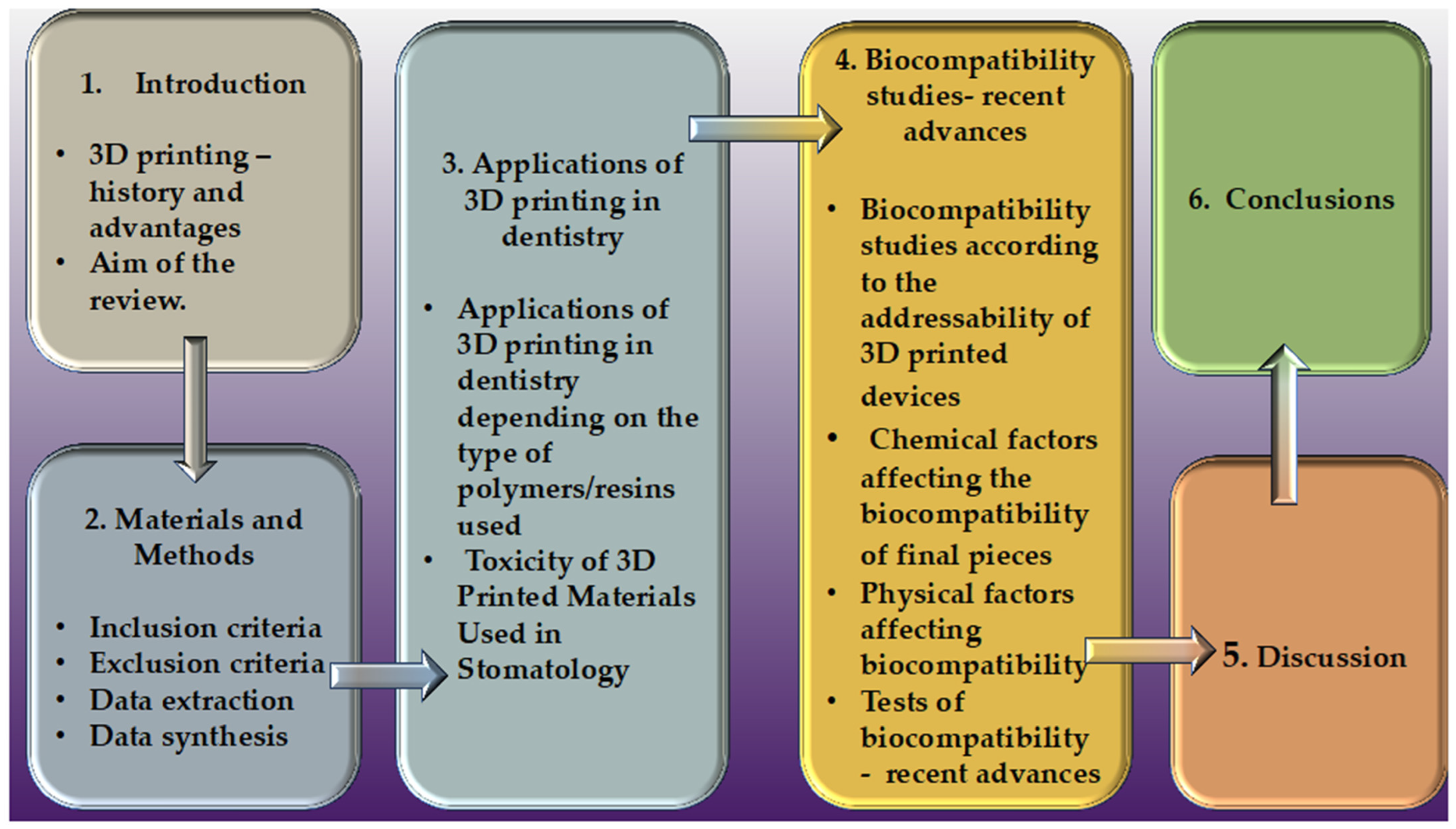
Polymeric Materials Used in 3DP in Dentistry—Biocompatibility Testing Challenges
Abstract
1. Introduction
2. Materials and Methods
3. Applications of 3D Printing in Dentistry
3.1. Applications of 3D Printing in Dentistry Depending on the Type of Polymers/Resins Used
3.2. Toxicity of 3D-Printed Materials Used in Stomatology
4. Biocompatibility Studies—Recent Advances
4.1. Biocompatibility Studies According to the Addressability of 3D-Printed Devices
4.2. Chemical Factors That Affect the Biocompatibility of Final Pieces
4.3. Physical Factors That Can Affect Biocompatibility
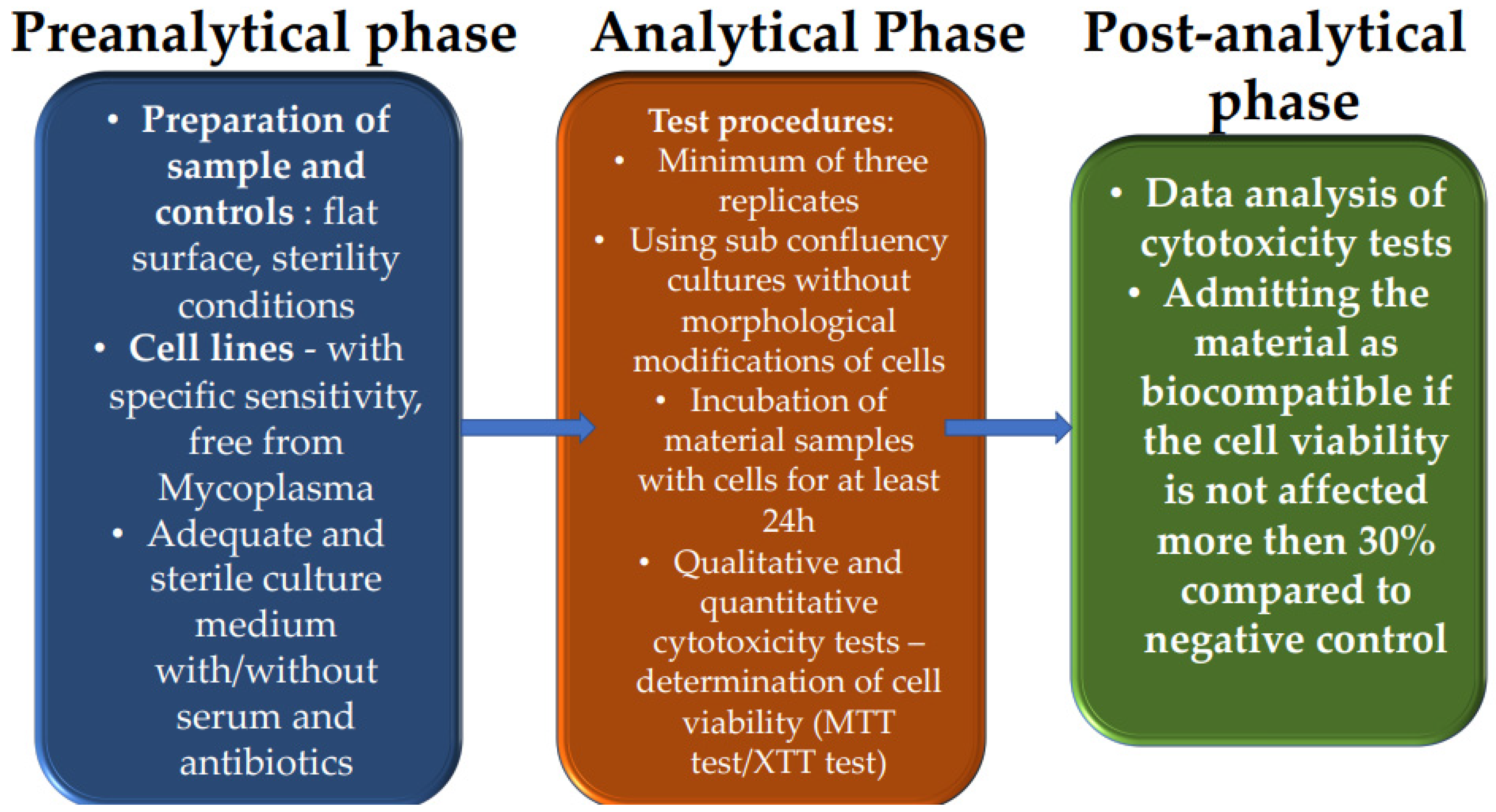
4.4. Tests of Biocompatibility Recent Advances
| Materials | Applications | Biocompatibility Tests | Influence on Biocompatibility of Diverse Processes in Manufacturing Techniques | References |
|---|---|---|---|---|
| Polymethyl methacrylate (PMMA) resin, ceramic, metals | Prosthodontics, orthodontics, orthognathics, endodontics, craniofacial, oral, and maxillofacial surgical procedures; manufacturing of implant-drill guides for guided surgery procedures | Cytotoxicity, genotoxicity, and irritation potential; regulation of standards USP Class IV and ISO 10993; cellular assays; cellular response; in vivo toxicity on model animals (zebrafish embryo, culture of mouse oocytes) | Exposure to UV so that the material can cross-link the residual monomers; role of the washing process in the elution of unreacted monomers; post-curing treatments; variation of temperature, | [13,16,17,18,24,25,26,42,43,44,65,72,73,74,75,76,80,82,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134] |
| Acrylonitrile butadiene styrene (ABS), polylactic acid (PLA), polycarbonate (PC), polyamide (nylon), thermoplastic materials | Orthodontic alignment trays; retention trays or whitening trays, whitening trays; removable partial prostheses | Cellular assays; cellular response; viability and toxicity tests; cell viability; tissue integration; in vitro human cell adhesion and proliferation; MTT and XTT assays | Variation of UV light intensity and wavelength; variation of curing time and temperature washing solutions (isopropyl alcohol and tripropylene glycol monomethyl ether) | [13,16,18,24,25,26,27,33,45,73,74,75,76,80,83,84,85,86,88,108,109,110,111,119,134,135] |
| Polymethyl methacrylate (PMMA), thermoplastics (polycarbonate, polyamides, polyvinyl chloride) (meth)acrylate monomers, oligomers, photoinitiators, waxes | Dentistry and orthodontic applications; clear aligners; 3D-printed denture teeth; crown and bridge | Cell viability, cytotoxicity, and status of human gingival fibroblasts; confocal laser scanning microscopy | Addition reaction; using various sources of heat, light, or various chemicals as activators; washing post-polymerization with alcoholic solutions | [11,13,18,24,25,26,27,33,35,36,42,45,72,73,74,75,76,77,78,79,80,84,85,86,87,88,89,90,92,93,94,95,96,97,98,99,100,101,103,104,105,106,109,110,111,112,113,114,115,116,119,120,121,131,133,134,135,136,137,138] |
| Metal materials and alloys: titanium (Ti), titanium-based alloys: niobium, tantalum, zirconium, molybdenum, tungsten (Ti-Nb, Ti-Zr, and Ti-Mo-W); nickel-based and cobalt-based metal alloys:cobalt-chromium (Co-Cr) | Crafting biocompatible dental implants and orthodontic appliances | Evaluating morphology and cell migration; confocal laser scanning microscopy | Variation of UV light intensity and wavelength; variation of curing time and temperature | [13,16,18,24,25,26,33,34,40,41,77,78,79,102,107,108,115,117,118] |
| Ceramics, resin Ceramics, metals | Dentistry and orthodontic applications, clear aligners; clear orthodontic aligners; 3D-printed denture teeth; crown and bridge | Morphology and cells migration; Confocal laser scanning microscopy | Variation of UV light intensity and wavelength; variation of curing time and temperature; washing post-polymerization with alcoholic solutions | [13,18,24,25,26,30,31,32,33,34,38,72,73,74,75,76,83,123] |
