Insufficient Evidence to Ascertain the Long-Term Survival of PEEK Dental Prostheses: A Systematic Review of Clinical Studies
Abstract
:1. Introduction
2. Materials and Methods
2.1. Focused Question and Protocol Registration
2.2. Eligibility Criteria
2.3. Literature Search
2.4. Data Extraction
2.5. Quality Assessment of Included Studies
3. Results
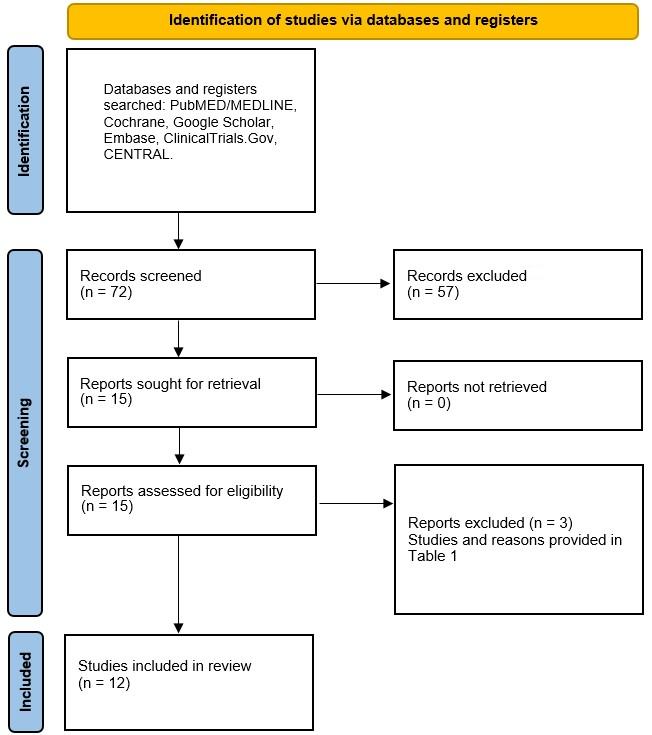
3.1. Results of the Literature Search
3.2. General Characteristics of Included Studies
3.3. Outcomes of the Included Studies
3.4. Results of the Quality Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chochlidakis, K.; Einarsdottir, E.; Tsigarida, A.; Papaspyridakos, P.; Romeo, D.; Barmak, A.B.; Ercoli, C. Survival rates and prosthetic complications of implant fixed complete dental prostheses: An up to 5-year retrospective study. J. Prosthet. Dent. 2020, 124, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, J. Bond strength of denture teeth to acrylic bases. J. Dent. 1993, 21, 274–280. [Google Scholar] [CrossRef]
- Meng, T.R.; Latta, M.A. Physical properties of four acrylic denture base resins. J. Contemp. Dent. Pract. 2005, 6, 93–100. [Google Scholar] [CrossRef] [Green Version]
- Shimizu, H.; Tsue, F.; Obukuro, M.; Kido, H.; Takahashi, Y.; Ohmura, H. Fracture strength of metal-based complete maxillary dentures with a newly designed metal framework. Int. Chin. J. Dent. 2005, 5, 35–38. [Google Scholar]
- Kreeft, A.; Krap, M.; Wismeijer, D.; Speksnijder, C.; Smeele, L.; Bosch, S.; Muijen, M.; Balm, A. Oral function after maxillectomy and reconstruction with an obturator. Int. J. Oral Maxillofac. Surg. 2012, 41, 1387–1392. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.M.; Cheng, L.Y.; Chow, T.; Clark, R.K. Effect of processing method on the dimensional accuracy and water sorption of acrylic resin dentures. J. Prosthet. Dent. 1999, 81, 300–304. [Google Scholar] [CrossRef]
- Al Jabbari, Y.S.; Zinelis, S.; Al Taweel, S.M.; Nagy, W.W. The effect of artificial aging on the bond strength of heat-activated acrylic resin to surface-treated nickel-chromium-beryllium Alloy. Open Dent. J. 2016, 10, 124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schweitzer, D.M.; Goldstein, G.R.; Ricci, J.L.; Silva, N.; Hittelman, E.L. Comparison of bond strength of a pressed ceramic fused to metal versus feldspathic porcelain fused to metal. J. Prosthodont. Implant Esthet. Reconstr. Dent. 2005, 14, 239–247. [Google Scholar] [CrossRef]
- Jorge, J.H.; Giampaolo, E.T.; Machado, A.L.; Vergani, C.E. Cytotoxicity of denture base acrylic resins: A literature review. J. Prosthet. Dent. 2003, 90, 190–193. [Google Scholar] [CrossRef]
- Spiechowicz, E.; Glantz, P.O.; Axell, T.; Grochowski, P. A long-term follow-up of allergy to nickel among fixed prostheses wearers. Eur. J. Prosthodont. Restor. Dent. 1999, 7, 41–44. [Google Scholar]
- De Backer, H.; Van Maele, G.; De Moor, N.; Van den Berghe, L. Long-term results of short-span versus long-span fixed dental prostheses: An up to 20-year retrospective study. Int. J. Prosthodont. 2008, 21, 75–85. [Google Scholar] [PubMed]
- Wang, F.; Roovers, J. Functionalization of poly(aryl ether ether ketone) (PEEK): Synthesis and properties of aldehyde and carboxylic acid substituted PEEK. Macromolecules 1993, 26, 5295–5302. [Google Scholar] [CrossRef]
