Surface Modification of Mesoporous Silica Nanoparticles for Application in Targeted Delivery Systems of Antitumour Drugs
Abstract
1. Introduction
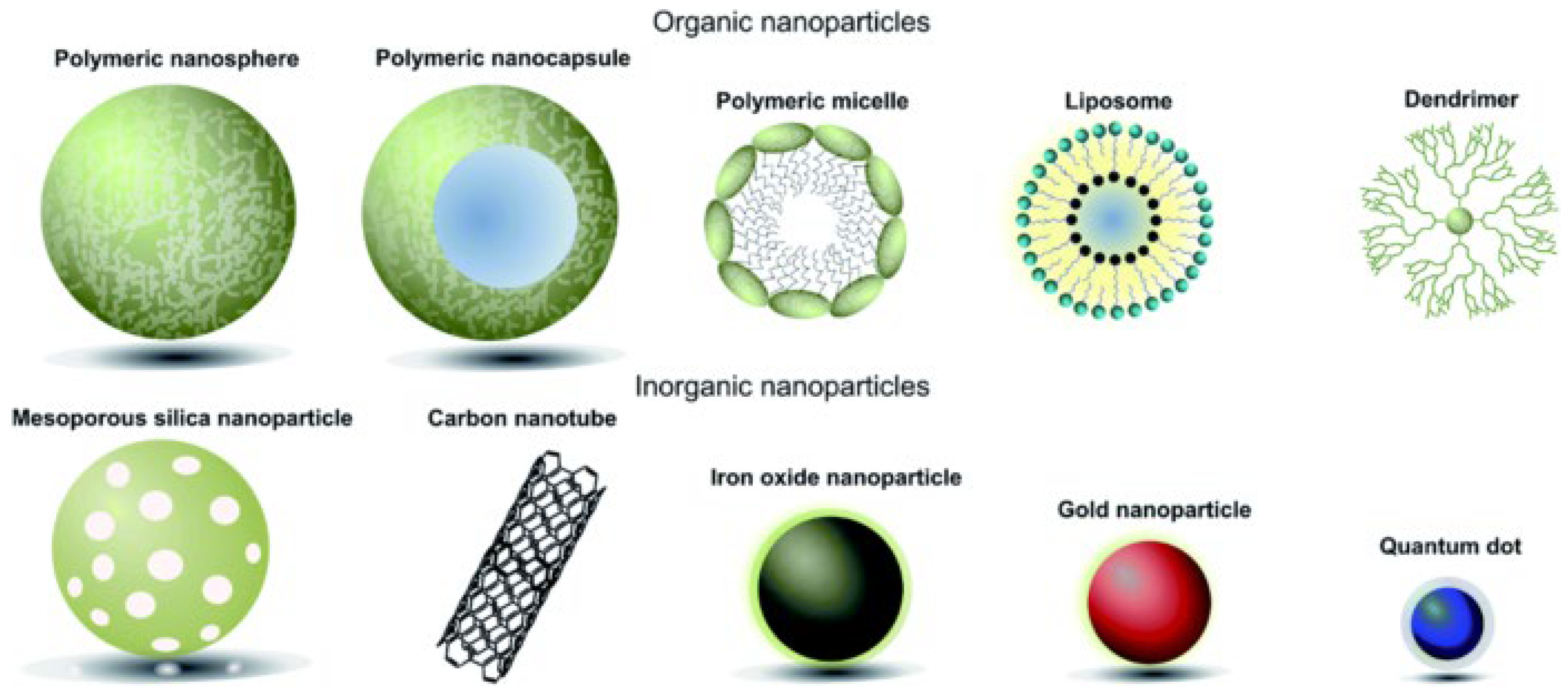
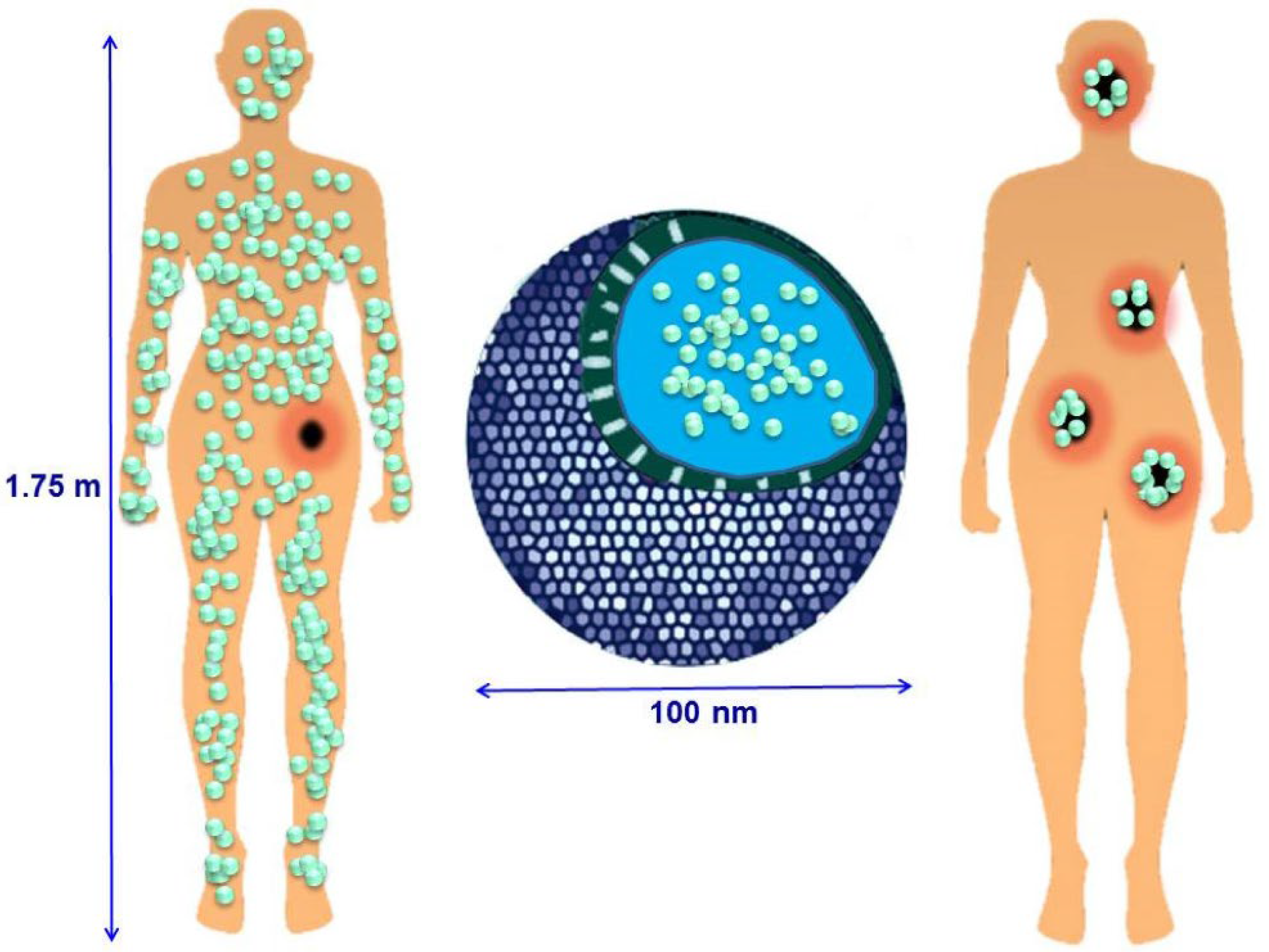
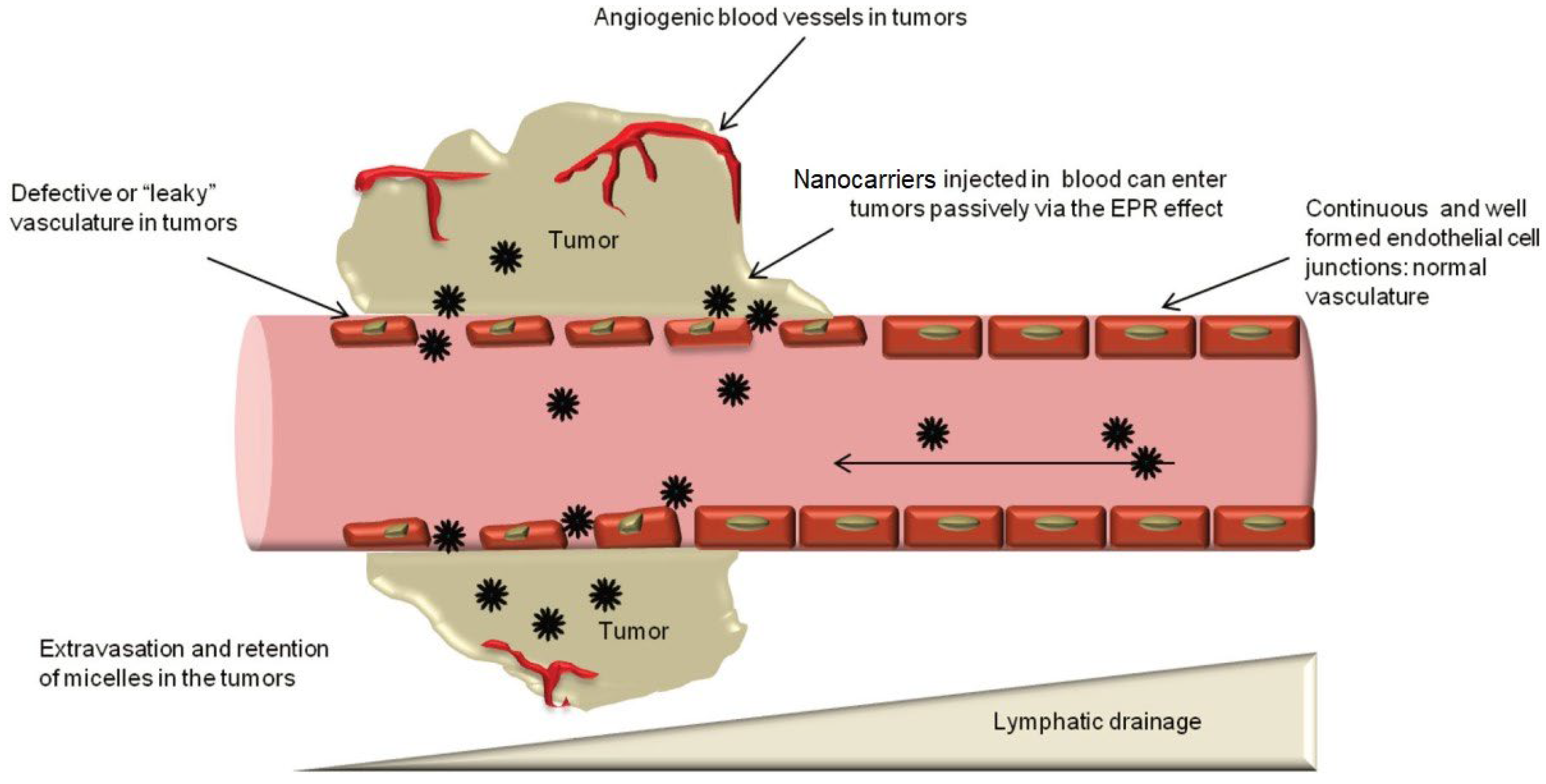
2. Application of Micro- and Nanoparticles in Drug Delivery Systems
- -
- -
- -
- -
- Ensuring convenience of administration [35].
- -
- -
- -
- Liposomes [53];
- -
- -
- -
- -

3. Mesoporous Silicon Dioxide Is a Promising Nanocarrier for Drugs
4. Factors Affecting Cytotoxicity, Cellular Uptake, and Biocompatibility of Nanoparticles
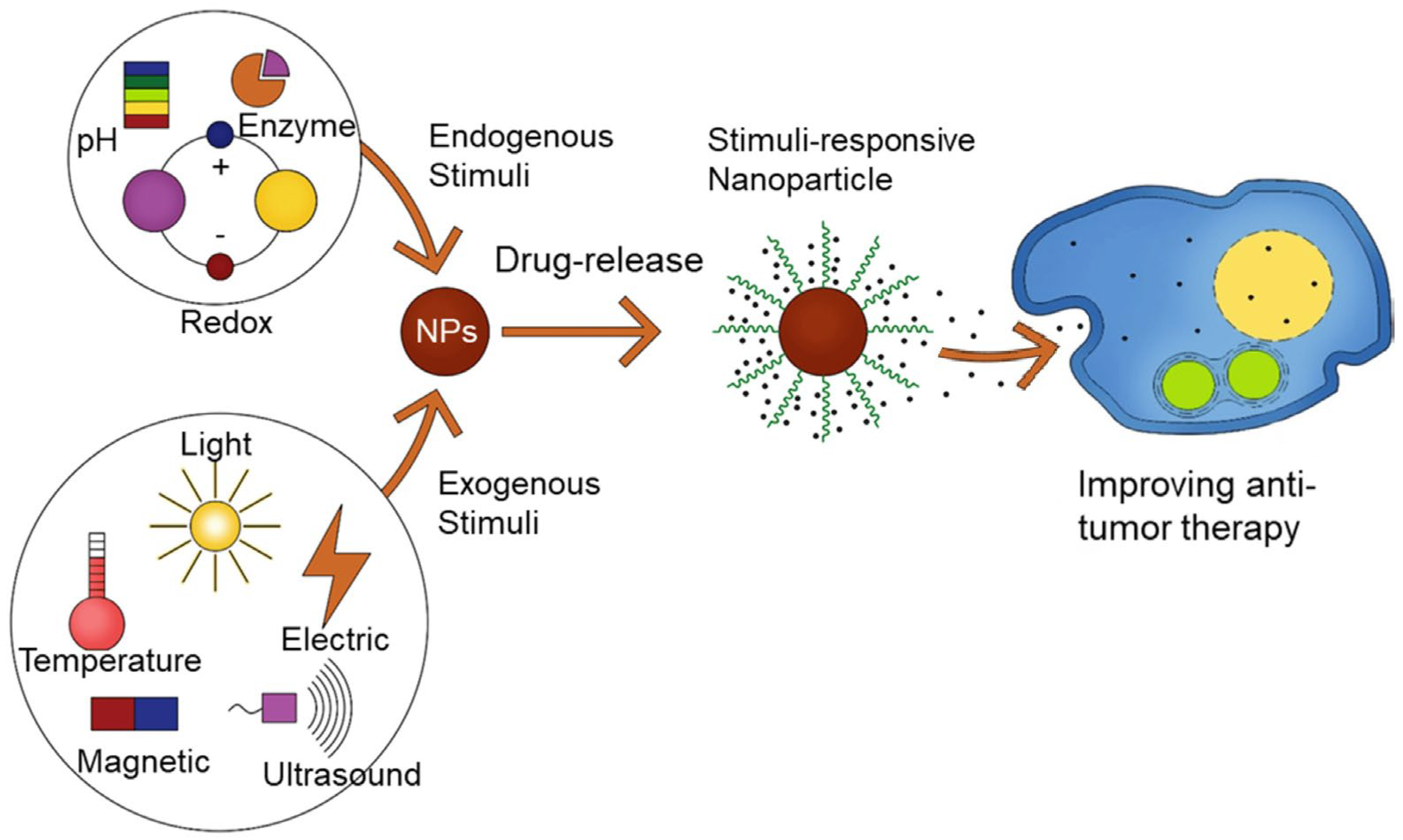
5. Stimuli That Control Drug Release
5.1. Temperature- and pH-Sensitive Nanocarriers Based on Mesoporous Silica
5.2. Redox Drug Delivery
6. Antitumour Drugs in Mesoporous-Silica-Based Delivery Systems
7. Conclusions
- -
- Improving biocompatibility;
- -
- Increasing the ability of nanoparticles to retain drugs;
- -
- Increasing the specificity of delivery;
- -
- Allowing controlled drug release.
