Assessing the Impact of Prolonged Sitting and Poor Posture on Lower Back Pain: A Photogrammetric and Machine Learning Approach
Abstract
1. Introduction
2. Materials and Methods
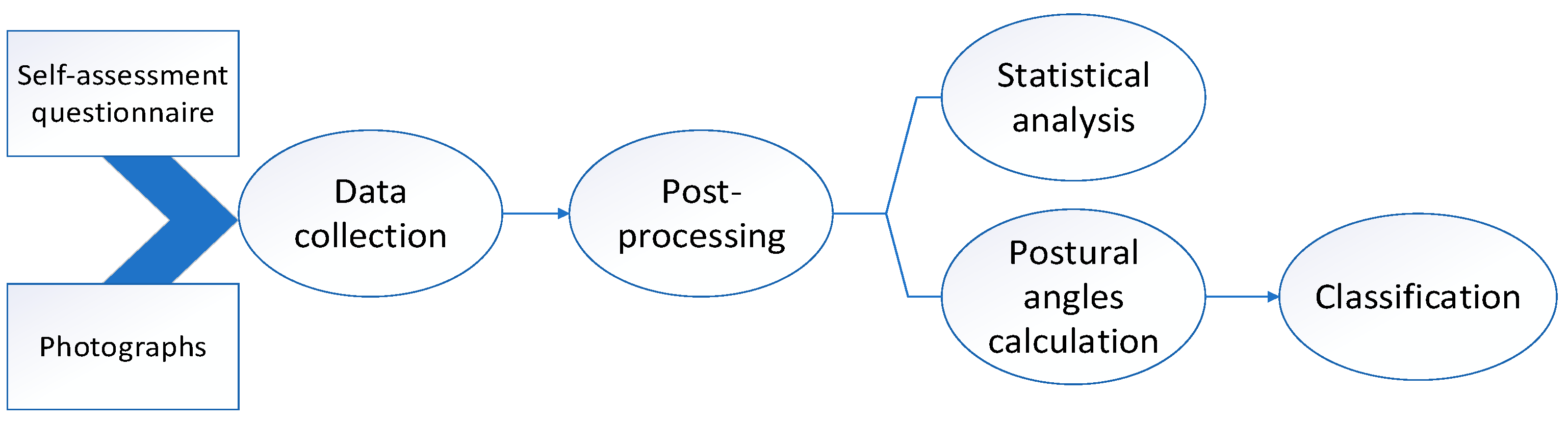
2.1. Experimental Procedure
- (1)
- Volunteers filled out a self-assessment questionnaire regarding their work habits, ergonomic practices, and instances of discomfort or pain.
- (2)
- Left lateral view photographs of the body were captured while volunteers were seated in their natural position in front of a computer, occupied with a game-like standard cognitive task.
- (3)
- A physiotherapist corrected the seating body position and additional left lateral view photographs of the body were captured.
- (4)
- The images of each of the 100 participants were post-processed and annotated by a physiotherapist with over 15 years of professional experience.
- (5)
- Based on the placed markers, postural angles related to LBP were calculated.
- (6)
- Statistical analysis of the self-assessment questionnaire responses was performed.
- (7)
- The angle values, along with tags for incorrect were collected in a LBPA dataset and used for machine learning purposes, aiming to construct a model for recognizing improper sitting postures related to the occurrence of low back pain risk.
- -
- Angle 2—Lumbar lordosis (LL), defined as the angle between tangential lines to the lower plateau of L5 and the top of L1.
- -
- Angle 6—Hip joint angle measurement—sitting position. This is an angle obtained by the intersection of two lines in the region of the greater trochanter of the femur. One line is vertical and parallel to the trunk, and the other line is parallel to the long axis of the femur in line with the lateral femoral condyle. The angular measurement method employed in this study was adapted from our previous research
- -
- Angle 7—Bent knee angle when sitting. This is an angle obtained by the intersection of two lines in the region of the lateral epicondyle of the femur. One line is horizontal and parallel to the femur to the greater trochanter, and the other line is parallel to the fibula to the lateral malleolus.

