Inhalable Spray-Dried Chondroitin Sulphate Microparticles: Effect of Different Solvents on Particle Properties and Drug Activity
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Polymer Purification
2.3. Microparticle Production
2.4. Characterisation of ChS-Based Microparticles
2.5. Determination of Drug Association and Release
2.6. Molecular Mass Distribution
2.7. Rheology: Steady-State Shear Measurements
2.8. Aerodynamic Characterisation of Microparticles Using an Andersen Cascade Impactor
2.9. In Vitro Determination of Antitubercular Activity
2.10. Statistical Analysis
3. Results and Discussion
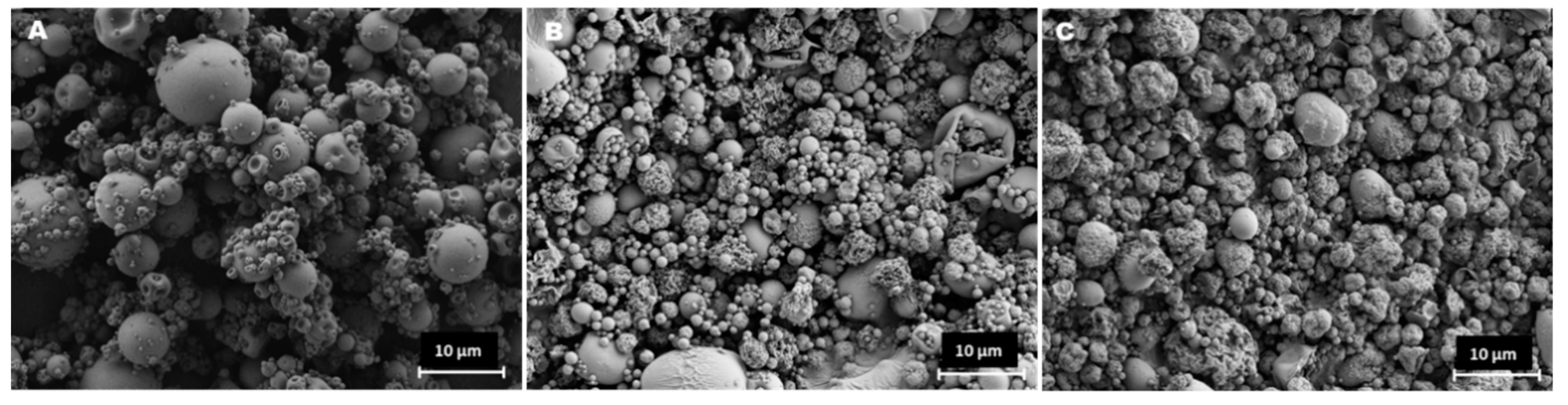
3.1. Preparation and Characterisation of ChS Microparticles
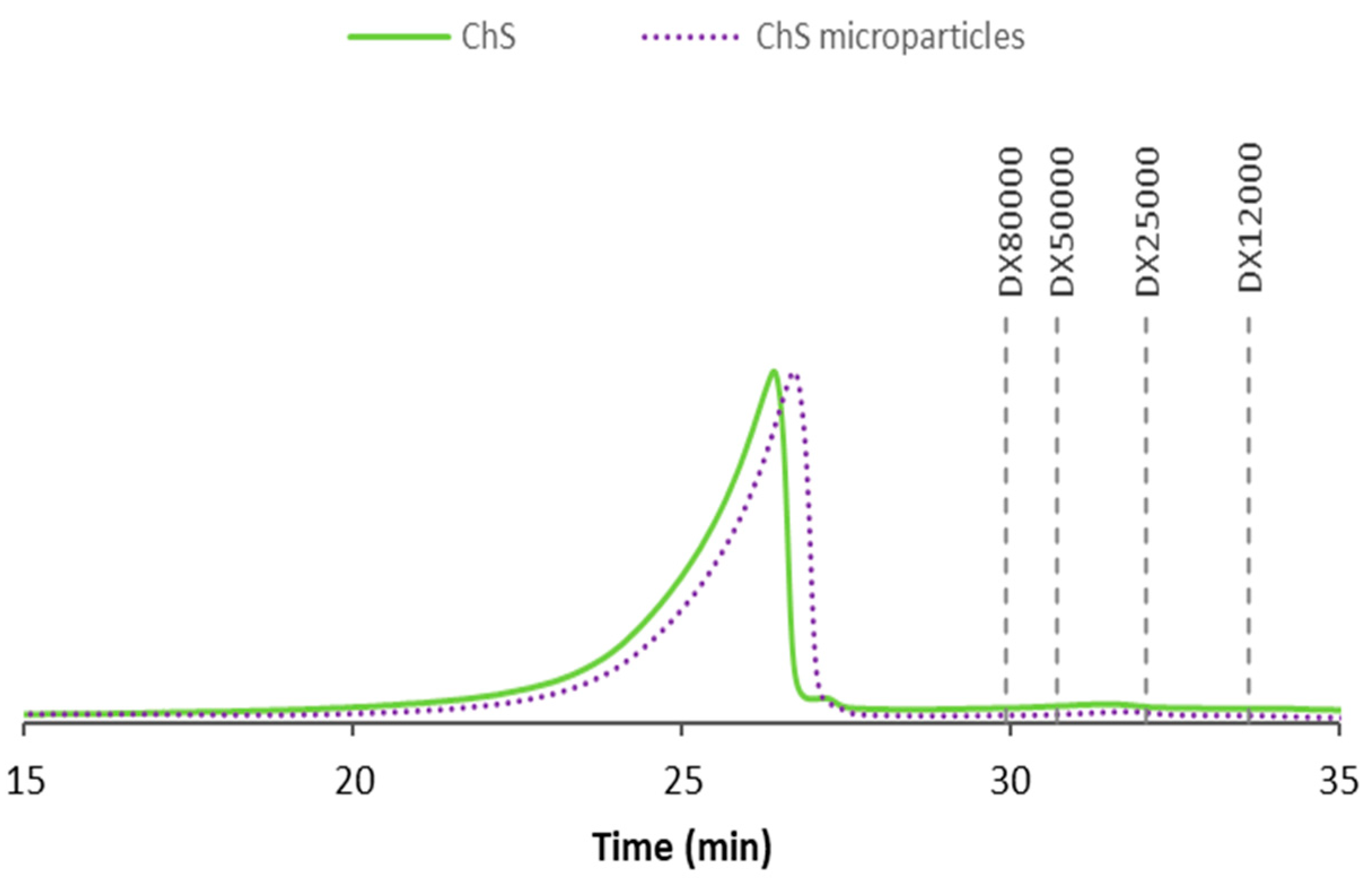
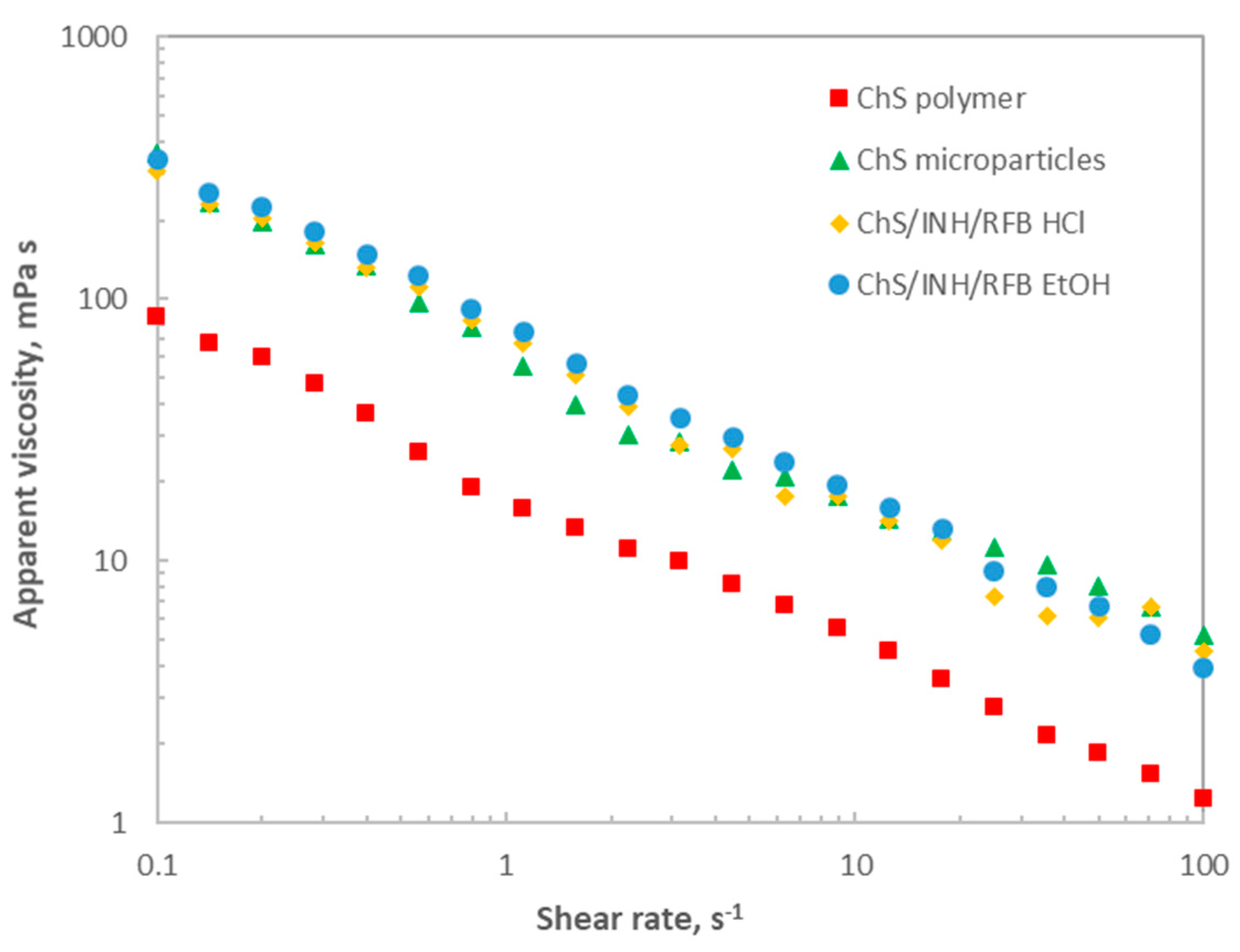
3.2. Impact of Spray-Drying on Polymer Characteristics
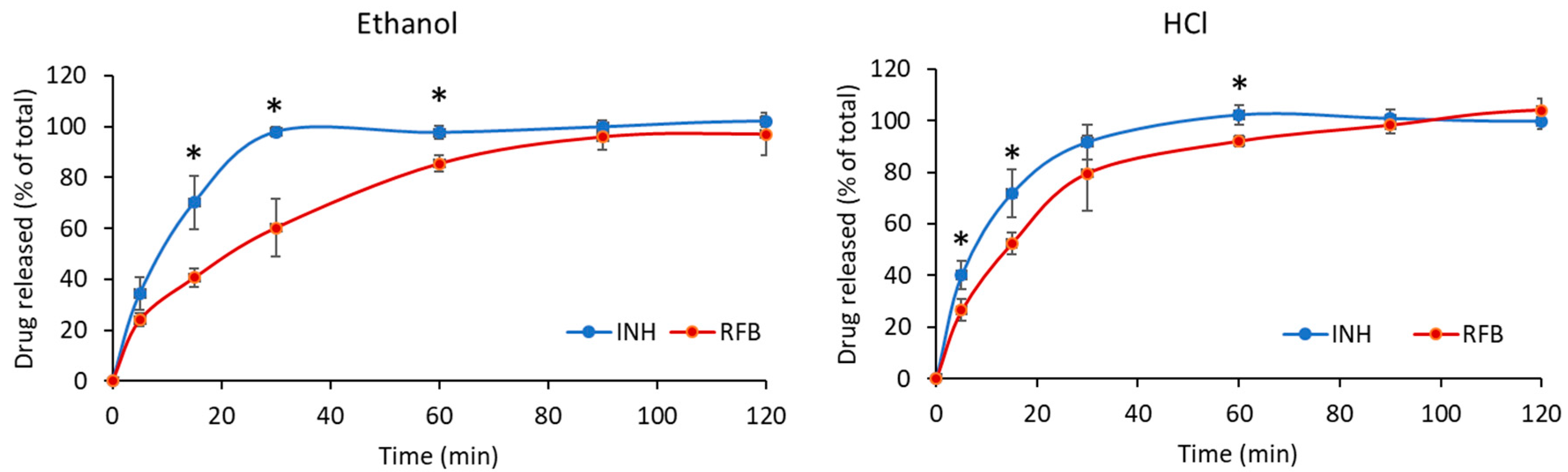
3.3. INH and RFB Release from ChS Microparticles
3.4. Antibacterial Activity of Drugs after Microencapsulation
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Smits, N.C.; Shworak, N.W.; Dekhuijzen, P.R.; Van Kuppevelt, T.H. Heparan sulfates in the lung: Structure, diversity, and role in pulmonary emphysema. Anat. Rec. (Hoboken) 2010, 293, 955–967. [Google Scholar] [CrossRef]
- Rachmilewitz, J.; Tykocinski, M.L. Differential effects of chondroitin sulfates A and B on monocyte and B-cell activation: Evidence for B-cell activation via a CD44-dependent pathway. Blood 1998, 92, 223–229. [Google Scholar] [CrossRef]