- Toth, J.M.; Wang, M.; Estes, B.; Scifert, J.L.; Seim, H.B.; Turner, A.S. Polyetheretherketone as a biomaterial for spinal applications. Biomaterials 2006, 27, 324–334. [Google Scholar] [CrossRef] [Green Version]
- Najeeb, S.; Zafar, M.S.; Khurshid, Z.; Siddiqui, F. Applications of polyetheretherketone (PEEK) in oral implantology and prosthodontics. J. Prosthodont. Res. 2016, 60, 12–19. [Google Scholar] [CrossRef] [PubMed]
- SanSandler, J.; Werner, P.; Shaffer, M.S.; Demchuk, V.; Altstädt, V.; Windle, A.H. Carbon-nanofibre-reinforced poly(ether ether ketone) composites. Compos. Part A Appl. Sci. Manuf. 2002, 33, 1033–1039. [Google Scholar] [CrossRef]
- Sarot, J.R.; Contar, C.M.M.; de Cruz, A.C.C.; Magini, R.d.S. Evaluation of the stress distribution in CFR-PEEK dental implants by the three-dimensional finite element method. J. Mater. Sci. Mater. Med. 2010, 21, 2079–2085. [Google Scholar] [CrossRef] [PubMed]
- Najeeb, S.; Khurshid, Z.; Matinlinna, J.P.; Siddiqui, F.; Nassani, M.Z.; Baroudi, K. Nanomodified Peek Dental Implants: Bioactive Composites and Surface Modification—A Review. Int. J. Dent. 2015, 2015, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Muhsin, S.A.; Hatton, P.V.; Johnson, A.; Sereno, N.; Wood, D.J. Determination of Polyetheretherketone (PEEK) mechanical properties as a denture material. Saudi Dent. J. 2019, 31, 382–391. [Google Scholar] [CrossRef]
- Villefort, R.F.; Tribst, J.P.M.; Piva, A.M.D.O.D.; Borges, A.L.; Binda, N.C.; Ferreira, C.E.D.A.; Bottino, M.A.; Von Zeidler, S.L.V. Stress distribution on different bar materials in implant-retained palatal obturator. PLoS ONE 2020, 15, e0241589. [Google Scholar] [CrossRef]
- Harb, I.E.; Abdel-Khalek, E.A.; Hegazy, S.A. CAD/CAM Constructed Poly(etheretherketone) (PEEK) Framework of Kennedy Class I Removable Partial Denture: A Clinical Report. J. Prosthodont. 2019, 28, e595–e598. [Google Scholar] [CrossRef]
- Arnold, C.; Hey, J.; Schweyen, R.; Setz, J.M. Accuracy of CAD-CAM-fabricated removable partial dentures. J. Prosthet. Dent. 2018, 119, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Golbang, A.; Mokhtari, M.; Harkin-Jones, E.; Archer, E.; McIlhagger, A. Additive manufacturing and injection moulding of high-performance IF-WS 2/PEEK nanocomposites: A comparative study. Front. Mater. 2021, 8, 745088. [Google Scholar] [CrossRef]
- Papathanasiou, I.; Kamposiora, P.; Papavasiliou, G.; Ferrari, M. The use of PEEK in digital prosthodontics: A narrative review. BMC Oral Health 2020, 20, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wu, P.; Liu, H.-L.; Zhang, L.; Liu, L.-P.; Ma, C.-F.; Chen, J.-H. Polyetheretherketone versus titanium CAD-CAM framework for implant-supported fixed complete dentures: A retrospective study with up to 5-year follow-up. J. Prosthodont. Res. 2021, 66, 279–287. [Google Scholar] [CrossRef]
- Pereira, A.L.C.; de Medeiros, A.K.B.; de Sousa Santos, K.; de Almeida, É.O.; Barbosa, G.A.S.; Carreiro, A.d.F.P. Accuracy of CAD-CAM systems for removable partial denture framework fabrication: A systematic review. J. Prosthet. Dent. 2021, 125, 241–248. [Google Scholar] [CrossRef]
