Heart Rate Variability-Based Stress Detection and Fall Risk Monitoring During Daily Activities: A Machine Learning Approach
Abstract
1. Introduction
1.1. Heart Rate Variability, Stress and Postural Balance
- RR Intervals: The intervals between consecutive heartbeats.
- The Standard Deviation of RR Intervals (SDRR): This measures the variability in RR intervals.
- The Root Mean Square of the Successive Differences in RR Intervals (RMSSD): This quantifies the short-term variability in RR intervals.
- The Proportion of NN50: The number of pairs of successive RR intervals that differ by more than 50 ms, divided by the total number of RR intervals, denoted as pNN50.
- Spectral Power in High-Frequency Components: This reflects the parasympathetic activity.
- Low-Frequency/High-Frequency Ratio (LF/HF Ratio): This indicates the balance between sympathetic and parasympathetic nervous system activities.
1.2. Machine Learning in HRV Analysis
1.3. Objectives of the Study
2. Materials and Methods
2.1. Participants
2.2. Data Collection
2.3. IBI Signal Pre-Processing
2.4. HRV Feature Extraction
2.4.1. Non-Linear Dynamics
2.4.2. Time Domain HRV
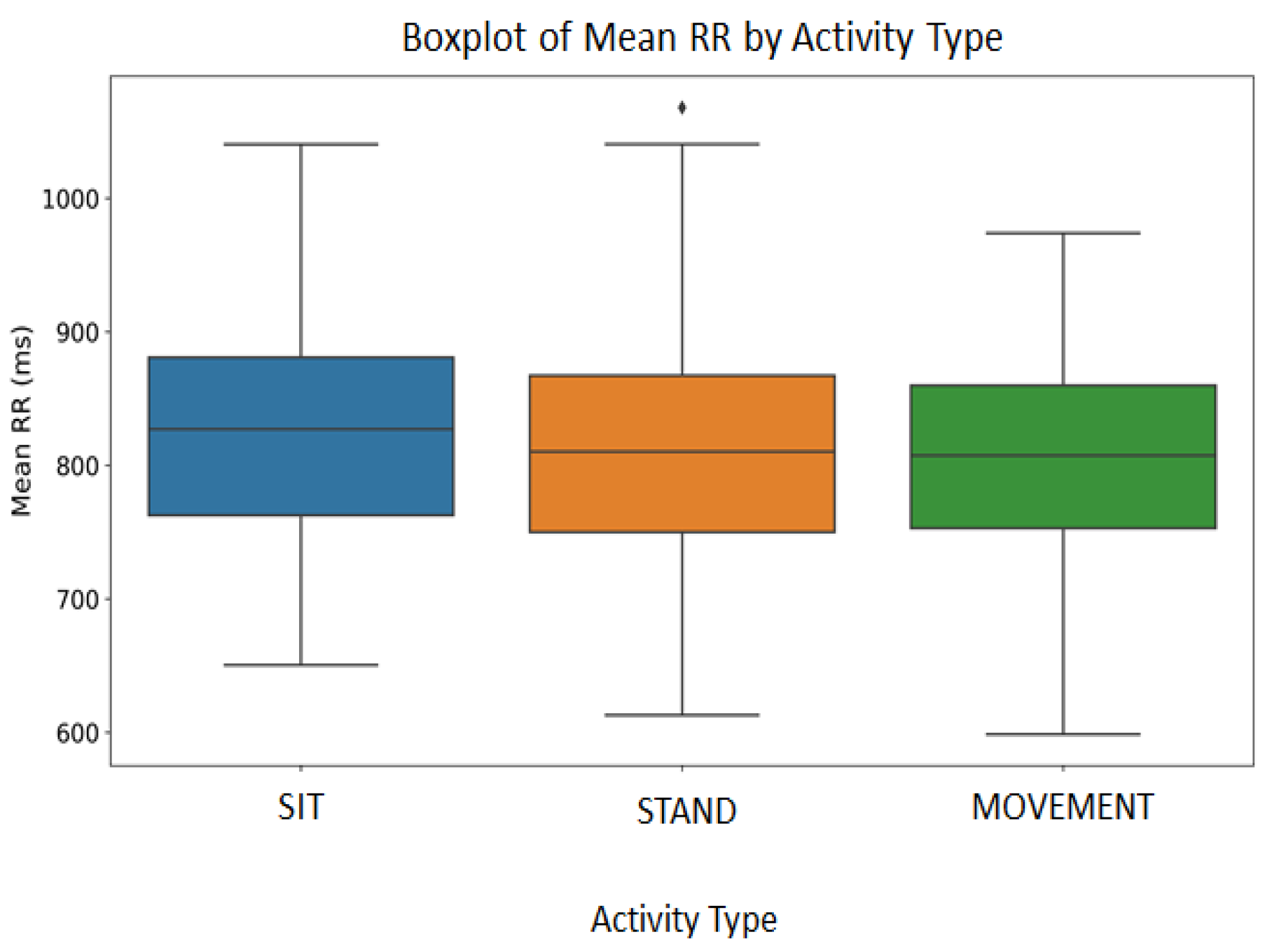
- Mean RR: We assumed that the IBI signals could be used as RR intervals. For each participant and each of the 14 BBS tasks, we calculated the mean of the IBI intervals.