- Leteux, C.; Chai, W.; Loveless, R.W.; Yuen, C.T.; Uhlin-Hansen, L.; Combarnous, Y.; Jankovic, M.; Maric, S.C.; Misulovin, Z.; Nussenzweig, M.C.; et al. The cysteine-rich domain of the macrophage mannose receptor is a multispecific lectin that recognizes chondroitin sulfates A and B and sulfated oligosaccharides of blood group Lewis(a) and Lewis(x) types in addition to the sulfated N-glycans of lutropin. J. Exp. Med. 2000, 191, 1117–1126. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, S.; Grenha, A. Activation of macrophages: Establishing a role for polysaccharides in drug delivery strategies envisaging antibacterial therapy. Curr. Pharm. Design. 2015, 21, 4869–4887. [Google Scholar] [CrossRef] [PubMed]
- Falzon, D.; Schünemann, H.J.; Harausz, E.; González-Angulo, L.; Lienhardt, C.; Jaramillo, E.; Weyer, K. World Health Organization treatment guidelines for drug-resistant tuberculosis, 2016 update. Eur. Respir. J. 2017, 49, 1602308. [Google Scholar] [CrossRef] [PubMed]
- Matteelli, A.; Olliaro, P.; Signorini, L.; Cadeo, G.; Scalzini, A.; Bonazzi, L.; Caligaris, S.; Tomasoni, L.; Tebaldi, A.; Carosi, G. Tolerability of twice-weekly rifabutin-isoniazid combinations versus daily isoniazid for latent tuberculosis in HIV-infected subjects: A pilot study. Int. J. Tuberc. Lung Dis. 1999, 3, 1043–1046. [Google Scholar] [PubMed]
- Belotti, S.; Rossi, A.; Colombo, P.; Bettini, R.; Rekkas, D.; Politis, S.; Colombo, G.; Balducci, A.G.; Buttini, F. Spray-dried amikacin sulphate powder for inhalation in cystic fibrosis patients: The role of ethanol in particle formation. Eur. J. Pharm. Biopharm. 2015, 93, 165–172. [Google Scholar] [CrossRef]
