A Phase I Study of Unimolecular Pentavalent (Globo-H-GM2-sTn-TF-Tn) Immunization of Patients with Epithelial Ovarian, Fallopian Tube, or Peritoneal Cancer in First Remission
Abstract
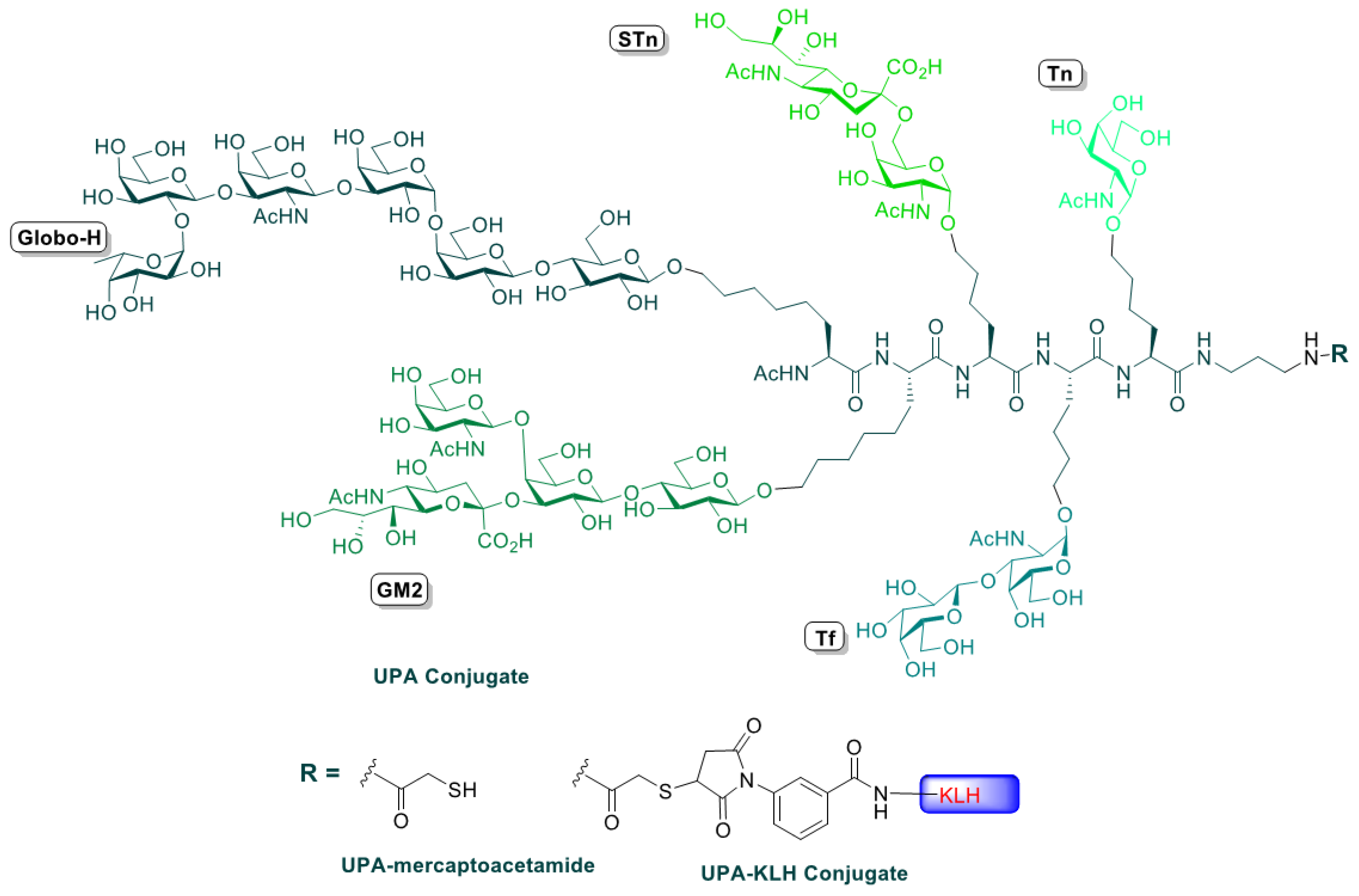
:1. Introduction
2. Experimental Section
2.1. Eligibility Criteria
2.2. Treatment Plan
2.3. Vaccine Preparation
2.4. Dose Adjustment and Toxicity Evaluation
2.5. Evaluation during Study
2.6. Statistical Considerations
2.7. Serological Analysis
3. Results
3.1. Patient Characteristics
3.2. Adverse Events
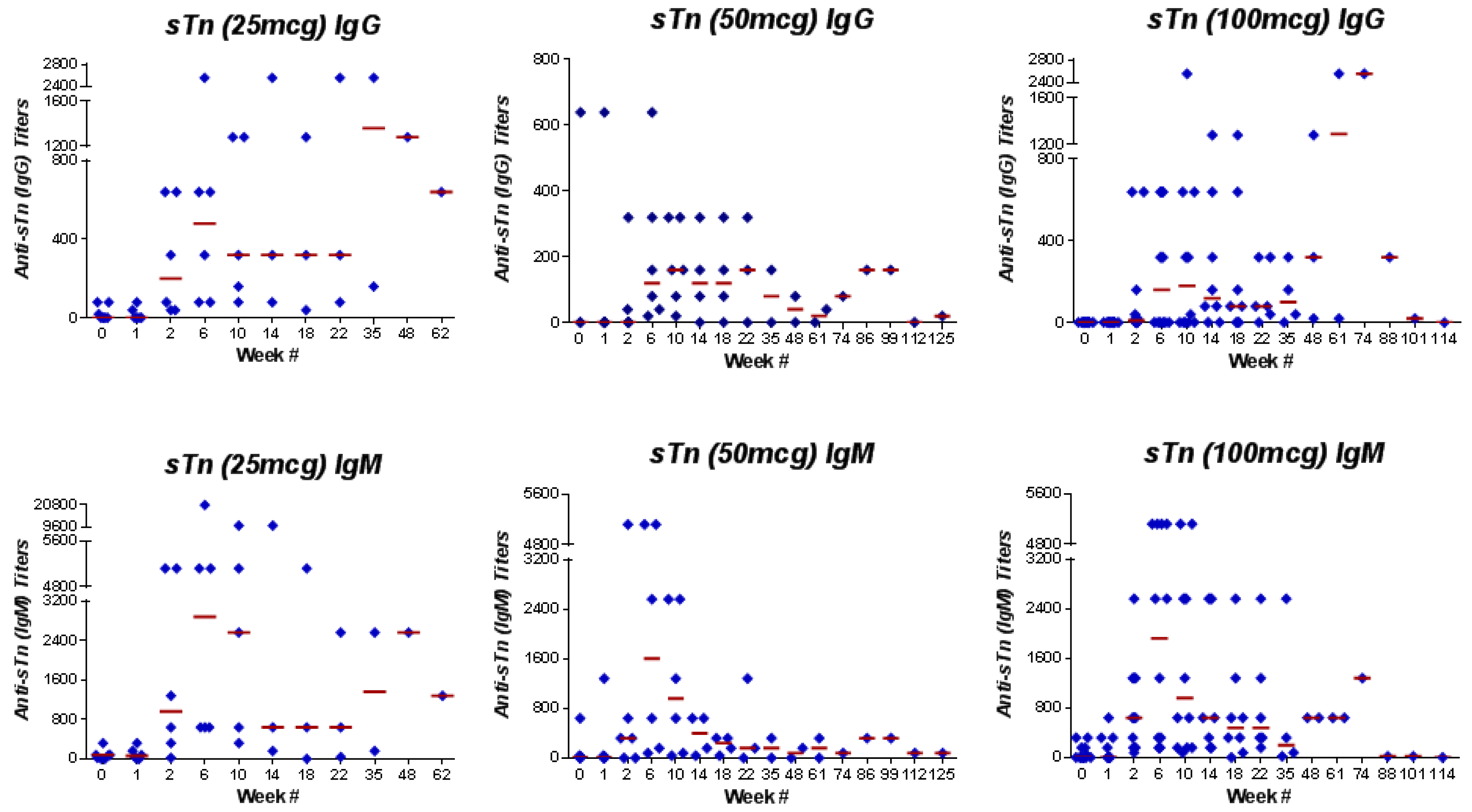
3.3. Immune Response
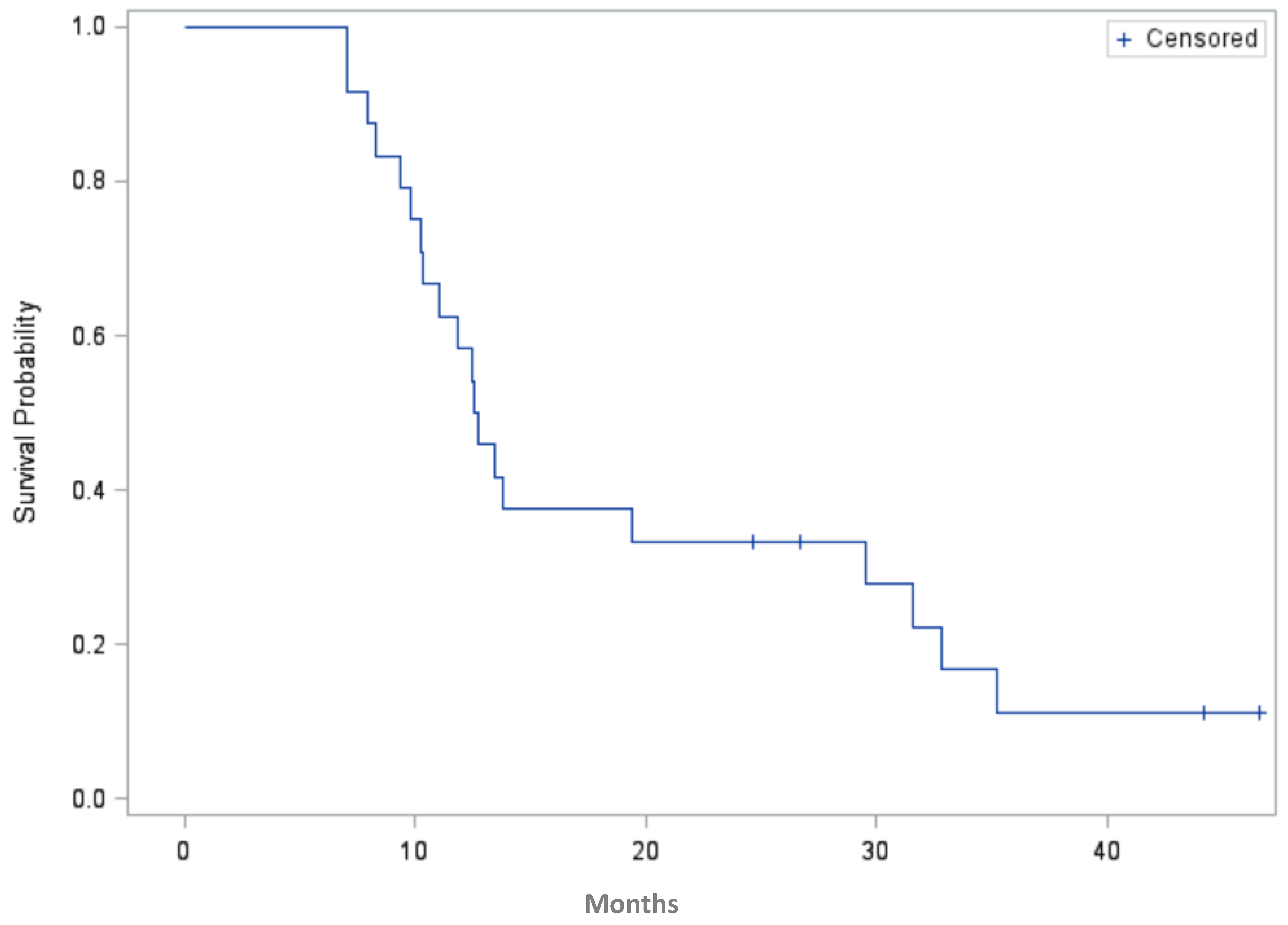
3.4. Progression-Free Survival
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Financial Support
Conflicts of Interest
References
- Markman, M.; Markman, J.; Webster, K.; Zanotti, K.; Kulp, B.; Peterson, G.; Belinson, J. Duration of response to second-line, platinum-based chemotherapy for ovarian cancer: Implications for patient management and clinical trial design. J. Clin. Oncol. 2004, 22, 3120–3125. [Google Scholar] [CrossRef] [PubMed]
- Syrios, J.; Banerjee, S.; Kaye, S.B. Advanced epithelial ovarian cancer: From standard chemotherapy to promising molecular pathway targets—where are we now? Anticancer Res. 2014, 34, 2069–2077. [Google Scholar] [PubMed]
- Sabbatini, P.; Spriggs, D.R. Consolidation for ovarian cancer in remission. J. Clin. Oncol. 2006, 24, 537–539. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Zhang, H.S.; Cordon-Cardo, C.; Ragupathi, G.; Livingston, P.O. Selection of tumor antigens as targets for immune attack using immunohistochemistry: Protein antigens. Clin. Cancer Res. 1998, 4, 2669–2676. [Google Scholar] [PubMed]
