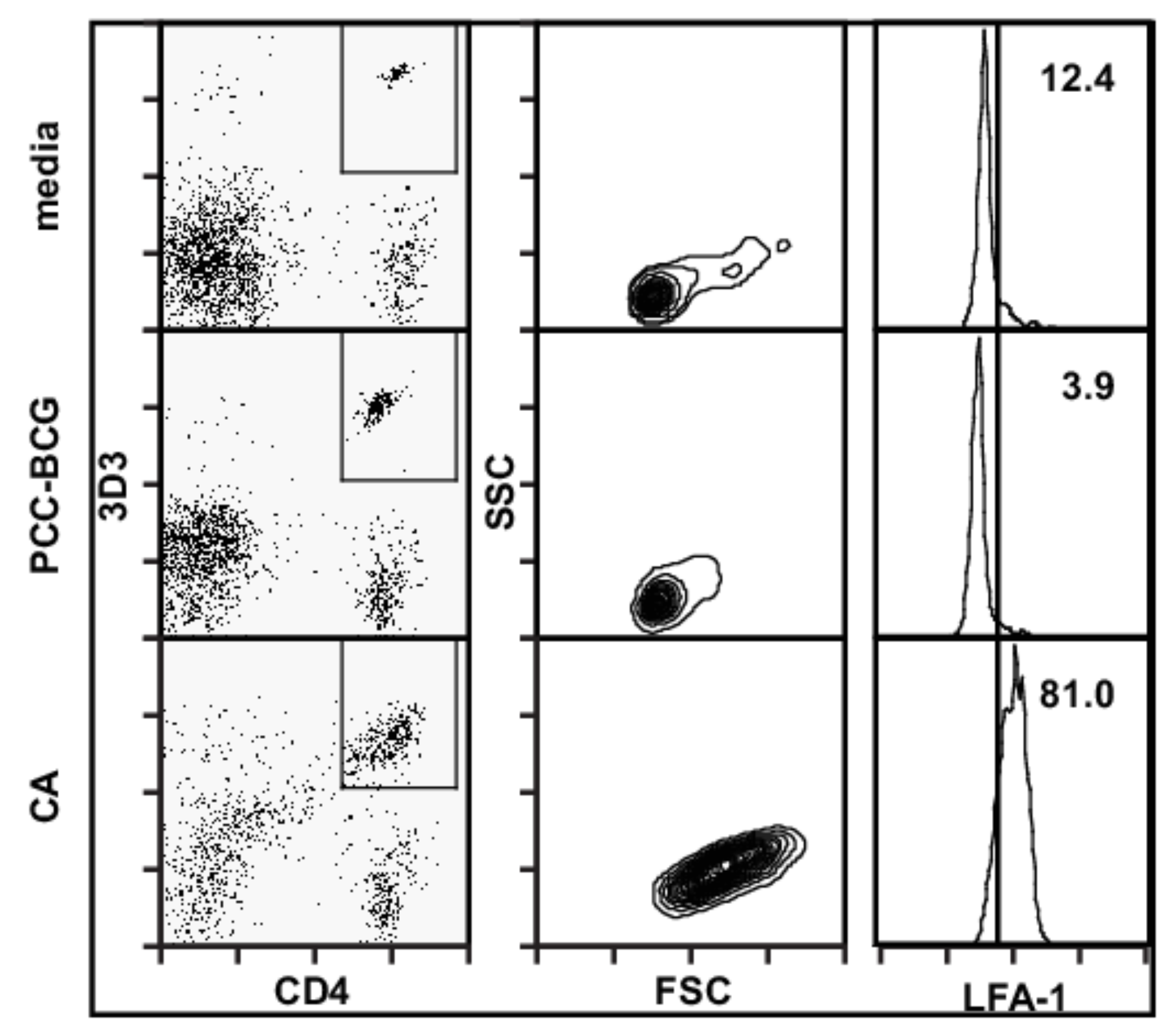
3.1. D10 T Cells Are Not Activated by PCC-BCG
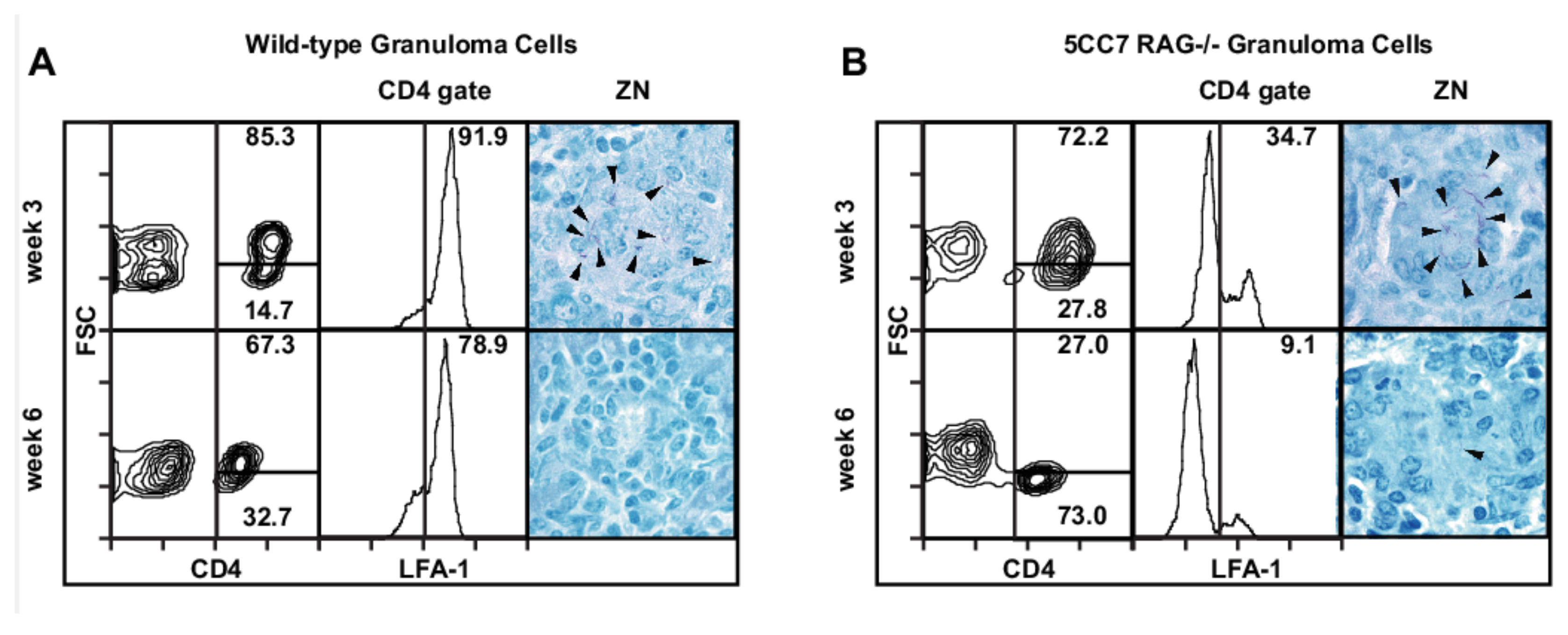
3.2. Acutely Activated BCG-Non-Specific T Cells Have Access to the Granuloma
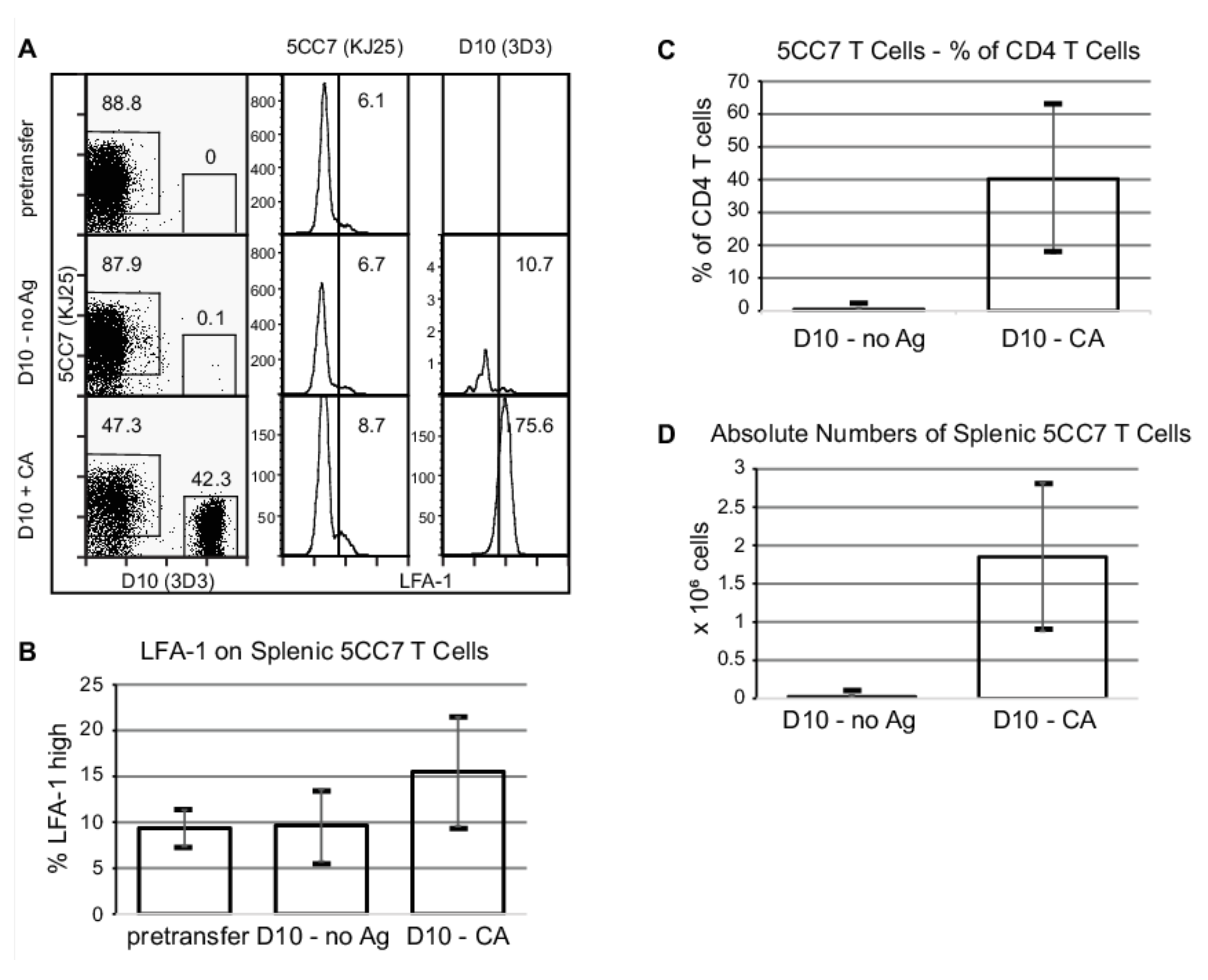
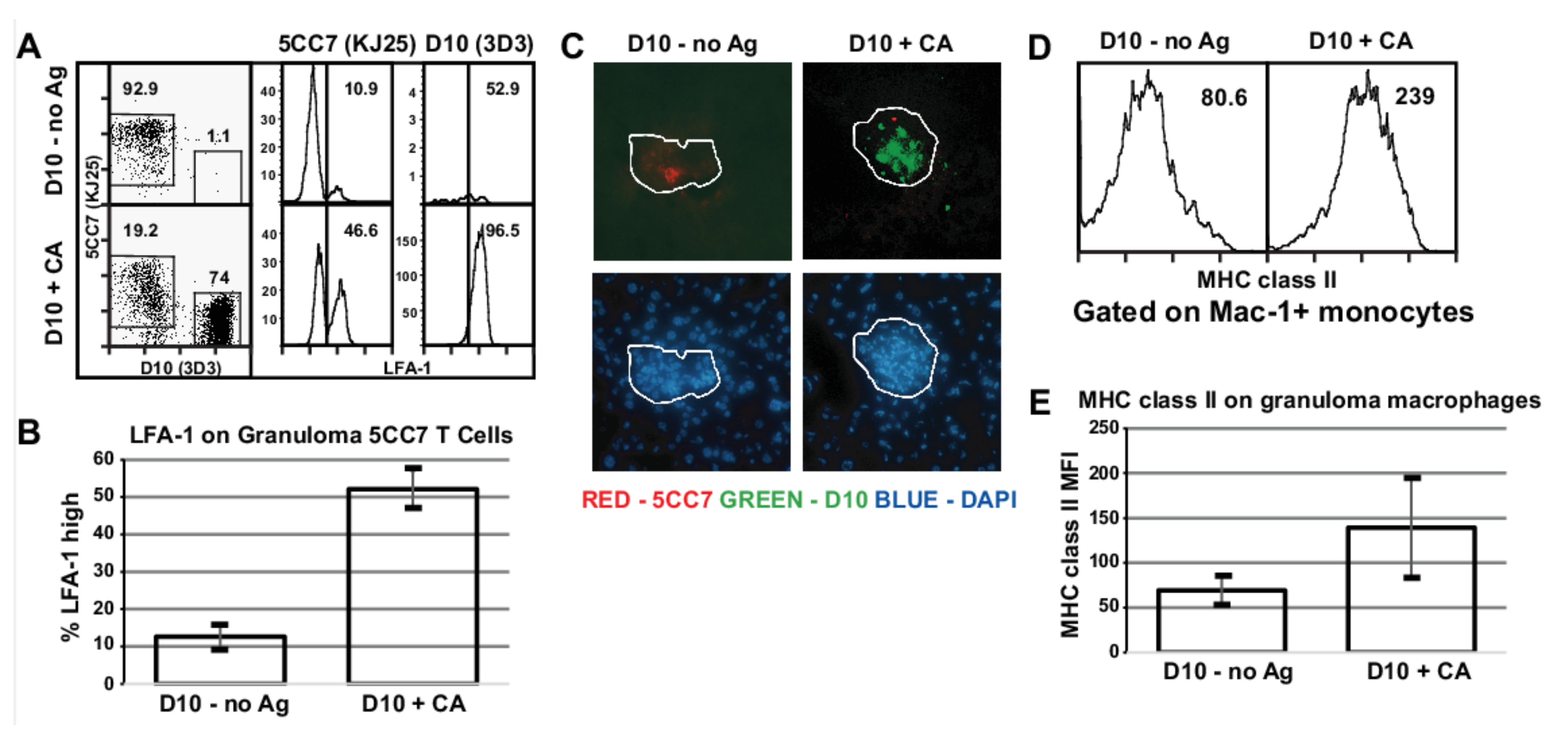
3.3. Acute Activation of Local Antigen Non-Specific T Cells Increases the Activation of Granuloma Antigen Specific T Cells
3.4. CA Restimulation of Granuloma-Infiltrating D10 T Cells from CA-Immunized Mice Elicits a Profile of Cytokines That Can Contribute to Protection against Mycobacteria
3.5. PCC-Stimulated Cytokine Secretion by Granuloma Infiltrating Cells Is Upregulated by Recruited Activated BCG-Non-Specific T Cells
3.6. Activation of Non-Specific T Cells Suppresses Cytokine Secretion by BCG-Specific Spleen Cells
3.7. Accumulation of Activated D10 T Cells Results in Increased Granuloma Macrophage Activation
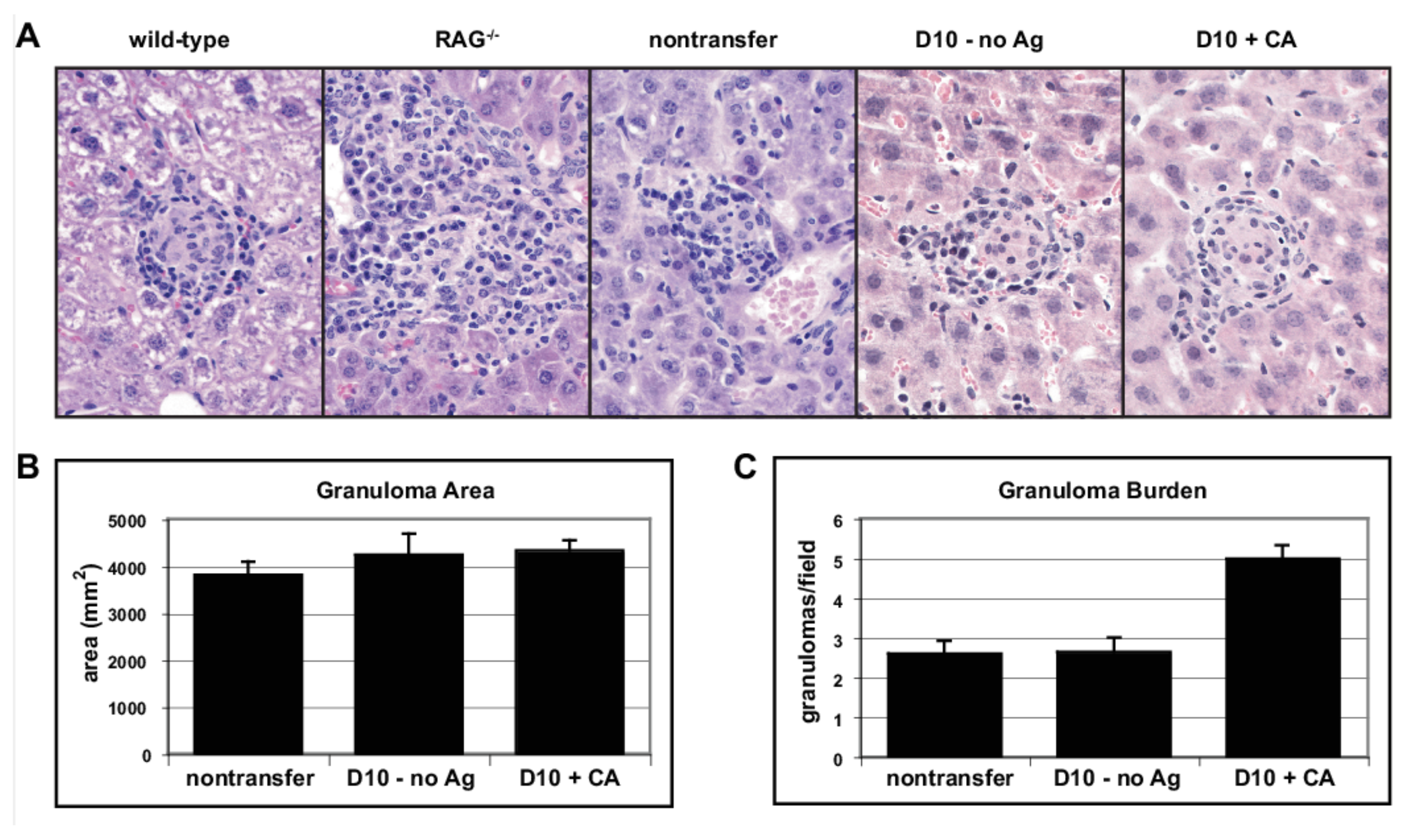
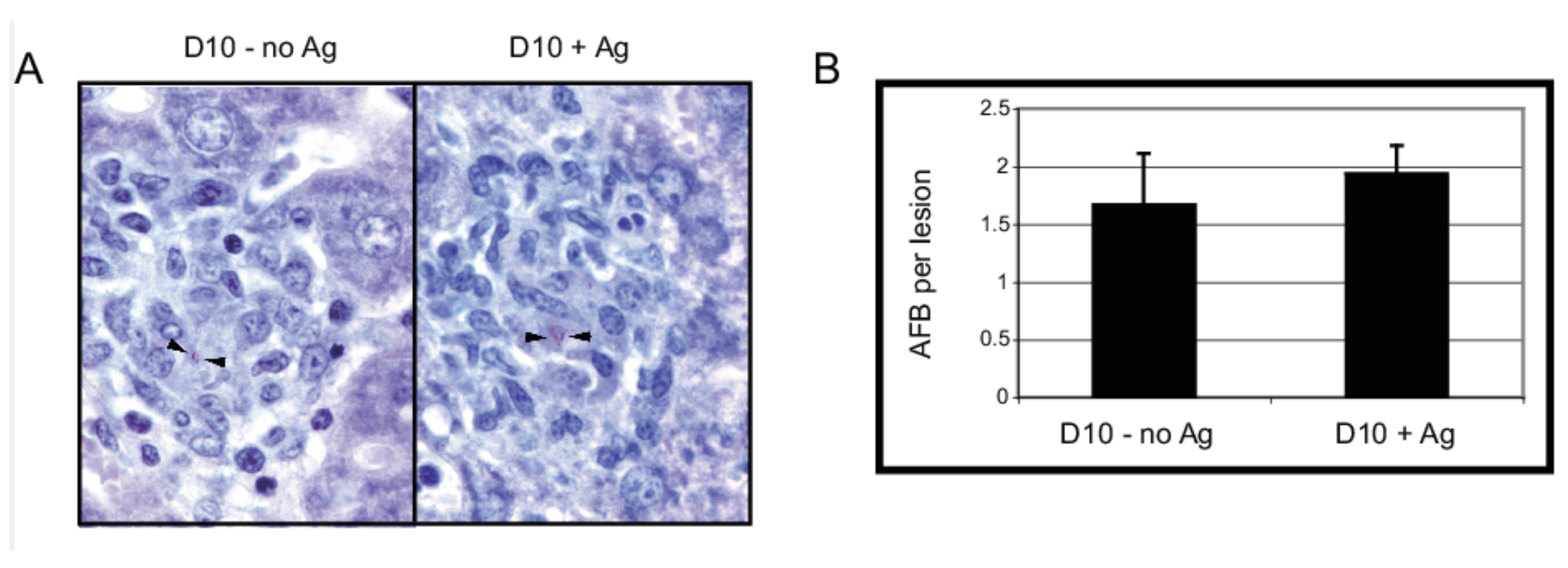
3.8. Effect of Non-Specific T Cells on Granuloma Structure and Function
4. Discussion
4.1. Accumulation of Non-Specific T Cells
4.2. Anergy and Granuloma Function
4.3. Activated D10 T Cells Suppress Systemic PCC-Specific T Cells
5. Summary
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CA | conalbumin |
| PCC | pigeon cytochrome C |
| HEL | hen egg lysozyme |
| BCG | Mycobacterium bovis strain bacille Calmette-Guérin |
| Mtb | M. tuberculosis |
| Tg | transgenic |
| AFB | acid-fast bacilli |
| LCMV | lymphocytic choriomeningitis virus. |
References
- Hingley-Wilson, S.M.; Sambandamurthy, V.K.; Jacobs, W.R., Jr. Survival perspectives from the world’s most successful pathogen, Mycobacterium tuberculosis. Nat. Immunol. 2003, 4, 949–955. [Google Scholar] [CrossRef] [PubMed]
- Flynn, J.L.; Chan, J. Immunology of tuberculosis. Annu. Rev. Immunol. 2001, 19, 93–129. [Google Scholar] [CrossRef] [PubMed]
- Saunders, B.M.; Cooper, A.M. Restraining mycobacteria: Role of granulomas in mycobacterial infections. Immunol. Cell. Biol. 2000, 78, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Saunders, B.M.; Frank, A.A.; Orme, I.M.; Cooper, A.M. CD4 is required for the development of a protective granulomatous response to pulmonary tuberculosis. Cell. Immunol. 2002, 216, 65–72. [Google Scholar] [CrossRef]
- Ladel, C.H.; Hess, J.; Daugelat, S.; Mombaerts, P.; Tonegawa, S.; Kaufmann, S.H. Contribution of alpha/beta and gamma/delta T lymphocytes to immunity against Mycobacterium bovis bacillus Calmette Guerin: Studies with T cell receptor-deficient mutant mice. Eur. J. Immunol. 1995, 25, 838–846. [Google Scholar] [CrossRef]