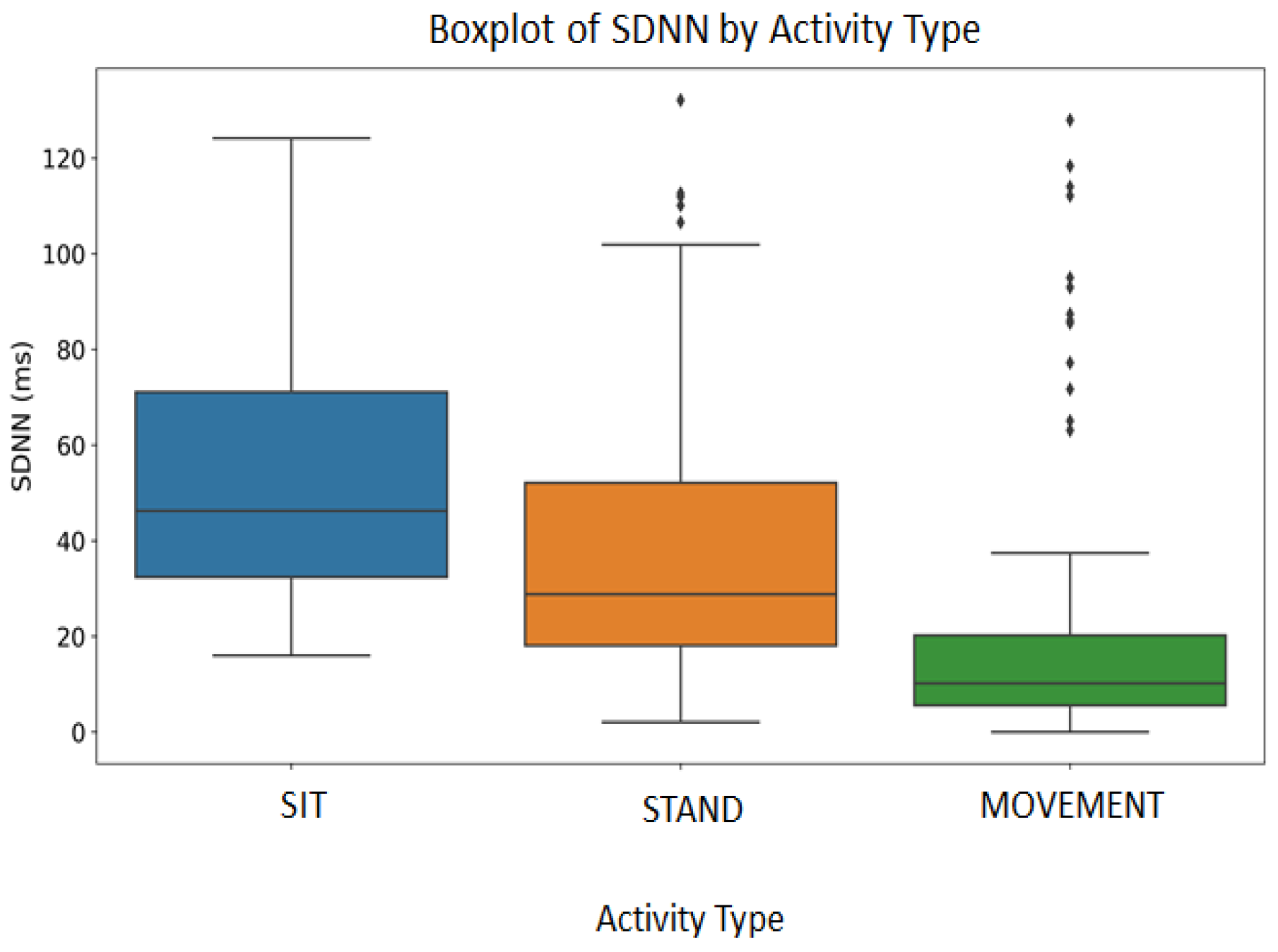
- SDNN: To evaluate the total HRV, we first extracted the successive changes between heartbeats that were considered normal, or NN intervals (normal-to-normal intervals), and then calculated their standard deviation. This metric captures the fluctuations in the HRV.