| Ceramics: compounds of metallic elements and non-metallic substances (oxides, nitrides, and silicates), most commonly used silica (SiO2) | Crafting biocompatible dental implants and orthodontic appliances | Mass spectroscopy; morphology and cell migration; confocal laser scanning microscopy | Variation of UV light intensity and wavelength; variation of curing time and temperature; washing post-polymerization with alcoholic solutions | [13,18,24,25,26,30,31,32,33,65,80,83,135] |
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cheramie, T.; Strother, E. The dentist’s armamentarium: A collection of 19th century instruments in the Louisiana State University School of Dentistry Library. J. Hist. Dent. 2008, 56, 107–118. [Google Scholar] [PubMed]
- Nesic, D.; Schaefer, B.M.; Sun, Y.; Saulacic, N.; Sailer, I. 3D Printing Approach in Dentistry: The Future for Personalized Oral Soft Tissue Regeneration. J. Clin. Med. 2020, 9, 2238. [Google Scholar] [CrossRef] [PubMed]
- Sears, N.A.; Seshadri, D.R.; Dhavalikar, P.S.; Cosgriff-Hernandez, E. A Review of Three-Dimensional Printing in Tissue Engineering. Tissue Eng. Part B Rev. 2016, 22, 298–310. [Google Scholar] [CrossRef] [PubMed]
- Shah, P.; Chong, B.S. 3D imaging, 3D printing and 3D virtual planning in endodontics. Clin. Oral Investig. 2018, 22, 641–654. [Google Scholar] [CrossRef]
- Barazanchi, A.; Li, K.C.; Al-Amleh, B.; Lyons, K.; Waddell, J.N. Additive Technology: Update on Current Materials and Applications in Dentistry. J. Prosthodont. 2017, 26, 156–163. [Google Scholar] [CrossRef]
- Jawahar, A.; Maragathavalli, G. Applications of 3D printing in dentistry—A review. J. Pharm. Sci. Res. 2019, 11, 1670–1675. [Google Scholar]
- Matai, I.; Kaur, G.; Seyedsalehi, A.; McClinton, A.; Laurencin, C.T. Progress in 3D bioprinting technology for tissue/organ regenerative engineering. Biomaterials 2020, 226, 119536. [Google Scholar] [CrossRef]
- Van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef]
- Kessler, A.; Hickel, R.; Reymus, M. 3D Printing in Dentistry—State of the Art. Oper. Dent. 2020, 45, 30–40. [Google Scholar] [CrossRef]
- Liaw, C.-Y.; Guvendiren, M. Current and emerging applications of 3D printing in medicine. Biofabrication 2017, 9, 024102. [Google Scholar] [CrossRef]
- Tian, Y.; Chen, C.; Xu, X.; Wang, J.; Hou, X.; Li, K.; Lu, X.; Shi, H.; Lee, E.-S.; Jiang, H.B. A Review of 3D Printing in Dentistry: Technologies, Affecting Factors, and Applications. Scanning 2021, 2021, 9950131. [Google Scholar] [CrossRef] [PubMed]
- Nulty, A. A comparison of trueness and precision of 12 3D printers used in dentistry. BDJ Open 2022, 8, 14. [Google Scholar] [CrossRef] [PubMed]
- Zinelis, S.; Panayi, N.; Polychronis, G.; Papageorgiou, S.N.; Eliades, T. Comparative analysis of mechanical properties of orthodontic aligners produced by different contemporary 3D printers. Orthod. Craniofacial Res. 2022, 25, 336–341. [Google Scholar] [CrossRef]
- Pituru, S.M.; Greabu, M.; Totan, A.; Imre, M.; Pantea, M.; Spinu, T.; Tancu, A.M.C.; Popoviciu, N.O.; Stanescu, I.-I.; Ionescu, E. A Review on the Biocompatibility of PMMA-Based Dental Materials for Interim Prosthetic Restorations with a Glimpse into Their Modern Manufacturing Techniques. Materials 2020, 13, 2894. [Google Scholar] [CrossRef] [PubMed]
- Wuersching, S.N.; Hickel, R.; Edelhoff, D.; Kollmuss, M. Initial biocompatibility of novel resins for 3D printed fixed dental prostheses. Dent. Mater. 2022, 38, 1587–1597. [Google Scholar] [CrossRef] [PubMed]
- Guttridge, C.; Shannon, A.; O’Sullivan, A.; O’Sullivan, K.J.; O’Sullivan, L.W. Biocompatible 3D printing resins for medical applications: A review of marketed intended use, biocompatibility certification, and post-processing guidance. Ann. 3D Print. Med. 2022, 5, 100044. [Google Scholar] [CrossRef]
- ISO 10993-5:2009; Biological Evaluation of Medical Devices—Part 5: Tests for In Vitro Cytotoxicity. ISO: Geneve, Switzerland, 2009.
- Guerrero-Gironés, J.; López-García, S.; Pecci-Lloret, M.R.; Lozano, F.J.R.; García-Bernal, D. In vitro biocompatibility testing of 3D printing and conventional resins for occlusal devices. J. Dent. 2022, 123, 104163. [Google Scholar] [CrossRef]
