Thermal Sensing of Photo-Activated Dental Resin Composites Using Infrared Thermography
Abstract
:1. Introduction
2. Materials and Methods
2.1. Tested Materials
2.2. Specimen Preparation
2.3. Heat-Measuring Systems
2.4. Cavity Restoration and Temperature Measurements
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
6. Highlights
- The thermal camera is a non-invasive technique that can provide instant data comparable to conventional methods.
- The elevation in dental composite temperature was mainly related to the filling technique.
- The chemical composition of the dental composite has no direct influence on heat retention in the material.
7. Clinical Application of This Research
- Material Selection: Dentists can make informed decisions about which composite materials to use for specific cases. For deep or large cavities where there is a higher risk of elevated temperatures, they may opt for materials with lower heat generation during polymerization to minimize the potential harm to the pulp.
- Monitoring: During composite placement, clinicians can monitor the temperature using tools or techniques to ensure it remains within a safe range. This proactive approach allows for adjustments as needed to prevent overheating.
- Patient Education: Dentists can better educate patients about post-operative sensitivity and symptoms to be expected after placing composite restorations. This understanding enables patients to recognize signs of pulp irritation and seek assistance if necessary.
- Research and Development: The information about increased temperature upon polymerization can be used by dental materials manufacturers to develop novel composite materials with superior properties, such as lower heat generation during polymerization to improve patient safety and comfort.
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cavalcanti, B.N.; Otani, C.; Rode, S.M. High-speed cavity preparation techniques with different water flows. J. Prosthet. Dent. 2002, 87, 158–161. [Google Scholar] [CrossRef] [PubMed]
- Schneider, L.F.; Consani, S.; Correr-Sobrinho, L.; Correr, A.B.; Sinhoreti, M.A. Halogen and LED light curing of composite: Temperature increase and Knoop hardness. Clin. Oral Investig. 2006, 10, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Kwon, S.-J.; Park, Y.-J.; Jun, S.-H.; Ahn, J.-S.; Lee, I.-B.; Cho, B.-H.; Son, H.-H.; Seo, D.-G. Thermal irritation of teeth during dental treatment procedures. Restor. Dent. Endod. 2013, 38, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Al-Qudah, A.A.; Mitchell, C.A.; Biagioni, P.A.; Hussey, D.L. Effect of composite shade, increment thickness and curing light on temperature rise during photocuring. J. Dent. 2007, 35, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Yam, F.; Hassan, Z. Innovative advances in LED technology. Microelectron. J. 2005, 36, 129–137. [Google Scholar] [CrossRef]