- Nolan, L.M.; Tajber, L.; McDonald, B.F.; Barham, A.S.; Corrigan, O.I.; Healy, A.M. Excipient-free nanoporous microparticles of budesonide for pulmonary delivery. Eur. J. Pharm. Sci. 2009, 37, 593–602. [Google Scholar] [CrossRef]
- Agency, E.M. Guideline on Quality of Oral Modified Release Products; European Medicines Agency: Amsterdam, The Netherlands, 2014; pp. 1–16. [Google Scholar]
- Hiremath, P.S.; Saha, R.N. Controlled release hydrophilic matrix tablet formulations of isoniazid: Design and in vitro studies. AAPS PharmSciTech 2008, 9, 1171–1178. [Google Scholar] [CrossRef]
- Alves, A.D.; Cavaco, J.S.; Guerreiro, F.; Lourenço, J.P.; Da Costa, A.R.; Grenha, A.; Da Costa, A.M.R. Inhalable antitubercular therapy mediated by locust bean gum microparticles. Molecules 2016, 21, 702. [Google Scholar] [CrossRef]
- Shah, V.P.; Tsong, Y.; Sathe, P.; Liu, J. In Vitro Dissolution Profile Comparison—Statistics and Analysis of the Similarity Factor, f2. Pharm. Res. 1998, 15, 889–896. [Google Scholar] [CrossRef] [PubMed]
- USP. United States Pharmacopeia USP-38; USP: Rockville, MD, USA, 2015. [Google Scholar]
- European Pharmacopoeia; European Directorate for the Quality of Medicines: Strasbourg, France, 2014.
- Zgoda, J.; Porter, J. A convenient microdilution method for screening natural products against bacteria and fungi. Pharm. Biol. 2001, 39, 221–225. [Google Scholar] [CrossRef]
- Caviedes, L.; Delgado, J.; Gilman, R.H. Tetrazolium microplate assay as a rapid and inexpensive colorimetric method for determination of antibiotic susceptibility of Mycobacterium tuberculosis. J. Clin. Microbiol. 2002, 40, 1873–1874. [Google Scholar] [CrossRef]