- Alkhateeb, R.I.; Algaoud, H.S.; Aldamanhori, R.B.; Alshubaili, R.R.; Alalawi, H.; Gad, M.M. Fracture Load 698 of 3D-Printed Interim Three-Unit Fixed Dental Prostheses: Impact of Printing Orientation and Post-Curing Time. Polymers 2023, 15, 1737. [Google Scholar] [CrossRef]
- Jain, S.; Sayed, M.E.; Shetty, M.; Alqahtani, S.M.; Al Wadei, M.H.D.; Gupta, S.G.; Othman, A.A.A.; Alshehri, A.H.; Alqarni, H.; Mobarki, A.H.; et al. Physical and Mechanical Properties of 3D-Printed Provisional Crowns and Fixed Dental Prosthesis Resins Compared to CAD/CAM Milled and Conventional Provisional Resins: A Systematic Review and Meta-Analysis. Polymers 2022, 14, 2691. [Google Scholar] [CrossRef]
- Narongdej, P.; Hassanpour, M.; Alterman, N.; Rawlins-Buchanan, F.; Barjasteh, E. Advancements in Clear Aligner Fabrication: A Comprehensive Review of Direct-3D Printing Technologies. Polymers 2024, 16, 371. [Google Scholar] [CrossRef]
- Rosentritt, M.; Behr, M.; Strasser, T.; Schmid, A. Pilot in-vitro study on insertion/removal performance of hand-cast, milled and 3D printed splints. J. Mech. Behav. Biomed. Mater. 2021, 121, 104612. [Google Scholar] [CrossRef] [PubMed]
- Tack, P.; Victor, J.; Gemmel, P.; Annemans, L. 3D-printing techniques in a medical setting: A systematic literature review. Biomed. Eng. Online 2016, 15, 115. [Google Scholar] [CrossRef] [PubMed]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Tartaglia, G.M.; Mapelli, A.; Maspero, C.; Santaniello, T.; Serafin, M.; Farronato, M.; Caprioglio, A. Direct 3D Printing of Clear Orthodontic Aligners: Current State and Future Possibilities. Materials 2021, 14, 1799. [Google Scholar] [CrossRef]
- Park, S.-M.; Park, J.-M.; Kim, S.-K.; Heo, S.-J.; Koak, J.-Y. Flexural Strength of 3D-Printing Resin Materials for Provisional Fixed Dental Prostheses. Materials 2020, 13, 3970. [Google Scholar] [CrossRef]
- Alageel, O. Three-dimensional printing technologies for dental prosthesis: A review. Rapid Prototyp. J. 2022, 28, 1764–1778. [Google Scholar] [CrossRef]
- Revilla-León, M.; Sadeghpour, M.; Özcan, M. An update on applications of 3D printing technologies used 726 for processing polymers used in implant dentistry. Odontology 2020, 108, 331–338. [Google Scholar] [CrossRef]
- Brandt, J.; Lauer, H.-C.; Peter, T.; Brandt, S. Digital process for an implant-supported fixed dental prosthesis: A clinical report. J. Prosthet. Dent. 2015, 114, 469–473. [Google Scholar] [CrossRef]
- Dehurtevent, M.; Robberecht, L.; Hornez, J.C.; Thuault, A.; Deveaux, E.; Béhin, P. Stereolithography: A new method for processing dental ceramics by additive computer-aided manufacturing. Dent. Mater. 2017, 33, 477–485. [Google Scholar] [CrossRef]
- Gronet, P.M.; Waskewicz, G.A.; Richardson, C. Preformed acrylic cranial implants using fused deposition modeling: A clinical report. J. Prosthet. Dent. 2003, 90, 429–433. [Google Scholar] [CrossRef]
- Xu, X.; He, L.; Zhu, B.; Li, J.; Li, J. Advances in polymeric materials for dental applications. Polym. Chem. 2017, 8, 807–823. [Google Scholar] [CrossRef]
- Duta, M. Advances in 3D Printing in Dentistry. In Proceedings of the 4th SGEM International Multidisciplinary Scientific Conferences on Social Sciences and Arts, Albena, Bulgaria, 24–30 August 2017. [Google Scholar] [CrossRef]
- Mayer, J.; Reymus, M.; Mayinger, F.; Edelhoff, D.; Hickel, R.; Stawarczyk, B. Temporary 3D-Printed Fixed 879 Dental Prosthesis Materials: Impact of Postprinting Cleaning Methods on Degree of Conversion and Surface 880 and Mechanical Properties. Int. J. Prosthodont. 2021, 34, 784–795. [Google Scholar] [CrossRef] [PubMed]
- González, G.; Baruffaldi, D.; Martinengo, C.; Angelini, A.; Chiappone, A.; Roppolo, I.; Pirri, C.F.; Frascella, F. Materials Testing for the Development of Biocompatible Devices through Vat-Polymerization 3D Printing. Nanomaterials 2020, 10, 1788. [Google Scholar] [CrossRef] [PubMed]
- Konuray, O.; Sola, A.; Bonada, J.; Tercjak, A.; Fabregat-Sanjuan, A.; Fernández-Francos, X.; Ramis, X. Cost-Effectively 3D-Printed Rigid and Versatile Interpenetrating Polymer Networks. Materials 2021, 14, 4544. [Google Scholar] [CrossRef]