2.2. Participants
2.3. Dataset
- Pictures with markers—Pictures in .jpg with markers ready to use (ten markers corresponding to body map). File name format is “ID.X”, where ID corresponds to Participant ID numbers and “X” denotes the natural sitting posture (5) and the corrected posture (6). Photo IDs correspond to Questionnaire IDs;
- Postural angle calculations—Angle.csv file containing in each column postural angle calculations (angle 2, angle 6, angle 7)
- a file with questionnaire responses
2.4. Data Processing and Statistics
3. Results
3.1. Questionnaire-Based Analysis
3.2. Photogrametric Analysis
3.3. Detection of Poor Body Posture
3.3.1. Natural Postures-Based Scenario
3.3.2. Corrected Postures-Based Scenario
4. Discussion
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Soares, C.; Shimano, S.G.N.; Marcacine, P.R.; Fernandes, L.F.R.M.; de Castro, L.L.P.T.; de Walsh, I.A.P. Ergonomic interventions for work in a sitting position: An integrative review. Rev. Bras. Med. Trab. 2023, 21, e2023770. [Google Scholar] [CrossRef]
- European Agency for Safety and Health at Work. Musculoskeletal Disorders. Available online: https://osha.europa.eu/en/themes/musculoskeletal-disorders (accessed on 1 March 2024).
- Jacquier-Bret, J.; Gorce, P. Effect of day time on smartphone use posture and related musculoskeletal disorders risk: A survey among university students. BMC Musculoskelet. Disord. 2023, 24, 725. [Google Scholar] [CrossRef] [PubMed]
- Sharan, D. Musculoskeletal disorders in 115 students due to overuse of electronic devices: Risk factors and clinic. In Proceedings of the 20th Congress of the International Ergonomics Association (IEA 2018), Florence, Italy, 26–30 August 2018. [Google Scholar]
- Montuori, P.; Cennamo, L.M.; Sorrentino, M.; Pennino, F.; Ferrante, B.; Nardo, A.; Mazzei, G.; Grasso, S.; Salomone, M.; Trama, U.; et al. Assessment on Practicing Correct Body Posture and Determinant Analyses in a Large Population of a Metropolitan Area. Behav. Sci. 2023, 13, 144. [Google Scholar] [CrossRef] [PubMed]
- Vachinska, S.; Markova, V.; Ganchev, T. A Risk Assessment Study on Musculoskeletal Disorders in Computer Users Based on A Modified Nordic Musculoskeletal Questionnaire. In The International Symposium on Bioinformatics and Biomedicine; Lecture Notes in Networks and Systems; Springer International Publishing: Cham, Switzerland, 2022; Volume 374. [Google Scholar] [CrossRef]
- Shin, J.-H.; Wang, S.; Yao, Q.; Wood, K.B.; Li, G. Investigation of coupled bending of the lumbar spine during dynamic axial rotation of the body. Eur. Spine J. 2013, 22, 2671–2677. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bernstein, I.A.; Malik, Q.; Carville, S.; Ward, S. Low back pain and sciatica: Summary of NICE guidance. BMJ 2017, 356, i6748, Erratum in BMJ 2021, 374, n1627. [Google Scholar] [CrossRef] [PubMed]
- Tousignant-Laflamme, Y.; Martel, M.O.; Joshi, A.B.; Cook, C.E. Rehabilitation management of low back pain—it’s time to pull it all together! J. Pain Res. 2017, 10, 2373–2385. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- O’Crawford, J.; Graveling, R.; Davis, A.; Giagloglou, E.; Fernandes, M.; Markowska, A.; Jones, M.; Fries-Tersch, E. European Risk Observatory Report, Work-Related Musculoskeletal Disorders: From Research to Practice. What Can Be Learnt? EU-OSHA: Bilbao, Spain, 2020. [Google Scholar] [CrossRef]
