Particulate Filler and Discontinuous Fiber Filler Resin Composite’s Adaptation and Bonding to Intra-Radicular Dentin
Abstract
:1. Introduction
2. Materials and Methods
2.1. Specimen Preparation
- G2 Bond Universal (GC Corporation, Tokyo, Japan) + EverX Flow (GC Co.)
- G-Premio Bond (GC Co.) + EverX Flow (GC Co.)
- G2 Bond Universal (GC Co.) + EverX Flow (GC Co.) with ultrasonic activation (UA).
- G-Premio Bond (GC Co.) + EverX Flow (GC Corporation) with ultrasonic activation (UA).
- G-Premio Bond (GC Co.) + a dual-cured composite resin cement (GradiaCore, GC Co.) + GC Fiber Post 1.6 mm (GC Co.), silanized with G-Multi Primer for 1 min (GC Co.)
- G-Premio Bond (GC Co.) + a dual-cured composite resin cement (GradiaCore, GC Co.) + GC Fiber Post 1.6 mm (GC Co.), silanized with G-Multi Primer for 1 min (GC Co.) with ultrasonic activation (UA).
- G2 Bond Universal + prefabricated FRC post (GC Co.) with ultrasonic activation (UA).
- -
- In groups 1, 3, and 7, a two-bottle universal adhesive (primer + bonding) G2 Bond Universal (GC Co.) was used according to the manufacturer’s instructions. The primer solution was applied in the canal with a microbrush (GC Co.). Excess adhesive was removed from the post space with gentle air blowing and absorbent paper points. After the bonding application, excess adhesive was removed by suction drying and light-cured for 20 s using a LED light (VALO Cordless-LED Curing Light—Ultradent, Milano, Italy).
- -
- In the other groups (2, 4, 5, 6), a one-bottle G-Premio Bond (GC Co.) universal adhesive was applied in a single step, the excess was removed with a gentle air blowing and the adhesive was cured.
2.2. Push-Out Loading Test
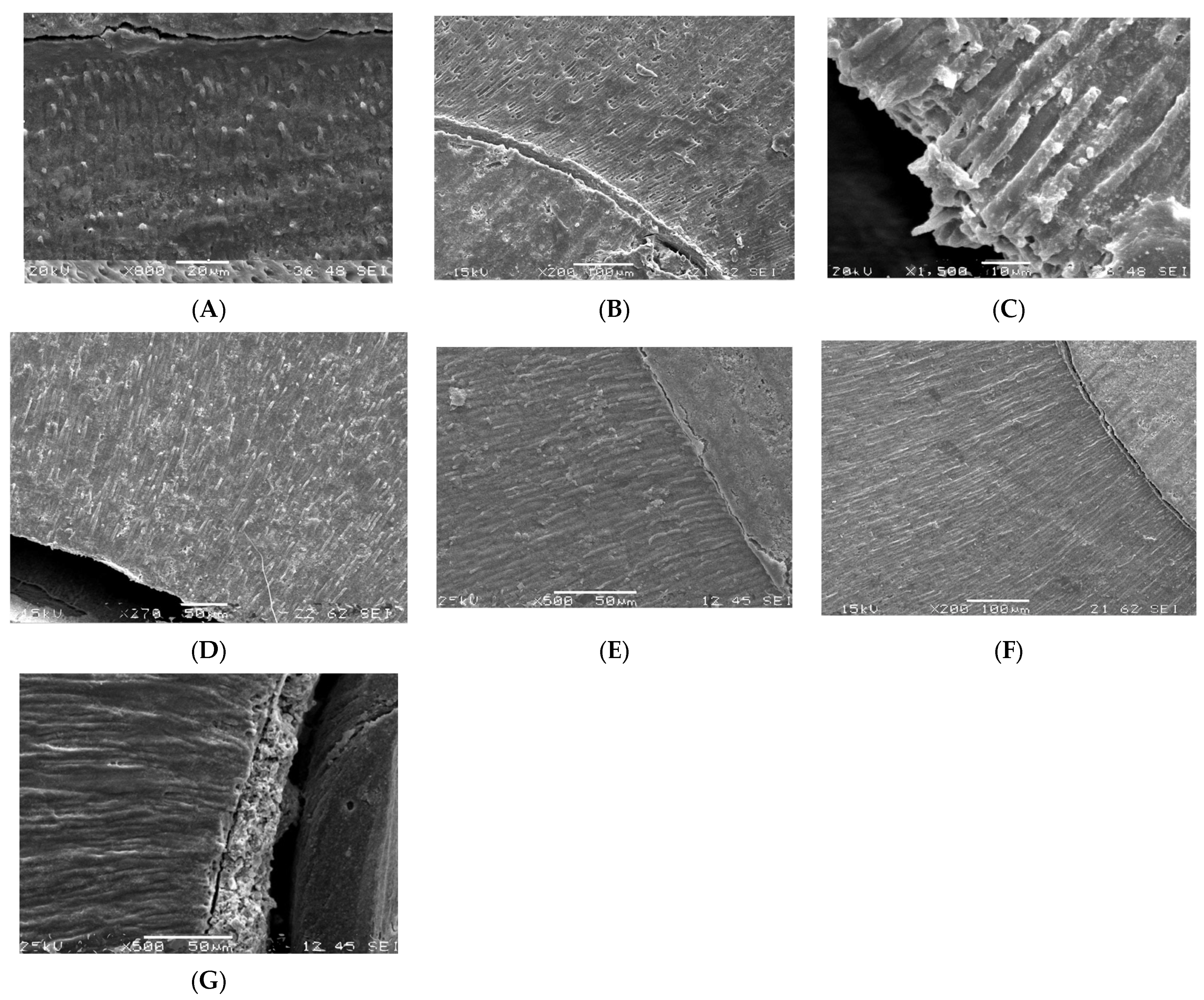
2.3. Microscopic Analysis
2.4. Statistical analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gillen, B.M.; Looney, S.W.; Gu, L.S.; Loushine, B.A.; Weller, R.N.; Loushine, R.J.; Pashley, D.H.; Tay, F.R. Impact of the quality of coronal restoration versus the quality of root canal fillings on the success of root canal treatment: A systematic review and meta-analysis. J. Endod. 2011, 37, 895–902. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barcellos, R.R.; Correia, D.P.; Farina, A.P.; Mesquita, M.F.; Ferraz, C.C.; Cecchin, D. Fracture resistance of endodontically treated teeth restored with intra-radicular post: The effects of post system and dentine thickness. J. Biomech. 2013, 46, 2572–2577. [Google Scholar] [CrossRef] [PubMed]
- Helfer, A.R.; Melnick, S.; Schilder, H. Determination of the moisture content of vital and pulpless teeth. Oral Surg. Oral Med. Oral Pathol. 1972, 34, 661–670. [Google Scholar] [CrossRef] [PubMed]