- Ragupathi, G.; Liu, N.X.; Musselli, C.; Powell, S.; Lloyd, K.; Livingston, P.O. Antibodies against tumor cell glycolipids and proteins, but not mucins, mediate complement-dependent cytotoxicity. J. Immunol. 2005, 174, 5706–5712. [Google Scholar] [CrossRef] [PubMed]
- Federici, M.F.; Kudryashov, V.; Saigo, P.E.; Finstad, C.L.; Lloyd, K.O. Selection of carbohydrate antigens in human epithelial ovarian cancers as targets for immunotherapy: Serous and mucinous tumors exhibit distinctive patterns of expression. Int. J. Cancer 1999, 81, 193–198. [Google Scholar] [CrossRef]
- Zhang, S.; Zhang, H.S.; Cordon-Cardo, C.; Reuter, V.E.; Singhal, A.K.; Lloyd, K.O.; Livingston, P.O. Selection of tumor antigens as targets for immune attack using immunohistochemistry: II. Blood group related antigens. Int. J. Cancer 1997, 73, 50–60. [Google Scholar] [CrossRef]
- Gilewski, T.; Ragupathi, G.; Bhuta, S.; Williams, L.J.; Musselli, C.; Zhang, X.F.; Bornmann, W.G.; Spassova, M.; Bencsath, K.P.; Panageas, K.S.; et al. Immunization of metastatic breast cancer patients with a fully synthetic globo H conjugate: A phase I trial. Proc. Natl. Acad. Sci. USA 2001, 98, 3270–3275. [Google Scholar] [CrossRef] [PubMed]
- Chapman, P.B.; Morrissey, D.M.; Panageas, K.S.; Hamilton, W.B.; Zhan, C.; Destro, A.N.; Williams, L.; Israel, R.J.; Livingston, P.O. Induction of antibodies against GM2 ganglioside by immunizing melanoma patients using GM2-keyhole limpet hemocyanin + QS21 vaccine: A dose-response study. Clin. Cancer Res. 2000, 6, 874–879. [Google Scholar] [PubMed]
- Sabbatini, P.J.; Kudryashov, V.; Ragupathi, G.; Danishefsky, S.J.; Livingston, P.O.; Bornmann, W.; Spassova, M.; Zatorski, A.; Spriggs, D.; Aghajanian, C. Immunization of ovarian cancer patients with a synthetic Lewis(y)-protein conjugate vaccine: A phase 1 trial. Int. J. Cancer 2000, 87, 79–85. [Google Scholar] [CrossRef]