- Cai, H.; Xu, X.; Lu, X.; Zhao, M.; Jia, Q.; Jiang, H.-B.; Kwon, J.-S. Dental Materials Applied to 3D and 4D Printing Technologies: A Review. Polymers 2023, 15, 2405. [Google Scholar] [CrossRef]
- Park, J.-H.; Lee, H.; Kim, J.-W.; Kim, J.-H. Cytocompatibility of 3D printed dental materials for temporary restorations on fibroblasts. BMC Oral Health 2020, 20, 157. [Google Scholar] [CrossRef]
- Kundu, J.; Shim, J.-H.; Jang, J.; Kim, S.-W.; Cho, D.-W. An additive manufacturing-based PCL-alginate-chondrocyte bioprinted scaffold for cartilage tissue engineering: PCL-alginate-chondrocyte 885 bioprinted scaffold for cartilage tissue engineering. J. Tissue Eng. Regen. Med. 2015, 9, 1286–1297. [Google Scholar] [CrossRef]
- Londono, J.; Tadros, M.; Salgueiro, M.; Baker, P.S. Digital design and 3D printing of an implant-supported prosthetic stent for protecting complete arch soft tissue grafts around dental implants: A dental technique. J. Prosthet. Dent. 2018, 120, 801–804. [Google Scholar] [CrossRef]
- Rezaie, F.; Farshbaf, M.; Dahri, M.; Masjedi, M.; Maleki, R.; Amini, F.; Wirth, J.; Moharamzadeh, K.; Weber, F.E.; Tayebi, L. 3D Printing of Dental Prostheses: Current and Emerging Applications. J. Compos. Sci. 2023, 7, 80. [Google Scholar] [CrossRef]
- Alqutaibi, A.Y.; Baik, A.; Almuzaini, S.A.; Farghal, A.E.; Alnazzawi, A.A.; Borzangy, S.; Aboalrejal, A.N.; AbdElaziz, M.H.; Mahmoud, I.I.; Zafar, M.S. Polymeric Denture Base Materials: A Review. Polymers 2023, 15, 3258. [Google Scholar] [CrossRef]
- Ellakany, P.; Al-Harbi, F.; El Tantawi, M.; Mohsen, C. Evaluation of the accuracy of digital and 3D-printed casts compared with conventional stone casts. J. Prosthet. Dent. 2022, 127, 438–444. [Google Scholar] [CrossRef]
- Yao, Q.; Morton, D.; Eckert, G.J.; Lin, W.-S. The effect of surface treatments on the color stability of CAD-CAM interim fixed dental prostheses. J. Prosthet. Dent. 2021, 126, 248–253. [Google Scholar] [CrossRef]
- Tzeng, J.-J.; Yang, T.-S.; Lee, W.-F.; Chen, H.; Chang, H.-M. Mechanical Properties and Biocompatibility of Urethane Acrylate-Based 3D-Printed Denture Base Resin. Polymers 2021, 13, 822. [Google Scholar] [CrossRef]
- Wesemann, C.; Spies, B.C.; Sterzenbach, G.; Beuer, F.; Kohal, R.; Wemken, G.; Krügel, M.; Pieralli, S. Polymers for conventional, subtractive, and additive manufacturing of occlusal devices differ in hardness and flexural properties but not in wear resistance. Dent. Mater. 2021, 37, 432–442. [Google Scholar] [CrossRef]
- Prpić, V.; Schauperl, Z.; Ćatić, A.; Dulčić, N.; Čimić, S. Comparison of mechanical properties of 3D-printed, CAD/CAM, and conventional denture base materials. J. Prosthodont. 2020, 29, 524–528. [Google Scholar] [CrossRef]
- Revilla-León, M.; Özcan, M. Additive Manufacturing Technologies used for 3D Metal Printing in Dentistry. Curr. Oral Health Rep. 2017, 4, 201–208. [Google Scholar] [CrossRef]
- Valenti, C.; Isabella Federici, M.; Masciotti, F.; Marinucci, L.; Xhimitiku, I.; Cianetti, S.; Pagano, S. Mechanical properties of 3D-printed prosthetic materials compared with milled and conventional processing. J. Prosthet. Dent. 2022, 132, 381–391. [Google Scholar] [CrossRef]
- Tan, K.; Chua, C.; Leong, K.; Cheah, C.; Cheang, P.; Abu Bakar, M.; Cha, S. Scaffold development using selective laser sintering of polyetheretherketonehydroxyapatite biocomposite blends. Biomaterials 2003, 24, 3115–3123. [Google Scholar] [CrossRef]
- von Wilmowsky, C.; Vairaktaris, E.; Pohle, D.; Rechtenwald, T.; Lutz, R.; Münstedt, H.; Koller, G.; Schmidt, M.; Neukam, F.W.; Schlegel, K.A.; et al. Effects of bioactive glass and beta-TCP containing threedimensional laser sintered polyetheretherketone composites on osteoblasts in vitro. J. Biomed. Mater. Res. A 2008, 87, 896–902. [Google Scholar] [CrossRef]
- Van de Velde, K.; Kiekens, P. Biopolymers: Overview of several properties and consequences on their applications. Polym. Test. 2002, 21, 433–442. [Google Scholar] [CrossRef]
- ISO 14577-1; Metallic Materials—Instrumented Indentation Test for Hardness and Materials Parameters—Part 1: Test Method. International Organization for Standardization: Geneva, Switzerland, 2002.