- Caruso, A.M.; Serbina, N.; Klein, E.; Triebold, K.; Bloom, B.R.; Flynn, J.L. Mice deficient in CD4 T cells have only transiently diminished levels of IFN-gamma, yet succumb to tuberculosis. J. Immunol. 1999, 162, 5407–5416. [Google Scholar]
- Ladel, C.H.; Daugelat, S.; Kaufmann, S.H. Immune response to Mycobacterium bovis bacille Calmette Guerin infection in major histocompatibility complex class I- and II-deficient knock-out mice: Contribution of CD4 and CD8 T cells to acquired resistance. Eur. J. Immunol. 1995, 25, 377–384. [Google Scholar] [CrossRef]
- Feng, C.G.; Britton, W.J. CD4+ and CD8+ T cells mediate adoptive immunity to aerosol infection of Mycobacterium bovis bacillus Calmette-Gu inverted question markerin. J. Infect. Dis. 2000, 181, 1846–1849. [Google Scholar] [CrossRef] [Green Version]
- Hogan, L.H.; MacVilay, K.; Barger, B.; Co, D.; Malkovska, I.; Fennelly, G.; Sandor, M. Mycobacterium bovis strain bacillus Calmette-Guerin-induced liver granulomas contain a diverse TCR repertoire, but a monoclonal T cell population is sufficient for protective granuloma formation. J. Immunol. 2001, 166, 6367–6375. [Google Scholar] [CrossRef] [Green Version]
- Co, D.O.; Hogan, L.H.; Il-Kim, S.; Sandor, M. T cell contributions to the different phases of granuloma formation. Immunol. Lett. 2004, 92, 135–142. [Google Scholar] [CrossRef]
- Roach, D.R.; Bean, A.G.; Demangel, C.; France, M.P.; Briscoe, H.; Britton, W.J. TNF regulates chemokine induction essential for cell recruitment, granuloma formation, and clearance of mycobacterial infection. J. Immunol. 2002, 168, 4620–4627. [Google Scholar] [CrossRef] [Green Version]
- Roach, D.R.; Briscoe, H.; Saunders, B.; France, M.P.; Riminton, S.; Britton, W.J. Secreted Lymphotoxin-alpha Is Essential for the Control of an Intracellular Bacterial Infection. J. Exp. Med. 2001, 193, 239–246. [Google Scholar] [CrossRef] [Green Version]
- Ehlers, S.; Kutsch, S.; Ehlers, E.M.; Benini, J.; Pfeffer, K. Lethal Granuloma Disintegration in Mycobacteria-Infected TNFRp55−/− Mice Is Dependent on T Cells and IL-12. J. Immunol. 2000, 165, 483–492. [Google Scholar] [CrossRef]
- Pearl, J.E.; Saunders, B.; Ehlers, S.; Orme, I.M.; Cooper, A.M. Inflammation and lymphocyte activation during mycobacterial infection in the interferon-gamma-deficient mouse. Cell. Immunol. 2001, 211, 43–50. [Google Scholar] [CrossRef]
- Hogan, L.H.; Markofski, W.; Bock, A.; Barger, B.; Morrissey, J.D.; Sandor, M. Mycobacterium bovis BCG-induced granuloma formation depends on gamma interferon and CD40 ligand but does not require CD28. Infect. Immun. 2001, 69, 2596–2603. [Google Scholar] [CrossRef] [Green Version]