- RMSSD: The parasympathetic ANS activity could be represented by the root mean square of successive deviations between the NN intervals. This measure could identify the quick variations in the HRV.
- pNN50: We quantified the number of times that IBIs differed by more than 50 ms (NN50) and expressed this as a percentage of the total (pNN50). This measure evaluates the frequency of significant changes in the HRV.
2.4.3. Frequency Domain HRV
- The LF Power, or the spectral power in the low-frequency band (0.04–0.14 Hz): The LF Power is typically associated with both sympathetic and parasympathetic ANS activities. This parameter may reflect baroreceptor activity and indicate the human body’s response to various stressors and regulatory processes related to blood pressure control [32].
- The HF Power, or the spectral power in the high-frequency band (0.15–0.50 Hz): The HF Power is predominantly associated with parasympathetic activity, reflecting respiratory sinus arrhythmia [33]. Since this parameter is responsive to breathing, it can assess the vagal tone, which is crucial for relaxation and rapid stress recovery.
- The LF/HF ratio: The ratio between the LF Power and HF Power can provide information on the balance between the sympathetic and parasympathetic ANS activities. A higher LF/HF ratio indicates the dominance of sympathetic activity relative to parasympathetic activity, while a lower ratio suggests the opposite.
- The Total Power, or TP: This measure simply takes the sum of the spectral power within the range from 0 to 0.5 Hz.
2.4.4. HR Measurements
2.5. Physical Activity Categorization
- SIT: This category included activities characterized by a long time of sitting or resting in a sitting posture. In these time periods, we expected participants to exert minimal physical effort, but their mental or cognitive load remains uncertain.
- STAND: Unlike sitting or vigorous exercise, activities that require participants to stay standing still for an extended period could put their cardiovascular systems through a distinct kind of strain. In this category, the standing activities included standing with one leg, standing with their eyes closed and standing with two legs in tandem.
- MOVEMENT: We considered that physical movements may cause greater cardiovascular activity, which could cause noticeable alterations in the HR and possibly also in the HRV. These activities included but were not limited to changing posture from sitting to standing and vice versa, turning around to look behind them, and squatting or bending over to pick up an object from the floor.
2.6. Clustering Analysis
2.7. Binary Classification of BBS
2.7.1. Data Preparation
- is an example of the minority class;
- is one of the k nearest neighbors of ;
- is a random number in the interval .
2.7.2. Machine Learning Classifiers, Performance Metrics and Cross-Validation
3. Results
3.1. Poincaré Plots
- Elliptical or Torpedo-Shaped Plots: Data from many participants displayed plots with a prominent, elongated elliptical shape (Participants 1, 3, 4, 6, 10 and 12), typically oriented along a 45-degree line through the origin. Such shapes generally suggested a healthy balance between sympathetic and parasympathetic ANS activities. The width on the x-axis of the ellipse (SD1) was a short-term HRV measure, while the length (SD2) on the y-axis indicated a long-term HRV variability measure [35].
- Dispersed Patterns: Some plots showed more scattered yet elliptical distributions (Participants 5, 7, 8, 9, 13 and 14). These patterns may indicate an irregular HRV, often linked to heightened stress responses [36].
