Marginal Micro-Seal and Tensile Bond Strength of a Biopolymer Hybrid Layer Coupled with Dental Prosthesis Using a Primerless-Wet System
Abstract
1. Introduction
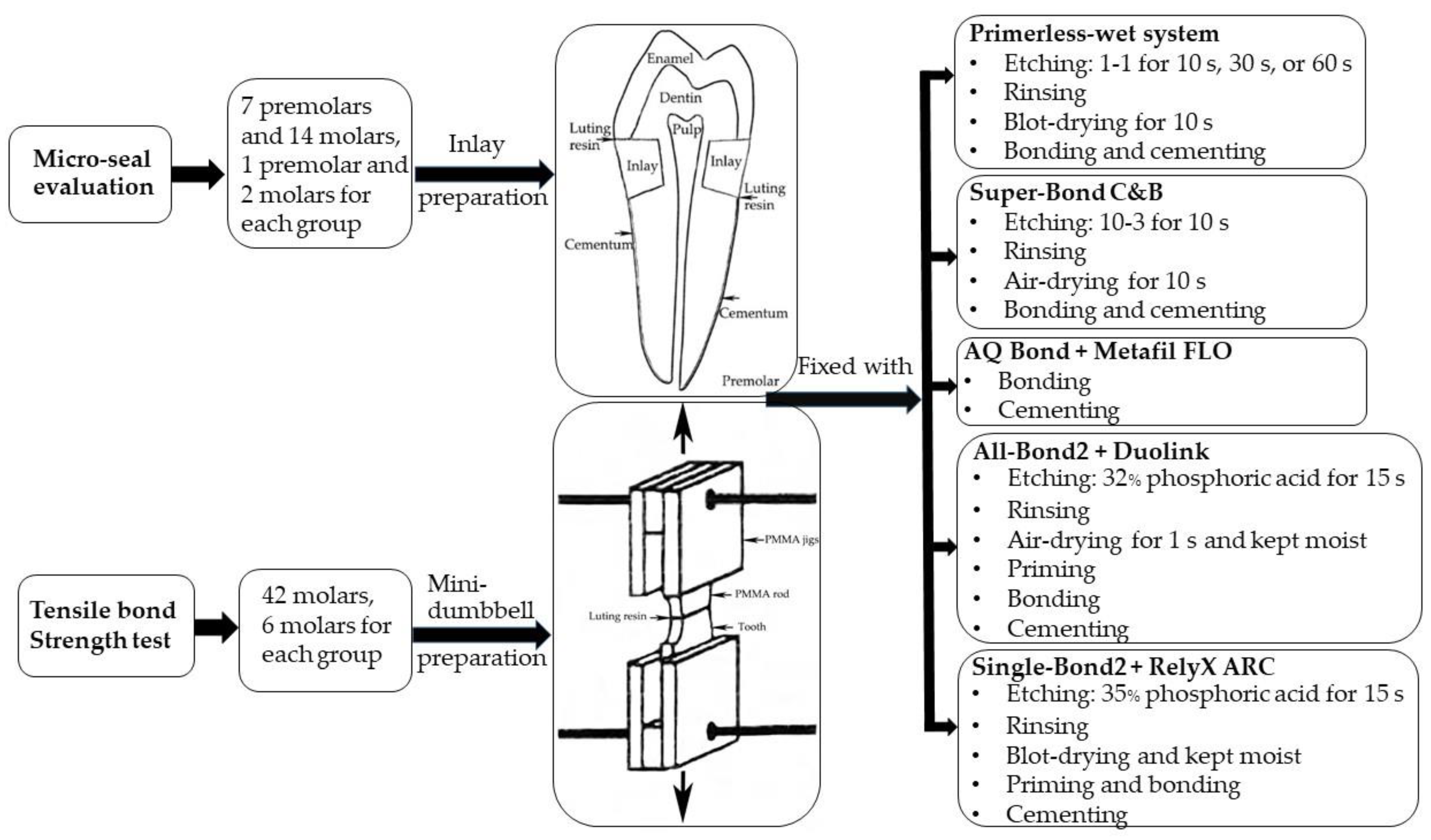
2. Materials and Methods
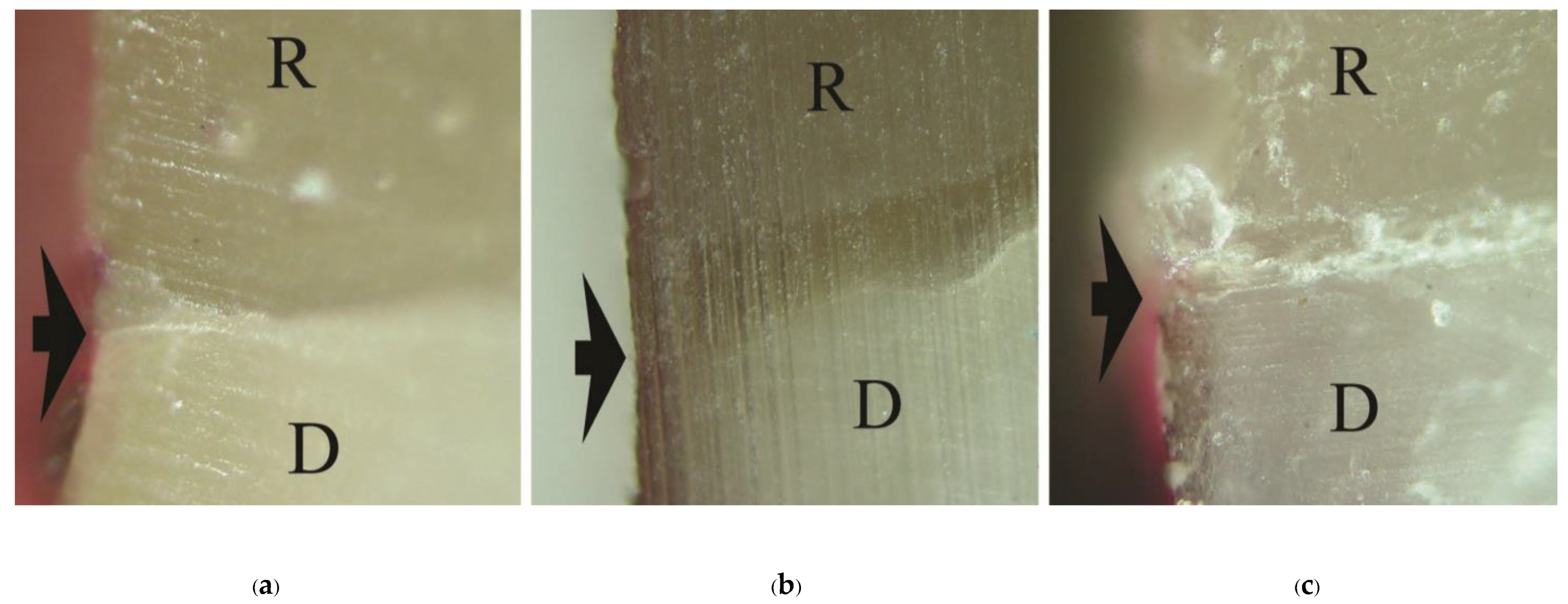
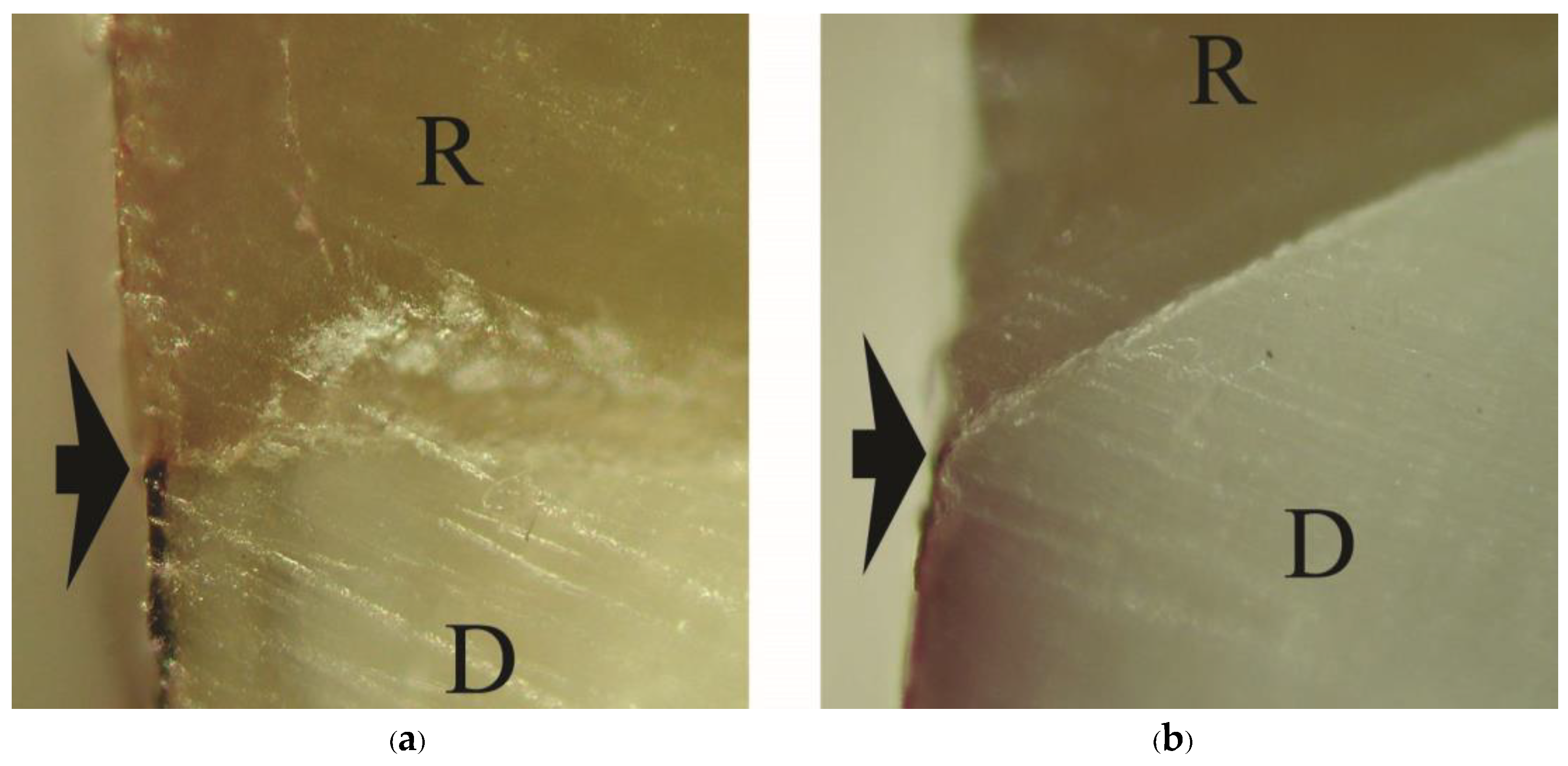
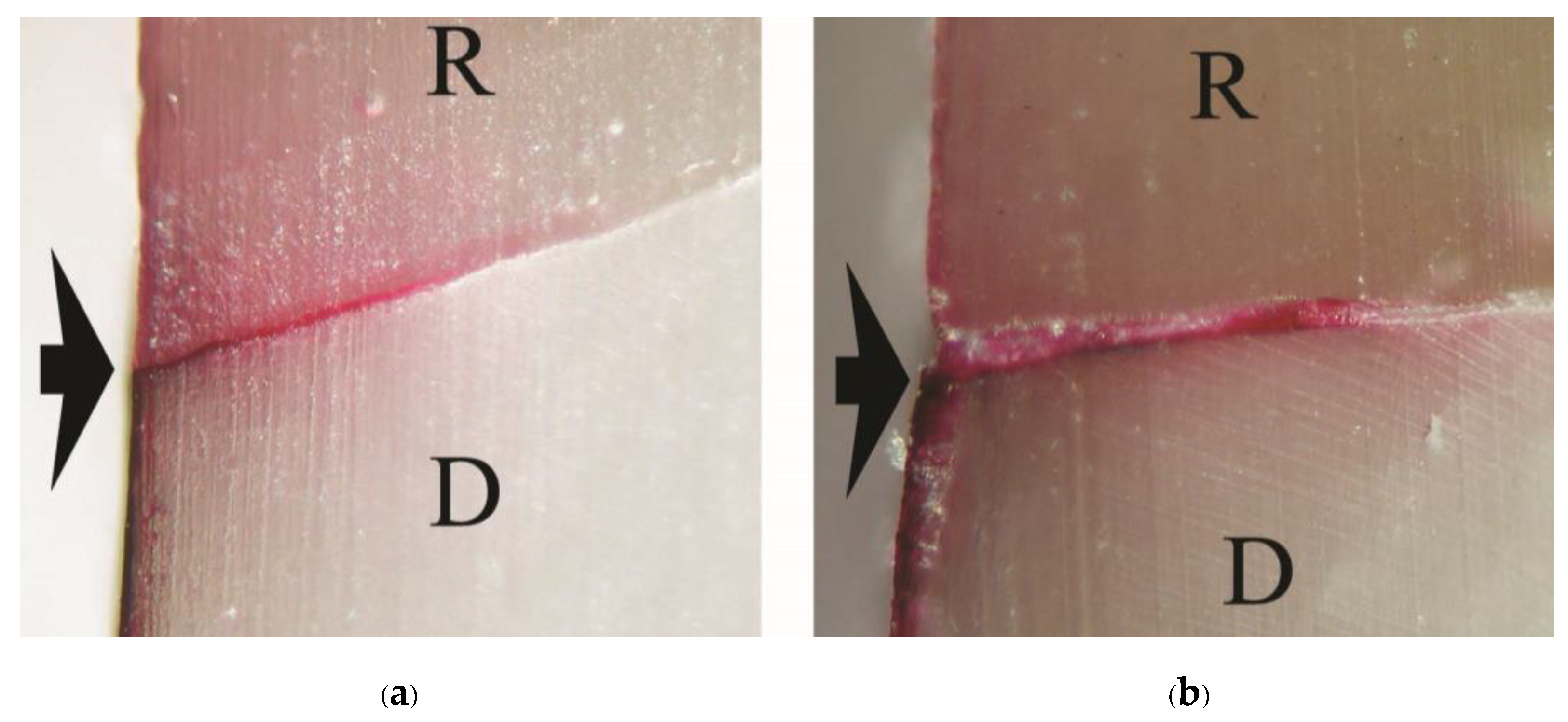
2.1. Micro-Seal Evaluation Using Dye Penetration
2.2. Tensile Bond Strength Test
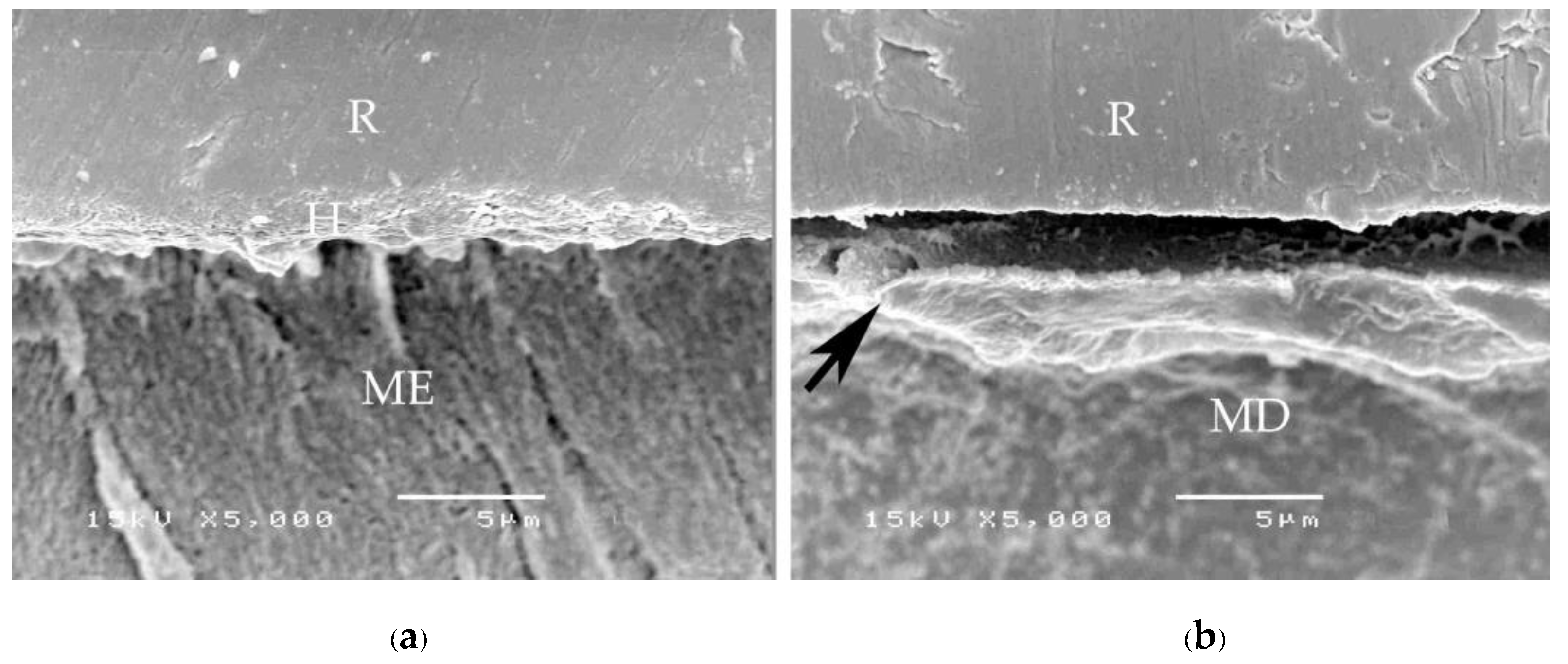
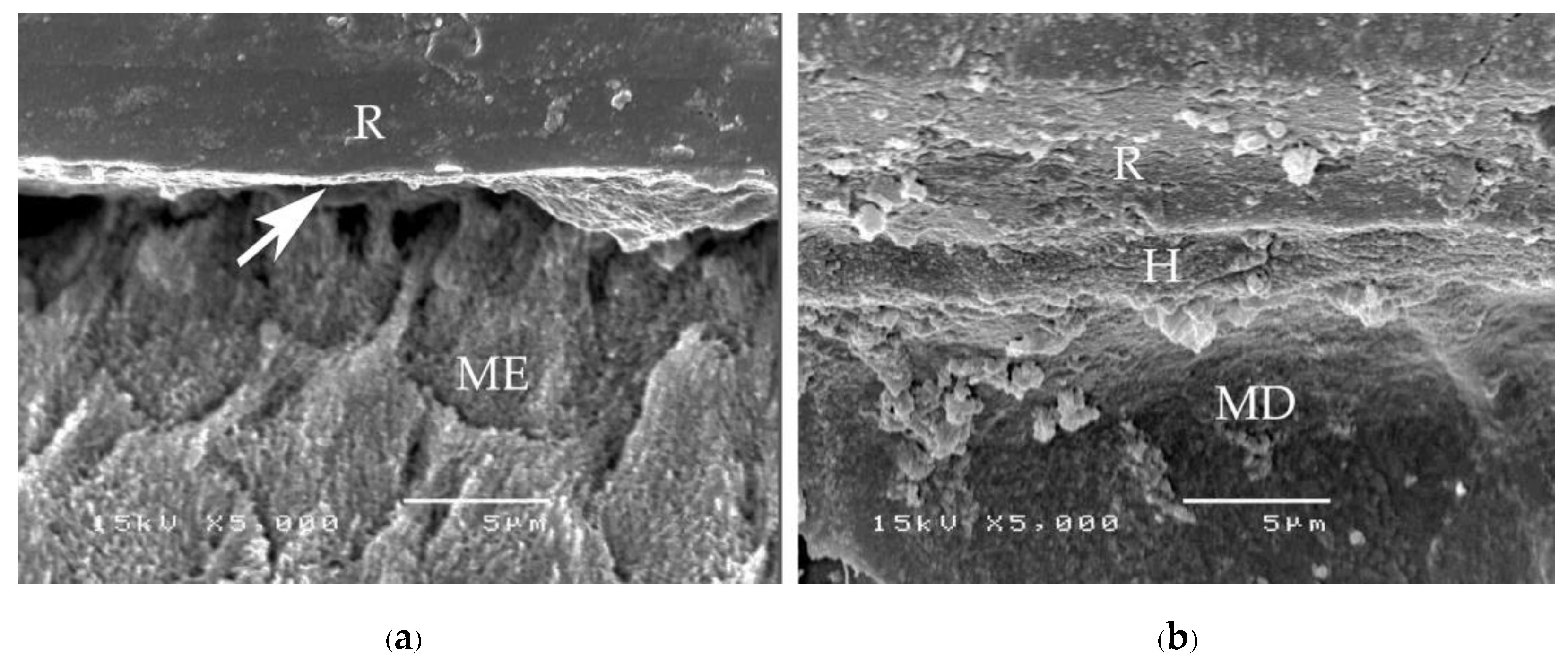
2.3. Characteristics Evaluation of Tooth-Resin Interfacial Biopolymer Layer
2.4. Statistical Analysis
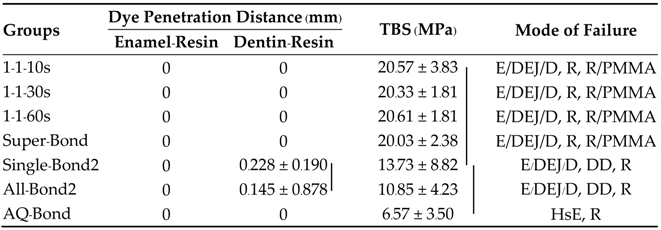
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Anusavice, K.J.; Shen, C.; Rawls, H.R. Phillips’s Science of Dental Materials, 12th ed.; Saunders: Philadelphia, PA, USA, 2013; pp. 309–313. [Google Scholar]
- Nakabayashi, N.; Pashley, D.H. Hybridization of Dental Hard Tissue; Quintessence: Tokyo, Japan, 1998; pp. 13–14, 76–77. [Google Scholar]
- Shinchi, M.J.; Soma, K.; Nakabayashi, N. The effect of phosphoric acid concentration on resin tag length and bond strength of a photo-cured resin to acid-etched enamel. Dent. Mater. 2000, 16, 324–329. [Google Scholar] [CrossRef] [PubMed]