- Moher, D.; Altman, D.G.; Liberati, A.; Tetzlaff, J. PRISMA statement. Epidemiology 2011, 22, 128. [Google Scholar] [CrossRef] [Green Version]
- Ye, H.; Wang, Z.; Sun, Y.; Zhou, Y. Fully digital workflow for the design and manufacture of prostheses for maxillectomy defects. J. Prosthet. Dent. 2021, 126, 257–261. [Google Scholar] [CrossRef]
- Yue, Q.; Yilmaz, B.; Abou-Ayash, S.; Zimmermann, P.; Brägger, U.; Schimmel, M. Use of an attachment system with angulated abutments and polyetheretherketone inserts to retain a maxillary overdenture: A clinical report. J. Prosthet. Dent. 2020, 124, 129–134. [Google Scholar] [CrossRef] [Green Version]
- Ichikawa, T.; Kurahashi, K.; Liu, L.; Matsuda, T.; Ishida, Y. Use of a Polyetheretherketone Clasp Retainer for Removable Partial Denture: A Case Report. Dent. J. 2019, 7, 4. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Schulz, K.F.; Altman, D.G.; Consort, G. The CONSORT Statement: Revised Recommendations for Improving the Quality of Reports of Parallel-Group Randomized Trials; Elsevier: Amsterdam, The Netherlands, 2001. [Google Scholar]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Bull. World Health Organ. 2007, 85, 867–872. [Google Scholar] [CrossRef]
- Riley, D.S.; Barber, M.S.; Kienle, G.S.; Aronson, J.K.; von Schoen-Angerer, T.; Tugwell, P.; Kiene, H.; Helfand, M.; Altman, D.G.; Sox, H.; et al. CARE 2013 explanations and elaborations: Reporting guidelines for case reports. J. Clin. Epidemiol. 2017, 89, 218–235. [Google Scholar] [CrossRef] [PubMed]
- Costa-Palau, S.; Torrents-Nicolas, J.; Barberà, M.B.-D.; Cabratosa-Termes, J. Use of polyetheretherketone in the fabrication of a maxillary obturator prosthesis: A clinical report. J. Prosthet. Dent. 2014, 112, 680–682. [Google Scholar] [CrossRef] [PubMed]
- Zoidis, P.; Papathanasiou, I. Modified PEEK resin-bonded fixed dental prosthesis as an interim restoration after implant placement. J. Prosthet. Dent. 2016, 116, 637–641. [Google Scholar] [CrossRef]
- Hahnel, S.; Scherl, C.; Rosentritt, M. Interim rehabilitation of occlusal vertical dimension using a double-crown-retained removable dental prosthesis with polyetheretherketone framework. J. Prosthet. Dent. 2018, 119, 315–318. [Google Scholar] [CrossRef] [PubMed]
- Zoidis, P. The all-on-4 modified polyetheretherketone treatment approach: A clinical report. J. Prosthet. Dent. 2018, 119, 516–521. [Google Scholar] [CrossRef]
- Sinha, N.; Gupta, N.; Reddy, K.M.; Shastry, Y.M. Versatility of PEEK as a fixed partial denture framework. J. Indian Prosthodont. Soc. 2017, 17, 80. [Google Scholar]
- Zoidis, P. Polyetheretherketone Overlay Prosthesis over High Noble Ball Attachments to Overcome Base Metal Sensitivity: A Clinical Report. J. Prosthodont. 2018, 27, 688–693. [Google Scholar] [CrossRef] [Green Version]
- Mangano, F.; Mangano, C.; Margiani, B.; Admakin, O. Combining Intraoral and Face Scans for the Design and Fabrication of Computer-Assisted Design/Computer-Assisted Manufacturing (CAD/CAM) Polyether-Ether-Ketone (PEEK) Implant-Supported Bars for Maxillary Overdentures. Scanning 2019, 2019, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Tasopoulos, T.; Chatziemmanouil, D.; Kouveliotis, G.; Karaiskou, G.; Wang, J.; Zoidis, P. PEEK Maxillary Obturator Prosthesis Fabrication Using Intraoral Scanning, 3D Printing, and CAD/CAM. Int. J. Prosthodont. 2020, 33, 333–340. [Google Scholar] [CrossRef]