- Gagg, G.; Ghassemieh, E.; Wiria, F.E. Effects of sintering temperature on morphology and mechanical characteristics of 3D printed porous titanium used as dental implant. Mater. Sci. Eng. C 2013, 33, 3858–3864. [Google Scholar] [CrossRef]
- Jiang, L.; Liao, Y.; Wan, Q.; Li, W. Effects of sintering temperature and particle size on the translucency of zirconium dioxide dental ceramic. J. Mater. Sci. Mater. Med. 2011, 22, 2429–2435. [Google Scholar] [CrossRef]
- Shiva, S.; Prabu, R.G.A.; Bajaj, G.; John, A.E.; Chandran, S.; Kumar, V.V.; Ramakrishna, S. A review on the recent applications of synthetic biopolymers in 3D printing for biomedical applications. J. Mater. Sci. Mater. Med. 2023, 34, 62. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jeong, M.; Radomski, K.; Lopez, D.; Liu, J.T.; Lee, J.D.; Lee, S.J. Materials and Applications of 3D Printing Technology in Dentistry: An Overview. Dent. J. 2023, 12, 1. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tsolakis, I.; Gizani, S.; Panayi, N.; Antonopoulos, G.; Tsolakis, A. Three-dimensional printing technology in orthodontics for dental models: A systematic review. Children 2022, 9, 1106. [Google Scholar] [CrossRef]
- Zembic, A.; Bösch, A.; Jung, R.E.; Hämmerle, C.H.F.; Sailer, I. Five-year results of a randomized controlled clinical trial comparing zirconia and titanium abutments supporting single-implant crowns in canine and posterior regions. Clin. Oral Implants Res. 2013, 24, 384–390. [Google Scholar] [CrossRef]
- Mitov, G.; Heintze, S.D.; Walz, S.; Woll, K.; Muecklich, F.; Pospiech, P. Wear behavior of dental Y-TZP ceramic against natural enamel after different finishing procedures. Dent. Mater. 2012, 28, 909–918. [Google Scholar] [CrossRef]
- Bateli, M.; Kern, M.; Wolkewitz, M.; Strub, J.R.; Att, W. A retrospective evaluation of teeth restored with zirconia ceramic posts: 10-year results. Clin. Oral Investig. 2014, 18, 1181–1187. [Google Scholar] [CrossRef]
- Schley, J.S.; Heussen, N.; Reich, S.; Fischer, J.; Haselhuhn, K.; Wolfart, S. Survival probability of zirconia-based fixed dental prostheses up to 5 yr: A systematic review of the literature. Eur. J. Oral Sci. 2010, 118, 443–450. [Google Scholar] [CrossRef]
- Abbas, M.K.G.; Ramesh, S.; Tasfy, S.F.H.; Lee, K.Y.S. A state-of-the-art review on alumina toughened zirconia ceramic composites. Mater. Today Commun. 2023, 37, 106964. [Google Scholar] [CrossRef]
- Mohd, N.; Razali, M.; Fauzi, M.B.; Kasim, N.H.A. In Vitro and In Vivo Biological Assessments of 3D-Bioprinted Scaffolds for Dental Applications. Int. J. Mol. Sci. 2023, 24, 12881. [Google Scholar] [CrossRef]
- Agarwalla, S.V.; Malhotra, R.; Rosa, V. Translucency, hardness and strength parameters of PMMA resin containing graphene-like material for CAD/CAM restorations. J. Mech. Behav. Biomed. Mater. 2019, 100, 103388. [Google Scholar] [CrossRef]
- Mai, H.-N.; Lee, K.-B.; Lee, D.-H. Fit of interim crowns fabricated using photopolymer-jetting 3D printing. J. Prosthet. Dent. 2017, 118, 208–215. [Google Scholar] [CrossRef]
- Totu, E.E.; Nechifor, A.C.; Nechifor, G.; Aboul-Enein, H.Y.; Cristache, C.M. Poly(methyl methacrylate) with TiO2 nanoparticles inclusion for stereolitographic complete denture manufacturing—The fututre in dental care for elderly edentulous patients? J. Dent. 2017, 59, 68–77. [Google Scholar] [CrossRef]
- Turagam, N.; Mudrakola, D.P. Effect of Micro-Additions of Carbon Nanotubes to Polymethylmethacrylate on Reduction in Polymerization Shrinkage. J. Prosthodont. 2013, 22, 105–111. [Google Scholar] [CrossRef]
- Zafar, M.S. Prosthodontic Applications of Polymethyl Methacrylate (PMMA): An Update. Polymers 2020, 12, 2299. [Google Scholar] [CrossRef]
- Braun, K.O.; Mello, J.A.N.; Rached, R.N.; Del Bel Cury, A.A. Surface texture and some properties of acrylic resins submitted to chemical polishing. J. Oral Rehabil. 2003, 30, 91–98. [Google Scholar] [CrossRef]
- Jorge, J.H.; Giampaolo, E.T.; Machado, A.L.; Vergani, C.E. Cytotoxicity of denture base acrylic resins: A literature review. J. Prosthet. Dent. 2003, 90, 190–193. [Google Scholar] [CrossRef]
- Ortensi, L.; Grande, F.; Testa, C.; Balma, A.M.; Pedraza, R.; Mussano, F.; La Rosa, G.R.M.; Pedullà, E. Fracture strength of 3-units fixed partial dentures fabricated with metal-ceramic, graphene doped PMMA and PMMA before and after ageing: An in-vitro study. J. Dent. 2024, 142, 104865. [Google Scholar] [CrossRef]
- Bürgers, R.; Schubert, A.; Müller, J.; Krohn, S.; Rödiger, M.; Leha, A.; Wassmann, T. Cytotoxicity of 3D-printed, milled, and conventional oral splint resins to L929 cells and human gingival fibroblasts. Clin. Exp. Dent. Res. 2022, 8, 650–657. [Google Scholar] [CrossRef]
- Punset, M.; Brizuela, A.; Pérez-Pevida, E.; Herrero-Climent, M.; Manero, J.M.; Gil, J. Mechanical Characterization of Dental Prostheses Manufactured with PMMA–Graphene Composites. Materials 2022, 15, 5391. [Google Scholar] [CrossRef]
- Borelli, B.; Zarone, F.; Rivieccio, V.; Riccitiello, F.; Simeone, M.; Sorrentino, R.; Rengo, S.; Spagnuolo, G.; Procino, A. Polyacrylic resins regulate transcriptional control of interleukin-6, gp80, and gp130 genes in human gingival fibroblasts. J. Oral Sci. 2017, 59, 87–91. [Google Scholar] [CrossRef]
- Lung, C.Y.K.; Darvell, B.W. Minimization of the inevitable residual monomer in denture base acrylic. Dent. Mater. 2005, 21, 1119–1128. [Google Scholar] [CrossRef]
- Garcia-Falcon, C.M.; Gil-Lopez, T.; Verdu-Vazquez, A.; Mirza-Rosca, J.C. Analysis and Comparison of the Corrosive Behavior of Nickel-Based and Cobalt-Based Dental Alloys. Materials 2021, 14, 4949. [Google Scholar] [CrossRef]
- Ghica, S.I.; Cotrut, C.M.; Buzatu, M.; Geanta, V.; Ghica, V.G.; Petrescu, M.I.; Iacob, G.; Ungureanu, E. Evaluation of The Corrosion Resistance of Timo-W Alloys in Simulated Body Fluid (SBF). Univ. Politeh. Buchar. Sci. Bull. Ser. B-Chem. Mater. Sci. 2022, 84, 189–198. [Google Scholar]
- Messer, R. Cytotoxicity of nickel–chromium alloys: Bulk alloys compared to multiple ion salt solutions. Dent. Mater. 2000, 16, 207–212. [Google Scholar] [CrossRef]
- ISO 10993-1:2018; Biological Evaluation of Medical Devices—Part 1: Evaluation and Testing Within a Risk Management Process. ISO: Geneve, Switzerland, 2018.