- Bakhsh, T.A.; Tagami, J.; Sadr, A.; Luong, M.N.; Turkistani, A.; Almhimeed, Y.; Alshouibi, E. Effect of light irradiation condition on gap formation under polymeric dental restoration; OCT study. Z. Med. Phys. 2020, 30, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Bouillaguet, S.; Caillot, G.; Forchelet, J.; Cattani-Lorente, M.; Wataha, J.C.; Krejci, I. Thermal risks from LED- and high-intensity QTH-curing units during polymerization of dental resins. J. Biomed. Mater. Res. B Appl. Biomater. 2005, 72, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Rosatto, C.M.; Bicalho, A.; Veríssimo, C.; Bragança, G.; Rodrigues, M.; Tantbirojn, D.; Versluis, A.; Soares, C. Mechanical properties, shrinkage stress, cuspal strain and fracture resistance of molars restored with bulk-fill composites and incremental filling technique. J. Dent. 2015, 43, 1519–1528. [Google Scholar] [CrossRef]
- Rudrapati, L.; Chandrasekhar, V.; Badami, V.; Tummala, M. Incremental techniques in direct composite restoration. J. Conserv. Dent. 2017, 20, 386–391. [Google Scholar] [CrossRef]
- Bakhsh, T.A.; Sadr, A.; Shimada, Y.; Mandurah, M.M.; Hariri, I.; Alsayed, E.Z.; Tagami, J.; Sumi, Y. Concurrent evaluation of composite internal adaptation and bond strength in a class-I cavity. J. Dent. 2013, 41, 60–70. [Google Scholar] [CrossRef]
- Bakhsh, T.A.; Sadr, A.; Shimada, Y.; Turkistani, A.; Abuljadayel, R.; Tagami, J. Does lining class-II cavities with flowable composite improve the interfacial adaptation? J. Adhes. Sci. Technol. 2020, 34, 400–416. [Google Scholar] [CrossRef]
- Leprince, J.G.; Palin, W.M.; Vanacker, J.; Sabbagh, J.; Devaux, J.; Leloup, G. Physico-mechanical characteristics of commercially available bulk-fill composites. J. Dent. 2014, 42, 993–1000. [Google Scholar] [CrossRef] [PubMed]
- Bakhsh, T.A.; Yagmoor, M.A.; Alsadi, F.M.; Jamleh, A. Evaluation of Vickers hardness of bulk-fill composites cured by different light sources. In Proceedings of the Lasers in Dentistry XXII, SPIE BiOS, San Francisco, CA, USA, 13–18 February 2016; SPIE: Bellingham, WA, USA, 2016; Volume 9692. [Google Scholar]
- Reis, A.F.; Vestphal, M.; Amaral, R.C.D.; Rodrigues, J.A.; Roulet, J.-F.; Roscoe, M.G. Efficiency of polymerization of bulk-fill composite resins: A systematic review. Braz. Oral Res. 2017, 31 (Suppl. S1), e59. [Google Scholar] [CrossRef] [PubMed]
- Francesco, P.; Gabriele, C.; Fiorillo, L.; Giuseppe, M.; Antonella, S.; Giancarlo, B.; Mirta, P.; Tribst, J.P.M.; Giudice, R.L. The Use of Bulk Fill Resin-Based Composite in the Sealing of Cavity with Margins in Radicular Cementum. Eur. J. Dent. 2022, 16, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Demarco, F.F.; Conde, M.C.M.; Cavalcanti, B.N.; Casagrande, L.; Sakai, V.T.; Nör, J.E. Dental pulp tissue engineering. Braz. Dent. J. 2011, 22, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Zach, L.; Cohen, G. Pulp Response to Externally Applied Heat. Oral Surg. Oral Med. Oral Pathol. 1965, 19, 515–530. [Google Scholar] [CrossRef] [PubMed]
- Mouhat, M.; Mercer, J.; Stangvaltaite, L.; Örtengren, U. Light-curing units used in dentistry: Factors associated with heat development-potential risk for patients. Clin. Oral Investig. 2017, 21, 1687–1696. [Google Scholar] [CrossRef] [PubMed]