- Dense Clustering: Some plots featured tightly clustered patterns (Participants 2 and 11), with points densely packed near the identity line (). This pattern could suggest a reduced HRV, potentially signaling cardiac instability or early-stage cardiovascular issues. Research has associated tightly clustered Poincaré plots with high risks of cardiac events [37].
3.2. Exploratory Data Analysis
3.3. K-Means Clustering
3.3.1. Significant Features
3.3.2. Vizualisation and Performance of K-Means Clustering
3.3.3. Relationship Between Clustering Membership and Activity Type
3.4. BBS Classification
4. Discussion
4.1. HRV and HR Among Various Physical Activities
4.2. Clustering Analysis Based on HRV and HR
4.3. Balance Loss Prediction
4.4. Methodological Considerations
4.5. Limitations
5. Conclusions and Future Work
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2024, 403, 2133–2161. [Google Scholar] [CrossRef]
- Organisation Mondiale de la Santé. Chutes. Available online: https://www.who.int/fr/news-room/fact-sheets/detail/falls (accessed on 30 November 2024).
- Shumway-Cook, A.; Woollacott, M. Motor control: Translating research into clinical practice. In Osteoporosis International; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2006. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Speechley, M.; Ginter, S.F. Risk factors for falls among elderly persons living in the community. N. Engl. J. Med. 1988, 319, 1701–1707. [Google Scholar] [CrossRef]
- Thayer, J.F.; Lane, R.D. A model of neurovisceral integration in emotion regulation and dysregulation. J. Affect. Disord. 2000, 61, 201–216. [Google Scholar] [CrossRef]
- Vieira, E.R.; Palmer, R.C.; Chaves, P.H. Prevention of falls in older people living in the community. BMJ 2016, 353, i1419. [Google Scholar] [CrossRef] [PubMed]
- Ye, P.; Liu, Y.; Zhang, J.; Peng, K.; Pan, X.; Xiao, S.; Armstrong, E.; Er, Y.; Duan, L.; Ivers, R.; et al. Falls prevention interventions for community-dwelling older people living in mainland China: A narrative systematic review. BMC Health Serv. Res. 2020, 20, 808. [Google Scholar] [CrossRef]
- Shaffer, F.; McCraty, R.; Zerr, C.L. A healthy heart is not a metronome: An integrative review of the heart’s anatomy and heart rate variability. Front. Psychol. 2014, 5, 1040. [Google Scholar] [CrossRef] [PubMed]
- Orsila, R.; Virtanen, M.; Luukkaala, T.; Tarvainen, M.; Karjalainen, P.; Viik, J.; Savinainen, M.; Nygård, C.-H. Perceived mental stress and reactions in heart rate variability—A pilot study among employees of an electronics company. Int. J. Occup. Saf. Ergon. (JOSE) 2008, 14, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Seo, Y.; Salahuddin, L. Decreased long term variations of heart rate variability in subjects with higher self-reporting stress scores. In Proceedings of the 2008 Second International Conference on Pervasive Computing Technologies for Healthcare, Tampere, Finland, 30 January–1 February 2008; pp. 289–292. [Google Scholar] [CrossRef]
- Castaldo, R.; Melillo, P.; Bracale, U.; Caserta, M.; Triassi, M.; Pecchia, L. Acute mental stress assessment via short-term HRV analysis in healthy adults: A systematic review with meta-analysis. Biomed. Signal Process. Control 2015, 18, 370–377. [Google Scholar] [CrossRef]
