Abstract
Reliable adaptation in Class II resin-based composite (RBC) restorations with margins on cementum remains challenging. This study compared the internal adaptation (IA) and closed porosity (CP) of three restorative strategies for such cavities, using either total-etch or self-etch adhesive approaches. Standardized box-only cavities were prepared on both proximal surfaces of 30 extracted molars, applying self-etch on mesial and total-etch on distal cavities. Group 1 used a layered microhybrid RBC; Group 2 used a flowable RBC base beneath a layered microhybrid RBC; and Group 3 used a thermoviscous RBC in a 4 mm bulk increment. Micro-computed tomography was employed to assess IA and CP. ANOVA, Tukey post hoc, and univariate analyses were used to evaluate group differences and the effects of adhesive/restorative strategies. Group 2 demonstrated the best adaptation (0.10%), whereas Group 3 exhibited the highest internal gap ratio (0.63%) and the lowest CP (p = 0.006). Total-etch adhesive significantly improved IA compared to self-etch (p < 0.001). These findings emphasize the impact of material selection and adhesive technique on the quality of restorations in cementum-located Class II cavities.
1. Introduction
The success of dental resin-based composites (RBCs) is contingent upon the internal adaptation of the material, which exerts a direct influence on the longevity of the restoration. Achieving an exact fit and minimizing interfacial gaps between the tooth structure and the restorative material is paramount in preventing microleakage and reducing the risk of postoperative sensitivity and secondary caries [1]. Minimizing interfacial gaps is also crucial in this regard. It is hypothesized that polymerization shrinkage of RBCs and the resultant shrinkage stress exert a deleterious effect on optimal internal adaptation by compromising adhesion to the tooth [2]. The extent of shrinkage is contingent on the composition of the RBC, primarily the quantity of filler, which determines the stiffness of the material during polymerization. However, the type of monomers utilized, the rate of the reaction, and the external constraints retrieved from the bonding to the tooth also have a significant impact [3,4,5,6,7]. Dental manufacturers have made efforts to address this deficiency. These endeavours have encompassed the formulation of advanced dental bonding agents and reduced shrinkage/shrinkage stress in RBCs. Furthermore, a range of clinical application methods have been employed to manage the shrinkage stress-induced complications. RBCs with a higher filler content, and thus higher elastic module, have become a widely adopted standard technique in the domain of layering placement [8]. Incremental application has been demonstrated to ensure adequate light cure penetration and to decrease shrinkage inherent to RBC by reducing the volume of cured layer [9,10,11].
The advent of single-increment bulk-fill RBCs, which can be utilized in thicknesses of up to 4–5 mm, was motivated by the objective of simplifying the filling process and eradicating the risk of air trapping [12]. Nevertheless, concerns have been raised regarding the shrinkage stress of bulk-fill RBCs as the material is applied in large volumes. In order to address this issue, a modified chemical composition with novel monomer technologies is employed in bulk-fill RBCs [13]. As demonstrated by comparative studies, it has been determined that there is no significant difference in the performance of bulk-fill and layered RBCs with regard to shrinkage stress and marginal adaptation. The preponderance of the findings from the experimental trials indicates a material-dependent nature of these parameters [14,15,16,17].
It was demonstrated that a negative correlation exists between the magnitude of shrinkage and shrinkage strain and the percentage of filler. It appears that this phenomenon may be attributable to a concomitant decrease in the volume fraction of monomers available for polymerization [18]. It is evident that the higher volume fraction of monomers plays a crucial role in the process of shrinkage increase. The lower elastic module of flowable RBCs allows the material to be applied as a stress-relieving thin layer under the RBC with a higher filler volume fraction [1,18]. A finite element analysis demonstrated that flowable RBC lining is capable of reducing polymerization shrinkage stress and occlusal force in enamel, dentin, the hybrid layer, and the adhesive layer to various degrees in tooth-restoration systems [19]. Furthermore, a reduction in RBC viscosity results in enhanced handling of the material and facilitates its application to cavities with complicated forms. This, in turn, leads to a reduction in the time taken for the procedure and an improvement in marginal adaptation [20].
However, should there be a wish to exploit the synergy of both parameters in conjunction with increased filler content and flowable consistency, RBC preheating constitutes a satisfactory alternative [21]. It has been demonstrated that the thermal energy transferred to the RBC has the capacity to enhance the molecular mobility of the resin monomers and the frequency of radical collisions. This enables the propagation process to persist for an extended duration prior to the initiation of autodeceleration [22]. The preheating of the RBCs has been demonstrated to enhance flow, reduce the film-forming thickness, and did not significantly affect other properties, such as linear shrinkage, flexural strength, and cytocompatibility [23,24,25]. Nonetheless, the extant literature on microleakage is the subject of considerable controversy. A number of studies have yielded favourable outcomes [26,27,28]. Conversely, other studies have not observed a decrease in microleakage. Nevertheless, even if microleakage is not improved, it is at least not adversely affected [29]. In contrast, other results demonstrated that the polymerization shrinkage strain of RBCs increased with elevated pre-polymerization temperatures [30]. In the absence of isothermal conditions, the abrupt decline in the temperature of the RBCs during the process of placement has the potential to interfere with the viscoelastic properties of the RBCs. This, in turn, may result in the material becoming detached from the walls prior to the onset of polymerization [23].
The problem has been overcome by the development of a solution that is specifically designed to preheat the material (VisCalor Bulk, Voco, Cuxhaven, Germany) in its delivery system (VisCalor Dispenser, Voco, Cuxhaven, Germany). This technology is known as Infrared Thermoviscous Technology. The solution in question allows a similar application to that of flowable RBC; however, due to the rapid cooling of the applied material, it can be sculpted immediately like a packable RBC, thereby reducing the gap created as a result of shrinkage after warming. The manufacturer asserts that the reduced volumetric shrinkage (1.44 vol%) and shrinkage stress (4.6 MPa) also play a significant role in preventing interfacial gap formation. The material under discussion offers a number of advantages. Firstly, it can be applied with no risk of void formation, and there is no requirement for an overlay. Furthermore, it exhibits excellent physical properties, which can be attributed to its high filler content (83 wt%). The validity of these claims has been substantiated by in vitro studies comparing VisCalor Bulk to regular bulk-filled RBCs [31], and moreover, the marginal integrity, which is critical to the success of RBC restorations, was found to be enhanced with VisCalor Bulk [32,33]. Conversely, the injection of the RBC into the cavity was found to be more significant for marginal adaptation than the preheating procedure [34]. In addition, preheated VisCalor Bulk, which is comparable to the other preheated bulk RBCs, exhibited a substantial increase in internal porosity when compared to the room temperature counterparts [35].
The decision-making process employed by dentists is not confined to the selection of RBC types; there is also the option to utilize different adhesive systems, such as total-etch, self-etch, or universal adhesives, when restoring teeth in disparate situations. An ex vivo study concluded that marginal integrity is not significantly influenced by the use of bulk-fill materials, bonding techniques, or variation in the location of cervical margins [17]. However, a subsequent systematic review determined that although the use of different adhesive protocols has an insignificant effect on the marginal adaptation and the bond strength of the interface between the material and the proximal dentin/cementum, the type of restorative material has a paramount effect on the test results [36].
The present study aims to evaluate and compare the internal adaptation (IA) and closed porosity (CP) across three distinct restorative strategies for Class II cavities located on cementum. The three strategies are as follows: conventional layered RBC, a combination of flowable base with conventional layered RBC, and preheated VisCalor Bulk, applying total-etch adhesive or a universal adhesive system in self-etch mode. This research utilizes a comprehensive analysis employing micro-computed tomography (micro-CT) to provide valuable data to the extant literature, thus guiding clinicians in their selection of materials for posterior restorations. The null-hypotheses were three-fold: (1) there is no difference in IA among the tested RBCs; (2) there is no difference in IA between the adhesive systems utilized, and (3) there is no difference in CP among the tested RBCs.
2. Materials and Methods
The study was approved by the Ethics Committee of the University of Szeged and the Medical Research Council of Hungary (BM/23566–1/2023) and adhered to the principles outlined in the Declaration of Helsinki. The restorations under study were made in extracted third molars that had been removed for orthodontic purposes. Informed consent was obtained from the patients. The extracted teeth were meticulously cleaned and stored in 0.9% saline solution for up to three months prior to use. To prevent microbial contamination, an antibiotic–antifungal mixture was used, consisting of 100 U/mL penicillin, 100 μg/mL streptomycin, and 2.5 μg/mL amphotericin B.