- Vipra, A.; Desai, S.N.; Junjappa, R.P.; Roy, P.; Poonacha, N.; Ravinder, P.; Sriram, B.; Padmanabhan, S. Determining the minimum inhibitory concentration of bacteriophages: Potential advantages. Adv. Microbiol. 2013, 3, 181. [Google Scholar] [CrossRef]
- Arpagaus, C.; Schafroth, N.; Labortechnik, A.G.B. Spray Dried Biodegradable Polymers as Target Material for Controlled Drug Delivery. Best@ Büchi 2007, 46. [Google Scholar]
- Lee, E.S.; Park, K.-H.; Kang, N.; Park, I.S.; Min, H.Y.; Lee, D.H.; Kim, S.; Kim, J.H.; Na, K. Protein complexed with chondroitin sulfate in poly(lactide-co-glycolide) microspheres. Biomaterials 2007, 28, 2754–2762. [Google Scholar] [CrossRef]
- Lim, J.J.; Hammoudi, T.M.; Bratt-Leal, A.M.; Hamilton, S.K.; Kepple, K.L.; Bloodworth, N.C.; McDevitt, T.C. Development of nano- and microscale chondroitin sulfate particles for controlled growth factor delivery. Acta Biomater. 2011, 7, 986–995. [Google Scholar] [CrossRef]
- Huang, L.; Sui, W.; Wang, Y.; Jiao, Q. Preparation of chitosan/chondroitin sulfate complex microcapsules and application in controlled release of 5-fluorouracil. Carbohydr. Polym. 2010, 80, 168–173. [Google Scholar] [CrossRef]
- Hirota, K.; Hasegawa, T.; Hinata, H.; Ito, F.; Inagawa, H.; Kochi, C.; Soma, G.-I.; Makino, K.; Terada, H. Optimum conditions for efficient phagocytosis of rifampicin-loaded PLGA microspheres by alveolar macrophages. J. Control Release 2007, 119, 69–76. [Google Scholar] [CrossRef]
- Audran, R.; Peter, K.; Dannull, J.; Men, Y.; Scandella, E.; Groettrup, M.; Gander, B.; Corradin, G. Encapsulation of peptides in biodegradable microspheres prolongs their MHC class-I presentation by dendritic cells and macrophages in vitro. Vaccine 2003, 21, 1250–1255. [Google Scholar] [CrossRef]