- Wang, L.; Hao, J.; Zhou, T.H.; Song, F. ECG stress detection model based on heart rate variability feature extraction. In Proceedings of the HP3C ’23: 7th International Conference on High Performance Compilation, Computing and Communications, Nanjing, China, 19–21 May 2023; pp. 184–188. [Google Scholar] [CrossRef]
- Salahuddin, L.; Kim, D. Detection of acute stress by heart rate variability using a prototype mobile ECG sensor. In Proceedings of the 2006 International Conference on Hybrid Information Technology, Cheju Island, Republic of Korea, 9–11 November 2006; pp. 453–459. [Google Scholar] [CrossRef]
- Dalmeida, K.M.; Masala, G.L. HRV Features as Viable Physiological Markers for Stress Detection Using Wearable Devices. Sensors 2021, 21, 2873. [Google Scholar] [CrossRef]
- Murty, P.S.R.C.; Anuradha, C.; Naidu, P.A.; Balaswamy, C.; Nagalingam, R.; Jagatheesaperumal, S.K.; Ponnusamy, M. An intelligent wearable embedded architecture for stress detection and psychological behavior monitoring using heart rate variability. J. Intell. Fuzzy Syst. 2023, 45, 8203–8216. [Google Scholar] [CrossRef]
- Schaffarczyk, M.; Rogers, B.; Reer, R.; Gronwald, T. Validity of the Polar H10 Sensor for Heart Rate Variability Analysis during Resting State and Incremental Exercise in Recreational Men and Women. Sensors 2022, 22, 6536. [Google Scholar] [CrossRef]
- Hernández-Vicente, A.; Hernando, D.; Marín-Puyalto, J.; Vicente-Rodríguez, G.; Garatachea, N.; Pueyo, E.; Bailón, R. Validity of the Polar H7 Heart Rate Sensor for Heart Rate Variability Analysis during Exercise in Different Age, Body Composition, and Fitness Level Groups. Sensors 2021, 21, 902. [Google Scholar] [CrossRef]
- Attar, E.T.; Balasubramanian, V.; Subasi, E.; Kaya, M. Stress Analysis Based on Simultaneous Heart Rate Variability and EEG Monitoring. IEEE J. Transl. Eng. Health Med. 2021, 9, 2700607. [Google Scholar] [CrossRef]
- Jarchi, D.; Andreu-Perez, J.; Kiani, M.; Vysata, O.; Kuchynka, J.; Prochazka, A.; Sanei, S. Recognition of Patient Groups with Sleep-Related Disorders Using Bio-signal Processing and Deep Learning. Sensors 2020, 20, 2594. [Google Scholar] [CrossRef] [PubMed]
- Pourmohammadi, S.; Maleki, A. Continuous mental stress level assessment using electrocardiogram and electromyogram signals. Biomed. Signal Process. Control 2021, 68, 102694. [Google Scholar] [CrossRef]
- Muñoz, J.E.; Gouveia, E.R.; Cameirão, M.S.; Bermúdez i Badia, S. PhysioLab—A multivariate physiological computing toolbox for ECG, EMG, and EDA signals: A case study of cardiorespiratory fitness assessment in the elderly population. Multimed. Tools Appl. 2018, 77, 11521–11546. [Google Scholar] [CrossRef]
- Thielmann, B.; Pohl, R.; Böckelmann, I. Heart rate variability as a strain indicator for psychological stress for emergency physicians during work and alert intervention: A systematic review. J. Occup. Med. Toxicol. 2021, 16, 24. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, S.; Dias, D.; Paiva, J.S.; Cunha, J.P.S. Psychophysiological Stress Assessment Among On-Duty Firefighters. In Proceedings of the 2018 Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Honolulu, HI, USA, 17–21 July 2018; pp. 4335–4338. [Google Scholar] [CrossRef]
- Prajod, P.; André, E. On the generalizability of ECG-based stress detection models. In Proceedings of the 2022 21st IEEE International Conference on Machine Learning and Applications (ICMLA), Nassau, Bahamas, 12–15 December 2022; pp. 549–554. [Google Scholar] [CrossRef]