- Sharaf, M.Y.; Eskander, A.E. PEEK versus Metallic Attachment-Retained Obturators for Patient Satisfaction: A Randomized Controlled Trial. Eur. J. Dent. 2022, 16, 80–95. [Google Scholar] [CrossRef]
- Lo Russo, L.; Chochlidakis, K.; Caradonna, G.; Molinelli, F.; Guida, L.; Ercoli, C. Removable Partial Dentures with Polyetheretherketone Framework: The Influence on Residual Ridge Stability. J. Prosthodont. Implant Esthet. Reconstr. Dent. 2021, 31, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Thoma, D.; Jung, R.; Zwahlen, M.; Zembic, A. A systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. Clin. Oral Implant. Res. 2012, 23, 22–38. [Google Scholar] [CrossRef] [PubMed]
- Scurria, M.S.; Bader, J.D.; Shugars, D.A. Meta-analysis of fixed partial denture survival: Prostheses and abutments. J. Prosthet. Dent. 1998, 79, 459–464. [Google Scholar] [CrossRef]
- Walmsley, A.D. Acrylic Partial Dentures. Dent. Update 2003, 30, 424–429. [Google Scholar] [CrossRef]
- Bergman, B.; Hugoson, A.; Olsson, C.-O. A 25 year longitudinal study of patients treated with removable partial dentures. J. Oral Rehabil. 1995, 22, 595–599. [Google Scholar] [CrossRef]
- Wyatt, C.C. The effect of prosthodontic treatment on alveolar bone loss: A review of the literature. J. Prosthet. Dent. 1998, 80, 362–366. [Google Scholar] [CrossRef]
- Jacobs, R.; van Steenberghe, D.; Nys, M.; Naert, I. Maxillary bone resorption in patients with mandibular implant-supported overdentures or fixed prostheses. J. Prosthet. Dent. 1993, 70, 135–140. [Google Scholar] [CrossRef]
- Lemos, C.A.A.; Nunes, R.G.; Santiago-Júnior, J.F.; Gomes, J.M.D.L.; Limirio, J.P.J.O.; Rosa, C.D.D.R.D.; Verri, F.R.; Pellizzer, E.P. Are implant-supported removable partial dentures a suitable treatment for partially edentulous patients? A systematic review and meta-analysis. J. Prosthet. Dent. 2021; in press. [Google Scholar] [CrossRef]
- Alrajhi, M.; Askar, O.; Habib, A.; Elsyad, M. Maxillary Bone Resorption with Conventional Dentures and Four-Implant–Supported Fixed Prosthesis Opposed by Distal-Extension Partial Dentures: A Preliminary 5-year Retrospective Study. Int. J. Oral Maxillofac. Implant. 2020, 35, 816–823. [Google Scholar] [CrossRef]
- Mutneja, P.; Shrivastava, S.P.; Dable, R.; Raj, A.N.; Srivastava, S.B.; Haque, M. Comparison of Mechanical Properties of PEEK and PMMA: An In Vitro Study. J. Contemp. Dent. Pract. 2021, 22, 179–183. [Google Scholar] [CrossRef]
- Darbar, U.R.; Huggett, R.; Harrison, A. Denture fracture—A survey. Br. Dent. J. 1994, 176, 342–345. [Google Scholar] [CrossRef] [PubMed]
- Mayinger, F.; Fiebig, M.; Roos, M.; Eichberger, M.; Lümkemann, N.; Stawarczyk, B. Bonding Behavior Between Polyetheretherketone and Polymethylmethacrylate Acrylic Denture Polymer. J. Adhes. Dent. 2021, 23, 145–158. [Google Scholar] [CrossRef] [PubMed]
| Study | Reason for Exclusion |
|---|---|
| Ye et al. [27] | Only workflow; PEEK denture not delivered to patient |
| Yue et al. [28] | PEEK framework not used |
| Ichikawa [29] | PEEK framework not used |
