Impact of Hydrofluoric Acid, Ytterbium Fiber Lasers, and Hydroxyapatite Nanoparticles on Surface Roughness and Bonding Strength of Resin Cement with Different Viscosities to Lithium Disilicate Glass Ceramic: SEM and EDX Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Preparation and Sample Size Calculation
2.1.1. Group 1: HFA-S (Control)
2.1.2. Group 2: YFL-S
2.1.3. Group 3: HANPs-S
2.2. Assessment of Ra
2.3. Topographic Changes in LDC Discs via SEM
2.4. Resin Cement Bonding
2.5. Thermocycling
2.6. SBS and Failure Mode Analysis
2.7. Statistical Analysis
3. Results
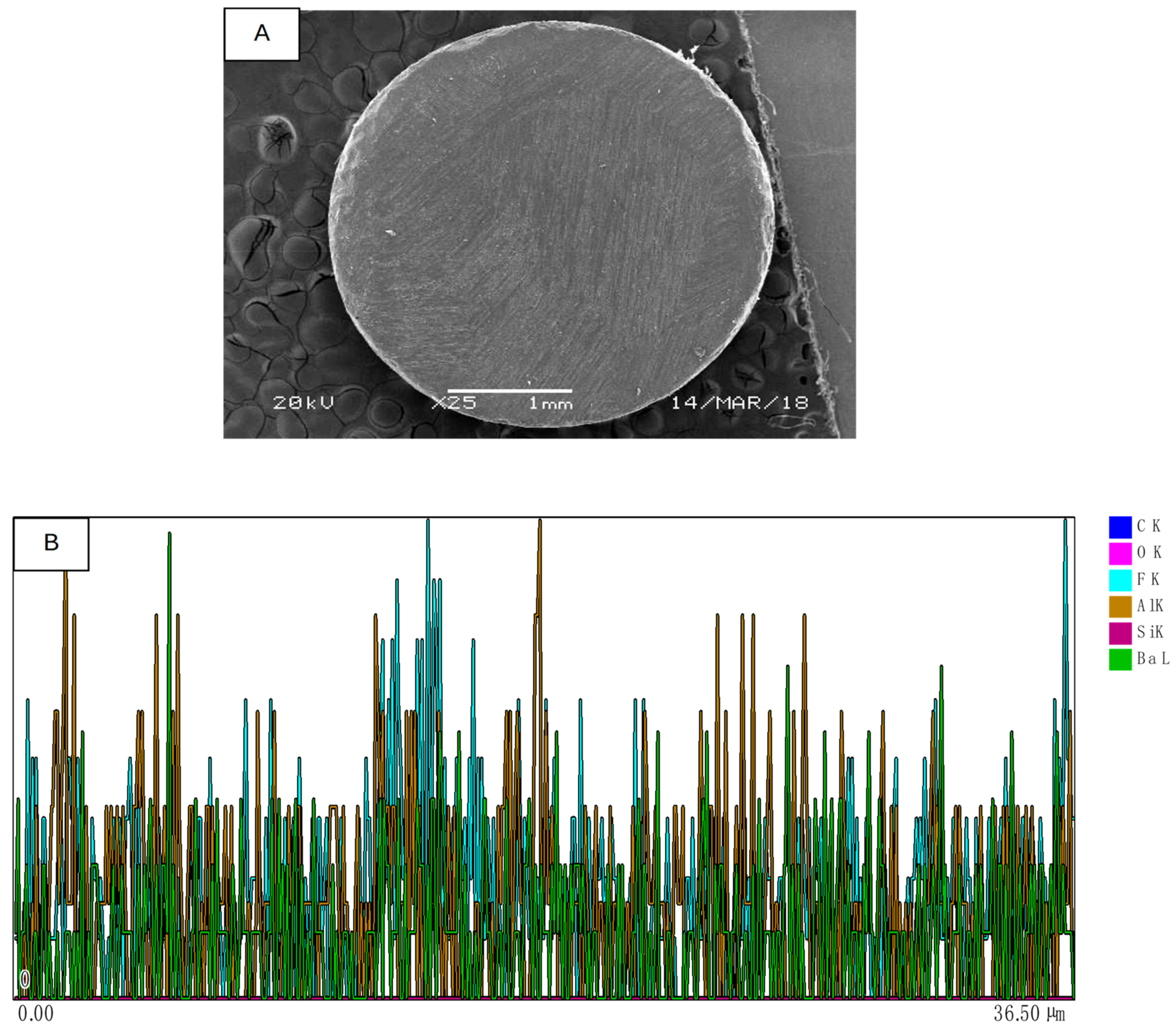
3.1. SEM and EDS Assessment
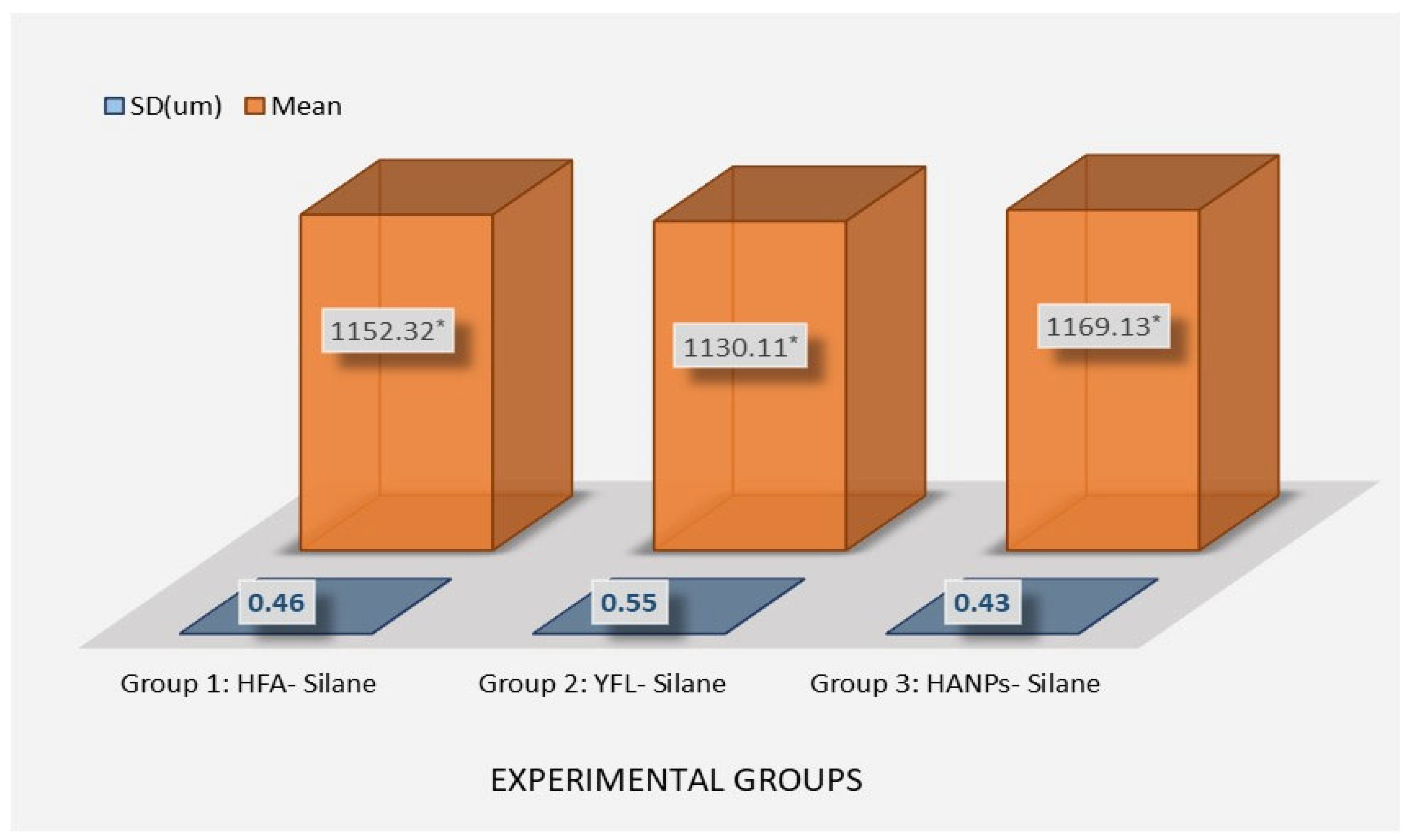
3.2. Ra Analysis
3.3. SBS Analysis
3.4. Fracture Pattern Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ahmed, K.E. We’re Going Digital: The Current State of CAD/CAM Dentistry in Prosthodontics. Prim. Dent. J. 2018, 7, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Maawadh, A.M.; Almohareb, T.; Al-Hamdan, R.S.; Al Deeb, M.; Naseem, M.; Alhenaki, A.M.; Vohra, F.; Abduljabbar, T. Repair Strength and Surface Topography of Lithium Disilicate and Hybrid Resin Ceramics with LLLT and Photodynamic Therapy in Comparison to Hydrofluoric Acid. J. Appl. Biomater. Funct. Mater. 2020, 18, 2280800020966938. [Google Scholar] [CrossRef] [PubMed]
- Alkhudhairy, F.; Naseem, M.; Ahmad, Z.H.; Alnooh, A.N.; Vohra, F. Efficacy of Phototherapy with Different Conventional Surface Treatments on Adhesive Quality of Lithium Disilicate Ceramics. Photodiagnosis Photodyn. Ther. 2019, 25, 292–295. [Google Scholar] [CrossRef] [PubMed]
- Chiapinotto, G.F.; da Rosa, L.S.; Scotti, N.; Kleverlaan, C.J.; Valandro, L.F.; Pereira, G.K.R. Does Adhesive Luting Promote Improved Fatigue Performance of Lithium Disilicate Simplified Crowns? J. Mech. Behav. Biomed. Mater. 2022, 134, 105373. [Google Scholar] [CrossRef] [PubMed]
- Albaker, A.M.; Al Deeb, L.; Alhenaki, A.M.; Aldeeb, M.; Al Ahdal, K.; Abduljabbar, T.; Vohra, F. Bonding Integrity and Compressive Strength of Re-Bonded, Surface Conditioned and Er Cr YSGG Laser Treated Lithium Disilicate Ceramics. J. Appl. Biomater. Funct. Mater. 2020, 18, 2280800020910954. [Google Scholar] [CrossRef] [PubMed]