- Hamze, F.; Nasab, S.A.G.; Eskandarizade, A.; Shahravan, A.; Fard, F.A.; Sinaee, N. Thermal Scanning of Dental Pulp Chamber by Thermocouple System and Infrared Camera during Photo Curing of Resin Composites. Iran. Endod. J. 2018, 13, 195–199. [Google Scholar]
- Khajuria, R.R.; Madan, R.; Agarwal, S.; Gupta, R.; Vadavadgi, S.V.; Sharma, V. Comparison of temperature rise in pulp chamber during polymerization of materials used for direct fabrication of provisional restorations: An in-vitro study. Eur. J. Dent. 2015, 9, 194–200. [Google Scholar] [CrossRef]
- Bakhsh, T.A.; Bakhsh, A.; Shokry, Y.; Jamleh, A. Assessment of thermal changes in different restorative materials using a thermal camera. In Proceedings of the Lasers in Dentistry XXVI, San Francisco, CA, USA, 1–6 February 2020; Volume 11217. [Google Scholar]
- Zhao, H.; Chen, Z.; Zhao, R.; Feng, L. Exceptional point engineered glass slide for microscopic thermal mapping. Nat. Commun. 2018, 9, 1764. [Google Scholar] [CrossRef]
- Vaidyanathan, T.K.; Vaidyanathan, J.; Lizymol, P.P.; Ariya, S.; Krishnan, K.V. Study of visible light activated polymerization in BisGMA-TEGDMA monomers with Type 1 and Type 2 photoinitiators using Raman spectroscopy. Dent. Mater. 2017, 33, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Rice, C.A.; Riehl, J.; Broman, K.; Soukup, J.W.; Gengler, W.R. Comparing the degree of exothermic polymerization in commonly used acrylic and provisional composite resins for intraoral appliances. J. Vet. Dent. 2012, 29, 78–83. [Google Scholar] [CrossRef] [PubMed]
- Kim, R.J.-Y.; Son, S.-A.; Hwang, J.-Y.; Lee, I.-B.; Seo, D.-G. Comparison of photopolymerization temperature increases in internal and external positions of composite and tooth cavities in real time: Incremental fillings of microhybrid composite vs. bulk filling of bulk fill composite. J. Dent. 2015, 43, 1093–1098. [Google Scholar] [CrossRef] [PubMed]
- Devaux, J.; Mullier, T.; Vreven, J.; Leloup, G.; Leprince, J.D.J.; AlShaafi, M.; Harlow, J.; Price, H.; Rueggeberg, F.; Labrie, D.; et al. Pulpal-temperature rise and polymerization efficiency of LED curing lights. Oper. Dent. 2010, 35, 220–230. [Google Scholar]
- Kim, R.J.-Y.; Lee, I.-B.; Yoo, J.-Y.; Park, S.-J.; Kim, S.-Y.; Yi, Y.-A.; Hwang, J.-Y.; Seo, D.-G. Real-Time Analysis of Temperature Changes in Composite Increments and Pulp Chamber during Photopolymerization. BioMed Res. Int. 2015, 2015, 923808. [Google Scholar] [CrossRef] [PubMed]
- Lau, X.E.; Liu, X.; Chua, H.; Wang, W.J.; Dias, M.; Choi, J.J.E. Heat generated during dental treatments affecting intrapulpal temperature: A review. Clin. Oral Investig. 2023, 27, 2277–2297. [Google Scholar] [CrossRef] [PubMed]
- Fu, L.; Engqvist, H.; Xia, W. Glass-Ceramics in Dentistry: A Review. Materials 2020, 13, 1049. [Google Scholar] [CrossRef]
- Schechtel, E.; Yan, Y.; Xu, X.; Cang, Y.; Tremel, W.; Wang, Z.; Li, B.; Fytas, G. Elastic Modulus and Thermal Conductivity of Thiolene/TiO2 Nanocomposites. J. Phys. Chem. C Nanomater. Interfaces 2017, 121, 25568–25575. [Google Scholar] [CrossRef]