- Fatemi, R.; Javid, M.; Najafabadi, E.M. Effects of William training on lumbosacral muscles function, lumbar curve, and pain. Back Musculoskelet. Rehabil. 2015, 28, 591–597. [Google Scholar] [CrossRef] [PubMed]
- Machado, G.C.; Maher, G.; Ferreira, P.; Harris, I.A.; Deyo, R.; McKay, D.; Li, Q.; Ferreira, M. Trends, Complications, and Costs for Hospital Admission and Surgery for Lumbar Spinal Stenosis. Spine 2017, 42, 1737–1743. [Google Scholar] [CrossRef]
- Lee, D.-E.; Seo, S.-M.; Woo, H.-S.; Won, S.-Y. Analysis of body imbalance in various writing sitting postures using sitting pressure measurement. J. Phys. Ther. Sci. 2018, 30, 343–346. [Google Scholar] [CrossRef][Green Version]
- Du, S.-H.; Zhang, Y.-H.; Yang, Q.-H.; Wang, Y.-C.; Fang, Y.; Wang, X.-Q. Spinal posture assessment and low back pain. EFORT Open Rev. 2023, 8, 708–718. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Korakakis, V.; O’Sullivan, K.; O’Sullivan, P.B.; Evagelinou, V.; Sotiralis, Y.; Sideris, A.; Sakellariou, K.; Karanasios, S.; Giakas, G. Physiotherapist perceptions of optimal sitting and standing posture. Musculoskelet. Sci. Pract. 2019, 39, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Bayar, B.; Güp, A.; Oruk, D.; Dongaz, Ö.; Doğu, E.; Bayar, K. Development of the postural habits and awareness scale: A reliability and validity study. Int. J. Occup. Saf. Ergon. 2022, 29, 815–820. [Google Scholar] [CrossRef] [PubMed]
- Schwertner, D.S.; da Silva Oliveira, R.A.N.; Swarowsky, A.; Felden, É.P.G.; Beltrame, T.S.; da Luz Koerich, M.H.A. Young people’s low back pain and awareness of postural habits: A cross-sectional study. J. Back Musculoskelet. Rehabil. 2022, 35, 983–992. [Google Scholar] [CrossRef] [PubMed]
- Jia, N.; Li, T.; Hu, S.; Zhu, X.; Sun, K.; Yi, L.; Zhang, Q.; Luo, G.; Li, Y.; Zhang, X.; et al. Prevalence and its risk factors for low back pain among operation and maintenance personnel in wind farms. BMC Musculoskelet. Disord. 2016, 17, 314. [Google Scholar] [CrossRef] [PubMed]
- Tsai, M.-C.; Chu, E.T.-H.; Lee, C.-R. An Automated Sitting Posture Recognition System Utilizing Pressure Sensors. Sensors 2023, 23, 5894. [Google Scholar] [CrossRef]
- Furlanetto, T.S.; Sedrez, J.A.; Candotti, C.T.; Loss, J.F. Photogrammetry as a tool for the postural evaluation of the spine: A systematic review. World J. Orthop. 2016, 7, 136–148. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kandasamy, G.; Bettany-Saltikov, J.; van Schaik, P. Posture and Back Shape Measurement Tools: A Narrative Literature Review. In Spinal Deformities in Adolescents, Adults and Older Adults; IntechOpen: New York, NY, USA, 2021. [Google Scholar] [CrossRef]
- Chan, V.C.H.; Ross, G.B.; Clouthier, A.L.; Fischer, S.L.; Graham, R.B. The role of machine learning in the primary prevention of work-related musculoskeletal disorders: A scoping review. Appl. Ergon. 2022, 98, 103574. [Google Scholar] [CrossRef]
- Laidi, R.; Khelladi, L.; Kessaissia, M.; Ouandjli, L. Bad Sitting Posture Detection and Alerting System using EMG Sensors and Machine Learning. In Proceedings of the 2023 International Conference on Artificial Intelligence in Information and Communication (ICAIIC), Bali, Indonesia, 20–23 February 2023; pp. 324–329. [Google Scholar] [CrossRef]
- Jeong, H.; Park, W. Developing and Evaluating a Mixed Sensor Smart Chair System for Real-Time Posture Classification: Combining Pressure and Distance Sensors. IEEE J. Biomed. Health Inform. 2021, 25, 1805–1813. [Google Scholar] [CrossRef]