- Basunbul, G.I.; Alzahrani, K.M.; Almutairi, B.; Alsunbul, H.; Abduljabbar, T. The Impact of Riboflavin, Nd: YAG Laser, and Ceramic Primer Pretreatment on Surface Roughness, Bond Failure, and Adhesive Strength of Resin Composite to Lithium Disilicate Ceramics: A Scanning Electron Microscopy (SEM) Analysis. J. Biomater. Tissue Eng. 2024, 13, 882–887. [Google Scholar] [CrossRef]
- Kim, K.J.; Park, Y.T.; Yoo, J.H.; Park, T.H. Hydrofluoric Acid Burns. Exog. Dermatol. 2004, 3, 12–18. [Google Scholar] [CrossRef]
- Özcan, M.; Allahbeickaraghi, A.; Dündar, M. Possible Hazardous Effects of Hydrofluoric Acid and Recommendations for Treatment Approach: A Review. Clin. Oral Investig. 2012, 16, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Alkhudhairy, F.; AlKheraif, A.; Bin-Shuwaish, M.; Al-Johany, S.; Naseem, M.; Vohra, F. Effect of Er,Cr:YSGG Laser and Ascorbic Acid on the Bond Strength and Microleakage of Bleached Enamel Surface. Photomed. Laser Surg. 2018, 36, 431–438. [Google Scholar] [CrossRef] [PubMed]
- Maziero Volpato, C.A.; Carvalho, O.; Özcan, M.; Fredel, M.C.; Silva, F.S. Effect of Laser Irradiation on the Adhesion of Resin-Based Materials to Zirconia: A Systematic Review and Meta-Analysis. J. Adhes. Sci. Technol. 2021, 35, 1035–1056. [Google Scholar] [CrossRef]
- Alkan Demetoğlu, G.; Talay Çevlïk, E. Evaluation of the Effect of Etching with Ytterbium Fiber Laser on the Bond Strength, Color Stability, and Fracture Analysis of Lithium Disilicate Ceramics to Bovine Teeth: An in Vitro Study. BMC Oral Health 2025, 25, 607. [Google Scholar] [CrossRef] [PubMed]
- Toyoda, K.; Taniguchi, Y.; Nakamura, K.; Isshi, K.; Kakura, K.; Ikeda, H.; Shimizu, H.; Kido, H.; Kawaguchi, T. Effects of Ytterbium Laser Surface Treatment on the Bonding of Two Resin Cements to Zirconia. Dent. Mater. J. 2022, 41, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Al-Hamdan, R.S.; Almutairi, B.; Kattan, H.F.; Alsuwailem, N.A.; Farooq, I.; Vohra, F.; Abduljabbar, T. Influence of Hydroxyapatite Nanospheres in Dentin Adhesive on the Dentin Bond Integrity and Degree of Conversion: A Scanning Electron Microscopy (SEM), Raman, Fourier Transform-Infrared (FTIR), and Microtensile Study. Polymers 2020, 12, 2948. [Google Scholar] [CrossRef] [PubMed]