- Bustos, D.; Cardoso, F.; Rios, M.; Vaz, M.; Guedes, J.; Costa, J.T.; Baptista, J.S.; Fernandes, R.J. Machine Learning Approach to Model Physical Fatigue during Incremental Exercise among Firefighters. Sensors 2022, 23, 194. [Google Scholar] [CrossRef]
- Tervonen, J.; Puttonen, S.; Sillanpää, M.J.; Hopsu, L.; Homorodi, Z.; Keränen, J.; Pajukanta, J.; Tolonen, A.; Lämsä, A.; Mäntyjärvi, J. Personalized mental stress detection with self-organizing map: From laboratory to the field. Comput. Biol. Med. 2020, 124, 103935. [Google Scholar] [CrossRef]
- Berg, K.O.; Wood-Dauphinee, S.L.; Williams, J.I.; Maki, B. Measuring balance in the elderly: Validation of an instrument. Can. J. Public Health 1992, 83 (Suppl. S2), S7–S11. [Google Scholar] [PubMed]
- Steffen, T.M.; Hacker, T.A.; Mollinger, L. Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys. Ther. 2002, 82, 128–137. [Google Scholar] [CrossRef]
- Aygun, A.; Ghasemzadeh, H.; Jafari, R. Robust Interbeat Interval and Heart Rate Variability Estimation Method From Various Morphological Features Using Wearable Sensors. IEEE J. Biomed. Health Inform. 2020, 24, 2238–2250. [Google Scholar] [CrossRef] [PubMed]
- Saleem, S.; Khandoker, A.H.; Alkhodari, M.; Hadjileontiadis, L.J.; Jelinek, H.F. A two-step pre-processing tool to remove Gaussian and ectopic noise for heart rate variability analysis. IEEE Access 2022, 10, 54081–54092. [Google Scholar] [CrossRef]
- Brennan, M.; Palaniswami, M.; Kamen, P. Poincaré plot interpretation using a physiological model of HRV based on a network of oscillators. Am. J. Physiol. Heart Circ. Physiol. 2002, 283, H1873–H1886. [Google Scholar] [CrossRef]
- Bernardi, L.; Leuzzi, S.; Radaelli, A.; Passino, C.; Johnston, J.A.; Sleight, P. Low-frequency spontaneous fluctuations of R-R interval and blood pressure in conscious humans: A baroreceptor or central phenomenon? Clin. Sci. 1994, 87, 649–654. [Google Scholar] [CrossRef]
- Yasuma, F.; Hayano, J. Respiratory sinus arrhythmia: Why does the heartbeat synchronize with respiratory rhythm? Chest 2004, 125, 683–690. [Google Scholar] [CrossRef]
- Pedregosa, F.; Varoquaux, G.; Gramfort, A.; Michel, V.; Thirion, B.; Grisel, O.; Blondel, M.; Prettenhofer, P.; Weiss, R.; Dubourg, V.; et al. Scikit-learn: Machine learning in Python. J. Mach. Learn. Res. 2011, 12, 2825–2830. [Google Scholar]
- Malik, M.; Camm, A.J.; Bigger, J.T.; Kleiger, R.E.; Malliani, A.; Moss, A.J.; Schwartz, P.J. Heart rate variability: Standards of measurement, physiological interpretation, and clinical use. Eur. Heart J. 1996, 17, 354–381. [Google Scholar] [CrossRef]
- Satti, R.; Abid, N.U.; Bottaro, M.; De Rui, M.; Garrido, M.; Raoufy, M.R.; Montagnese, S.; Manj, A.R. The Application of the Extended Poincaré Plot in the Analysis of Physiological Variabilities. Front. Physiol. 2019, 10, 116. [Google Scholar] [CrossRef]
- Stein, M.B.; Roy-Byrne, P.P.; Craske, M.G.; Bystritsky, A.; Sullivan, G.; Pyne, J.M.; Katon, W.; Sherbourne, C. Functional impact and health utility of anxiety disorders in primary care outpatients. Med. Care 2005, 43, 1164–1170. [Google Scholar] [CrossRef] [PubMed]
- Nakao, M. Heart Rate Variability and Perceived Stress as Measurements of Relaxation Response. J. Clin. Med. 2019, 8, 1704. [Google Scholar] [CrossRef]