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Parkin, D.M.; Piñeros, M.; Znaor, A.; Bray, F. Cancer Statistics for the Year 2020: An Overview. Int. J. Cancer 2021, 149, 778–789. [Google Scholar] [CrossRef]
- Taillibert, S.; Le Rhun, E.; Chamberlain, M.C. Chemotherapy-Related Neurotoxicity. Curr. Neurol. Neurosci. Rep. 2016, 16, 81. [Google Scholar] [CrossRef]
- McGowan, J.V.; Chung, R.; Maulik, A.; Piotrowska, I.; Walker, J.M.; Yellon, D.M. Anthracycline Chemotherapy and Cardiotoxicity. Cardiovasc. Drugs Ther. 2017, 31, 63–75. [Google Scholar] [CrossRef] [PubMed]
- Morgensztern, D.; Samson, P.S.; Waqar, S.N.; Devarakonda, S.; Robinson, C.G.; Govindan, R.; Puri, V. Early Mortality in Patients Undergoing Adjuvant Chemotherapy for Non–Small Cell Lung Cancer. J. Thorac. Oncol. 2018, 13, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Gray, E.; Figueroa, J.D.; Oikonomidou, O.; MacPherson, I.; Urquhart, G.; Cameron, D.A.; Hall, P.S. Variation in Chemotherapy Prescribing Rates and Mortality in Early Breast Cancer over Two Decades: A National Data Linkage Study. ESMO Open 2021, 6, 100331. [Google Scholar] [CrossRef]
- Taylor, C.W.; Kirby, A.M. Cardiac Side-Effects from Breast Cancer Radiotherapy. Clin. Oncol. 2015, 27, 621–629. [Google Scholar] [CrossRef]
- Vanmarcke, D.; Menten, J.; Defraene, G.; Van Calenbergh, F.; De Vleeschouwer, S.; Lambrecht, M. Stroke Rate after External Fractionated Radiotherapy for Benign Meningioma. J. Neurooncol. 2021, 152, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Hermanek, P.; Sobin, L.H. Breast Tumours (ICD-O 174). In TNM Classification of Malignant Tumours; Springer: Berlin/Heidelberg, Germany, 1987; pp. 93–99. [Google Scholar]
- Obermair, A.; Asher, R.; Pareja, R.; Frumovitz, M.; Lopez, A.; Moretti-Marques, R.; Rendon, G.; Ribeiro, R.; Tsunoda, A.; Behan, V.; et al. Incidence of Adverse Events in Minimally Invasive vs Open Radical Hysterectomy in Early Cervical Cancer: Results of a Randomized Controlled Trial. Am. J. Obstet. Gynecol. 2020, 222, 249.e1–249.e10. [Google Scholar] [CrossRef] [PubMed]
- Ohta, T.; Nagase, S.; Okui, Y.; Enomoto, T.; Yamagami, W.; Mikami, M.; Tokunaga, H.; Ino, K.; Ushijima, K.; Shozu, M.; et al. Surveillance of Radical Hysterectomy for Early-Stage Cervical Cancer in the Early Experienced Period of Minimally Invasive Surgery in Japan. Int. J. Clin. Oncol. 2021, 26, 2318–2330. [Google Scholar] [CrossRef]
- Chowdhry, V.K.; Bushey, J.A.; Kwait, R.M.; Goldberg, S.; Ritchie, J.; Ji, Y.-L.; McKee, R.; Palladino, D.; Proulx, G.M. Intraoperative Radiation Therapy as Part of Planned Monotherapy for Early-Stage Breast Cancer. J. Radiat. Oncol. 2018, 7, 167–173. [Google Scholar] [CrossRef]
- Jang, J.-U.; Han, M.-S.; Kim, G.-J.; Seo, S.-Y.; Yoo, S.-J.; Jeon, M.-C. Recent Technical Trends in Radiation Therapy. J. Korean Magn. Soc. 2019, 29, 196–207. [Google Scholar] [CrossRef]
- Park, H.S.; Jung, M.; Kim, H.S.; Kim, H.-I.; An, J.Y.; Cheong, J.-H.; Hyung, W.J.; Noh, S.H.; Kim, Y.I.; Chung, H.C.; et al. Proper Timing of Adjuvant Chemotherapy Affects Survival in Patients with Stage 2 and 3 Gastric Cancer. Ann. Surg. Oncol. 2015, 22, 224–231. [Google Scholar] [CrossRef]
- Ginesi, M.C.; Bliggenstorfer, J.T.; Kwesiga, D.M.; Xu, S.H.; Jodeh, D.; Eva Selfridge, J.; Stein, S.L.; Steinhagen, E.F. Factors Associated with Receipt of Adjuvant Chemotherapy in Stage II Colon Cancer. Ann. Surg. Oncol. 2023, 30, 5511–5518. [Google Scholar] [CrossRef] [PubMed]
- Cascone, T.; Fradette, J.; Pradhan, M.; Gibbons, D.L. Tumor Immunology and Immunotherapy of Non-Small-Cell Lung Cancer. Cold Spring Harb. Perspect. Med. 2022, 12, a037895. [Google Scholar] [CrossRef] [PubMed]
- Morganti, S.; Tolaney, S.M. Role of Immunotherapy in Early- and Late-Stage Triple-Negative Breast Cancer. Hematol. Oncol. Clin. N. Am. 2023, 37, 133–150. [Google Scholar] [CrossRef] [PubMed]
- Nichol, A.M.; Chan, E.K.; Lucas, S.; Smith, S.L.; Gondara, L.; Speers, C.; Tyldesley, S. The Use of Hormone Therapy Alone Versus Hormone Therapy and Radiation Therapy for Breast Cancer in Elderly Women: A Population-Based Study. Int. J. Radiat. Oncol. *Biol. *Phys. 2017, 98, 829–839. [Google Scholar] [CrossRef] [PubMed]
- Dong, Z.; Wang, H.; Xu, M.; Li, Y.; Hou, M.; Wei, Y.; Liu, X.; Wang, Z.; Xie, X. Intermittent Hormone Therapy versus Continuous Hormone Therapy for Locally Advanced Prostate Cancer: A Meta-Analysis. Aging Male 2015, 18, 233–237. [Google Scholar] [CrossRef]
- Lee, Y.T.; Tan, Y.J.; Oon, C.E. Molecular Targeted Therapy: Treating Cancer with Specificity. Eur. J. Pharmacol. 2018, 834, 188–196. [Google Scholar] [CrossRef]
- Mullard, A. BTK Inhibitors Get a Boost. Nat. Rev. Drug Discov. 2017, 16, 818. [Google Scholar] [CrossRef]
- Ilies, D.C.; Zlatev, Z.; Ilies, A.; Zharas, B.; Pantea, E.; Hodor, N.; Indrie, L.; Turza, A.; Taghiyari, H.R.; Caciora, T.; et al. Interdisciplinary Research to Advance Digital Imagery and Natural Compounds for Eco-Cleaning and for Preserving Textile Cultural Heritage. Sensors 2022, 22, 4442. [Google Scholar] [CrossRef]
- Watermann, A.; Brieger, J. Mesoporous Silica Nanoparticles as Drug Delivery Vehicles in Cancer. Nanomaterials 2017, 7, 189. [Google Scholar] [CrossRef] [PubMed]
- Kesse, S.; Boakye-Yiadom, K.; Ochete, B.; Opoku-Damoah, Y.; Akhtar, F.; Filli, M.; Asim Farooq, M.; Aquib, M.; Maviah Mily, B.; Murtaza, G.; et al. Mesoporous Silica Nanomaterials: Versatile Nanocarriers for Cancer Theranostics and Drug and Gene Delivery. Pharmaceutics 2019, 11, 77. [Google Scholar] [CrossRef]
- Ghaferi, M.; Koohi Moftakhari Esfahani, M.; Raza, A.; Al Harthi, S.; Ebrahimi Shahmabadi, H.; Alavi, S.E. Mesoporous Silica Nanoparticles: Synthesis Methods and Their Therapeutic Use-Recent Advances. J. Drug Target. 2021, 29, 131–154. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.; Sun, H.-Y.; Wang, Z.-C.; Xu, X.-D.; Song, J.-C.; Gong, Z.-J. Fabrication of Alginate/Calcium Carbonate Hybrid Microparticles for Synergistic Drug Delivery. Chemotherapy 2016, 61, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Mi, Y.; Mu, C.; Wolfram, J.; Deng, Z.; Hu, T.Y.; Liu, X.; Blanco, E.; Shen, H.; Ferrari, M. A Micro/Nano Composite for Combination Treatment of Melanoma Lung Metastasis. Adv. Healthc. Mater. 2016, 5, 936–946. [Google Scholar] [CrossRef]
- Yang, B.; Ni, X.; Chen, L.; Zhang, H.; Ren, P.; Feng, Y.; Chen, Y.; Fu, S.; Wu, J. Honokiol-Loaded Polymeric Nanoparticles: An Active Targeting Drug Delivery System for the Treatment of Nasopharyngeal Carcinoma. Drug Deliv. 2017, 24, 660–669. [Google Scholar] [CrossRef]
- Zheng, K.; Zhou, D.; Wu, L.; Li, J.; Zhao, B.; Zhang, S.; He, R.; Xiao, L.; Zoya, I.; Yu, L.; et al. K. Zheng et al. Gold-Nanoparticle-Based Multistage Drug Delivery System for Antitumor Therapy. Drug Deliv. 2022, 29, 3186–3196. [Google Scholar] [CrossRef] [PubMed]
- Batool, S.; Sohail, S.; ud Din, F.; Alamri, A.H.; Alqahtani, A.S.; Alshahrani, M.A.; Alshehri, M.A.; Choi, H.G. A Detailed Insight of the Tumor Targeting Using Nanocarrier Drug Delivery System. Drug Deliv. 2023, 30, 2183815. [Google Scholar] [CrossRef] [PubMed]
- Nam, H.Y.; Kwon, S.M.; Chung, H.; Lee, S.-Y.; Kwon, S.-H.; Jeon, H.; Kim, Y.; Park, J.H.; Kim, J.; Her, S.; et al. Cellular Uptake Mechanism and Intracellular Fate of Hydrophobically Modified Glycol Chitosan Nanoparticles. J. Control. Release 2009, 135, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Chen, J.; Han, Q.; Luo, Q.; Zhang, H.; Wang, Y. Construction of Doxorubicin-Conjugated Lentinan Nanoparticles for Enhancing the Cytotoxocity Effects against Breast Cancer Cells. Colloids Surf. A Physicochem. Eng. Asp. 2019, 579, 123657. [Google Scholar] [CrossRef]
- Tu, T.-Y.; Yang, S.-J.; Tsai, M.-H.; Wang, C.-H.; Lee, S.-Y.; Young, T.-H.; Shieh, M.-J. Dual-Triggered Drug-Release Vehicles for Synergistic Cancer Therapy. Colloids Surf. B Biointerfaces 2019, 173, 788–797. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Hu, Y.; Hao, Y.; Li, L.; Zheng, C.; Zhao, H.; Niu, M.; Yin, Y.; Zhang, Z.; Zhang, Y. Tumor-Targeting Core-Shell Structured Nanoparticles for Drug Procedural Controlled Release and Cancer Sonodynamic Combined Therapy. J. Control. Release 2018, 286, 74–84. [Google Scholar] [CrossRef] [PubMed]
- Haidary, S.M.; Mohammed, A.B.; Córcoles, E.P.; Ali, N.K.; Ahmad, M.R. Effect of Coatings and Surface Modification on Porous Silicon Nanoparticles for Delivery of the Anticancer Drug Tamoxifen. Microelectron. Eng. 2016, 161, 1–6. [Google Scholar] [CrossRef]
- Prajapati, R.; Garcia-Garrido, E.; Somoza, Á. Albumin-Based Nanoparticles for the Delivery of Doxorubicin in Breast Cancer. Cancers 2021, 13, 3011. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Cheng, K.; Chen, K.; Xu, C.; Ma, P.; Dang, G.; Yang, Y.; Lei, Q.; Huang, H.; Yu, Y.; et al. Nanoparticle-Based Medicines in Clinical Cancer Therapy. Nano Today 2022, 45, 101512. [Google Scholar] [CrossRef]