- Reddy, S.T.; Swartz, M.A.; Hubbell, J.A. Targeting dendritic cells with biomaterials: Developing the next generation of vaccines. Trends Immunol. 2006, 27, 573–579. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.T.; Qu, L.; Larson, I.; Stewart, P.J.; Morton, D.A. Improving aerosolization of drug powders by reducing powder intrinsic cohesion via a mechanical dry coating approach. Int. J. Pharmaceut. 2010, 394, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Deng, Q.; Deng, L.; Miao, Y.; Guo, X.; Li, Y. Particle deposition in the human lung: Health implications of particulate matter from different sources. Environ. Res. 2019, 169, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Heyder, J.; Gebhart, J.; Rudolf, G.; Schiller, C.; Stahlhofen, W. Deposition of particles in the human respiratory tract in the size range 0.005–15 μm. J. Aerosol. Sci. 1986, 17, 811–825. [Google Scholar] [CrossRef]
- Rani, A.; Baruah, R.; Goyal, A. Physicochemical, antioxidant and biocompatible properties of chondroitin sulphate isolated from chicken keel bone for potential biomedical applications. Carbohyd. Polym. 2017, 159, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Imeson, A. Food Stabilisers, Thickeners and Gelling Agents; Wiley Online Library: Oxford, UK, 2010. [Google Scholar]
- Kyle, H.; Ward, J.; Widdicombe, J. Control. of pH of airway surface liquid of the ferret trachea in vitro. J. Appl. Physiol. 1990, 68, 135–140. [Google Scholar] [CrossRef]