- do Rosário, J.L.P. Photographic analysis of human posture: A literature review. J. Bodyw. Mov. Ther. 2014, 18, 56–61. [Google Scholar] [CrossRef]
- Pereira, R.C.M.; Vigário, P.S.; Mainenti, M.R.M.; Silva, D.T.R.; Lima, T.R.L.; Lemos, T. Computerized photogrammetric assessment of postural alignment in visually impaired athletes. J. Bodyw. Mov. Ther. 2019, 23, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Markova, V.; Ganchev, T.; Filkova, S.; Markov, M. MMD-MSD: A Multimodal Multisensory Dataset in Support of Research and Technology Development for Musculoskeletal Disorders. Algorithms 2024, 17, 187. [Google Scholar] [CrossRef]
- Bontrup, C.; Taylor, W.R.; Fliesser, M.; Visscher, P.; Green, T.; Wippert, P.M.; Zemp, R. Low back pain and its relationship with sitting behaviour among sedentary office workers. Appl. Ergon. 2019, 81, 102894. [Google Scholar] [CrossRef] [PubMed]
- Keskin, Y.; Ürkmez, B.; Öztürk, F.; Kepekçi, M.; Aydın, T. Correlation between Sitting Duration and Position and Lumbar Pain among Office Workers. Haydarpasa Numune Med. J. 2021, 61, 1–6. [Google Scholar] [CrossRef]
- Kett, A.R.; Sichting, F.; Milani, T.L. The Effect of Sitting Posture and Postural Activity on Low Back Muscle Stiffness. Biomechanics 2021, 1, 214–224. [Google Scholar] [CrossRef]
- Slater, D.; Korakakis, V.; O’Sullivan, P.; Nolan, D.; O’Sullivan, K. “Sit Up Straight”: Time to Re-evaluate. J. Orthop. Sports Phys. Ther. 2019, 49, 562–564. [Google Scholar] [CrossRef] [PubMed]
- Swain, C.T.V.; Pan, F.; Owen, P.J.; Schmidt, H.; Belavy, D.L. No consensus on causality of spine postures or physical exposure and low back pain: A systematic review of systematic reviews. J. Biomech. 2020, 102, 109312. [Google Scholar] [CrossRef]
- O’Sullivan, K.; McCarthy, R.; White, A.; O’Sullivan, L.; Dankaerts, W. Can we reduce the effort of maintaining a neutral sitting posture? A pilot study. Man. Ther. 2012, 17, 566–571. [Google Scholar] [CrossRef]
- Schmidt, H.; Bashkuev, M.; Weerts, J.; Graichen, F.; Altenscheidt, J.; Maier, C.H.; Reitmaier, S. How do we stand? Variations during repeated standing phases of asymptomatic subjects and low back pain patients. J. Biomech. 2018, 70, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Gosain, L.; Ahmad, I.; Rizvi, M.R.; Sharma, A.; Saxena, S. Prevalence of musculoskeletal pain among computer users working from home during the COVID-19 pandemic: A cross-sectional survey. Bull. Fac. Phys. Ther. 2022, 27, 51. [Google Scholar] [CrossRef] [PubMed Central]
- Kok, J.; Vroonhof, P.; Snijders, J.; Roullis, G.; Clarke, M.; Peereboom, K.; van Dorst, P.; Isusi, I. Work-Related Musculoskeletal Disorders: Prevalence, Costs and Demographics in the EU-European Risk Observatory Report; European Agency for Safety and Health at Work, Publications Office of the European Union: Luxembourg, 2019. [Google Scholar]




| Degree of Pain/Discomfort | Mild Pain | Moderate Pain | Severe Pain | Very Severe | Worst Pain Possible |
|---|---|---|---|---|---|
| Back pain | 12 | 18 | 20 | 4 | 2 |
| Low back pain | 9 | 16 | 21 | 7 | 1 |
| Pain in the buttock | 10 | 11 | 12 | 2 | 2 |
| Total people with pain or discomfort (%) | 31% | 45% | 53% | 13% | 5% |
| Classifier Type | Accuracy [%], st.dev. [%] | Recall [%], st.dev. [%] | Precision [%], st.dev. [%] | F-Measure [%], st.dev. [%] |
|---|---|---|---|---|
| Naïve Bayes | 75.3% ± 11.2% | 95.0% ± 11.2% | 73.3% ± 19.0% | 80.7% ± 9.0% |