- ISO 10993-12:2021; Biological Evaluation of Medical Devices—Part 12: Sample Preparation and Reference Materials. ISO: Geneve, Switzerland, 2021.
- Clark, M.; Needham, C. The role of the general dental practitioner in the care of the implant patient. Prim. Dent. J. 2024, 13, 39–46. [Google Scholar] [CrossRef]
- Bayarsaikhan, E.; Lim, J.-H.; Shin, S.-H.; Park, K.-H.; Park, Y.-B.; Lee, J.-H.; Kim, J.-E. Effects of Postcuring Temperature on the Mechanical Properties and Biocompatibility of Three-Dimensional Printed Dental Resin Material. Polymers 2021, 13, 1180. [Google Scholar] [CrossRef]
- Cheah, C.M.; Nee, A.Y.C.; Fuh, J.Y.H.; Lu, L.; Choo, Y.S.; Miyazawa, T. Characteristics of photopolymeric material used in rapid prototypes Part I. Mechanical properties in the green state. J. Mater. Process. Technol. 1997, 67, 41–45. [Google Scholar] [CrossRef]
- Fuh, J.Y.H.; Lu, L.; Tan, C.C.; Shen, Z.X.; Chew, S. Processing and characterising photo-sensitive polymer in the rapid prototyping process. J. Mater. Process. Technol. 1999, 89, 211–217. [Google Scholar] [CrossRef]
- Hossain, M.; Liao, Z. An additively manufactured silicone polymer: Thermo-viscoelastic experimental study and computational modelling. Addit. Manuf. 2020, 35, 101395. [Google Scholar] [CrossRef]
- Lee, A.Y.; An, J.; Chua, C.K. Two-Way 4D Printing: A Review on the Reversibility of 3D-Printed Shape Memory Materials. Engineering 2017, 3, 663–674. [Google Scholar] [CrossRef]
- Farjana, N. 3D dentistry—A Boon to Mankind. Int. J. Appl. Res. 2019, 5, 226–229. [Google Scholar]
- Zhang, X.; Zhang, Q.; Meng, X.; Ye, Y.; Feng, D.; Xue, J.; Wang, H.; Huang, H.; Wang, M.; Wang, J. Rheological and Mechanical Properties of Resin-Based Materials Applied in Dental Restorations. Polymers 2021, 13, 2975. [Google Scholar] [CrossRef]
- Kumar, D.S.; Shukla, M.J.; Mahato, K.K.; Rathore, D.K.; Prusty, R.K.; Ray, B.C. Effect of post-curing on thermal and mechanical behavior of GFRP composites. IOP Conf. Ser. Mater. Sci. Eng. 2015, 75, 012012. [Google Scholar] [CrossRef]
- Calheiros, F.C.; Daronch, M.; Rueggeberg, F.A.; Braga, R.R. Degree of conversion and mechanical properties of a BisGMA:TEGDMA composite as a function of the applied radiant exposure. J. Biomed. Mater. Res. 2008, 84, 503–509. [Google Scholar] [CrossRef]
- Leonhardt, S.; Klare, M.; Scheer, M.; Fischer, T.; Cordes, B.; Eblenkamp, M. Biocompatibility of photopolymers for additive manufacturing. Curr. Dir. Biomed. Eng. 2016, 2, 113–116. [Google Scholar] [CrossRef]
- Dos Santos, R.L.; De Sampaio, G.A.; De Carvalho, F.G.; Pithon, M.M.; Guênes, G.M.; Alves, P.M. Influence of Degree of Conversion on the Biocompatibility of Different Composites In Vivo. J. Adhes. Dent. 2014, 16, 15–20. [Google Scholar] [CrossRef]
- Kim, J.-E.; Mangal, U.; Yu, J.-H.; Kim, G.-T.; Kim, H.; Seo, J.-Y.; Cha, J.-Y.; Lee, K.-J.; Kwon, J.-S.; Choi, S.-H. Evaluation of the effects of temperature and centrifugation time on elimination of uncured resin from 3D-printed dental aligners. Sci. Rep. 2024, 14, 15206. [Google Scholar] [CrossRef]
- Salmoria, G.V.; Ahrens, C.H.; Beal, V.E.; Pires, A.T.N.; Soldi, V. Evaluation of post-curing and laser manufacturing parameters on the properties of SOMOS 7110 photosensitive resin used in stereolithography. Mater. Des. 2009, 30, 758–763. [Google Scholar] [CrossRef]
- Lee, M.-J.; Kim, M.-J.; Kwon, J.-S.; Lee, S.-B.; Kim, K.-M. Cytotoxicity of Light-Cured Dental Materials according to Different Sample Preparation Methods. Materials 2017, 10, 288. [Google Scholar] [CrossRef]
- Accorinte, M.D.L.R.; Loguercio, A.D.; Reis, A.; Muench, A.; De Araújo, V.C. Adverse effects of human pulps after direct pulp capping with the different components from a total-etch, three-step adhesive system. Dent. Mater. 2005, 21, 599–607. [Google Scholar] [CrossRef]
- Goldberg, M. In vitro and in vivo studies on the toxicity of dental resin components: A review. Clin. Oral Investig. 2008, 12, 1–8. [Google Scholar] [CrossRef]
- Lefeuvre, M.; Amjaad, W.; Goldberg, M.; Stanislawski, L. TEGDMA induces mitochondrial damage and oxidative stress in human gingival fibroblasts. Biomaterials 2005, 26, 5130–5137. [Google Scholar] [CrossRef]
- Peumans, M.; Van Meerbeek, B.; Lambrechts, P.; Vanherle, G.; Quirynen, M. The Influence of Direct Composite Additions for the Correction of Tooth Form and/or Position on Periodontal Health. A Retrospective Study. J. Periodontol. 1998, 69, 422–427. [Google Scholar] [CrossRef]
- Suh, B.I. Oxygen-Inhibited Layer in Adhesion Dentistry. J. Esthet. Restor. Dent. 2004, 16, 316–323. [Google Scholar] [CrossRef]
- Menzies, K.L.; Jones, L. The Impact of Contact Angle on the Biocompatibility of Biomaterials. Optom. Vis. Sci. 2010, 87, 387–399. [Google Scholar] [CrossRef]
- Aguiar, F.H.B.; Braceiro, A.T.B.; Ambrosano, G.M.B.; Lovadino, J.R. Hardness and diametral tensile strength of a hybrid composite resin polymerized with different modes and immersed in ethanol or distilled water media. Dent. Mater. 2005, 21, 1098–1103. [Google Scholar] [CrossRef]
- Basavarajappa, S.; Al-Kheraif, A.A.A.; ElSharawy, M.; Vallittu, P.K. Effect of solvent/disinfectant ethanol on the micro-surface structure and properties of multiphase denture base polymers. J. Mech. Behav. Biomed. Mater. 2016, 54, 1–7. [Google Scholar] [CrossRef]
- Hansel, C.; Leyhausen, G.; Mai, U.E.H.; Geurtsen, W. Effects of Various Resin Composite (Co)monomers and Extracts on Two Caries-associated Micro-organisms in vitro. J. Dent. Res. 1998, 77, 60–67. [Google Scholar] [CrossRef]
