The WNT/ROR Pathway in Cancer: From Signaling to Therapeutic Intervention
Abstract
1. Introduction
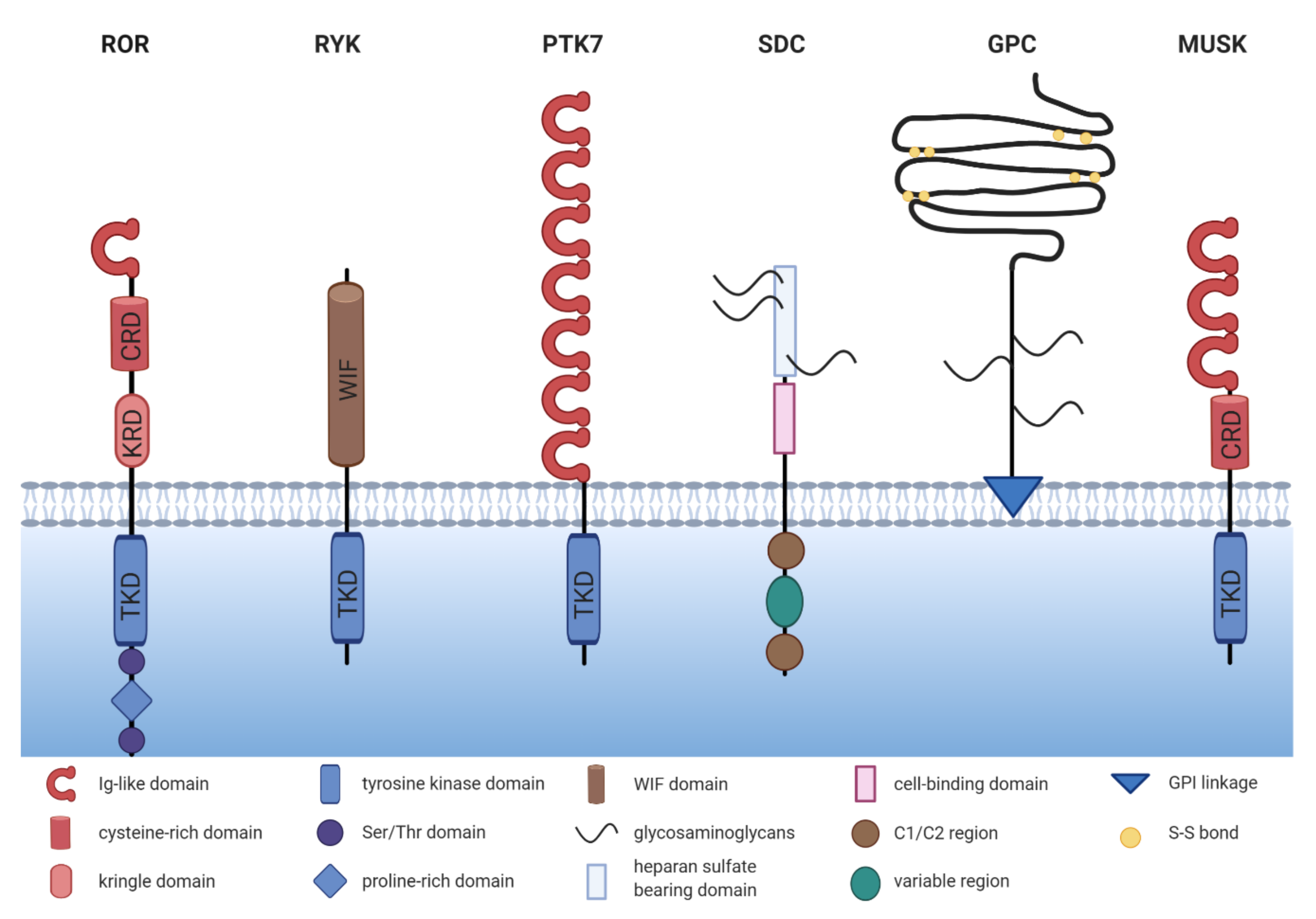
2. The ROR Family
3. Expression of ROR1/2 in Cancer
3.1. Expression of ROR1/2 in Healthy Tissue
3.2. Expression of ROR1/2 in Hematological Malignancies
3.3. Expression of ROR1 in Solid Tumors
3.4. Expression of ROR2 in Solid Tumors—It Is Not Always That Simple
3.5. ROR1/2 in the Tumor Stroma
4. The Function of ROR1/2 in Cancer
4.1. ROR1/2 in Cell Proliferation and Survival
4.2. ROR1/2 in Therapy Resistance and Cancer Stem Cells
4.3. ROR1/2 in EMT and Metastasis
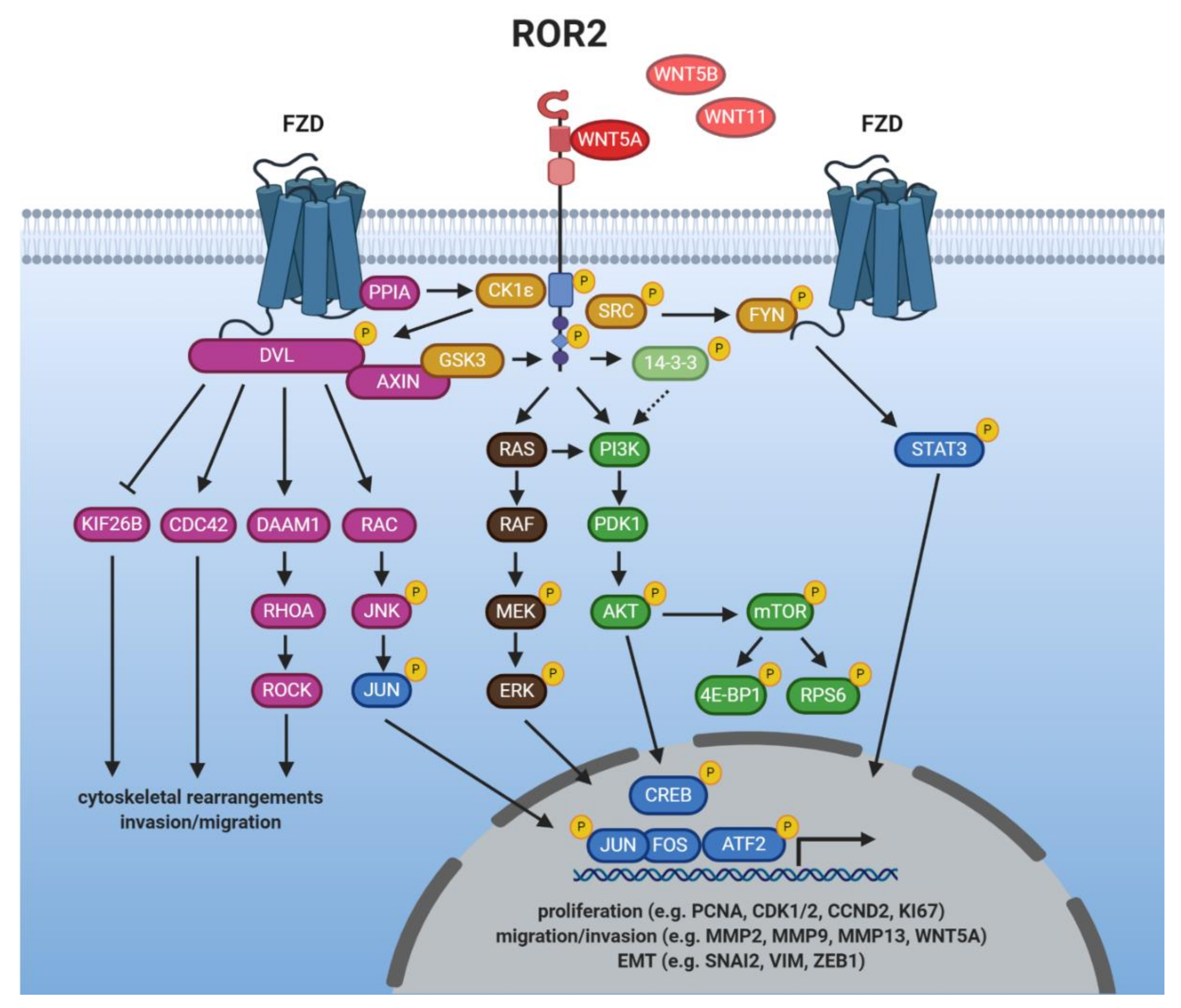
5. WNT/ROR Signaling at a Glance
5.1. Ligands of ROR1/2
5.2. Getting the RORs Started: Receptor Activation
5.3. Induction of Non-Canonical WNT Signaling
5.4. Crosstalk with Canonical WNT Signaling
5.5. Crosstalk with Other Major Cancer Signaling Pathways
5.6. ROR1/2 in the Nucleus—More Than Hearsay?
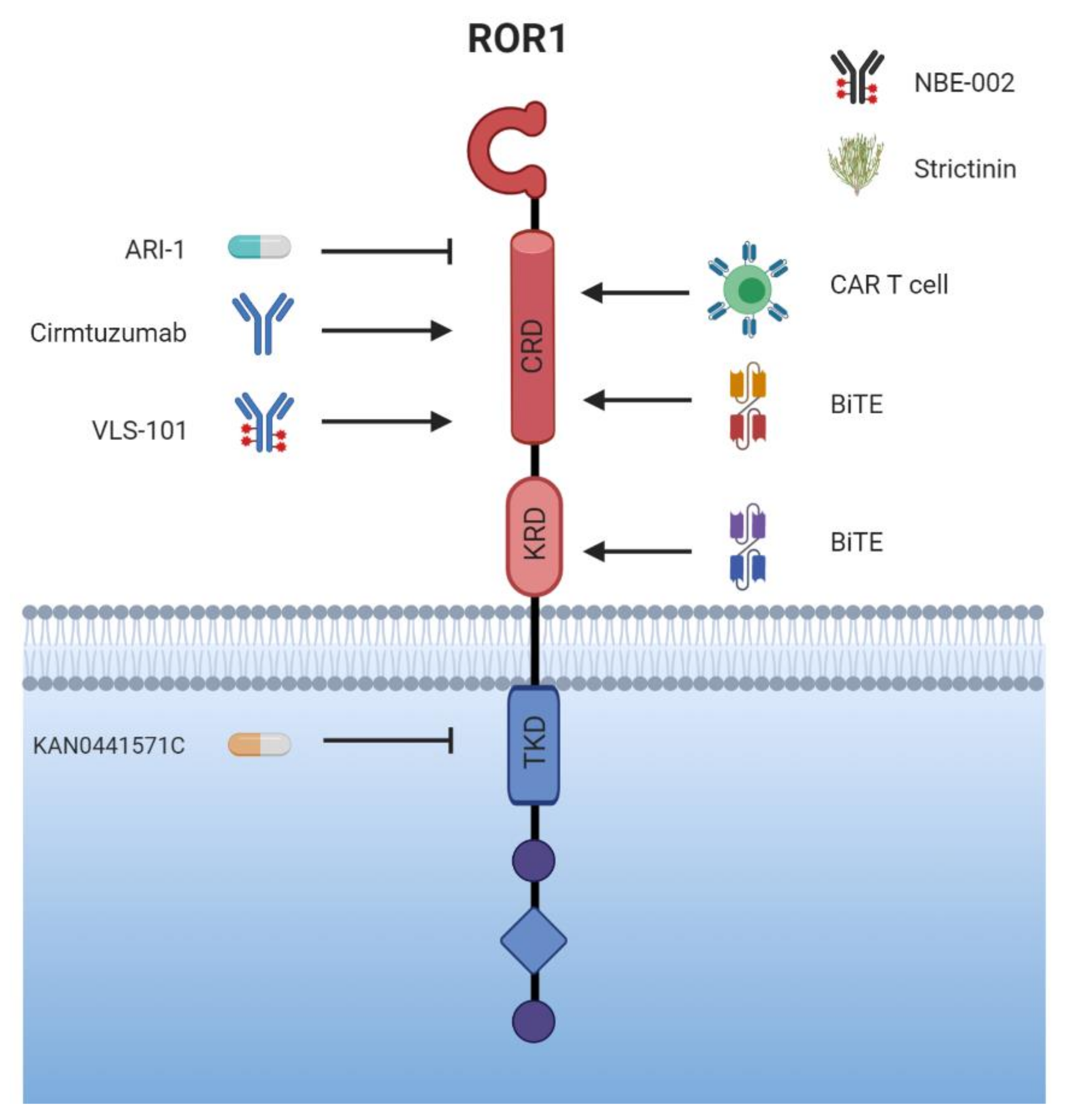
6. Targeted Therapy
6.1. For Starters: The Humanized Monoclonal Antibody (mAb) Cirmtuzumab
6.2. New Approaches—Going beyond Cirmtuzumab?
6.3. More Is More: Conjugates and Bispecific Antibodies
6.4. CAR-T Cells—Promising Future or More about Adverse Events?
6.5. Small Molecule—Big Impact?
6.6. ROR2, the Wallflower?—To Be Continued
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nusse, R.; Clevers, H. Wnt/β-Catenin Signaling, Disease, and Emerging Therapeutic Modalities. Cell 2017, 169, 985–999. [Google Scholar] [CrossRef] [PubMed]
- Mikels, A.J.; Nusse, R. Purified Wnt5a Protein Activates or Inhibits Beta-Catenin-TCF Signaling Depending on Receptor Context. PLoS Biol. 2006, 4, e115. [Google Scholar] [CrossRef] [PubMed]
- Anthony, C.C.; Robbins, D.J.; Ahmed, Y.; Lee, E. Nuclear Regulation of Wnt/β-Catenin Signaling: It’s a Complex Situation. Genes 2020, 11, 886. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Mlodzik, M. Wnt-Frizzled/Planar Cell Polarity Signaling: Cellular Orientation by Facing the Wind (Wnt). Annu. Rev. Cell Dev. Biol. 2015, 31, 623–646. [Google Scholar] [CrossRef]
- Haseeb, M.; Pirzada, R.H.; Ain, Q.U.; Choi, S. Wnt Signaling in the Regulation of Immune Cell and Cancer Therapeutics. Cells 2019, 8, 1380. [Google Scholar] [CrossRef]
- DeChiara, T.M.; Kimble, R.B.; Poueymirou, W.T.; Rojas, J.; Masiakowski, P.; Valenzuela, D.M.; Yancopoulos, G.D. Ror2, Encoding a Receptor-like Tyrosine Kinase, Is Required for Cartilage and Growth Plate Development. Nat. Genet. 2000, 24, 271–274. [Google Scholar] [CrossRef]
- Takeuchi, S.; Takeda, K.; Oishi, I.; Nomi, M.; Ikeya, M.; Itoh, K.; Tamura, S.; Ueda, T.; Hatta, T.; Otani, H.; et al. Mouse Ror2 Receptor Tyrosine Kinase Is Required for the Heart Development and Limb Formation. Genes Cells 2000, 5, 71–78. [Google Scholar] [CrossRef]
- Nomi, M.; Oishi, I.; Kani, S.; Suzuki, H.; Matsuda, T.; Yoda, A.; Kitamura, M.; Itoh, K.; Takeuchi, S.; Takeda, K.; et al. Loss of MRor1 Enhances the Heart and Skeletal Abnormalities in MRor2-Deficient Mice: Redundant and Pleiotropic Functions of MRor1 and MRor2 Receptor Tyrosine Kinases. Mol. Cell. Biol. 2001, 21, 8329–8335. [Google Scholar] [CrossRef]
- Oldridge, M.; Fortuna, A.M.; Maringa, M.; Propping, P.; Mansour, S.; Pollitt, C.; DeChiara, T.M.; Kimble, R.B.; Valenzuela, D.M.; Yancopoulos, G.D.; et al. Dominant Mutations in ROR2, Encoding an Orphan Receptor Tyrosine Kinase, Cause Brachydactyly Type B. Nat. Genet. 2000, 24, 275–278. [Google Scholar] [CrossRef]
- Afzal, A.R.; Rajab, A.; Fenske, C.D.; Oldridge, M.; Elanko, N.; Ternes-Pereira, E.; Tüysüz, B.; Murday, V.A.; Patton, M.A.; Wilkie, A.O.; et al. Recessive Robinow Syndrome, Allelic to Dominant Brachydactyly Type B, Is Caused by Mutation of ROR2. Nat. Genet. 2000, 25, 419–422. [Google Scholar] [CrossRef]
- Van Bokhoven, H.; Celli, J.; Kayserili, H.; van Beusekom, E.; Balci, S.; Brussel, W.; Skovby, F.; Kerr, B.; Percin, E.F.; Akarsu, N.; et al. Mutation of the Gene Encoding the ROR2 Tyrosine Kinase Causes Autosomal Recessive Robinow Syndrome. Nat. Genet. 2000, 25, 423–426. [Google Scholar] [CrossRef] [PubMed]
- Masiakowski, P.; Carroll, R.D. A Novel Family of Cell Surface Receptors with Tyrosine Kinase-like Domain. J. Biol. Chem. 1992, 267, 26181–26190. [Google Scholar] [CrossRef]
- Masiakowski, P.; Yancopoulos, G.D. The Wnt Receptor CRD Domain Is Also Found in MuSK and Related Orphan Receptor Tyrosine Kinases. Curr. Biol. 1998, 8, R407. [Google Scholar] [CrossRef]
- Xu, Y.K.; Nusse, R. The Frizzled CRD Domain Is Conserved in Diverse Proteins Including Several Receptor Tyrosine Kinases. Curr. Biol. 1998, 8, R405–R406. [Google Scholar] [CrossRef]
- Yu, J.; Chen, L.; Cui, B.; Widhopf, G.F.; Shen, Z.; Wu, R.; Zhang, L.; Zhang, S.; Briggs, S.P.; Kipps, T.J. Wnt5a Induces ROR1/ROR2 Heterooligomerization to Enhance Leukemia Chemotaxis and Proliferation. J. Clin. Investig. 2016, 126, 585–598. [Google Scholar] [CrossRef]
- Gentile, A.; Lazzari, L.; Benvenuti, S.; Trusolino, L.; Comoglio, P.M. The ROR1 Pseudokinase Diversifies Signaling Outputs in MET-Addicted Cancer Cells. Int. J. Cancer 2014, 135, 2305–2316. [Google Scholar] [CrossRef]
- Gentile, A.; Lazzari, L.; Benvenuti, S.; Trusolino, L.; Comoglio, P.M. Ror1 Is a Pseudokinase that Is Crucial for Met-Driven Tumorigenesis. Cancer Res. 2011, 71, 3132–3141. [Google Scholar] [CrossRef]
- Bicocca, V.T.; Chang, B.H.; Masouleh, B.K.; Muschen, M.; Loriaux, M.M.; Druker, B.J.; Tyner, J.W. Crosstalk between ROR1 and the Pre-B-Cell Receptor Promotes Survival of t(1;19) Acute Lymphoblastic Leukemia. Cancer Cell 2012, 22, 656–667. [Google Scholar] [CrossRef]
- Bainbridge, T.W.; DeAlmeida, V.I.; Izrael-Tomasevic, A.; Chalouni, C.; Pan, B.; Goldsmith, J.; Schoen, A.P.; Quiñones, G.A.; Kelly, R.; Lill, J.R.; et al. Evolutionary Divergence in the Catalytic Activity of the CAM-1, ROR1 and ROR2 Kinase Domains. PLoS ONE 2014, 9, e102695. [Google Scholar] [CrossRef]
- Forrester, W.C. The Ror Receptor Tyrosine Kinase Family. Cell. Mol. Life Sci. CMLS 2002, 59, 83–96. [Google Scholar] [CrossRef]
- Tseng, H.-C.; Lyu, P.-C.; Lin, W. Nuclear Localization of Orphan Receptor Protein Kinase (Ror1) Is Mediated through the Juxtamembrane Domain. BMC Cell Biol. 2010, 11, 48. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Chen, L.; Wang-Rodriguez, J.; Zhang, L.; Cui, B.; Frankel, W.; Wu, R.; Kipps, T.J. The Onco-Embryonic Antigen ROR1 Is Expressed by a Variety of Human Cancers. Am. J. Pathol. 2012, 181, 1903–1910. [Google Scholar] [CrossRef] [PubMed]
- Mei, H.; Lian, S.; Zhang, S.; Wang, W.; Mao, Q.; Wang, H. High Expression of ROR2 in Cancer Cell Correlates with Unfavorable Prognosis in Colorectal Cancer. Biochem. Biophys. Res. Commun. 2014, 453, 703–709. [Google Scholar] [CrossRef] [PubMed]
- Henry, C.; Quadir, A.; Hawkins, N.J.; Jary, E.; Llamosas, E.; Kumar, D.; Daniels, B.; Ward, R.L.; Ford, C.E. Expression of the Novel Wnt Receptor ROR2 Is Increased in Breast Cancer and May Regulate Both β-Catenin Dependent and Independent Wnt Signalling. J. Cancer Res. Clin. Oncol. 2015, 141, 243–254. [Google Scholar] [CrossRef] [PubMed]
- Balakrishnan, A.; Goodpaster, T.; Randolph-Habecker, J.; Hoffstrom, B.G.; Jalikis, F.G.; Koch, L.K.; Berger, C.; Kosasih, P.L.; Rajan, A.; Sommermeyer, D.; et al. Analysis of ROR1 Protein Expression in Human Cancer and Normal Tissues. Clin. Cancer Res. 2017, 23, 3061–3071. [Google Scholar] [CrossRef]
- Carbone, C.; Piro, G.; Gaianigo, N.; Ligorio, F.; Santoro, R.; Merz, V.; Simionato, F.; Zecchetto, C.; Falco, G.; Conti, G.; et al. Adipocytes Sustain Pancreatic Cancer Progression through a Non-Canonical WNT Paracrine Network Inducing ROR2 Nuclear Shuttling. Int. J. Obes. 2018, 42, 334–343. [Google Scholar] [CrossRef] [PubMed]