- Barnes, P.F.; Bloch, A.B.; Davidson, P.T.; Snider, D.E., Jr. Tuberculosis in patients with human immunodeficiency virus infection. N. Engl. J. Med. 1991, 324, 1644–1650. [Google Scholar] [CrossRef]
- Scanga, C.A.; Mohan, V.P.; Yu, K.; Joseph, H.; Tanaka, K.; Chan, J.; Flynn, J.L. Depletion of CD4+ T Cells Causes Reactivation of Murine Persistent Tuberculosis Despite Continued Expression of Interferon Gamma and Nitric Oxide Synthase 2. J. Exp. Med. 2000, 192, 347–358. [Google Scholar] [CrossRef]
- Hogan, L.H.; Wang, M.; Suresh, M.; Co, D.O.; Weinstock, J.V.; Sandor, M. CD4+ TCR repertoire heterogeneity in Schistosoma mansoni-induced granulomas. J. Immunol. 2002, 169, 6386–6393. [Google Scholar] [CrossRef]
- Mempel, M.; Musette, P.; Flageul, B.; Schnopp, C.; Remling, R.; Gachelin, G.; Kourilsky, P.; Ring, J.; Abeck, D. T-cell receptor repertoire and cytokine pattern in granuloma annulare: Defining a particular type of cutaneous granulomatous inflammation. J. Invest. Derm. 2002, 118, 957–966. [Google Scholar] [CrossRef] [Green Version]
- Seder, R.A.; Paul, W.E.; Davis, M.M.; Fazekas de St Groth, B. The Presence of Interleukin-4 during in Vitro Priming Determines the Lymphokine-producing Potential of CD4+ T Cells from T Cell Receptor Transgenic Mice. J. Exp. Med. 1992, 176, 1091–1098. [Google Scholar] [CrossRef]
- Sant’Angelo, D.B.; Waterbury, G.; Preston-Hurlburt, P.; Yoon, S.T.; Medzhitov, R.; Hong, S.C.; Janeway, C.A., Jr. The specificity and orientation of a TCR to its peptide-MHC class II ligands. Immunity 1996, 4, 367–376. [Google Scholar] [CrossRef] [Green Version]
- Kaye, J.; Porcelli, S.; Tite, J.; Jones, B.; Janeway, C.A., Jr. Both a monoclonal antibody and antisera specific for determinants unique to individual cloned helper T cell lines can substitute for antigen and antigen-presenting cells in the activation of T cells. J. Exp. Med. 1983, 158, 836–856. [Google Scholar] [CrossRef] [Green Version]
- Yang, H.Y.; Dundon, P.L.; Nahill, S.R.; Welsh, R.M. Virus-induced polyclonal cytotoxic T lymphocyte stimulation. J. Immunol. 1989, 142, 1710–1718. [Google Scholar]
- Morgan, J.; Muskat, K.; Tippalagama, R.; Sette, A.; Burel, J.; Lindestam Arlehamn, C.S. Classical CD4 T cells as the cornerstone of antimycobacterial immunity. Immunol. Rev. 2021, 301, 10–29. [Google Scholar] [CrossRef]
- Behar, S.M.; Carpenter, S.M.; Booty, M.G.; Barber, D.L.; Jayaraman, P. Orchestration of pulmonary T cell immunity during Mycobacterium tuberculosis infection: Immunity interruptus. Semin. Immunol. 2014, 26, 559–577. [Google Scholar] [CrossRef] [Green Version]