- Griese, M. Pulmonary surfactant in health and human lung diseases: State of the art. Eur. Respr. J. 1999, 13, 1455–1476. [Google Scholar] [CrossRef]
- Vostrikov, V.V.; Selishcheva, A.A.; Sorokoumova, G.M.; Shakina, Y.N.; Shvets, V.I.; Savel’Ev, O.Y.; Polshakov, V.I. Distribution coefficient of rifabutin in liposome/water system as measured by different methods. Eur. J. Pharm. Biopharm. 2008, 68, 400–405. [Google Scholar] [CrossRef]
- Cunha, L.; Rodrigues, S.; Da Costa, A.R.; Faleiro, M.L.; Buttini, F.; Grenha, A.; Da Costa, A.M.R. Inhalable Fucoidan Microparticles Combining Two Antitubercular Drugs with Potential Application in Pulmonary Tuberculosis Therapy. Polymers 2018, 10, 636. [Google Scholar] [CrossRef]
- Rodrigues, S.; Alves, A.D.; Cavaco, J.S.; Pontes, J.F.; Guerreiro, F.; Da Costa, A.M.R.; Buttini, F.; Grenha, A. Dual antibiotherapy of tuberculosis mediated by inhalable locust bean gum microparticles. Int. J. Pharm. 2017, 529, 433–441. [Google Scholar] [CrossRef]
- Cunha, L.; Rodrigues, S.; Da Costa, A.M.R.; Faleiro, L.; Buttini, F.; Grenha, A. Inhalable chitosan microparticles for simultaneous delivery of isoniazid and rifabutin in lung tuberculosis treatment. Drug Dev. Ind. Pharm. 2019, 45, 1313–1320. [Google Scholar] [CrossRef] [PubMed]
- Gupta, K.C.; Jabrail, F.H. Effect of molecular weight and degree of deacetylation on controlled release of isoniazid from chitosan microspheres. Polym. Adv. Technol. 2008, 19, 432–441. [Google Scholar] [CrossRef]