- Inokoshi, S.; Hosoda, H.; Harniratissai, C.; Shimida, Y.; Tatsumi, T. A study on the resin-impregnated layer of dentin. Part A. Comparative study on the decalcified and undecalcified sections and the application of argon ion beam etching to disclose the resin-impregnated layer of dentin. Jpn. J. Conser Dent. 1990, 33, 427–442. [Google Scholar]
- Tay, F.R.; Gwinnett, A.J.; Wei, S.H. The overwet phenomenon: A scanning electron microscopic study of surface moisture in the acid-conditioned, resin-dentin interface. Am. J. Dent. 1996, 9, 109–114. [Google Scholar] [PubMed]
- Piemjai, M.; Watanabe, A.; Iwasaki, Y.; Nakabayashi, N. Effect of remaining demineralised dentin on dental microleakage ac-cessed by a dye penetration: How to inhibit microleakage? J. Dent. 2004, 32, 495–501. [Google Scholar] [CrossRef]
- Piemjai, M.; Waleepitackdej, O.; Garcia-Godoy, F.; Nakabayashi, N. Dentin protection by a primer-less adhesive technique. Am. J. Dent. 2011, 24, 284–288. [Google Scholar]
- Piemjai, M.; Chantarawej, P.; Nakabayashi, N.; Garcia-Godoy, F. Prognosis test by visualization of demineralized dentin under restorations to prevent initial wall-lesions initiated by lactic acid. Am. J. Dent. 2017, 30, 119–124. [Google Scholar]
- Piemjai, M.; Chantarawej, P.; Nakabayashi, N. Evaluation of caries-free restorations bonded with various adhesive systems: In-vitro study. Int. J. Dent. 2020, 2020, 5859835. [Google Scholar] [CrossRef]