- Sakai, S.; Mayer-Barber, K.D.; Barber, D.L. Defining features of protective CD4 T cell responses to Mycobacterium tuberculosis. Curr. Opin. Immunol. 2014, 29, 137–142. [Google Scholar] [CrossRef] [Green Version]
- Reinhardt, R.L.; Bullard, D.C.; Weaver, C.T.; Jenkins, M.K. Preferential accumulation of antigen-specific effector CD4 T cells at an antigen injection site involves CD62E-dependent migration but not local proliferation. J. Exp. Med. 2003, 197, 751–762. [Google Scholar] [CrossRef]
- Topham, D.J.; Castrucci, M.R.; Wingo, F.S.; Belz, G.T.; Doherty, P.C. The role of antigen in the localization of naive, acutely activated, and memory CD8(+) T cells to the lung during influenza pneumonia. J. Immunol. 2001, 167, 6983–6990. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sewell, D.L.; Reinke, E.K.; Co, D.O.; Hogan, L.H.; Fritz, R.B.; Sandor, M.; Fabry, Z. Infection with Mycobacterium bovis BCG diverts traffic of myelin oligodendroglial glycoprotein autoantigen-specific T cells away from the central nervous system and ameliorates experimental autoimmune encephalomyelitis. Clin. Diagn. Lab. Immunol. 2003, 10, 564–572. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moser, B.; Loetscher, P. Lymphocyte traffic control by chemokines. Nat. Immunol. 2001, 2, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Campbell, D.J.; Debes, G.F.; Johnston, B.; Wilson, E.; Butcher, E.C. Targeting T cell responses by selective chemokine receptor expression. Semin. Immunol. 2003, 15, 277–286. [Google Scholar] [CrossRef]
- Cotterell, S.E.; Engwerda, C.R.; Kaye, P.M. Leishmania donovani infection initiates T cell-independent chemokine responses, which are subsequently amplified in a T cell-dependent manner. Eur. J. Immunol. 1999, 29, 203–214. [Google Scholar] [CrossRef]
- Millar, J.A.; Butler, J.R.; Evans, S.; Mattila, J.T.; Linderman, J.J.; Flynn, J.L.; Kirschner, D.E. Spatial Organization and Recruitment of Non-Specific T Cells May Limit T Cell-Macrophage Interactions Within Mycobacterium tuberculosis Granulomas. Front. Immunol. 2020, 11, 613638. [Google Scholar] [CrossRef]
- Zea, A.H.; Ochoa, M.T.; Ghosh, P.; Longo, D.L.; Alvord, W.G.; Valderrama, L.; Falabella, R.; Harvey, L.K.; Saravia, N.; Moreno, L.H.; et al. Changes in expression of signal transduction proteins in T lymphocytes of patients with leprosy. Infect. Immun. 1998, 66, 499–504. [Google Scholar] [CrossRef] [Green Version]
- Seitzer, U.; Kayser, K.; Hohn, H.; Entzian, P.; Wacker, H.H.; Ploetz, S.; Flad, H.D.; Gerdes, J.; Maeurer, M.J. Reduced T-cell receptor CD3zeta-chain protein and sustained CD3epsilon expression at the site of mycobacterial infection. Immunology 2001, 104, 269–277. [Google Scholar] [CrossRef]