- Bou-belda, E.; Indrie, L.; Ilieș, D.C.; Hodor, N.; Berdenov, Z.; Herman, G.; Caciora, T. Chitosan—A Non-Invasive Approach for the Preservation of Historical Textiles. Ind. Textila 2020, 71, 576–579. [Google Scholar] [CrossRef]
- Martínez-Carmona, M.; Colilla, M.; Vallet-Regí, M. Smart Mesoporous Nanomaterials for Antitumor Therapy. Nanomaterials 2015, 5, 1906–1937. [Google Scholar] [CrossRef] [PubMed]
- Matsumura, Y.; Maeda, H. A New Concept for Macromolecular Therapeutics in Cancer Chemotherapy: Mechanism of Tumoritropic Accumulation of Proteins and the Antitumor Agent Smancs. Cancer Res. 1986, 46, 6387–6392. [Google Scholar] [PubMed]
- Jhaveri, A.M.; Torchilin, V.P. Multifunctional Polymeric Micelles for Delivery of Drugs and SiRNA. Front. Pharmacol. 2014, 5, 77. [Google Scholar] [CrossRef]
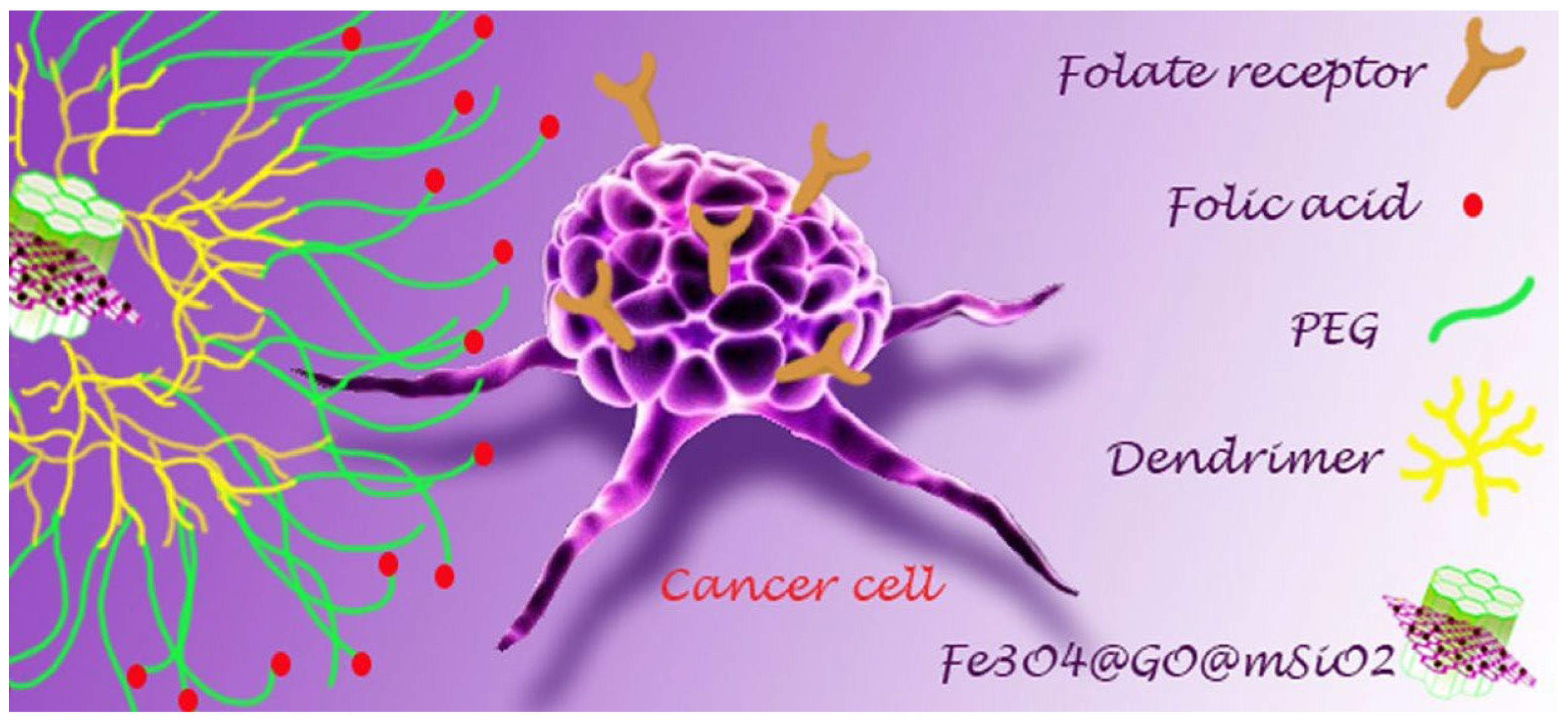
- Pourjavadi, A.; Tehrani, Z.M.; Moghanaki, A.A. Folate-Conjugated PH-Responsive Nanocarrier Designed for Active Tumor Targeting and Controlled Release of Gemcitabine. Pharm. Res. 2016, 33, 417–432. [Google Scholar] [CrossRef]
- Sun, X.; Wang, N.; Yang, L.-Y.; Ouyang, X.-K.; Huang, F. Folic Acid and PEI Modified Mesoporous Silica for Targeted Delivery of Curcumin. Pharmaceutics 2019, 11, 430. [Google Scholar] [CrossRef] [PubMed]
- Al-Nadaf, A.H.; Dahabiyeh, L.A.; Jawarneh, S.; Bardaweel, S.; Mahmoud, N.N. Folic Acid-Hydrophilic Polymer Coated Mesoporous Silica Nanoparticles Target Doxorubicin Delivery. Pharm. Dev. Technol. 2021, 26, 582–591. [Google Scholar] [CrossRef]
- Mao, J.; Meng, X.; Zhao, C.; Yang, Y.; Liu, G. Development of Transferrin-Modified Poly(Lactic-Co-Glycolic Acid) Nanoparticles for Glioma Therapy. Anticancer. Drugs 2019, 30, 604–610. [Google Scholar] [CrossRef] [PubMed]
- Venkatesan, P.; Thirumalaivasan, N.; Yu, H.-P.; Lai, P.-S.; Wu, S.-P. Redox Stimuli Delivery Vehicle Based on Transferrin-Capped MSNPs for Targeted Drug Delivery in Cancer Therapy. ACS Appl. Bio Mater. 2019, 2, 1623–1633. [Google Scholar] [CrossRef] [PubMed]
- Xin, Y.; Huang, Q.; Tang, J.-Q.; Hou, X.-Y.; Zhang, P.; Zhang, L.Z.; Jiang, G. Nanoscale Drug Delivery for Targeted Chemotherapy. Cancer Lett. 2016, 379, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Shair Mohammad, I.; Chaurasiya, B.; Yang, X.; Lin, C.; Rong, H.; He, W. Homotype-Targeted Biogenic Nanoparticles to Kill Multidrug-Resistant Cancer Cells. Pharmaceutics 2020, 12, 950. [Google Scholar] [CrossRef] [PubMed]
- Song, S.J.; Choi, J.S. Enzyme-Responsive Amphiphilic Peptide Nanoparticles for Biocompatible and Efficient Drug Delivery. Pharmaceutics 2022, 14, 143. [Google Scholar] [CrossRef]
- Lin, W.; Ma, G.; Yuan, Z.; Qian, H.; Xu, L.; Sidransky, E.; Chen, S. Development of Zwitterionic Polypeptide Nanoformulation with High Doxorubicin Loading Content for Targeted Drug Delivery. Langmuir 2019, 35, 1273–1283. [Google Scholar] [CrossRef]
- Liao, H.; Liu, H.; Li, Y.; Zhang, M.; Tomás, H.; Shen, M.; Shi, X. Antitumor Efficacy of Doxorubicin Encapsulated within PEGylated Poly(Amidoamine) Dendrimers. J. Appl. Polym. Sci. 2014, 131. [Google Scholar] [CrossRef]
- Hascicek, C.; Sengel-Turk, C.T.; Gumustas, M.; Ozkan, A.S.; Bakar, F.; Das-Evcimen, N.; Savaser, A.; Ozkan, Y. Fulvestrant-Loaded Polymer-Based Nanoparticles for Local Drug Delivery: Preparation and in Vitro Characterization. J. Drug Deliv. Sci. Technol. 2017, 40, 73–82. [Google Scholar] [CrossRef]
- Adhikari, C. Polymer Nanoparticles-Preparations, Applications and Future Insights: A Concise Review. Polym. Plast. Technol. Mater. 2021, 60, 1996–2024. [Google Scholar] [CrossRef]
- Guimarães, D.; Cavaco-Paulo, A.; Nogueira, E. Design of Liposomes as Drug Delivery System for Therapeutic Applications. Int. J. Pharm. 2021, 601, 120571. [Google Scholar] [CrossRef]
- Winter, P.M.; Cai, K.; Caruthers, S.D.; Wickline, S.A.; Lanza, G.M. Emerging Nanomedicine Opportunities with Perfluorocarbon Nanoparticles. Expert. Rev. Med. Devices 2007, 4, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Shen, Y.; Wang, Y.; Zhu, L.; Zhu, C.; Qian, C.; Sun, M.; Oupicky, D. Perfluorocarbon Nanoemulsions for Combined Pulmonary SiRNA Treatment of Lung Metastatic Osteosarcoma. Adv. Ther. 2019, 2, 1900039. [Google Scholar] [CrossRef]
- Zhao, Q.; Lin, Y.; Han, N.; Li, X.; Geng, H.; Wang, X.; Cui, Y.; Wang, S. Mesoporous Carbon Nanomaterials in Drug Delivery and Biomedical Application. Drug Deliv. 2017, 24, 94–107. [Google Scholar] [CrossRef] [PubMed]
- Bayda, S.; Hadla, M.; Palazzolo, S.; Kumar, V.; Caligiuri, I.; Ambrosi, E.; Pontoglio, E.; Agostini, M.; Tuccinardi, T.; Benedetti, A.; et al. Bottom-up Synthesis of Carbon Nanoparticles with Higher Doxorubicin Efficacy. J. Control. Release 2017, 248, 144–152. [Google Scholar] [CrossRef]
- Chernysheva, M.G.; Melik-Nubarov, N.S.; Grozdova, I.D.; Myasnikov, I.Y.; Tashlitsky, V.N.; Badun, G.A. Reduction of Cytotoxicity of Myramistin by Adsorption on Nanodiamonds. Mendeleev Commun. 2017, 27, 421–423. [Google Scholar] [CrossRef]
- Paul, W.; Sharma, C.P. Inorganic Nanoparticles for Targeted Drug Delivery. In Biointegration of Medical Implant Materials; Elsevier: Amsterdam, The Netherlands, 2010; pp. 204–235. [Google Scholar]
- Jarosz, M.; Pawlik, A.; Szuwarzyński, M.; Jaskuła, M.; Sulka, G.D. Nanoporous Anodic Titanium Dioxide Layers as Potential Drug Delivery Systems: Drug Release Kinetics and Mechanism. Colloids Surf. B Biointerfaces 2016, 143, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Dukhopelnykov, E.V.; Blyzniuk, Y.N.; Skuratovska, A.A.; Bereznyak, E.G.; Gladkovskaya, N.A. Interaction of Doxorubicin Delivered by Superparamagnetic Iron Oxide Nanoparticles with DNA. Colloids Surf. B Biointerfaces 2022, 219, 112815. [Google Scholar] [CrossRef] [PubMed]
- Rawat, P.; Imam, S.S.; Gupta, S. Formulation of Cabotegravir Loaded Gold Nanoparticles: Optimization, Characterization to In-Vitro Cytotoxicity Study. J. Clust. Sci. 2023, 34, 893–905. [Google Scholar] [CrossRef] [PubMed]
- Korolkov, I.V.; Ludzik, K.; Lisovskaya, L.I.; Zibert, A.V.; Yeszhanov, A.B.; Zdorovets, M.V. Modification of Magnetic Fe3O4 Nanoparticles for Targeted Delivery of Payloads. Bull. Karaganda Univ. “Chem.” Ser. 2021, 101, 99–108. [Google Scholar] [CrossRef]
- Zhao, M.-X.; Zhu, B.-J. The Research and Applications of Quantum Dots as Nano-Carriers for Targeted Drug Delivery and Cancer Therapy. Nanoscale Res. Lett. 2016, 11, 207. [Google Scholar] [CrossRef] [PubMed]
- Felix, D.M.; Rebelo Alencar, L.M.; Duarte de Menezes, F.; Midlej, V.d.V.P.; Aguiar, L.; Gemini Piperni, S.; Zhang, J.; Liu, Y.; Ricci-Junior, E.; Alexis, F.; et al. Graphene Quantum Dots Decorated with Imatinib for Leukemia Treatment. J. Drug Deliv. Sci. Technol. 2021, 61, 102117. [Google Scholar] [CrossRef]
- Richards, D.A.; Maruani, A.; Chudasama, V. Antibody Fragments as Nanoparticle Targeting Ligands: A Step in the Right Direction. Chem. Sci. 2017, 8, 63–77. [Google Scholar] [CrossRef] [PubMed]
- Ueno, Y. Mesoporous Silica. Anal. Sci. 2019, 35, 121–122. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Gou, K.; Yang, B.; Wang, Y.; Pu, X.; Li, S.; Li, H. Enlarged Pore Size Chiral Mesoporous Silica Nanoparticles Loaded Poorly Water-Soluble Drug Perform Superior Delivery Effect. Molecules 2019, 24, 3552. [Google Scholar] [CrossRef] [PubMed]
- Dleam, E.A.; Kareem, S.H. Mesoporous Silica Nanoparticles as a System for Ciprofloxacin Drug Delivery; Kinetic of Adsorption and Releasing. Baghdad Sci. J. 2021, 18, 0357. [Google Scholar] [CrossRef]
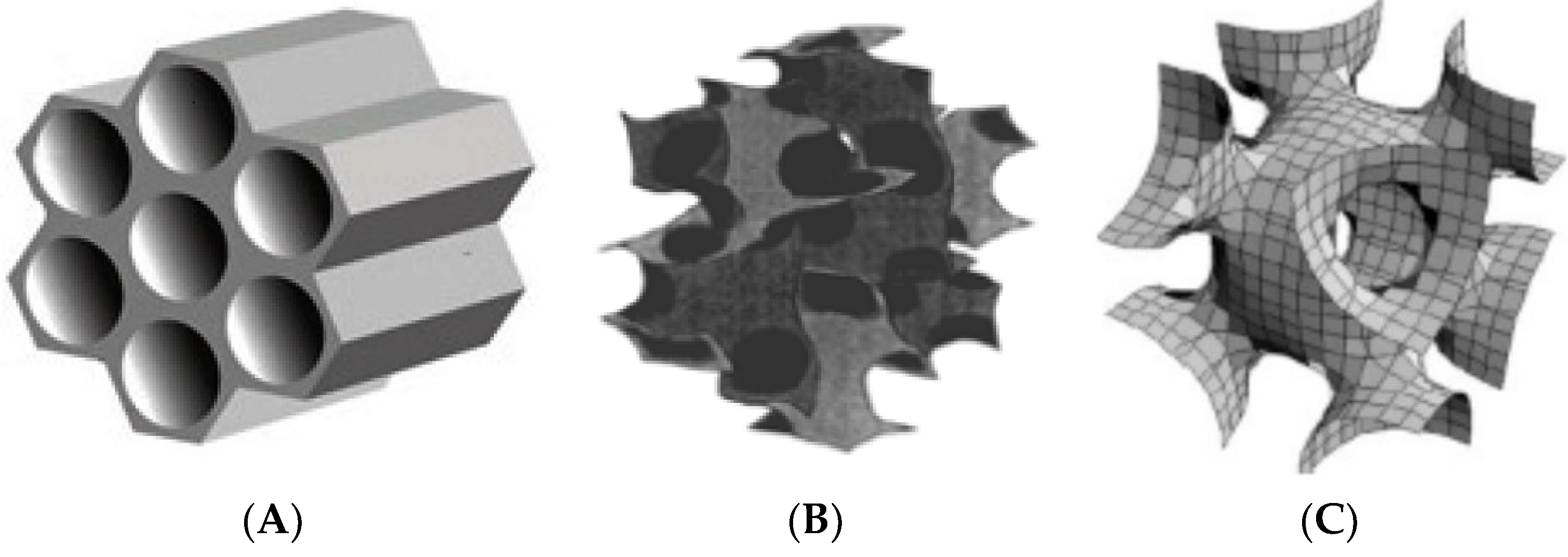
- Beck, J.S.; Vartuli, J.C.; Roth, W.J.; Leonowicz, M.E.; Kresge, C.T.; Schmitt, K.D.; Chu, C.T.W.; Olson, D.H.; Sheppard, E.W.; McCullen, S.B.; et al. A New Family of Mesoporous Molecular Sieves Prepared with Liquid Crystal Templates. J. Am. Chem. Soc. 1992, 114, 10834–10843. [Google Scholar] [CrossRef]
- Nefedova, T.; Roessner, F.; Selemenev, V. Mesoporous Silica MCM-48: Synthesis and Application Prospects. Sorpt. Chromatogr. Process. 2020, 20, 31–39. [Google Scholar] [CrossRef]
- Gonzalez, G.; Sagarzazu, A.; Cordova, A.; Gomes, M.E.; Salas, J.; Contreras, L.; Noris-Suarez, K.; Lascano, L. Comparative Study of Two Silica Mesoporous Materials (SBA-16 and SBA-15) Modified with a Hydroxyapatite Layer for Clindamycin Controlled Delivery. Microporous Mesoporous Mater. 2018, 256, 251–265. [Google Scholar] [CrossRef]
- Dadej, A.; Woźniak-Braszak, A.; Bilski, P.; Piotrowska-Kempisty, H.; Józkowiak, M.; Stawny, M.; Dadej, D.; Mrotek, M.; Jelińska, A. APTES-Modified SBA-15 as a Non-Toxic Carrier for Phenylbutazone. Materials 2022, 15, 946. [Google Scholar] [CrossRef] [PubMed]