- Piemjai, M.; Nakabayashi, N. Effect of dentin conditioners on wet bonding of 4- META/MMA-TBB resin. J. Adhesive Dent. 2001, 3, 325–331. [Google Scholar]
- Iwasaki, Y.; Toida, T.; Nakabayashi, N. Improved wet bonding of methyl methacrylate-tri-n-butylborane resin to dentin etched with ten percent phosphoric acid in the presence of ferric ions. J. Biomed. Mater. Res. 2004, 68A, 566–572. [Google Scholar] [CrossRef]
- Watanabe, I.; Nakabayashi, N. Bonding durability of Photocured phenyl-P in TEGDMA to smear layer—Retained bovine dentin. Quintessence Int. 1993, 24, 335–342. [Google Scholar]
- Piemjai, M.; Thaveeratana, A.; Nakabayashi, N. Marginal integrity between a prefabricated composite block and enamel, DEJ and dentin bonded by three adhesive resins. Am. J. Dent. 2010, 23, 285–291. [Google Scholar] [PubMed]
- Monticelli, F.; Osorio, R.; Mazzitelli, C.; Ferrari, M.; Toledado, M. Limited decalcification/diffusion of self-adhesive cements into dentin. J. Dent. Res. 2008, 87, 974–979. [Google Scholar] [CrossRef] [PubMed]
- Sengar, E.V.; Mulay, S.; Beri, L.; Gupta, A.; Almohareb, T.; Binalrimal, S.; Robaian, A.; Bahammam, M.A.; Bahammam, H.A.; Bahammam, S.A.; et al. Comparative evaluation of microleakage of flowable composite resin using etch and rinse, self-etch adhesive systems, and self-adhesive flowable composite resin in Class V cavities: Confocal laser microscopic study. Materials 2022, 15, 4963. [Google Scholar] [CrossRef] [PubMed]