| No. | Study—Author(s) and Year | Type of Study | Patient (s) (n) | Age (Mean/Range) | Type/Brand of PEEK | Rehabilitation Details and/or Study Groups | Fabrication | Implants Placed (n) | Implant Dimensions (mm) | Duration of Study |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Costa-Palau et al., 2014 | Case report | 1 | 58 years | PEEK-Optima | Maxillary obturator. | Mechanical duplication of old obturator. | 0 | N/A | 6 months |
| 2 | Zoidis and Papathanasiou, 2016 | Case report | 1 | 52 years | BioHPP PEEK | Interim fixed implant-supported 3-unit prosthesis. | Digital scanning of wax pattern and injection molding. | 2 | L = 11.5 D = 4 | 4 months |
| 3 | Hahnel et al., 2017 | Case report | 1 | 76 years | Ceramill PEEK | Interim maxillary all-on-four implant-supported PEEK fixed prosthesis. | Conventional wax pattern. CAM | 4 | NR | 3 months |
| 4 | Zoidis 2017 | Case report | 1 | 65 years | BioHPP PEEK | Definitive maxillary fixed all-on-four implant-supported PEEK framework and PMMA base and veneers. | Conventional impression. Lost-wax and casting. | 4 | L = 11.5 D = 4 | 2 years |
| 5 | Sinha et al., 2017 | Case report | 1 | 32 years | PEEK-Optima | FPD. Upper and lower incisors replaced with canine–canine abutments. PEEK framework with resin composite veneers. | Conventional impression. Lost-wax and casting. | 0 | N/A | 6 months |
| 6 | Zoidis 2018 | Case report | 1 | 85 years | BioHPP PEEK | Removable mandibular PEEK framework and PMMA base retained by high noble ball attachments on both canines. | Conventional impression. Lost-wax casting. | 0 | N/A | Not reported |
| 7 | Harb et al., 2018 | Case report | 1 | 56 years | CeraMill PEEK | Removable PEEK mandibular Kennedy class I framework and PMMA base to replace first and second molars. | Conventional impressions. Digital scanning of a wax pattern. CAM. | 0 | N/A | Not reported |
| 8 | Mangano et al., 2019 | Prospective cohort | 15 | 68.8 ± 4.7 years | Not recorded | Each patient received one removable maxillary overdenture supported by 4 implants and PEEK bar. | CAD–CAM replication of a relined denture. CAD: Meshmixer, Autodesk CAM: 3500 PD 3D printer, DWS | 60 | L = 8–14 D = 3.3–4.8 | 1 year |
| 9 | Tasopoulos et al., 2020 | Case report | 1 | 47 years | BioHPP | Two-piece PEEK maxillary obturator; Kennedy Class II (canine to second molar). Acrylic supported by PEEK framework. | Material: BioHPP Construction of 3D model using wax pattern. CAD: 3Shape Dental CAM: External laboratory | 0 | N/A | 1 year |
| 10 | Wang et al., 2021 | Retrospective cohort | 43 | 59.8 years | BioHPP | Full-mouth FDP, 6 implants per arch (n = 60): Group I: PEEK framework and PMMA veneers (n = 29) Group II: Titanium framework and PMMA veneers (n = 31). | CAD: D2000 3D Scanner, 3Shape A/S CAM: 308 B, Willemin-Macodel (Ti), D3608, Sirona (PEEK) Dental Systems | 331 | N/A | 5 years |
| 11 | Sharaf and Eskandar 2021 | Randomised control trial | 18 | Not stated | Dental Direkt | Group I: Attachment-retained obturator with PEEK framework (n = 6) Group II: Attachment-retained obturator with metallic framework (n = 6) Group III: Conventional clasp-retained obturators with metallic framework (n = 6) | Conventional impressions. Digital scanning of wax pattern. CAM: Exocad GmbH | 0 | N/A | 12 months |