- Yadav, R.; Meena, A.; Patnaik, A. Tribological Behavior of Zinc Oxide-hydroxyapatite Particulates Filled Dental Restorative Composite Materials. Polym. Compos. 2022, 43, 3029–3040. [Google Scholar] [CrossRef]
- Huang, S.; Gao, S.; Cheng, L.; Yu, H. Remineralization Potential of Nano-Hydroxyapatite on Initial Enamel Lesions: An in Vitro Study. Caries Res. 2011, 45, 460–468. [Google Scholar] [CrossRef] [PubMed]
- Butera, A.; Gallo, S.; Pascadopoli, M.; Montasser, M.A.; Abd El Latief, M.H.; Modica, G.G.; Scribante, A. Home Oral Care with Biomimetic Hydroxyapatite vs. Conventional Fluoridated Toothpaste for the Remineralization and Desensitizing of White Spot Lesions: Randomized Clinical Trial. Int. J. Environ. Res. Public Health 2022, 19, 8676. [Google Scholar] [CrossRef] [PubMed]
- Alkhudhairy, F.; Shono, N.N. Surface Roughness and Shear Bond Strength of Y-TZP Treated via Tri-Biochemical Silica Coating, Femtosecond Laser, and Nano-Hydroxyapatite: An SEM Assessment. J. Ceram. Sci. Technol. 2025, 16, 45–50. [Google Scholar] [CrossRef]
- Marshall, S.J.; Bayne, S.C.; Baier, R.; Tomsia, A.P.; Marshall, G.W. A Review of Adhesion Science. Dent. Mater. 2010, 26, e11–e16. [Google Scholar] [CrossRef] [PubMed]
- Barbon, F.J.; Moraes, R.R.; Isolan, C.P.; Spazzin, A.O.; Boscato, N. Influence of Inorganic Filler Content of Resin Luting Agents and Use of Adhesive on the Performance of Bonded Ceramic. J. Prosthet. Dent. 2019, 122, 566.e1–566.e11. [Google Scholar] [CrossRef] [PubMed]
- Beketova, A.; Tzanakakis, E.G.C.; Vouvoudi, E.; Anastasiadis, K.; Rigos, A.E.; Pandoleon, P.; Bikiaris, D.; Tzoutzas, I.G.; Kontonasaki, E. Zirconia Nanoparticles as Reinforcing Agents for Contemporary Dental Luting Cements: Physicochemical Properties and Shear Bond Strength to Monolithic Zirconia. Int. J. Mol. Sci. 2023, 24, 2067. [Google Scholar] [CrossRef] [PubMed]
- Alkhudhairy, F.; AlFawaz, Y.F. Pretreatment of Hybrid Ceramics Using Ho: YAG, Low-Level Laser Therapy Activated Malachite Green, and Non-Thermal Plasma on Surface Roughness, Bond Strength, and Color Change, SEM and EDX Analysis. Ceramics 2024, 7, 944–957. [Google Scholar] [CrossRef]