- Koibuchi, H.; Yasuda, N.; Nakabayashi, N. Bonding to dentin with a self-etching primer: The effect of smear layers. Dent. Mater. 2001, 17, 122–126. [Google Scholar] [CrossRef] [PubMed]
- Piemjai, M.; Waleepitackdej, O.; Nakabayashi, N. Influence of dentin substrates to simplify wet-bonding: A leakage-free and reliable tensile strength interface for long-lasting restorations. J. Biomed. Mater. Res. 2011, 99B, 321–327. [Google Scholar] [CrossRef]
- Manhart, J.; Chen, H.Y.; Hamm, G.; Hickel, R. Buonocore memorial lecture: Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. Oper Dent. 2004, 29, 481–508. [Google Scholar]
- De Backer, H.; Van Maele, G.; De Moor, N.; Van den Berghe, L.; De Boever, J. An 18-year retrospective survival study of full crowns with or without posts. Int. J. Prosthodont. 2006, 19, 136–142. [Google Scholar]
- Walton, T.R. The up to 25-year survival and clinical performance of 2,340 high gold-based metal-ceramic single crowns. Int. J. Prosthodont. 2013, 26, 151–160. [Google Scholar] [CrossRef]
- Piemjai, M.; Adunphichet, N. Impact of hybrid layer formation on the 15-year survival, complications and failures of full-coverage retainers. J. Prosthodont. Res. 2022, 66, 131–140. [Google Scholar] [CrossRef]