- Reddy, U.R.; Phatak, S.; Pleasure, D. Human Neural Tissues Express a Truncated Ror1 Receptor Tyrosine Kinase, Lacking Both Extracellular and Transmembrane Domains. Oncogene 1996, 13, 1555–1559. [Google Scholar]
- Kaucká, M.; Krejčí, P.; Plevová, K.; Pavlová, S.; Procházková, J.; Janovská, P.; Valnohová, J.; Kozubík, A.; Pospíšilová, S.; Bryja, V. Post-Translational Modifications Regulate Signalling by Ror1. Acta Physiol. Oxf. Engl. 2011, 203, 351–362. [Google Scholar] [CrossRef]
- Hojjat-Farsangi, M.; Ghaemimanesh, F.; Daneshmanesh, A.H.; Bayat, A.-A.; Mahmoudian, J.; Jeddi-Tehrani, M.; Rabbani, H.; Mellstedt, H. Inhibition of the Receptor Tyrosine Kinase ROR1 by Anti-ROR1 Monoclonal Antibodies and SiRNA Induced Apoptosis of Melanoma Cells. PLoS ONE 2013, 8, e61167. [Google Scholar] [CrossRef]
- Dave, H.; Anver, M.R.; Butcher, D.O.; Brown, P.; Khan, J.; Wayne, A.S.; Baskar, S.; Rader, C. Restricted Cell Surface Expression of Receptor Tyrosine Kinase ROR1 in Pediatric B-Lineage Acute Lymphoblastic Leukemia Suggests Targetability with Therapeutic Monoclonal Antibodies. PLoS ONE 2012, 7, e52655. [Google Scholar] [CrossRef]
- Baskar, S.; Kwong, K.Y.; Hofer, T.; Levy, J.M.; Kennedy, M.G.; Lee, E.; Staudt, L.M.; Wilson, W.H.; Wiestner, A.; Rader, C. Unique Cell Surface Expression of Receptor Tyrosine Kinase ROR1 in Human B-Cell Chronic Lymphocytic Leukemia. Clin. Cancer Res. 2008, 14, 396–404. [Google Scholar] [CrossRef] [PubMed]
- DaneshManesh, A.H.; Mikaelsson, E.; Jeddi-Tehrani, M.; Bayat, A.A.; Ghods, R.; Ostadkarampour, M.; Akhondi, M.; Lagercrantz, S.; Larsson, C.; Österborg, A.; et al. Ror1, a Cell Surface Receptor Tyrosine Kinase Is Expressed in Chronic Lymphocytic Leukemia and May Serve as a Putative Target for Therapy. Int. J. Cancer 2008, 123, 1190–1195. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, T.; Chen, L.; Endo, T.; Tang, L.; Lu, D.; Castro, J.E.; Widhopf, G.F.; Rassenti, L.Z.; Cantwell, M.J.; Prussak, C.E.; et al. Antisera Induced by Infusions of Autologous Ad-CD154-Leukemia B Cells Identify ROR1 as an Oncofetal Antigen and Receptor for Wnt5a. Proc. Natl. Acad. Sci. USA 2008, 105, 3047–3052. [Google Scholar] [CrossRef] [PubMed]
- Klein, U.; Tu, Y.; Stolovitzky, G.A.; Mattioli, M.; Cattoretti, G.; Husson, H.; Freedman, A.; Inghirami, G.; Cro, L.; Baldini, L.; et al. Gene Expression Profiling of B Cell Chronic Lymphocytic Leukemia Reveals a Homogeneous Phenotype Related to Memory B Cells. J. Exp. Med. 2001, 194, 1625–1638. [Google Scholar] [CrossRef]
- Rosenwald, A.; Alizadeh, A.A.; Widhopf, G.; Simon, R.; Davis, R.E.; Yu, X.; Yang, L.; Pickeral, O.K.; Rassenti, L.Z.; Powell, J.; et al. Relation of Gene Expression Phenotype to Immunoglobulin Mutation Genotype in B Cell Chronic Lymphocytic Leukemia. J. Exp. Med. 2001, 194, 1639–1648. [Google Scholar] [CrossRef]
- Cui, B.; Ghia, E.M.; Chen, L.; Rassenti, L.Z.; DeBoever, C.; Widhopf, G.F.; Yu, J.; Neuberg, D.S.; Wierda, W.G.; Rai, K.R.; et al. High-Level ROR1 Associates with Accelerated Disease Progression in Chronic Lymphocytic Leukemia. Blood 2016, 128, 2931–2940. [Google Scholar] [CrossRef]
- Barna, G.; Mihalik, R.; Timár, B.; Tömböl, J.; Csende, Z.; Sebestyén, A.; Bödör, C.; Csernus, B.; Reiniger, L.; Peták, I.; et al. ROR1 Expression Is Not a Unique Marker of CLL. Hematol. Oncol. 2011, 29, 17–21. [Google Scholar] [CrossRef]
- Ghaderi, A.; Daneshmanesh, A.H.; Moshfegh, A.; Kokhaei, P.; Vågberg, J.; Schultz, J.; Olin, T.; Harrysson, S.; Smedby, K.E.; Drakos, E.; et al. ROR1 Is Expressed in Diffuse Large B-Cell Lymphoma (DLBCL) and a Small Molecule Inhibitor of ROR1 (KAN0441571C) Induced Apoptosis of Lymphoma Cells. Biomedicines 2020, 8, 170. [Google Scholar] [CrossRef]
- Hudecek, M.; Schmitt, T.M.; Baskar, S.; Lupo-Stanghellini, M.T.; Nishida, T.; Yamamoto, T.N.; Bleakley, M.; Turtle, C.J.; Chang, W.-C.; Greisman, H.A.; et al. The B-Cell Tumor–Associated Antigen ROR1 Can Be Targeted with T Cells Modified to Express a ROR1-Specific Chimeric Antigen Receptor. Blood 2010, 116, 4532–4541. [Google Scholar] [CrossRef]
- Frenquelli, M.; Caridi, N.; Antonini, E.; Storti, F.; Viganò, V.; Gaviraghi, M.; Occhionorelli, M.; Bianchessi, S.; Bongiovanni, L.; Spinelli, A.; et al. The WNT Receptor ROR2 Drives the Interaction of Multiple Myeloma Cells with the Microenvironment through AKT Activation. Leukemia 2020, 34, 257–270. [Google Scholar] [CrossRef]
- Zhang, S.; Chen, L.; Cui, B.; Chuang, H.-Y.; Yu, J.; Wang-Rodriguez, J.; Tang, L.; Chen, G.; Basak, G.W.; Kipps, T.J. ROR1 Is Expressed in Human Breast Cancer and Associated with Enhanced Tumor-Cell Growth. PLoS ONE 2012, 7, e31127. [Google Scholar] [CrossRef] [PubMed]
- Cui, B.; Zhang, S.; Chen, L.; Yu, J.; Widhopf, G.F.; Fecteau, J.-F.; Rassenti, L.Z.; Kipps, T.J. Targeting ROR1 Inhibits Epithelial–Mesenchymal Transition and Metastasis. Cancer Res. 2013, 73, 3649–3660. [Google Scholar] [CrossRef] [PubMed]
- Chien, H.-P.; Ueng, S.-H.; Chen, S.-C.; Chang, Y.-S.; Lin, Y.-C.; Lo, Y.-F.; Chang, H.-K.; Chuang, W.-Y.; Huang, Y.-T.; Cheung, Y.-C.; et al. Expression of ROR1 Has Prognostic Significance in Triple Negative Breast Cancer. Virchows Arch. 2016, 468, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Guo, M.; Ma, G.; Zhang, X.; Tang, W.; Shi, J.; Wang, Q.; Cheng, Y.; Zhang, B.; Xu, J. ROR2 Knockdown Suppresses Breast Cancer Growth through PI3K/ATK Signaling. Aging 2020, 12, 13115–13127. [Google Scholar] [CrossRef] [PubMed]
- Sun, B.; Ye, X.; Lin, L.; Shen, M.; Jiang, T. Up-Regulation of ROR2 Is Associated with Unfavorable Prognosis and Tumor Progression in Cervical Cancer. Int. J. Clin. Exp. Pathol. 2015, 8, 856–861. [Google Scholar]
- Zhou, J.-K.; Zheng, Y.-Z.; Liu, X.-S.; Gou, Q.; Ma, R.; Guo, C.-L.; Croce, C.M.; Liu, L.; Peng, Y. ROR1 Expression as a Biomarker for Predicting Prognosis in Patients with Colorectal Cancer. Oncotarget 2017, 8, 32864–32872. [Google Scholar] [CrossRef] [PubMed]
- Lara, E.; Calvanese, V.; Huidobro, C.; Fernández, A.F.; Moncada-Pazos, Á.; Obaya, Á.J.; Aguilera, O.; González-Sancho, J.M.; Sánchez, L.; Astudillo, A.; et al. Epigenetic Repression of ROR2 Has a Wnt-Mediated, pro-Tumourigenic Role in Colon Cancer. Mol. Cancer 2010, 9, 170. [Google Scholar] [CrossRef]
- Henry, C.E.; Llamosas, E.; Daniels, B.; Coopes, A.; Tang, K.; Ford, C.E. ROR1 and ROR2 Play Distinct and Opposing Roles in Endometrial Cancer. Gynecol. Oncol. 2018, 148, 576–584. [Google Scholar] [CrossRef]
- Liu, D.; Gunther, K.; Enriquez, L.A.; Daniels, B.; O’Mara, T.A.; Tang, K.; Spurdle, A.B.; Ford, C.E. ROR1 Is Upregulated in Endometrial Cancer and Represents a Novel Therapeutic Target. Sci. Rep. 2020, 10, 1–13. [Google Scholar] [CrossRef]
- Chang, H.; Jung, W.Y.; Kang, Y.; Lee, H.; Kim, A.; Kim, B. Expression of ROR1, PAkt, and PCREB in Gastric Adenocarcinoma. Ann. Diagn. Pathol. 2015, 19, 330–334. [Google Scholar] [CrossRef]
- Tao, J.; Zhi, X.; Zhang, X.; Fu, M.; Huang, H.; Fan, Y.; Guan, W.; Zou, C. MiR-27b-3p Suppresses Cell Proliferation through Targeting Receptor Tyrosine Kinase like Orphan Receptor 1 in Gastric Cancer. J. Exp. Clin. Cancer Res. CR 2015, 34, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Yan, L.; Du, Q.; Yao, J.; Liu, R. ROR2 Inhibits the Proliferation of Gastric Carcinoma Cells via Activation of Non-Canonical Wnt Signaling. Exp. Ther. Med. 2016, 12, 4128–4134. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Hong, M.; Do, I.-G.; Ha, S.Y.; Lee, D.; Suh, Y.-L. Wnt5a, Ryk and Ror2 Expression in Glioblastoma Subgroups. Pathol. Res. Pract. 2015, 211, 963–972. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.-Z.; Ma, R.; Zhou, J.-K.; Guo, C.-L.; Wang, Y.-S.; Li, Z.-G.; Liu, L.-X.; Peng, Y. ROR1 Is a Novel Prognostic Biomarker in Patients with Lung Adenocarcinoma. Sci. Rep. 2016, 6, 36447. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Wang, X.; Zhu, H.; Feng, J.; Ni, S.; Huang, J. Over-Expression of ROR2 and Wnt5a Cooperatively Correlates with Unfavorable Prognosis in Patients with Non-Small Cell Lung Cancer. Oncotarget 2015, 6, 24912–24921. [Google Scholar] [CrossRef]