- Mutluay Unal, S.; Ozkir, S.E.; Seyfioglu Polat, Z.; Guven, S.; Asutay, H. The Effect of Ytterbium-Doped Fiber Laser with Different Parameters on Physical Properties of Zirconia Surface. Photomed. Laser Surg. 2017, 35, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Fornaini, C.; Poli, F.; Merigo, E.; Lutey, A.; Cucinotta, A.; Chevalier, M.; Mckee, S.; Brulat, N.; Rocca, J.P.; Trevisi, G. Nanosecond Pulsed Fiber Laser Irradiation for Enhanced Zirconia Crown Adhesion: Morphological, Chemical, Thermal and Mechanical Analysis. J. Photochem. Photobiol. B Biol. 2021, 219, 112189. [Google Scholar] [CrossRef] [PubMed]
- Almohareb, T.; Maawadh, A.; AlDeeb, L.; Alahdal, K.; Alshamrani, A.S.; Alrahlah, A. Influence of High- and Low-Viscosity Resin Cement and Artificial Aging on Bond Integrity and Surface Roughness of Lithium Disilicate Ceramics Pretreated with Ho:YAG Laser and Nano-Hydroxyapatite Coatings. J. Ceram. Sci. Technol. 2025, 16, 29–36. [Google Scholar] [CrossRef]
- Cho, J.H.; Kim, S.J.; Shim, J.S.; Lee, K.W. Effect of Zirconia Surface Treatment Using Nitric Acid-Hydrofluoric Acid on the Shear Bond Strengths of Resin Cements. J. Adv. Prosthodont. 2017, 9, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Dapieve, K.S.; Pereira, G.K.R.; Venturini, A.B.; Daudt, N.; Valcanaia, A.; Bottino, M.C.; Valandro, L.F. Do Resin Cement Viscosity and Ceramic Surface Etching Influence the Fatigue Performance of Bonded Lithium Disilicate Glass-Ceramic Crowns? Dent. Mater. 2022, 38, e59–e67. [Google Scholar] [CrossRef] [PubMed]
- Guarda, G.B.; Correr, A.B.; Gonçalves, L.S.; Costa, A.R.; Borges, G.A.; Sinhoreti, M.A.C.; Correr-Sobrinho, L. Effects of Surface Treatments, Thermocycling, and Cyclic Loading on the Bond Strength of a Resin Cement Bonded to a Lithium Disilicate Glass Ceramic. Oper. Dent. 2013, 38, 208–217. [Google Scholar] [CrossRef] [PubMed]
- Alrahlah, A.; Awad, M.M.; Vohra, F.; Al-Mudahi, A.; Al jeaidi, Z.A.; Elsharawy, M. Effect of Self Etching Ceramic Primer and Universal Adhesive on Bond Strength of Lithium Disilicate Ceramic. J. Adhes. Sci. Technol. 2017, 31, 2611–2619. [Google Scholar] [CrossRef]
- Vohra, F.; Labban, N.; Al-Hussaini, A.; Al-Jarboua, M.; Zawawi, R.; Alrahlah, A.; Naseem, M. Influence of Er;Cr:YSGG Laser on Shear Bond Strength and Color Stability of Lithium Disilicate Ceramics: An in Vitro Study. Photobiomodulation Photomed. Laser Surg. 2019, 37, 483–488. [Google Scholar] [CrossRef] [PubMed]