- Bart, I.; Dobler, B.; Schmidlin, K.; Zwahlen, M.; Salvi, G.E.; Lang, N.P.; Bragger, U. Complication and failure rates of tooth-supported fixed dental prostheses after 7 to 19 years in function. Int. J. Prosthodont. 2012, 25, 360–367. [Google Scholar]
- Beier, U.S.; Kapferer, I.; Dumfahrt, H. Clinical long-term evaluation and failure characteristics of 1,335 all-ceramic restorations. Int. J. Prosthodont. 2012, 25, 70–78. [Google Scholar] [PubMed]
- Kenyon, B.J.; Frederickson, D.; Hagge, M.S. Gingival seal of deep Class II direct and indirect composite restorations. Am. J. Dent. 2007, 21, 3–6. [Google Scholar]
- Piemjai, M.; Nakabayashi, N. Direct tensile strength and characteristics of dentin restored with all-ceramic, resin-composite and cast metal prostheses cemented with resin adhesives. BioMed Res. Int. 2015, 2015, 656948. [Google Scholar] [CrossRef] [PubMed]
- Piemjai, M. Advanced Fixed Prosthodontics: Dentin Protection for Life-long Function; Samcharoen Panich: Bangkok, Thailand, 2015; pp. 160–197. [Google Scholar]
- Masaka, N.; Yoneda, S.; Masaka, K. An up to 43-year longitudinal study of fixed prosthetic restorations retained with 4-META/MMA-TBB resin cement or zinc phosphate cement. J. Prosthet. Dent. 2021. Online ahead of print. [Google Scholar] [CrossRef] [PubMed]