- Hwangbo, N.-K.; Nam, N.-E.; Choi, J.-H.; Kim, J.-E. Effects of the Washing Time and Washing Solution on the Biocompatibility and Mechanical Properties of 3D Printed Dental Resin Materials. Polymers 2021, 13, 4410. [Google Scholar] [CrossRef]
- Alamo, L.; Cassiano, F.B.; Bordini, E.A.F.; Stuani, V.T.; Pacheco, L.E.; Gallinari, M.d.O.; Costa, C.A.S.; Mondelli, R.F.L.; Soares, D.G. An organotypic model of oral mucosa cells for the biological assessment of 3D printed resins for interim restorations. J. Prosthet. Dent. 2024, 132, 251–259. [Google Scholar] [CrossRef]
- Jockusch, J.; Özcan, M. Additive manufacturing of dental polymers: An overview on processes, materials and applications. Dent. Mater. J. 2020, 39, 345–354. [Google Scholar] [CrossRef]
- Ha, S.-W.; Kirch, M.; Birchler, F.; Eckert, K.-L.; Mayer, J.; Wintermantel, E.; Sittig, C.; Pfund-Klingenfuss, I.; Textor, M.; Spencer, N.; et al. Surface activation of polyetheretherketone (PEEK) and formation of calcium phosphate coatings by precipitation. J. Mater. Sci. Mater. Med. 1997, 8, 683–690. [Google Scholar] [CrossRef]
- Kizuki, T.; Matsushita, T.; Kokubo, T. Apatite-forming PEEK with TiO2 surface layer coating. J. Mater. Sci. Mater. Med. 2015, 26, 41. [Google Scholar] [CrossRef]
- Thummawanich, W.; Wiwatwarrapan, C.; Sirichompun, C. Effect of Ultrasonic Bath Immersion on Physical Properties of an MMA-based Orthodontic Base-plate Material. J. Clin. Diagn. Res. 2018, 12, 11. [Google Scholar] [CrossRef]
- Vallittu, P.K.; Ruyter, I.E.; Buykuilmaz, S. Effect of polymerization temperature and time on the residual monomer content of denture base polymers. Eur. J. Oral Sci. 1998, 106, 588–593. [Google Scholar] [CrossRef]
- Hart, L.R.; Li, S.; Sturgess, C.; Wildman, R.; Jones, J.R.; Hayes, W. 3D Printing of Biocompatible Supramolecular Polymers and their Composites. ACS Appl. Mater. Interfaces 2016, 8, 3115–3122. [Google Scholar] [CrossRef]
- Steinhaus, J.; Hausnerova, B.; Moeginger, B.; Harrach, M.; Guenther, D.; Moegele, F. Characterization of the auto-curing behavior of rapid prototyping materials for three-dimensional printing using dielectric analysis. Polym. Eng. Sci. 2015, 55, 1485–1493. [Google Scholar] [CrossRef]
- Pitzanti, G.; Mohylyuk, V.; Corduas, F.; Byrne, N.M.; Coulter, J.A.; Lamprou, D.A. Urethane dimethacrylate-based photopolymerizable resins for stereolithography 3D printing: A physicochemical characterisation and biocompatibility evaluation. Drug Deliv. Transl. Res. 2024, 14, 177–190. [Google Scholar] [CrossRef]
- Aduba, D.C.; Margaretta, E.D.; Marnot, A.E.; Heifferon, K.V.; Surbey, W.R.; Chartrain, N.A.; Whittington, A.R.; Long, T.E.; Williams, C.B. Vat photopolymerization 3D printing of acid-cleavable PEG-methacrylate networks for biomaterial applications. Mater. Today Commun. 2019, 19, 204–211. [Google Scholar] [CrossRef]
- Kumar, A.M.; Khan, A.; Hussein, M.; Khan, M.Y.; Dafalla, H.; Suresh, B.; Ramakrishna, S. Hybrid nanocomposite coatings from PEDOT and BN-TiO2 nanosheets: Enhanced invitro corrosion resistance, wettability and biocompatibility for biomedical applications. Prog. Org. Coat. 2022, 170, 106946. [Google Scholar] [CrossRef]
- Sun, L.; Guo, J.; Chen, H.; Zhang, D.; Shang, L.; Zhang, B.; Zhao, Y. Tailoring Materials with Specific Wettability in Biomedical Engineering. Adv. Sci. 2021, 8, 2100126. [Google Scholar] [CrossRef]
- Syed, M. Allergic Reactions to Dental Materials—A Systematic Review. J. Clin. Diagn. Res. 2015, 9, ZE04–ZE09. [Google Scholar] [CrossRef]
- Tammaro, L.; Vittoria, V.; Calarco, A.; Petillo, O.; Riccitiello, F.; Peluso, G. Effect of layered double hydroxide intercalated with fluoride ions on the physical, biological and release properties of a dental composite resin. J. Dent. 2014, 42, 60–67. [Google Scholar] [CrossRef]
- Thaitammayanon, P.; Sirichompun, C.; Wiwatwarrapan, C. Ultrasonic treatment reduced residual monomer in methyl methacrylate-based orthodontic base-plate materials. Dent. Oral Craniofacial Res. 2017, 4, 1–5. [Google Scholar] [CrossRef]
- Bacali, C.; Baldea, I.; Moldovan, M.; Carpa, R.; Olteanu, D.E.; Filip, G.A.; Nastase, V.; Lascu, L.; Badea, M.; Constantiniuc, M.; et al. Flexural strength, biocompatibility, and antimicrobial activity of a polymethyl methacrylate denture resin enhanced with graphene and silver nanoparticles. Clin. Oral Investig. 2020, 24, 2713–2725. [Google Scholar] [CrossRef]
- Baldi, A.; Carossa, M.; Comba, A.; Alovisi, M.; Femiano, F.; Pasqualini, D.; Berutti, E.; Scotti, N. Wear Behaviour of Polymer-Infiltrated Network Ceramics, Lithium Disilicate and Cubic Zirconia against Enamel in a Bruxism-Simulated Scenario. Biomedicines 2022, 10, 1682. [Google Scholar] [CrossRef]
- Barillet, S.; Jugan, M.-L.; Laye, M.; Leconte, Y.; Herlin-Boime, N.; Reynaud, C.; Carrière, M. In vitro evaluation of SiC nanoparticles impact on A549 pulmonary cells: Cyto-, genotoxicity and oxidative stress. Toxicol. Lett. 2010, 198, 324–330. [Google Scholar] [CrossRef]
- Elshahawy, W.M.; Watanabe, I.; Kramer, P. In vitro cytotoxicity evaluation of elemental ions released from different prosthodontic materials. Dent. Mater. 2009, 25, 1551–1555. [Google Scholar] [CrossRef]
- Hazeveld, A.; Slater, J.J.R.H.; Ren, Y. Accuracy and reproducibility of dental replica models reconstructed by different rapid prototyping techniques. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Kedia, S.; Checker, R.; Sandur, S.K.; Nilaya, J.P. Picosecond laser-induced hybrid groove structures on Ti-6Al-4V bio-alloy to accelerate osseointegration. J. Biomed. Mater. Res. 2023, 111, 1775–1784. [Google Scholar] [CrossRef] [PubMed]