| 12 | Russo et al., 2021 | Case-control | 16 | 46–72 years | Not specified | Group I: RPD (n = 10) Group II: Untreated partially edentulous (n = 6) Changes in residual ridge investigated for 1 year. | CAD: TRIOS 3, 3Shape A/S CAM: SmilesPeek | 0 | N/A | 1 year |
| No. | Study—Author(s) and Year | Implant Outcomes | Prosthodontic Outcomes |
|---|---|---|---|
| 1 | Costa-Palau et al., 2014 | No implants placed | No complications reported |
| 2 | Zoidis and Papathanasiou, 2016 | No complications reported | No complications reported |
| 3 | Hahnel et al., 2017 | No complications reported | No complications reported. OVD increased successfully on final follow-up |
| 4 | Zoidis 2017 | No complications reported | No complications reported |
| 5 | Sinha et al., 2017 | No implants placed | No complications reported |
| 6 | Zoidis 2018 | No implants placed | No complications reported |
| 7 | Harb et al., 2018 | No implants placed | No complications reported |
| 8 | Mangano et al., 2019 | Peri-implantitis developed around 2 implants | 20% of the dentures failed due to inadequate passive fit. 2 fractured dentures had to be repaired. |
| 9 | Tasopoulos et al., 2020 | No implants placed | No complications reported |
| 10 | Wang et al., 2021 | BOP: PEEK: 13.8%; Ti: 16.1% Soft tissue inflammationl: PEEK: 3.4%; Ti: 3.2% TMJ disorders: PEEK: None; Ti; 6.5% VBL: PEEK: 0.70 mm; Ti: 0.96 mm | 5-year survival rate of PEEK and titanium overdentures comparable (93.1% and 93.5%, respectively). |
| 11 | Sharaf and Eskandar 2021 | No implants placed | Group I and II exhibited lesser bone loss and greater patient satisfaction than Group III. No statistical difference between Groups I and II. |
| 12 | Russo et al., 2021 | No implants placed | No significant differences between residual ridge changes in both groups |
| Study Characteristics | Study | |||||||
| Costa-Palau et al., 2013 | Zoidis and Papathanasiou, 2016 | Hahnel et al., 2017 | Zoidis 2017 | Sinha et al., 2017 | Zoidis 2017 | Harb et al., 2018 | Tasopoulos et al., 2020 |
| The diagnosis or intervention of primary focus followed by the words “case report” | Yes | Yes | Yes | Yes | No | Yes | Yes | No |
| ||||||||
| 2 to 5 keywords that identify diagnoses or interventions in this case report, including “case report” | No | No | No | No | Yes | Yes | Yes | No |
| ||||||||
| Introduction | No | No | Yes | Yes | Yes | Yes | No | No |
| Symptoms/findings | No | No | No | No | No | No | No | No |
| Diagnoses and prosthodontic outcomes | No | No | Yes | No | No | No | No | No |
| Conclusions | Yes | Yes | Yes | Yes | No | No | No | Yes |
| ||||||||
| One or two paragraphs summarising why this case is unique | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| ||||||||
| De-identified patient information | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Chief concerns and symptoms | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Medical, family, psycho-social history, genetic information | Yes | No | No | Yes | No | No | No | Yes |
| Relevant past interventions with outcomes | Yes | No | Yes | Yes | No | No | Yes | Yes |
| ||||||||