- Fernández, N.B.; Lorenzo, D.; Picco, M.E.; Barbero, G.; Dergan-Dylon, L.S.; Marks, M.P.; García-Rivello, H.; Gimenez, L.; Labovsky, V.; Grumolato, L.; et al. ROR1 Contributes to Melanoma Cell Growth and Migration by Regulating N-Cadherin Expression via the PI3K/Akt Pathway. Mol. Carcinog. 2016, 55, 1772–1785. [Google Scholar] [CrossRef]
- Saji, T.; Nishita, M.; Ogawa, H.; Doi, T.; Sakai, Y.; Maniwa, Y.; Minami, Y. Critical Role of the Ror-Family of Receptor Tyrosine Kinases in Invasion and Proliferation of Malignant Pleural Mesothelioma Cells. Genes Cells 2018, 23, 606–613. [Google Scholar] [CrossRef]
- Zhang, H.; Qiu, J.; Ye, C.; Yang, D.; Gao, L.; Su, Y.; Tang, X.; Xu, N.; Zhang, D.; Xiong, L.; et al. ROR1 Expression Correlated with Poor Clinical Outcome in Human Ovarian Cancer. Sci. Rep. 2014, 4, 5811. [Google Scholar] [CrossRef]
- Henry, C.; Llamosas, E.; Knipprath-Mészáros, A.; Schoetzau, A.; Obermann, E.; Fuenfschilling, M.; Caduff, R.; Fink, D.; Hacker, N.; Ward, R.; et al. Targeting the ROR1 and ROR2 Receptors in Epithelial Ovarian Cancer Inhibits Cell Migration and Invasion. Oncotarget 2015, 6, 40310–40326. [Google Scholar] [CrossRef]
- Li, R.; Liu, T.; Shi, J.; Luan, W.; Wei, X.; Yu, J.; Mao, H.; Liu, P. ROR2 Induces Cell Apoptosis via Activating IRE1α/JNK/CHOP Pathway in High-Grade Serous Ovarian Carcinoma In Vitro and In Vivo. J. Transl. Med. 2019, 17, 1–17. [Google Scholar] [CrossRef]
- Morioka, K.; Tanikawa, C.; Ochi, K.; Daigo, Y.; Katagiri, T.; Kawano, H.; Kawaguchi, H.; Myoui, A.; Yoshikawa, H.; Naka, N.; et al. Orphan Receptor Tyrosine Kinase ROR2 as a Potential Therapeutic Target for Osteosarcoma. Cancer Sci. 2009, 100, 1227–1233. [Google Scholar] [CrossRef] [PubMed]
- Edris, B.; Espinosa, I.; Mikels, A.; Lee, C.-H.; Steigen, S.E.; Zhu, S.; Montgomery, K.D.; Lazar, A.J.F.; Lev, D.; Fletcher, J.A.; et al. ROR2 Is a Novel Prognostic Biomarker and a Potential Therapeutic Target in Leiomyosarcoma and Gastrointestinal Stromal Tumour. J. Pathol. 2012, 227, 223–233. [Google Scholar] [CrossRef] [PubMed]
- Xu, G.-L.; Shen, J.; Xu, Y.-H.; Wang, W.-S.; Ni, C.-F. ROR1 Is Highly Expressed in Circulating Tumor Cells and Promotes Invasion of Pancreatic Cancer. Mol. Med. Rep. 2018, 18, 5087–5094. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Fan, X.; Wang, X.; Lu, Y.; Zhu, H.; Wang, W.; Zhang, S.; Wang, Z. High ROR2 Expression in Tumor Cells and Stroma Is Correlated with Poor Prognosis in Pancreatic Ductal Adenocarcinoma. Sci. Rep. 2015, 5, 12991. [Google Scholar] [CrossRef]
- Tseng, J.-C.; Huang, S.-H.; Lin, C.-Y.; Wang, B.-J.; Huang, S.-F.; Shen, Y.-Y.; Chuu, C.-P. ROR2 Suppresses Metastasis of Prostate Cancer via Regulation of MiR-199a-5p–PIAS3–AKT2 Signaling Axis. Cell Death Dis. 2020, 11, 1–11. [Google Scholar] [CrossRef]
- Oishi, I.; Takeuchi, S.; Hashimoto, R.; Nagabukuro, A.; Ueda, T.; Liu, Z.-J.; Hatta, T.; Akira, S.; Matsuda, Y.; Yamamura, H.; et al. Spatio-Temporally Regulated Expression of Receptor Tyrosine Kinases, MRor1, MRor2, during Mouse Development: Implications in Development and Function of the Nervous System. Genes Cells 1999, 4, 41–56. [Google Scholar] [CrossRef]
- Al-Shawi, R.; Ashton, S.V.; Underwood, C.; Simons, J.P. Expression of the Ror1 and Ror2 Receptor Tyrosine Kinase Genes during Mouse Development. Dev. Genes Evol. 2001, 211, 161–171. [Google Scholar] [CrossRef]
- Matsuda, T.; Nomi, M.; Ikeya, M.; Kani, S.; Oishi, I.; Terashima, T.; Takada, S.; Minami, Y. Expression of the Receptor Tyrosine Kinase Genes, Ror1 and Ror2, during Mouse Development. Mech. Dev. 2001, 105, 153–156. [Google Scholar] [CrossRef]
- Berger, C.; Sommermeyer, D.; Hudecek, M.; Berger, M.; Balakrishnan, A.; Paszkiewicz, P.J.; Kosasih, P.L.; Rader, C.; Riddell, S.R. Safety of Targeting ROR1 in Primates with Chimeric Antigen Receptor–Modified T Cells. Cancer Immunol. Res. 2015, 3, 206–216. [Google Scholar] [CrossRef]
- Potratz, J.; Tillmanns, A.; Berning, P.; Korsching, E.; Schaefer, C.; Lechtape, B.; Schleithoff, C.; Unland, R.; Schäfer, K.-L.; Müller-Tidow, C.; et al. Receptor Tyrosine Kinase Gene Expression Profiles of Ewing Sarcomas Reveal ROR1 as a Potential Therapeutic Target in Metastatic Disease. Mol. Oncol. 2016, 10, 677–692. [Google Scholar] [CrossRef]
- Broome, H.E.; Rassenti, L.Z.; Wang, H.-Y.; Meyer, L.M.; Kipps, T.J. ROR1 Is Expressed on Hematogones (Non-Neoplastic Human B-Lymphocyte Precursors) and a Minority of Precursor-B Acute Lymphoblastic Leukemia. Leuk. Res. 2011, 35, 1390–1394. [Google Scholar] [CrossRef] [PubMed]
- Daneshmanesh, A.H.; Porwit, A.; Hojjat-Farsangi, M.; Jeddi-Tehrani, M.; Tamm, K.P.; Grandér, D.; Lehmann, S.; Norin, S.; Shokri, F.; Rabbani, H.; et al. Orphan Receptor Tyrosine Kinases ROR1 and ROR2 in Hematological Malignancies. Leuk. Lymphoma 2013, 54, 843–850. [Google Scholar] [CrossRef] [PubMed]
- Billiard, J.; Way, D.S.; Seestaller-Wehr, L.M.; Moran, R.A.; Mangine, A.; Bodine, P.V.N. The Orphan Receptor Tyrosine Kinase Ror2 Modulates Canonical Wnt Signaling in Osteoblastic Cells. Mol. Endocrinol. 2005, 19, 90–101. [Google Scholar] [CrossRef]
- Klemm, F.; Bleckmann, A.; Siam, L.; Chuang, H.N.; Rietkötter, E.; Behme, D.; Schulz, M.; Schaffrinski, M.; Schindler, S.; Trümper, L.; et al. β-Catenin-Independent WNT Signaling in Basal-like Breast Cancer and Brain Metastasis. Carcinogenesis 2011, 32, 434–442. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, T.; Yanagisawa, K.; Sugiyama, R.; Hosono, Y.; Shimada, Y.; Arima, C.; Kato, S.; Tomida, S.; Suzuki, M.; Osada, H.; et al. NKX2-1/TITF1/TTF-1-Induced ROR1 Is Required to Sustain EGFR Survival Signaling in Lung Adenocarcinoma. Cancer Cell 2012, 21, 348–361. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Yang, H.; Chen, T.; Luo, Y.; Xu, Z.; Li, Y.; Yang, J. Silencing of Receptor Tyrosine Kinase ROR1 Inhibits Tumor-Cell Proliferation via PI3K/AKT/MTOR Signaling Pathway in Lung Adenocarcinoma. PLoS ONE 2015, 10, e0127092. [Google Scholar] [CrossRef]
- Ma, S.S.Q.; Henry, C.E.; Llamosas, E.; Higgins, R.; Daniels, B.; Hesson, L.B.; Hawkins, N.J.; Ward, R.L.; Ford, C.E. Validation of Specificity of Antibodies for Immunohistochemistry: The Case of ROR2. Virchows Arch. Int. J. Pathol. 2017, 470, 99–108. [Google Scholar] [CrossRef]
- Dave, H.; Butcher, D.; Anver, M.; Bollard, C.M. ROR1 and ROR2-Novel Targets for Neuroblastoma. Pediatric Hematol. Oncol. 2019, 36, 352–364. [Google Scholar] [CrossRef]
- O’Connell, M.P.; Fiori, J.L.; Xu, M.; Carter, A.D.; Frank, B.P.; Camilli, T.C.; French, A.D.; Dissanayake, S.K.; Indig, F.E.; Bernier, M.; et al. The Orphan Tyrosine Kinase Receptor, ROR2, Mediates Wnt5A Signaling in Metastatic Melanoma. Oncogene 2010, 29, 34–44. [Google Scholar] [CrossRef]
- Xu, J.; Shi, J.; Tang, W.; Jiang, P.; Guo, M.; Zhang, B.; Ma, G. ROR2 Promotes the Epithelial-Mesenchymal Transition by Regulating MAPK/P38 Signaling Pathway in Breast Cancer. J. Cell. Biochem. 2020, 121, 4142–4153. [Google Scholar] [CrossRef]
- Henry, C.; Emmanuel, C.; Lambie, N.; Loo, C.; Kan, B.; Kennedy, C.; de Fazio, A.; Hacker, N.; Ford, C. Distinct Patterns of Stromal and Tumor Expression of ROR1 and ROR2 in Histological Subtypes of Epithelial Ovarian Cancer. Transl. Oncol. 2017, 10, 346–356. [Google Scholar] [CrossRef] [PubMed]
- Endo, M.; Ubulkasim, G.; Kobayashi, C.; Onishi, R.; Aiba, A.; Minami, Y. Critical Role of Ror2 Receptor Tyrosine Kinase in Regulating Cell Cycle Progression of Reactive Astrocytes Following Brain Injury. Glia 2017, 65, 182–197. [Google Scholar] [CrossRef] [PubMed]