- Nelson, S.K.; Wataha, J.C.; Lockwoodc, P.E. Accelerated toxicity testing of casting alloys and reduction of intraoral release of elements. J. Prosthet. Dent. 1999, 81, 715–720. [Google Scholar] [CrossRef] [PubMed]
- Wankhede, V.; Untawale, S.; Jaju, S. Comprehensive study & Innovative trends in dentistry along with variations. In Proceedings of the 2024 International Conference on Innovations and Challenges in Emerging Technologies (ICICET), Nagpur, India, 7–8 June 2024; IEEE: New York, NY, USA, 2024; pp. 1–7. [Google Scholar] [CrossRef]
- Kanďarova, H.; Pôbiš, P. The ‘Big Three’ in biocompatibility testing of medical devices: Implementation of alternatives to animal experimentation—Are we there yet? Front. Toxicol. 2024, 5, 1337468. [Google Scholar] [CrossRef] [PubMed]
- Kollmuss, M.; Edelhoff, D.; Schwendicke, F.; Wuersching, S.N. In Vitro Cytotoxic and Inflammatory Response of Gingival Fibroblasts and Oral Mucosal Keratinocytes to 3D Printed Oral Devices. Polymers 2024, 16, 1336. [Google Scholar] [CrossRef]
- Riss, T.L.; Moravec, R.A.; Niles, A.L.; Duellman, S.; Benink, H.A.; Worzella, T.J.; Minor, L. Cell Viability Assays. In Assay Guidance Manual; Markossian, S., Grossman., A., Arkin, M., Auld, D., Austin, C., Baell, J., Brimacombe, K., Chung, T.D.Y., Coussens, N.P., Dahlin, J.L., et al., Eds.; Eli Lilly & Company and the National Center for Advancing Translational Sciences: Bethesda, MD, USA, 2004. Available online: http://www.ncbi.nlm.nih.gov/books/NBK144065/ (accessed on 5 November 2024).
- Rogers, H.B.; Zhou, L.T.; Kusuhara, A.; Zaniker, E.; Shafaie, S.; Owen, B.C.; Duncan, F.E.; Woodruff, T.K. Dental resins used in 3D printing technologies release ovo-toxic leachates. Chemosphere 2021, 270, 129003. [Google Scholar] [CrossRef]
- Chuchulska, B.; Dimitrova, M.; Vlahova, A.; Hristov, I.; Tomova, Z.; Kazakova, R. Comparative Analysis of the Mechanical Properties and Biocompatibility between CAD/CAM and Conventional Polymers Applied in Prosthetic Dentistry. Polymers 2024, 16, 877. [Google Scholar] [CrossRef]
- Kucher, M.; Dannemann, M.; Modler, N.; Hannig, C.; Weber, M.-T. Effects of Endodontic Irrigants on Material and Surface Properties of Biocompatible Thermoplastics. Dent. J. 2019, 7, 26. [Google Scholar] [CrossRef]
- Imazato, S.; Horikawa, D.; Nishida, M.; Ebisu, S. Effects of monomers eluted from dental resin restoratives on osteoblast-like cells. J. Biomed. Mater. Res. 2009, 88, 378–386. [Google Scholar] [CrossRef]
- Wedekind, L.; Güth, J.-F.; Schweiger, J.; Kollmuss, M.; Reichl, F.-X.; Edelhoff, D.; Högg, C. Elution behavior of a 3D-printed, milled and conventional resin-based occlusal splint material. Dent. Mater. 2021, 37, 701–710. [Google Scholar] [CrossRef]
- Gruber, S.; Nickel, A. Toxic or not toxic? The specifications of the standard ISO 10993-5 are not explicit enough to yield comparable results in the cytotoxicity assessment of an identical medical device. Front. Med. Technol. 2023, 5, 1195529. [Google Scholar] [CrossRef]
| Tipe of Materials | Manufactured Pieces | Temperature Range Processing (FST) | Hardness Vickers and Martens Methods (N/mm2) | References |
|---|---|---|---|---|
| Synthetic polymers: Polyether ether ketone (PEEK), polycaprolactone (PCL), polymethyl methacrylate (PMMA), polylactic acid (PLA), poly(lactic-co-glycolic acid) (PLGA), and ultraviolet (UV) resins. | AM-printed occlusal appliances; Clear aligners; Crown or bridge copings; Implant abutments; 3D-printed denture teeth. | Between 58 °C and 430 °C, various periods of time depending on the designed pieces to be printed. | 142–2926 | [45,46,47,48,49,50,51,52,53] |
| Metals and metal alloys: Titanium (Ti) and cobalt-chromium (Co-Cr) alloys. | Implants, prosthetics, dental restorations. | 900–2370 °C | 44.3–286 GPa | [46,47,48,49,52,53,54,55,56] |
| Ceramics: Glass, zirconia, alumina. | Dental implants; Prosthetic implant abutments; Bridges; Root posts; Ceramic crown. | 800–1600 °C | 30–800 MPa 0.7–5 MPa·m 1/2 | [49,53,57,58,59,60,61,62,63] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rus, F.; Neculau, C.; Imre, M.; Duica, F.; Popa, A.; Moisa, R.M.; Voicu-Balasea, B.; Radulescu, R.; Ripszky, A.; Ene, R.; et al. Polymeric Materials Used in 3DP in Dentistry—Biocompatibility Testing Challenges. Polymers 2024, 16, 3550. https://doi.org/10.3390/polym16243550
Rus F, Neculau C, Imre M, Duica F, Popa A, Moisa RM, Voicu-Balasea B, Radulescu R, Ripszky A, Ene R, et al. Polymeric Materials Used in 3DP in Dentistry—Biocompatibility Testing Challenges. Polymers. 2024; 16(24):3550. https://doi.org/10.3390/polym16243550
Chicago/Turabian StyleRus, Florentina, Cristina Neculau, Marina Imre, Florentina Duica, Alexandra Popa, Radu Mihai Moisa, Bianca Voicu-Balasea, Radu Radulescu, Alexandra Ripszky, Razvan Ene, and et al. 2024. "Polymeric Materials Used in 3DP in Dentistry—Biocompatibility Testing Challenges" Polymers 16, no. 24: 3550. https://doi.org/10.3390/polym16243550
APA StyleRus, F., Neculau, C., Imre, M., Duica, F., Popa, A., Moisa, R. M., Voicu-Balasea, B., Radulescu, R., Ripszky, A., Ene, R., & Pituru, S. (2024). Polymeric Materials Used in 3DP in Dentistry—Biocompatibility Testing Challenges. Polymers, 16(24), 3550. https://doi.org/10.3390/polym16243550