- Maurice, M.M.; Lankester, A.C.; Bezemer, A.C.; Geertsma, M.F.; Tak, P.P.; Breedveld, F.C.; van Lier, R.A.; Verweij, C.L. Defective TCR-mediated signaling in synovial T cells in rheumatoid arthritis. J. Immunol. 1997, 159, 2973–2978. [Google Scholar]
- Wherry, E.J.; Blattman, J.N.; Murali-Krishna, K.; van der Most, R.; Ahmed, R. Viral persistence alters CD8 T-cell immunodominance and tissue distribution and results in distinct stages of functional impairment. J. Virol. 2003, 77, 4911–4927. [Google Scholar] [CrossRef] [Green Version]
- Oxenius, A.; Zinkernagel, R.M.; Hengartner, H. Comparison of activation versus induction of unresponsiveness of virus-specific CD4+ and CD8+ T cells upon acute versus persistent viral infection. Immunity 1998, 9, 449–457. [Google Scholar] [CrossRef] [Green Version]
- Akkaraju, S.; Ho, W.Y.; Leong, D.; Canaan, K.; Davis, M.M.; Goodnow, C.C. A range of CD4 T cell tolerance: Partial inactivation to organ-specific antigen allows nondestructive thyroiditis or insulitis. Immunity 1997, 7, 255–271. [Google Scholar] [CrossRef] [Green Version]
- Rocha, B.; Tanchot, C.; Von Boehmer, H. Clonal anergy blocks in vivo growth of mature T cells and can be reversed in the absence of antigen. J. Exp. Med. 1993, 177, 1517–1521. [Google Scholar] [CrossRef]
- Egen, J.G.; Rothfuchs, A.G.; Feng, C.G.; Winter, N.; Sher, A.; Germain, R.N. Macrophage and T cell dynamics during the development and disintegration of mycobacterial granulomas. Immunity 2008, 28, 271–284. [Google Scholar] [CrossRef] [Green Version]
- Egen, J.G.; Rothfuchs, A.G.; Feng, C.G.; Horwitz, M.A.; Sher, A.; Germain, R.N. Intravital imaging reveals limited antigen presentation and T cell effector function in mycobacterial granulomas. Immunity 2011, 34, 807–819. [Google Scholar] [CrossRef] [Green Version]
- Patankar, Y.R.; Sutiwisesak, R.; Boyce, S.; Lai, R.; Lindestam Arlehamn, C.S.; Sette, A.; Behar, S.M. Limited recognition of Mycobacterium tuberculosis-infected macrophages by polyclonal CD4 and CD8 T cells from the lungs of infected mice. Mucosal Immunol. 2020, 13, 140–148. [Google Scholar] [CrossRef]
- Clark, J.M.; Annenkov, A.E.; Panesar, M.; Isomaki, P.; Chernajovsky, Y.; Cope, A.P. T cell receptor zeta reconstitution fails to restore responses of T cells rendered hyporesponsive by tumor necrosis factor alpha. Proc. Natl. Acad. Sci. USA 2004, 101, 1696–1701. [Google Scholar] [CrossRef] [Green Version]
- Isomaki, P.; Panesar, M.; Annenkov, A.; Clark, J.M.; Foxwell, B.M.; Chernajovsky, Y.; Cope, A.P. Prolonged exposure of T cells to TNF down-regulates TCR zeta and expression of the TCR/CD3 complex at the cell surface. J. Immunol. 2001, 166, 5495–5507. [Google Scholar] [CrossRef] [Green Version]