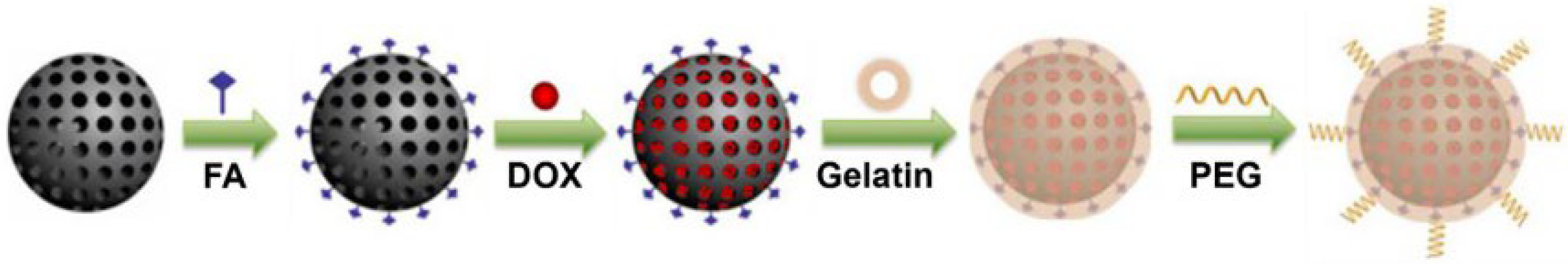
- Xu, J.-H.; Gao, F.-P.; Li, L.-L.; Ma, H.L.; Fan, Y.-S.; Liu, W.; Guo, S.-S.; Zhao, X.-Z.; Wang, H. Gelatin-Mesoporous Silica Nanoparticles as Matrix Metalloproteinases-Degradable Drug Delivery Systems in Vivo. Microporous Mesoporous Mater. 2013, 182, 165–172. [Google Scholar] [CrossRef]
- Carvalho, G.C.; Sábio, R.M.; de Cássia Ribeiro, T.; Monteiro, A.S.; Pereira, D.V.; Ribeiro, S.J.L.; Chorilli, M. Highlights in Mesoporous Silica Nanoparticles as a Multifunctional Controlled Drug Delivery Nanoplatform for Infectious Diseases Treatment. Pharm. Res. 2020, 37, 191. [Google Scholar] [CrossRef]
- Kruk, M.; Jaroniec, M.; Ko, C.H.; Ryoo, R. Characterization of the Porous Structure of SBA-15. Chem. Mater. 2000, 12, 1961–1968. [Google Scholar] [CrossRef]
- Arbenin, A.Y.; Zemtsova, E.G.; Smirnov, V.M. Regulation of the Geometric Parameters of Mesoporous Silica SBA-15 Using the Method of Molecular Layering and Investigation of Their Porous Structure. Nanotechnol. Russ. 2012, 7, 117–121. [Google Scholar] [CrossRef]
- Rivera-Muñoz, E.M.; Huirache-Acuña, R. Sol Gel-Derived SBA-16 Mesoporous Material. Int. J. Mol. Sci. 2010, 11, 3069–3086. [Google Scholar] [CrossRef]
- Luo, S.; Lutkenhaus, J.L.; Nasrabadi, H. Confinement-Induced Supercriticality and Phase Equilibria of Hydrocarbons in Nanopores. Langmuir 2016, 32, 11506–11513. [Google Scholar] [CrossRef]
- Bharti, C.; Gulati, N.; Nagaich, U.; Pal, A. Mesoporous Silica Nanoparticles in Target Drug Delivery System: A Review. Int. J. Pharm. Investig. 2015, 5, 124. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Shi, S.; Goel, S.; Shen, X.; Xie, X.; Chen, Z.; Zhang, H.; Li, S.; Qin, X.; Yang, H.; et al. Recent Advancements in Mesoporous Silica Nanoparticles towards Therapeutic Applications for Cancer. Acta Biomater. 2019, 89, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.-S.; Chang, K.L.B.; Hwang, D.-F.; Kong, Z.-L. In Vitro Cytotoxicitiy of Silica Nanoparticles at High Concentrations Strongly Depends on the Metabolic Activity Type of the Cell Line. Environ. Sci. Technol. 2007, 41, 2064–2068. [Google Scholar] [CrossRef]
- Lin, Y.-S.; Haynes, C.L. Impacts of Mesoporous Silica Nanoparticle Size, Pore Ordering, and Pore Integrity on Hemolytic Activity. J. Am. Chem. Soc. 2010, 132, 4834–4842. [Google Scholar] [CrossRef] [PubMed]
- Fisichella, M.; Dabboue, H.; Bhattacharyya, S.; Lelong, G.; Saboungi, M.-L.; Warmont, F.; Midoux, P.; Pichon, C.; Guérin, M.; Hevor, T.; et al. Uptake of Functionalized Mesoporous Silica Nanoparticles by Human Cancer Cells. J. Nanosci. Nanotechnol. 2010, 10, 2314–2324. [Google Scholar] [CrossRef]
- Zhang, G.; Gao, J.; Qian, J.; Zhang, L.; Zheng, K.; Zhong, K.; Cai, D.; Zhang, X.; Wu, Z. Hydroxylated Mesoporous Nanosilica Coated by Polyethylenimine Coupled with Gadolinium and Folic Acid: A Tumor-Targeted T-1 Magnetic Resonance Contrast Agent and Drug Delivery System. ACS Appl. Mater. Interfaces 2015, 7, 14192–14200. [Google Scholar] [CrossRef] [PubMed]
- Peng, S.; Huang, B.; Lin, Y.; Pei, G.; Zhang, L. Effect of Surface Functionalization and Pore Structure Type on the Release Performance of Mesoporous Silica Nanoparticles. Microporous Mesoporous Mater. 2022, 336, 111862. [Google Scholar] [CrossRef]
- Meng, H.; Liong, M.; Xia, T.; Li, Z.; Ji, Z.; Zink, J.I.; Nel, A.E. Engineered Design of Mesoporous Silica Nanoparticles to Deliver Doxorubicin and P-Glycoprotein SiRNA to Overcome Drug Resistance in a Cancer Cell Line. ACS Nano 2010, 4, 4539–4550. [Google Scholar] [CrossRef]
- Talavera-Pech, W.A.; Ávila-Ortega, A.; Pacheco-Catalán, D.; Quintana-Owen, P.; Barrón-Zambrano, J.A. Effect of Functionalization Synthesis Type of Amino-MCM-41 Mesoporous Silica Nanoparticles on Its RB5 Adsorption Capacity and Kinetics. Silicon 2019, 11, 1547–1555. [Google Scholar] [CrossRef]
- Narayan, R.; Gadag, S.; Garg, S.; Nayak, U.Y. Understanding the Effect of Functionalization on Loading Capacity and Release of Drug from Mesoporous Silica Nanoparticles: A Computationally Driven Study. ACS Omega 2022, 7, 8229–8245. [Google Scholar] [CrossRef] [PubMed]
- von Baeckmann, C.; Guillet-Nicolas, R.; Renfer, D.; Kählig, H.; Kleitz, F. A Toolbox for the Synthesis of Multifunctionalized Mesoporous Silica Nanoparticles for Biomedical Applications. ACS Omega 2018, 3, 17496–17510. [Google Scholar] [CrossRef]
- Yismaw, S.; Ebbinghaus, S.G.; Wenzel, M.; Poppitz, D.; Gläser, R.; Matysik, J.; Bauer, F.; Enke, D. Selective Functionalization of the Outer Surface of MCM-48-Type Mesoporous Silica Nanoparticles at Room Temperature. J. Nanoparticle Res. 2020, 22, 279. [Google Scholar] [CrossRef]
- Ghafoorzadeh, S.; Askarbioki, M.; Saniei, E.; Shirmardi, S.P.; Khakshournia, S.; Kargar, S.; Amooee, A.; Ranjbar Jamalabadi, R. Feasibility Study of Mesoporous Silica MCM-41 Functionalization by Electron-Beam Irradiation. J. Test. Eval. 2022, 50, 20200754. [Google Scholar] [CrossRef]
- Shahabi, S.; Döscher, S.; Bollhorst, T.; Treccani, L.; Maas, M.; Dringen, R.; Rezwan, K. Enhancing Cellular Uptake and Doxorubicin Delivery of Mesoporous Silica Nanoparticles via Surface Functionalization: Effects of Serum. ACS Appl. Mater. Interfaces 2015, 7, 26880–26891. [Google Scholar] [CrossRef] [PubMed]
- Ferenc, M.; Katir, N.; Milowska, K.; Bousmina, M.; Brahmi, Y.; Felczak, A.; Lisowska, K.; Bryszewska, M.; El Kadib, A. Impact of Mesoporous Silica Surface Functionalization on Human Serum Albumin Interaction, Cytotoxicity and Antibacterial Activity. Microporous Mesoporous Mater. 2016, 231, 47–56. [Google Scholar] [CrossRef]
- Laghaei, M.; Sadeghi, M.; Ghalei, B.; Dinari, M. The Effect of Various Types of Post-Synthetic Modifications on the Structure and Properties of MCM-41 Mesoporous Silica. Prog. Org. Coat. 2016, 90, 163–170. [Google Scholar] [CrossRef]
- Salis, A.; Fanti, M.; Medda, L.; Nairi, V.; Cugia, F.; Piludu, M.; Sogos, V.; Monduzzi, M. Mesoporous Silica Nanoparticles Functionalized with Hyaluronic Acid and Chitosan Biopolymers. Effect of Functionalization on Cell Internalization. ACS Biomater. Sci. Eng. 2016, 2, 741–751. [Google Scholar] [CrossRef] [PubMed]
- Fuentes, C.; Ruiz-Rico, M.; Fuentes, A.; Ruiz, M.J.; Barat, J.M. Degradation of Silica Particles Functionalised with Essential Oil Components under Simulated Physiological Conditions. J. Hazard. Mater. 2020, 399, 123120. [Google Scholar] [CrossRef] [PubMed]
- Meléndez-Ortiz, H.I.; Puente-Urbina, B.; Ibarra-Vallejo, E.; García-Uriostegui, L.; Ortega, A. Polyacrylamide-Coated MCM-48 Mesoporous Silica Spheres: Synthesis, Characterization and Drug Delivery Study. J. Porous Mater. 2018, 25, 649–656. [Google Scholar] [CrossRef]
- Alotaibi, K.M.; Almethen, A.A.; Beagan, A.M.; Alfhaid, L.H.; Ahamed, M.; El-Toni, A.M.; Alswieleh, A.M. Poly(Oligo(Ethylene Glycol) Methyl Ether Methacrylate) Capped PH-Responsive Poly(2-(Diethylamino)Ethyl Methacrylate) Brushes Grafted on Mesoporous Silica Nanoparticles as Nanocarrier. Polymers 2021, 13, 823. [Google Scholar] [CrossRef]
- Napierska, D.; Thomassen, L.C.J.; Rabolli, V.; Lison, D.; Gonzalez, L.; Kirsch-Volders, M.; Martens, J.A.; Hoet, P.H. Size-Dependent Cytotoxicity of Monodisperse Silica Nanoparticles in Human Endothelial Cells. Small 2009, 5, 846–853. [Google Scholar] [CrossRef]
- Baharifar, H.; Amani, A. Cytotoxicity of Chitosan/Streptokinase Nanoparticles as a Function of Size: An Artificial Neural Networks Study. Nanomedicine 2016, 12, 171–180. [Google Scholar] [CrossRef]
- Lee, K.; Lee, J.; Kwak, M.; Cho, Y.-L.; Hwang, B.; Cho, M.J.; Lee, N.G.; Park, J.; Lee, S.-H.; Park, J.-G.; et al. Two Distinct Cellular Pathways Leading to Endothelial Cell Cytotoxicity by Silica Nanoparticle Size. J. Nanobiotechnology 2019, 17, 24. [Google Scholar] [CrossRef] [PubMed]
- Lu, F.; Wu, S.H.; Hung, Y.; Mou, C.Y. Size Effect on Cell Uptake in Well-Suspended, Uniform Mesoporous Silica Nanoparticles. Small 2009, 5, 1408–1413. [Google Scholar] [CrossRef] [PubMed]
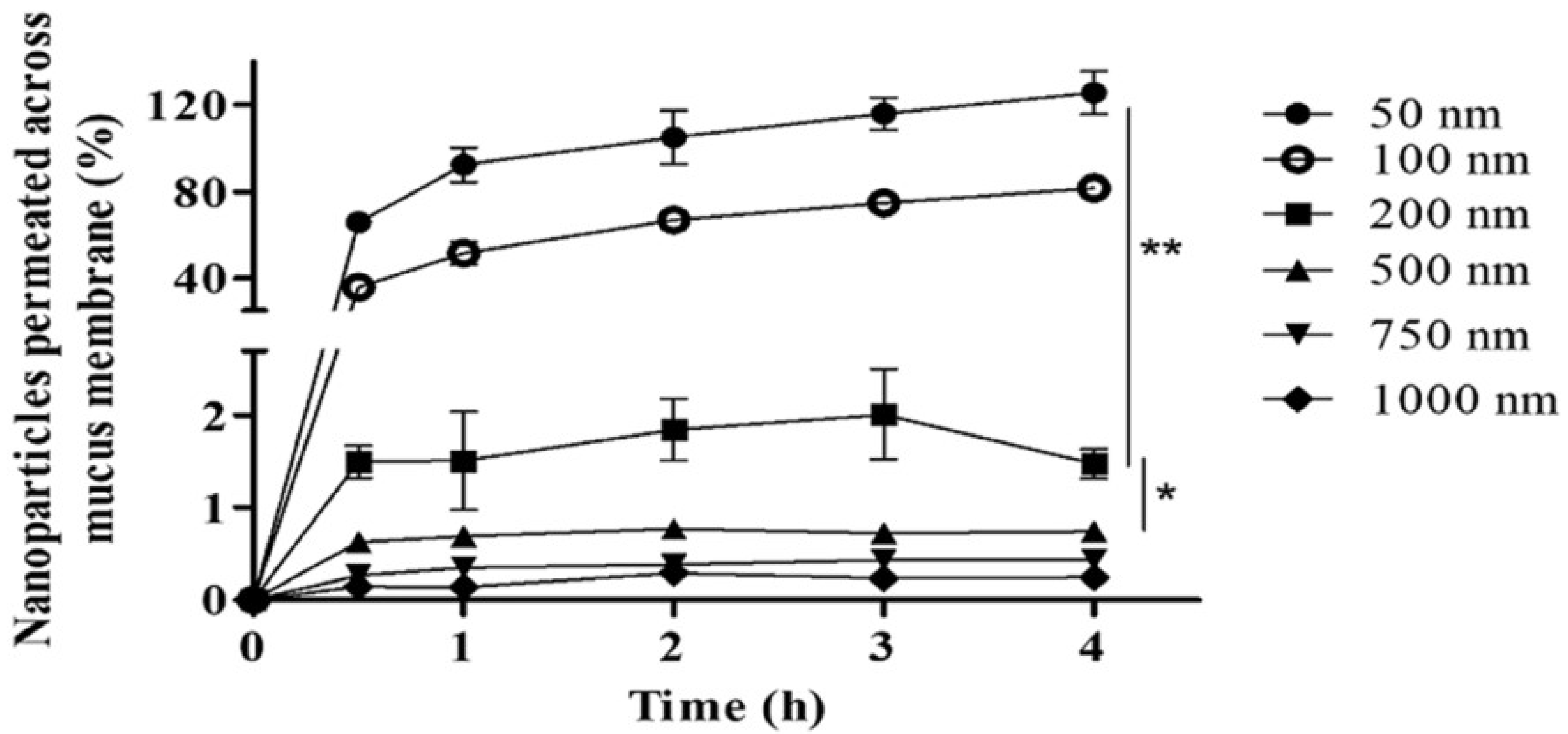
- Suen, W.-L.L.; Chau, Y. Size-Dependent Internalisation of Folate-Decorated Nanoparticles via the Pathways of Clathrin and Caveolae-Mediated Endocytosis in ARPE-19 Cells. J. Pharm. Pharmacol. 2014, 66, 564–573. [Google Scholar] [CrossRef] [PubMed]
- Bandi, S.P.; Kumbhar, Y.S.; Venuganti, V.V.K. Effect of Particle Size and Surface Charge of Nanoparticles in Penetration through Intestinal Mucus Barrier. J. Nanoparticle Res. 2020, 22, 62. [Google Scholar] [CrossRef]
- Kim, I.-Y.; Joachim, E.; Choi, H.; Kim, K. Toxicity of Silica Nanoparticles Depends on Size, Dose, and Cell Type. Nanomedicine 2015, 11, 1407–1416. [Google Scholar] [CrossRef] [PubMed]