| Systems | Primerless-Wet | Dry | Self-Etched | Moist with Primer | |||
|---|---|---|---|---|---|---|---|
| Groups | 1-1-10s | 1-1-30s | 1-1-60s | Super-Bond C&B | AQ-Bond | All-Bond2 | Single-Bond2 |
| Acid conditioner | 1-1 | 1-1 | 1-1 | 10-3 | - | 32% phosphoric acid | 35% phosphoric acid |
| Conditioning time | 10 s | 30 s | 60 s | 10 s | - | 15 s | 15 s |
| Rinse off | 10 s | 10 s | 10 s | 10 s | - | 15 s | 10 s |
| Surface treatment | Blot-dried 10 s | Air-dried 10 s | - | Air-dried 1 s, kept moist | Blot-dried and kept moist | ||
| Manipulations of luting adhesives | Mixed 4 drops of 4-META/MMA and 1 drop of TBB in a cool porcelain container applied using brush-dip technique with PMMA powder for auto-curing on the conditioned tooth-surface and resin-composite inlay or PMMA block prior fixation | Same as primerless-wet groups | Scrubbed sponge impregnated with monomers on tooth surface for 20 s, air-dried for 5 s, light-cured for 10 s. Applied metafil FLO on resin-composite inlay or PMMA block prior to fixation, light-cured for 60 s. | Mixed 1 drop of primer A: B, coated on conditioned tooth-surface 5 times, gently air-dried for 5 s, applied D&E resin, light-cured for 20 s. Mixed Duolink cement and applied on resin-composite inlay or PMMA block prior to fixation, light-cured for 60 s. | Applied