2.1. Specimen Preparation and Restorative Procedures
Table 1 presents an overview of the investigated materials, including their respective manufacturers and compositions.

Table 1.
Materials, manufacturers, and composition of the investigated resin composites.
The occlusal surface of the extracted teeth (n = 30) was reduced to a plane (919 diamond separator disc, Komet, Lemgo, Germany), 3 mm from the cemento-enamel junction, with the objective of standardising the size of the cavities and the uniform distance of the curing unit from the RBC.
Next, 3 × 3 mm wide box-only cavities were prepared (840G diamond cylinder bur, Hager & Meisinger, Neuss, Germany) with a vertical depth of 4 mm on the mesio- and disto-approximal surfaces of the teeth, according to the two types of adhesives utilised in the study. The gingival floor was set to terminate 1 mm apically from the cemento-enamel junction. The internal line angles were rounded. The oro-vestibular and mesio-distal dimensions of the cavities were measured using a digital caliper, with a precision of 0.01 mm (Mitutoyo Corp., Kawasaki, Japan). The 4 mm depth of the cavity along the axial walls was evaluated using a periodontal probe (546/1, Medesy, Maniago, Italy). Preparation of butt-joint cavosurface margins (~90°) was undertaken. The bur was replaced following the preparation of each tenth tooth.
Prior to the commencement of the restoration process, a Tofflemire universal matrix band retainer (Henry Schein, Melville, NY, USA) was securely affixed to the crown in conjunction with a contoured metal band (thickness: 0.04 mm, width: 6.3 mm; Polydentia, Mezzovico-Vira, Switzerland).
The mesial cavities were then subjected to a self-etch adhesive procedure in accordance with the manufacturer’s instructions. Prime & Bond Universal adhesive was meticulously rubbed onto the prepared cavity walls for 20 s, followed by a 10 s drying and 20 s polymerization period in standard mode (LED.D, Woodpecker, Guillin, China; irradiance: 1150 mW/cm2; wavelength: 420–480 nm; light guide tip diameter: 8 mm). The same curing unit was utilized for the entirety of the polymerization processes during the investigation. The tip of the fiberglass light guide was positioned at the centre of the sample, with a distance of 1 mm being maintained from the occlusal orifice of the cavities. Prior to each instance of polymerization, the light irradiance was measured and subsequently controlled using a radiometer (Bluephase Meter II, Ivoclar, Schaan, Liechtenstein).
The distal cavities were subjected to a total-etch adhesive procedure involving the application of 35% phosphoric acid (Ultra-Etch, Ultradent, South Jordan, UT, USA), initially on the enamel margins and subsequently on the dentin for a duration of 15 s. This was followed by a thorough washing process that lasted for 20 s. Thereafter, the cavity was gently dried. Subsequently, the Adper Single Bond 2 adhesive was applied, followed by a rubbing process for 10 s. This was then followed by a drying period of 10 s, and finally, a 20-second polymerization stage.
In Group 1, both the mesial and distal cavities were restored using Filtek Z250 microhybrid RBC in 1.5–2 mm oblique layers. Each layer was polymerized for a duration of 20 s.
In Group 2, Filtek Supreme Flow nanofill flowable RBC was applied in a 1 mm layer thickness to the gingival floor of both mesial and distal cavities. This was followed by the application of two subsequent ~1.5 mm thick oblique layers of Filtek Z250 microhybrid RBC. It is noteworthy that both the flowable RBC layer and the oblique condensable RBC layers were polymerized separately for 20 s.
The restoration of the mesial and distal cavities of Group 3 was achieved through the utilization of the thermoviscous VisCalor Bulk, which was applied in a 4 mm thick bulk increment. Prior to the application, the RBC was preheated in a gun-style variety VisCalor Dispenser using the T1 setting. The efficacy of this setting mode has been demonstrated through its ability to preheat both the warming device and the RBC to 68 °C within a span of 30 s.
The Filtek Z250 and VisCalor RBCs were subjected to a process of condensation, which was carried out at ambient temperature using a handheld instrument (LM-Arte Condensa, LM Dental, Parainen, Finland) that was operated manually.
The RBC restorations were finished and polished with a series of Sof-Lex discs (8691 C, M, F, SF; 3M, St. Paul, MN, USA). All the restorations were prepared by a single operator.
The arrangement of the study groups is presented in Table 2. Figure 1 provides a visual representation of the restoration process applied to the investigated groups.

Table 2.
Study group arrangements.
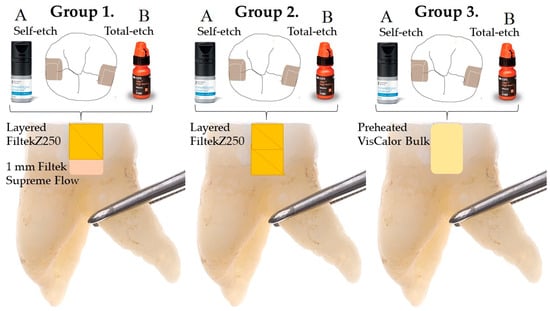
Figure 1.
Schematic diagram of the tested settings.
The restored teeth were stored in distilled water in an incubator (Cultura incubator, Ivoclar Vivadent, Schaan, Liechtenstein) at 37 °C for a period of three months, with the water being changed on a weekly basis. To prevent microbial contamination, an antibiotic–antifungal mixture was used, consisting of 100 U/mL penicillin, 100 μg/mL of streptomycin, and 2.5 μg/mL of amphotericin B.
2.2. Micro-Computed Tomography Measurement—3D Internal Adaptation and Porosity
The images were captured using a Skyscan 1176 micro-CT version 1.1 (build 12) (Bruker, Kontich, Belgium), with the samples positioned at the centre of the field of view, ensuring the axis of the recording field was parallel to the axial plane of the tooth samples. Each tooth was scanned for a duration of 35 min. The X-ray tube was operated with the following parameters during the measurements [37]: tube voltage: 80 kV, current: 310 µA, exposure time: 1500 ms, resolution (pixel size): 8.74 µm, filter: Al 1 mm. The reconstruction was performed using NRecon software (Bruker, version 1.7.4.2). The reconstructed image sequences contained two different fillings in the tooth samples. These were saved in separate image sequences in the axial, coronal, and sagittal planes using the DataViewer software version 1.5.6.2 (Bruker, Kontich, Belgium) (Figure 2). The raw images were subjected to a uniform reconstruction process, resulting in the creation of multiplanar image sequences. Subsequently, the images (initial pixel dimensions 8.74 µm) were converted to a full detector resolution of 1404 × 1404 pixels, employing the *.bmp format. The reconstructed image sequences were also analyzed using CTan software version 1.20.8.0+ (Bruker, Kontich, Belgium). The reconstruction process was executed in accordance with the following parameters: reconstruction duration: 0.8 s for each slice; reconstruction angular range: 197.4°; angular step: 0.7°; ring artefact correction set at 20; edge smoothing at 0.0; and the radius gain set at 20%. In order to achieve the maximum possible level of image detail, the filter cutoff relative to the Nyquist frequency was set at 100 (filter type: Hamming, Alpha = 0.54). A comprehensive dataset was utilized for the reconstruction process, with the undersampling factor fixed at 1, the threshold for the defect pixel mask set to 0%, and the beam hardening correction set at 20%. The reconstructed image sequences were also subjected to analysis using CTan software version 1.20.8.0+ (Bruker, Kontich, Belgium).
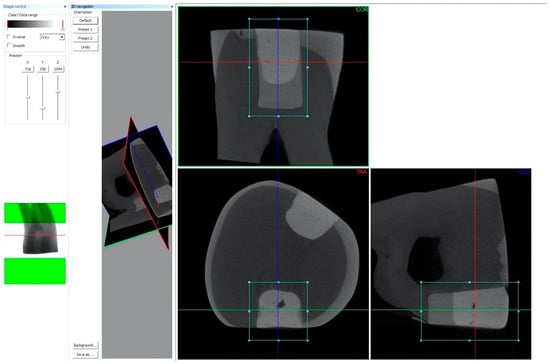
Figure 2.
Reconstruction of the mesial and distal restorations in the tooth samples in coronal, axial, and sagittal views using the DataViewer software (Bruker, version 1.5.6.2).
The solid volumes of tooth and RBC filling were determined according to the grey scale area. The grey scale in the ROI was representative of the solid volume of the samples, with dark colors denoting the gap volume between the filling and the corresponding tooth.