- Rivera, E.M.; Yamauchi, M. Site comparisons of dentine collagen cross-links from extracted human teeth. Arch. Oral Biol. 1993, 38, 541–546. [Google Scholar] [CrossRef]
- Al-Omiri, M.K.; Mahmoud, A.A.; Rayyan, M.R.; Abu-Hammad, O. Fracture resistance of teeth restored with post-retained res- torations: An overview. J. Endod. 2010, 36, 1439–1449. [Google Scholar] [CrossRef] [PubMed]
- Taha, N.A.; Palamara, J.E.; Messer, H.H. Fracture strength and fracture patterns of root filled teeth restored with direct resin resto-rations. J. Dent. 2011, 39, 527–535. [Google Scholar] [CrossRef]
- Wu, Y.; Cathro, P.; Marino, V. Fracture resistance and pattern of the upper premolars with obturated canals and restored endodontic occlusal access cavities. J. Biomed. Res. 2010, 24, 474–478. [Google Scholar] [CrossRef] [Green Version]
- Oskoee, P.A.; Ajami, A.A.; Navimipour, E.J.; Oskoee, S.S.; Sadjadi, J. The effect of three composite fiber insertion techniques on fracture resistance of root-filled teeth. J. Endod. 2009, 35, 413–416. [Google Scholar] [CrossRef]
- Dietschi, D.; Duc, O.; Krejci, I.; Sadan, A. Biomechanical considerations for the restoration of endodontically treated teeth: A systematic review of the literature—Part 1. Composition and micro- and macro- structure alterations. Quintessence Int. 2007, 38, 733–743. [Google Scholar]
- Ferrari, M.; Sorrentino, R.; Juloski, J.; Grandini, S.; Carrabba, M.; Discepoli, N.; Ferrari Cagidiaco, E. Post-Retained Single Crowns versus Fixed Dental Prostheses: A 7-Year Prospective Clinical Study. J. Dent. Res. 2017, 96, 250–262. [Google Scholar] [CrossRef]
- Goracci, C.; Grandini, S.; Bossù, M.; Bertelli, E.; Ferrari, M. Laboratory assessment of the retentive potential of adhesive posts: A review. J. Dent. 2007, 35, 827–835. [Google Scholar] [CrossRef] [PubMed]
- Zavattini, A.; Feitosa, V.P.; Mannocci, F.; Foschi, F.; Babbar, A.; Luzi, A.; Ottria, L.; Mangani, F.; Casula, I.; Sauro, S. Bonding ability of experimental resin-based materials containing (ion-releasing)-microfillers applied on water-wet or ethanol-wet root canal dentine. Int. J. Adhes. 2014, 54, 214–223. [Google Scholar] [CrossRef]
- Ferrari, M.; Cagidiaco, M.C.; Goracci, C.; Vichi, A.; Mason, P.N.; Radovic, I. Long-term retrospective study of the clinical performance of fibre posts. Am. J. Dent. 2002, 20, 287–291. [Google Scholar]
- Seow, L.L.; Toh, C.G.; Wilson, N.H. Strain measurements and fracture resistance of endodontically treated premolars restored with all-ceramic restorations. J. Dent. 2015, 43, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Nothdurft, F.P.; Seidel, E.; Gebhart, F.; Naumann, M.; Motter, P.J.; Pospiech, P.R. The fracture behavior of premolar teeth with class II cavities restored by both direct composite restorations and endodontic post systems. J. Dent. 2008, 36, 444–449. [Google Scholar] [CrossRef] [PubMed]