- Shao, X.; Wei, X.; Song, X.; Hao, L.; Cai, X.; Zhang, Z.; Peng, Q.; Lin, Y. Independent Effect of Polymeric Nanoparticle Zeta Potential/Surface Charge, on Their Cytotoxicity and Affinity to Cells. Cell Prolif. 2015, 48, 465–474. [Google Scholar] [CrossRef] [PubMed]
- Tarn, D.; Ashley, C.E.; Xue, M.; Carnes, E.C.; Zink, J.I.; Brinker, C.J. Mesoporous Silica Nanoparticle Nanocarriers: Biofunctionality and Biocompatibility. Acc. Chem. Res. 2013, 46, 792–801. [Google Scholar] [CrossRef] [PubMed]
- Pada, A.-K.; Desai, D.; Sun, K.; Govardhanam, N.P.; Tornquist, K.; Zhang, J.; Rosenholm, J.M. Comparison of Polydopamine-Coated Mesoporous Silica Nanorods and Spheres for the Delivery of Hydrophilic and Hydrophobic Anticancer Drugs. Int. J. Mol. Sci. 2019, 20, 3408. [Google Scholar] [CrossRef]
- Tang, F.; Li, L.; Chen, D. Mesoporous Silica Nanoparticles: Synthesis, Biocompatibility and Drug Delivery. Adv. Mater. 2012, 24, 1504–1534. [Google Scholar] [CrossRef] [PubMed]
- Xie, Z.; Gong, H.; Liu, M.; Zhu, H.; Sun, H. The Properties of Mesoporous Silica Nanoparticles Functionalized with Different PEG-Chain Length via the Disulfide Bond Linker and Drug Release in Glutathione Medium. J. Biomater. Sci. Polym. Ed. 2016, 27, 55–68. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.H.; Tran, D.L.; Truong-Thi, N.; Nguyen, C.K.; Tran, C.T.; Nguyen, D.H. Simply and Effectively Control the Shell Thickness of Hollow Mesoporous Silica Nanoparticles by Polyethylene Glycol for Drug Delivery Applications. J. Appl. Polym. Sci. 2022, 139, e53126. [Google Scholar] [CrossRef]
- Hatakeyama, H.; Akita, H.; Harashima, H. A Multifunctional Envelope Type Nano Device (MEND) for Gene Delivery to Tumours Based on the EPR Effect: A Strategy for Overcoming the PEG Dilemma. Adv. Drug Deliv. Rev. 2011, 63, 152–160. [Google Scholar] [CrossRef] [PubMed]
- Kramer, L.; Winter, G.; Baur, B.; Kuntz, A.J.; Kull, T.; Solbach, C.; Beer, A.J.; Lindén, M. Quantitative and Correlative Biodistribution Analysis of 89 Zr-Labeled Mesoporous Silica Nanoparticles Intravenously Injected into Tumor-Bearing Mice. Nanoscale 2017, 9, 9743–9753. [Google Scholar] [CrossRef] [PubMed]
- Zou, Z.; He, X.; He, D.; Wang, K.; Qing, Z.; Yang, X.; Wen, L.; Xiong, J.; Li, L.; Cai, L. Programmed Packaging of Mesoporous Silica Nanocarriers for Matrix Metalloprotease 2-Triggered Tumor Targeting and Release. Biomaterials 2015, 58, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.; Karambelkar, A.; Gu, L.; Lin, K.; Miller, J.S.; Chen, C.S.; Sailor, M.J.; Bhatia, S.N. Bioresponsive Mesoporous Silica Nanoparticles for Triggered Drug Release. J. Am. Chem. Soc. 2011, 133, 19582–19585. [Google Scholar] [CrossRef] [PubMed]
- Trendafilova, I.; Szegedi, A.; Yoncheva, K.; Shestakova, P.; Mihaly, J.; Ristic, A.; Konstantinov, S.; Popova, M. A PH Dependent Delivery of Mesalazine from Polymer Coated and Drug-Loaded SBA-16 Systems. Eur. J. Pharm. Sci. 2016, 81, 75–81. [Google Scholar] [CrossRef]
- Tzankov, B.; Tzankova, V.; Aluani, D.; Yordanov, Y.; Spassova, I.; Kovacheva, D.; Avramova, K.; Valoti, M.; Yoncheva, K. Development of MCM-41 Mesoporous Silica Nanoparticles as a Platform for Pramipexole Delivery. J. Drug Deliv. Sci. Technol. 2019, 51, 26–35. [Google Scholar] [CrossRef]
- Meng, H.; Xue, M.; Xia, T.; Ji, Z.; Tarn, D.Y.; Zink, J.I.; Nel, A.E. Use of Size and a Copolymer Design Feature To Improve the Biodistribution and the Enhanced Permeability and Retention Effect of Doxorubicin-Loaded Mesoporous Silica Nanoparticles in a Murine Xenograft Tumor Model. ACS Nano 2011, 5, 4131–4144. [Google Scholar] [CrossRef] [PubMed]
- Hanafi-Bojd, M.Y.; Jaafari, M.R.; Ramezanian, N.; Abnous, K.; Malaekeh-Nikouei, B. Co-Delivery of Epirubicin and SiRNA Using Functionalized Mesoporous Silica Nanoparticles Enhances In Vitro and In Vivo Drug Efficacy. Curr. Drug Deliv. 2016, 13, 1176–1182. [Google Scholar] [CrossRef] [PubMed]
- Pourjavadi, A.; Tehrani, Z.M. Mesoporous Silica Nanoparticles with Bilayer Coating of Poly(Acrylic Acid-Co-Itaconic Acid) and Human Serum Albumin (HSA): A PH-Sensitive Carrier for Gemcitabine Delivery. Mater. Sci. Eng. C 2016, 61, 782–790. [Google Scholar] [CrossRef]
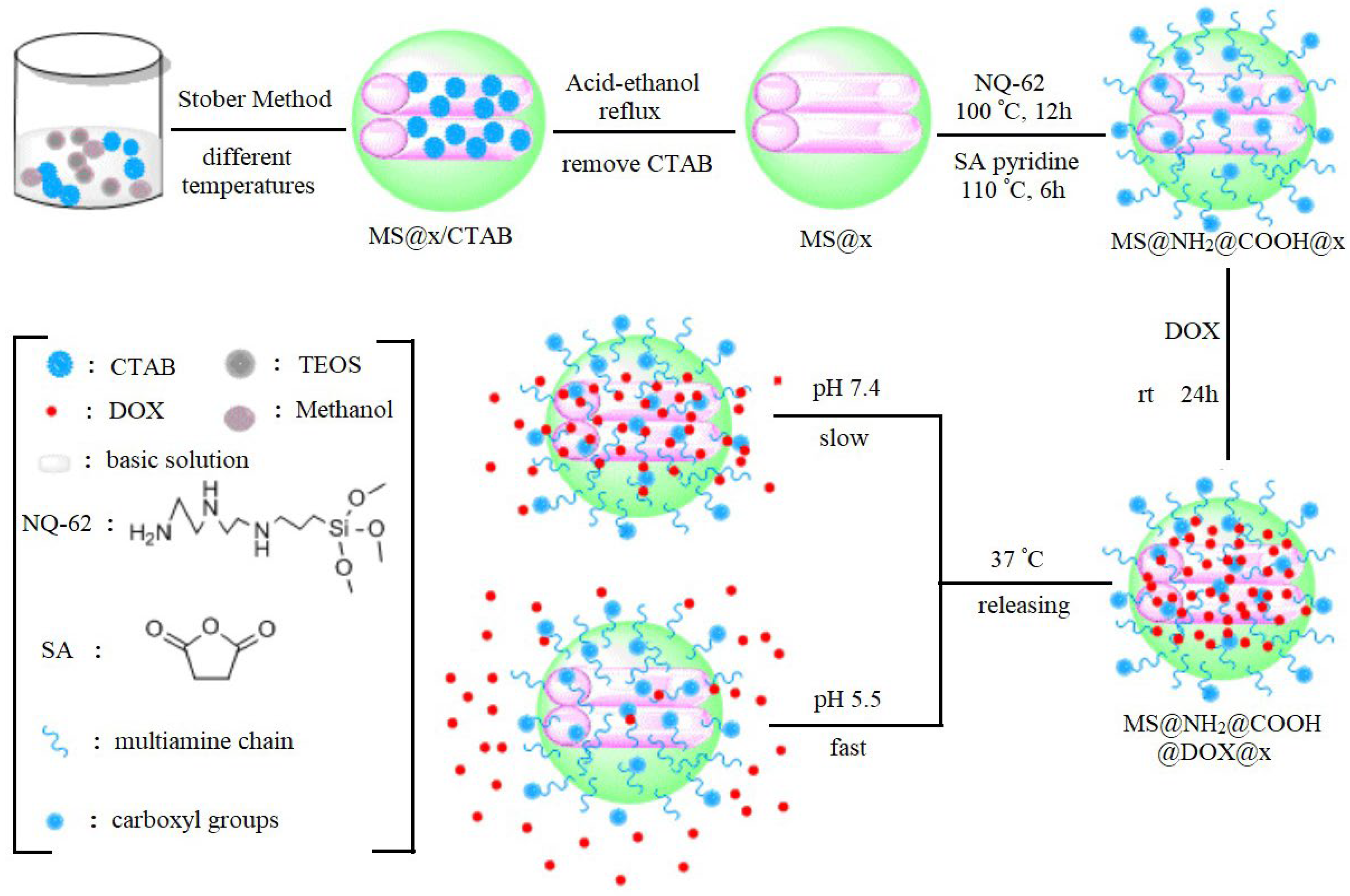
- Wang, S.; Song, F.X.; Zhang, L.; Zhang, X.; Li, Y. Organic Functionalization of Mesoporous Silica Spheres as a Nanovehicle for DOX PH-Triggered Delivery. Nano 2019, 14, 1950094. [Google Scholar] [CrossRef]
- Park, S.S.; Jung, M.H.; Lee, Y.-S.; Bae, J.-H.; Kim, S.-H.; Ha, C.-S. Functionalised Mesoporous Silica Nanoparticles with Excellent Cytotoxicity against Various Cancer Cells for PH-Responsive and Controlled Drug Delivery. Mater. Des. 2019, 184, 108187. [Google Scholar] [CrossRef]
- Ortiz-Islas, E.; Sosa-Arróniz, A.; Manríquez-Ramírez, M.E.; Rodríguez-Pérez, C.E.; Tzompantzi, F.; Padilla, J.M. Mesoporous Silica Nanoparticles Functionalized with Folic Acid for Targeted Release Cis-Pt to Glioblastoma Cells. Rev. Adv. Mater. Sci. 2021, 60, 25–37. [Google Scholar] [CrossRef]
- Kumar, H.; Kumar, J.; Pani, B.; Kumar, P. Multifunctional Folic Acid-coated and Doxorubicin Encapsulated Mesoporous Silica Nanocomposites (FA/DOX@Silica) for Cancer Therapeutics, Bioimaging and Invitro Studies. ChemistrySelect 2022, 7, e202203113. [Google Scholar] [CrossRef]
- Pham, S.H.; Choi, Y.; Choi, J. Stimuli-Responsive Nanomaterials for Application in Antitumor Therapy and Drug Delivery. Pharmaceutics 2020, 12, 630. [Google Scholar] [CrossRef]
- Pourjavadi, A.; Tehrani, Z.M. Mesoporous Silica Nanoparticles (MCM-41) Coated PEGylated Chitosan as a PH-Responsive Nanocarrier for Triggered Release of Erythromycin. Int. J. Polym. Mater. Polym. Biomater. 2014, 63, 692–697. [Google Scholar] [CrossRef]
- Yang, K.; Luo, H.; Zeng, M.; Jiang, Y.; Li, J.; Fu, X. Intracellular PH-Triggered, Targeted Drug Delivery to Cancer Cells by Multifunctional Envelope-Type Mesoporous Silica Nanocontainers. ACS Appl. Mater. Interfaces 2015, 7, 17399–17407. [Google Scholar] [CrossRef]
- Porrang, S.; Rahemi, N.; Davaran, S.; Mahdavi, M.; Hassanzadeh, B. Synthesis of Temperature/PH Dual-Responsive Mesoporous Silica Nanoparticles by Surface Modification and Radical Polymerization for Anti-Cancer Drug Delivery. Colloids Surf. A Physicochem. Eng. Asp. 2021, 623, 126719. [Google Scholar] [CrossRef]
- Thirupathi, K.; Santhamoorthy, M.; Radhakrishnan, S.; Ulagesan, S.; Nam, T.-J.; Phan, T.T.V.; Kim, S.-C. Thermosensitive Polymer-Modified Mesoporous Silica for PH and Temperature-Responsive Drug Delivery. Pharmaceutics 2023, 15, 795. [Google Scholar] [CrossRef]
- Keldibekova, R.; Suleimenova, S.; Nurgozhina, G.; Kopishev, E. Interpolymer Complexes Based on Cellulose Ethers: Application. Polymers 2023, 15, 3326. [Google Scholar] [CrossRef]
- Budtova, T.; Suleimenov, I. Swelling Behaviour of a Polyelectrolyte Network under Load. Polymer 1997, 38, 5947–5951. [Google Scholar] [CrossRef]
- Zheng, Q.; Lin, T.; Wu, H.; Guo, L.; Ye, P.; Hao, Y.; Guo, Q.; Jiang, J.; Fu, F.; Chen, G. Mussel-Inspired Polydopamine Coated Mesoporous Silica Nanoparticles as PH-Sensitive Nanocarriers for Controlled Release. Int. J. Pharm. 2014, 463, 22–26. [Google Scholar] [CrossRef]
- Peng, H.; Dong, R.; Wang, S.; Zhang, Z.; Luo, M.; Bai, C.; Zhao, Q.; Li, J.; Chen, L.; Xiong, H. A PH-Responsive Nano-Carrier with Mesoporous Silica Nanoparticles Cores and Poly(Acrylic Acid) Shell-Layers: Fabrication, Characterization and Properties for Controlled Release of Salidroside. Int. J. Pharm. 2013, 446, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Chang, B.; Sha, X.; Guo, J.; Jiao, Y.; Wang, C.; Yang, W. Thermo and PH Dual Responsive, Polymer Shell Coated, Magnetic Mesoporous Silica Nanoparticles for Controlled Drug Release. J. Mater. Chem. 2011, 21, 9239–9247. [Google Scholar] [CrossRef]
- Chen, Y.; Yang, W.; Chang, B.; Hu, H.; Fang, X.; Sha, X. In Vivo Distribution and Antitumor Activity of Doxorubicin-Loaded N-Isopropylacrylamide-Co-Methacrylic Acid Coated Mesoporous Silica Nanoparticles and Safety Evaluation. Eur. J. Pharm. Biopharm. 2013, 85, 406–412. [Google Scholar] [CrossRef]
- Tian, Z.; Yu, X.; Ruan, Z.; Zhu, M.; Zhu, Y.; Hanagata, N. Magnetic Mesoporous Silica Nanoparticles Coated with Thermo-Responsive Copolymer for Potential Chemo- and Magnetic Hyperthermia Therapy. Microporous Mesoporous Mater. 2018, 256, 1–9. [Google Scholar] [CrossRef]
- Shu, Y.; Song, R.; Zheng, A.; Huang, J.; Chen, M.; Wang, J. Thermo/PH Dual-Stimuli-Responsive Drug Delivery for Chemo-/Photothermal Therapy Monitored by Cell Imaging. Talanta 2018, 181, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Li, Q.; Zhang, J.; Huang, L.; Qi, C.; Xu, L.; Liu, X.; Wang, G.; Wang, L.; Wang, Z. Safe and Effective Reversal of Cancer Multidrug Resistance Using Sericin-Coated Mesoporous Silica Nanoparticles for Lysosome-Targeting Delivery in Mice. Small 2017, 13, 1602567. [Google Scholar] [CrossRef]