| Generalized Linear Model | 57.3% ± 18.2% | 95.0% ± 11.2% | 55.3% ± 18.3% | 68.2% ± 14.6% |
| Logistic Regression | 60.7% ± 13.6% | 90.0% ± 13.7% | 60.7% ± 13.6% | 71.5% ± 10.8% |
| Fast Large Margin | 60.7% ± 13.6% | 90.0% ± 13.7% | 60.7% ± 13.6% | 71.5% ± 10.8% |
| Deep Learning | 63.3% ± 22.9% | 95.0% ± 11.2% | 63.3% ± 22.9% | 74.1% ± 16.6% |
| Decision Tree | 59.3% ± 18.9% | 100.0% ± 0.0% | 59.3% ± 18.9% | 73.0% ± 15.2% |
| Random Forest | 61.3% ± 16.8% | 95.0% ± 11.2% | 61.0% ± 20.1% | 72.0% ± 14.8% |
| Gradient Boosted Trees | 59.3% ± 25.2% | 95.0% ± 11.2% | 61.3% ± 24.7% | 72.2% ± 18.2% |
| SVM | 64.7% ± 19.5% | 100.0% ± 0.0% | 62.0% ± 21.0% | 74.8% ± 18.6% |
| Classifier Type | Accuracy [%], st.dev. [%] | Recall [%], st.dev. [%] | Precision [%], st.dev. [%] | F-Measure [%], st.dev. [%] |
|---|---|---|---|---|
| Naïve Bayes | 73.3% ± 7.2% | 46.7% ± 13.9% | 100.0% ± 0.0% | 62.7% ± 12.8% |
| Generalized Linear Model | 76.7% ± 7.2% | 71.7% ± 18.3% | 84.3% ± 15.1% | 75.4% ± 9.4% |
| Logistic Regression | 76.7% ± 7.2% | 71.7% ± 18.3% | 84.3% ± 15.1% | 75.4% ± 9.4% |
| Fast Large Margin | 74.3% ± 6.4% | 73.3% ± 18.1% | 78.3% ± 12.6% | 73.8% ± 7.9% |
| Deep Learning | 79.5% ± 7.5% | 71.7% ± 29.8% | 83.3% ± 15.6% | 71.5% ± 13.9% |
| Decision Tree | 72.9% ± 14.6% | 93.3% ± 14.9% | 66.3% ± 11.9% | 77.3% ± 12.5% |
| Random Forest | 80.0% ± 16.3% | 93.3% ± 14.9% | 79.0% ± 14.3% | 83.7% ± 6.1% |
| Gradient Boosted Trees | 78.6% ± 18.9% | 73.3% ± 36.5% | 81.0% ± 20.7% | 72.9% ± 26.3% |
| SVM | 73.3% ± 12.4% | 61.7% ± 28.6% | 79.3% ± 21.7% | 66.3% ± 21.5% |
| Classifier Type | Optimal Parameters | Accuracy [%] | Recall [%] | Precision [%] | F-Measure [%] |
|---|---|---|---|---|---|
| Random Forest | number of trees 100; criterion Gain Ratio; max depth 10; voting strategy: majority vote | 85.00% ± 12.30% | 85.0% ± 21.44% | 86.79% ± 12.88% | 85.89% ± 12.63% |
| Deep Learning | 3/100/100/2 architecture; the first three layers—neurons with Maxout activation functions, and the two output neurons have SoftMax activation functions. | 82.50% ± 12.08% | 91.67% ± 11.79% | 80.19% ± 15.40% | 85.55% ± 10.16% |
| Gradient Boosted Trees | number of trees: 50; max depth: 3; learning rate: 0.01 | 81.67% ± 16.57% | 80.00% ± 17.21% | 83.95% ± 18.02% | 81.93% ± 12.45% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Markova, V.; Markov, M.; Petrova, Z.; Filkova, S. Assessing the Impact of Prolonged Sitting and Poor Posture on Lower Back Pain: A Photogrammetric and Machine Learning Approach. Computers 2024, 13, 231. https://doi.org/10.3390/computers13090231
Markova V, Markov M, Petrova Z, Filkova S. Assessing the Impact of Prolonged Sitting and Poor Posture on Lower Back Pain: A Photogrammetric and Machine Learning Approach. Computers. 2024; 13(9):231. https://doi.org/10.3390/computers13090231
Chicago/Turabian StyleMarkova, Valentina, Miroslav Markov, Zornica Petrova, and Silviya Filkova. 2024. "Assessing the Impact of Prolonged Sitting and Poor Posture on Lower Back Pain: A Photogrammetric and Machine Learning Approach" Computers 13, no. 9: 231. https://doi.org/10.3390/computers13090231
APA StyleMarkova, V., Markov, M., Petrova, Z., & Filkova, S. (2024). Assessing the Impact of Prolonged Sitting and Poor Posture on Lower Back Pain: A Photogrammetric and Machine Learning Approach. Computers, 13(9), 231. https://doi.org/10.3390/computers13090231