- Martinez, A.W.; Caves, J.M.; Ravi, S.; Li, W.; Chaikof, E.L. Effects of crosslinking on the mechanical properties, drug release and cytocompatibility of protein polymers. Acta Biomater. 2014, 10, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Fronius, M.; Clauss, W.G.; Althaus, M. Why do we have to move fluid to be able to breathe? Front. Physiol. 2012, 3, 146. [Google Scholar] [CrossRef] [PubMed]
- Ritz, N.; Tebruegge, M.; Connell, T.G.; Sievers, A.; Robins-Browne, R.; Curtis, N. Susceptibility of Mycobacterium bovis BCG vaccine strains to antituberculous antibiotics. Antimicrob. Agents Chemother. 2009, 53, 316–318. [Google Scholar] [CrossRef] [PubMed]
- Shishido, Y.; Mitarai, S.; Otomo, K.; Seki, M.; Sato, A.; Yano, I.; Koyama, A.; Hattori, T. Anti-tuberculosis drug susceptibility testing of Mycobacterium bovis BCG Tokyo strain. Int. J. Tuberc. Lung D 2007, 11, 1334–1338. [Google Scholar]
| Stage-1 | Stage-0 | Stage 1 | Stage 2 | Stage 3 | Stage 4 | Stage 5 | Stage 6 |
|---|---|---|---|---|---|---|---|
| 8.60 | 6.50 | 4.40 | 3.20 | 1.90 | 1.20 | 0.55 | 0.26 |
| Microparticles | PY (%) | Dv50 (µm) | Span | Tap density (g/cm3) | AE% | LC% |
|---|---|---|---|---|---|---|
| ChS | 73.3 ± 4.4a | 9.6 ± 0.2c | 2.0 ± 0.0e | 0.50 ± 0.01g | n. a. | n. a. |
| ChS/INH/RFB (ethanol) | 83.4 ± 1.0b | 4.1 ± 0.1d | 2.9 ± 0.1f | 0.32 ± 0.03h | INH: 94.9 ± 5.7j | INH: 8.2 ± 0.5m |
| RFB: 59.0 ± 6.9k | RFB: 2.6 ± 0.3n | |||||
| ChS/INH/RFB (HCl) | 84.9 ± 1.1b | 4.1 ± 0.0d | 3.1 ± 0.1f | 0.58 ± 0.02i | INH: 94.6 ± 4.0j | INH: 8.2 ± 0.3m |
| RFB: 67.6 ± 1.4l | RFB: 2.9 ± 0.1o |
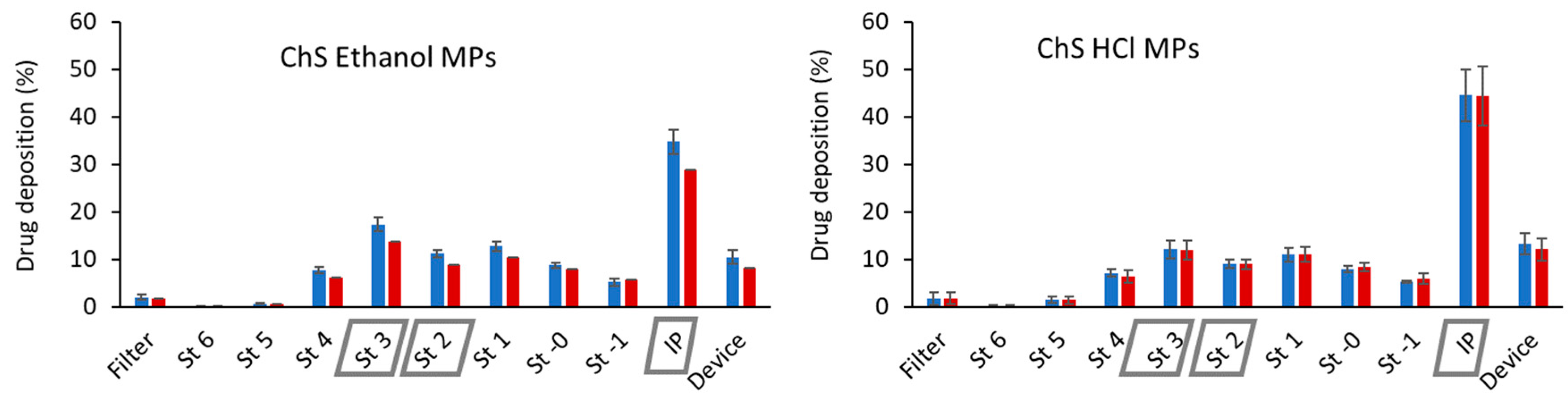
| Microparticles | Powder Emitted Dose (%) | Drug | MMAD (µm) | GSD (µm) | FPD (mg) | FPF (%) |
|---|---|---|---|---|---|---|