- Sarukhan, A.; Lanoue, A.; Franzke, A.; Brousse, N.; Buer, J.; von Boehmer, H. Changes in function of antigen-specific lymphocytes correlating with progression towards diabetes in a transgenic model. EMBO J. 1998, 17, 71–80. [Google Scholar] [CrossRef] [Green Version]
- Grewal, I.S.; Grewal, K.D.; Wong, F.S.; Picarella, D.E.; Janeway, C.A., Jr.; Flavell, R.A. Local expression of transgene encoded TNF alpha in islets prevents autoimmune diabetes in nonobese diabetic (NOD) mice by preventing the development of auto-reactive islet-specific T cells. J. Exp. Med. 1996, 184, 1963–1974. [Google Scholar] [CrossRef] [Green Version]
- Schreiber, H.A.; Hulseberg, P.D.; Lee, J.; Prechl, J.; Barta, P.; Szlavik, N.; Harding, J.S.; Fabry, Z.; Sandor, M. Dendritic cells in chronic mycobacterial granulomas restrict local anti-bacterial T cell response in a murine model. PLoS ONE 2010, 5, e11453. [Google Scholar] [CrossRef]
- Schwartz, R.H. T cell anergy. Annu. Rev. Immunol. 2003, 21, 305–334. [Google Scholar] [CrossRef]
- Chakir, H.; Lam, D.K.; Lemay, A.M.; Webb, J.R. “Bystander polarization” of CD4+ T cells: Activation with high-dose IL-2 renders naive T cells responsive to IL-12 and/or IL-18 in the absence of TCR ligation. Eur. J. Immunol. 2003, 33, 1788–1798. [Google Scholar] [CrossRef]
- Marsland, B.J.; Harris, N.L.; Camberis, M.; Kopf, M.; Hook, S.M.; Le Gros, G. Bystander suppression of allergic airway inflammation by lung resident memory CD8+ T cells. Proc. Natl. Acad. Sci. USA 2004, 101, 6116–6121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Unutmaz, D.; Pileri, P.; Abrignani, S. Antigen-independent activation of naive and memory resting T cells by a cytokine combination. J. Exp. Med. 1994, 180, 1159–1164. [Google Scholar] [CrossRef] [PubMed]
- Beverly, B.; Kang, S.M.; Lenardo, M.J.; Schwartz, R.H. Reversal of in vitro T cell clonal anergy by IL-2 stimulation. Int. Immunol. 1992, 4, 661–671. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, M.K.; Chen, C.A.; Jung, G.; Mueller, D.L.; Schwartz, R.H. Inhibition of antigen-specific proliferation of type 1 murine T cell clones after stimulation with immobilized anti-CD3 monoclonal antibody. J. Immunol. 1990, 144, 16–22. [Google Scholar]
- Cowley, S.C.; Elkins, K.L. CD4+ T cells mediate IFN-gamma-independent control of Mycobacterium tuberculosis infection both in vitro and in vivo. J. Immunol. 2003, 171, 4689–4699. [Google Scholar] [CrossRef] [Green Version]
- Gallegos, A.M.; van Heijst, J.W.; Samstein, M.; Su, X.; Pamer, E.G.; Glickman, M.S. A gamma interferon independent mechanism of CD4 T cell mediated control of M. tuberculosis infection in vivo. PLoS Pathog. 2011, 7, e1002052. [Google Scholar] [CrossRef] [Green Version]