- Zou, Z.; He, D.; He, X.; Wang, K.; Yang, X.; Qing, Z.; Zhou, Q. Natural Gelatin Capped Mesoporous Silica Nanoparticles for Intracellular Acid-Triggered Drug Delivery. Langmuir 2013, 29, 12804–12810. [Google Scholar] [CrossRef]
- Martínez-Carmona, M.; Lozano, D.; Colilla, M.; Vallet-Regí, M. Selective Topotecan Delivery to Cancer Cells by Targeted PH-Sensitive Mesoporous Silica Nanoparticles. RSC Adv. 2016, 6, 50923–50932. [Google Scholar] [CrossRef]
- Vo, U.V.; Nguyen, V.C.; Vo, X.V.D.; Vo, M.K.T.; Pham, H.A.L.; Tran, T.T.N.; Nguyen, D.H.; Nguyen, C.K. Synthesize and Survey the Drug Loading Efficiency of the Porous Nano Silica Modified by Gelatin. Adv. Nat. Sci. Nanosci. Nanotechnol. 2019, 10, 035017. [Google Scholar] [CrossRef]
- Li, X.; Xie, C.; Xia, H.; Wang, Z. PH and Ultrasound Dual-Responsive Polydopamine-Coated Mesoporous Silica Nanoparticles for Controlled Drug Delivery. Langmuir 2018, 34, 9974–9981. [Google Scholar] [CrossRef]
- Zhao, X.; Zhao, J.; Lin, Z.Y.W.; Pan, G.; Zhu, Y.; Cheng, Y.; Cui, W. Self-Coated Interfacial Layer at Organic/Inorganic Phase for Temporally Controlling Dual-Drug Delivery from Electrospun Fibers. Colloids Surf. B Biointerfaces 2015, 130, 1–9. [Google Scholar] [CrossRef]
- Duo, Y.; Li, Y.; Chen, C.; Liu, B.; Wang, X.; Zeng, X.; Chen, H. DOX-Loaded PH-Sensitive Mesoporous Silica Nanoparticles Coated with PDA and PEG Induce pro-Death Autophagy in Breast Cancer. RSC Adv. 2017, 7, 39641–39650. [Google Scholar] [CrossRef]
- Li, X.; Garamus, V.M.; Li, N.; Gong, Y.; Zhe, Z.; Tian, Z.; Zou, A. Preparation and Characterization of a PH-Responsive Mesoporous Silica Nanoparticle Dual-Modified with Biopolymers. Colloids Surf. A Physicochem. Eng. Asp. 2018, 548, 61–69. [Google Scholar] [CrossRef]
- Wang, X.; Du, J.; Zhou, F.; Ye, Q.; Chen, Y.; Sun, D.; Chen, H.; Lv, Y.; Sun, X. Enhanced Nuclear Accumulation of Doxorubicin Delivered by PH-Triggered Polydopamine-Shelled Mesoporous Silica for Chemo-Photothermal Therapy. AAPS PharmSciTech 2022, 24, 3. [Google Scholar] [CrossRef] [PubMed]
- Hou, J.; Guo, C.; Shi, Y.; Liu, E.; Dong, W.; Yu, B.; Liu, S.; Gong, J. A Novel High Drug Loading Mussel-Inspired Polydopamine Hybrid Nanoparticle as a PH-Sensitive Vehicle for Drug Delivery. Int. J. Pharm. 2017, 533, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Cheng, W.; Nie, J.; Xu, L.; Liang, C.; Peng, Y.; Liu, G.; Wang, T.; Mei, L.; Huang, L.; Zeng, X. PH-Sensitive Delivery Vehicle Based on Folic Acid-Conjugated Polydopamine-Modified Mesoporous Silica Nanoparticles for Targeted Cancer Therapy. ACS Appl. Mater. Interfaces 2017, 9, 18462–18473. [Google Scholar] [CrossRef] [PubMed]
- Feng, W.; Nie, W.; He, C.; Zhou, X.; Chen, L.; Qiu, K.; Wang, W.; Yin, Z. Effect of PH-Responsive Alginate/Chitosan Multilayers Coating on Delivery Efficiency, Cellular Uptake and Biodistribution of Mesoporous Silica Nanoparticles Based Nanocarriers. ACS Appl. Mater. Interfaces 2014, 6, 8447–8460. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Lü, S.; Gao, C.; Bai, X.; Feng, C.; Gao, N.; Liu, M. Multifunctional Drug Carriers Comprised of Mesoporous Silica Nanoparticles and Polyamidoamine Dendrimers Based on Layer-by-Layer Assembly. Mater. Des. 2015, 88, 1127–1133. [Google Scholar] [CrossRef]
- Gong, H.; Xie, Z.; Liu, M.; Zhu, H.; Sun, H. Redox-Sensitive Mesoporous Silica Nanoparticles Functionalized with PEG through a Disulfide Bond Linker for Potential Anticancer Drug Delivery. RSC Adv. 2015, 5, 59576–59582. [Google Scholar] [CrossRef]
- Chen, X.; Sun, H.; Hu, J.; Han, X.; Liu, H.; Hu, Y. Transferrin Gated Mesoporous Silica Nanoparticles for Redox-Responsive and Targeted Drug Delivery. Colloids Surf. B Biointerfaces 2017, 152, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Zhang, Y.; Ma, Y. Construction of a Redox-Responsive Drug Delivery System Utilizing the Volume of AS1411 Spatial Configuration Gating Mesoporous Silica Pores. Nanoscale Adv. 2022, 4, 4059–4065. [Google Scholar] [CrossRef]
- Lin, J.-T.; Liu, Z.-K.; Zhu, Q.-L.; Rong, X.-H.; Liang, C.-L.; Wang, J.; Ma, D.; Sun, J.; Wang, G.-H. Redox-Responsive Nanocarriers for Drug and Gene Co-Delivery Based on Chitosan Derivatives Modified Mesoporous Silica Nanoparticles. Colloids Surf. B Biointerfaces 2017, 155, 41–50. [Google Scholar] [CrossRef]
- Cui, Y.; Dong, H.; Cai, X.; Wang, D.; Li, Y. Mesoporous Silica Nanoparticles Capped with Disulfide-Linked PEG Gatekeepers for Glutathione-Mediated Controlled Release. ACS Appl. Mater. Interfaces 2012, 4, 3177–3183. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Luo, Z.; Liu, J.; Ding, X.; Li, J.; Cai, K. Cytochrome c End-Capped Mesoporous Silica Nanoparticles as Redox-Responsive Drug Delivery Vehicles for Liver Tumor-Targeted Triplex Therapy in Vitro and in Vivo. J. Control. Release 2014, 192, 192–201. [Google Scholar] [CrossRef] [PubMed]
- Yan, J.; Xu, X.; Zhou, J.; Liu, C.; Zhang, L.; Wang, D.; Yang, F.; Zhang, H. Fabrication of a PH/Redox-Triggered Mesoporous Silica-Based Nanoparticle with Microfluidics for Anticancer Drugs Doxorubicin and Paclitaxel Codelivery. ACS Appl. Bio Mater. 2020, 3, 1216–1225. [Google Scholar] [CrossRef]
- Zhang, Y.; Xing, Y.; Xian, M.; Shuang, S.; Dong, C. Folate-Targeting and Bovine Serum Albumin-Gated Mesoporous Silica Nanoparticles as a Redox-Responsive Carrier for Epirubicin Release. New J. Chem. 2019, 43, 2694–2701. [Google Scholar] [CrossRef]
- Li, L.; Lan, S.; Ma, D. Ultrastable and Versatile Layer-by-Layer Coating Based on Kinetically Trapped Host-Guest Complexation for Mesoporous Silica Nanoparticles. Part. Part. Syst. Charact. 2020, 37, 2000075. [Google Scholar] [CrossRef]
- Che, E.; Gao, Y.; Wan, L.; Zhang, Y.; Han, N.; Bai, J.; Li, J.; Sha, Z.; Wang, S. Paclitaxel/Gelatin Coated Magnetic Mesoporous Silica Nanoparticles: Preparation and Antitumor Efficacy in Vivo. Microporous Mesoporous Mater. 2015, 204, 226–234. [Google Scholar] [CrossRef]
- Xu, X.; Wu, C.; Bai, A.; Liu, X.; Lv, H.; Liu, Y. Folate-Functionalized Mesoporous Silica Nanoparticles as a Liver Tumor-Targeted Drug Delivery System to Improve the Antitumor Effect of Paclitaxel. J. Nanomater. 2017, 2017, 2069685. [Google Scholar] [CrossRef]
- Zhao, Q.; Wang, Y.; Zhang, W.; Wang, Y.; Wang, S. Succinylated Casein Functionalized Mesoporous Silica Nanoplatforms to Overcome Multiple Gastrointestinal Barriers. J. Drug Deliv. Sci. Technol. 2020, 60, 102068. [Google Scholar] [CrossRef]
- Malfanti, A.; Miletto, I.; Bottinelli, E.; Zonari, D.; Blandino, G.; Berlier, G.; Arpicco, S. Delivery of Gemcitabine Prodrugs Employing Mesoporous Silica Nanoparticles. Molecules 2016, 21, 522. [Google Scholar] [CrossRef]
- Saini, K.; Prabhuraj, R.S.; Bandyopadhyaya, R. Development of Mesoporous Silica Nanoparticles of Tunable Pore Diameter for Superior Gemcitabine Drug Delivery in Pancreatic Cancer Cells. J. Nanosci. Nanotechnol. 2020, 20, 3084–3096. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, A.; Murayama, S.; Karasawa, K.; Yamamoto, E.; Morikawa, S.; Takita, R.; Murata, S.; Kato, M. A Simple and Easy Method of Monitoring Doxorubicin Release from a Liposomal Drug Formulation in the Serum Using Fluorescence Spectroscopy. Chem. Pharm. Bull. 2019, 67, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Wu, T.; Kong, J.-L. In Situ Monitoring of Intracellular Controlled Drug Release from Mesoporous Silica Nanoparticles Coated with PH-Responsive Charge-Reversal Polymer. ACS Appl. Mater. Interfaces 2014, 6, 17446–17453. [Google Scholar] [CrossRef]
- Tang, H.; Guo, J.; Sun, Y.; Chang, B.; Ren, Q.; Yang, W. Facile Synthesis of PH Sensitive Polymer-Coated Mesoporous Silica Nanoparticles and Their Application in Drug Delivery. Int. J. Pharm. 2011, 421, 388–396. [Google Scholar] [CrossRef] [PubMed]
- Fang, W.; Wang, Z.; Zong, S.; Chen, H.; Zhu, D.; Zhong, Y.; Cui, Y. PH-Controllable Drug Carrier with SERS Activity for Targeting Cancer Cells. Biosens. Bioelectron. 2014, 57, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Chang, B.; Chen, D.; Wang, Y.; Chen, Y.; Jiao, Y.; Sha, X.; Yang, W. Bioresponsive Controlled Drug Release Based on Mesoporous Silica Nanoparticles Coated with Reductively Sheddable Polymer Shell. Chem. Mater. 2013, 25, 574–585. [Google Scholar] [CrossRef]
- Sun, J.-T.; Piao, J.-G.; Wang, L.-H.; Javed, M.; Hong, C.-Y.; Pan, C.-Y. One-Pot Synthesis of Redox-Responsive Polymers-Coated Mesoporous Silica Nanoparticles and Their Controlled Drug Release. Macromol. Rapid Commun. 2013, 34, 1387–1394. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.-L.; Sun, Y.; Sun, Y.-L.; Wen, J.; Zhou, Y.; Bing, Q.-M.; Isaacs, L.D.; Jin, Y.; Gao, H.; Yang, Y.-W. Mesoporous Silica Nanoparticles Coated by Layer-by-Layer Self-Assembly Using Cucurbit{[}7]Uril for in Vitro and in Vivo Anticancer Drug Release. Chem. Mater. 2014, 26, 6418–6431. [Google Scholar] [CrossRef]