In order to analyze the 3D microarchitecture, the position of the reconstructed scan sequences was standardized in the coronal plane, so that the plane of the image slices was perpendicular to the vertical axis of the restoration (DataViewer: version 1.5.6.2 64-bit). The subsequent workflow was then applied to each tooth in order to evaluate the IA (interfacial gap) between the RBC restoration and the cavity walls. The procedure entailed the identification and manual delineation of the region of interest (ROI), including 0.1 mm (~10 voxel) tooth and 0.1 mm (~10 voxel) restoration along the tooth-restoration interface. Image filtering was employed for the purpose of noise reduction, thereby facilitating straightforward recognition of gaps at the interface by the software. Binary segmentation was utilized to enable uncomplicated separation of the object from the background. Gap identification was conducted in 3D using a binary mask derived from the lowest threshold range. The objective was accomplished through the implementation of a region-growing approach, whereby regions exhibiting equivalent density to that of air were selected. This process was initiated from a designated seed point and involved the incorporation of adjacent voxels that demonstrated analogous intensity. A 3D analysis was performed along the interface of the entire restoration (CTan software, version 1.20.8.0+). The ratio of gap volume to ROI volume was calculated and expressed as a percentage (internal adaptation in percentage, IA%).
In order to assess the CP volume, it was necessary to incorporate the entire RBC restoration within the ROI. The porosity was calculated using grayscale images that had been processed with a Gaussian low-pass filter in order to reduce noise. A histogram-based global thresholding method was applied to segment the grey scale images into binary images, assigning black and white values based on intensity ranges corresponding to material and void, respectively. The process of region growing was utilized for the isolation of internal voids. The CP volume relative to the total volume of the restorations was calculated as a percentage by measuring the internal voids and specimen volumes of each RBC sample.
2.3. Statistical Analysis
Sample size formula [38] and previous study results [37] were used to estimate sample size for micro-CT (IA% and CP) measurements.
where z = standard score; α = probability of Type I error at 95% confidence level = 0.05; z1 − α/2 = 1.96 for 95% confidence; β = probability of Type II error = 0.20; 1 − β = the power of the test = 0.80; z1 − β = value of standard normal variate corresponding to 0.80 value of power = 0.84; s1 = standard deviation of the outcome variable of group 1 = 0.05; s2 = standard deviation of the outcome variable of group 2 = 0.07; M1 = mean of the outcome variable of group 1 = 0.42; M2 = mean of the outcome variable of group 2 = 0.26. The predicted sample size (n) for IA% measurements was found to be a total of 3.7 samples per group. In order to enhance the power of our results, a sample size of 10 subjects per group was determined for the IA% and CP measurements.
The statistical analyses were conducted using the SPSS software program (Version 28.0; IBM, Armonk, NY, USA). The Kolmogorov–Smirnov test was employed to ascertain the normality of the data distribution. This was followed by the implementation of a parametric statistical test. The internal gap volume-to-total interface volume ratio, along with the CP volume of the samples, was subjected to comparison with the outcomes of the one-way analysis of variance (ANOVA). Tukey’s post hoc adjustment was utilized for the purpose of conducting multiple comparisons. Univariate analysis of variance was applied to test the effect size of the filling method (layered vs. flow + layered vs. bulk), adhesive (self-etch vs. total-etch), and their interaction on the IA%. p values below 0.05 were considered statistically significant.
3. Results
3.1. Micro-Computed Tomography Measurement—3D Internal Adaptation
As demonstrated in Figure 3, the calculated ratio of interfacial gap volume to total interface volume is employed to analyze the IA.
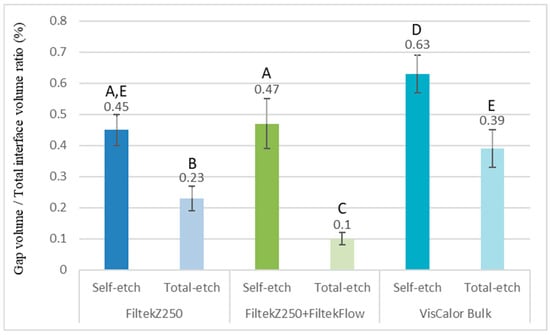
Figure 3.
The ratio of interfacial gap volume to the total volume of the region of interest (ROI, designated examined cavity-restoration interfacial area), assessed using micro-computed tomography analysis. The utilization of different capital letters is indicative of a statistically significant difference, as determined using the one-way ANOVA and Tukey’s post hoc tests.
A multiple comparison of the investigated groups in terms of the internal gap ratio is presented in Table 3. The most substantial gap formation exhibiting a significant discrepancy from the other groups (p < 0.001) was identified in Group 3/A, which underwent restoration with preheated VisCalor Bulk in conjunction with universal adhesive in self-etch mode (internal gap ratio: 0.63%). It was observed that Group 1/B, which involved the restoration of the cavity with a layered conventional RBC and an additional lining with flowable RBC, yielded the most favorable outcomes (internal gap ratio: 0.10%). With regard to the choice of adhesive system, the universal adhesive in the self-etch mode yielded results that were significantly less optimal than those of the groups treated with two-step total-etch adhesive (p < 0.001; 95% CI: 0.23–0.32). The application of one-way analysis of variance (ANOVA) to stratified samples in relation to adhesives revealed significant variations among all filling techniques in total-etch mode (p < 0.001). In contrast, VisCalor demonstrated a substantial reduction in IA in the self-etch mode [FZF_SE vs. VC_SE p < 0.001, 95% CI: −0.22 − (−0.08); FZ_SE vs. VC_SE p < 0.001, 95% CI: −0.24 − (−0.11)]. This finding was in contrast to the layered techniques, where the discrepancy was not deemed to be significant (FZF_SE vs. FZ_SE p = 0.72, 95% CI: −0.05–0.09).

Table 3.
Multiple comparison of the investigated groups in terms of the internal gap ratio (one-way ANOVA and Tukey’s post-hoc test).
Univariate analysis of variance demonstrated a significant effect of the filling method and the adhesive type on the IA (F(2,54) = 95.46, p < 0.001; F(1,54) = 399,19, p < 0.001, respectively). The partial eta-squared was considered to be large (ƞp2 = 0.78 and 0.88, respectively). Their interaction (filling method × adhesive type) was also found to be a significant contributing factor to the gap formation [F(5,54) = 11.69, p = < 0.001; ƞp2 = 0.30]. The observed power for the filling method and adhesive type was 0.96 and 1.00, respectively.
As illustrated in Figure 4, Figure 5 and Figure 6, the images depict the IA and CP of the Filtek Z250 layered restoration, with and without the Filtek Supreme Flowable Base, and the preheated VisCalor Bulk restoration in combination with self-etch or total-etch adhesives.
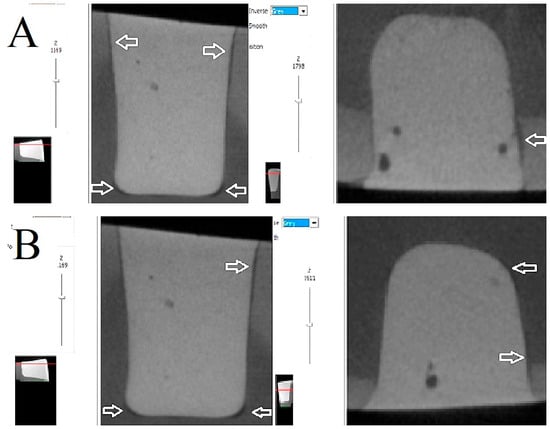
Figure 4.
Representative images of microcomputed tomography analysis of Filtek Z250 layered restorations bonded with self-etch (A) and total-etch (B) adhesives. The presence of white arrows denotes the location of the internal gap.
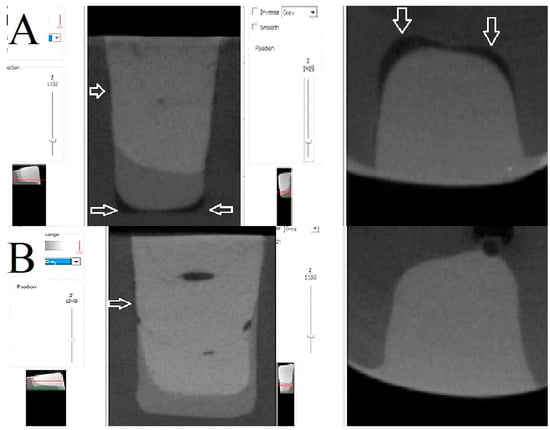
Figure 5.
Representative images of microcomputed tomography analysis of Filtek Z250 layered restorations in combination with Filtek Supreme Flowable base, bonded with self-etch (A) and total-etch (B) adhesives. The presence of white arrows denotes the location of the internal gap.