- Attia, A. Bond Strength of Three Luting Agents to Zirconia Ceramic—Influence of Surface Treatment and Thermocycling. J. Appl. Oral Sci. 2011, 19, 388–395. [Google Scholar] [CrossRef] [PubMed]
- Kukiattrakoon, B.; Thammasitboon, K. The Effect of Different Etching Times of Acidulated Phosphate Fluoride Gel on the Shear Bond Strength of High-Leucite Ceramics Bonded to Composite Resin. J. Prosthet. Dent. 2007, 98, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Strasser, T.; Preis, V.; Behr, M.; Rosentritt, M. Roughness, Surface Energy, and Superficial Damages of CAD/CAM Materials after Surface Treatment. Clin. Oral Investig. 2018, 22, 2787–2797. [Google Scholar] [CrossRef] [PubMed]
- Yavuz, T.; Eraslan, O. The Effect of Silane Applied to Glass Ceramics on Surface Structure and Bonding Strength at Different Temperatures. J. Adv. Prosthodont. 2016, 8, 75–84. [Google Scholar] [CrossRef] [PubMed]
- Simões, A.C.; Miranda, J.S.; Souza, R.O.d.A.e.; Kimpara, E.T.; Leite, F.P.P. Bond and Topography Evaluation of a Y-TZP Ceramic with a Superficial Low-Fusing Porcelain Glass Layer After Different Hydrofluoric Acid Etching Protocols. Rev. Odontol. UNESP 2018, 47, 348–353. [Google Scholar] [CrossRef]
- Siwen, L.; Shishi, L.; Yanhong, W.; Hongmei, M. Effects of Different Surface Modifications on Micro-Structure and Adhesion of Zirconia Ceramic: An In Vitro Study. Hua Xi Kou Qiang Yi Xue Za Zhi 2017, 35, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Alkhudhairy, F.; Shono, N.N. An Investigation of Y-TZP Surface Characteristics and Adhesive Properties Following Treatment with Tri-Biochemical Silica Coating, Femtosecond Laser, and Nano-Hydroxyapatite: A Scanning Electron Microscopy Evaluation. Pakistan J. Med. Sci. 2025, 41, 758–762. [Google Scholar] [CrossRef] [PubMed]
- Upadhyay, A.; Pradhan, L.; Yenurkar, D.; Kumar, K.; Mukherjee, S. Advancement in Ceramic Biomaterials for Dental Implants. Int. J. Appl. Ceram. Technol. 2024, 21, 2796–2817. [Google Scholar] [CrossRef]
- Aljamhan, A.S.; Alrefeai, M.H.; Alhabdan, A.; Alhusseini, S.A.; Farooq, I.; Vohra, F.; Naseem, M.; Alkhudhairy, F. Influence of ER-CR-YSGG Laser and Photodynamic Therapy on the Dentin Bond Integrity of Nano-Hydroxyapatite Containing Resin Dentin Adhesive: SEM-EDX, Micro-Raman, Micro-Tensile, and FTIR Evaluation. Polymers 2021, 13, 1903. [Google Scholar] [CrossRef] [PubMed]