- Ma, M.; Zheng, S.; Chen, H.; Yao, M.; Zhang, K.; Jia, X.; Mou, J.; Xu, H.; Wu, R.; Shi, J. A Combined “RAFT” and “Graft From” Polymerization Strategy for Surface Modification of Mesoporous Silica Nanoparticles: Towards Enhanced Tumor Accumulation and Cancer Therapy Efficacy. J. Mater. Chem. B 2014, 2, 5828–5836. [Google Scholar] [CrossRef]
- Guo, W.; Yang, C.; Lin, H.; Qu, F. P(EO-Co-LLA) Functionalized Fe3O4@mSiO(2) Nanocomposites for Thermo/PH Responsive Drug Controlled Release and Hyperthermia. Dalton Trans. 2014, 43, 18056–18065. [Google Scholar] [CrossRef]
- Pourjavadi, A.; Tehrani, Z.M.; Bennett, C. PEG-Co-Polyvinyl Pyridine Coated Magnetic Mesoporous Silica Nanoparticles for PH-Responsive Controlled Release of Doxorubicin. Int. J. Polym. Mater. Polym. Biomater. 2015, 64, 570–577. [Google Scholar] [CrossRef]
- Bafkary, R.; Ahmadi, S.; Fayazi, F.; Karimi, M.; Fatahi, Y.; Ebrahimi, S.M.; Atyabi, F.; Dinarvand, R. Amphiphilic Hyperbranched Polyester Coated Rod Mesoporous Silica Nanoparticles for PH-Responsive Doxorubicin Delivery. Daru-J. Pharm. Sci. 2020, 28, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Dabbagh, A.; Abdullah, B.J.J.; Abu Kasim, N.H.; Abdullah, H.; Hamdi, M. A New Mechanism of Thermal Sensitivity for Rapid Drug Release and Low Systemic Toxicity in Hyperthermia and Thermal Ablation Temperature Ranges. Int. J. Hyperth. 2015, 31, 375–385. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ang, C.Y.; Li, M.; Tan, S.Y.; Qu, Q.; Luo, Z.; Zhao, Y. Polymer-Coated Hollow Mesoporous Silica Nanoparticles for Triple-Responsive Drug Delivery. ACS Appl. Mater. Interfaces 2015, 7, 18179–18187. [Google Scholar] [CrossRef] [PubMed]
- Hakeem, A.; Zahid, F.; Zhan, G.; Yi, P.; Yang, H.; Gan, L.; Yang, X. Polyaspartic Acid-Anchored Mesoporous Silica Nanoparticles for PH-Responsive Doxorubicin Release. Int. J. Nanomed. 2018, 13, 1029–1040. [Google Scholar] [CrossRef] [PubMed]
- Tonbul, H.; Sahin, A.; Tavukcuoglu, E.; Ultav, G.; Akbas, S.; Aktas, Y.; Esendaglı, G.; Capan, Y. Folic Acid Decoration of Mesoporous Silica Nanoparticles to Increase Cellular Uptake and Cytotoxic Activity of Doxorubicin in Human Breast Cancer Cells. J. Drug Deliv. Sci. Technol. 2021, 63, 102535. [Google Scholar] [CrossRef]
- Qi, S.-S.; Sun, J.-H.; Yu, H.-H.; Yu, S.-Q. Co-Delivery Nanoparticles of Anti-Cancer Drugs for Improving Chemotherapy Efficacy. Drug Deliv. 2017, 24, 1909–1926. [Google Scholar] [CrossRef] [PubMed]
- Moodley, T.; Singh, M. Polymeric Mesoporous Silica Nanoparticles for Combination Drug Delivery In Vitro. Biointerface Res. Appl. Chem. 2021, 11, 11905–11919. [Google Scholar] [CrossRef]
- Meng, H.; Wang, M.; Liu, H.; Liu, X.; Situ, A.; Wu, B.; Ji, Z.; Chang, C.H.; Nel, A.E. Use of a Lipid-Coated Mesoporous Silica Nanoparticle Platform for Synergistic Gemcitabine and Paclitaxel Delivery to Human Pancreatic Cancer in Mice. ACS Nano 2015, 9, 3540–3557. [Google Scholar] [CrossRef] [PubMed]
- Vivero-Escoto, J.; Elnagheeb, M. Mesoporous Silica Nanoparticles Loaded with Cisplatin and Phthalocyanine for Combination Chemotherapy and Photodynamic Therapy in Vitro. Nanomaterials 2015, 5, 2302–2316. [Google Scholar] [CrossRef] [PubMed]
- Zarkesh, K.; Heidari, R.; Iranpour, P.; Azarpira, N.; Ahmadi, F.; Mohammadi-Samani, S.; Farjadian, F. Theranostic Hyaluronan Coated EDTA Modified Magnetic Mesoporous Silica Nanoparticles for Targeted Delivery of Cisplatin. J. Drug Deliv. Sci. Technol. 2022, 77, 103903. [Google Scholar] [CrossRef]
- Mu, S.; Liu, Y.; Wang, T.; Zhang, J.; Jiang, D.; Yu, X.; Zhang, N. Unsaturated Nitrogen-Rich Polymer Poly(l-Histidine) Gated Reversibly Switchable Mesoporous Silica Nanoparticles Using “Graft to” Strategy for Drug Controlled Release. Acta Biomater. 2017, 63, 150–162. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.-Y.; Yin, Y.-F.; Guo, Y.; Li, H.; Xu, M.-Q.; Liu, M.; Wang, J.-R.; Feng, Z.-H.; Duan, X.-C.; Zhang, S.; et al. Enhancing Anti-Tumor Activity of Sorafenib Mesoporous Silica Nanomatrix in Metastatic Breast Tumor and Hepatocellular Carcinoma via the Co-Administration with Flufenamic Acid. Int. J. Nanomed. 2020, 15, 1809–1821. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Tang, M.; Huang, Q.; Zhao, G.; Huang, N.; Zhang, X.; Tan, Y.; Cheng, Y. Combination of 3-Methyladenine Therapy and Asn-Gly-Arg (NGR)-Modified Mesoporous Silica Nanoparticles Loaded with Temozolomide for Glioma Therapy in Vitro. Biochem. Biophys. Res. Commun. 2019, 509, 549–556. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Cao, F.; Zhang, J.; Tan, Y.; Yao, S. Temozolomide and Chloroquine Co-Loaded Mesoporous Silica Nanoparticles Are Effective against Glioma. Heliyon 2023, 9, e18490. [Google Scholar] [CrossRef]
- Šuleková, M.; Váhovská, L.; Hudák, A.; Žid, L.; Zeleňák, V. A Study of 5-Fluorouracil Desorption from Mesoporous Silica by RP-UHPLC. Molecules 2019, 24, 1317. [Google Scholar] [CrossRef]
- Li, S.; Dai, W.; Yin, Z.-Z.; Gao, J.; Wu, D.; Kong, Y. Synthesis of Oxidized Pullulan Coated Mesoporous Silica for PH-Sensitive Drug Delivery. Eur. Polym. J. 2020, 122, 109399. [Google Scholar] [CrossRef]
- Narayan, R.; Gadag, S.; Mudakavi, R.J.; Garg, S.; Raichur, A.M.; Nayak, Y.; Kini, S.G.; Pai, K.S.R.; Nayak, U.Y. Mesoporous Silica Nanoparticles Capped with Chitosan-Glucuronic Acid Conjugate for PH-Responsive Targeted Delivery of 5-Fluorouracil. J. Drug Deliv. Sci. Technol. 2021, 63, 102472. [Google Scholar] [CrossRef]
- Liu, X.; Situ, A.; Kang, Y.; Villabroza, K.R.; Liao, Y.; Chang, C.H.; Donahue, T.; Nel, A.E.; Meng, H. Irinotecan Delivery by Lipid-Coated Mesoporous Silica Nanoparticles Shows Improved Efficacy and Safety over Liposomes for Pancreatic Cancer. ACS Nano 2016, 10, 2702–2715. [Google Scholar] [CrossRef] [PubMed]
- Brezoiu, A.-M.; Prelipcean, A.-M.; Lincu, D.; Deaconu, M.; Vasile, E.; Tatia, R.; Seciu-Grama, A.-M.; Matei, C.; Berger, D. Nanoplatforms for Irinotecan Delivery Based on Mesoporous Silica Modified with a Natural Polysaccharide. Materials 2022, 15, 7003. [Google Scholar] [CrossRef] [PubMed]
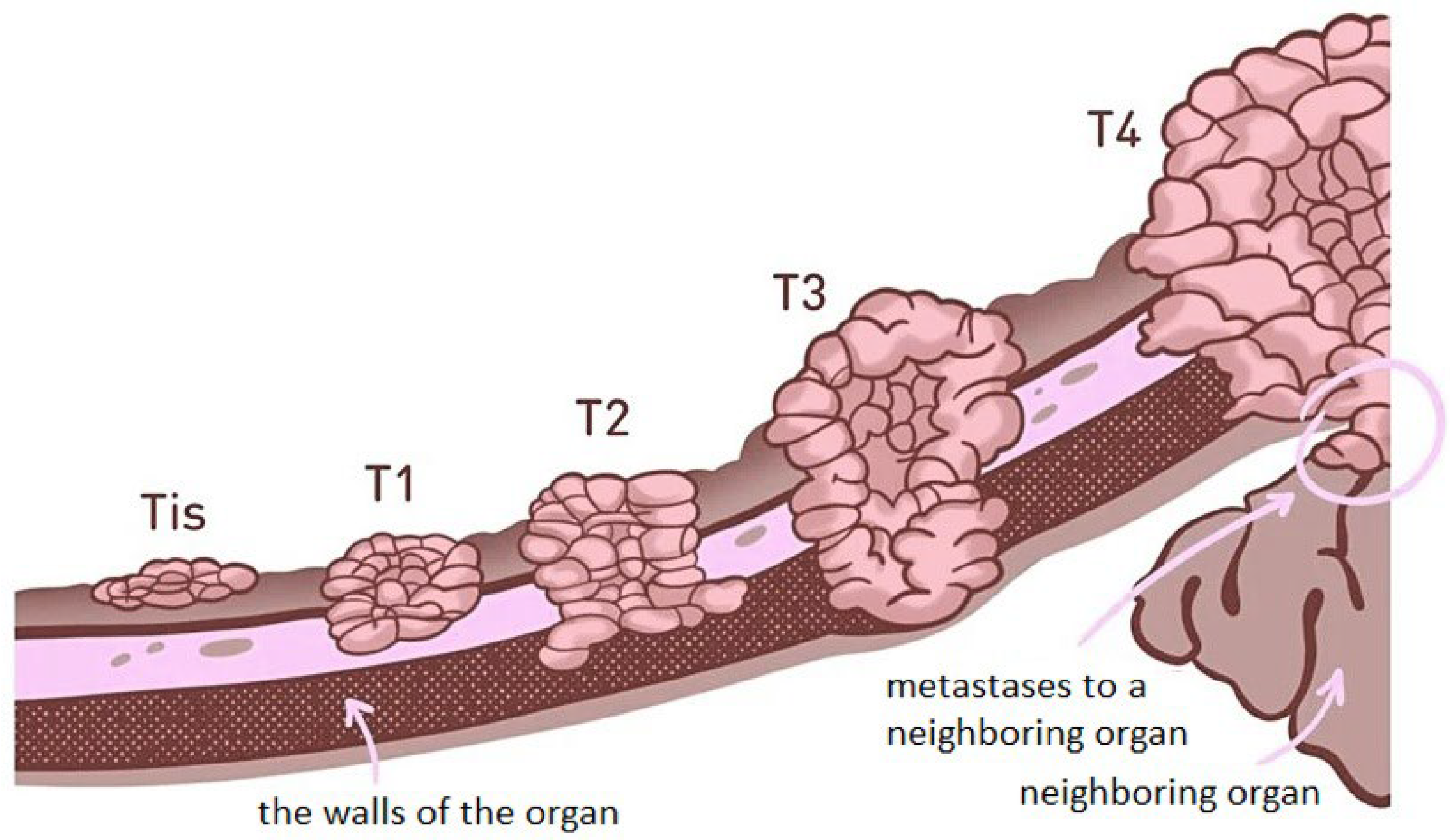



| Stage of Development | Stage 0 (Tis) | Stage I (T1) | Stage II (T2) | Stage III (T3) | Stage IV (T4) |
|---|---|---|---|---|---|
| Localisation | Cancer is in place (in situ), does not manifest itself in any way, does not form vessels for its supply | Tumour measures up to 2 cm, localised, not extending outside the wall | 2 to 5 cm tumour, extends beyond the wall, lymphatic involvement | Tumour measures more than 5 cm, is growing into surrounding tissues, multiple lymph node involvement | Tumour of any size, locally spreading, sprouting into surrounding tissues and organs |
| Surgical option | not recommended | operable | operable | mission-capable | inoperable |
| Metastasis | none | none | none | none | present |
| Forecast | favourable | favourable | treatable | treatable | incurable |
| Surface Modification | Method of Coating/Functionalisation | Study Model/Release | In Vitro/In Vivo Evaluation | Ref. |
|---|---|---|---|---|
| Polyethyleneimine and polyethylene glycol copolymer (co-PEI-PEG) | Graft copolymerisation | Human carcinoma xenograft in nude mice after intravenous injection/- | -/Reduced particle opsonisation, improved doxorubicin delivery to tumour xenograft site, reduced side effects | [119] |
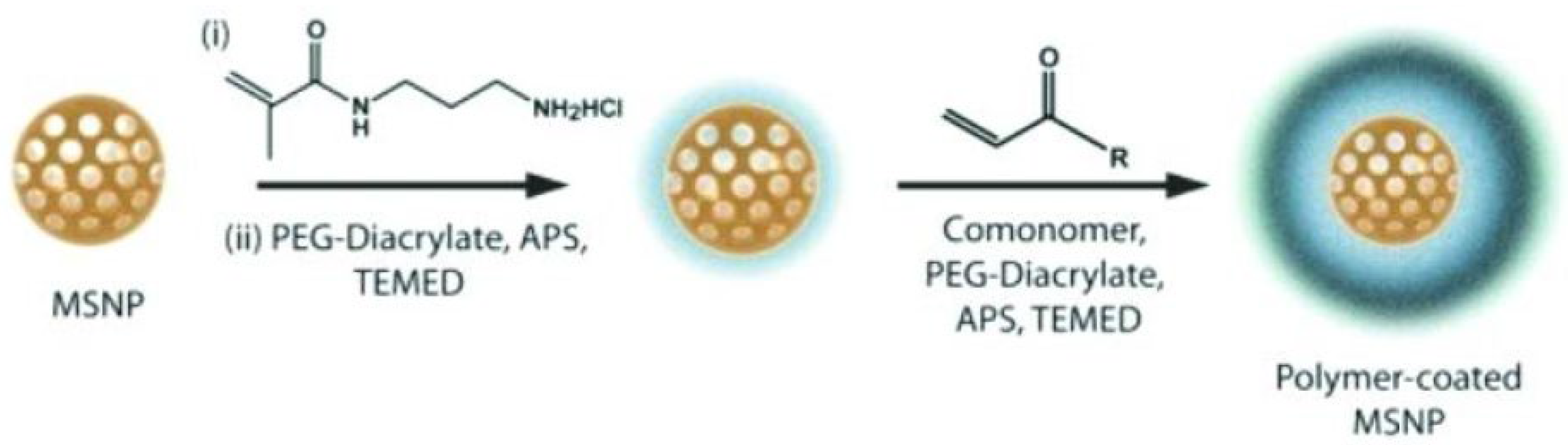
| Poly-N-isopropylacrylamide—polyethylene glycol diacrylate (pNIPAm-co-PEGDA) | Surface radical polymerisation | Mouse models of subcutaneous human sarcoma xenograft/Release triggered by endogenous protease | -/Offers colloidal stability, temperature sensitivity, prolonged circulation in the blood, high loading capacity, and customisable release | [116] |
| Poly-N-isopropylacrylamide—methacrylic acid p(NIPAm-co-MAA) | Precipitation copolymerisation method | Model buffer solutions; mice carrying murine sarcoma cell line S-180/Sensitive to pH change | Great antitumour activity. DOX release at pH = 5.0 85.2% ± 4.8 for 48 h and 12.9% ± 2.2 at pH = 7.4/Significantly increased the duration of drug circulation and decreased DOX accumulation in the heart | [136] |
| Poly-N-isopropylacrylamide—methacrylic acid p(NIPAm-co-MAA) | Precipitation copolymerisation method | Phosphate buffer (PBS) with different pH values (7.4 and 5.0) and human cells (HeLa)/Sensitive to temperature and pH changes | At pH 7.4, 9–12% of DOX was released in 8 h at 37 °C or 50 °C. At pH 5.0, the release was 19% at 37 °C and 44% at 50 °C for 8 h. HeLa cells exhibited low cytotoxicity and efficient cellular uptake of MMSN@P(NIPAM-co-MAA) nanoparticles when incubated for 4 h and 48 h/- | [137] |