- Barfeie, A.; Thomas, M.B.W.; Watts, A.; Rees, J. Failure mechanisms of fibre posts: A literature review. Eur. J. Prosthod. Rest. Dent. 2015, 23, 115–127. [Google Scholar]
- Sorrentino, R.; Di Mauro, M.I.; Ferrari, M.; Leone, R.; Zarone, F. Complications of endodontically treated teeth restored with fiber posts and single crowns or fixed dental prostheses—A systematic review. Clin. Oral Investig. 2016, 20, 1449–1457. [Google Scholar] [CrossRef] [Green Version]
- Garoushi, S.; Vallittu, P.K.; Lassila, L.V. Short glass fiber reinforced restorative composite resin with semi-interpenetrating polymer network matrix. Dent. Mater. 2007, 23, 1356–1362. [Google Scholar] [CrossRef]
- Giovannetti, A.; Goracci, C.; Vichi, A.; Chieffi, N.; Polimeni, A.; Ferrari, M. Post retentive ability of a new resin composite with low stress behaviour. J. Dent. 2012, 40, 322–328. [Google Scholar] [CrossRef]
- Juloski, J.; Goracci, C.; Radovic, I.; Chieffi, N.; Vichi, A.; Vulicevic, Z.R.; Ferrari, M. Post-retentive ability of new flowable resin composites. Am. J. Dent. 2013, 26, 324–328. [Google Scholar]
- Garoushi, S.; Vallittu, P.K.; Lippo, V.J. Lassila. Direct restoration of severely damaged incisors using short fiber-reinforced composite resin. J. Dent. 2007, 35, 731–736. [Google Scholar] [CrossRef]
- Forster, A.; Sáry, T.; Braunitzer, G.; Fráter, M. In vitro fracture resistance of endodontically treated premolar teeth restored with a direct layered fiber-reinforced composite post and core. J. Adhes. Sci. Technol. 2016, 31, 1454–1466. [Google Scholar] [CrossRef] [Green Version]
- Ktastl, G.; Izquierdo, A.; Büttel, L.; Zitzmann, N.U.; Schmitter, M.; Weiger, R. Does an intracanal composite anchorage replace posts? Clin. Oral Investig. 2014, 18, 147–153. [Google Scholar] [CrossRef] [Green Version]
- Gürel, M.A.; Helvacioğlu Kivanç, B.; Ekici, A.; Alaçam, T. Fracture resistance of premolars restored either with short fiber or polyethylene woven fiber-reinforced composite. J. Esthet. Restor. Dent. 2016, 28, 412–418. [Google Scholar] [CrossRef]
- Amarnath, G.S.; Swetha, M.U.; Muddugangadhar, B.C.; Sonika, R.; Garg, A.; Rao, T.R.P. Effect of Post Material and Length on Fracture Resistance of Endodontically Treated Premolars: An In-Vitro Study. J. Int. Oral Health 2015, 7, 22–28. [Google Scholar]