- Kamizaki, K.; Doi, R.; Hayashi, M.; Saji, T.; Kanagawa, M.; Toda, T.; Fukada, S.; Ho, H.-Y.H.; Greenberg, M.E.; Endo, M.; et al. The Ror1 Receptor Tyrosine Kinase Plays a Critical Role in Regulating Satellite Cell Proliferation during Regeneration of Injured Muscle. J. Biol. Chem. 2017, 292, 15939–15951. [Google Scholar] [CrossRef] [PubMed]
- MacKeigan, J.P.; Murphy, L.O.; Blenis, J. Sensitized RNAi Screen of Human Kinases and Phosphatases Identifies New Regulators of Apoptosis and Chemoresistance. Nat. Cell Biol. 2005, 7, 591–600. [Google Scholar] [CrossRef] [PubMed]
- Widhopf, G.F.; Cui, B.; Ghia, E.M.; Chen, L.; Messer, K.; Shen, Z.; Briggs, S.P.; Croce, C.M.; Kipps, T.J. ROR1 Can Interact with TCL1 and Enhance Leukemogenesis in Eµ-TCL1 Transgenic Mice. Proc. Natl. Acad. Sci. USA 2014, 111, 793–798. [Google Scholar] [CrossRef] [PubMed]
- Balatti, V.; Croce, C.M. MicroRNA Dysregulation and Multi-Targeted Therapy for Cancer Treatment. Adv. Biol. Regul. 2020, 75, 100669. [Google Scholar] [CrossRef]
- Zhou, Q.; Zhou, S.; Wang, H.; Li, Y.; Xiao, X.; Yang, J. Stable Silencing of ROR1 Regulates Cell Cycle, Apoptosis, and Autophagy in a Lung Adenocarcinoma Cell Line. Int. J. Clin. Exp. Pathol. 2020, 13, 1108–1120. [Google Scholar]
- Fultang, N.; Illendula, A.; Lin, J.; Pandey, M.K.; Klase, Z.; Peethambaran, B. ROR1 Regulates Chemoresistance in Breast Cancer via Modulation of Drug Efflux Pump ABCB1. Sci. Rep. 2020, 10, 1–12. [Google Scholar] [CrossRef]
- Wright, T.M.; Brannon, A.R.; Gordan, J.D.; Mikels, A.J.; Mitchell, C.; Chen, S.; Espinosa, I.; van de Rijn, M.; Pruthi, R.; Wallen, E.; et al. Ror2, a Developmentally Regulated Kinase, Promotes Tumor Growth Potential in Renal Cell Carcinoma. Oncogene 2009, 28, 2513–2523. [Google Scholar] [CrossRef]
- Yang, C.-M.; Ji, S.; Li, Y.; Fu, L.-Y.; Jiang, T.; Meng, F.-D. Ror2, a Developmentally Regulated Kinase, Is Associated With Tumor Growth, Apoptosis, Migration, and Invasion in Renal Cell Carcinoma. Oncol. Res. 2017, 25, 195–205. [Google Scholar] [CrossRef]
- Roarty, K.; Pfefferle, A.D.; Creighton, C.J.; Perou, C.M.; Rosen, J.M. Ror2-Mediated Alternative Wnt Signaling Regulates Cell Fate and Adhesion during Mammary Tumor Progression. Oncogene 2017, 36, 5958–5968. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Shi, Y.; Li, H.; Tan, D.; Yang, M.; Wu, X. Knockdown of Receptor Tyrosine Kinase-like Orphan Receptor 2 Inhibits Cell Proliferation and Colony Formation in Osteosarcoma Cells by Inducing Arrest in Cell Cycle Progression. Oncol. Lett. 2015, 10, 3705–3711. [Google Scholar] [CrossRef][Green Version]
- Endo, M.; Tanaka, Y.; Otsuka, M.; Minami, Y. E2F1-Ror2 Signaling Mediates Coordinated Transcriptional Regulation to Promote G1/S Phase Transition in BFGF-Stimulated NIH/3T3 Fibroblasts. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2020, 34, 3413–3428. [Google Scholar] [CrossRef] [PubMed]
- Nishita, M.; Yoo, S.K.; Nomachi, A.; Kani, S.; Sougawa, N.; Ohta, Y.; Takada, S.; Kikuchi, A.; Minami, Y. Filopodia Formation Mediated by Receptor Tyrosine Kinase Ror2 Is Required for Wnt5a-Induced Cell Migration. J. Cell Biol. 2006, 175, 555–562. [Google Scholar] [CrossRef] [PubMed]
- Mattes, B.; Dang, Y.; Greicius, G.; Kaufmann, L.T.; Prunsche, B.; Rosenbauer, J.; Stegmaier, J.; Mikut, R.; Özbek, S.; Nienhaus, G.U.; et al. Wnt/PCP Controls Spreading of Wnt/β-Catenin Signals by Cytonemes in Vertebrates. eLife 2018, 7, e36953. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, T.; Lu, C.; Ida, L.; Yanagisawa, K.; Usukura, J.; Cheng, J.; Hotta, N.; Shimada, Y.; Isomura, H.; Suzuki, M.; et al. ROR1 Sustains Caveolae and Survival Signalling as a Scaffold of Cavin-1 and Caveolin-1. Nat. Commun. 2016, 7, 10060. [Google Scholar] [CrossRef]
- Yamaguchi, T.; Hayashi, M.; Ida, L.; Yamamoto, M.; Lu, C.; Kajino, T.; Cheng, J.; Nakatochi, M.; Isomura, H.; Yamazaki, M.; et al. ROR1-CAVIN3 Interaction Required for Caveolae-Dependent Endocytosis and pro-Survival Signaling in Lung Adenocarcinoma. Oncogene 2019, 38, 5142–5157. [Google Scholar] [CrossRef]
- Wang, H.-L.; Liu, Y.-C.; Long, M.-P.; Zheng, C.; Yang, J.-H. Blocking ROR1 Enhances the Roles of Erlotinib in Lung Adenocarcinoma Cell Lines. Oncol. Lett. 2019, 18, 2977–2984. [Google Scholar] [CrossRef]
- Henry, C.E.; Llamosas, E.; Djordjevic, A.; Hacker, N.F.; Ford, C.E. Migration and Invasion Is Inhibited by Silencing ROR1 and ROR2 in Chemoresistant Ovarian Cancer. Oncogenesis 2016, 5, e226. [Google Scholar] [CrossRef]
- Islam, S.S.; Uddin, M.; Noman, A.S.M.; Akter, H.; Dity, N.J.; Basiruzzman, M.; Uddin, F.; Ahsan, J.; Annoor, S.; Alaiya, A.A.; et al. Antibody-Drug Conjugate T-DM1 Treatment for HER2+ Breast Cancer Induces ROR1 and Confers Resistance through Activation of Hippo Transcriptional Coactivator YAP1. EBioMedicine 2019, 43, 211–224. [Google Scholar] [CrossRef]
- Veskimäe, K.; Scaravilli, M.; Niininen, W.; Karvonen, H.; Jaatinen, S.; Nykter, M.; Visakorpi, T.; Mäenpää, J.; Ungureanu, D.; Staff, S. Expression Analysis of Platinum Sensitive and Resistant Epithelial Ovarian Cancer Patient Samples Reveals New Candidates for Targeted Therapies. Transl. Oncol. 2018, 11, 1160–1170. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Zhang, H.; Ghia, E.M.; Huang, J.; Wu, L.; Zhang, J.; Lam, S.; Lei, Y.; He, J.; Cui, B.; et al. Inhibition of Chemotherapy Resistant Breast Cancer Stem Cells by a ROR1 Specific Antibody. Proc. Natl. Acad. Sci. USA 2019, 116, 1370–1377. [Google Scholar] [CrossRef] [PubMed]
- O’Connell, M.P.; Marchbank, K.; Webster, M.R.; Valiga, A.A.; Kaur, A.; Vultur, A.; Li, L.; Herlyn, M.; Villanueva, J.; Liu, Q.; et al. Hypoxia Induces Phenotypic Plasticity and Therapy Resistance in Melanoma via the Tyrosine Kinase Receptors ROR1 and ROR2. Cancer Discov. 2013, 3, 1378–1393. [Google Scholar] [CrossRef] [PubMed]
- Faião-Flores, F.; Emmons, M.F.; Durante, M.A.; Kinose, F.; Saha, B.; Fang, B.; Koomen, J.M.; Chellappan, S.; Maria-Engler, S.S.; Rix, U.; et al. HDAC Inhibition Enhances the in Vivo Efficacy of MEK Inhibitor Therapy in Uveal Melanoma. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2019, 25, 5686–5701. [Google Scholar] [CrossRef] [PubMed]
- Karvonen, H.; Perttilä, R.; Niininen, W.; Hautanen, V.; Barker, H.; Murumägi, A.; Heckman, C.A.; Ungureanu, D. Wnt5a and ROR1 Activate Non-Canonical Wnt Signaling via RhoA in TCF3-PBX1 Acute Lymphoblastic Leukemia and Highlight New Treatment Strategies via Bcl-2 Co-Targeting. Oncogene 2019, 38, 3288–3300. [Google Scholar] [CrossRef] [PubMed]
- Karvonen, H.; Chiron, D.; Niininen, W.; Ek, S.; Jerkeman, M.; Moradi, E.; Nykter, M.; Heckman, C.A.; Kallioniemi, O.; Murumägi, A.; et al. Crosstalk between ROR1 and BCR Pathways Defines Novel Treatment Strategies in Mantle Cell Lymphoma. Blood Adv. 2017, 1, 2257–2268. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Wang, H.Y.; Liu, X.; Nunez-Cruz, S.; Jillab, M.; Melnikov, O.; Nath, K.; Glickson, J.; Wasik, M.A. Cutting Edge: ROR1/CD19 Receptor Complex Promotes Growth of Mantle Cell Lymphoma Cells Independently of the B Cell Receptor–BTK Signaling Pathway. J. Immunol. 2019, 203, 2043–2048. [Google Scholar] [CrossRef]
- Yu, J.; Chen, L.; Cui, B.; Wu, C.; Choi, M.Y.; Chen, Y.; Zhang, L.; Rassenti, L.Z.; Widhopf II, G.F.; Kipps, T.J. Cirmtuzumab Inhibits Wnt5a-Induced Rac1 Activation in Chronic Lymphocytic Leukemia Treated with Ibrutinib. Leukemia 2017, 31, 1333–1339. [Google Scholar] [CrossRef]
- Obradović, M.M.S.; Hamelin, B.; Manevski, N.; Couto, J.P.; Sethi, A.; Coissieux, M.-M.; Münst, S.; Okamoto, R.; Kohler, H.; Schmidt, A.; et al. Glucocorticoids Promote Breast Cancer Metastasis. Nature 2019, 567, 540–544. [Google Scholar] [CrossRef]