- Kagan, E.; Ragupathi, G.; Yi, S.S.; Reis, C.A.; Gildersleeve, J.; Kahne, D.; Clausen, H.; Danishefsky, S.J.; Livingston, P.O. Comparison of antigen constructs and carrier molecules for augmenting the immunogenicity of the monosaccharide epithelial cancer antigen Tn. Cancer Immunol. Immunother. 2005, 54, 424–430. [Google Scholar] [CrossRef] [PubMed]
- Slovin, S.F.; Ragupathi, G.; Musselli, C.; Fernandez, C.; Diani, M.; Verbel, D.; Danishefsky, S.; Livingston, P.; Scher, H.I. Thomsen-Friedenreich (TF) antigen as a target for prostate cancer vaccine: Clinical trial results with TF cluster (c)-KLH plus QS21 conjugate vaccine in patients with biochemically relapsed prostate cancer. Cancer Immunol. Immunother. 2005, 54, 694–702. [Google Scholar] [CrossRef] [PubMed]
- Sabbatini, P.J.; Ragupathi, G.; Hood, C.; Aghajanian, C.A.; Juretzka, M.; Iasonos, A.; Hensley, M.L.; Spassova, M.K.; Ouerfelli, O.; Spriggs, D.R.; et al. Pilot study of a heptavalent vaccine-keyhole limpet hemocyanin conjugate plus QS21 in patients with epithelial ovarian, fallopian tube, or peritoneal cancer. Clin. Cancer Res. 2007, 13, 4170–4177. [Google Scholar] [CrossRef] [PubMed]
- Ragupathi, G.; Koide, F.; Livingston, P.O.; Cho, Y.S.; Endo, A.; Wan, Q.; Spassova, M.K.; Keding, S.J.; Allen, J.; Ouerfelli, O.; et al. Preparation and evaluation of unimolecular pentavalent and hexavalent antigenic constructs targeting prostate and breast cancer: A synthetic route to anticancer vaccine candidates. J. Am. Chem. Soc. 2006, 128, 2715–2725. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; Wan, Q.; Lee, D.; Yang, G.; Spassova, M.K.; Ouerfelli, O.; Ragupathi, G.; Damani, P.; Livingston, P.O.; Danishefsky, S.J. From synthesis to biologics: Preclinical data on a chemistry derived anticancer vaccine. J. Am. Chem. Soc. 2009, 131, 9298–9303. [Google Scholar] [CrossRef] [PubMed]