- Bosso, K.; Gonini Júnior, A.; Guiraldo, R.D.; Berger, S.B.; Lopes, M.B. Stress Generated by Customized Glass Fiber Posts and Other Types by Photoelastic Analysis. Braz. Dent. J. 2015, 26, 222–227. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Shu, X.; Zhang, Y.; Yang, B.; Jian, Y.; Zhao, K. Evaluation of Fiber Posts vs Metal Posts for Restoring Severely Damaged Endodontically Treated Teeth: A Systematic Review and Meta-Analysis. Quintessence Int. 2019, 50, 8–20. [Google Scholar]
- Gomes, G.M.; Gomes, O.M.; Reis, A.; Gomes, J.C.; Loguercio, A.D.; Calixto, A.L. Effect of operator experience on the outcome of fiber post cementation with different resin cements. Oper. Dent. 2013, 38, 555–564. [Google Scholar] [CrossRef] [Green Version]
- Naumann, M.; Preuss, A.; Rosentritt, M. Effect of Incomplete Crown Ferrules on Load Capacity of Endodontically Treated Maxillary Incisors Restored with Fiber Posts, Composite Build-Ups, and All-Ceramic Crowns: An in Vitro Evaluation after Chewing Simulation. Acta Odontol. Scand. 2006, 64, 31–36. [Google Scholar] [CrossRef]
- Ferrari, M.; Ferrari Cagidiaco, E.; Goracci, C.; Sorrentino, R.; Zarone, F.; Grandini, S.; Joda, T.A. Posterior partial crowns of lithium disilicate (LS2) with or without posts: A randomized controlled prospective clinical trial with a 3-year follow up. J. Dent. 2019, 83, 12–17. [Google Scholar] [CrossRef]
- Juloski, J.; Fadda, G.M.; Monticelli, F.; Fajó-Pascual, M.; Goracci, C.; Ferrari, M. Four-year Survival of Endodontically Treated Premolars Restored with Fiber Posts. J. Dent. Res. 2014, 93, 52S–58S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vallittu, P.K. Are we misusing fiber posts? Guest editorial. Dent. Mater. 2016, 32, 125–126. [Google Scholar] [CrossRef] [PubMed]
- Rengo, C.; Spagnuolo, G.; Ametrano, G.; Juloski, J.; Rengo, S.; Ferrari, M. Micro-computerized tomographic analysis of premolars restored with oval and circular posts. Clin. Oral Investig. 2014, 18, 571–578. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bitter, K.; Priehn, K.; Martus, P.; Kielbassa, A.M. In Vitro Evaluation of Push-out Bond Strengths of Various Luting Agents to Tooth-Colored Posts. J. Prosthet. Dent. 2006, 95, 302–310. [Google Scholar] [CrossRef]
- Braga, N.M.A.; Paulino, S.M.; Alfredo, E.; Sousa-Neto, M.D.; Vansan, L.P. Removal Resistance of Glass-Fiber and Metallic Cast Posts with Different Lengths. J. Oral Sci. 2006, 48, 15–20. [Google Scholar] [CrossRef] [Green Version]
- Shah, S.; Shilpa-Jain, D.P.; Velmurugan, N.; Sooriaprakas, C.; Krithikadatta, J. Performance of fibre reinforced composite as a post-endodontic restoration on different endodontic cavity designs- an in-vitro study. J. Mech. Behav. Biomed. Mater. 2020, 104, 1036–1050. [Google Scholar] [CrossRef]
- Fráter, M.; Sáry, T.; Jókai, B.; Braunitzer, G.; Säilynoja, E.; Pekka, K.; Vallittu, P.K.; Lassila, L.; Garoushi, S. Fatigue behavior of endodontically treated premolars restored with different fiber-reinforced designs. Dent. Mater. 2021, 37, 391–402. [Google Scholar] [CrossRef]