- Karvonen, H.; Barker, H.; Kaleva, L.; Niininen, W.; Ungureanu, D. Molecular Mechanisms Associated with ROR1-Mediated Drug Resistance: Crosstalk with Hippo-YAP/TAZ and BMI-1 Pathways. Cells 2019, 8, 812. [Google Scholar] [CrossRef]
- Zhang, S.; Cui, B.; Lai, H.; Liu, G.; Ghia, E.M.; Widhopf, G.F.; Zhang, Z.; Wu, C.C.N.; Chen, L.; Wu, R.; et al. Ovarian Cancer Stem Cells Express ROR1, Which Can Be Targeted for Anti–Cancer-Stem-Cell Therapy. Proc. Natl. Acad. Sci. USA 2014, 111, 17266–17271. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.Y.; Widhopf, G.F.; Ghia, E.M.; Kidwell, R.L.; Hasan, M.K.; Yu, J.; Rassenti, L.Z.; Chen, L.; Chen, Y.; Pittman, E.; et al. Phase I Trial: Cirmtuzumab Inhibits ROR1 Signaling and Stemness Signatures in Patients with Chronic Lymphocytic Leukemia. Cell Stem Cell 2018, 22, 951–959.e3. [Google Scholar] [CrossRef] [PubMed]
- Jung, E.-H.; Lee, H.-N.; Han, G.-Y.; Kim, M.-J.; Kim, C.-W. Targeting ROR1 Inhibits the Self-Renewal and Invasive Ability of Glioblastoma Stem Cells. Cell Biochem. Funct. 2016, 34, 149–157. [Google Scholar] [CrossRef]
- Bleckmann, A.; Conradi, L.-C.; Menck, K.; Schmick, N.A.; Schubert, A.; Rietkötter, E.; Arackal, J.; Middel, P.; Schambony, A.; Liersch, T.; et al. β-Catenin-Independent WNT Signaling and Ki67 in Contrast to the Estrogen Receptor Status Are Prognostic and Associated with Poor Prognosis in Breast Cancer Liver Metastases. Clin. Exp. Metastasis 2016, 33, 309–323. [Google Scholar] [CrossRef]
- Nomachi, A.; Nishita, M.; Inaba, D.; Enomoto, M.; Hamasaki, M.; Minami, Y. Receptor Tyrosine Kinase Ror2 Mediates Wnt5a-Induced Polarized Cell Migration by Activating c-Jun N-Terminal Kinase via Actin-Binding Protein Filamin A. J. Biol. Chem. 2008, 283, 27973–27981. [Google Scholar] [CrossRef] [PubMed]
- Arabzadeh, S.; Hossein, G.; Salehi-Dulabi, Z.; Zarnani, A.H. WNT5A–ROR2 Is Induced by Inflammatory Mediators and Is Involved in the Migration of Human Ovarian Cancer Cell Line SKOV-3. Cell. Mol. Biol. Lett. 2016, 21, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Ma, Y.-H.; Pang, Y.-X.; Zhao, Z.; Lu, J.-J.; Mao, H.-L.; Liu, P.-S. Ectopic Repression of Receptor Tyrosine Kinase–like Orphan Receptor 2 Inhibits Malignant Transformation of Ovarian Cancer Cells by Reversing Epithelial–Mesenchymal Transition. Tumor Biol. 2017, 39, 1010428317701627. [Google Scholar] [CrossRef]
- Yamamoto, H.; Oue, N.; Sato, A.; Hasegawa, Y.; Yamamoto, H.; Matsubara, A.; Yasui, W.; Kikuchi, A. Wnt5a Signaling Is Involved in the Aggressiveness of Prostate Cancer and Expression of Metalloproteinase. Oncogene 2010, 29, 2036–2046. [Google Scholar] [CrossRef]
- Cao, J.; Wang, X.; Dai, T.; Wu, Y.; Zhang, M.; Cao, R.; Zhang, R.; Wang, G.; Jiang, R.; Zhou, B.P.; et al. Twist Promotes Tumor Metastasis in Basal-like Breast Cancer by Transcriptionally Upregulating ROR1. Theranostics 2018, 8, 2739–2751. [Google Scholar] [CrossRef]
- Ren, D.; Minami, Y.; Nishita, M. Critical Role of Wnt5a–Ror2 Signaling in Motility and Invasiveness of Carcinoma Cells Following Snail-Mediated Epithelial–Mesenchymal Transition. Genes Cells 2011, 16, 304–315. [Google Scholar] [CrossRef]
- Enomoto, M.; Hayakawa, S.; Itsukushima, S.; Ren, D.Y.; Matsuo, M.; Tamada, K.; Oneyama, C.; Okada, M.; Takumi, T.; Nishita, M.; et al. Autonomous Regulation of Osteosarcoma Cell Invasiveness by Wnt5a/Ror2 Signaling. Oncogene 2009, 28, 3197–3208. [Google Scholar] [CrossRef] [PubMed]
- Nishita, M.; Park, S.-Y.; Nishio, T.; Kamizaki, K.; Wang, Z.; Tamada, K.; Takumi, T.; Hashimoto, R.; Otani, H.; Pazour, G.J.; et al. Ror2 Signaling Regulates Golgi Structure and Transport through IFT20 for Tumor Invasiveness. Sci. Rep. 2017, 7, 1. [Google Scholar] [CrossRef] [PubMed]
- Susman, M.W.; Karuna, E.P.; Kunz, R.C.; Gujral, T.S.; Cantú, A.V.; Choi, S.S.; Jong, B.Y.; Okada, K.; Scales, M.K.; Hum, J.; et al. Kinesin Superfamily Protein Kif26b Links Wnt5a-Ror Signaling to the Control of Cell and Tissue Behaviors in Vertebrates. eLife 2017, 6, e26509. [Google Scholar] [CrossRef] [PubMed]
- Cetin, M.; Odabas, G.; Douglas, L.R.; Duriez, P.J.; Balcik-Ercin, P.; Yalim-Camci, I.; Sayan, A.E.; Yagci, T. ROR1 Expression and Its Functional Significance in Hepatocellular Carcinoma Cells. Cells 2019, 8, 210. [Google Scholar] [CrossRef] [PubMed]
- Ren, D.; Dai, Y.; Yang, Q.; Zhang, X.; Guo, W.; Ye, L.; Huang, S.; Chen, X.; Lai, Y.; Du, H.; et al. Wnt5a Induces and Maintains Prostate Cancer Cells Dormancy in Bone. J. Exp. Med. 2019, 216, 428–449. [Google Scholar] [CrossRef]
- Ma, S.S.Q.; Srivastava, S.; Llamosas, E.; Hawkins, N.J.; Hesson, L.B.; Ward, R.L.; Ford, C.E. ROR2 Is Epigenetically Inactivated in the Early Stages of Colorectal Neoplasia and Is Associated with Proliferation and Migration. BMC Cancer 2016, 16, 508. [Google Scholar] [CrossRef] [PubMed]
- Oishi, I.; Suzuki, H.; Onishi, N.; Takada, R.; Kani, S.; Ohkawara, B.; Koshida, I.; Suzuki, K.; Yamada, G.; Schwabe, G.C.; et al. The Receptor Tyrosine Kinase Ror2 Is Involved in Non-Canonical Wnt5a/JNK Signalling Pathway. Genes Cells Devoted Mol. Cell. Mech. 2003, 8, 645–654. [Google Scholar] [CrossRef]
- Janovska, P.; Poppova, L.; Plevova, K.; Plesingerova, H.; Behal, M.; Kaucka, M.; Ovesna, P.; Hlozkova, M.; Borsky, M.; Stehlikova, O.; et al. Autocrine Signaling by Wnt-5a Deregulates Chemotaxis of Leukemic Cells and Predicts Clinical Outcome in Chronic Lymphocytic Leukemia. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2016, 22, 459–469. [Google Scholar] [CrossRef]
- Menck, K.; Heinrichs, S.; Wlochowitz, D.; Sitte, M.; Noeding, H.; Janshoff, A.; Treiber, H.; Ruhwedel, T.; Schatlo, B.; von der Brelie, C.; et al. WNT11 Is a Novel Ligand for ROR2 in Human Breast Cancer. bioRxiv 2020. [Google Scholar] [CrossRef]
- Akbarzadeh, S.; Wheldon, L.M.; Sweet, S.M.M.; Talma, S.; Mardakheh, F.K.; Heath, J.K. The Deleted in Brachydactyly B Domain of ROR2 Is Required for Receptor Activation by Recruitment of Src. PLoS ONE 2008, 3, e1873. [Google Scholar] [CrossRef]
- Mikels, A.; Minami, Y.; Nusse, R. Ror2 Receptor Requires Tyrosine Kinase Activity to Mediate Wnt5A Signaling. J. Biol. Chem. 2009, 284, 30167–30176. [Google Scholar] [CrossRef] [PubMed]
- Grumolato, L.; Liu, G.; Mong, P.; Mudbhary, R.; Biswas, R.; Arroyave, R.; Vijayakumar, S.; Economides, A.N.; Aaronson, S.A. Canonical and Noncanonical Wnts Use a Common Mechanism to Activate Completely Unrelated Coreceptors. Genes Dev. 2010, 24, 2517–2530. [Google Scholar] [CrossRef] [PubMed]
- Sitte, M.; Menck, K.; Wachter, A.; Reinz, E.; Korf, U.; Wiemann, S.; Bleckmann, A.; Beissbarth, T. Reconstruction of Different Modes of WNT Dependent Protein Networks from Time Series Protein Quantification. Stud. Health Technol. Inform. 2019, 267, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Harris, D.; Liu, Z.; Liu, J.; Keating, M.; Estrov, Z. Stat3 Activates the Receptor Tyrosine Kinase Like Orphan Receptor-1 Gene in Chronic Lymphocytic Leukemia Cells. PLoS ONE 2010, 5, e11859. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Y.; Niu, C.C.; Deng, G.; Li, Z.Q.; Pan, J.; Zhao, C.; Yang, Z.L.; Si, W.K. The Wnt5a/Ror2 Noncanonical Signaling Pathway Inhibits Canonical Wnt Signaling in K562 Cells. Int. J. Mol. Med. 2011, 27, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Ross, J.F.; Bodine, P.V.N.; Billiard, J. Homodimerization of Ror2 Tyrosine Kinase Receptor Induces 14-3-3β Phosphorylation and Promotes Osteoblast Differentiation and Bone Formation. Mol. Endocrinol. 2007, 21, 3050–3061. [Google Scholar] [CrossRef]
- Wu, X.; Yan, T.; Hao, L.; Zhu, Y. Wnt5a Induces ROR1 and ROR2 to Activate RhoA in Esophageal Squamous Cell Carcinoma Cells. Cancer Manag. Res. 2019, 11, 2803–2815. [Google Scholar] [CrossRef]