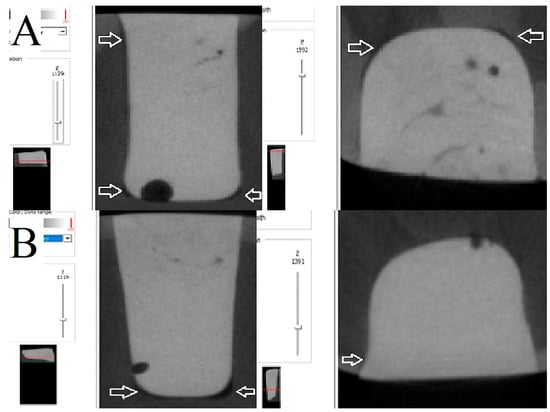
Figure 6.
Representative images of microcomputed tomography analysis of preheated VisCalor Bulk restorations bonded with self-etch (A) and total-etch (B) adhesives. The presence of white arrows denotes the location of the internal gap.
With regard to the localization of the internal gaps formed, the majority of debonding was found on the lateral wall of the cavities. In the case of self-etch adhesives, this was often formed in the enamel–dentin junction area, involving the enamel.
3.2. Micro-Computed Tomography Measurement—3D Closed Porosity
As illustrated in Table 4, a multiple comparison of the groups under investigation has been conducted with regard to the CP volume in relation to the total volume of the restoration. The three-dimensional evaluation demonstrated that the preheated VisCalor Bulk exhibited significantly diminished values with respect to CP, when considered as a proportion of the total volume of the RBC sample (p = 0.006, 95% CI: 0.04–0.24) (Figure 7). No significant differences were identified between the samples prepared using the simple layering technique or the layering technique in combination with a flowable RBC base (p = 1.000, 95% CI: −0.10–0.10). The adhesive technique used had no discernible effect on CP (p = 0.518, 95% CI: −0.09–0.05).

Table 4.
Multiple comparison of the test groups for closed porosity (one-way ANOVA and Tukey’s post-hoc test).
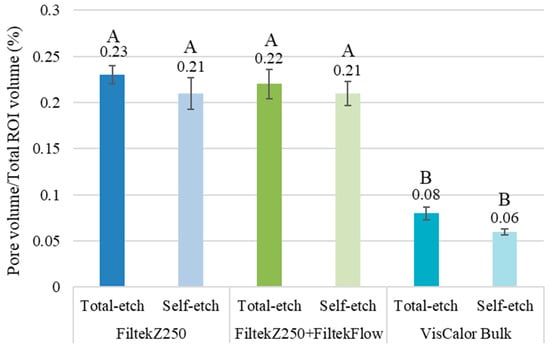
Figure 7.
The ratio of closed pore volume to the total volume of the region of interest (ROI, resin composite restoration) was evaluated using micro-computed tomography analysis. The utilization of different capital letters is indicative of a statistically significant difference, as determined by the one-way ANOVA and Tukey’s post hoc tests.
Univariate analysis of variance demonstrated a significant effect of the filling method [F(2,54) = 18.01, p < 0.001], yet no significant effect of the adhesive type was observed with regard to the IA [F(1,54) = 0.97, p = 0.33]. The partial eta-squared was considered to be large for the filling method (ƞp2 = 0.40) and small the adhesive type (ƞp2 = 0.02). Their interaction (filling method * adhesive type) had a negligible effect on the CP [F(2,54) = 0.18, p = 0.84; ƞp2 = 0.01]. The observed power for the filling method and adhesive type was 1.00 and 0.16, respectively.
4. Discussion
The objective of this ex vivo study was to evaluate the IA and porosity of different restorative strategies employed in Class II cavities, using micro-CT analysis. The materials that were the focus of the investigation comprised thermoviscous bulk-fill RBC (VisCalor Bulk), a conventional RBC (Filtek Z250) applied in 2 mm increments with and without a flowable RBC liner (Filtek Supreme Flow), in combination with either a two-step total-etch or a universal self-etch adhesive. The findings of this study demonstrated that both the type of restorative technique and the adhesive strategy employed had a significant impact on the quality of internal adaptation. The highest volume of interfacial gaps was observed in the VisCalor Bulk group when used with the universal self-etch adhesive. In contrast, the most optimal adaptation was achieved through the combination of the stratification technique and the flowable RBC liner using a two-step total-etch adhesive system. Consequently, the null hypothesis—that there was no difference in IA among the tested RBCs—was rejected. The second null hypothesis, which stated that there is no difference in IA between the adhesive systems utilized, should also be rejected. This outcome can be attributed to the statistical analysis, which revealed substantial disparities between adhesives in favor of the two-step total-etch adhesive. The investigation revealed that the application of the layering technique resulted in a significantly higher number of voids in the restoration compared to the bulk-fill RBC restoration, as measured using micro-CT. Consequently, the third null hypothesis was refuted, which postulated that there was no difference in closed porosity among the tested RBCs.
The inferior performance of the VisCalor Bulk in combination with the universal adhesive in self-etch mode may be attributed to several factors. Initially, preheating the RBC improves flowability and adaptation; however, it may also accelerate polymerization kinetics and, in theory, may increase shrinkage stress once light curing begins [20,23,39]. A comparison of BisGMA-containing (VisCalor) and BisGMA-free RBCs revealed that the shrinkage strain was significantly higher for preheated BisGMA-containing RBCs [30]. In contrast, other research has revealed that preheating RBCs does not lead to an increase in shrinkage strain for some types of RBCs, due to a reduction in their viscosity [40,41]. A number of studies have indicated that VisCalor Bulk exhibits a reduced level of shrinkage stress in comparison to other bulk RBCs [31,32].
The viscoelastic properties of RBCs are known to be temperature-dependent. It is evident that an increase in temperature will result in an increase in energy, and consequently, the velocity of the particles will also increase. It has been demonstrated that achieving a pre-polymerization temperature of 45–60 °C results in a viscosity reduction of at least 30–84% [42,43]. However, the material cools immediately upon removal from the heating apparatus. This alteration transpires within a brief interval. It was ascertained that 50% of the attained temperature was forfeited within 120 s, and approximately 90% within 300 s [44]. An experimental investigation was conducted for the purpose of ascertaining the precise temperature change of VisCalor heated in a dispenser. The research test yielded a measurement of 60 °C, a result that was significantly lower than the stipulated 68 °C. A temperature drop of 26 °C was demonstrated from the time of heating until the initiation of polymerization during the application of the RBC [45]. Following this process, the viscoelastic properties of RBCs undergo a rapid transition. As the temperature is reduced, there is a significant increase in viscosity, which leads to a reduction in flowability and an impaired capacity to adapt to the internal contours of the cavity. Furthermore, as the material cools, its elastic modulus increases, resulting in a stiffer consistency that is less capable of compensating for polymerization shrinkage stress. However, it has been demonstrated that the elevated pre-polymerization temperature, in conjunction with the heat generated during polymerization, can substantially augment the thermal expansion coefficient mismatch between the polymer matrix and the fillers. This can result in the development of stress at the filler–matrix interface and the generation of internal stresses around the fillers [46]. As demonstrated in [47], there appears to be a direct proportionality between residual stress and temperature increase. Furthermore, the thermal volumetric change exhibited by RBCs is found to be six to eight times greater than that of the surrounding tooth structures [22]. Polymerization shrinkage in conjunction with thermal contraction has been shown to generate elevated interfacial stresses in preheated RBCs upon thermal equilibrium, exerting deleterious effects on internal and marginal adaptation [48]. Additionally, the kinetics of polymerization can be influenced by the temperature of the material during the curing process. It has been hypothesized that RBCs with higher temperatures may demonstrate accelerated polymerization, a reduced gel phase, and an augmented degree of conversion. This may result in a diminished capacity to alleviate stress through flow during the curing process [49]. Consequently, the benefits of preheating are highly time-sensitive. It is important to note that any delay in placement may negate these advantages [27], potentially resulting in poorer adaptation than expected.