| Oral examination and important clinical findings | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| ||||||||
| Historical and current information from this episode of care organised as a timeline | No | No | No | No | No | No | No | No |
| ||||||||
| Oral examination | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Previous denture history | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Oral hygiene/periodontal status | No | No | No | No | Yes | Yes | No | |
| ||||||||
| Clinical procedures (impressions, intraoral scanning, surgery, etc.) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Laboratory procedures (wax-up, casting, fabrication, etc.) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Prosthesis design | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| ||||||||
| Follow-up time period | Yes | Yes | Yes | Yes | Yes | No | No | Yes |
| Patient-reported outcomes | Yes | Yes | Yes | Yes | No | No | Yes | No |
| Prosthesis and/or implant outcomes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes |
| Complications/adverse effects | No | Yes | Yes | Yes | Yes | No | No | No |
| ||||||||
| Strengths and limitations | No | No | No | No | No | No | No | No |
| Review of relevant literature | No | Yes | Yes | No | No | Yes | Yes | Yes |
| The scientific rationale for any conclusions | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes |
| Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| No | No | No | No | No | No | No | No |
| Overall quality | Low | Low | Medium | Medium | Low | Low | Low | Low |
| Section/Topic | Mangano et al., 2019 | Wang et al., 2021 | Russo et al., 2021 |
|---|---|---|---|
| |||
| Study design in title | No | Yes | No |
| Adequate abstract | Yes | Yes | Yes |
| |||
| Scientific background and rationale | Yes | Yes | Yes |
| State specific objectives and hypothesis | Yes | Yes | Yes |
| |||
| Study design | Yes | Yes | Yes |
| Recruitment, exposure, follow-up, and data collection | Yes | Yes | Yes |
| Participants | |||
| Eligibility criteria | No | Yes | No |
| Number of exposed and unexposed | No | No | No |
| Variables | |||
| Adequate description of variables | Yes | Yes | Yes |
| Data measurement | |||
| Sources and methods of measurement | Yes | Yes | Yes |
| Bias | |||
| Methods to reduce bias (randomisation or blinding) | No | No | No |
| Study size | |||
| Statistical calculation of sample size | No | No | No |
| Quantitative analysis | |||
| Description of quantitative variables | No | No | No |
| Statistical methods | |||
| Description of statistical methods | Yes | Yes | Yes |
| Subgroup analysis | No | No | No |
| Handling of missing data | No | No | No |
| Loss to follow-up | No | No | No |
| Sensitivity | No | No | No |
| |||
| Participants | |||
| Number analysed | Yes | Yes | Yes |
| Reasons for drop-out | No | No | No |
| Flow-diagram for recruitment | No | No | No |
| Descriptive data | |||
| Demographic, clinical and social data | No | No | No |
| Missing data | No | No | No |
| Follow-up time | Yes | Yes | Yes |
| Outcomes | |||
| Outcome events or summary measures | Yes | Yes | Yes |
| Main results | |||
| Confidence-interval | Yes | Yes | No |
| Category boundaries | No | No | No |