| ChS/INH/RFB (ethanol) | 90.9 ± 1.0a | INH | 3.8 ± 0.1b | 1.9 ± 0.1c | 3.1 ± 0.3d | 43.7 ± 2.4g |
| RFB | 3.9 ± 0.1 b | 2.0 ± 0.1c | 1.5 ± 0.1e | 42.6 ± 1.7g | ||
| ChS/INH/RFB (HCl) | 89.6 ± 1.8a | INH | 4.0 ± 0.2 b | 2.0 ± 0.0c | 2.9 ± 0.1d | 35.0 ± 1.7h |
| RFB | 4.0 ± 0.3 b | 2.1 ± 0.1c | 1.2 ± 0.1f | 34.0 ± 3.7h |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodrigues, S.; da Costa, A.M.R.; Flórez-Fernández, N.; Torres, M.D.; Faleiro, M.L.; Buttini, F.; Grenha, A. Inhalable Spray-Dried Chondroitin Sulphate Microparticles: Effect of Different Solvents on Particle Properties and Drug Activity. Polymers 2020, 12, 425. https://doi.org/10.3390/polym12020425
Rodrigues S, da Costa AMR, Flórez-Fernández N, Torres MD, Faleiro ML, Buttini F, Grenha A. Inhalable Spray-Dried Chondroitin Sulphate Microparticles: Effect of Different Solvents on Particle Properties and Drug Activity. Polymers. 2020; 12(2):425. https://doi.org/10.3390/polym12020425
Chicago/Turabian StyleRodrigues, Susana, Ana M. Rosa da Costa, Noelia Flórez-Fernández, María Dolores Torres, Maria Leonor Faleiro, Francesca Buttini, and Ana Grenha. 2020. "Inhalable Spray-Dried Chondroitin Sulphate Microparticles: Effect of Different Solvents on Particle Properties and Drug Activity" Polymers 12, no. 2: 425. https://doi.org/10.3390/polym12020425
APA StyleRodrigues, S., da Costa, A. M. R., Flórez-Fernández, N., Torres, M. D., Faleiro, M. L., Buttini, F., & Grenha, A. (2020). Inhalable Spray-Dried Chondroitin Sulphate Microparticles: Effect of Different Solvents on Particle Properties and Drug Activity. Polymers, 12(2), 425. https://doi.org/10.3390/polym12020425