The adhesive system employed, or indeed the combination of adhesive system and RBC type, also played a crucial role in marginal sealing. A comparison of adhesive systems across all restorative techniques was conducted, and the results demonstrated that the self-etch application mode of the universal adhesive resulted in significantly higher gap formation than the two-step total-etch approach. This outcome is consistent with the results of other in vitro studies that evaluated the microleakage of Class II restorations using the same self-etch adhesive, which was employed in the present study. The total-etch and selective etch techniques have been demonstrated to exhibit superior performance in comparison to self-etch adhesive [50,51]. Etching dentin with phosphoric acid effectively removes the smear layer while exposing the collagen matrix, thus enabling better infiltration of the adhesive and stronger hybrid layer formation [52]. Despite the evident advantages offered by universal adhesives in terms of ease of application, it is important to note that their performance is subject to significant variation depending on the composition of the adhesive and the method of application [53]. Notwithstanding the presence of 10-methacryloyloxydecyl dihydrogen phosphate (10-MDP) and pentaerythritol (PENTA) monomers, it was demonstrated that the 2-hydroxyethyl methacrylate (HEMA)-free Prime & Bond Universal exhibited the weakest bond strength in self-etch mode when compared to other universal adhesives utilizing divergent etching strategies [54]. It has been demonstrated that 10-MDP enhances adhesion by forming a stable ionic bond with dentin calcium [55]. However, the erythritol phosphate group of the polymer network strengthener PENTA may impede calcium bonding due to steric hindrance [54]. The substandard performance observed in the self-etch mode can be attributed to the use of the solvent isopropanol, which possesses a lower dielectric constant compared to ethanol. It has been hypothesized that this may result in an increase in the pKa of acidic monomers, leading to a reduction in hydrolyzed species and an impairment of calcium interaction [56]. Furthermore, in comparison to ethanol, the weak hydrogen bonding capacity of isopropanol can render the adhesive less effective at breaking interpeptide hydrogen bonds that would stabilize collagen fibrils. The lower stiffening rate of the former may increase matrix shrinkage and reduce resin infiltration [57]. In addition, research has demonstrated that the pH of self-etch adhesives can significantly impact the strength of the adhesive bond [58]. The employment of ultra-mild (pH > 2.5) or mild (pH 2–2.5) universal adhesives is associated with limitations in terms of their capacity to penetrate the smear layer. This phenomenon has the potential to compromise the short- and long-term bonding stability [54]. A comprehensive meta-analysis incorporating both in vivo and in vitro studies also confirms that the formation of internal and marginal gaps varies depending on the type of adhesive used. In the majority of cases, etch-and-rinse adhesives demonstrated superior performance, irrespective of the RBC filling application technique employed [59]. This outcome lends support to the hypothesis that, while universal adhesives offer versatility, their bonding efficacy—particularly in self-etch mode—may be inadequate in high C-factor cavities or in enamel-rich regions, unless additional selective enamel etching is employed [60,61,62].
In addition to the aforementioned issues, it has been established that the bulk utilization of RBC is known to engender augmented polymerization shrinkage stress due to the increased volume of the cured material. This phenomenon may contribute to the formation of gaps if adequate compensation is not provided by the adhesive interface [63]. Conversely, a meta-analysis study has demonstrated that bulk-fill RBCs exhibit superior polymerization shrinkage and shrinkage stress values in comparison to conventional RBCs [64]. In the present study, it was demonstrated that restorations placed incrementally with a conventional RBC, especially those with a flowable liner, exhibited superior adaptation. The utilization of a flowable RBC as a stress-absorbing intermediate layer is hypothesized to have enhanced marginal seal by compensating for polymerization shrinkage and adapting more effectively to the cavity walls. These findings are consistent with those of previous studies, which reported enhanced IA with flowable liners and incremental layering techniques in comparison to bulk-fill strategies [65,66,67]. In contrast, other studies have demonstrated that a flowable liner is less effective than preheating the RBC in reducing microleakage [27]. Furthermore, research has indicated that the utilization of preheated VisCalor in lieu of non-preheated bulk-fills or layered conventional RBC can result in a reduction in the formation of marginal or internal gaps [32,33,68].
A further salient point pertains to the interpretation of the results: given the necessity to standardize the samples for an in vitro study, the cavities were prepared with blue diamond burs (~100 µm grit size). It is hypothesized that this process resulted in the formation of a thick and dense smear layer on the surface of the dentin. It has been demonstrated through rigorous research that the smear layer left behind by the diamond abrasive is challenging to penetrate, particularly for mild and ultra-mild self-etching systems. This has been shown to result in impaired bond strength [69]. The detrimental effect of the unpenetrated smear layer can further exacerbate the formation of unfavorable shrinkage vectors caused by a high C-factor cavity, which already has a deleterious effect on adhesion [70]. Notwithstanding the advantages of bulk-fill restoratives, including ease of application and reduced chair time, it has been demonstrated that not all bulk fills can achieve the same level of adhesion as conventional layered materials in high C-factor cavities. In addition, the etch-and-rinse approach has been shown to result in enhanced bond strength and superior resistance to the deleterious effects of ageing in cases where high C-factor cavities were restored with bulk-fill RBCs [71].
While the internal adaptation of VisCalor Bulk with both self-etch and total-etch adhesive systems demonstrated inferior results in comparison to those achieved with conventional RBCs, significantly superior outcomes were observed in relation to closed porosity. It is important to note that internal pores and voids in RBC restorations can be regarded as defects. Such defects have been shown to have a detrimental effect on the material’s strength, thus increasing the risk of fracture. Furthermore, these defects can lead to microleakage, which can potentially result in secondary caries [72]. The findings of this study are consistent with the extant literature, which demonstrates that VisCalor Bulk exhibited the lowest void ratio subsequent to the adaptation of bulk-fill RBCs to the cavity, as determined using micro-CT analysis [73,74]. In contrast, a study that evaluated the effect of preheating on the internal pore formation of high-viscosity conventional layered and bulk-filled samples found that elevated pre-polymerization temperatures significantly increased the closed pore volume relative to the total volume of RBC samples [35]. In essence, void formation is a multifactorial phenomenon influenced by a number of factors. The factors to be considered include the polymerization kinetics of the material, the composition of the resin matrix, the filler load, the architecture of the polymer network, and its heterogeneity [75]. Nevertheless, the presence of fewer internal voids is observed in more flowable materials and when the application of heat is employed [76]. However, a recent study has demonstrated that preheating alone does not reduce the formation of internal voids in RBCs, including VisCalor Bulk. Rather, injection has been shown to have a beneficial effect [34].
However, it is imperative to acknowledge the limitations of the study, which are as follows:
Notwithstanding the samples having been immersed in distilled water for a period of three months following the restorative procedure, this does not take into account the intraoral variables such as thermal cycling, occlusal loading, and long-term hydrolytic degradation. As demonstrated in [59], these factors have been shown to be detrimental to marginal adaptation, irrespective of the material that is applied and the technique by which it is applied. Consequently, in order to obtain results that are more closely aligned with the clinical situation, it is proposed that similar studies in the future be complemented with thermocycling, aging, and mechanical loading simulating chewing. In the present study, a limited number of RBC-adhesive combinations were examined. Consequently, it is not possible to extrapolate these findings to all cases. A comprehensive investigation into the properties of various RBCs and adhesive combinations is warranted as a future research direction, with the aim of identifying the most efficacious combinations for the purpose of minimizing internal gap formation and porosity. It can be hypothesized that, due to the reduced distance, there will be an increased degree of conversion and possibly increased polymerization shrinkage. Despite the minor discrepancies between this experimental protocol and the actual clinical scenario, all samples were subjected to the same protocol. This ensures a valid basis for comparative analysis of the restorative procedures.
Furthermore, although micro-CT provides non-destructive 3D evaluation, its resolution may limit the detection of micro-gaps smaller than the voxel size. Moreover, earlier studies have indicated that high-dose X-ray exposure, particularly in the context of small samples and polymer-based materials, has the potential to induce structural alterations or polymer degradation during micro-CT scanning [77]. In the context of RBCs, it has been demonstrated that the presence of a high ratio of inorganic filler content relative to the organic matrix can result in the attenuation of ionizing radiation. Consequently, no discernible mechanical or thermal change is identifiable [77]. In order to minimize potential radiation-induced artefacts, the scan parameters (tube voltage, current, and exposure time) were meticulously optimized to achieve a balance between image quality and sample integrity. Nevertheless, micro-CT remains the gold standard for highly accurate imaging in experimental dental research due to its ability to deliver reproducible, high-resolution visualizations and quantitative analyses of internal adaptation, polymerization shrinkage, mineral density, and material porosity, among others. The technology under discussion facilitates the extraction of detailed 2D and 3D data of mineralized hard tissues, soft tissues, as well as solid and liquid materials, that would otherwise be unattainable using conventional techniques [78,79,80].