- Nishita, M.; Itsukushima, S.; Nomachi, A.; Endo, M.; Wang, Z.; Inaba, D.; Qiao, S.; Takada, S.; Kikuchi, A.; Minami, Y. Ror2/Frizzled Complex Mediates Wnt5a-Induced AP-1 Activation by Regulating Dishevelled Polymerization. Mol. Cell. Biol. 2010, 30, 3610–3619. [Google Scholar] [CrossRef]
- Lee, J.G.; Heur, M. Interleukin-1β-Induced Wnt5a Enhances Human Corneal Endothelial Cell Migration through Regulation of Cdc42 and RhoA. Mol. Cell. Biol. 2014, 34, 3535–3545. [Google Scholar] [CrossRef]
- Martinez, S.; Scerbo, P.; Giordano, M.; Daulat, A.M.; Lhoumeau, A.-C.; Thomé, V.; Kodjabachian, L.; Borg, J.-P. The PTK7 and ROR2 Protein Receptors Interact in the Vertebrate WNT/Planar Cell Polarity (PCP) Pathway. J. Biol. Chem. 2015, 290, 30562–30572. [Google Scholar] [CrossRef]
- Sheetz, J.B.; Mathea, S.; Karvonen, H.; Malhotra, K.; Chatterjee, D.; Niininen, W.; Perttilä, R.; Preuss, F.; Suresh, K.; Stayrook, S.E.; et al. Structural Insights into Pseudokinase Domains of Receptor Tyrosine Kinases. Mol. Cell 2020, 79, 390–405.e7. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, H.; Yoo, S.K.; Nishita, M.; Kikuchi, A.; Minami, Y. Wnt5a Modulates Glycogen Synthase Kinase 3 to Induce Phosphorylation of Receptor Tyrosine Kinase Ror2. Genes Cells Devoted Mol. Cell. Mech. 2007, 12, 1215–1223. [Google Scholar] [CrossRef] [PubMed]
- Curto, J.; Del Valle-Pérez, B.; Villarroel, A.; Fuertes, G.; Vinyoles, M.; Peña, R.; García de Herreros, A.; Duñach, M. CK1ε and P120-Catenin Control Ror2 Function in Noncanonical Wnt Signaling. Mol. Oncol. 2018, 12, 611–629. [Google Scholar] [CrossRef]
- Kani, S.; Oishi, I.; Yamamoto, H.; Yoda, A.; Suzuki, H.; Nomachi, A.; Iozumi, K.; Nishita, M.; Kikuchi, A.; Takumi, T.; et al. The Receptor Tyrosine Kinase Ror2 Associates with and Is Activated by Casein Kinase Iϵ. J. Biol. Chem. 2004, 279, 50102–50109. [Google Scholar] [CrossRef] [PubMed]
- Kaucká, M.; Plevová, K.; Pavlová, Š.; Janovská, P.; Mishra, A.; Verner, J.; Procházková, J.; Krejčí, P.; Kotašková, J.; Ovesná, P.; et al. The Planar Cell Polarity Pathway Drives Pathogenesis of Chronic Lymphocytic Leukemia by the Regulation of B-Lymphocyte Migration. Cancer Res. 2013, 73, 1491–1501. [Google Scholar] [CrossRef]
- Sharma, M.; Castro-Piedras, I.; Simmons, G.E.; Pruitt, K. Dishevelled: A Masterful Conductor of Complex Wnt Signals. Cell. Signal. 2018, 47, 52–64. [Google Scholar] [CrossRef]
- Zhu, Y.; Tian, Y.; Du, J.; Hu, Z.; Yang, L.; Liu, J.; Gu, L. Dvl2-Dependent Activation of Daam1 and RhoA Regulates Wnt5a-Induced Breast Cancer Cell Migration. PLoS ONE 2012, 7, e37823. [Google Scholar] [CrossRef]
- Hasan, M.K.; Yu, J.; Chen, L.; Cui, B.; Widhopf II, G.F.; Rassenti, L.; Shen, Z.; Briggs, S.P.; Kipps, T.J. Wnt5a Induces ROR1 to Complex with HS1 to Enhance Migration of Chronic Lymphocytic Leukemia Cells. Leukemia 2017, 31, 2615–2622. [Google Scholar] [CrossRef]
- Hasan, M.K.; Yu, J.; Widhopf, G.F.; Rassenti, L.Z.; Chen, L.; Shen, Z.; Briggs, S.P.; Neuberg, D.S.; Kipps, T.J. Wnt5a Induces ROR1 to Recruit DOCK2 to Activate Rac1/2 in Chronic Lymphocytic Leukemia. Blood 2018, 132, 170–178. [Google Scholar] [CrossRef]
- Hasan, M.K.; Widhopf, G.F.; Zhang, S.; Lam, S.M.; Shen, Z.; Briggs, S.P.; Parker, B.A.; Kipps, T.J. Wnt5a Induces ROR1 to Recruit Cortactin to Promote Breast-Cancer Migration and Metastasis. NPJ Breast Cancer 2019, 5, 1–11. [Google Scholar] [CrossRef]
- Witte, F.; Bernatik, O.; Kirchner, K.; Masek, J.; Mahl, A.; Krejci, P.; Mundlos, S.; Schambony, A.; Bryja, V.; Stricker, S. Negative Regulation of Wnt Signaling Mediated by CK1-Phosphorylated Dishevelled via Ror2. FASEB J. 2010, 24, 2417–2426. [Google Scholar] [CrossRef] [PubMed]
- Bayerlová, M.; Klemm, F.; Kramer, F.; Pukrop, T.; Beißbarth, T.; Bleckmann, A. Newly Constructed Network Models of Different WNT Signaling Cascades Applied to Breast Cancer Expression Data. PLoS ONE 2015, 10, e0144014. [Google Scholar] [CrossRef]
- Bayerlová, M.; Menck, K.; Klemm, F.; Wolff, A.; Pukrop, T.; Binder, C.; Beißbarth, T.; Bleckmann, A. Ror2 Signaling and Its Relevance in Breast Cancer Progression. Front. Oncol. 2017, 7, 135. [Google Scholar] [CrossRef]
- Voloshanenko, O.; Schwartz, U.; Kranz, D.; Rauscher, B.; Linnebacher, M.; Augustin, I.; Boutros, M. β-Catenin-Independent Regulation of Wnt Target Genes by RoR2 and ATF2/ATF4 in Colon Cancer Cells. Sci. Rep. 2018, 8, 1–14. [Google Scholar] [CrossRef]
- Flores-Hernández, E.; Velázquez, D.M.; Castañeda-Patlán, M.C.; Fuentes-García, G.; Fonseca-Camarillo, G.; Yamamoto-Furusho, J.K.; Romero-Avila, M.T.; García-Sáinz, J.A.; Robles-Flores, M. Canonical and Non-Canonical Wnt Signaling Are Simultaneously Activated by Wnts in Colon Cancer Cells. Cell. Signal. 2020, 72, 109636. [Google Scholar] [CrossRef]
- Li, C.; Chen, H.; Hu, L.; Xing, Y.; Sasaki, T.; Villosis, M.F.; Li, J.; Nishita, M.; Minami, Y.; Minoo, P. Ror2 Modulates the Canonical Wnt Signaling in Lung Epithelial Cells through Cooperation with Fzd2. BMC Mol. Biol. 2008, 9, 11. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, N.R.; Wright, T.M.; Brooks, S.A.; Hacker, K.E.; Debebe, Z.; Sendor, A.B.; Walker, M.P.; Major, M.B.; Green, J.; Wahl, G.M.; et al. Receptor Tyrosine Kinase-like Orphan Receptor 2 (Ror2) Expression Creates a Poised State of Wnt Signaling in Renal Cancer. J. Biol. Chem. 2013, 288, 26301–26310. [Google Scholar] [CrossRef]
- Daneshmanesh, A.H.; Hojjat-Farsangi, M.; Moshfegh, A.; Khan, A.S.; Mikaelsson, E.; Österborg, A.; Mellstedt, H. The PI3K/AKT/MTOR Pathway Is Involved in Direct Apoptosis of CLL Cells Induced by ROR1 Monoclonal Antibodies. Br. J. Haematol. 2015, 169, 455–458. [Google Scholar] [CrossRef] [PubMed]
- Dai, B.; Yan, T.; Zhang, A. ROR2 Receptor Promotes the Migration of Osteosarcoma Cells in Response to Wnt5a. Cancer Cell Int. 2017, 17, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Lopez, E.; Ghia, E.M.; Antonucci, L.; Sharma, N.; Rassenti, L.Z.; Xu, J.; Sun, B.; Kipps, T.J.; Karin, M. NF-ΚB-P62-NRF2 Survival Signaling Is Associated with High ROR1 Expression in Chronic Lymphocytic Leukemia. Cell Death Differ. 2020, 27, 2206–2216. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Chen, L.; Chen, Y.; Hasan, M.K.; Ghia, E.M.; Zhang, L.; Wu, R.; Rassenti, L.Z.; Widhopf, G.F.; Shen, Z.; et al. Wnt5a Induces ROR1 to Associate with 14-3-3ζ for Enhanced Chemotaxis and Proliferation of Chronic Lymphocytic Leukemia Cells. Leukemia 2017, 31, 2608–2614. [Google Scholar] [CrossRef] [PubMed]
- Neal, C.L.; Xu, J.; Li, P.; Mori, S.; Yang, J.; Neal, N.N.; Zhou, X.; Wyszomierski, S.L.; Yu, D. Overexpression of 14-3-3ζ in Cancer Cells Activates PI3K via Binding the P85 Regulatory Subunit. Oncogene 2012, 31, 897–906. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.; Lv, P.; Sun, Z.; Han, L.; Zhou, W. 14-3-3β Promotes Migration and Invasion of Human Hepatocellular Carcinoma Cells by Modulating Expression of MMP2 and MMP9 through PI3K/Akt/NF-ΚB Pathway. PLoS ONE 2016, 11, e0146070. [Google Scholar] [CrossRef] [PubMed]
- Karimi Roshan, M.; Soltani, A.; Soleimani, A.; Rezaie Kahkhaie, K.; Afshari, A.R.; Soukhtanloo, M. Role of AKT and MTOR Signaling Pathways in the Induction of Epithelial-Mesenchymal Transition (EMT) Process. Biochimie 2019, 165, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Farhan, M.; Wang, H.; Gaur, U.; Little, P.J.; Xu, J.; Zheng, W. FOXO Signaling Pathways as Therapeutic Targets in Cancer. Int. J. Biol. Sci. 2017, 13, 815–827. [Google Scholar] [CrossRef] [PubMed]
- Ida, L.; Yamaguchi, T.; Yanagisawa, K.; Kajino, T.; Shimada, Y.; Suzuki, M.; Takahashi, T. Receptor Tyrosine Kinase-like Orphan Receptor 1, a Target of NKX2-1/TTF-1 Lineage-survival Oncogene, Inhibits Apoptosis Signal-regulating Kinase 1-mediated Pro-apoptotic Signaling in Lung Adenocarcinoma. Cancer Sci. 2016, 107, 155–161. [Google Scholar] [CrossRef]