- Taelman, J.; Vandeput, S.; Spaepen, A.; Huffel, S.V. Influence of Mental Stress on Heart Rate and Heart Rate Variability. In Proceedings of the World Congress on Medical Physics and Biomedical Engineering, Munich, Germany, 7–12 September 2009; pp. 1360–1363. [Google Scholar] [CrossRef]
- Berntson, G.G.; Cacioppo, J.T.; Binkley, P.F.; Uchino, B.N.; Quigley, K.S.; Fieldstone, A. Autonomic cardiac control. III. Psychological stress and cardiac response in autonomic space as revealed by pharmacological blockades. Psychophysiology 1994, 31, 599–608. [Google Scholar] [CrossRef]
- Yıldız, A.Y.; Kalayci, A. Gradient boosting decision trees on medical diagnosis over tabular data. arXiv 2024, arXiv:2410.03705. [Google Scholar] [CrossRef]
- Lynam, A.L.; Dennis, J.M.; Owen, K.R.; Oram, R.A.; Jones, A.G.; Shields, B.M.; Ferrat, L.A. Logistic regression has similar performance to optimised machine learning algorithms in a clinical setting: Application to the discrimination between type 1 and type 2 diabetes in young adults. Diagn. Progn. Res. 2020, 4, 6. [Google Scholar] [CrossRef] [PubMed]
- Bentéjac, C.; Csörgő, A.; Martínez-Muñoz, G. A comparative analysis of gradient boosting algorithms. Artif. Intell. Rev. 2021, 54, 1937–1967. [Google Scholar] [CrossRef]
- Gungor, M.A.; Karagoz, I. The effects of the median filter with different window sizes for ultrasound image. In Proceedings of the 2016 2nd IEEE International Conference on Computer and Communications (ICCC), Chengdu, China, 14–17 October 2016; pp. 549–552. [Google Scholar] [CrossRef]
- Task Force of the European Society of Cardiology; the North American Society of Pacing and Electrophysiology. Heart rate variability: Standards of measurement, physiological interpretation, and clinical use. Circulation 1996, 93, 1043–1065. [Google Scholar] [CrossRef]
- Shaffer, F.; Ginsberg, J.P. An Overview of Heart Rate Variability Metrics and Norms. Front. Public Health 2017, 5, 258. [Google Scholar] [CrossRef] [PubMed]
- Gañán-Calvo, A.; Fajardo-López, J. Universal structures of normal and pathological heart rate variability. Sci. Rep. 2016, 6, 21749. [Google Scholar] [CrossRef]
- Gañán-Calvo, A.M.; Hnatkova, K.; Romero-Calvo, Á.; Fajardo-López, J.; Malik, M. Risk stratifiers for arrhythmic and non-arrhythmic mortality after acute myocardial infarction. Sci. Rep. 2018, 8, 9897. [Google Scholar] [CrossRef]
- Gherbi, Y.; Thamsuwan, O. Berg balance test for predicting a fall risk in older adults living at home: A preliminary study on the effect of pre-existing health conditions on postural balance. In Proceedings of the 22nd Triennial Congress of the International Ergonomics Association (IEA), Jeju, Republic of Korea, 25–29 August 2024. [Google Scholar]




| Model | Hyperparameter | Values Tested |
|---|---|---|
| Logistic Regression | C | [0.01, 0.1, 1, 10, 100, 1000] |
| solver | [‘liblinear’, ‘saga’, ‘lbfgs’] | |
| Random Forest | n_estimators | [50, 100, 200, 300, 500] |
| max_depth | [None, 10, 20, 30, 40] | |
| min_samples_split | [2, 5, 10] | |
| min_samples_leaf | [1, 2, 4] | |
| SVM | C | [0.01, 0.1, 1, 10, 100] |
| kernel | [‘linear’, ‘rbf’, ‘poly’, ‘sigmoid’] | |
| gamma | [‘scale’, ‘auto’] | |
| Gradient Boosting | n_estimators | [50, 100, 200, 300] |
| learning_rate | [0.01, 0.05, 0.1, 0.2] | |
| max_depth | [3, 4, 5, 6] | |
| min_samples_split | [2, 5, 10] | |
| min_samples_leaf | [1, 2, 4] | |
| XGBoost | n_estimators | [50, 100, 200, 300] |
| learning_rate | [0.01, 0.05, 0.1, 0.2] | |
| max_depth | [3, 4, 5, 6] | |