Future research should be expanded to encompass mechanical testing, including microtensile bond strength, and the implementation of ageing protocols. These additional studies will facilitate enhanced prediction of the restorations’ behaviour and the potential clinical durability
5. Conclusions
The findings of this ex vivo study suggest that thermoviscous VisCalor Bulk RBC may offer advantages in reducing internal porosity. However, its internal adaptation was found to be inferior, particularly when combined with Prime & Bond Universal adhesive in a self-etch strategy. In contrast, incremental layering with conventional Filtek Z250 RBC, especially when used with a flowable liner (Filtek Supreme Flowable Restorative) and a total-etch adhesive (Adper Single Bond 2), proved effective in minimizing interfacial gaps. This technique, though, has been observed to be associated with an increase in internal porosity.
Author Contributions
Conceptualization, E.L.; methodology, E.L.; software, E.L.; validation, E.L., T.K.; formal analysis, E.L., T.K.; investigation, D.J., V.V., T.K.; resources, E.L.; data curation, E.L., T.K.; writing—original draft preparation, D.J., E.L.; writing—review and editing, J.S., M.F., E.L.; visualization, E.L.; supervision, J.S.; project administration, D.J., E.L.; funding acquisition, E.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the ÁOK TANDEM Research Grant of the University of Pécs Medical School (KA-2024/28).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the University of Szeged and the Medical Research Council of Hungary (approval number: BM/23566-1/2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. All data were anonymized in line with patient confidentiality guidelines.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Acknowledgments
The research was performed in collaboration with the Department of Pharmacology and Pharmacotherapy of the University of Pécs Medical School.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analysis, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Abbreviations
The following abbreviations are used in this manuscript:
| RBC | Resin-based composite |
| IA | Internal adaptation |
| CP | Closed porosity |
| Micro-CT | Micro-computed tomography |
| BisGMA | Bisphenol-A diglycidyl ether dimethacrylate |
| BisEMA | Bisphenol-A polyethylene glycol diether dimethacrylate |
| DMA | Dimethacrylate |
| HEMA | Hydroxyethyl methacrylate |
| PENTA | Dipentaerythritol pentacrylate phosphate |
| TEGDMA | Triethylene glycol dimethacrylate |
| UDMA | Urethane dimethacrylate |
| 10-MDP | 10-methacryloyloxydecyl dihydrogen phosphate |
| wt% | Weight% |
| SE | Self-etch adhesive |
| TE | Total-etch adhesive |
| FZ_SE | Filtek Z250 layered_self-etch adhesive |
| FZ_TE | Filtek Z250 layered_total-etch adhesive |
| FZF_SE | Filtek Z250 layered + Filtek Supreme Flowable base_self-etch adhesive |
| FZF_TE | Filtek Z250 layered + Filtek Supreme Flowable base_total-etch adhesive |
| VC_SE | Preheated VisCalor Bulk_self-etch adhesive |
| VC_TE | Preheated VisCalor Bulk_total-etch adhesive |
| ROI | Region of interest |
| ANOVA | One-way analysis of variance |
| CI | Confidence interval |
References
- Sadeghi, M.; Lynch, C.D. The effect of flowable materials on the microleakage of Class II composite restorations that extend apical to the cemento-enamel junction. Oper. Dent. 2009, 34, 306–311. [Google Scholar] [CrossRef]
- Han, S.H.; Sadr, A.; Shimada, Y.; Tagami, J.; Park, S.H. Internal adaptation of composite restorations with or without an intermediate layer: Effect of polymerization shrinkage parameters of the layer material. J. Dent. 2019, 80, 41–48. [Google Scholar] [CrossRef]
- Ferracane, J.L. Buonocore Lecture. Placing dental composites—A stressful experience. Oper. Dent. 2008, 33, 247–257. [Google Scholar] [CrossRef]
- Wang, Z.; Chiang, M.Y. System compliance dictates the effect of composite filler content on polymerization shrinkage stress. Dent. Mater. 2016, 32, 551–560. [Google Scholar] [CrossRef]
- Pratap, B.; Gupta, R.K.; Bhardwaj, B.; Nag, M. Resin based restorative dental materials: Characteristics and future perspectives. Jpn. Dent. Sci. Rev. 2019, 55, 126–138. [Google Scholar] [CrossRef]
- Pałka, K.; Janiczuk, P.; Kleczewska, J. Polymerization shrinkage of resin mixtures used in dental composites. Eng. Biomater. 2020, 154, 16–21. [Google Scholar]
- Yamamoto, T.; Nishide, A.; Swain, M.V.; Ferracane, J.L.; Sakaguchi, R.L.; Momoi, Y. Contraction stresses in dental composites adjacent to and at the bonded interface as measured by crack analysis. Acta Biomater. 2011, 7, 417–423. [Google Scholar] [CrossRef]
- Ferracane, J.L. Resin composite—State of the art. Dent. Mater. 2011, 27, 29–38. [Google Scholar] [CrossRef]
- Kwon, Y.; Ferracane, J.L.; Lee, I.B. Effect of layering methods, composite type, and flowable liner on the polymerization shrinkage stress of light cured composites. Dent. Mater. 2012, 28, 801–809. [Google Scholar] [CrossRef]
- Ferracane, J.L.; Hilton, T.J. Polymerization stress—Is it clinically meaningful? Dent. Mater. 2016, 32, 1–10. [Google Scholar] [CrossRef]
- Kim, M.E.; Park, S.H. Comparison of premolar cuspal deflection in bulk or in incremental composite restoration methods. Oper. Dent. 2011, 36, 326–334. [Google Scholar] [CrossRef]
- Lima, R.B.W.; Troconis, C.C.M.; Moreno, M.B.P.; Murillo-Gómez, F.; De Goes, M.F. Depth of cure of bulk fill resin composites: A systematic review. J. Esthetic. Restor. Dent. 2018, 30, 492–501. [Google Scholar] [CrossRef]
- Reis, A.F.; Vestphal, M.; Amaral, R.C.; Rodrigues, J.A.; Roulet, J.F.; Roscoe, M.G. Efficiency of polymerization of bulk-fill composite resins: A systematic review. Braz. Oral Res. 2017, 31, e59. [Google Scholar] [CrossRef]
- Yu, P.; Xu, Y.X.; Liu, Y.S. Polymerization shrinkage and shrinkage stress of bulk-fill and non-bulk-fill resin-based composites. J. Dent. Sci. 2022, 17, 1212–1216. [Google Scholar] [CrossRef]
- McHugh, L.E.J.; Politi, I.; Al-Fodeh, R.S.; Fleming, G.J.P. Implications of resin-based composite (RBC) restoration on cuspal deflection and microleakage score in molar teeth: Placement protocol and restorative material. Dent. Mater. 2017, 33, e329–e335. [Google Scholar] [CrossRef]
- Duarte, R.; Somacal, D.; Braga, L.; Borges, G.; Spohr, A. Cuspal deflection and marginal integrity of Class II cavities restored with bulk-fill resin composites. Open. Dent. J. 2023, 17, e187421062309180. [Google Scholar] [CrossRef]
- Al-Harbi, F.; Kaisarly, D.; Bader, D.; El Gezawi, M. Marginal integrity of bulk versus incremental fill Class II composite restorations. Oper. Dent. 2016, 41, 146–156. [Google Scholar] [CrossRef]
- Baroudi, K.; Saleh, A.M.; Silikas, N.; Watts, D.C. Shrinkage behaviour of flowable resin-composites related to conversion and filler-fraction. J. Dent. 2007, 35, 651–655. [Google Scholar] [CrossRef]
- Anatavara, S.; Sitthiseripratip, K.; Senawongse, P. Stress relieving behaviour of flowable composite liners: A finite element analysis. Dent. Mater. J. 2016, 35, 369–378. [Google Scholar] [CrossRef]
- Baroudi, K.; Mahmoud, S. Improving composite resin performance through decreasing its viscosity by different methods. Open. Dent. J. 2015, 9, 235–242. [Google Scholar] [CrossRef]