- Ruiz van Haperen, V.W.; Veerman, G.; Boven, E.; Noordhuis, P.; Vermorken, J.B.; Peters, G.J. Schedule dependence of sensitivity to2′,2′-difluorodeoxycytidine in relation to accumulation and retention of its triphophate in solid tumor cell lines and solid tumors. Biochem. Pharmacol. 1994, 48, 1327–1339. [Google Scholar] [CrossRef]
- Yao, T.J.; Begg, C.B.; Livingston, P.O. Optimal sample size for a series of pilot trials of new agents. Biometrics 1996, 52, 992–1001. [Google Scholar] [CrossRef] [PubMed]
| Variable | Number of Patients (%) |
|---|---|
| Median age (Range) | 54 years (36–68) |
| FIGO * Stage at diagnosis | |
| III | 18 (75%) |
| IV | 6 (25%) |
| Cancer type | |
| Ovarian | 20 (83%) |
| Primary Peritoneal | 1 (4%) |
| Fallopian Tube | 3 (13%) |
| Median Karnofsky Performance Status (range) | 90 (80–100) |
| Race | |
| Caucasian | 22 (92%) |
| Asian | 2 (8%) |
| Histologic subtype | |
| High-grade serous carcinoma | 22 (92%) |
| Clear cell | 2 (8%) |
| Treatment-Related Adverse Events | Grade 2 n (%) | Grade 3 n (%) | Grade 4 n (%) |
|---|---|---|---|
| Injection site reaction | 2 (8%) | 0 | 0 |
| Hyperglycemia | 2 (8%) | 0 | 0 |
| Hypoglycemia | 1 (4%) | 0 | 0 |
| Thrombocytopenia | 1 (4%) | 0 | 0 |
| Neutropenia | 1 (4%) | 0 | 0 |
| Leukopenia | 1 (4%) | 0 | 0 |
| Elevated alanine aminotransferase | 1 (4%) | 0 | 0 |
| Fever | 1 (4%) | 0 | 0 |
| Antigen | IgM Response n (%) | IgG Response n (%) |
|---|---|---|
| GM2 | 3 (25%) | 2 (17%) |
| Globo-H | 1 (8%) | 7 (58%) |
| Tn | 7 (58%) | 10 (83%) |