| Sericin (Ser) | Covalent envelopment (cross-linking with glutaric aldehyde) | Phosphate buffer (PBS) with different pH values, human cells (HeLa (liver cancer), HepG2 (hepatocytic carcinoma) and MCF-7 (breast cancer), female BALB/c mice /Sensitive to pH change | The loading efficiency of DOX was 29.1%. DOX release rates: 16.4% and 24.1% at pH 7.4, and 6.5, respectively, for 72 h. Under acidic conditions (pH 5.0), 53.9% was released within 72 h/No significant cardiac damage or degeneration were observed in mice treated with DOX@SMSNs | [139] |
| Gelatin (Gel) | Formation of the coating layer through adsorption, followed by crosslinking with glutaric aldehyde | Hep-G2 cells, model buffer solutions, xenografted mice/Sensitive to pH change | Good biocompatibility and efficient intracellular drug release. Release rates: approximately 18%, 44%, 54% and 83% of the drug within 440 min at pH 6.0, 5.0, 4.0 and 2.0 respectively/Tumour growth in mice was significantly inhibited without marked reduction in body weight | [74,140] |
| Polidophamine (PDA) | Oxidative self-polymerisation | Phosphate and acetate buffer solutions for simulating normal physiological conditions and intracellular conditions of cancer cells/Sensitive to pH changes | Under normal physiological conditions (pH 7.4), no detectable release of DOX was observed. In acidic solutions (pH 5.0, 4.0, 3.0), the release rate increased as the acidity increased. At pH 4.4, 60% of DOX was released within 72 h/- | [133,167] |
| Pegelated polydophamine modified with folic acid | Absorption, self-polymerisation | PBS buffer, 4T1 cells (breast cancer cells), eight-week-old female BALB/c mice/Sensitive to pH change | DOX loading efficiency is up to (35.43 ± 0.59%). DOX release: 80% release at pH 5.0 vs. 20% release at pH 7.4/Effectively accumulates in 4T1 tumour and demonstrates superior tumour inhibition effect | [148,149] |
| Two bilayers alginate/chitosan | Layer-by-layer assembly method (LbL) | Model buffer solutions (acetate, phosphate) and HeLa cells/Sensitive to pH change | Throughout the time period, approximately 10.7%, 48.6%, and 60.1% of DOX was released at pH 6.8, 5.2, and 4.0, respectively. The nanocarriers exhibited sustained intracellular DOX release and prolonged retention of DOX in the nucleus/- | [150] |
| Polyamidoamine (PAMAM) dendrimers and chondroitin sulphate (CS) | Layer-by-layer assembly method (LbL) | Phosphate-buffered saline (PBS)/Sensitive to pH change | Slow and sustained release of DOX and CUR at neutral pH, much faster in an acidic environment (pH = 3), 35% DOX and 17% CUR released within 28 h/- | [151] |
| Chitosan-polymethacrylic acid (CS-PMAA) | In situ polymerisation | HeLa cells/Sensitive to pH change | The release rate when the pH was lowered to 5.5 reached 70 wt.% after 24 h, which is almost four times higher than at pH 7.4/- | [168,169] |
| Poly N-vinylcaprolactam-methacrylic acid p(VCL- co -MAA) | Precipitation copolymerisation method | Model buffer solutions/Sensitive to temperature and pH changes | DOX release: 5.4% of drug in buffer with pH 7.4 within 24 h, at pH 6.5 and pH 5.0, 34.1% and 64.2%, respectively/- | [170] |
| Oligo ethylene glycol acrylate—N,N′ -cystamine bismethacrylamide poly(OEGA-co-CBMA) | Grafting of crosslinked copolymer | Phosphate buffered saline PBS + dithiothreitol DTT/By reduction-oxidation reactions | About 32% of the loaded DOX was released in pure PBS after 25 h. In PBS DTT solution (20 × 10−3 M), 85% of the drug was released after 10 h/- | [171] |
| Polyglycerol methacrylate (PGOHMA) and cucurbituryl (CB) | Self-assembly technology layer—by —layer (LbL) | Model buffer solutions, BALB/c nude mouse models/Sensitive to pH change | DOX molecules are tightly held inside the nanopores at pH = 7.4. When the pH is lowered to 5, the interaction between CB and PGOHMA layers weakens, and DOX is released/Showed high inhibition of tumour growth by 63% on day 28 | [172] |
| Copolymer of dimethylamino-ethyl acrylate and polyethylene glycol methacrylate Poly(DMAEA-co-PEGMA) | Use of a combined “RAFT” polymerisation and “Graft From” strategy | Hela cell xenografts in nude mice, Model buffer solutions/Sensitive to pH change | Rapid drug release when soaked in acidic solution (pH 5.5) Soaking in acidic solution (pH 5.5)/Significantly increased EPR effect and tumour growth inhibition rate of 68.7% | [173] |
| Diblock copolymers of polyethylene oxide and L-lactide (Poly(EO-co-LLA)) | Block copolymer grafting | Model buffer solutions/Sensitive to temperature and pH changes | Release at 45 °C is easier than at 25 °C. Reaching the maximum release (92.7%) at pH 4 takes only 24 h. When the pH value is increased to 7.4., the release decreases to 38.0%/- | [174] |
| Poly N-succinimidylacrylate (PSA) | Grafting with an acetal linker | Model buffer solutions (acetate, phosphate), HepG2 cell line/Sensitive to pH change | The cumulative amount of DOX released is up to 37.9% at pH 6.5, 78.4% at pH 5.0, and 93.5% at pH 2.0. Capable of targeting accumulation in cancer cells and effectively destroying cancer cells/- | [128] |
| Polyethylene glycol-co-polyvinylpyridine (PEG-co-PVP) | Through electrostatic interaction with grafted carboxylate groups | Model buffer solutions (acetate, phosphate)/Sensitive to pH change | At neutral pH (pH = 7.4), about 34% of DOX is released within 72 h. A change in pH = 5.5 results in increased release (about 75% within 72 h)/- | [175] |
| Boltorn H40 polyester, amine-functionalised polyethylene glycol (PEG-H40) | Grafting of H40 and modification with tertiary amine and PEG via chemical bond formation | Model buffer solutions, MCF-7 cells, male Balb/c mice /Sensitive to pH change | Payload efficiency: 36.5%; capture efficiency: 57.4%. DOX release at pH 7.4 and pH 6.8 was only 9.7% and 20%, respectively, after 48 h, and increased to 49% at pH 5.5/Very low cytotoxicity in mouse kidneys and liver and excellent biocompatibility with blood | [176] |
| Polyacrylamide (PAA) | Graft polymerisation method | Aqueous solution of nanoparticles containing doxorubicin/Sensitive to temperature change | Released 11.5 ± 2.4% in aqueous solution at 37 °C after 30 min and 67.6 ± 2.5% at 60 °C/- | [177] |
| Poly (2-diethylamino- ethyl methacrylate) (PDEAEMA) | Surface-initiated radical polymerisation with atom transfer (ATRP) | Model buffer solutions (phosphate, acetate), HeLa cells/sensitive to pH change, recovery, and light | At pH 7.4, less than 12% of DOX is released within 22 h, and at pH 5.0, about 64% of DOX is released. After pH 5.0 treatment with dithiothreitol (DTT), the most complete release of DOX occurs, enhanced by UV irradiation/- | [178] |
| Polyaspartic acid (PAsA) | Conjugation on the surface of MSNs via amide bonding | PBS with different pH values, HepG2 cells/sensitive to pH changes | DOX@P-MSNs were efficiently internalised by HepG2 cells, with 73% inhibition of cell growth and only 30% and 33% inhibition of cell growth with free DOX and DOX@MSNs. 10% of DOX was released at pH 7.4 and almost 56% at pH 4.5/- | [179] |
| Folic acid (FA) | Conjugation on the surface of MSNs via amide bonding | Model buffer solutions, ZR-75-1 and T47-D cell lines/sensitive to pH change | The loading efficiency of DOX is about 68%. At pH 7.4 < 20% and at pH 5.5 about 45% of DOX is released within 24 h. Empty MSN-FA shows no cytotoxicity, DOX@MSN-FA is significantly more effective in inducing cell death than DOX solution at different concentrations/- | [180] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kovtareva, S.; Kusepova, L.; Tazhkenova, G.; Mashan, T.; Bazarbaeva, K.; Kopishev, E. Surface Modification of Mesoporous Silica Nanoparticles for Application in Targeted Delivery Systems of Antitumour Drugs. Polymers 2024, 16, 1105. https://doi.org/10.3390/polym16081105
Kovtareva S, Kusepova L, Tazhkenova G, Mashan T, Bazarbaeva K, Kopishev E. Surface Modification of Mesoporous Silica Nanoparticles for Application in Targeted Delivery Systems of Antitumour Drugs. Polymers. 2024; 16(8):1105. https://doi.org/10.3390/polym16081105
Chicago/Turabian StyleKovtareva, Svetlana, Lyazat Kusepova, Gaukhar Tazhkenova, Togzhan Mashan, Karlygash Bazarbaeva, and Eldar Kopishev. 2024. "Surface Modification of Mesoporous Silica Nanoparticles for Application in Targeted Delivery Systems of Antitumour Drugs" Polymers 16, no. 8: 1105. https://doi.org/10.3390/polym16081105
APA StyleKovtareva, S., Kusepova, L., Tazhkenova, G., Mashan, T., Bazarbaeva, K., & Kopishev, E. (2024). Surface Modification of Mesoporous Silica Nanoparticles for Application in Targeted Delivery Systems of Antitumour Drugs. Polymers, 16(8), 1105. https://doi.org/10.3390/polym16081105