| Translation of relative to absolute risk | Yes | No | No |
| |||
| Key results | Yes | Yes | Yes |
| Limitations | Yes | Yes | Yes |
| Interpretation | Yes | Yes | Yes |
| Generalisability | Yes | Yes | Yes |
| Yes | Yes | Yes |
| Overall quality | Medium | Medium | Medium |
| Section/Topic | Quality Assessment |
|---|---|
| Study: Sharaf and Eskandar 2021 |
| Identification as a randomised trial | Yes |
| Structured summary of the study | Yes |
| |
| Scientific background and rationale | Yes |
| Specific objectives or hypotheses | Yes |
| |
| Description of trial design | Yes |
| Changes to methods | No |
| Eligibility criteria for participants | Yes |
| Settings and locations where the data were collected | No |
| The interventions for each group. | Yes |
| Primary and secondary outcome measures | |
| Any changes to trial outcomes | No |
| Sample size calculation | Yes |
| Method used to generate the random allocation sequence | Yes |
| Type of randomisation | Yes |
| Mechanism used to implement the random allocation sequence | Yes |
| Who generated the allocation sequence, who enrolled participants | No |
| Blinding of investigators | Yes |
| Description of the similarity of interventions | No |
| Appropriate statistics | Yes |
| |
| Number analysed | Yes |
| Losses and exclusions | Yes |
| Dates of recruitment and follow up | Yes |
| Why the trial ended or was stopped | No |
| Demographic and clinical characteristics for each group | No |
| For each group, number of participants included in each analysis | Yes |
| Estimated effect size and its precision (such as 95% confidence interval) | Yes |
| Absolute and relative effect sizes | No |
| Subgroup analysis | No |
| Harms or unintended effects in each group | No |
| |
| Trial limitations and addressing sources of potential bias | No |
| Generalisability of the trial findings | Yes |
| Interpretation consistent with results | Yes |
| |
| Registration number | Yes |
| Accessible protocol | Yes |
| Funding | Yes |
| Overall quality | Medium |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khurshid, Z.; Nedumgottil, B.M.; Ali, R.M.M.; Bencharit, S.; Najeeb, S. Insufficient Evidence to Ascertain the Long-Term Survival of PEEK Dental Prostheses: A Systematic Review of Clinical Studies. Polymers 2022, 14, 2441. https://doi.org/10.3390/polym14122441
Khurshid Z, Nedumgottil BM, Ali RMM, Bencharit S, Najeeb S. Insufficient Evidence to Ascertain the Long-Term Survival of PEEK Dental Prostheses: A Systematic Review of Clinical Studies. Polymers. 2022; 14(12):2441. https://doi.org/10.3390/polym14122441
Chicago/Turabian StyleKhurshid, Zohaib, Binoy Mathews Nedumgottil, Ramy Moustafa Moustafa Ali, Sompop Bencharit, and Shariq Najeeb. 2022. "Insufficient Evidence to Ascertain the Long-Term Survival of PEEK Dental Prostheses: A Systematic Review of Clinical Studies" Polymers 14, no. 12: 2441. https://doi.org/10.3390/polym14122441
APA StyleKhurshid, Z., Nedumgottil, B. M., Ali, R. M. M., Bencharit, S., & Najeeb, S. (2022). Insufficient Evidence to Ascertain the Long-Term Survival of PEEK Dental Prostheses: A Systematic Review of Clinical Studies. Polymers, 14(12), 2441. https://doi.org/10.3390/polym14122441