- Karvonen, H.; Arjama, M.; Kaleva, L.; Niininen, W.; Barker, H.; Koivisto-Korander, R.; Tapper, J.; Pakarinen, P.; Lassus, H.; Loukovaara, M.; et al. Glucocorticoids Induce Differentiation and Chemoresistance in Ovarian Cancer by Promoting ROR1-Mediated Stemness. Cell Death Dis. 2020, 11, 790. [Google Scholar] [CrossRef]
- Hasan, M.K.; Ghia, E.M.; Rassenti, L.Z.; Widhopf, G.F.; Kipps, T.J. Wnt5a Enhances Proliferation of Chronic Lymphocytic Leukemia and ERK1/2 Phosphorylation via a ROR1/DOCK2-Dependent Mechanism. Leukemia 2020, 1–10. [Google Scholar] [CrossRef]
- Villarroel, A.; Del Valle-Pérez, B.; Fuertes, G.; Curto, J.; Ontiveros, N.; Garcia de Herreros, A.; Duñach, M. Src and Fyn Define a New Signaling Cascade Activated by Canonical and Non-Canonical Wnt Ligands and Required for Gene Transcription and Cell Invasion. Cell. Mol. Life Sci. 2020, 77, 919–935. [Google Scholar] [CrossRef]
- Chen, Y.; Chen, L.; Yu, J.; Ghia, E.M.; Choi, M.Y.; Zhang, L.; Zhang, S.; Sanchez-Lopez, E.; Widhopf, G.F.; Messer, K.; et al. Cirmtuzumab Blocks Wnt5a/ROR1 Stimulation of NF-ΚB to Repress Autocrine STAT3 Activation in Chronic Lymphocytic Leukemia. Blood 2019, 134, 1084–1094. [Google Scholar] [CrossRef]
- Tseng, H.-C.; Kao, H.-W.; Ho, M.-R.; Chen, Y.-R.; Lin, T.-W.; Lyu, P.-C.; Lin, W.-C. Cytoskeleton Network and Cellular Migration Modulated by Nuclear-Localized Receptor Tyrosine Kinase ROR1. Anticancer Res. 2011, 31, 4239–4249. [Google Scholar] [PubMed]
- Choi, M.Y.; Widhopf, G.F.; Wu, C.C.N.; Cui, B.; Lao, F.; Sadarangani, A.; Cavagnaro, J.; Prussak, C.; Carson, D.A.; Jamieson, C.; et al. Pre-Clinical Specificity and Safety of UC-961, a First-In-Class Monoclonal Antibody Targeting ROR1. Clin. Lymphoma Myeloma Leuk. 2015, 15, S167–S169. [Google Scholar] [CrossRef] [PubMed]
- Mian, Y.A.; Widhopf II, G.F.; Vo, T.-T.; Jessen, K.; Rassenti, L.Z.; Kipps, T.J. Development of Cirmtuzumab Antibody-Drug Conjugates (ADCs) Targeting Receptor Tyrosine Kinase-like Orphan Receptor 1 (ROR1). Blood 2018, 132, 1862. [Google Scholar] [CrossRef]
- Choi, M.Y.; Wierda, W.G.; Lee, H.J.; Tzachanis, D.; Ianopulos, X.; Jezior, D.; Breitmeyer, J.B.; Jamieson, C.H.; Kipps, T.J. Phase 1/2 Trial of Cirmtuzumab and Ibrutinib: Planned Analysis of Phase 1 CLL Cohorts. J. Clin. Oncol. 2019, 37, 7527. [Google Scholar] [CrossRef]
- Shatsky, R.A.; Schwab, R.B.; Helsten, T.L.; Pittman, E.I.; Chen, R.; Breitmeyer, J.B.; Jamieson, C.H.; Kipps, T.J.; Parker, B.A. Abstract P3-10-18: Phase 1b Trial of Cirmtuzumab and Paclitaxel for Locally Advanced, Unresectable and Metastatic Breast Cancer. Cancer Res. 2020, 80, Abstract nr P3-10–18. [Google Scholar] [CrossRef]
- Bayat, A.-A.; Sadeghi, N.; Fatemi, R.; Nowroozi, M.R.; Ohadian Moghadam, S.; Borzuee, M.; Radmanesh, A.; Khodadoost, M.; Sarrafzadeh, A.R.; Zarei, O.; et al. Monoclonal Antibody Against ROR1 Induces Apoptosis in Human Bladder Carcinoma Cells. Avicenna J. Med. Biotechnol. 2020, 12, 165–171. [Google Scholar]
- Wu, D.; Yu, X.; Wang, J.; Hui, X.; Zhang, Y.; Cai, Y.; Ren, M.; Guo, M.; Zhao, F.; Dou, J. Ovarian Cancer Stem Cells with High ROR1 Expression Serve as a New Prophylactic Vaccine for Ovarian Cancer. J. Immunol. Res. 2019, 2019, 9394615. [Google Scholar] [CrossRef]
- Suryadevara, C.M.; Gedeon, P.C.; Sanchez-Perez, L.; Verla, T.; Alvarez-Breckenridge, C.; Choi, B.D.; Fecci, P.E.; Sampson, J.H. Are BiTEs the “Missing Link” in Cancer Therapy? OncoImmunology 2015, 4, e1008339. [Google Scholar] [CrossRef]
- Qi, J.; Li, X.; Peng, H.; Cook, E.M.; Dadashian, E.L.; Wiestner, A.; Park, H.; Rader, C. Potent and Selective Antitumor Activity of a T Cell-Engaging Bispecific Antibody Targeting a Membrane-Proximal Epitope of ROR1. Proc. Natl. Acad. Sci. USA 2018, 115, e5467–e5476. [Google Scholar] [CrossRef]
- Li, J.; Stagg, N.J.; Johnston, J.; Harris, M.J.; Menzies, S.A.; DiCara, D.; Clark, V.; Hristopoulos, M.; Cook, R.; Slaga, D.; et al. Membrane-Proximal Epitope Facilitates Efficient T Cell Synapse Formation by Anti-FcRH5/CD3 and Is a Requirement for Myeloma Cell Killing. Cancer Cell 2017, 31, 383–395. [Google Scholar] [CrossRef]
- Gohil, S.H.; Paredes-Moscosso, S.R.; Harrasser, M.; Vezzalini, M.; Scarpa, A.; Morris, E.; Davidoff, A.M.; Sorio, C.; Nathwani, A.C.; Peruta, M.D. An ROR1 Bi-Specific T-Cell Engager Provides Effective Targeting and Cytotoxicity against a Range of Solid Tumors. OncoImmunology 2017, 6, e1326437. [Google Scholar] [CrossRef] [PubMed]
- Kroschinsky, F.; Stölzel, F.; von Bonin, S.; Beutel, G.; Kochanek, M.; Kiehl, M.; Schellongowski, P.; Intensive Care in Hematological and Oncological Patients (iCHOP) Collaborative Group. New Drugs, New Toxicities: Severe Side Effects of Modern Targeted and Immunotherapy of Cancer and Their Management. Crit. Care 2017, 21, 89. [Google Scholar] [CrossRef]
- Cui, B.; Widhopf, G.F., II; Prussak, C.E.; Wu, C.C.N.; Sadarangani, A.; Zhang, S.; Lao, F.; Jamieson, C.H.; Carson, D.A.; Kipps, T.J. Cirmtuzumab Vedotin (UC-961ADC3), An Anti-ROR1-Monomethyl Auristatin E Antibody-Drug Conjugate, Is a Potential Treatment For ROR1-Positive Leukemia and Solid Tumors. Blood 2013, 122, 1637. [Google Scholar] [CrossRef]
- Vaisitti, T.; Jessen, K.; Vo, T.-T.; Ko, M.; Arruga, F.; Vitale, N.; Braggio, E.; Di Napoli, A.; Chadburn, A.; Allan, J.N.; et al. Vls-101 Is a Novel Therapeutic Antibody-Drug Conjugate (ADC) Targeting Receptor Tyrosine Kinase-like Orphan Receptor 1 (ROR1) in Richter’s Syndrome (RS). Blood 2019, 134, 2856. [Google Scholar] [CrossRef]
- Beerli, R.R.; Waldmeier, L.; Gébleux, R.; Pretto, F.; Grawunder, U. Abstract LB-197: NBE-002, an Anthracycline-Based Immune-Stimulatory Antibody Drug Conjugate (IADC) Targeting ROR1 for the Treatment of Triple-Negative Breast Cancer. Cancer Res. 2019, 79, LB-197. [Google Scholar] [CrossRef]
- Hu, E.; Do, P.; Mani, R.; Frissora, F.; Pearson, R.; Lozanski, G.; Peng, H.; Waldmeier, L.; Beerli, R.; Rader, C.; et al. Abstract 1541: Evaluation of ROR1 Targeted Antibody Drug Conjugate in ROR1 Positive Leukemia. Cancer Res. 2019, 79, 1541. [Google Scholar] [CrossRef]
- June, C.H.; O’Connor, R.S.; Kawalekar, O.U.; Ghassemi, S.; Milone, M.C. CAR T Cell Immunotherapy for Human Cancer. Science 2018, 359, 1361–1365. [Google Scholar] [CrossRef]
- Heyman, B.; Yang, Y. Chimeric Antigen Receptor T Cell Therapy for Solid Tumors: Current Status, Obstacles and Future Strategies. Cancers 2019, 11, 191. [Google Scholar] [CrossRef]
- Srivastava, S.; Salter, A.I.; Liggitt, D.; Yechan-Gunja, S.; Sarvothama, M.; Cooper, K.; Smythe, K.S.; Dudakov, J.A.; Pierce, R.H.; Rader, C.; et al. Logic-Gated ROR1 Chimeric Antigen Receptor Expression Rescues T Cell-Mediated Toxicity to Normal Tissues and Enables Selective Tumor Targeting. Cancer Cell 2019, 35, 489–503.e8. [Google Scholar] [CrossRef]
- Wallstabe, L.; Göttlich, C.; Nelke, L.C.; Kühnemundt, J.; Schwarz, T.; Nerreter, T.; Einsele, H.; Walles, H.; Dandekar, G.; Nietzer, S.L.; et al. ROR1-CAR T Cells Are Effective against Lung and Breast Cancer in Advanced Microphysiologic 3D Tumor Models. JCI Insight 2019, 4, 18. [Google Scholar] [CrossRef]
- Huang, X.; Park, H.; Greene, J.; Pao, J.; Mulvey, E.; Zhou, S.X.; Albert, C.M.; Moy, F.; Sachdev, D.; Yee, D.; et al. IGF1R- and ROR1-Specific CAR T Cells as a Potential Therapy for High Risk Sarcomas. PLoS ONE 2015, 10, e0133152. [Google Scholar] [CrossRef] [PubMed]
- Hojjat-Farsangi, M.; Daneshmanesh, A.H.; Khan, A.S.; Shetye, J.; Mozaffari, F.; Kharaziha, P.; Rathje, L.-S.; Kokhaei, P.; Hansson, L.; Vågberg, J.; et al. First-in-Class Oral Small Molecule Inhibitor of the Tyrosine Kinase ROR1 (KAN0439834) Induced Significant Apoptosis of Chronic Lymphocytic Leukemia Cells. Leukemia 2018, 32, 2291–2295. [Google Scholar] [CrossRef] [PubMed]