- Rehman, S.U.; Javaid, S.; Shahid, M.; Ahmad, N.M.; Rashid, B.; Szczepanski, C.R.; Shahzad, A. The Synergistic Effect of Polystyrene/Modified Boron Nitride Composites for Enhanced Mechanical, Thermal and Conductive Properties. Polymers 2023, 15, 235. [Google Scholar] [CrossRef]
- Behery, H.; El-Mowafy, O.; El-Badrawy, W.; Nabih, S.; Saleh, B. Gingival microleakage of class II bulk-fill composite resin restorations. Dent. Med. Probl. 2018, 55, 383–388. [Google Scholar] [CrossRef]
- Al-Harbi, F.; Kaisarly, D.; Bader, D.; El Gezawi, M. Marginal Integrity of Bulk Versus Incremental Fill Class II Composite Restorations. Oper. Dent. 2016, 41, 146–156. [Google Scholar] [CrossRef]
- Turkistani, A.; Ata, A.; Alhammad, R.; Ghurab, R.; Alahmadi, Y.; Shuman, M.; Jamleh, A.; Naguib, G.; Bakhsh, T. Bulk-fill composite marginal adaptation evaluated by cross-polarization optical coherence tomography. Cogent Eng. 2019, 6, 1643976. [Google Scholar] [CrossRef]
- Teshima, W.; Nomura, Y.; Ikeda, A.; Kawahara, T.; Okazaki, M.; Nahara, Y. Thermal degradation of photo-polymerized BisGMA/TEGDMA-based dental resins. Polym. Degrad. Stab. 2004, 84, 167–172. [Google Scholar] [CrossRef]
- Shortall, A.; El-Mahy, W.; Stewardson, D.; Addison, O.; Palin, W. Initial fracture resistance and curing temperature rise of ten contemporary resin-based composites with increasing radiant exposure. J. Dent. 2013, 41, 455–463. [Google Scholar] [CrossRef]




| Material | Manufacture (Country) | Composition (% by Wt) |
|---|---|---|
| Filtek Z350 XT Flowable Restorative | 3M ESPE (USA) |
|
| Filtek Bulk Fill Flowable Restorative | 3M ESPE (USA) |
|
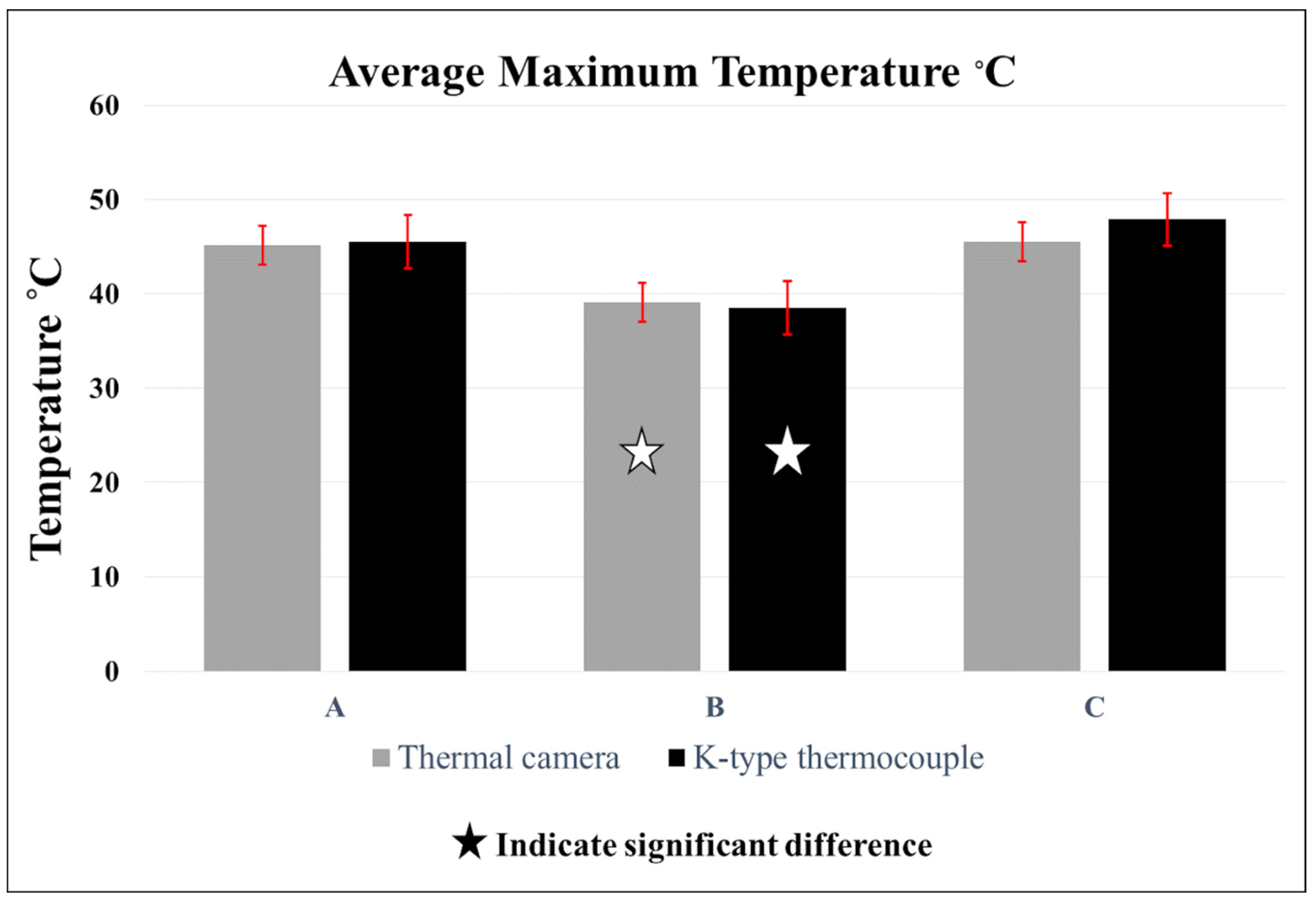
| Group | Filling Technique |
|---|---|
| A | Incremental: Filtek Z350 XT Flowable Restorative composite, 3 incremental layers. |
| B | Bulk: Filtek Bulk Fill Flowable Restorative composite, one layer. |
| C | Incremental: Filtek Bulk Fill Flowable Restorative composite, 3 incremental layers. |
| Average Maximum Temperature °C (±SD) | |||
|---|---|---|---|
| Group A | Group B | Group C | |
| IRT Camera | 45.12 °C (±2.7) aA | 39.14 °C (±1.8) bA | 45.52 °C (±2.4) aA |
| Thermocouple | 45.54 °C (±2.7) aA | 38.54 °C (±2.3) bA | 47.88 °C (±1.9) aA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bakhsh, T.A.; Alfaifi, A.; Alghamdi, Y.; Nassar, M.; Abuljadyel, R.A. Thermal Sensing of Photo-Activated Dental Resin Composites Using Infrared Thermography. Polymers 2023, 15, 4117. https://doi.org/10.3390/polym15204117
Bakhsh TA, Alfaifi A, Alghamdi Y, Nassar M, Abuljadyel RA. Thermal Sensing of Photo-Activated Dental Resin Composites Using Infrared Thermography. Polymers. 2023; 15(20):4117. https://doi.org/10.3390/polym15204117
Chicago/Turabian StyleBakhsh, Turki A., Abdulaziz Alfaifi, Yousef Alghamdi, Mohannad Nassar, and Roaa A. Abuljadyel. 2023. "Thermal Sensing of Photo-Activated Dental Resin Composites Using Infrared Thermography" Polymers 15, no. 20: 4117. https://doi.org/10.3390/polym15204117
APA StyleBakhsh, T. A., Alfaifi, A., Alghamdi, Y., Nassar, M., & Abuljadyel, R. A. (2023). Thermal Sensing of Photo-Activated Dental Resin Composites Using Infrared Thermography. Polymers, 15(20), 4117. https://doi.org/10.3390/polym15204117