- Kedl, R.M.; Rees, W.A.; Hildeman, D.A.; Schaefer, B.; Mitchell, T.; Kappler, J.; Marrack, P. T cells compete for access to antigen-bearing antigen-presenting cells. J. Exp. Med. 2000, 192, 1105–1114. [Google Scholar] [CrossRef]
- Kedl, R.M.; Schaefer, B.C.; Kappler, J.W.; Marrack, P. T cells down-modulate peptide-MHC complexes on APCs in vivo. Nat. Immunol. 2002, 3, 27–32. [Google Scholar] [CrossRef]
- Smith, A.L.; Wikstrom, M.E.; Fazekas de St Groth, B. Visualizing T cell competition for peptide/MHC complexes: A specific mechanism to minimize the effect of precursor frequency. Immunity 2000, 13, 783–794. [Google Scholar] [CrossRef] [Green Version]
- Duthoit, C.T.; Nguyen, P.; Geiger, T.L. Antigen nonspecific suppression of T cell responses by activated stimulation-refractory CD4(+) T cells. J. Immunol. 2004, 172, 2238–2246. [Google Scholar] [CrossRef] [Green Version]

| D10 Transferred, CA Immunized | ||||
|---|---|---|---|---|
| Spleen | Granuloma | |||
| Media | CA | Media | CA | |
| Cytokines | ||||
| IL-2 | <3.2 | 1894.3 | <3.2 | 520.1 |
| IFN-γ | <3.2 | >10,000 | 57 | >10,000 |
| TNF | 13.3 | 1323.2 | 145.1 | 488.9 |
| IL-17 | <3.2 | 61.1 | 3.9 | 246.9 |
| IL-4 | <3.2 | 368 | <3.2 | 118.6 |
| IL-5 | <3.2 | 32.6 | 17.7 | 114.7 |
| IL-9 | <3.2 | 7.8 | <3.2 | 14.2 |
| IL-13 | <3.2 | 414.4 | <3.2 | 86.2 |
| IL-1α | <3.2 | 172.8 | 9.3 | 215.7 |
| IL-1ß | 12.5 | 211 | 66.9 | 314 |
| IL-6 | 83.6 | >18,000 | 4968.2 | 9256.5 |
| IL-10 | <3.2 | 231.7 | 81 | 396.2 |
| Chemokines | ||||
| MIP-1α | 21 | 1401 | 66 | >10,000 |
| MCP-1 | 243 | 2101 | 2057 | 1536 |
| RANTES | <3.2 | 70 | 84 | 179 |
| IP-10 | 237.6 | 400 | 310.6 | 531.5 |
| KC | <3.2 | 7 | 333 | 456 |
| Macrophage Growth Factors | ||||
| GM-CSF | <3.2 | 7439 | 115 | 4908 |
| G-CSF | <3.2 | 2034.6 | 858.1 | 1991 |
| D10 T cells/106 cells | 8.55 × 104 | 6.7 × 104 | ||
| Spleen | Granuloma | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nontransfer | D10—No Ag | D10 + CA | Nontransfer | D10—No Ag | D10 + CA | |||||||
| Media | PCC | Media | PCC | Media | PCC | Media | PCC | Media | PCC | Media | PCC | |
| Cytokines | ||||||||||||
| IL-2 | <3.2 | 515.9 | <3.2 | 363.1 | <3.2 | 46.3 | <3.2 | <3.2 | <3.2 | <3.2 | <3.2 | 15.9 |
| IFN-γ | <3.2 | >10,000 | <3.2 | >10,000 | <3.2 | 934 | <3.2 | <3.2 | <3.2 | <3.2 | 57 | 377 |
| TNF | 6.2 | 455.5 | 7.7 | 494 | 13.3 | 208.9 | 10.7 | 18.6 | 3.9 | 13.5 | 145.1 | 190.5 |
| IL-17 | <3.2 | 32 | <3.2 | 6.4 | <3.2 | 9.6 | <3.2 | <3.2 | <3.2 | <3.2 | 3.9 | 72.4 |
| IL-4 | <3.2 | 3.7 | <3.2 | 11 | <3.2 | <3.2 | <3.2 | <3.2 | <3.2 | <3.2 | <3.2 | <3.2 |