Single-Bond 2 on conditioned tooth surface for 15 s, gently air-dried for 5 s, light cured for 10 s. Mixed RelyX ARC cement and applied on resin-composite inlay or PMMA block before fixation, light-cured 60 s. | ||
| Materials | Chemical Composition |
|---|---|
| Primerless-wet | Etchant: 1% citric acid and 1% ferric chloride (1-1); water Monomers: 4-methacryloyloxyethyl trimellitate anhydride in methyl methacrylate initiated by tri-n-butyl borane (4-META/MMA-TBB) Powder: poly(methyl methacrylate) (PMMA) |
| Super-Bond C&B | Etchant: 10% citric acid and 3% ferric chloride (10-3); water Monomers: 4-META/MMA-TBB Powder: PMMA |
| AQ-Bond Plus Metafil FLO | Monomers: methyl methacrylate (MMA); 4-META; urethane dimethacrylate (UDMA); 2-hydroxyethyl methacrylate (HEMA); acetone; water Sponge: polyurethane foam; amine-p-toluenesulfonic acid sodium salt (p-TSNa) Luting: UDMA; triethylene glycol dimethacrylate (TEGDMA); trimethylolpropane trimethacrylate (TMPT); barium glass |
| All-Bond2 Duolink | Etchant: 32% phosphoric acid; water Primer: 2% NTG-GMA (N-tolylglycine-glycidyl methacrylate); 16% BPDM (biphenyl dimethacrylate); acetone Bonding: bisphenol A-glycidyl methacrylate (bis-GMA); UDMA, HEMA Luting: bis-GMA; TEGDMA; UDMA; glass filler |