- Blalock, J.S.; Holmes, R.G.; Rueggeberg, F.A. Effect of temperature on unpolymerized composite resin film thickness. J. Prosthet. Dent. 2006, 96, 424–432. [Google Scholar] [CrossRef]
- Fróes-Salgado, N.R.; Silva, L.M.; Kawano, Y.; Francci, C.; Reis, A.; Loguercio, A.D. Composite pre-heating: Effects on marginal adaptation, degree of conversion and mechanical properties. Dent. Mater. 2010, 26, 908–914. [Google Scholar] [CrossRef]
- Deb, S.; Di Silvio, L.; Mackler, H.E.; Millar, B.J. Pre-warming of dental composites. Dent. Mater. 2011, 27, e51–e59. [Google Scholar] [CrossRef]
- da Costa, J.; McPharlin, R.; Hilton, T.; Ferracane, J. Effect of heat on the flow of commercial composites. Am. J. Dent. 2009, 22, 92–96. [Google Scholar]
- Dunavári, E.K.; Kőházy, A.; Vecsernyés, M.; Szalma, J.; Lovász, B.V.; Berta, G.; Lempel, E. Does preheating influence the cytotoxic potential of dental resin composites? Polymers 2024, 16, 174. [Google Scholar] [CrossRef]
- Yang, J.N.C.; James, D.R.; Herald, S. Effects of preheated composite on micro leakage-An in-vitro study. J. Clin. Diagn. Res. 2016, 10, 36–38. [Google Scholar] [CrossRef]
- Wagner, W.C.; Aksu, M.N.; Neme, A.M.; Linger, J.B.; Pink, F.E.; Walker, S. Effect of pre-heating resin composite on restoration microleakage. Oper. Dent. 2008, 33, 72–78. [Google Scholar] [CrossRef]
- dos Santos, R.E.; Lima, A.F.; Soares, G.P.; Ambrosano, G.M.; Marchi, G.M.; Lovadino, J.R.; Aguiar, F.H. Effect of preheating resin composite and light-curing units on the microleakage of Class II restorations submitted to thermocycling. Oper. Dent. 2011, 36, 60–65. [Google Scholar] [CrossRef]
- Karaarslan, E.S.; Usumez, A.; Ozturk, B.; Cebe, M.A. Effect of cavity preparation techniques and different preheating procedures on microleakage of class v resin restorations. Eur. J. Dent. 2012, 6, 87–94. [Google Scholar] [CrossRef][Green Version]
- Lotfy, M.; Mahmoud, N.A.; Riad, M.I. Effect of preheating on polymerization shrinkage strain of BIS-GMA free and containing resin composite restorative materials (in vitro study). Bull. Natl. Res. Cent. 2022, 46, 74. [Google Scholar] [CrossRef]
- Hordones Ribeiro, M.T.; Felipe de Bragança, G.; Sales Oliveira, L.R.; Lourenço Braga, S.S.; Quirino de Oliveira, H.L.; Price, R.B.; Soares, C.J. Effect of pre-heating methods and devices on the mechanical properties, post-gel shrinkage, and shrinkage stress of bulk-fill materials. J. Mech. Behav. Biomed. Mater. 2023, 138, 105605. [Google Scholar] [CrossRef]
- Soares, B.M.; Barbosa, M.P.; de Almeida, R.V.; Jardim, R.N.; da Silva, E.M. Marginal integrity and physicomechanical properties of a thermoviscous and regular bulk-fill resin composites. Clin. Oral Investig. 2024, 28, 496. [Google Scholar] [CrossRef]
- Demirel, G.; Orhan, A.I.; Irmak, O.; Aydın, F.; Büyüksungur, A.; Bilecenoğlu, B.; Orhan, K. Effects of preheating and sonic delivery techniques on the internal adaptation of bulk-fill resin composites. Oper. Dent. 2021, 46, 226–233. [Google Scholar] [CrossRef]
- Sá, V.A.; Bittencourt, H.R.; Burnett Júnior, L.H.; Spohr, A.M. Preheated and injected bulk-fill resin composites: A micro-CT analysis of internal voids and marginal adaptation in Class II restorations. Materials 2025, 18, 327. [Google Scholar] [CrossRef]
- Dunavári, E.; Berta, G.; Kiss, T.; Szalma, J.; Fráter, M.; Böddi, K.; Lempel, E. Effect of pre-heating on the monomer elution and porosity of conventional and bulk-fill resin-based dental composites. Int. J. Mol. Sci. 2022, 23, 16188. [Google Scholar] [CrossRef]
- Ismail, H.S.; Ali, A.I.; Mehesen, R.E.; Juloski, J.; Garcia-Godoy, F.; Mahmoud, S.H. Deep proximal margin rebuilding with direct esthetic restorations: A systematic review of marginal adaptation and bond strength. Restor. Dent. Endod. 2022, 47, e15. [Google Scholar] [CrossRef]
- Néma, V.; Kunsági-Máté, S.; Őri, Z.; Kiss, T.; Szabó, P.; Szalma, J.; Fráter, M.; Lempel, E. Relation between internal adaptation and degree of conversion of short-fiber reinforced resin composites applied in bulk or layered technique in deep MOD cavities. Dent. Mater. 2024, 40, 581–592. [Google Scholar] [CrossRef]
- Padam, S. Sample size for experimental studies. J. Clin. Prev. Card. 2012, 1, 88–93. [Google Scholar]
- Lohbauer, U.; Zinelis, S.; Rahiotis, C.; Petschelt, A.; Eliades, G. The effect of resin composite pre-heating on monomer conversion and polymerization shrinkage. Dent. Mater. 2009, 25, 514–519. [Google Scholar] [CrossRef]
- Tauböck, T.T.; Tarle, Z.; Marovic, D.; Attin, T. Pre-heating of high-viscosity bulk-fill resin composites: Effects on shrinkage force and monomer conversion. J. Dent. 2015, 43, 1358–1364. [Google Scholar] [CrossRef]
- Yang, J.; Silikas, N.; Watts, D.C. Pre-heating time and exposure duration: Effects on post-irradiation properties of a thermo-viscous resin-composite. Dent. Mater. 2020, 36, 787–793. [Google Scholar] [CrossRef]
- Loumprinis, N.; Maier, E.; Belli, R.; Petschelt, A.; Eliades, G.; Lohbauer, U. Viscosity and stickiness of dental resin composites at elevated temperatures. Dent. Mater. 2021, 37, 413–422. [Google Scholar] [CrossRef]
- Poubel, D.L.D.N.; da Silva, R.C.; Ribeiro, A.P.D.; Garcia, F.C.P. Effect of preheating on the viscosity of composite resins. J. Conserv. Dent. Endod. 2024, 27, 360–365. [Google Scholar] [CrossRef]
- Daronch, M.; Rueggeberg, F.A.; Hall, G.; De Goes, M.F. Effect of composite temperature on in vitro intrapulpal temperature rise. Dent. Mater. 2007, 23, 1283–1288. [Google Scholar] [CrossRef]
- Kincses, D.; Böddi, K.; Őri, Z.; Lovász, B.V.; Jeges, S.; Szalma, J.; Kunsági-Máté, S.; Lempel, E. Pre-heating effect on monomer elution and degree of conversion of contemporary and thermoviscous bulk-fill resin-based dental composites. Polymers 2021, 13, 3599. [Google Scholar] [CrossRef]
- Ferracane, J.L. Developing a more complete understanding of stresses produced in dental composites during polymerization. Dent. Mater. 2005, 21, 36–42. [Google Scholar] [CrossRef]
- Prasanna, N.; Pallavi Reddy, Y.; Kavitha, S.; Lakshmi Narayanan, L. Degree of conversion and residual stress of preheated and room-temperature composites. Ind. J. Dent. Res. 2007, 18, 173–176. [Google Scholar] [CrossRef]
- Watts, D.C.; Issa, M.; Ibrahim, A.; Wakiaga, K.; Al-Samadini, M.; Silikas, N. Edge strength of resin-composite margins. Dent. Mater. 2008, 24, 129–133. [Google Scholar] [CrossRef]
- El-Korashy, D.I. Post-gel shrinkage strain and degree of conversion of preheated resin composite cured using different regimens. Oper. Dent. 2010, 35, 172–179. [Google Scholar] [CrossRef]
- Yollar, M.; Karaoglanoglu, S.; Altiparmak, E.T.; Aybala Oktay, E.; Aydin, N.; Ersoz, B. The effects of dental adhesives total etch; self-etch and selective etch application procedures on microleakage in Class II composite restorations. Eur. Oral Res. 2023, 57, 151–158. [Google Scholar] [CrossRef]
- Signore, A.; Solimei, L.; Arakelyan, M.G.; Arzukanyan, A.V.; De Angelis, N.; Amaroli, A. Marginal quality of a full-body bulk-fill composite placed with an universal adhesive system in etch-and-rinse and self-etch mode: An in vitro study. J. Clin. Exp. Dent. 2021, 13, e835–e844. [Google Scholar] [CrossRef]