| TF | 8 (67%) | 3 (25%) |
| sTn | 11 (92%) | 8 (67%) |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
O’Cearbhaill, R.E.; Ragupathi, G.; Zhu, J.; Wan, Q.; Mironov, S.; Yang, G.; Spassova, M.K.; Iasonos, A.; Kravetz, S.; Ouerfelli, O.; et al. A Phase I Study of Unimolecular Pentavalent (Globo-H-GM2-sTn-TF-Tn) Immunization of Patients with Epithelial Ovarian, Fallopian Tube, or Peritoneal Cancer in First Remission. Cancers 2016, 8, 46. https://doi.org/10.3390/cancers8040046
O’Cearbhaill RE, Ragupathi G, Zhu J, Wan Q, Mironov S, Yang G, Spassova MK, Iasonos A, Kravetz S, Ouerfelli O, et al. A Phase I Study of Unimolecular Pentavalent (Globo-H-GM2-sTn-TF-Tn) Immunization of Patients with Epithelial Ovarian, Fallopian Tube, or Peritoneal Cancer in First Remission. Cancers. 2016; 8(4):46. https://doi.org/10.3390/cancers8040046
Chicago/Turabian StyleO’Cearbhaill, Roisin E., Govind Ragupathi, Jianglong Zhu, Qian Wan, Svetlana Mironov, Guangbin Yang, Maria K. Spassova, Alexia Iasonos, Sara Kravetz, Ouathek Ouerfelli, and et al. 2016. "A Phase I Study of Unimolecular Pentavalent (Globo-H-GM2-sTn-TF-Tn) Immunization of Patients with Epithelial Ovarian, Fallopian Tube, or Peritoneal Cancer in First Remission" Cancers 8, no. 4: 46. https://doi.org/10.3390/cancers8040046
APA StyleO’Cearbhaill, R. E., Ragupathi, G., Zhu, J., Wan, Q., Mironov, S., Yang, G., Spassova, M. K., Iasonos, A., Kravetz, S., Ouerfelli, O., Spriggs, D. R., Danishefsky, S. J., & Sabbatini, P. J. (2016). A Phase I Study of Unimolecular Pentavalent (Globo-H-GM2-sTn-TF-Tn) Immunization of Patients with Epithelial Ovarian, Fallopian Tube, or Peritoneal Cancer in First Remission. Cancers, 8(4), 46. https://doi.org/10.3390/cancers8040046