| Single-Bond2 RelyX ARC | Etchant: 35% phosphoric acid; water Bonding: bis-GMA; HEMA; dimethacrylates, ethanol, water; methacrylate functional copolymer of polyacrylic and polyitaconic acids Luting: bis-GMA; TEGDMA; zirconia/silica filler |
| Metafil CX | Inlay: UDMA; TEGDMA; TMPT; colloidal silica |
 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piemjai, M.; Waleepitackdej, O.; Garcia-Godoy, F. Marginal Micro-Seal and Tensile Bond Strength of a Biopolymer Hybrid Layer Coupled with Dental Prosthesis Using a Primerless-Wet System. Polymers 2023, 15, 283. https://doi.org/10.3390/polym15020283
Piemjai M, Waleepitackdej O, Garcia-Godoy F. Marginal Micro-Seal and Tensile Bond Strength of a Biopolymer Hybrid Layer Coupled with Dental Prosthesis Using a Primerless-Wet System. Polymers. 2023; 15(2):283. https://doi.org/10.3390/polym15020283
Chicago/Turabian StylePiemjai, Morakot, Onusa Waleepitackdej, and Franklin Garcia-Godoy. 2023. "Marginal Micro-Seal and Tensile Bond Strength of a Biopolymer Hybrid Layer Coupled with Dental Prosthesis Using a Primerless-Wet System" Polymers 15, no. 2: 283. https://doi.org/10.3390/polym15020283
APA StylePiemjai, M., Waleepitackdej, O., & Garcia-Godoy, F. (2023). Marginal Micro-Seal and Tensile Bond Strength of a Biopolymer Hybrid Layer Coupled with Dental Prosthesis Using a Primerless-Wet System. Polymers, 15(2), 283. https://doi.org/10.3390/polym15020283