- Dapieve, K.S.; Velho, H.C.; da Rosa, L.S.; Pivetta, J.P.; Maidana, F.C.; Venturini, A.B.; Kleverlaan, C.J.; Pereira, G.K.R.; Valandro, L.F. Ceramic Surface Conditioning, Resin Cement Viscosity, and Aging Relationships Affect the Load-Bearing Capacity Under Fatigue of Bonded Glass-Ceramics. J. Mech. Behav. Biomed. Mater. 2023, 139, 105667. [Google Scholar] [CrossRef] [PubMed]
- Alnazeh, A.A. Pretreatment of Enamel with Riboflavin Activated Photodynamic Therapy and Er, Cr: YSGG Laser for Bonding of Orthodontic Bracket with Adhesive Modified with Cerium Oxide Nanoparticles. Photodiagnosis Photodyn. Ther. 2024, 49, 104285. [Google Scholar] [CrossRef] [PubMed]
- Erdur, E.A.; Basciftci, F.A. Effect of Ti:Sapphire-Femtosecond Laser on the Surface Roughness of Ceramics. Lasers Surg. Med. 2015, 47, 833–838. [Google Scholar] [CrossRef] [PubMed]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aljamhan, A.; Alkhudhairy, F. Impact of Hydrofluoric Acid, Ytterbium Fiber Lasers, and Hydroxyapatite Nanoparticles on Surface Roughness and Bonding Strength of Resin Cement with Different Viscosities to Lithium Disilicate Glass Ceramic: SEM and EDX Analysis. Crystals 2025, 15, 661. https://doi.org/10.3390/cryst15070661
Aljamhan A, Alkhudhairy F. Impact of Hydrofluoric Acid, Ytterbium Fiber Lasers, and Hydroxyapatite Nanoparticles on Surface Roughness and Bonding Strength of Resin Cement with Different Viscosities to Lithium Disilicate Glass Ceramic: SEM and EDX Analysis. Crystals. 2025; 15(7):661. https://doi.org/10.3390/cryst15070661
Chicago/Turabian StyleAljamhan, Abdullah, and Fahad Alkhudhairy. 2025. "Impact of Hydrofluoric Acid, Ytterbium Fiber Lasers, and Hydroxyapatite Nanoparticles on Surface Roughness and Bonding Strength of Resin Cement with Different Viscosities to Lithium Disilicate Glass Ceramic: SEM and EDX Analysis" Crystals 15, no. 7: 661. https://doi.org/10.3390/cryst15070661
APA StyleAljamhan, A., & Alkhudhairy, F. (2025). Impact of Hydrofluoric Acid, Ytterbium Fiber Lasers, and Hydroxyapatite Nanoparticles on Surface Roughness and Bonding Strength of Resin Cement with Different Viscosities to Lithium Disilicate Glass Ceramic: SEM and EDX Analysis. Crystals, 15(7), 661. https://doi.org/10.3390/cryst15070661