- Daneshmanesh, A.H.; Hojjat-Farsangi, M.; Ghaderi, A.; Moshfegh, A.; Hansson, L.; Schultz, J.; Vågberg, J.; Byström, S.; Olsson, E.; Olin, T.; et al. A Receptor Tyrosine Kinase ROR1 Inhibitor (KAN0439834) Induced Significant Apoptosis of Pancreatic Cells Which Was Enhanced by Erlotinib and Ibrutinib. PLoS ONE 2018, 13, e0198038. [Google Scholar] [CrossRef] [PubMed]
- Gao, W.; Wang, M.; Wang, L.; Lu, H.; Wu, S.; Dai, B.; Ou, Z.; Zhang, L.; Heymach, J.V.; Gold, K.A.; et al. Selective Antitumor Activity of Ibrutinib in EGFR-Mutant Non–Small Cell Lung Cancer Cells. JNCI J. Natl. Cancer Inst. 2014, 106. [Google Scholar] [CrossRef]
- Liu, X.; Pu, W.; He, H.; Fan, X.; Zheng, Y.; Zhou, J.-K.; Ma, R.; He, J.; Zheng, Y.; Wu, K.; et al. Novel ROR1 Inhibitor ARI-1 Suppresses the Development of Non-Small Cell Lung Cancer. Cancer Lett. 2019, 458, 76–85. [Google Scholar] [CrossRef]
- Fultang, N.; Illendula, A.; Chen, B.; Wu, C.; Jonnalagadda, S.; Baird, N.; Klase, Z.; Peethambaran, B. Strictinin, a Novel ROR1-Inhibitor, Represses Triple Negative Breast Cancer Survival and Migration via Modulation of PI3K/AKT/GSK3ß Activity. PLoS ONE 2019, 14, e217789. [Google Scholar] [CrossRef]
- Ford, C.E.; Qian Ma, S.S.; Quadir, A.; Ward, R.L. The Dual Role of the Novel Wnt Receptor Tyrosine Kinase, ROR2, in Human Carcinogenesis. Int. J. Cancer 2013, 133, 779–787. [Google Scholar] [CrossRef]
- Peng, H.; Nerreter, T.; Chang, J.; Qi, J.; Li, X.; Karunadharma, P.; Martinez, G.J.; Fallahi, M.; Soden, J.; Freeth, J.; et al. Mining Naïve Rabbit Antibody Repertoires by Phage Display for Monoclonal Antibodies of Therapeutic Utility. J. Mol. Biol. 2017, 429, 2954–2973. [Google Scholar] [CrossRef]
- Goydel, R.S.; Weber, J.; Peng, H.; Qi, J.; Soden, J.; Freeth, J.; Park, H.; Rader, C. Affinity Maturation, Humanization, and Co-Crystallization of a Rabbit Anti-Human ROR2 Monoclonal Antibody for Therapeutic Applications. J. Biol. Chem. 2020, 295, 5995–6006. [Google Scholar] [CrossRef]
- Hellmann, I.; Waldmeier, L.; Bannwarth-Escher, M.-C.; Maslova, K.; Wolter, F.I.; Grawunder, U.; Beerli, R.R. Novel Antibody Drug Conjugates Targeting Tumor-Associated Receptor Tyrosine Kinase ROR2 by Functional Screening of Fully Human Antibody Libraries Using Transpo-MAb Display on Progenitor B Cells. Front. Immunol. 2018, 9, 2490. [Google Scholar] [CrossRef]
- Sharp, L.L.; Chang, C.; Frey, G.; Wang, J.; Liu, H.; Xing, C.; Yalcin, S.; Walls, M.; Ben, Y.; Boyle, W.J.; et al. Abstract 833: Anti-Tumor Efficacy of BA3021, a Novel Conditionally Active Biologic (CAB) Anti-ROR2 ADC. Cancer Res. 2018, 78, 833. [Google Scholar] [CrossRef]

| Cancer Entity | Expression 1 | Correlation with Survival | Reference |
|---|---|---|---|
| Hematological Malignancies | |||
| acute lymphocytic leukemia | ROR1 + | no correlation found | [18,30] |
| chronic lymphocytic leukemia | ROR1 + | high ROR1 correlates with poor OS and TFS | [31,32,33,34,35,36] |
| diffuse large B cell lymphoma | ROR1 + | n.d. | [37,38] |
| follicular lymphoma | ROR1 + | n.d. | [37,38] |
| mantle cell lymphoma | ROR1 + | n.d. | [37,39] |
| marginal zone lymphoma | ROR1 + | n.d. | [37] |
| multiple myeloma | ROR2 + | n.d. | [40] |
| Solid Tumors | |||
| breast cancer | ROR1 + | high ROR1 correlated with poor OS, MFS and DFS | [41,42,43] |
| ROR2 + | high ROR2 correlated with poor DFS | [44] | |
| cervical cancer | ROR2 + | high ROR2 correlated with poor OS and RFS | [45] |
| colorectal cancer | ROR1 + | high ROR1 correlated with poor OS | [46] |
| ROR2 +/− | high ROR2 correlated with poor OS | [23,47] | |
| endometrial cancer | ROR1 + | high ROR1 correlated with poor OS and PFS | [48,49] |
| ROR2 + | no correlation found for ROR2 | ||
| gastric cancer | ROR1 + | no correlation found for ROR1 | [50,51] |
| ROR2 − | n.d. | [52] | |
| glioblastoma | ROR2 + | no correlation found | [53] |
| lung cancer | ROR1 + | high ROR1 correlated with poor OS | [22,54] |
| ROR2 + | high ROR2 correlated with poor OS | [55] | |
| melanoma | ROR1 + | high ROR1 correlated with poor PRS | [56] |
| mesothelioma | ROR1 + | n.d. | [57] |
| ROR2 + | |||
| ovarian cancer | ROR1 + | high ROR1 correlated with poor OS and DFS | [58] |
| ROR2 +/− | no correlation found for ROR2 | [59,60] | |
| sarcoma | ROR2 + | high ROR2 correlated with poor OS in GIST high ROR2 correlated with poor DSS in leiomyosarcoma | [61,62] |
| pancreatic cancer | ROR1 + | n.d. | [63] |
| ROR2 + | high ROR2 correlated with poor OS | [64] | |
| prostate cancer | ROR2 − | n.d. | [65] |
| Study | Clinicaltrials.gov Identifier | Regimen | Disease | Phase of Development | Estimated Study Completion Date | Status | Sponsor |
|---|---|---|---|---|---|---|---|
| UC-961 (Cirmtuzumab) in Relapsed or Refractory CLL | NCT02222688 | cirmtuzumab | CLL | I | October 2017 | completed | University of California, San Diego |
| An Extension Study of UC-961 (Cirmtuzumab) for Patients With CLL Treated Previously With UC-961 | NCT02860676 | cirmtuzumab | CLL | I | February 2018 | completed | University of California, San Diego |
| A Study of Cirmtuzumab and Paclitaxel for Metastatic or Locally Advanced, Unresectable Breast Cancer | NCT02776917 | cirmtuzumab + paclitaxel | breast cancer | Ib | June 2021 | recruiting | University of California, San Diego |
| A Study of Cirmtuzumab and Ibrutinib in Patients With B-Cell Lymphoid Malignancies | NCT03088878 | cirmtuzumab + ibrutinib | B-CLL MCL SLL | I/II | December 2022 | recruiting | University of California, San Diego |
| A Study of VLS-101 in Patients With Solid Tumors | NCT04504916 | VLS-101 | lung cancer breast cancer | II | July 2022 | recruiting | VelosBio Inc. |
| A Phase 1 Dose-Escalation and Cohort-Expansion of VLS-101 in Hematologic Malignancies | NCT03833180 | VLS-101 | hematologic malignancies | I | June 2021 | recruiting | VelosBio Inc. |
| NBE-002 in Patients With Advanced Solid Tumors | NCT04441099 | NBE-002 | breast cancer and other solid tumors | I/II | July 2023 | recruiting | NBE-Therapeutics AG |
| CAB-ROR2-ADC Safety and Efficacy Study in Patients With Solid Tumors | NCT03504488 | CAB-ROR2-ADC | lung cancer breast cancer sarcoma and other solid tumors | I/II | May 2022 | recruiting | BioAtla, LLC |
| Genetically Modified T-Cell Therapy in Treating Patients With Advanced ROR1+ Malignancies | NCT02706392 | ROR1 CAR T cells | lung cancer breast cancer ALL MCL CLL | I | December 2021 | recruiting | Fred Hutchinson Cancer Research Center, Seattle |
| Safety and Efficacy of CCT301 CAR-T in Adult Subjects With Recurrent or Refractory Stage IV Renal Cell Carcinoma | NCT03393936 | ROR2 CAR T cells | renal cell carcinoma | I/II | January 2021 | not yet recruiting | Shanghai PerHum Therapeutics Co., Ltd. |
| A Study of CCT301-59 CAR T Therapy in Adult Subjects With Recurrent or Refractory Solid Tumors | NCT03960060 | ROR2 CAR T cells | sarcoma gastric cancer pancreatic cancer bladder cancer and other solid tumors | I | February 2021 | not yet recruiting | Shanghai PerHum Therapeutics Co., Ltd. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Menck, K.; Heinrichs, S.; Baden, C.; Bleckmann, A. The WNT/ROR Pathway in Cancer: From Signaling to Therapeutic Intervention. Cells 2021, 10, 142. https://doi.org/10.3390/cells10010142
Menck K, Heinrichs S, Baden C, Bleckmann A. The WNT/ROR Pathway in Cancer: From Signaling to Therapeutic Intervention. Cells. 2021; 10(1):142. https://doi.org/10.3390/cells10010142
Chicago/Turabian StyleMenck, Kerstin, Saskia Heinrichs, Cornelia Baden, and Annalen Bleckmann. 2021. "The WNT/ROR Pathway in Cancer: From Signaling to Therapeutic Intervention" Cells 10, no. 1: 142. https://doi.org/10.3390/cells10010142
APA StyleMenck, K., Heinrichs, S., Baden, C., & Bleckmann, A. (2021). The WNT/ROR Pathway in Cancer: From Signaling to Therapeutic Intervention. Cells, 10(1), 142. https://doi.org/10.3390/cells10010142