- de Souza, J.; Ñaupari-Villasante, R.; Hass, V.; Arana-Gordillo, L.A.; Gutiérrez, M.F.; Gomes, G.M.; Loguercio, A.D.; Gomes, J.C. Optimizing phosphoric acid etching times across different formulations: Impact on dentin structure, roughness, and adhesive performance after 4 years. Dent. Mater. 2025, 41, 850–861. [Google Scholar] [CrossRef]
- Giannini, M.; Vermelho, P.M.; de Araújo Neto, V.G.; Soto-Montero, J. An update on universal adhesives: Indications and limitations. Curr. Oral Health Rep. 2022, 9, 57–65. [Google Scholar] [CrossRef]
- Ismail, H.S.; Soliman, H.A.N. Short dentin etching with universal adhesives: Effect on bond strength and gingival margin adaptation. BMC Oral Health 2025, 25, 128. [Google Scholar] [CrossRef]
- Yoshihara, K.; Nagaoka, N.; Hayakawa, S.; Okihara, T.; Yoshida, Y.; Van Meerbeek, B. Chemical interaction of glycero-phosphate dimethacrylate (GPDM) with hydroxyapatite and dentin. Dent. Mater. 2018, 34, 1072–1081. [Google Scholar] [CrossRef]
- Salz, U.; Mücke, A.; Zimmermann, J.; Tay, F.R.; Pashley, D.H. pKa value and buffering capacity of acidic monomers commonly used in self-etching primers. J. Adhes. Dent. 2006, 8, 143–150. [Google Scholar]
- Ekambaram, M.; Yiu, C.K.Y.; Matinlinna, J.P. An overview of solvents in resin–dentin bonding. Int. J. Adhes. Adhes. 2015, 57, 22–33. [Google Scholar] [CrossRef]
- Kenshima, S.; Reis, A.; Uceda-Gomez, N.; Tancredo Lde, L.; Filho, L.E.; Nogueira, F.N.; Loguercio, A.D. Effect of smear layer thickness and pH of self-etching adhesive systems on the bond strength and gap formation to dentin. J. Adhes. Dent. 2005, 7, 117–126. [Google Scholar]
- Ferracane, J.L.; Lawson, N.C. Probing the hierarchy of evidence to identify the best strategy for placing class II dental composite restorations using current materials. J. Esthet. Restor. Dent. 2021, 33, 39–50. [Google Scholar] [CrossRef]
- Suzuki, T.; Takamizawa, T.; Barkmeier, W.W.; Tsujimoto, A.; Endo, H.; Erickson, R.L.; Latta, M.A.; Miyazaki, M. Influence of etching mode on enamel bond durability of universal adhesive systems. Oper. Dent. 2016, 41, 520–530. [Google Scholar] [CrossRef]
- Hardan, L.; Bourgi, R.; Kharouf, N.; Mancino, D.; Zarow, M.; Jakubowicz, N.; Haikel, Y.; Cuevas-Suárez, C.E. Bond strength of universal adhesives to dentin: A systematic review and meta-analysis. Polymers 2021, 13, 814. [Google Scholar] [CrossRef]
- Loguercio, A.D.; Reis, A.; Bortoli, G.; Patzlaft, R.; Kenshima, S.; Rodrigues Filho, L.E.; Accorinte Mde, L.; van Dijken, J.W. Influence of adhesive systems on interfacial dentin gap formation in vitro. Oper. Dent. 2006, 31, 431–441. [Google Scholar] [CrossRef]
- Kim, R.J.; Kim, Y.J.; Choi, N.S.; Lee, I.B. Polymerization shrinkage, modulus, and shrinkage stress related to tooth-restoration interfacial debonding in bulk-fill composites. J. Dent. 2015, 43, 430–439. [Google Scholar] [CrossRef]
- Cidreira Boaro, L.C.; Pereira Lopes, D.; de Souza, A.S.C.; Lie Nakano, E.; Ayala Perez, M.D.; Pfeifer, C.S.; Gonçalves, F. Clinical performance and chemical-physical properties of bulk fill composites resin —A systematic review and meta-analysis. Dent. Mater. 2019, 35, e249–e264. [Google Scholar] [CrossRef]
- Han, S.H.; Park, S.H. Incremental and bulk-fill techniques with bulk-fill resin composite in different cavity configurations. Oper. Dent. 2018, 43, 631–641. [Google Scholar] [CrossRef]
- Alqudaihi, F.S.; Cook, N.B.; Diefenderfer, K.E.; Bottino, M.C.; Platt, J.A. Comparison of internal adaptation of bulk-fill and increment-fill resin composite materials. Oper. Dent. 2019, 44, E32–E44. [Google Scholar] [CrossRef]
- Kaisarly, D.; Meierhofer, D.; El Gezawi, M.; Rösch, P.; Kunzelmann, K.H. Effects of flowable liners on the shrinkage vectors of bulk-fill composites. Clin. Oral Investig. 2021, 25, 4927–4940. [Google Scholar] [CrossRef]
- Ramadan, N.A.; Hasan, M.M.A.; Abdalla, A.I. Marginal adaptation of thermoviscous bulk-fill composite in class II cavities. Tanta Dent. J. 2023, 20, 77–83. [Google Scholar] [CrossRef]
- Saikaew, P.; Sattabanasuk, V.; Harnirattisai, C.; Chowdhury, A.F.M.A.; Carvalho, R.; Sano, H. Role of the smear layer in adhesive dentistry and the clinical applications to improve bonding performance. Jpn. Dent. Sci. Rev. 2022, 58, 59–66. [Google Scholar] [CrossRef]
- Marques, M.S.; Kenshima, S.; Muench, A.; Ballester, R.Y.; Rodrigues Filho, L.E. Effect of the C-factor and dentin preparation method in the bond strength of a mild self-etch adhesive. Oper. Dent. 2009, 34, 452–459. [Google Scholar] [CrossRef]
- Eichler, E.; Vach, K.; Schlueter, N.; Jacker-Guhr, S.; Luehrs, A.K. Dentin adhesion of bulk-fill composites and universal adhesives in class I cavities with high C-factor. J. Dent. 2024, 142, 104852. [Google Scholar] [CrossRef]
- Sarna-Boś, K.; Skic, K.; Sobieszczański, J.; Boguta, P.; Chałas, R. Contemporary approach to the porosity of dental materials and methods of its measurement. Int. J. Mol. Sci. 2021, 22, 8903. [Google Scholar] [CrossRef]
- Özdemir, S.; Ayaz, İ.; Çetin Tuncer, N.; Barutçugil, Ç.; Dündar, A. Evaluation of polymerization shrinkage, microhardness, and depth of cure of different types of bulk-fill composites. J. Esthet. Restor. Dent. 2025, 37, 1920–1929. [Google Scholar] [CrossRef]
- Demirel, G.; Orhan, A.I.; Irmak, O.; Aydin, F.; Buyuksungur, A.; Bilecenoğlu, B.; Orhan, K. Micro-computed tomographic evaluation of the effects of pre-heating and sonic delivery on the internal void formation of bulk-fill composites. Dent. Mater. J. 2021, 40, 525–531. [Google Scholar] [CrossRef]
- Buelvas, D.D.A.; Besegato, J.F.; Vicentin, B.L.S.; Jussiani, E.I.; Hoeppner, M.G.; Andrello, A.C.; Di Mauro, E. Impact of light-cure protocols on the porosity and shrinkage of commercial bulk fill resin composites with different flowability. J. Polym. Res. 2020, 27, 292. [Google Scholar] [CrossRef]
- Gigova, R.; Hristov, K. Micro-CT assessment of internal and external void formation in Class II restorations of primary molars using bulk-fill composites. Materials 2025, 18, 2621. [Google Scholar] [CrossRef]
- Koenig, A.; Schmohl, L.; Scheffler, J.; Fuchs, F.; Schulz-Siegmund, M.; Doerfler, H.-M.; Jankuhn, S.; Hahnel, S. Is Micro X-ray Computer Tomography a Suitable Non-Destructive Method for the Characterisation of Dental Materials? Polymers 2021, 13, 1271. [Google Scholar] [CrossRef]
- Ghavami-Lahiji, M.; Davalloo, R.T.; Tajziehchi, G.; Shams, P. Micro-computed tomography in preventive and restorative dental research: A review. Imaging Sci. Dent. 2021, 51, 341–350. [Google Scholar] [CrossRef]
- Campioni, I.; Pecci, R.; Bedini, R. Ten Years of Micro-CT in Dentistry and Maxillofacial Surgery: A Literature Overview. Appl. Sci. 2020, 10, 4328. [Google Scholar] [CrossRef]
- Nagdalian, A.A.; Rzhepakovsky, I.V.; Siddiqui, S.A.; Piskov, S.I.; Oboturova, N.P.; Timchenko, L.D.; Lodygin, A.D.; Blinov, A.V.; Ibrahim, S.A. Analysis of the content of mechanically separated poultry meat in sausage using computing microtomography. J. Food Compos. Anal. 2021, 100, 103918. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).