- Fráter, M.; Lassila, L.; Braunitzer, G.; Pekka, K.; Vallittu, P.K.; Garoushi, S. Fracture resistance and marginal gap formation of post-core restorations: Influence of different fiber-reinforced composites. Clin. Oral Investig. 2020, 24, 265–276. [Google Scholar] [CrossRef] [Green Version]
- Uctasli, S.; Boz, Y.; Sungur, S.; Vallittu, P.K.; Garoushi, S.; Lassila, L. Influence of Post-Core and Crown Type on the Fracture Resistance of Incisors Submitted to Quasistatic Loading. Polymers 2021, 13, 1130. [Google Scholar] [CrossRef]
- Lassila, L.; Haapsaari, A.; Vallittu, P.K.; Garoushi, S. Fracture Resistance of Anterior Crowns Reinforced by Short-Fiber Composite. Polymers 2022, 14, 1809. [Google Scholar] [CrossRef]
- Sharma, A.; Amittharaj, L.V.; Sanjeev, K.; Mahalaxmi, S. Fracture Resistance of Endodontically Treated Premolars Restored with Flowable Short Fibre-Reinforced Resin Composite–An In Vitro Study. Eur. Endod. J. 2022, 7, 161–166. [Google Scholar]
- Bijelic-Donova, J.; Garoushi, S.; Lassila, L.V.; Keulemans, F.; Vallittu, P.K. Mechanical and structural characterization of discontinuous fiber-reinforced dental resin composite. J. Dent. 2016, 52, 70–78. [Google Scholar] [CrossRef]
- Paul, S.J.; Leach, M.; Rueggeberg, F.A.; Pashley, D.H. Effect of water content on the physical properties of model dentine primer and bonding resins. J. Dent. 1999, 27, 209–214. [Google Scholar] [CrossRef]
- Choi, A.-N.; Lee, J.-H.; Son, S.; Jung, K.-H.; Kwon, Y.H.; Park, J.-K. Effect of dentin wetness on the bond strength of universal adhesives. Materials 2017, 10, 1224–1229. [Google Scholar] [CrossRef] [Green Version]
- Alex, G. Universal adhesives: The next evolution in adhesive dentistry. Compend. Contin. Educ. Dent. 2015, 36, 15–26. [Google Scholar]
- Yiu, C.K.Y.; Pashley, E.L.; Hiraishi, N.; King, N.M.; Goracci, C.; Ferrari, M.; Carvalho, R.M.; Pashley, D.H.; Tay, F.R. Solvent and water retention in dental adhesive blends after evaporation. Biomaterials 2005, 26, 6863–6872. [Google Scholar] [CrossRef] [Green Version]
- British Dental Journal. The new standard in adhesive dentistry. Br. Dent. J. 2021, 230, 263. [Google Scholar] [CrossRef]
- GC America Inc. Safety Data Sheet for G2-BOND Universal (2-BOND). Available online: https://www.gcamerica.com/products/operatory/G2-BOND/downloads/G2-BONDUniversal(2BOND)1303USRev1SDS24Jan2021.pdf (accessed on 11 March 2021).
- GC America Inc. Brochure. Available online: https://www.gcamerica.com/products/operatory/G2-BOND/GCA_G2-BOND_Universal_Brochure-02-09-2021_Ver1-digital.pdf (accessed on 11 March 2021).