| colsample_bytree | [0.3, 0.7] | |
| LightGBM | n_estimators | [50, 100, 200, 300] |
| learning_rate | [0.01, 0.05, 0.1, 0.2] | |
| num_leaves | [31, 40, 50] | |
| boosting_type | [‘gbdt’, ‘dart’] | |
| CatBoost | iterations | [50, 100, 200, 300] |
| learning_rate | [0.01, 0.05, 0.1, 0.2] | |
| depth | [3, 4, 5, 6] | |
| AdaBoost | n_estimators | [50, 100, 200, 300] |
| learning_rate | [0.01, 0.05, 0.1, 0.2] | |
| Neural Network | hidden_layer_sizes | [(50, 50), (100, 50)] |
| activation | [‘tanh’, ‘relu’] | |
| solver | [‘adam’, ‘sgd’] | |
| alpha | [0.0001, 0.001, 0.01] |
| Metric | Cluster 0 (N = 163) | Cluster 1 (N = 59) | Cluster 2 (N = 2) |
|---|---|---|---|
| Mean IBI (ms) | 845.60 (64.42) | 684.93 (45.15) | 837.16 (2.61) |
| SDNN (ms) | 39.00 (33.77) | 16.52 (14.45) | 120.85 (4.73) |
| RMSSD (ms) | 33.61 (49.17) | 8.30 (5.80) | 171.13 (12.89) |
| NN50 (count) | 4.53 (14.44) | 0.90 (3.45) | 462.00 (2.83) |
| pNN50 (%) | 13.53 (27.66) | 0.46 (1.97) | 77.13 (0.47) |
| Mean HR (bpm) | 71.63 (5.39) | 88.05 (5.73) | 73.31 (0.43) |
| STD HR (bpm) | 3.60 (3.39) | 2.10 (1.84) | 11.70 (1.12) |
| Min HR (bpm) | 66.04 (5.35) | 83.80 (7.13) | 50.60 (0.94) |
| Max HR (bpm) | 78.74 (11.43) | 91.70 (7.91) | 134.00 (17.68) |
| LF Power (ms2) | 2.15 × 105 (4.60 × 105) | 1.74 × 105 (6.40 × 105) | 1.07 × 107 (8.07 × 104) |
| HF Power (ms2) | 1.30 × 105 (4.60 × 105) | 2.76 × 104 (1.14 × 105) | 2.42 × 107 (7.87 × 105) |
| LF/HF Ratio | 6.20 (7.19) | 8.76 (20.13) | 0.44 (0.02) |
| TP (ms2) | 2.23 × 1011 (9.40 × 1011) | 1.05 × 1011 (3.85 × 1011) | 2.92 × 1012 (3.90 × 1010) |
| SD1 (ms) | 24.40 (37.32) | 5.40 (4.10) | 121.11 (9.12) |
| SD2 (ms) | 45.80 (35.70) | 22.52 (20.25) | 120.51 (0.31) |
| Cluster | SIT | STAND | MOVEMENT |
|---|---|---|---|
| “0” | 20 | 75 | 68 |
| “1” | 6 | 23 | 30 |
| “2” | 2 | 0 | 0 |
| Model | Precision | Recall | F1 Score | Overall Accuracy |
|---|---|---|---|---|
| Logistic Regression | 88.89% | 71.43% | 55.56% | 72.41% |
| Random Forest | 83.33% | 42.86% | 50.00% | 79.31% |
| Support Vector Machine (SVM) | 84.21% | 57.14% | 47.06% | 68.97% |
| Gradient Boosting | 95.45% | 85.71% | 85.71% | 93.10% |
| XGBoost | 90.48% | 71.43% | 66.67% | 82.76% |
| LightGBM | 83.33% | 42.86% | 50.00% | 79.31% |
| CatBoost | 86.96% | 57.14% | 61.54% | 82.76% |
| AdaBoost | 91.30% | 71.43% | 76.92% | 89.66% |
| Neural Network | 76.19% | 28.57% | 26.67% | 62.07% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Messaoud, I.B.; Thamsuwan, O. Heart Rate Variability-Based Stress Detection and Fall Risk Monitoring During Daily Activities: A Machine Learning Approach. Computers 2025, 14, 45. https://doi.org/10.3390/computers14020045
Messaoud IB, Thamsuwan O. Heart Rate Variability-Based Stress Detection and Fall Risk Monitoring During Daily Activities: A Machine Learning Approach. Computers. 2025; 14(2):45. https://doi.org/10.3390/computers14020045
Chicago/Turabian StyleMessaoud, Ines Belhaj, and Ornwipa Thamsuwan. 2025. "Heart Rate Variability-Based Stress Detection and Fall Risk Monitoring During Daily Activities: A Machine Learning Approach" Computers 14, no. 2: 45. https://doi.org/10.3390/computers14020045
APA StyleMessaoud, I. B., & Thamsuwan, O. (2025). Heart Rate Variability-Based Stress Detection and Fall Risk Monitoring During Daily Activities: A Machine Learning Approach. Computers, 14(2), 45. https://doi.org/10.3390/computers14020045