| IL-5 | <3.2 | 12.1 | <3.2 | 10.5 | <3.2 | 3.4 | <3.2 | <3.2 | <3.2 | <3.2 | 17.7 | 45.4 |
| IL-9 | <3.2 | <3.2 | 6.5 | 6.5 | <3.2 | <3.2 | 10.1 | <3.2 | <3.2 | <3.2 | <3.2 | <3.2 |
| IL-13 | <3.2 | 6.6 | <3.2 | 9.5 | <3.2 | <3.2 | <3.2 | <3.2 | <3.2 | <3.2 | <3.2 | 7.9 |
| IL-1α | <3.2 | 114.3 | <3.2 | 105.8 | <3.2 | 9.6 | <3.2 | <3.2 | <3.2 | <3.2 | 9.3 | 27.4 |
| IL-1ß | 6.1 | 111.4 | 8.2 | 91.6 | 12.5 | 30.2 | <3.2 | <3.2 | <3.2 | <3.2 | 66.9 | 83.8 |
| IL-6 | 15.2 | 7913.2 | 32.8 | 8930.1 | 83.6 | 2486.4 | 489.2 | 633.3 | 45.5 | 66.6 | 4968.2 | 8554.9 |
| IL-10 | <3.2 | 91 | 8.3 | 84.1 | <3.2 | 53.4 | <3.2 | 10.5 | <3.2 | <3.2 | 81 | 169.4 |
| Chemokines | ||||||||||||
| MIP-1α | 22 | 4259 | 34 | 1201 | 21 | 89 | 66 | 126 | 5 | 25 | 66 | 755 |
| MCP-1 | 191 | 803 | 338 | 1442 | 243 | 1459 | 465 | 455 | 43 | 55 | 2057 | 2637 |
| RANTES | <3.2 | 516 | <3.2 | 379 | <3.2 | 76 | 4 | 11 | <3.2 | 6 | 84 | 184 |
| IP-10 | 271.9 | 681.2 | 263.7 | 367.1 | 237.6 | 369.8 | 31.7 | 33.9 | <3.2 | 9.4 | 310.6 | 590 |
| KC | <3.2 | 9 | <3.2 | 5 | <3.2 | <3.2 | 75 | 114 | 10 | 14 | 333 | 580 |
| Macrophage Growth Factors | ||||||||||||
| GM-CSF | <3.2 | 762 | 21 | 1126 | <3.2 | 422 | 15 | 21 | <3.2 | <3.2 | 115 | 354 |
| G-CSF | <3.2 | 915.1 | <3.2 | 1254.2 | <3.2 | 408.5 | 51.9 | 73.5 | 9.7 | 16.4 | 858.1 | 2348.3 |
| 5CC7 T cells/106 cells | 3.9 × 105 | 2.0 × 105 | 1.2 × 105 | 4.0 × 104 | 4.7 × 104 | 1.7 × 104 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Co, D.O.; Hogan, L.H.; Karman, J.; Herbath, M.; Fabry, Z.; Sandor, M. T Cell Interactions in Mycobacterial Granulomas: Non-Specific T Cells Regulate Mycobacteria-Specific T Cells in Granulomatous Lesions. Cells 2021, 10, 3285. https://doi.org/10.3390/cells10123285
Co DO, Hogan LH, Karman J, Herbath M, Fabry Z, Sandor M. T Cell Interactions in Mycobacterial Granulomas: Non-Specific T Cells Regulate Mycobacteria-Specific T Cells in Granulomatous Lesions. Cells. 2021; 10(12):3285. https://doi.org/10.3390/cells10123285
Chicago/Turabian StyleCo, Dominic O., Laura H. Hogan, Jozsef Karman, Melinda Herbath, Zsuzsanna Fabry, and Matyas Sandor. 2021. "T Cell Interactions in Mycobacterial Granulomas: Non-Specific T Cells Regulate Mycobacteria-Specific T Cells in Granulomatous Lesions" Cells 10, no. 12: 3285. https://doi.org/10.3390/cells10123285
APA StyleCo, D. O., Hogan, L. H., Karman, J., Herbath, M., Fabry, Z., & Sandor, M. (2021). T Cell Interactions in Mycobacterial Granulomas: Non-Specific T Cells Regulate Mycobacteria-Specific T Cells in Granulomatous Lesions. Cells, 10(12), 3285. https://doi.org/10.3390/cells10123285