- Gu, X.H.; Mao, C.Y.; Kern, M. Effect of different irrigation on smear layer removal after post space preparation. J. Endod. 2009, 35, 583–586. [Google Scholar] [CrossRef]
- Koskinen, K.P.; Meurman, J.H.; Stenval, H. Appearance of chemically treated root canal walls in the scanning electron microscope. Scand. J. Dent. Res. 1980, 88, 397–405. [Google Scholar]
- Sen, B.H.; Wesselink, P.R.; Türkün, M. The smear layer: A phenomenon in root canal therapy. Int. Endod. J. 1995, 28, 141–148. [Google Scholar] [CrossRef]
- Martin, H.; Cunningham, M.J.; Morris, J.P.; Cotton, W.R. Ultrasonic versus hand filing of dentine: A quantitative study. Oral Surg. Oral Med. Oral Pat. 1980, 49, 79–81. [Google Scholar] [CrossRef] [PubMed]
- Cameron, J.A. Factors affecting the clinical efficiency of ultrasonic endodontics: A scanning electron microscopy study. Int. Endod. J. 1995, 28, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Küçükekenci, F.F.; Küçükekenci, A.S. Effect of ultrasonic and Nd: Yag laser activation on irrigants on the push-out bond strength of fiber post to the root canal. J. Appl. Oral Sci. 2019, 27, e20180420. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Material | Composition |
|---|---|
| G-Premio Bond (GC Co., Tokyo, Japan) | 10-MDP, 4-META, 10-MDTP, methacrylate acid ester, distilled water, acetone, photoinitiators, fine powdered silica |
| G2 Bond Universal (GC. Co.) | Primer: 4-META, MDP, dimethacrylate, photoinitiator, water, acetone, silica, MDTP Bond: Dimethacrylate, photoinitiator, silica |
| EverX Flow (SFRC) (GC. Co.) | Bis-EMA, TEGDMA, UDMA, micrometer scale glass fiber filler 100–300 μm and Ø7 μm, Barium glass 70 wt%, 46 vol% |
| Gradia Core (GC. Co.) | Methacrylic acid ester 20–30 wt%, fluoro-alumino-silicate glass 70–75 wt%, silicon dioxide 1–5 wt%. |
| GC Fiber Post (GC. Co.) | Glass fibers, dimethacrylate matrix |
| G Multi Primer (GC. Co.) | MPTMS, 10-MDP, MDTP, BisGMA, TEGDMA, Ethanol |
| Group | N | Median | Interquartile Range |
|---|---|---|---|
| 1 | 44 | 7.35 | 5.35–11.11 |
| 2 | 38 | 6.66 | 5.87–8.75 |
| 3 | 36 | 8.37 | 6.46–10.55 |
| 4 | 43 | 7.72 | 5.34–10.71 |
| 5 | 33 | 7.14 | 4.65–10.31 |
| 6 | 42 | 6.78 | 4.49–13.59 |
| 7 | 39 | 7.99 | 4.62–8.92 |
| Group | N | A | C | M |
|---|---|---|---|---|
| 1 | 44 | 20 | / | 24 |
| 2 | 38 | 23 | / | 15 |
| 3 | 36 | 10 | 7 | 19 |
| 4 | 43 | 18 | 2 | 23 |
| 5 | 33 | 14 | / | 19 |
| 6 | 42 | 12 | 1 | 29 |
| 7 | 39 | 22 | 4 | 13 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferrari, M.; Lettieri, E.; Pontoriero, D.I.K.; Vallittu, P.; Ferrari Cagidiaco, E. Particulate Filler and Discontinuous Fiber Filler Resin Composite’s Adaptation and Bonding to Intra-Radicular Dentin. Polymers 2023, 15, 3180. https://doi.org/10.3390/polym15153180
Ferrari M, Lettieri E, Pontoriero DIK, Vallittu P, Ferrari Cagidiaco E. Particulate Filler and Discontinuous Fiber Filler Resin Composite’s Adaptation and Bonding to Intra-Radicular Dentin. Polymers. 2023; 15(15):3180. https://doi.org/10.3390/polym15153180
Chicago/Turabian StyleFerrari, Marco, Eugenia Lettieri, Denise Irene Karin Pontoriero, Pekka Vallittu, and Edoardo Ferrari Cagidiaco. 2023. "Particulate Filler and Discontinuous Fiber Filler Resin Composite’s Adaptation and Bonding to Intra-Radicular Dentin" Polymers 15, no. 15: 3180. https://doi.org/10.3390/polym15153180
APA StyleFerrari, M., Lettieri, E., Pontoriero, D. I. K., Vallittu, P., & Ferrari Cagidiaco, E. (2023). Particulate Filler and Discontinuous Fiber Filler Resin Composite’s Adaptation and Bonding to Intra-Radicular Dentin. Polymers, 15(15), 3180. https://doi.org/10.3390/polym15153180







